Psychiatric Nursing Mohammed Z Aish Master community mental

- Slides: 55
Psychiatric Nursing Mohammed Z Aish Master community mental health
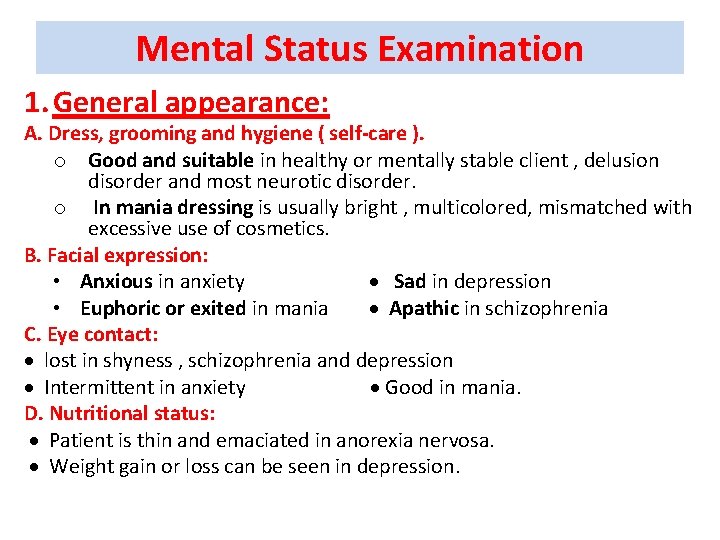
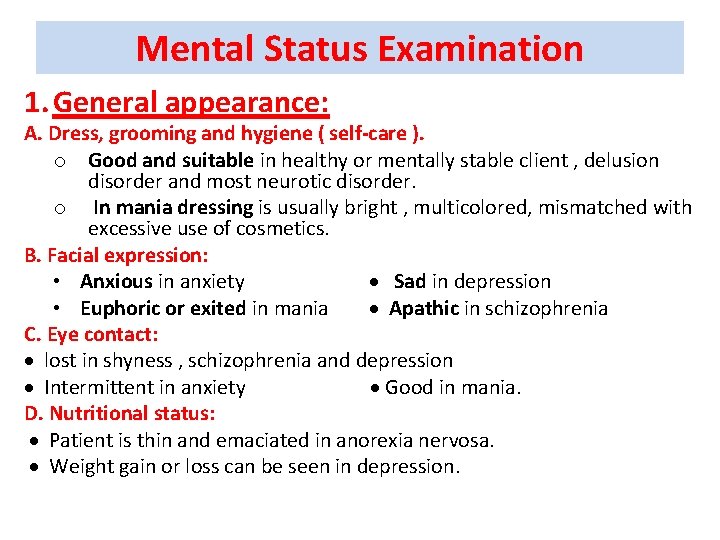
Mental Status Examination 1. General appearance: A. Dress, grooming and hygiene ( self-care ). o Good and suitable in healthy or mentally stable client , delusion disorder and most neurotic disorder. o In mania dressing is usually bright , multicolored, mismatched with excessive use of cosmetics. B. Facial expression: • Anxious in anxiety Sad in depression • Euphoric or exited in mania Apathic in schizophrenia C. Eye contact: lost in shyness , schizophrenia and depression Intermittent in anxiety Good in mania. D. Nutritional status: Patient is thin and emaciated in anorexia nervosa. Weight gain or loss can be seen in depression.
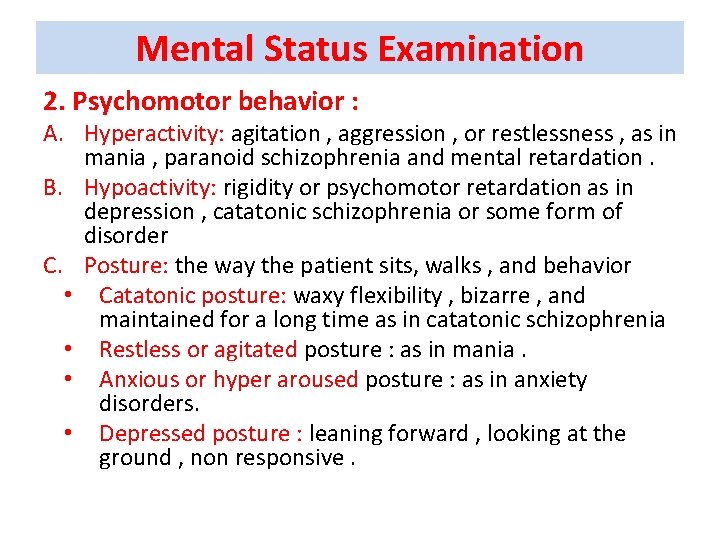
Mental Status Examination 2. Psychomotor behavior : A. Hyperactivity: agitation , aggression , or restlessness , as in mania , paranoid schizophrenia and mental retardation. B. Hypoactivity: rigidity or psychomotor retardation as in depression , catatonic schizophrenia or some form of disorder C. Posture: the way the patient sits, walks , and behavior • Catatonic posture: waxy flexibility , bizarre , and maintained for a long time as in catatonic schizophrenia • Restless or agitated posture : as in mania. • Anxious or hyper aroused posture : as in anxiety disorders. • Depressed posture : leaning forward , looking at the ground , non responsive.
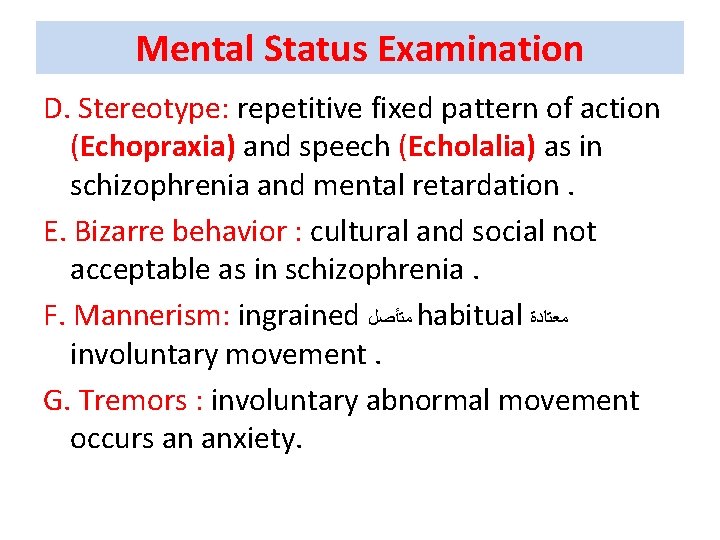
Mental Status Examination D. Stereotype: repetitive fixed pattern of action (Echopraxia) and speech (Echolalia) as in schizophrenia and mental retardation. E. Bizarre behavior : cultural and social not acceptable as in schizophrenia. F. Mannerism: ingrained ﻣﺘﺄﺼﻞ habitual ﻣﻌﺘﺎﺩﺓ involuntary movement. G. Tremors : involuntary abnormal movement occurs an anxiety.
Mental Status Examination 3. Attitude: client interaction with mental health team that may be : • Cooperative : as in anxiety disorders and residual schizophrenia. • Resistive: as in acute psychosis and personality disorder. • Aggressive: as in mania and paranoid schizophrenia.
Mental Status Examination 4. Speech : A. Quantity : • Poverty in content : as in depression and catatonic schizophrenia. B. Quality: • Monotonous , soft and slow in depression. • Talkative , stereotyped , pressured and loud in mania. • Incoherent in schizophrenia. • Slurred and dysrythmic in anxiety disorder. • Repetitious as in dementia and organic brain disorder • Slurred speech ( dysrythmic ) can be seen in organic brain disorders.
Mental Status Examination 5. Mood: Is the subjective sustained internal emotional state as reported by the patient. Ø Euthymic mood: normal range with absence of depressed or elevated mood. Ø Dysphoric mood: feeling unpleasant as in dysthymia. Ø Depressed mood : feeling of sadness as in depression. Ø Irritable mood : easily annoyed anger as in mania. Ø Euphoric mood : intense elation with feeling of grandeur as in mania. Ø Anxious mood : feeling of fear of unknown , tension , and expecting the worst. Ø Mood swing : between euphoria and depressed as in bipolar disorder. Ø Anhedonia : loss of interest in all pleasurable activities as in depression.
Mental Status Examination 6. Affect: The external emotional expression of feeling as observed by others. Ø Appropriate affect: Normal condition in which the emotional tone is in harmony with the accompanied idea. Ø Inappropriate affect: Dis-harmony between the emotional tone and the as in schizophrenia. Ø Flat affect: absence of any signs of affective expression as in schizophrenia. Ø Blunt affect: severe reduction in the external feeling tones as in schizophrenia. Ø Labile affect: rapid and abrupt changes in the external emotional tones unrelated to external stimuli as in senile dementia.
Mental Status Examination 7. Perception: Mental process by which sensory stimuli are brought to awareness and transferred to psychological information A. Hallucination: False sensory perception not associated with real external stimuli and indicate psychotic disturbances when it is associated with impairment in reality testing. Ø Auditory : False perception of sound usually voice as in psychotic disorder. Ø Visual: False perception of sight of people or flashes of light as organic brain disorder. Ø Olfactory: False perception of smell as in organic disorders. Ø Gustatory : False perception of taste as unpleasant taste after seizure Ø Tactile: False perception of touch as in amputated (phantom) limb , and formication ﺍﻟﺘﻨﻤﻴﻞ in drug abuse.
Mental Status Examination B. Illusion: Misperception of real external sensory stimuli as in anxiety disorder. C. Depersonalization: Subjective sense of being unreal , strange or unfamiliar to onset as in panic disorder. D. De-realization: Subjective sense that the environment is change or unreal as in panic disorder.
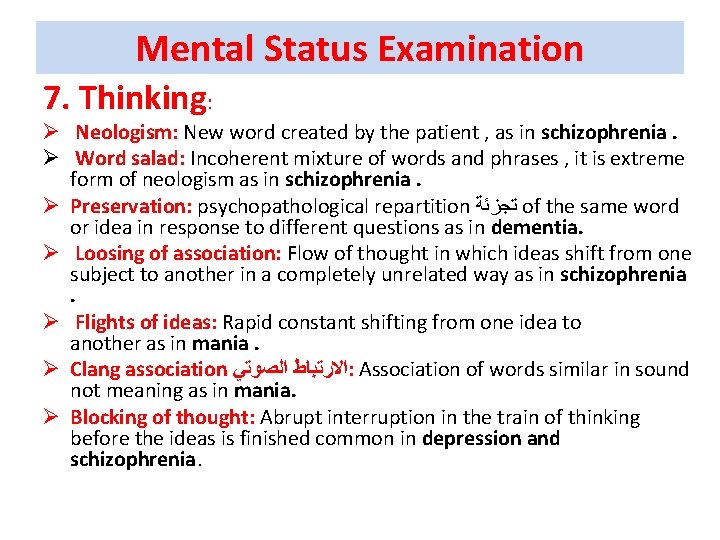
Mental Status Examination 7. Thinking: Ø Neologism: New word created by the patient , as in schizophrenia. Ø Word salad: Incoherent mixture of words and phrases , it is extreme form of neologism as in schizophrenia. Ø Preservation: psychopathological repartition ﺗﺠﺰﺋﺔ of the same word or idea in response to different questions as in dementia. Ø Loosing of association: Flow of thought in which ideas shift from one subject to another in a completely unrelated way as in schizophrenia . Ø Flights of ideas: Rapid constant shifting from one idea to another as in mania. Ø Clang association ﺍﻻﺭﺗﺒﺎﻁ ﺍﻟﺼﻮﺗﻲ : Association of words similar in sound not meaning as in mania. Ø Blocking of thought: Abrupt interruption in the train of thinking before the ideas is finished common in depression and schizophrenia.
