Psoriasis Skin Cancer Revision Dermatology History PC Whats


- Slides: 28
Psoriasis & Skin Cancer Revision
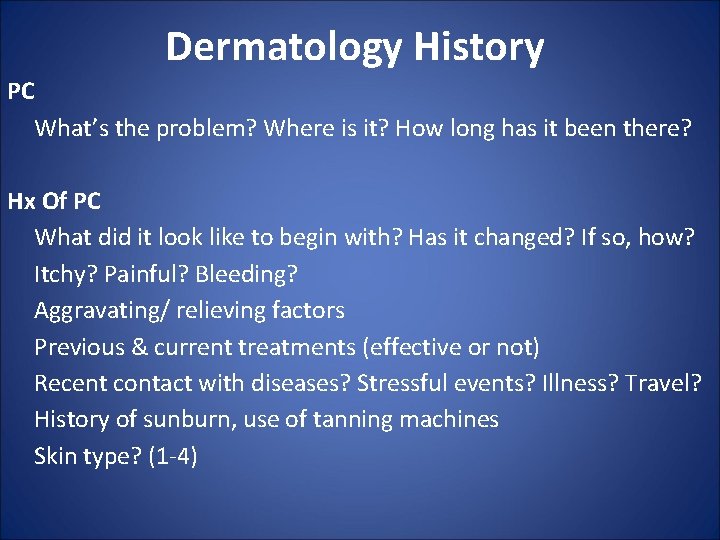
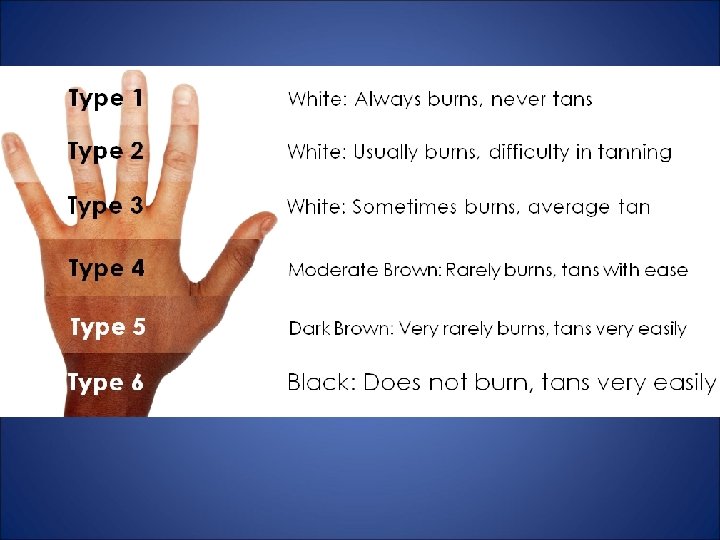
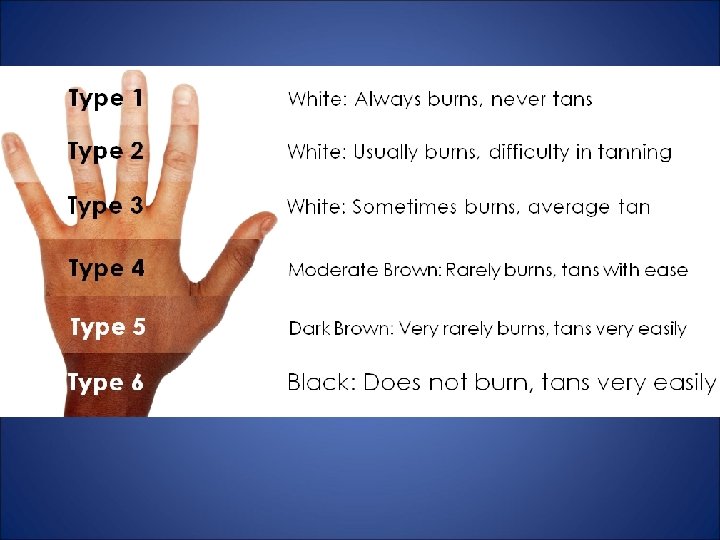
Dermatology History PC What’s the problem? Where is it? How long has it been there? Hx Of PC What did it look like to begin with? Has it changed? If so, how? Itchy? Painful? Bleeding? Aggravating/ relieving factors Previous & current treatments (effective or not) Recent contact with diseases? Stressful events? Illness? Travel? History of sunburn, use of tanning machines Skin type? (1 -4)
Past medical history History of atopy i. e. asthma, allergic rhinitis, eczema History of skin cancer & any suspicious skin lesions Medication & allergies