Psychiatry and medicine Introduction Thousands years ago people




- Slides: 30
Psychiatry and medicine
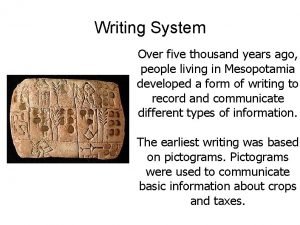
Introduction. • Thousands years ago, people of Mesopotamia ( the land of two rivers ) used to treat their patients with magic, chemicals extracted from herbs, if no help by prayers & begging for cure from “ Gods. ” • They used to have many Gods ; God of medicine ( Nun-asu ) , God of knowledge ( Nun-Keseda who was represented by as a stick & snake. • They use to differentiate between the magician ( Aspu ) & the doctor ( Asu. ( • Many prescriptions were found in the ruins of the Iraqi civilization, written on bars of clay in old Iraqi script ( cuneiform writing of Sumer. (
Introduction ( cont(. • Abn-sina, during Abbasian times, was the first to describe the effect of psyche on the body ( what is known as psychosomatic now a day ) in the case of young man who was emaciated because he couldn't marry the girl he loved, by monitoring his pulse while mentioning special places in the town, the pulse, he noticed, increased while approaching the house of his love due to the emotion it stirred. • Al-razi said that doctors must always persuade patients that they would be cured from their sufferings. . • ﻋﻠﻰ ﺍﻟﻄﺒﻴﺐ ﺃﻦ ﻳﻮﻫﻢ ﺍﻟﻤﺮﻳﺾ ﺩﺍﺋﻤﺎ ﺑﺎﻟﺸﻔﺎﺀ
Psychiatry and Medicine • Physical & psychiatric symptoms occur commonly together in patients who consult doctors. • Psychiatric disorder often presents with physical complaints. • Psychological symptoms are a frequent consequence of acute & chronic organic illness. • At least a quarter of patients with physical complaints can be diagnosed as suffering from psychiatric disorder.
Associations between physical and psychiatric disorder. • Chance association: physical & psychiatric disorders are both common. • Psychological factors as a cause of physical disorder. • Psychiatric complications of physical illness & its treatment ( e. g. heart disease, delirium & dementia. ( • Some psychiatric disorders can cause physical symptoms ( e. g. palpitation in an anxiety disorder. ( • Physical complications of psychiatric disorder ( e. g. deliberate self- harm, eating disorders. (

Epidemiology • Unexplained physical symptoms are among the commonest reasons for seeking treatment & are often due to psychiatric disorder. • Psychological problems are especially frequent in accident & emergency , gynaecological & medical out-patient clinics, medical & geriatric wards. • Affective disorders are common in younger women, organic mental disorders in the elderly & drinking problems in young men. • About a quarter of patients in medical wards have a psychiatric disorder of some kind. . • 15% of o. p. with definite medical diagnosis have an associated psychiatric disorder. • . 40% of those with no medical diagnosis have a psychiatric disorder
Psychological complications of physical illness. • Most people are resilient when ill and carry on without undue distress. • About a quarter of cases may have substantial psychological impact. • Disturbances of mental state, which may be severe enough to be classified as psychiatric disorder. • Impaired quality of life. • Unnecessarily poor physical outcome. • Adverse effects on family and others. • Inappropriate or excessive consultation. • Poor compliance with treatment.