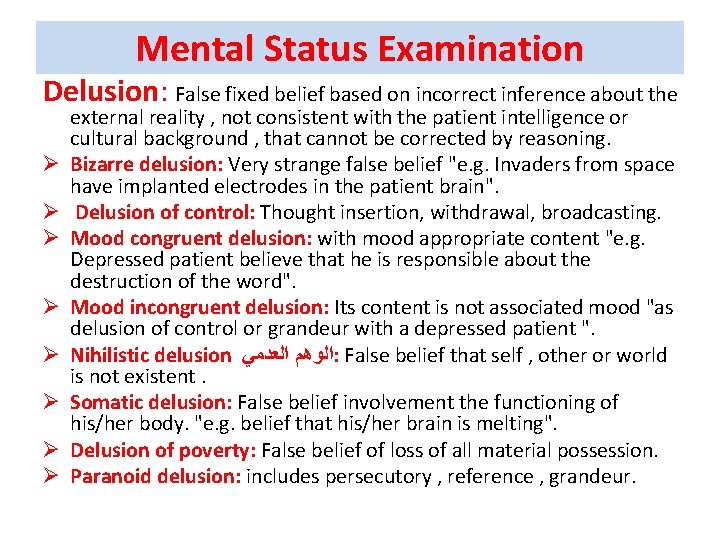
Mental Status Examination Delusion: False fixed belief based on incorrect inference about the Ø Ø Ø Ø external reality , not consistent with the patient intelligence or cultural background , that cannot be corrected by reasoning. Bizarre delusion: Very strange false belief "e. g. Invaders from space have implanted electrodes in the patient brain". Delusion of control: Thought insertion, withdrawal, broadcasting. Mood congruent delusion: with mood appropriate content "e. g. Depressed patient believe that he is responsible about the destruction of the word". Mood incongruent delusion: Its content is not associated mood "as delusion of control or grandeur with a depressed patient ". Nihilistic delusion ﺍﻟﻮﻫﻢ ﺍﻟﻌﺪﻣﻲ : False belief that self , other or world is not existent. Somatic delusion: False belief involvement the functioning of his/her body. "e. g. belief that his/her brain is melting". Delusion of poverty: False belief of loss of all material possession. Paranoid delusion: includes persecutory , reference , grandeur.
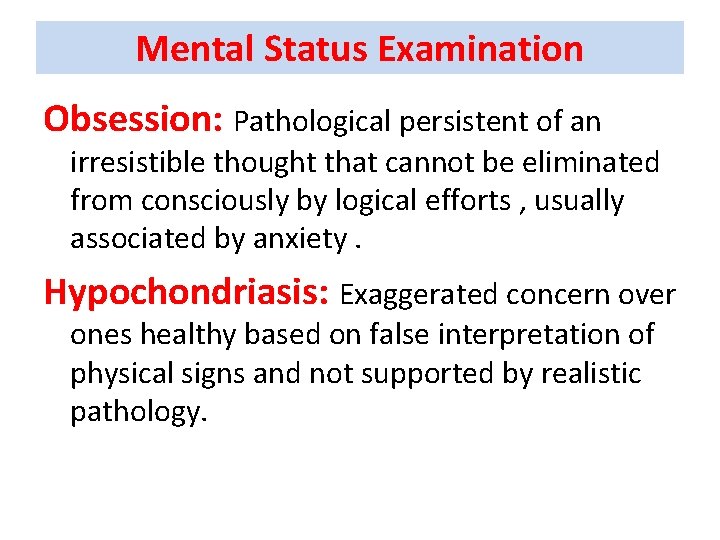
Mental Status Examination Obsession: Pathological persistent of an irresistible thought that cannot be eliminated from consciously by logical efforts , usually associated by anxiety. Hypochondriasis: Exaggerated concern over ones healthy based on false interpretation of physical signs and not supported by realistic pathology.
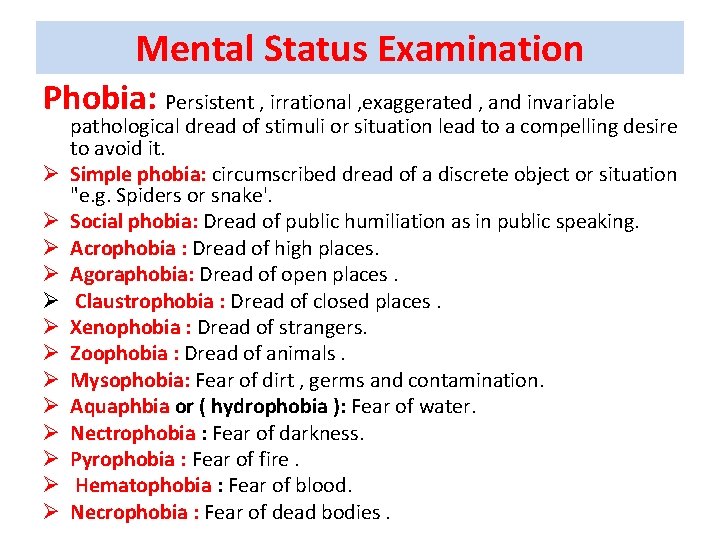
Mental Status Examination Phobia: Persistent , irrational , exaggerated , and invariable Ø Ø Ø Ø pathological dread of stimuli or situation lead to a compelling desire to avoid it. Simple phobia: circumscribed dread of a discrete object or situation "e. g. Spiders or snake'. Social phobia: Dread of public humiliation as in public speaking. Acrophobia : Dread of high places. Agoraphobia: Dread of open places. Claustrophobia : Dread of closed places. Xenophobia : Dread of strangers. Zoophobia : Dread of animals. Mysophobia: Fear of dirt , germs and contamination. Aquaphbia or ( hydrophobia ): Fear of water. Nectrophobia : Fear of darkness. Pyrophobia : Fear of fire. Hematophobia : Fear of blood. Necrophobia : Fear of dead bodies.
Mental Status Examination Abstract vs concrete thinking Abstract thinking: The ability to deal with concept. E. g. “ The ability to explain a known proverb or similarity between two things as an orange and apple are fruits. Patient with concrete thinking says both orange and apple are round , as in schizophrenia and organic disorder.
Mental Status Examination Memory: the ability to recall information. It is divided into: Ø Immediate memory: The ability to recall perceived objects within seconds. Ø Recent "short" memory: The ability to recall events in the past days. Ø Remote memory: The ability to recall of the events in the distance past. Disturbances in memory include: Ø Amnesia : Partial or total inability to recall past experience may be organic or emotional as in posttraumatic Stress disorders "PTSD".
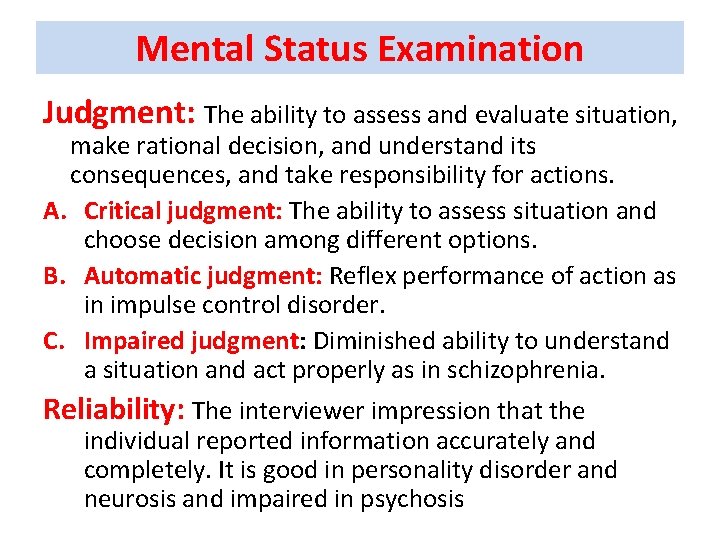
Mental Status Examination Judgment: The ability to assess and evaluate situation, make rational decision, and understand its consequences, and take responsibility for actions. A. Critical judgment: The ability to assess situation and choose decision among different options. B. Automatic judgment: Reflex performance of action as in impulse control disorder. C. Impaired judgment: Diminished ability to understand a situation and act properly as in schizophrenia. Reliability: The interviewer impression that the individual reported information accurately and completely. It is good in personality disorder and neurosis and impaired in psychosis
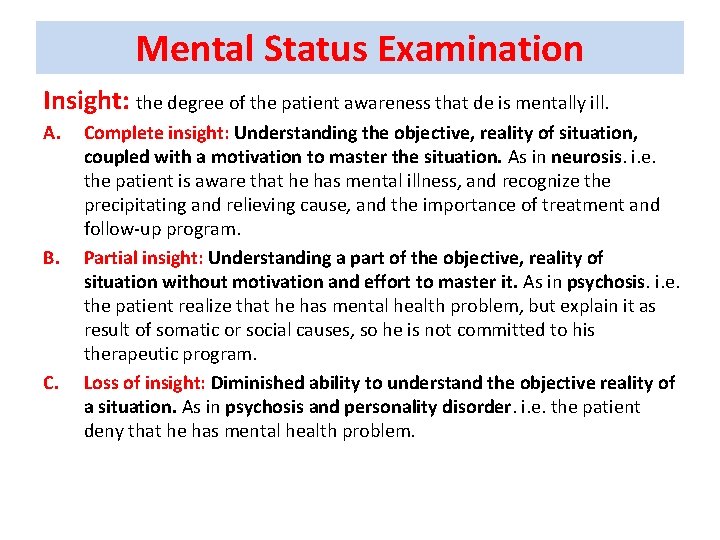
Mental Status Examination Insight: the degree of the patient awareness that de is mentally ill. A. B. Complete insight: Understanding the objective, reality of situation, coupled with a motivation to master the situation. As in neurosis. i. e. the patient is aware that he has mental illness, and recognize the precipitating and relieving cause, and the importance of treatment and follow-up program. Partial insight: Understanding a part of the objective, reality of situation without motivation and effort to master it. As in psychosis. i. e. the patient realize that he has mental health problem, but explain it as result of somatic or social causes, so he is not committed to his therapeutic program. Loss of insight: Diminished ability to understand the objective reality of a situation. As in psychosis and personality disorder. i. e. the patient deny that he has mental health problem.