Family history Social history Occupation- alcohol gel, over washing of hands, gloves Improvement of lesions when on annual leave Smoke/Drink? ICE

Examination • INSPECT • DESCRIBE • PALPATE • SYSTEMATIC CHECK
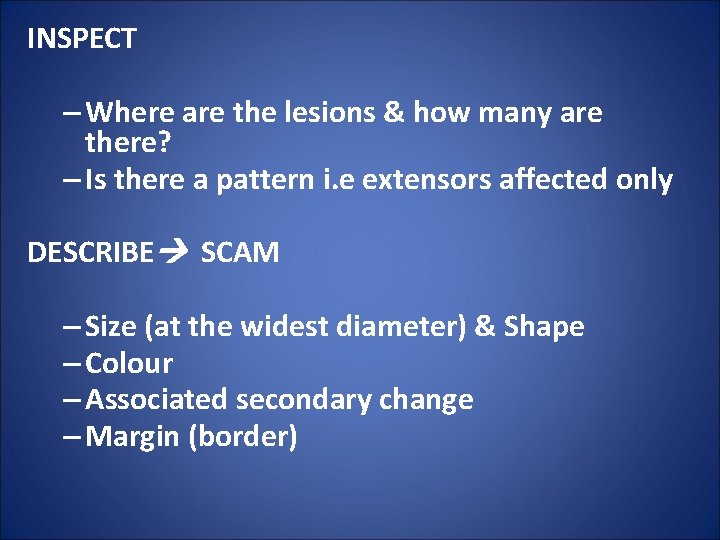
INSPECT – Where are the lesions & how many are there? – Is there a pattern i. e extensors affected only DESCRIBE SCAM – Size (at the widest diameter) & Shape – Colour – Associated secondary change – Margin (border)
If lesion is pigmented ABCDE – Asymmetry – Irregular Border – Two or more Colours within the lesion – Diameter > 6 mm – Evolution- change in size, shape over time? Started to bleed?
• PALPATE & comment on: – Consistency – Mobility – Tenderness – Temperature • SYSTEMATIC CHECK Examine: – Nails – Scalp – Hair – mucous membranes – Regional lymph nodes • General examination