• Common psychiatric disorders in the physically ill • More common ( adjustment, depressive, anxiety disorders & delirium. ( • Less common ( somatoform disorders, dementia, panic & phobic disorder, p. t. s. d. , mania, schizophrenia & delusional disorders. • The usual reaction to acute illness ( anxiety, depression, delirium & complete or partial denial of the diagnosis. ( • In disabling chronic illness ( adjustment, anxiety & depressive disorders. ( • Major medical & surgical treatments are also important causes of psychological symptoms. • Drug treatment ( depression, delirium, psychotic symptoms & elation. ( • Chemotherapy of cancer ( cause very great distress. ( • Radiotherapy ( anxiety & depression. ( • Surgical treatment ( anxiety before & after operation. (
Medications reported to cause depression. • Cardiovascular drugs ( Alpha-methyldopa, Reserpin, Propranolol, Guanithidine, Clonidine, Thiazide diuretics, Digitalis. ( • Hormones ( Oral contraceptives, A. C. T. H. , Anabolic steroids. ( • Psychotropics ( Benzodiazepines, Neurotropics. ( • Anticancer drugs ( Cyclserine. ( • Anti-inflammatory ( NSAIDs. ( • Anti-infective agents ( Ethambutol, Sulfonamides. ( • Others ( Cocaine withdrawal, Amphetamines, L-dopa, Cimetidine, Rantidine, Disulfiram, Metoclopramide. (

Medication reported to cause other psychiatric symptoms. • Delirium ( CNS depressants, Digoxin, Cimetidine & Anti-cholinergic drugs. ( • Psychotic symptoms Hallucinogenic drugs, Appetite suppressants, Sympathomimetic drugs & Corticosteroids. ( • Elation ( Anti-depressants, Corticosteroids, Izoniazide & Anti- cholinergic drugs. (
Determinants of the psychological impact of physical illness. • Most anxiety & depression following physical illness is part of a psychological reaction. • Several medical disorders also cause anxiety & depressive symptoms directly ( Parkinson’s disease, stroke, infections, endocrine disorders & malignancy. ( • Illness factors ( pain, threat to life, course, duration & disability. ( • Treatment factors ( side effects, uncertainty of outcome & self-care demands. ( • Patients factors ( psychological vulnerability, social circumstances, other stresses & reactions of others. ( • Factors associated with high risk of psychiatric problems include ( severity of illness, unpleasant treatment & vulnerable patients. (
Psychiatric assessment of a physically ill patient. • Psychiatric assessment is similar to that of psychiatric patient except that it requires knowledge of the nature and prognosis of the physical illness. • Screening questions for psychiatric symptoms ( e. g. have you been very worried about your health? How have you been sleeping? Etc. (. • Screening questions about the psychiatric history. • Screening question about social factors. • Observation of the patient ( mood & behaviour during the interview. ( • If emotional disorder is suspected , take a full psychiatric history.
Management • Some emotional distress is an almost inevitable accompaniment of the stress of physical illness & its treatment, it can be often reduced by appropriate treatment. Advice, explanation & discussion. • Treatment of any specific psychiatric disorder is similar to that of physically healthy person, particular attention should be paid to the side effect of the psychotropic drugs. • Adjustment disorder needs further opportunity for problem solving & follow-up. • Anxiety disorder, brief treatment with a benzodiazepine can be helpful. • Depressive disorder can be helped by support or problemsolving counselling, but more severe requires antidepressant medication.
Psychological problem associated with cancer • The doctor needs to set aside adequate time to explain the prognosis and what treatment can be offered • Emotional reaction on diagnosis or recurrence is manifested by severe distress in the form of an adjustment disorder or, in over a third of patients, a psychiatric disorder ( anxiety & depression. ( • Emotional reactions to surgery, radiotherapy, or chemotherapy. • Anticipatory nausea with chemotherapy. • Organic mental disorder due to metastasis, metabolic changes, or chemotherapy. • Neuropsychiatric syndrome. • Depressive & other reactions to terminal illness.
Psychological problem associated with accidents & trauma. • Psychological factors are important contributory causes of accidents ( e. g. overactivity & conduct disorder in children, alcohol & drug abuse in young adults, and organic mental disorders in the elderly. • Following accidents, anxiety & depressive symptoms are common especially when there is injury to the head. • Some road accident victims develop phobic travel anxiety or, less frequently PTSD. • Compensation neurosis ( or accident neurosis ) has been used for physical or mental symptoms caused psychologically and occurring when there is an unsettled claim for compensation. • Prolonging the disability.
Psychological problems associated with myocardial infarction • The sudden onset of severe chest pain frequently causes anxiety. • In severe infarcts, delirium is frequent. • A sizable minority of patients show denial with little distress, if denial persist it may lead to non-compliant with treatment. • In the weeks after an infarct patients frequently describe depressive symptoms. • A few patients develop a depressive illness and this is associated with increased mortality in the ensuing month. • Cardiac aftercare and rehabilitation concentrates on physical fitness should take into account anxiety about physical activity, sexual problems as well as any depressive disorder.