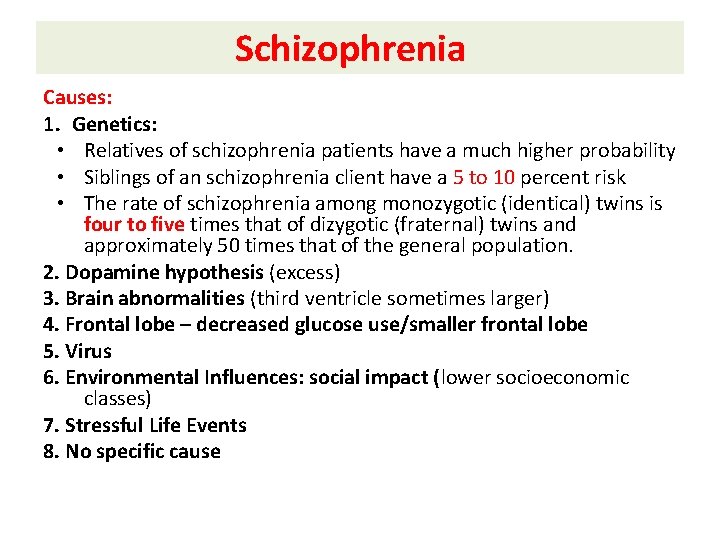
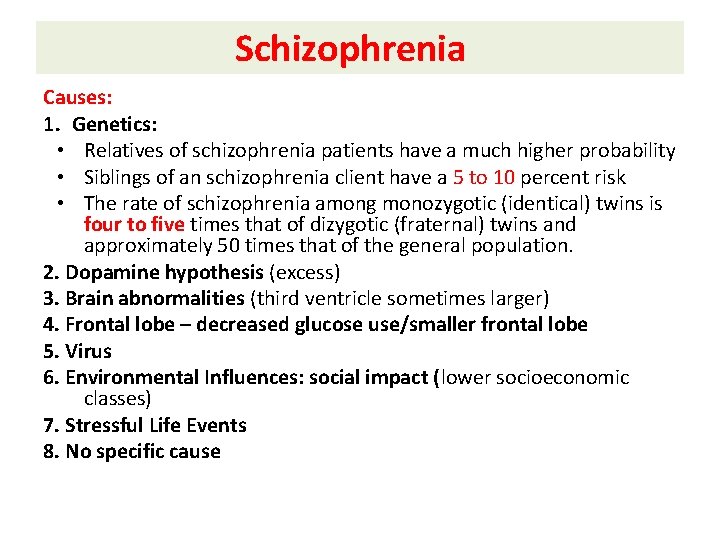
Schizophrenia Causes: 1. Genetics: • Relatives of schizophrenia patients have a much higher probability • Siblings of an schizophrenia client have a 5 to 10 percent risk • The rate of schizophrenia among monozygotic (identical) twins is four to five times that of dizygotic (fraternal) twins and approximately 50 times that of the general population. 2. Dopamine hypothesis (excess) 3. Brain abnormalities (third ventricle sometimes larger) 4. Frontal lobe – decreased glucose use/smaller frontal lobe 5. Virus 6. Environmental Influences: social impact (lower socioeconomic classes) 7. Stressful Life Events 8. No specific cause
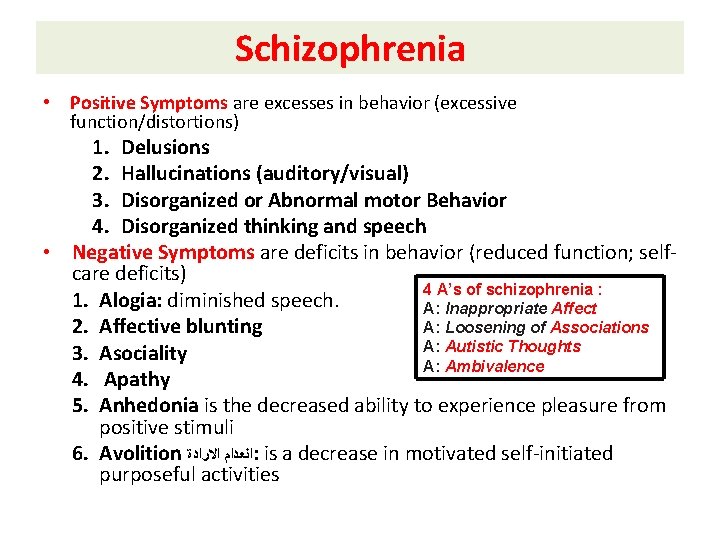
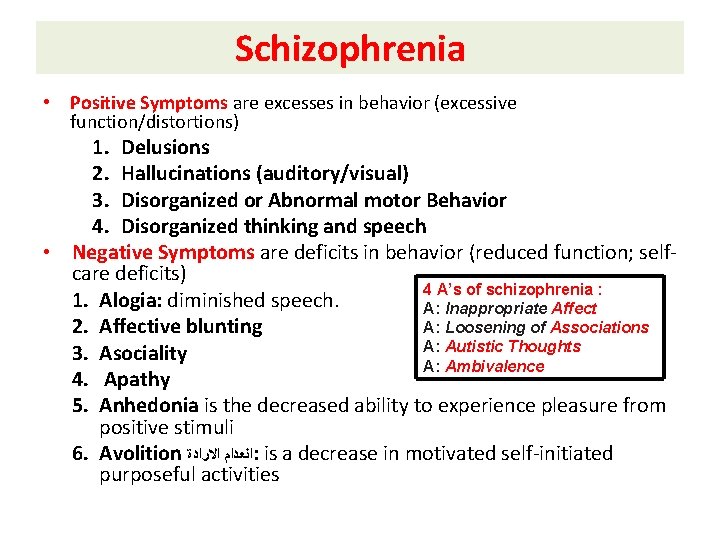
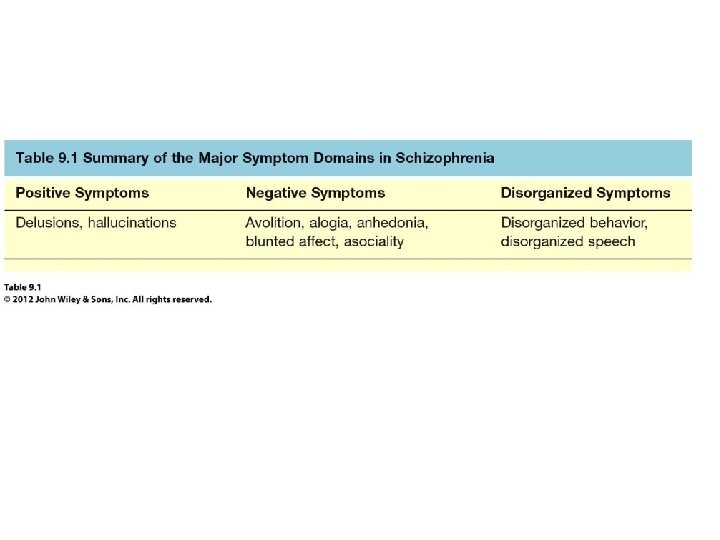
Schizophrenia • Positive Symptoms are excesses in behavior (excessive function/distortions) 1. Delusions 2. Hallucinations (auditory/visual) 3. Disorganized or Abnormal motor Behavior 4. Disorganized thinking and speech • Negative Symptoms are deficits in behavior (reduced function; selfcare deficits) 4 A’s of schizophrenia : 1. Alogia: diminished speech. A: Inappropriate Affect A: Loosening of Associations 2. Affective blunting A: Autistic Thoughts 3. Asociality A: Ambivalence 4. Apathy 5. Anhedonia is the decreased ability to experience pleasure from positive stimuli 6. Avolition ﺍﻧﻌﺪﺍﻡ ﺍﻻﺭﺍﺩﺓ : is a decrease in motivated self-initiated purposeful activities
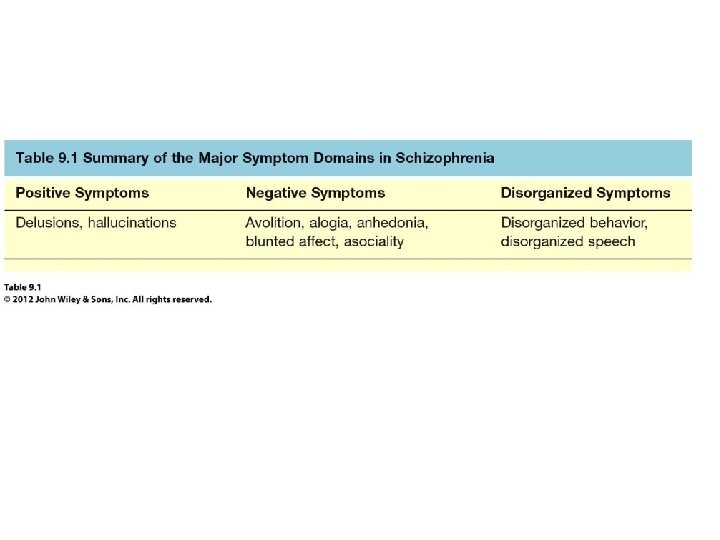
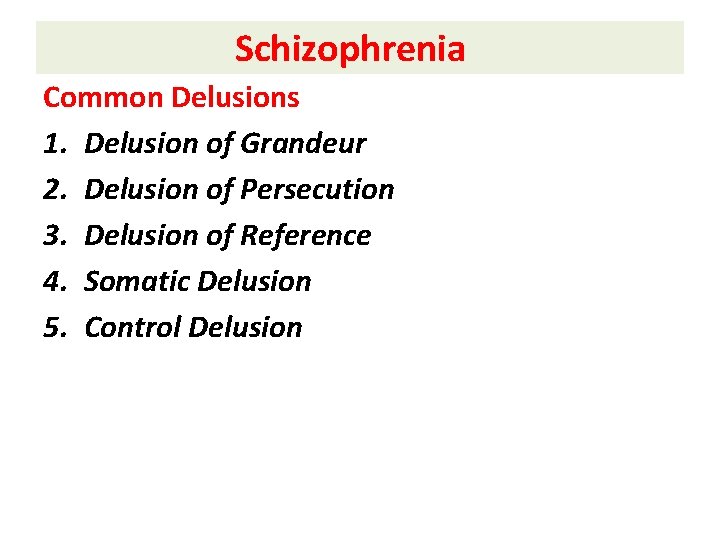
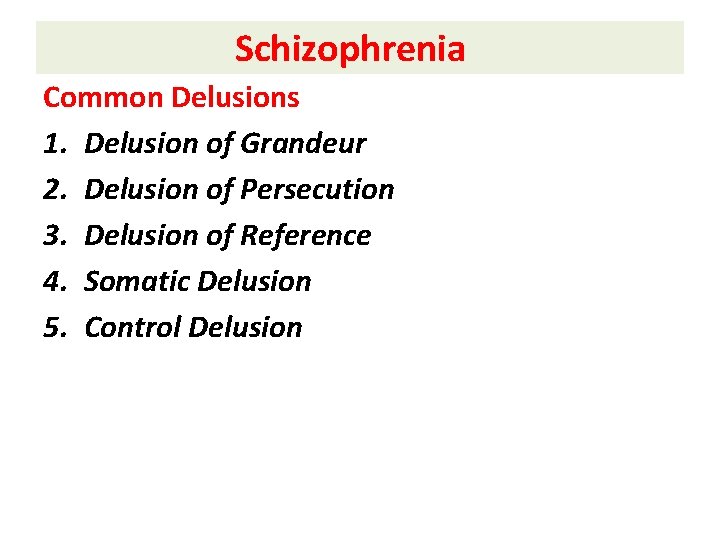
Schizophrenia Common Delusions 1. Delusion of Grandeur 2. Delusion of Persecution 3. Delusion of Reference 4. Somatic Delusion 5. Control Delusion
Schizophrenia Hallucinations • Auditory hallucinations are the most common in schizophrenia and related disorders. • The second most common type is visual hallucinations, while other hallucinations may be rare.
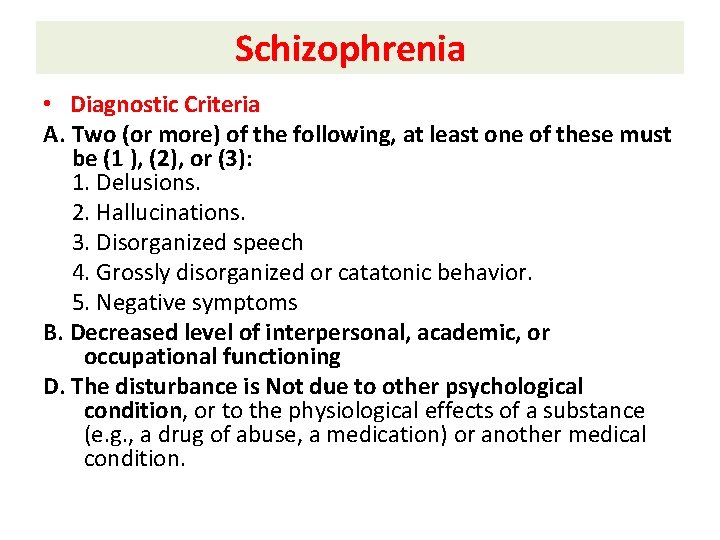
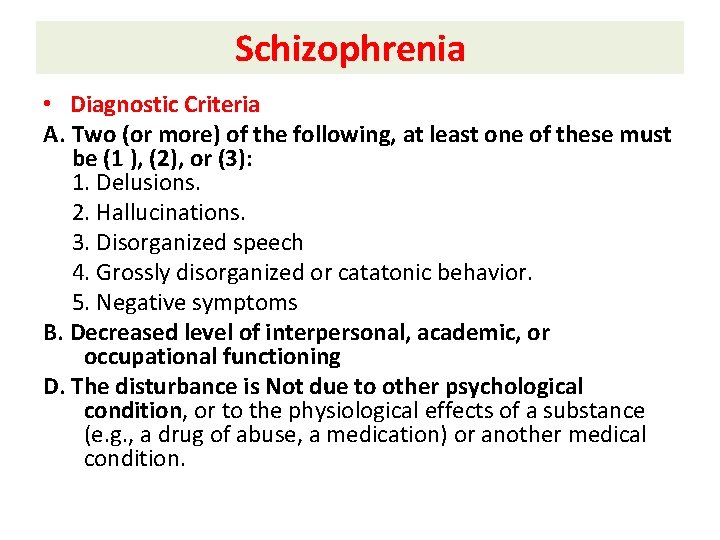
Schizophrenia • Diagnostic Criteria A. Two (or more) of the following, at least one of these must be (1 ), (2), or (3): 1. Delusions. 2. Hallucinations. 3. Disorganized speech 4. Grossly disorganized or catatonic behavior. 5. Negative symptoms B. Decreased level of interpersonal, academic, or occupational functioning D. The disturbance is Not due to other psychological condition, or to the physiological effects of a substance (e. g. , a drug of abuse, a medication) or another medical condition.