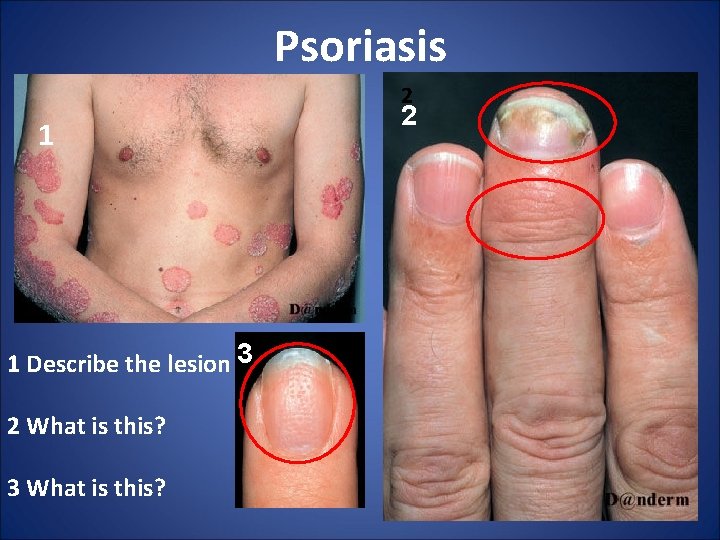
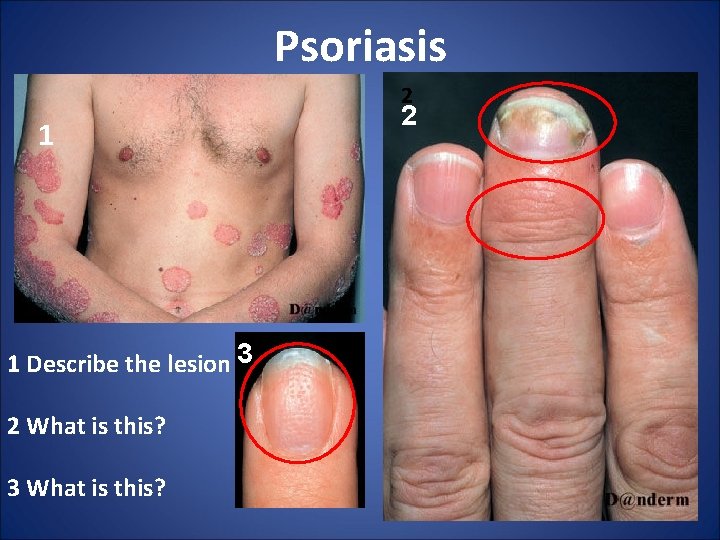
Psoriasis 2 1 1 Describe the lesion 33 2 What is this? 3 What is this? 2
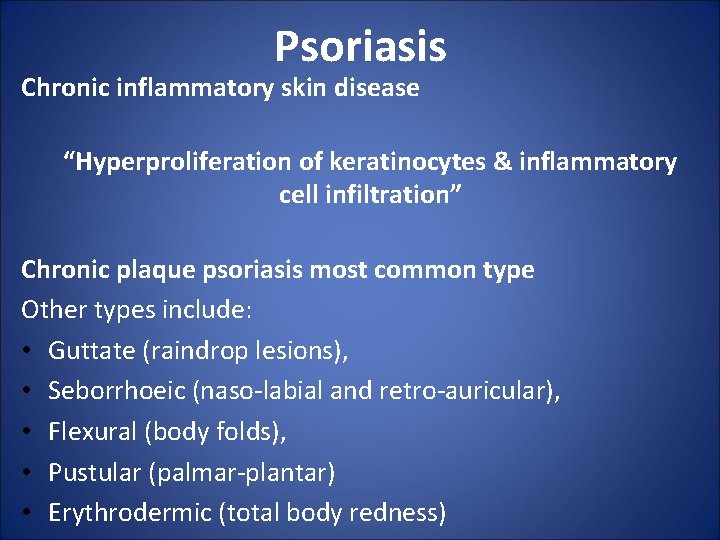
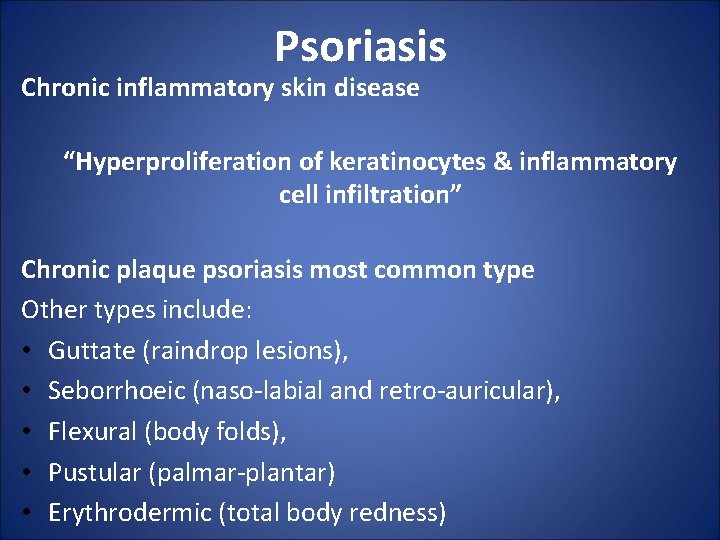
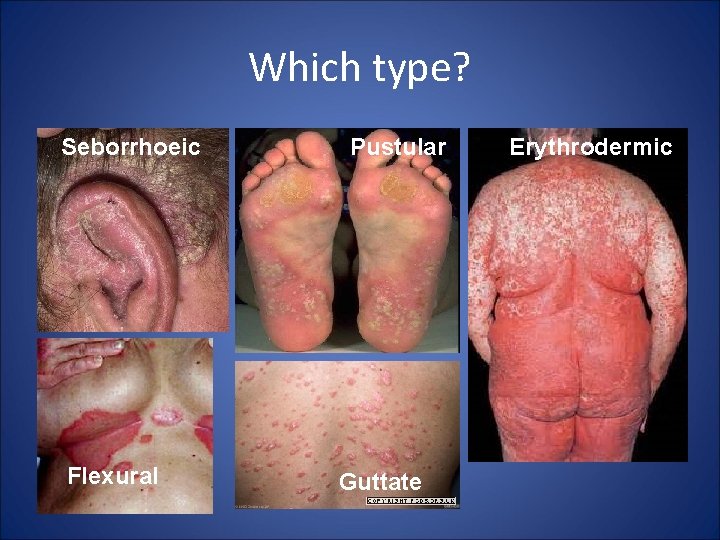
Psoriasis Chronic inflammatory skin disease “Hyperproliferation of keratinocytes & inflammatory cell infiltration” Chronic plaque psoriasis most common type Other types include: • Guttate (raindrop lesions), • Seborrhoeic (naso-labial and retro-auricular), • Flexural (body folds), • Pustular (palmar-plantar) • Erythrodermic (total body redness)
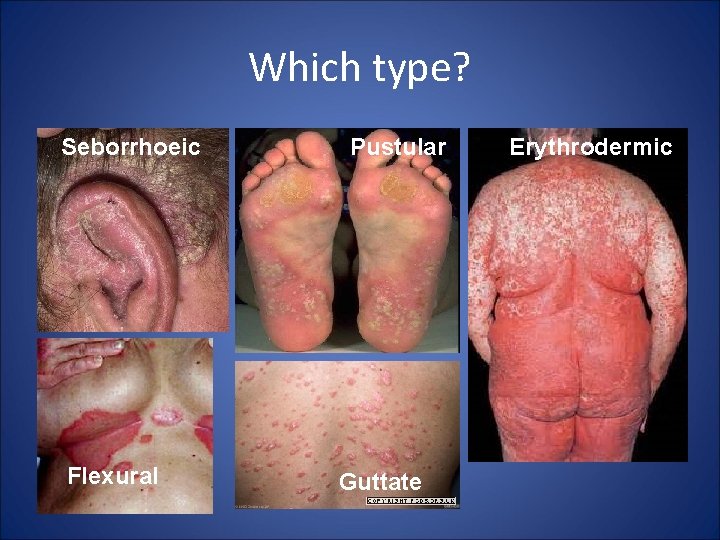
Which type? Seborrhoeic Flexural Pustular Guttate Erythrodermic