• • • Psychological problems associated with endocrine disorders Diabetes: psychiatric disorders especially eating disorder. In advanced cases, cerebrovascular diseases, poor glycaemia control may lead to cognitive impairment. Hyperthyroidism: restlessness, irritability, and distractibility may resemble an anxiety disorder. Medical treatment usually results in improvement in the psychological symptoms. Hypothyroidism: in infancy leads to retardation. In adult leads to mental slowness, apathy, poor memory and occasionally organic mental disorder or severe depression. Paranoid symptoms are common. Early treatment usually reverse the psychiatric symptoms. Cushing’s syndrom: depressive symptoms are frequent Corticosteroids treatment: depression but a manic disorder is more common. Phaeochromocytoma: episodic attacks of anxiety with blushing, sweating, palpitation, headache, and raised blood pressure.
Psychological problems associated with movement disorders • Parkinson’s disease: there is increase incidence of dementia & depression. Anticholinergics may cause excitement, delusions and hallucinations. Levodopa may cause delirium. • Spasmodic torticollis: psychological factors can increase the symptoms, however, it is more likely to have organic cause. • Tics: they are more common in childhood than in adults. more common in boys than girls. worsened by anxiety. • Writer’s and occupational cramps: these conditions are thought to be psychogenic.
Some specific symptoms and syndromes. • Chronic fatigue syndrome. • Chronic pain. • Multiple chronic symptoms ( somatization disorder. ( • Headache & atypical facial pain. • Non-cardiac chest pain & benign palpitations. • Irritable bowel syndrome & abdominal pain. • Dissociative & conversion disorders. Hysteria • Self-inflicted & simulated illness. Factitious disorder. Malingering.
Management of unexplained physical symptoms • Presenting for the first time: Appropriate physical investigations. Possible psychological causes. • Treatment: Acknowledge reality of the symptoms. treat any psychiatric disorder. • Persistent symptoms: review the need for further investigations. Take full psychiatric history. discuss with relatives. Cognitive therapy. • Failure to improve: physical reassessment. consider referral to a psychiatrist or clinical psychologist.
Management of multiple somatic symptoms. • Take full history & interview relatives. • Review medical notes; discuss with doctors currently involved. Attempt to simplify the medical care. perform only essential investigations. Minimize the use of psychotropic drugs. • Arrange brief regular appointments. • Avoid repeating reassurance about the symptoms • Focus on coping with disability & psychosocial problems. • Encourage gradual return to normal activities.
Treatment of chronic pain. • Acknowledge the reality of the symptoms. • Explain the origin of the pain & discuss the patient’s concern. • Treat any cause if possible. • Agree a regime of analgesics with the patient. • Discuss how the patient might cope better with the pain. • Involve the family in the management plan. • Consider antidepressant medication.
Psychiatric services in general hospital • In large hospital psychiatric advice is needed from a special consultation liaison service. • Emergency service for patients admitted after deliberate self-harm. • Emergency consultation for other accident and emergency department attenders. • Consultation service for in-patients. • Out-patient care for patients referred with psychiatric complications of physical illness or functional somatic symptoms. • Regular liaison visits to selected medical, surgical and gynaecological units in which psychiatric problems are especially common ( e. g. neurology, renal dialysis, terminal care. (
Psychiatric emergencies in general hospital practice. • Thorough clinical assessment, like any other medical emergency. • Establish a good relationship with the patient, to take a brief history, observe behaviour, and assess the mental state. • When the patient’s behaviour is very disturbed, the history may be taken from other people such as relatives or nurses. • Mistakes will be avoided and time saved if the assessment is as complete as the circumstances permit.
Acute disturbed behaviour and violence. • Delirium, schizophrenia, mania, agitated depression and alcohol & drug-related problems are the most common. • The first task is to assess the risk of violence. • Arrange for adequate help to be available. • The doctor should appear calm and helpful, avoid confrontation, and try to persuade the patient to talk about the reason for his anger. • If the patient responds so aggressively, restrain should be accomplished quickly by an adequate number of people. • Help of the police may be required for patient thought to possess any of offensive weapon.