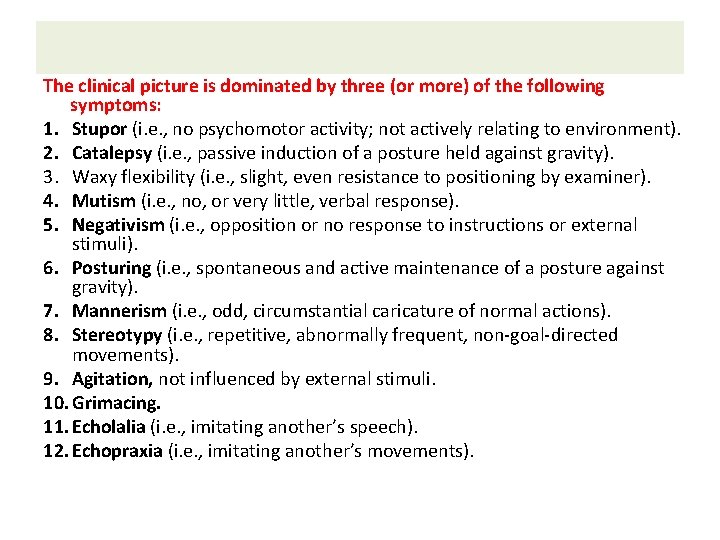
The clinical picture is dominated by three (or more) of the following symptoms: 1. Stupor (i. e. , no psychomotor activity; not actively relating to environment). 2. Catalepsy (i. e. , passive induction of a posture held against gravity). 3. Waxy flexibility (i. e. , slight, even resistance to positioning by examiner). 4. Mutism (i. e. , no, or very little, verbal response). 5. Negativism (i. e. , opposition or no response to instructions or external stimuli). 6. Posturing (i. e. , spontaneous and active maintenance of a posture against gravity). 7. Mannerism (i. e. , odd, circumstantial caricature of normal actions). 8. Stereotypy (i. e. , repetitive, abnormally frequent, non-goal-directed movements). 9. Agitation, not influenced by external stimuli. 10. Grimacing. 11. Echolalia (i. e. , imitating another’s speech). 12. Echopraxia (i. e. , imitating another’s movements).
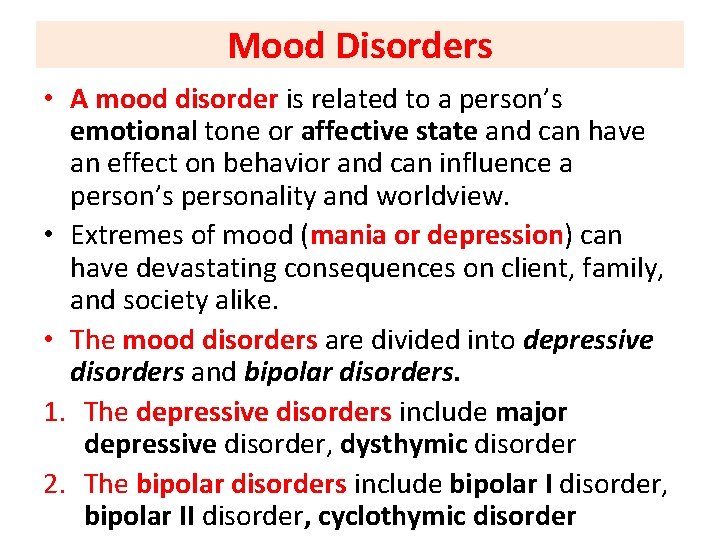
Mood Disorders • A mood disorder is related to a person’s emotional tone or affective state and can have an effect on behavior and can influence a person’s personality and worldview. • Extremes of mood (mania or depression) can have devastating consequences on client, family, and society alike. • The mood disorders are divided into depressive disorders and bipolar disorders. 1. The depressive disorders include major depressive disorder, dysthymic disorder 2. The bipolar disorders include bipolar I disorder, bipolar II disorder, cyclothymic disorder
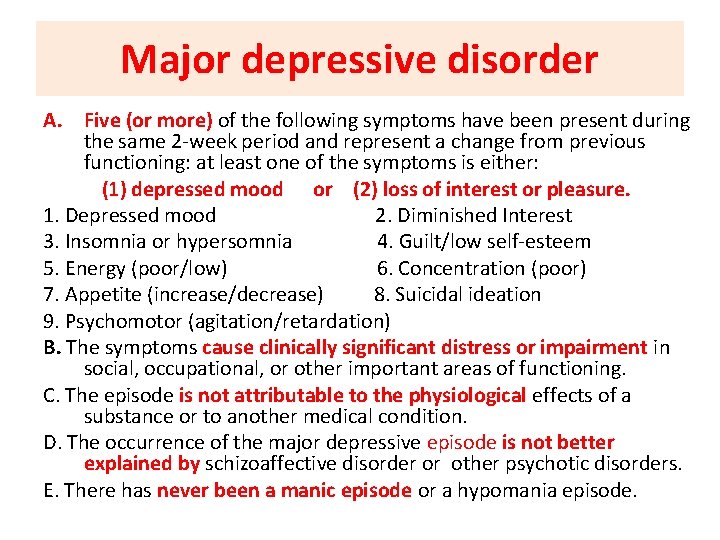
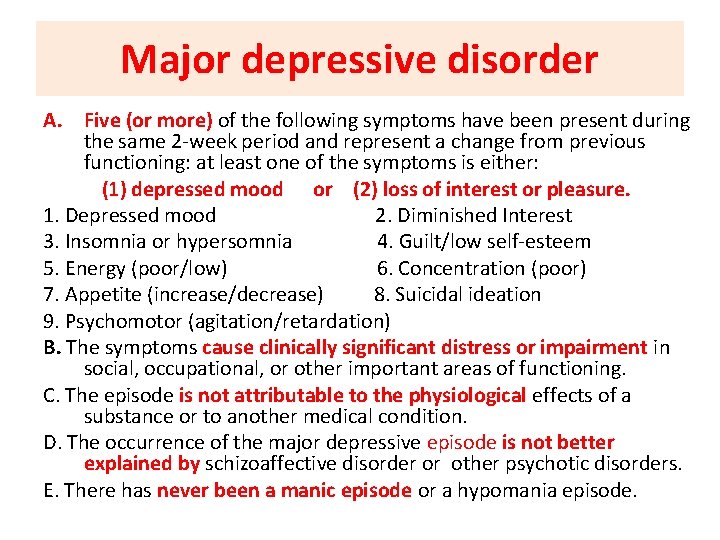
Major depressive disorder A. Five (or more) of the following symptoms have been present during the same 2 -week period and represent a change from previous functioning: at least one of the symptoms is either: (1) depressed mood or (2) loss of interest or pleasure. 1. Depressed mood 2. Diminished Interest 3. Insomnia or hypersomnia 4. Guilt/low self-esteem 5. Energy (poor/low) 6. Concentration (poor) 7. Appetite (increase/decrease) 8. Suicidal ideation 9. Psychomotor (agitation/retardation) B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. C. The episode is not attributable to the physiological effects of a substance or to another medical condition. D. The occurrence of the major depressive episode is not better explained by schizoaffective disorder or other psychotic disorders. E. There has never been a manic episode or a hypomania episode.
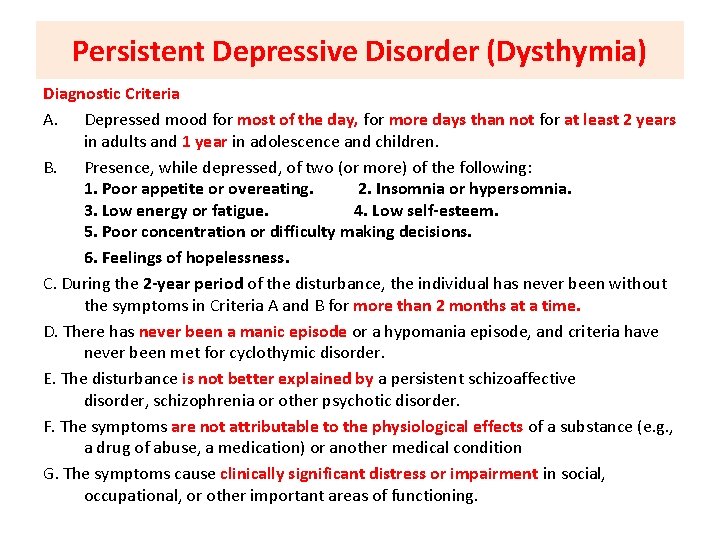
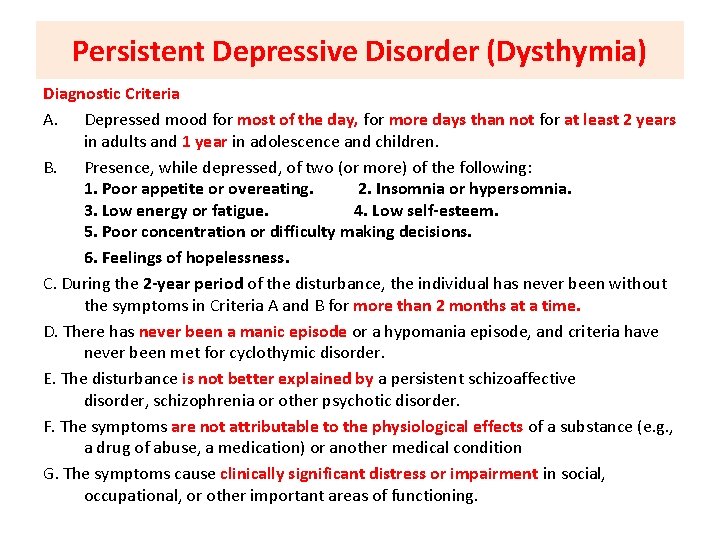
Persistent Depressive Disorder (Dysthymia) Diagnostic Criteria A. Depressed mood for most of the day, for more days than not for at least 2 years in adults and 1 year in adolescence and children. B. Presence, while depressed, of two (or more) of the following: 1. Poor appetite or overeating. 2. Insomnia or hypersomnia. 3. Low energy or fatigue. 4. Low self-esteem. 5. Poor concentration or difficulty making decisions. 6. Feelings of hopelessness. C. During the 2 -year period of the disturbance, the individual has never been without the symptoms in Criteria A and B for more than 2 months at a time. D. There has never been a manic episode or a hypomania episode, and criteria have never been met for cyclothymic disorder. E. The disturbance is not better explained by a persistent schizoaffective disorder, schizophrenia or other psychotic disorder. F. The symptoms are not attributable to the physiological effects of a substance (e. g. , a drug of abuse, a medication) or another medical condition G. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
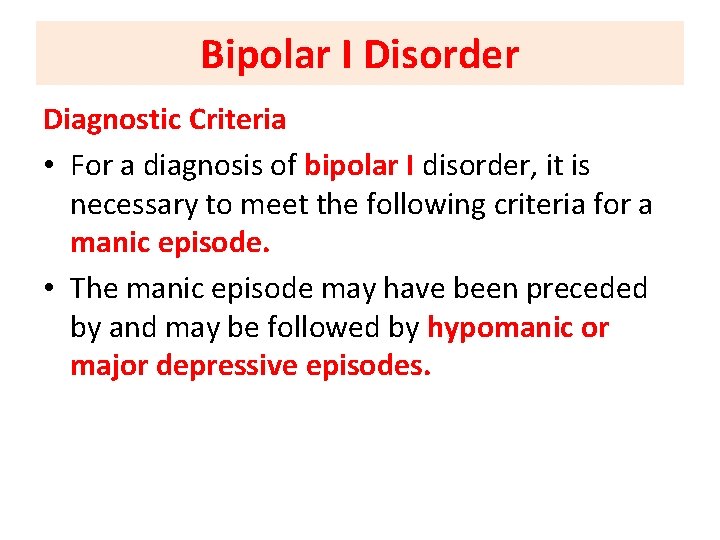
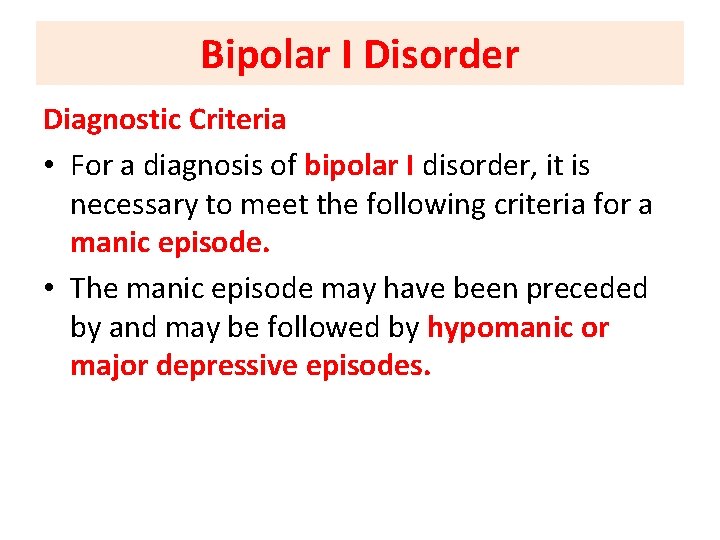
Bipolar I Disorder Diagnostic Criteria • For a diagnosis of bipolar I disorder, it is necessary to meet the following criteria for a manic episode. • The manic episode may have been preceded by and may be followed by hypomanic or major depressive episodes.