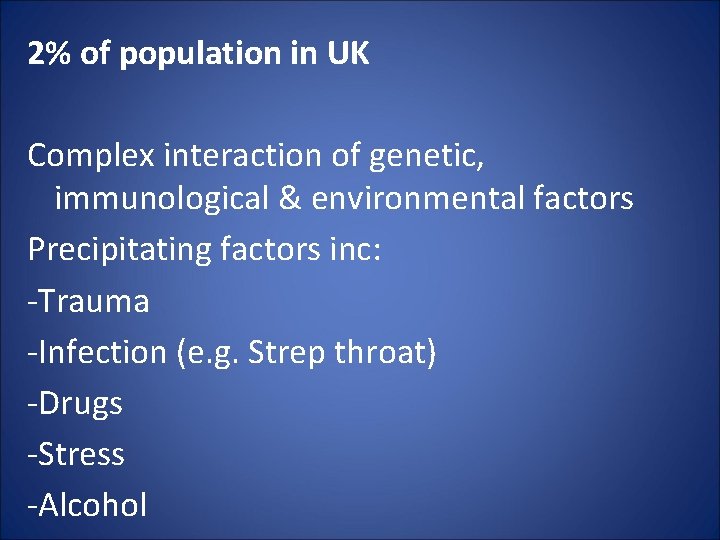
2% of population in UK Complex interaction of genetic, immunological & environmental factors Precipitating factors inc: -Trauma -Infection (e. g. Strep throat) -Drugs -Stress -Alcohol
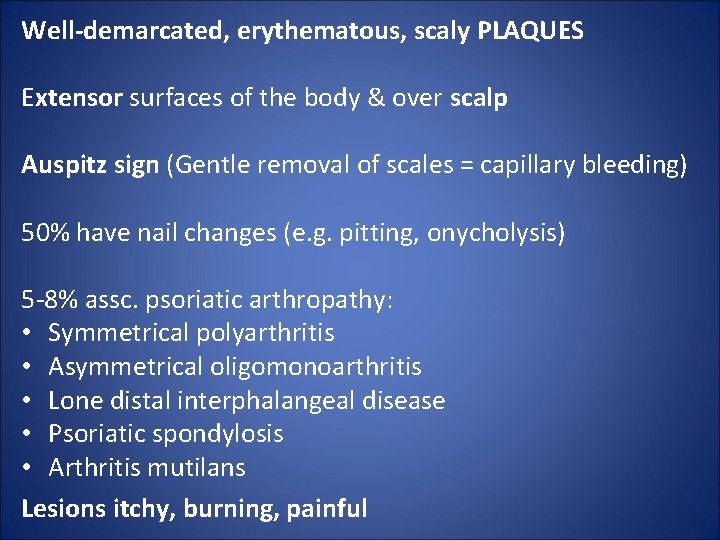
Well-demarcated, erythematous, scaly PLAQUES Extensor surfaces of the body & over scalp Auspitz sign (Gentle removal of scales = capillary bleeding) 50% have nail changes (e. g. pitting, onycholysis) 5 -8% assc. psoriatic arthropathy: • Symmetrical polyarthritis • Asymmetrical oligomonoarthritis • Lone distal interphalangeal disease • Psoriatic spondylosis • Arthritis mutilans Lesions itchy, burning, painful
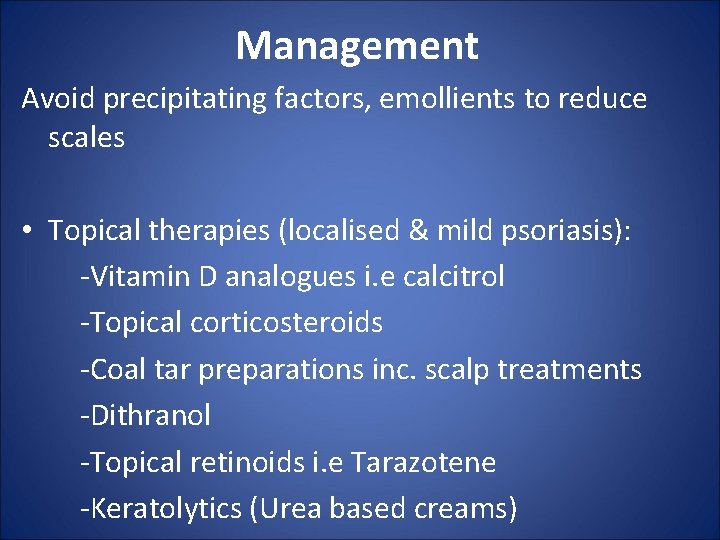
Management Avoid precipitating factors, emollients to reduce scales • Topical therapies (localised & mild psoriasis): -Vitamin D analogues i. e calcitrol -Topical corticosteroids -Coal tar preparations inc. scalp treatments -Dithranol -Topical retinoids i. e Tarazotene -Keratolytics (Urea based creams)
• Phototherapy (extensive disease) - Mainly UVA -UVB can be used when UVA fails- can cause sunburn • Oral therapies (extensive, severe psoriasis & psoriasis with systemic involvement) -Methotrexate -Retinoids -Ciclosporin -Mycophenolate mofetil -Biological agents (e. g. infliximab, etanercept, efalizumab)

Skin Cancer Skin SCC BCC Solar Keratosis Malignant Melanoma
Skin cancer can be divided into: • Non-melanoma (basal cell carcinoma & squamous cell carcinoma) • Melanoma (malignant melanoma).