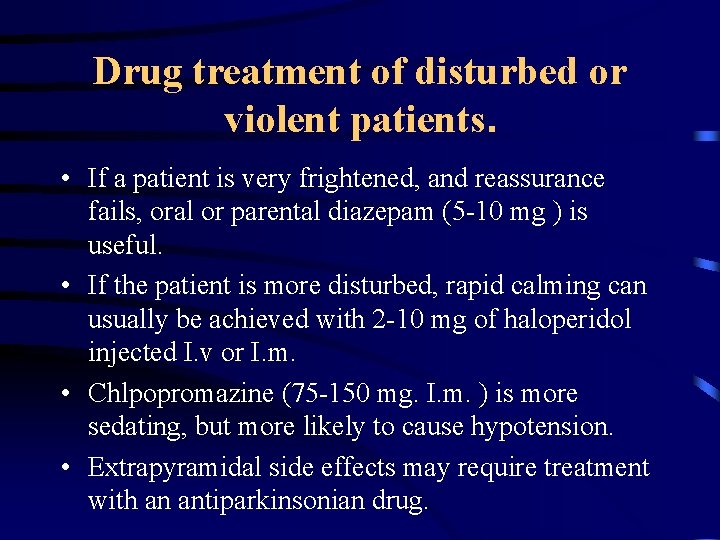
Drug treatment of disturbed or violent patients. • If a patient is very frightened, and reassurance fails, oral or parental diazepam (5 -10 mg ) is useful. • If the patient is more disturbed, rapid calming can usually be achieved with 2 -10 mg of haloperidol injected I. v or I. m. • Chlpopromazine (75 -150 mg. I. m. ) is more sedating, but more likely to cause hypotension. • Extrapyramidal side effects may require treatment with an antiparkinsonian drug.

Psychiatric aspect of obestetrics and gynaecology. • Pregnancy ( unwanted pregnancy, hyperemesis gravidarum, pseudocyesis & couvade syndrome. ( • Loss of a fetus & stillbirth. • Post-partum mental disorders ( maternity ‘ blues’, puerpural depression & psychosis. ( • Menstrual disorders ( premenstrual syndrome, the menopause & hysterectomy. (

The impact of culture on physical illness. • Consultation: - with the increasing health services available, people of the Emirates like other Arab countries, started to attend hospital & other health facilities seeking medical treatment. Islam believers know that illnesses are both God creation & God who will cure. The doctors are intermediate, try to ease people sufferings until cure or death. • Interview: - Emirates like other developing countries are keen on expressing their suffering, but few found it difficult & may even think that
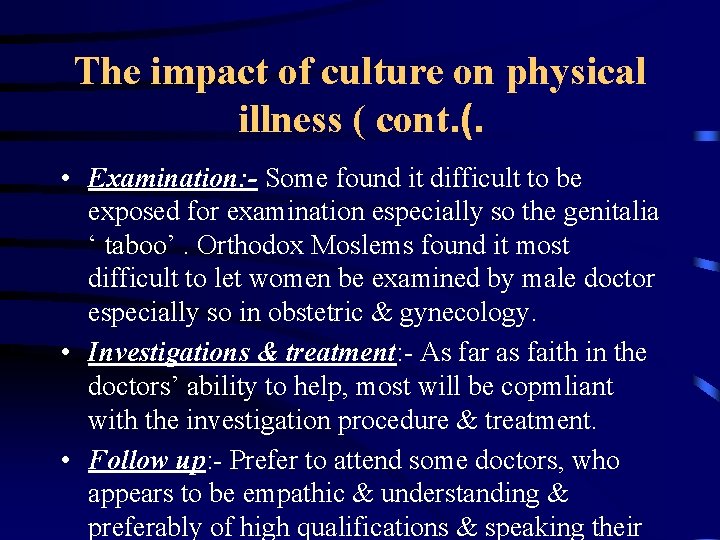
The impact of culture on physical illness ( cont. (. • Examination: - Some found it difficult to be exposed for examination especially so the genitalia ‘ taboo’. Orthodox Moslems found it most difficult to let women be examined by male doctor especially so in obstetric & gynecology. • Investigations & treatment: - As far as faith in the doctors’ ability to help, most will be copmliant with the investigation procedure & treatment. • Follow up: - Prefer to attend some doctors, who appears to be empathic & understanding & preferably of high qualifications & speaking their
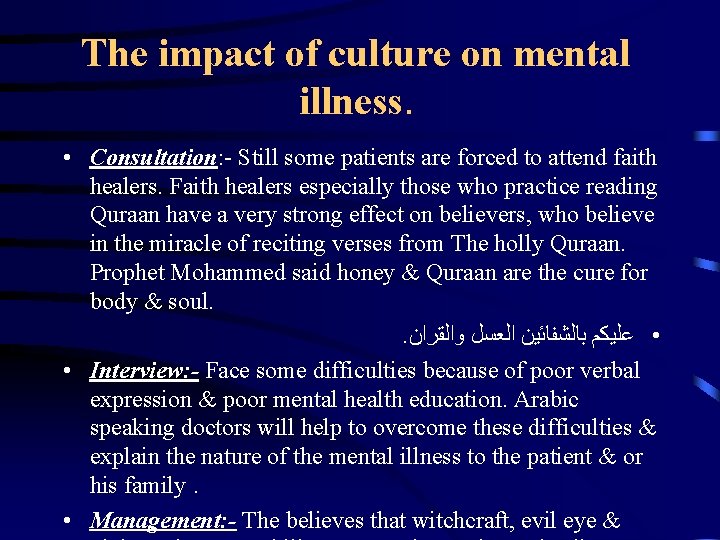
The impact of culture on mental illness. • Consultation: - Still some patients are forced to attend faith healers. Faith healers especially those who practice reading Quraan have a very strong effect on believers, who believe in the miracle of reciting verses from The holly Quraan. Prophet Mohammed said honey & Quraan are the cure for body & soul. . • ﻋﻠﻴﻜﻢ ﺑﺎﻟﺸﻔﺎﺋﻴﻦ ﺍﻟﻌﺴﻞ ﻭﺍﻟﻘﺮﺍﻥ • Interview: - Face some difficulties because of poor verbal expression & poor mental health education. Arabic speaking doctors will help to overcome these difficulties & explain the nature of the mental illness to the patient & or his family. • Management: - The believes that witchcraft, evil eye &