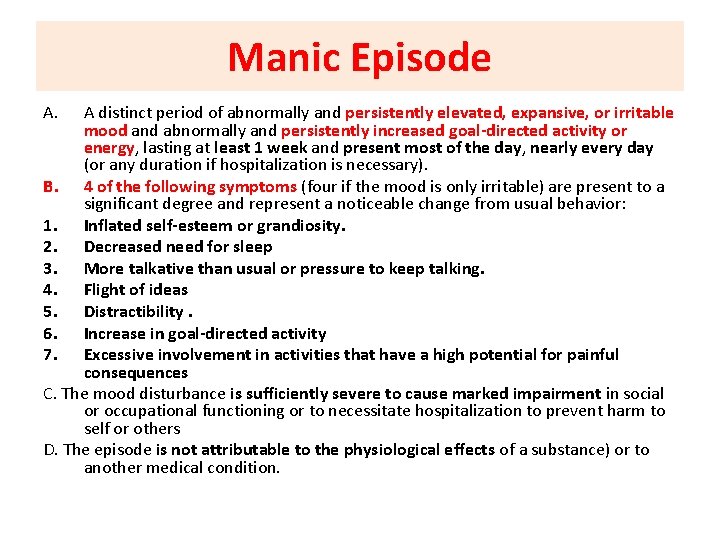
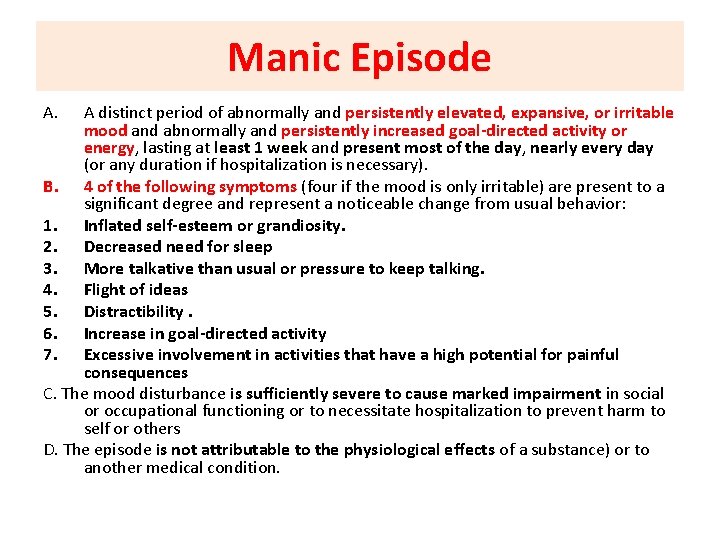
Manic Episode A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, lasting at least 1 week and present most of the day, nearly every day (or any duration if hospitalization is necessary). B. 4 of the following symptoms (four if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior: 1. Inflated self-esteem or grandiosity. 2. Decreased need for sleep 3. More talkative than usual or pressure to keep talking. 4. Flight of ideas 5. Distractibility. 6. Increase in goal-directed activity 7. Excessive involvement in activities that have a high potential for painful consequences C. The mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning or to necessitate hospitalization to prevent harm to self or others D. The episode is not attributable to the physiological effects of a substance) or to another medical condition.
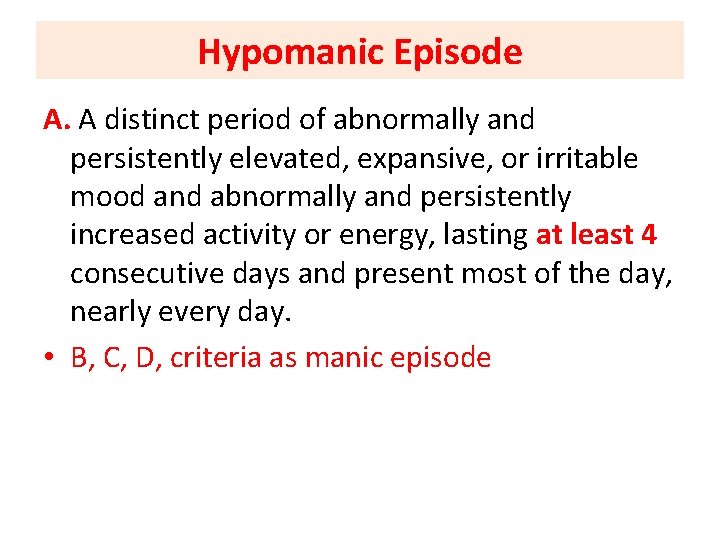
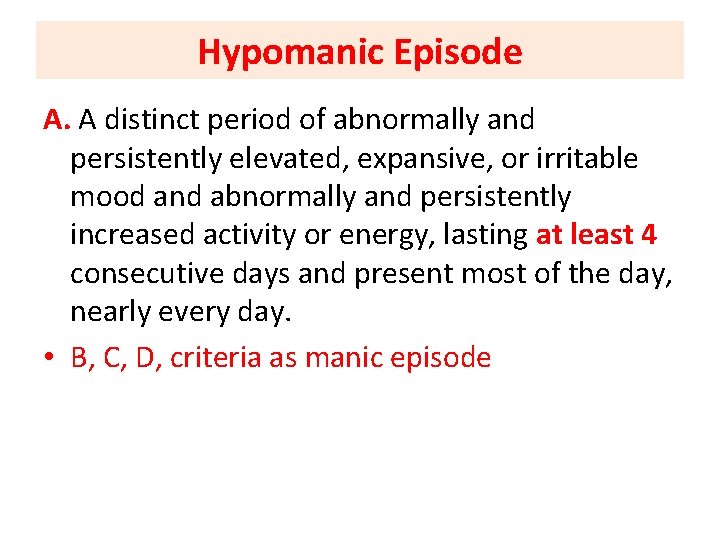
Hypomanic Episode A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy, lasting at least 4 consecutive days and present most of the day, nearly every day. • B, C, D, criteria as manic episode
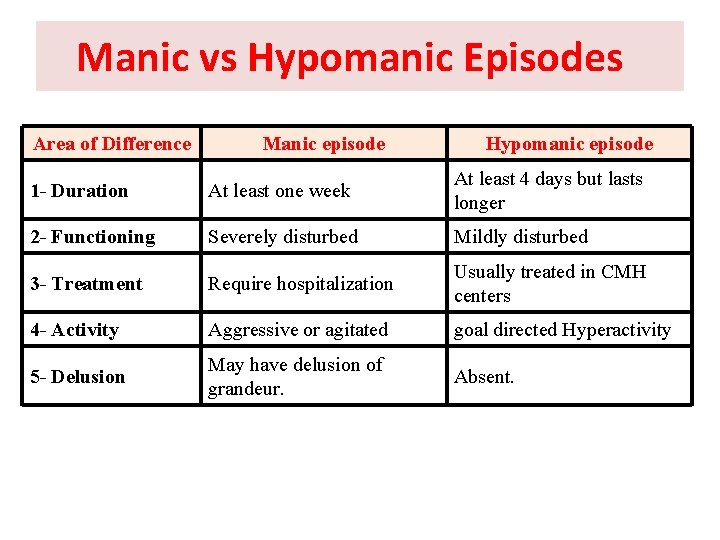
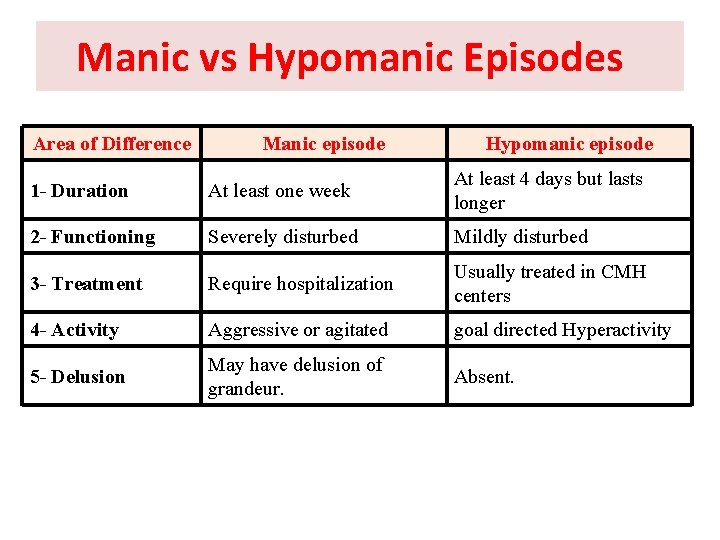
Manic vs Hypomanic Episodes Area of Difference Manic episode Hypomanic episode 1 - Duration At least one week At least 4 days but lasts longer 2 - Functioning Severely disturbed Mildly disturbed 3 - Treatment Require hospitalization Usually treated in CMH centers 4 - Activity Aggressive or agitated goal directed Hyperactivity 5 - Delusion May have delusion of grandeur. Absent.