Basal Cell Carcinoma Slow-growing, locally invasive tumour epidermal keratinocytes- affect basal layers of skin Malignant but rarely metastasises Most common malignant skin tumour Risk factors include: -UV exposure -History of frequent/ severe sunburn in childhood -Skin type 1 -Increasing age -Being male -Immunosuppression -Previous history of skin cancer -Genetic predisposition
Nodular most common Small, skin-coloured papule or nodule Surface telangiectasia, Pearly rolled edge May have necrotic/ ulcerated centre rodent ulcer Head & neck involvement Management • Surgical excision • Radiotherapy - when surgery is not appropriate • Cryotherapy • Topical photodynamic therapy • Topical treatment (imiquimod cream) -small, lowrisk lesions
Squamous Cell Carcinoma Locally invasive malignant tumour of epidermal keratinocytes - affect squamous layer of skin. Potential to metastasise • • • Causes Risk factors include: Excessive UV exposure Actinic/ Solar keratoses chronic inflammation (leg ulcers, wound scars) Immunosuppression Genetic predisposition
Keratotic (scaly, crusty), ill-defined nodule May ulcerate Management • Surgical excision - treatment of choice • Radiotherapy - for large, non-resectable tumours
Malignant Melanoma Invasive malignant tumour of epidermal melanocytes Potential to metastasise Causes Risk factors include: • Excessive UV exposure • Skin type 1 • History of multiple moles/ atypical moles • Family history or previous history of melanoma The ‘ABCDE Symptoms’ rule → What are they? Legs in women & trunk in men
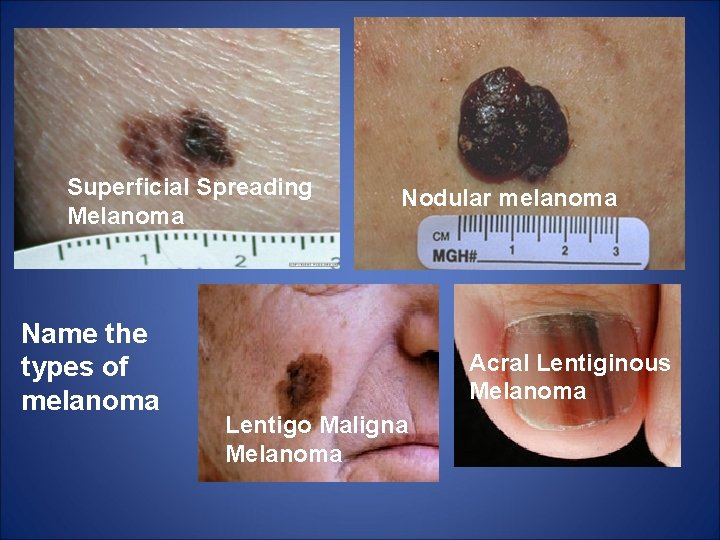
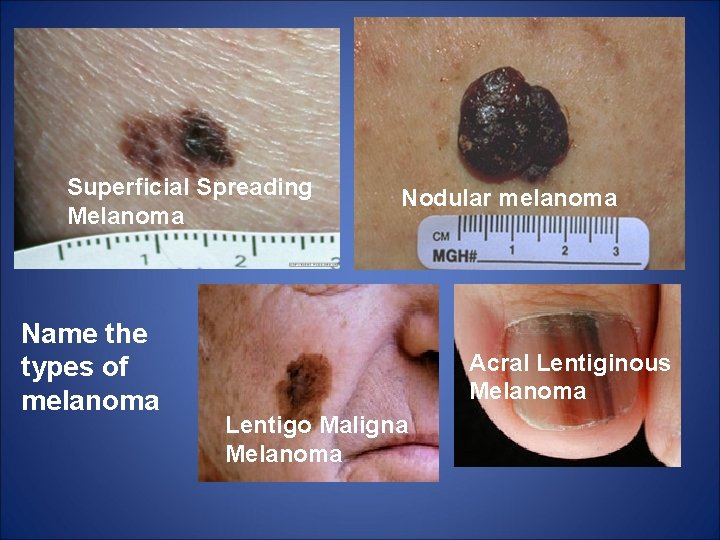
Superficial Spreading Melanoma Name the types of melanoma Nodular melanoma Acral Lentiginous Melanoma Lentigo Maligna Melanoma
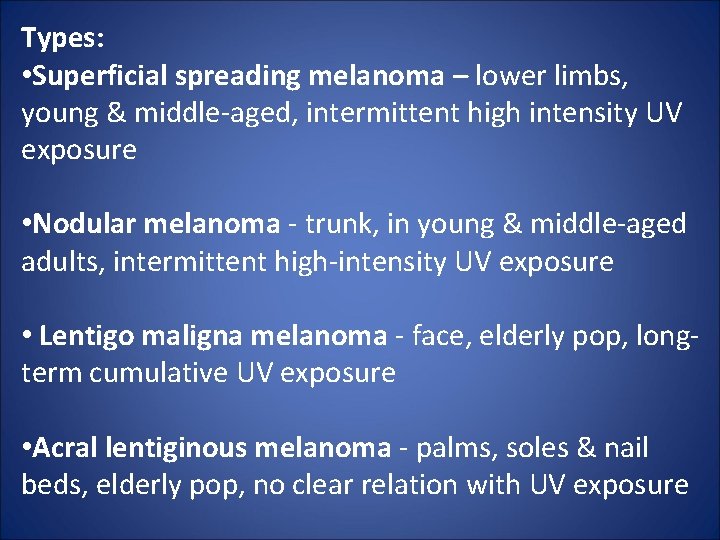
Types: • Superficial spreading melanoma – lower limbs, young & middle-aged, intermittent high intensity UV exposure • Nodular melanoma - trunk, in young & middle-aged adults, intermittent high-intensity UV exposure • Lentigo maligna melanoma - face, elderly pop, longterm cumulative UV exposure • Acral lentiginous melanoma - palms, soles & nail beds, elderly pop, no clear relation with UV exposure
Management • Surgical excision • Radiotherapy • Chemotherapy for mets
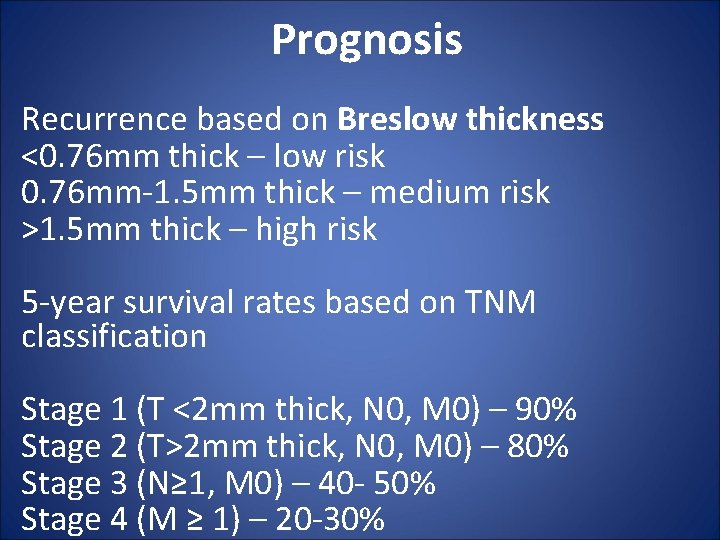
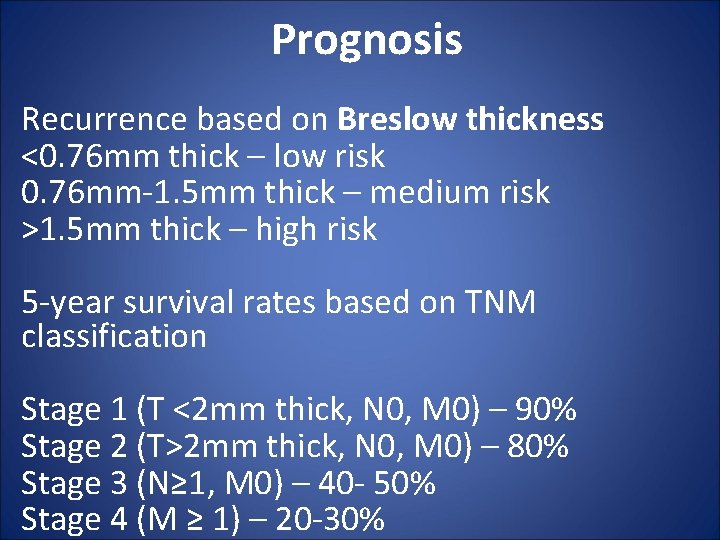
Prognosis Recurrence based on Breslow thickness <0. 76 mm thick – low risk 0. 76 mm-1. 5 mm thick – medium risk >1. 5 mm thick – high risk 5 -year survival rates based on TNM classification Stage 1 (T <2 mm thick, N 0, M 0) – 90% Stage 2 (T>2 mm thick, N 0, M 0) – 80% Stage 3 (N≥ 1, M 0) – 40 - 50% Stage 4 (M ≥ 1) – 20 -30%
Thank You For Listening & Good Luck