 How long is “four score and seven years”?
How long is “four score and seven years”? Despite being thousands of years old
Despite being thousands of years old Four score and seven years ago
Four score and seven years ago Compare and contrast fashion today with twenty years ago
Compare and contrast fashion today with twenty years ago How long is four score and seven years?
How long is four score and seven years? Every year thousands
Every year thousands Eight years ago today
Eight years ago today You can easily forget how different life was 50 years ago
You can easily forget how different life was 50 years ago Saturn 4 billion years ago
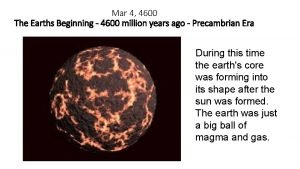
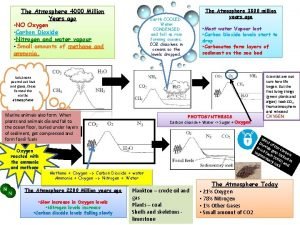
Saturn 4 billion years ago Earth 4600 million years ago
Earth 4600 million years ago Earth 200 million years ago
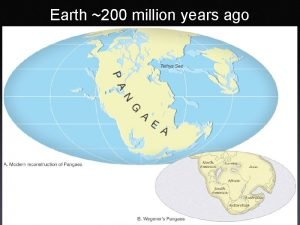
Earth 200 million years ago Marbled crested lizard
Marbled crested lizard Halloween 2000 years ago
Halloween 2000 years ago Dinosaurs lived millions of years ago what did they eat
Dinosaurs lived millions of years ago what did they eat Technicom 15 years ago as a small
Technicom 15 years ago as a small 10 million years ago
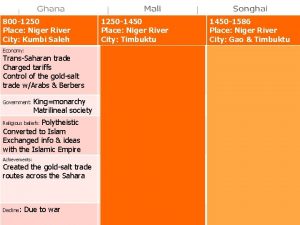
10 million years ago Africa 1000 years ago
Africa 1000 years ago Australia 50 000 years ago
Australia 50 000 years ago 125 years ago today
125 years ago today 4 000 years ago
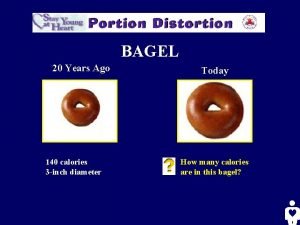
4 000 years ago One cup spaghetti calories
One cup spaghetti calories Family life 100 years ago
Family life 100 years ago Why did the barley sign change shape?
Why did the barley sign change shape? 4000 million
4000 million Shenzhen 30 years ago
Shenzhen 30 years ago Once upon a king
Once upon a king Two years ago jenny was diagnosed with schizophrenia
Two years ago jenny was diagnosed with schizophrenia Goat years to human years
Goat years to human years 300 solar years to lunar years
300 solar years to lunar years Radical psychiatry sociology
Radical psychiatry sociology Assessment skills
Assessment skills