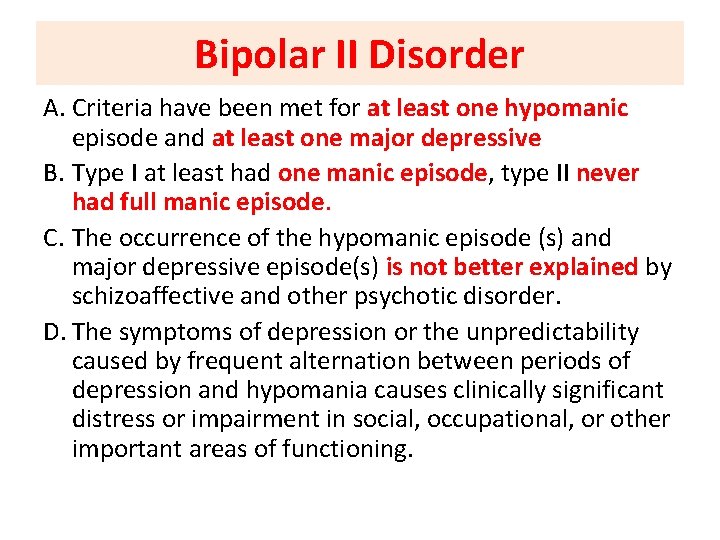
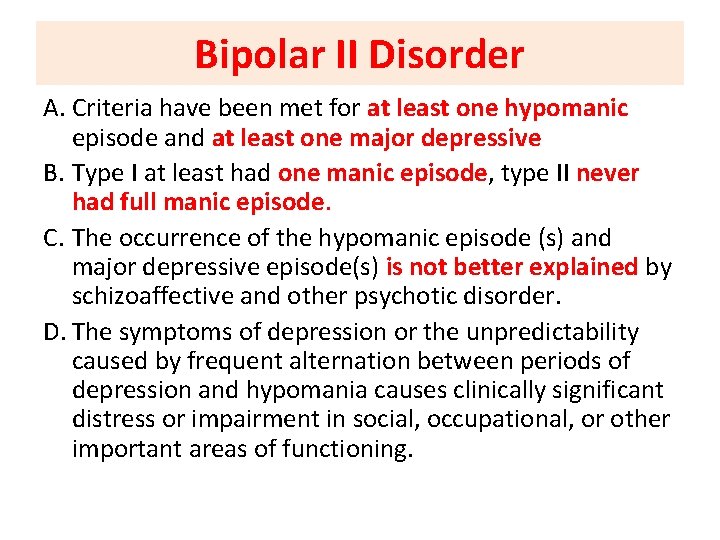
Bipolar II Disorder A. Criteria have been met for at least one hypomanic episode and at least one major depressive B. Type I at least had one manic episode, type II never had full manic episode. C. The occurrence of the hypomanic episode (s) and major depressive episode(s) is not better explained by schizoaffective and other psychotic disorder. D. The symptoms of depression or the unpredictability caused by frequent alternation between periods of depression and hypomania causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
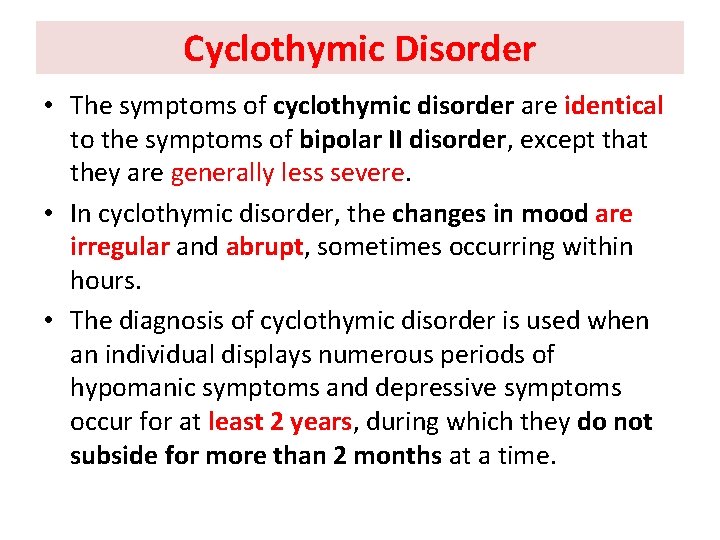
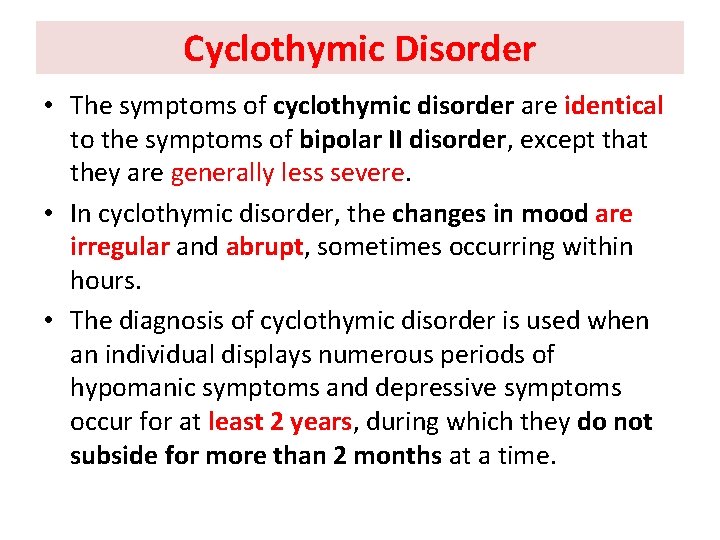
Cyclothymic Disorder • The symptoms of cyclothymic disorder are identical to the symptoms of bipolar II disorder, except that they are generally less severe. • In cyclothymic disorder, the changes in mood are irregular and abrupt, sometimes occurring within hours. • The diagnosis of cyclothymic disorder is used when an individual displays numerous periods of hypomanic symptoms and depressive symptoms occur for at least 2 years, during which they do not subside for more than 2 months at a time.
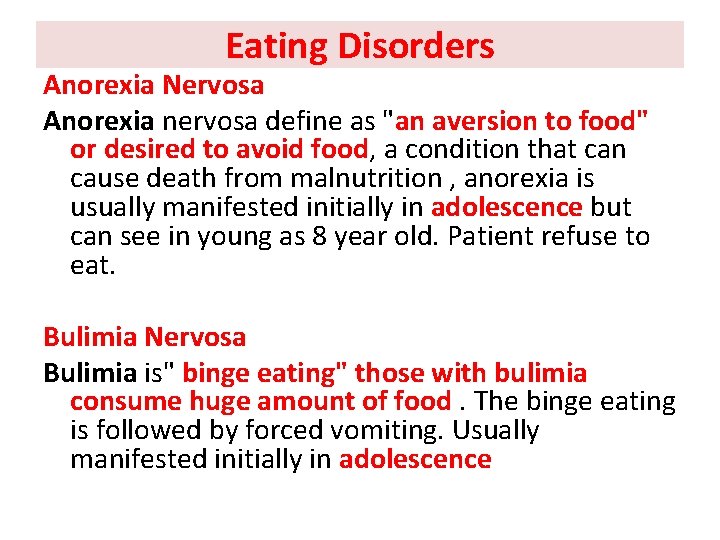
Eating Disorders Anorexia Nervosa Anorexia nervosa define as "an aversion to food" or desired to avoid food, a condition that can cause death from malnutrition , anorexia is usually manifested initially in adolescence but can see in young as 8 year old. Patient refuse to eat. Bulimia Nervosa Bulimia is" binge eating" those with bulimia consume huge amount of food. The binge eating is followed by forced vomiting. Usually manifested initially in adolescence
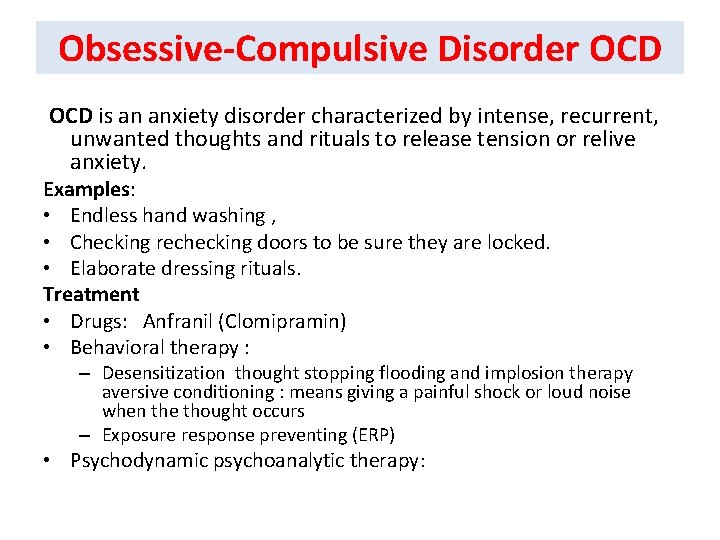
Obsessive-Compulsive Disorder OCD is an anxiety disorder characterized by intense, recurrent, unwanted thoughts and rituals to release tension or relive anxiety. Examples: • Endless hand washing , • Checking rechecking doors to be sure they are locked. • Elaborate dressing rituals. Treatment • Drugs: Anfranil (Clomipramin) • Behavioral therapy : – Desensitization thought stopping flooding and implosion therapy aversive conditioning : means giving a painful shock or loud noise when the thought occurs – Exposure response preventing (ERP) • Psychodynamic psychoanalytic therapy:
Anxiety • An uncomfortable feeling that occurs in response to the fear of being hurt or losing something valued. Types of Anxiety Disorders : 1. General Anxiety Disorder- GAD • Persistent anxiety without phobias or panic attacks • Worry excessively about everyday concerns • May become preoccupied with catastrophic thoughts 2. Panic Attack • The highest level of anxiety, characterized by disorganized thinking, feelings of terror and helplessness, and non purposeful behavior • Intense feel like they are about to die, lose control, or go crazy.
Anxiety 3. Panic disorder • Recurrent panic attacks • Usually affects young adults • Can occur with or without agoraphobia • Sudden onset, unexpected, intense fear, a feeling of doom, catastrophic thinking • May manifest in respiratory, cardiovascular symptoms.
Post Traumatic Stress Disorder • PTSD is psychological disorder that develops in some individuals after a major traumatic experience such as war, rape, domestic violence, or accident. • PTSD is an anxiety disorder characterized by a terrifying physical or emotional event (trauma) causing the person who survived the event to have persistent, frightening thoughts and memories, or flashbacks, of the ordeal. • Persons with PTSD often feel chronically, emotionally numb.
Personality disorders • Cluster "A" personality disorders • is a pattern of distrust and suspiciousness such that others' motives are interpreted as malevolent. • • Schizoid personality disorder is a pattern of detachment from social relationships and a restricted range of emotional expression. • • Schizotypal personality disorder is a pattern of acute discomfort in close relationships, cognitive or perceptual distortions, and eccentricities of behavior
Cluster "B" personality disorders • • Antisocial personality disorder: is a pattern of disregard for, and violation of, the rights of others. The essential defect is the individuals are unable to control their impulses, and termed psychopathic. • • Borderline personality disorder is a pattern of instability in interpersonal relationships, selfimage, and affects, and marked impulsivity, the border between neurosis and psychosis, female are 75% of the cases
• • Histrionic personality disorder is a pattern of excessive emotionality and attention, females are diagnosed much more than males. • Men with similar pattern are diagnosed as narcissistic, somatization and depression are common. • • Narcissistic personality disorder: A pervasive pattern of grandiosity, need for admiration, sensitivity to criticism, and lack of empathy. depressed mood is common,
Cluster "C" personality disorders: • • Avoidant personality disorder is a pattern of social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation. It differs from schizoid personality disorder that clients avoids social contact due to fears of being rejected or criticized, if they have strong guarantees of uncritical acceptance, they will make friends.
• • Dependent personality disorder is a pervasive and excessive need to be taken care of that leads to submissive, dependent and clinging behavior and fears of separation, history of separation anxiety is common, it is diagnosed more frequently in females • • Obsessive-compulsive personality disorder is a pattern of preoccupation with orderliness, perfectionism, and control at the expense of flexibility, openness, and efficiency. obsessive-compulsive personality disorder appears to be diagnosed about twice as often among males
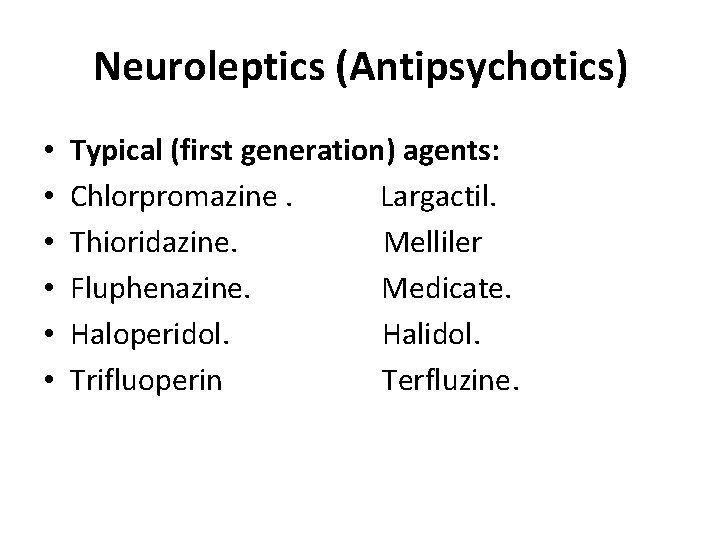
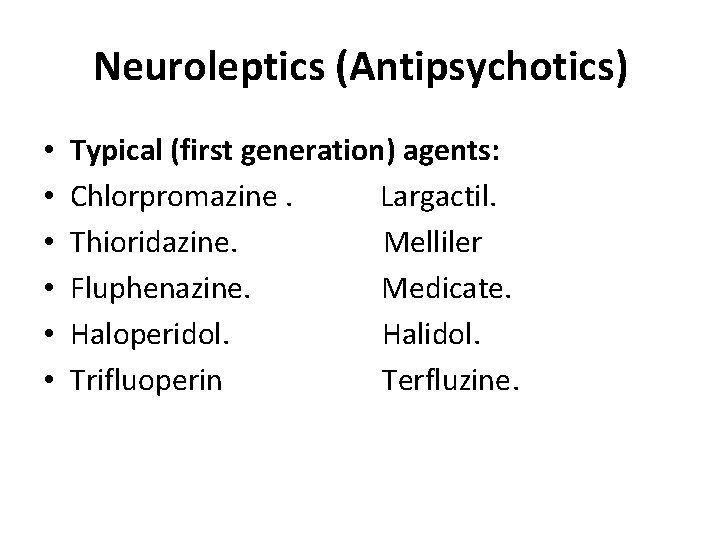
Neuroleptics (Antipsychotics) • • • Typical (first generation) agents: Chlorpromazine. Largactil. Thioridazine. Melliler Fluphenazine. Medicate. Haloperidol. Halidol. Trifluoperin Terfluzine.
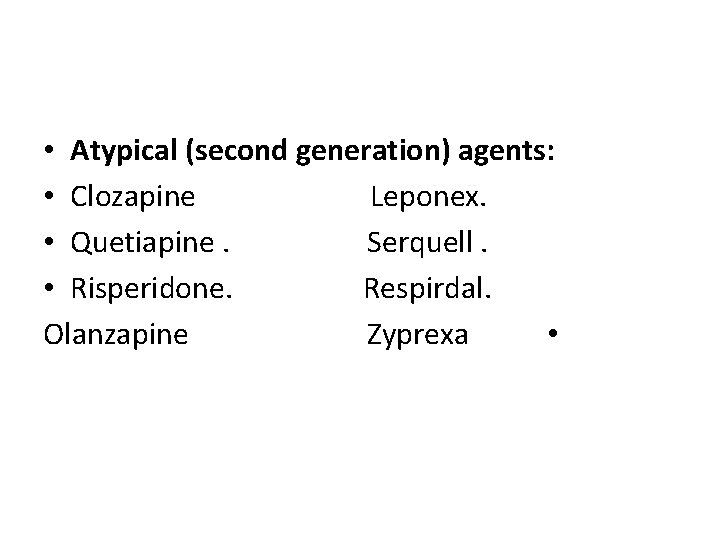
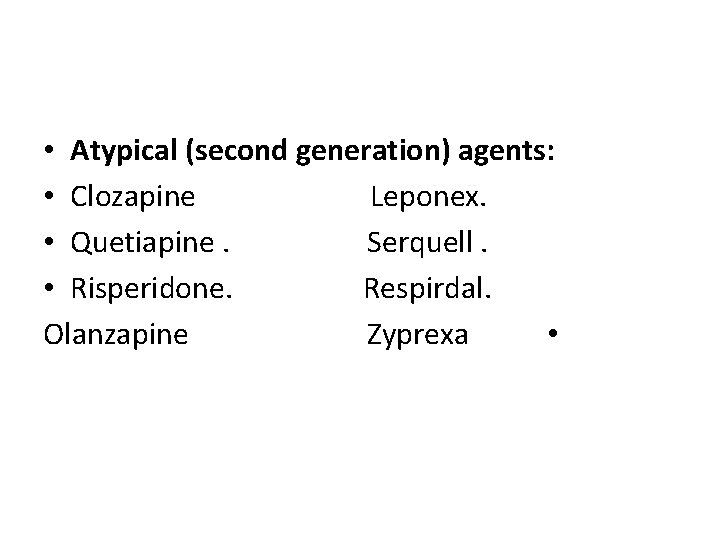
• Atypical (second generation) agents: • Clozapine Leponex. • Quetiapine. Serquell. • Risperidone. Respirdal. Olanzapine Zyprexa •
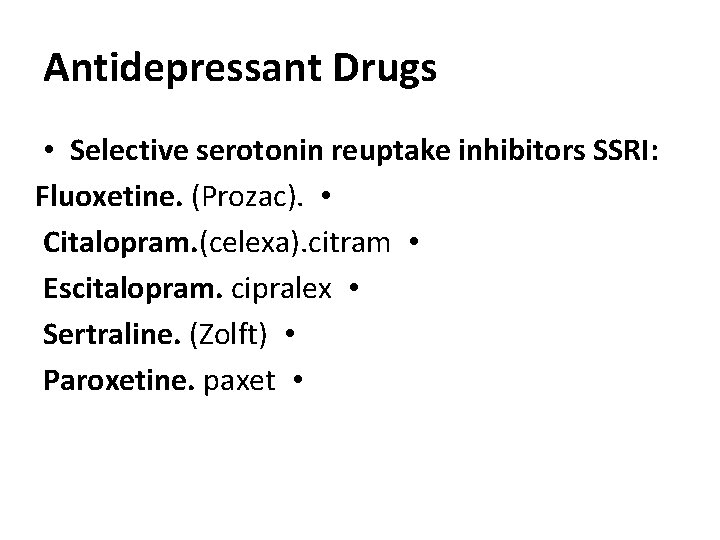
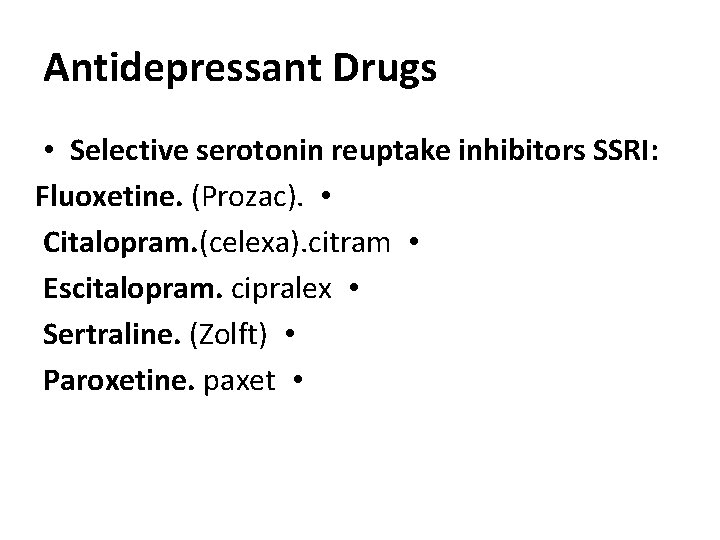
Antidepressant Drugs • Selective serotonin reuptake inhibitors SSRI: Fluoxetine. (Prozac). • Citalopram. (celexa). citram • Escitalopram. cipralex • Sertraline. (Zolft) • Paroxetine. paxet •
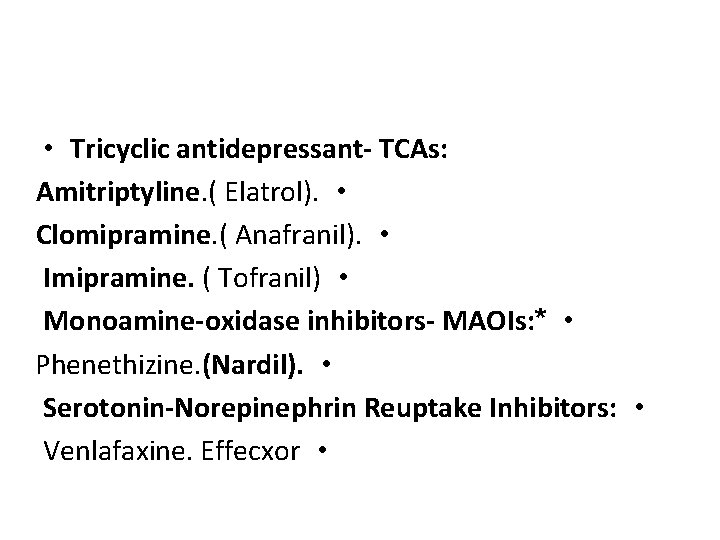
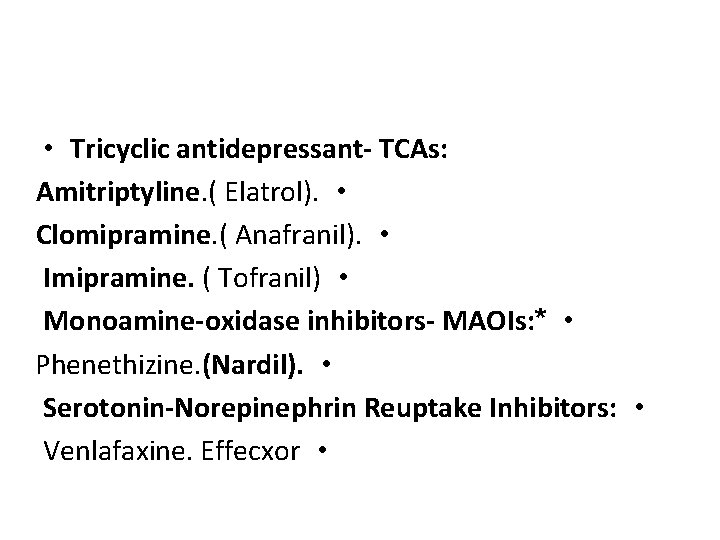
• Tricyclic antidepressant- TCAs: Amitriptyline. ( Elatrol). • Clomipramine. ( Anafranil). • Imipramine. ( Tofranil) • Monoamine-oxidase inhibitors- MAOIs: * • Phenethizine. (Nardil). • Serotonin-Norepinephrin Reuptake Inhibitors: • Venlafaxine. Effecxor •
Antiparkinsonism • Trihexphenadyle. (Artan): •
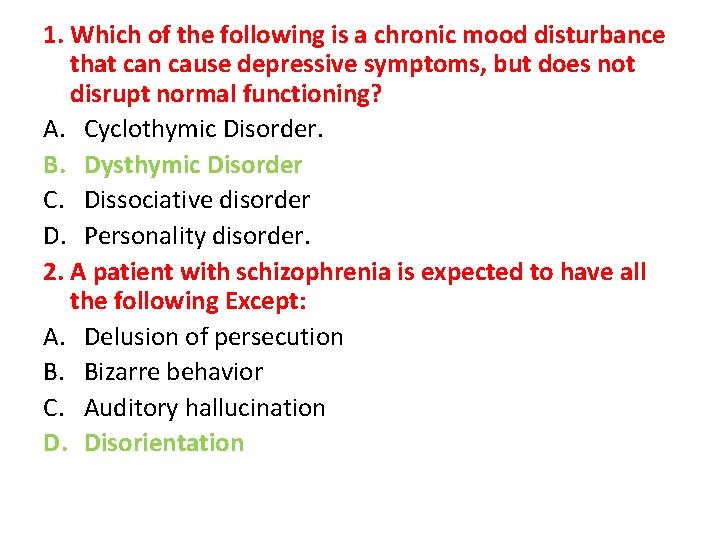
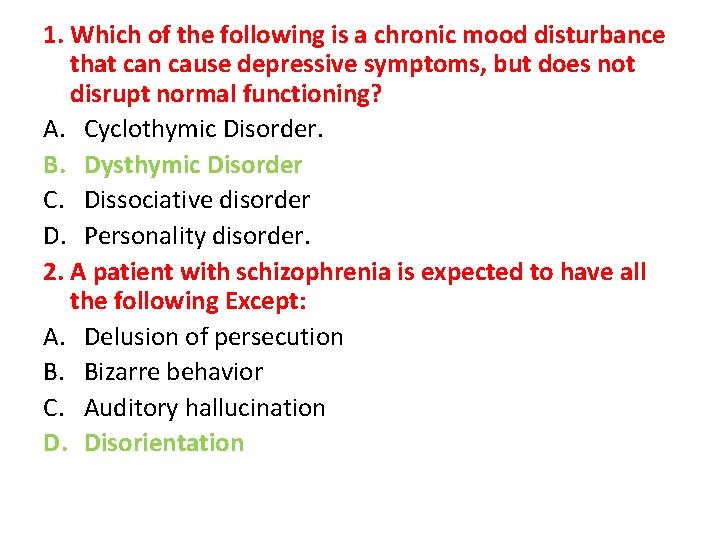
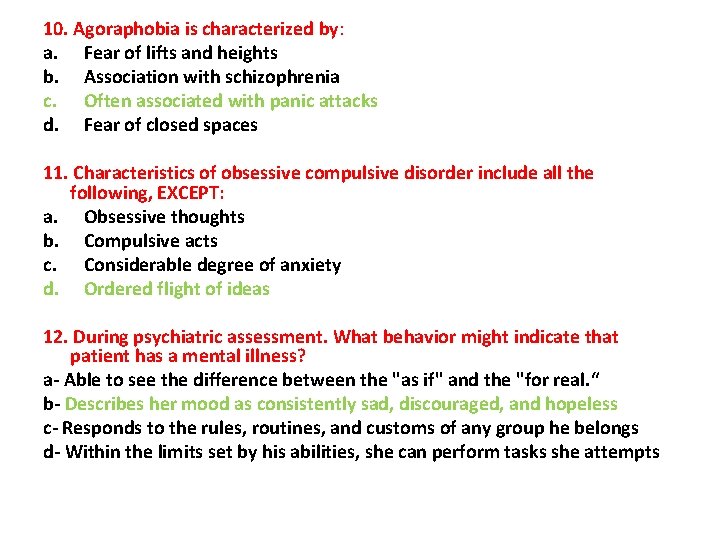
1. Which of the following is a chronic mood disturbance that can cause depressive symptoms, but does not disrupt normal functioning? A. Cyclothymic Disorder. B. Dysthymic Disorder C. Dissociative disorder D. Personality disorder. 2. A patient with schizophrenia is expected to have all the following Except: A. Delusion of persecution B. Bizarre behavior C. Auditory hallucination D. Disorientation
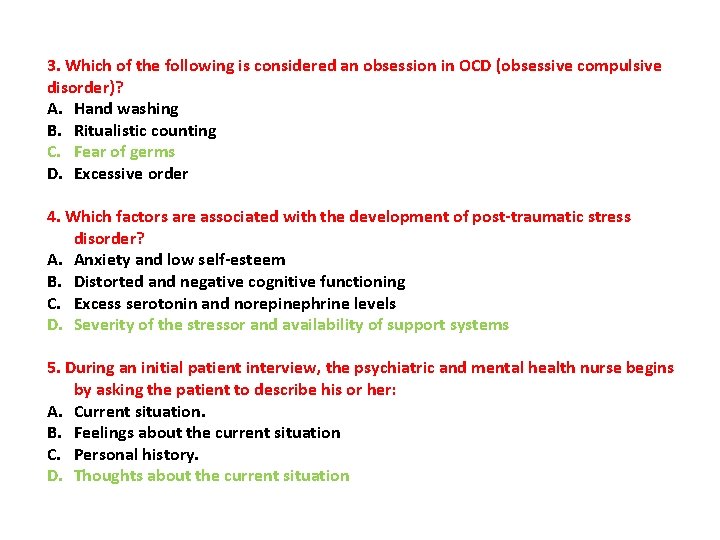
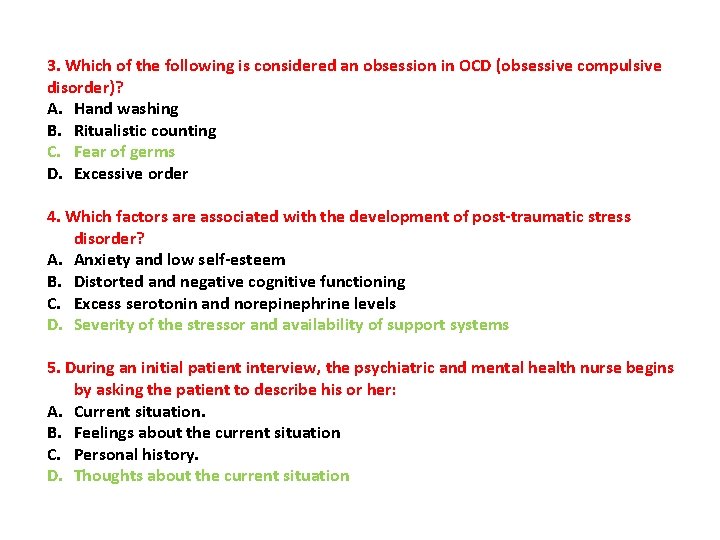
3. Which of the following is considered an obsession in OCD (obsessive compulsive disorder)? A. Hand washing B. Ritualistic counting C. Fear of germs D. Excessive order 4. Which factors are associated with the development of post-traumatic stress disorder? A. Anxiety and low self-esteem B. Distorted and negative cognitive functioning C. Excess serotonin and norepinephrine levels D. Severity of the stressor and availability of support systems 5. During an initial patient interview, the psychiatric and mental health nurse begins by asking the patient to describe his or her: A. Current situation. B. Feelings about the current situation C. Personal history. D. Thoughts about the current situation
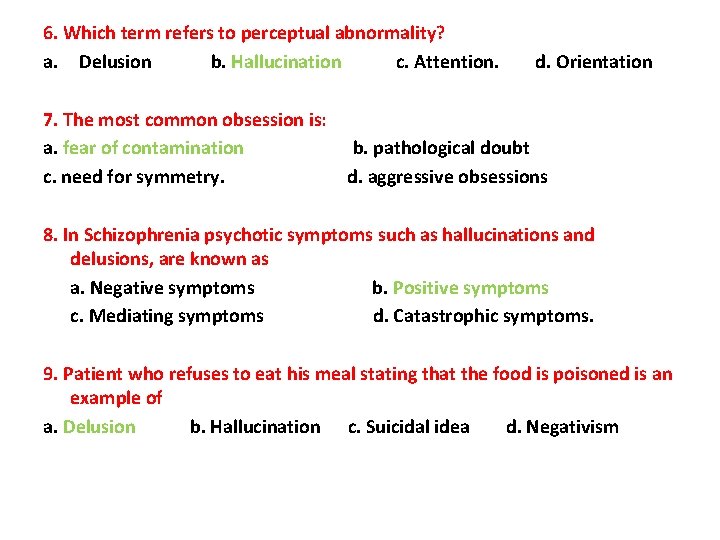
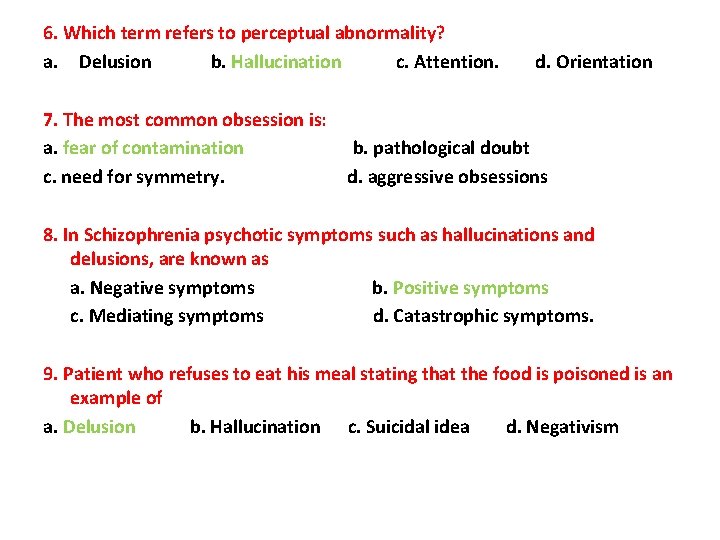
6. Which term refers to perceptual abnormality? a. Delusion b. Hallucination c. Attention. d. Orientation 7. The most common obsession is: a. fear of contamination b. pathological doubt c. need for symmetry. d. aggressive obsessions 8. In Schizophrenia psychotic symptoms such as hallucinations and delusions, are known as a. Negative symptoms b. Positive symptoms c. Mediating symptoms d. Catastrophic symptoms. 9. Patient who refuses to eat his meal stating that the food is poisoned is an example of a. Delusion b. Hallucination c. Suicidal idea d. Negativism
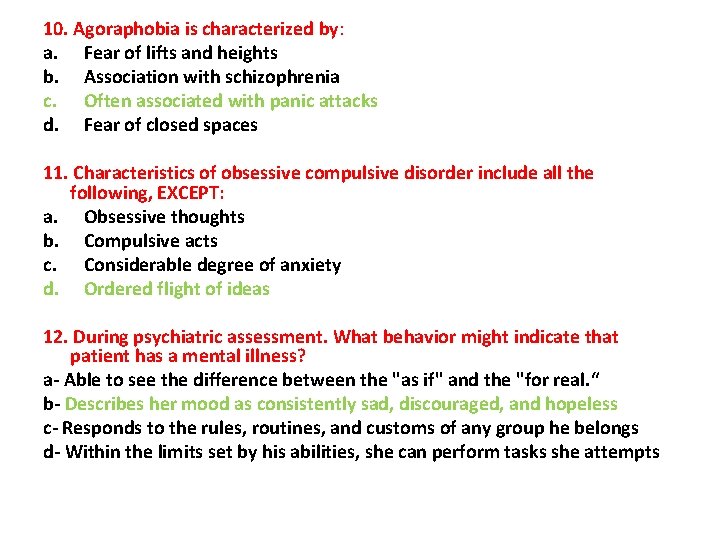
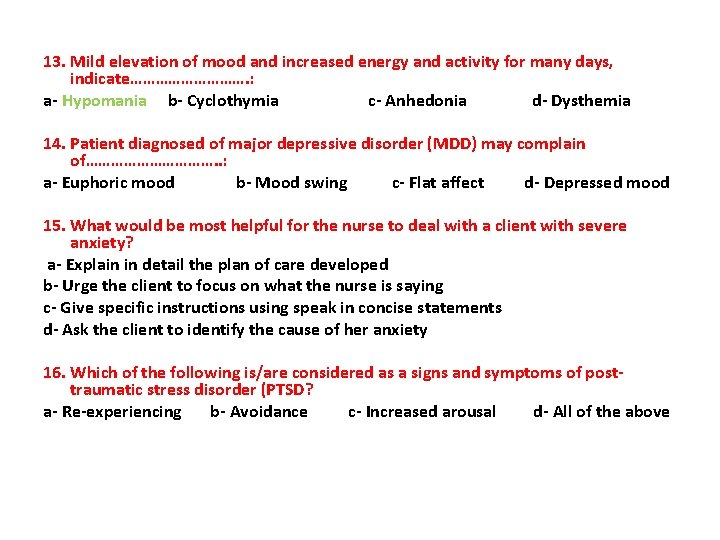
10. Agoraphobia is characterized by: a. Fear of lifts and heights b. Association with schizophrenia c. Often associated with panic attacks d. Fear of closed spaces 11. Characteristics of obsessive compulsive disorder include all the following, EXCEPT: a. Obsessive thoughts b. Compulsive acts c. Considerable degree of anxiety d. Ordered flight of ideas 12. During psychiatric assessment. What behavior might indicate that patient has a mental illness? a- Able to see the difference between the "as if" and the "for real. “ b- Describes her mood as consistently sad, discouraged, and hopeless c- Responds to the rules, routines, and customs of any group he belongs d- Within the limits set by his abilities, she can perform tasks she attempts
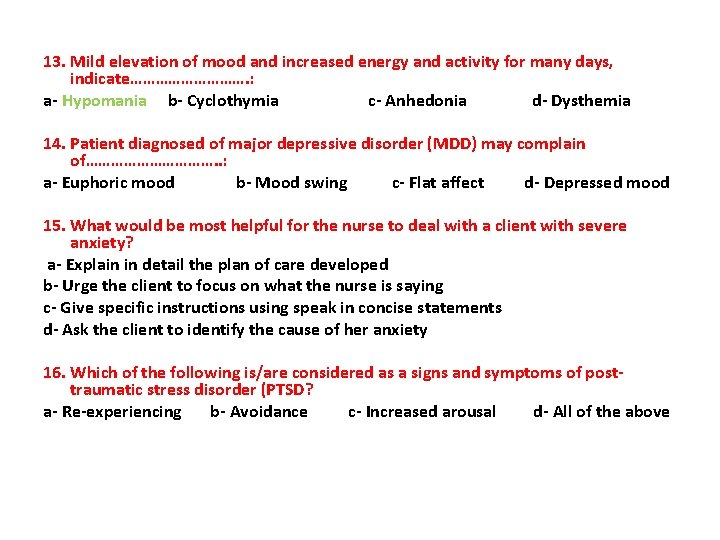
13. Mild elevation of mood and increased energy and activity for many days, indicate……………. : a- Hypomania b- Cyclothymia c- Anhedonia d- Dysthemia 14. Patient diagnosed of major depressive disorder (MDD) may complain of……………. . : a- Euphoric mood b- Mood swing c- Flat affect d- Depressed mood 15. What would be most helpful for the nurse to deal with a client with severe anxiety? a- Explain in detail the plan of care developed b- Urge the client to focus on what the nurse is saying c- Give specific instructions using speak in concise statements d- Ask the client to identify the cause of her anxiety 16. Which of the following is/are considered as a signs and symptoms of post- traumatic stress disorder (PTSD? a- Re-experiencing b- Avoidance c- Increased arousal d- All of the above
