Proximal humeral fracturesan update on treatment protocols AO

- Slides: 41
Proximal humeral fractures—an update on treatment protocols AO Trauma Basic Principles Course
Learning objectives • Describe the different approaches to treatment • Consider minimally invasive osteosynthesis (MIO) as an option • Discuss the advantage of locking plate constructs and other treatment options (IM nailing)
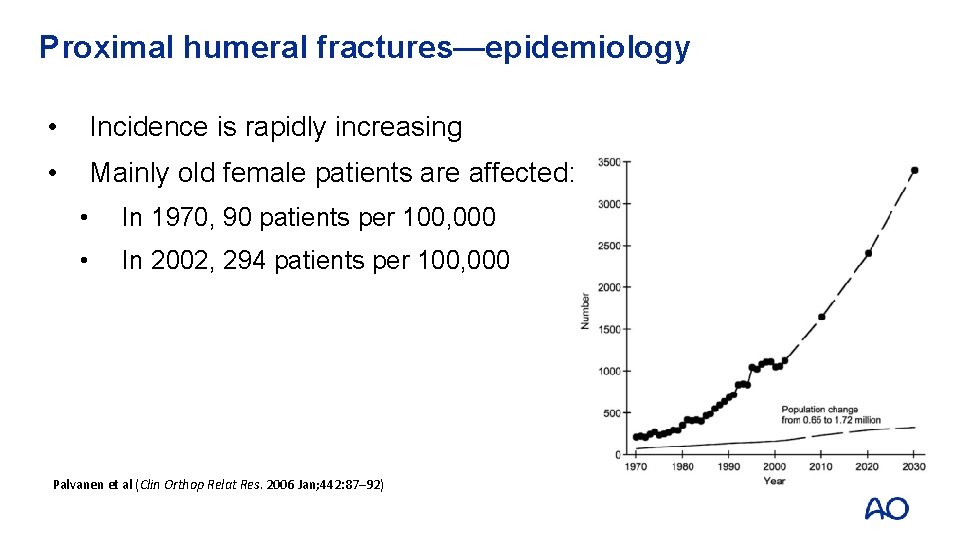
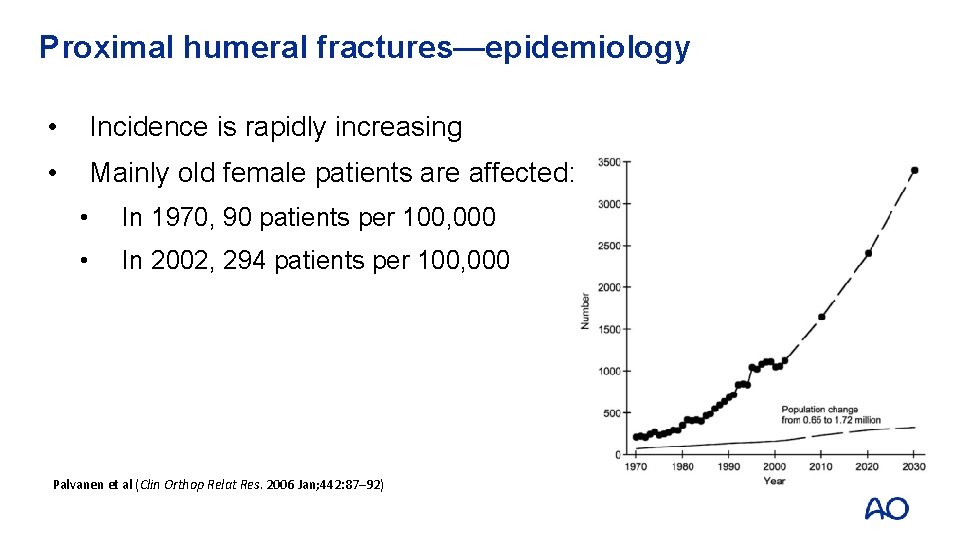
Proximal humeral fractures—epidemiology • Incidence is rapidly increasing • Mainly old female patients are affected: • In 1970, 90 patients per 100, 000 • In 2002, 294 patients per 100, 000 Palvanen et al (Clin Orthop Relat Res. 2006 Jan; 442: 87– 92)
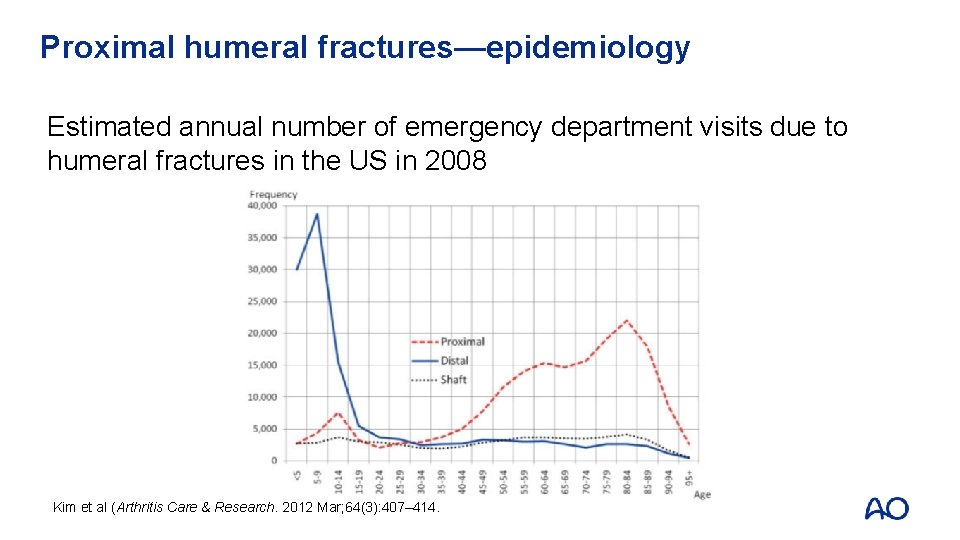
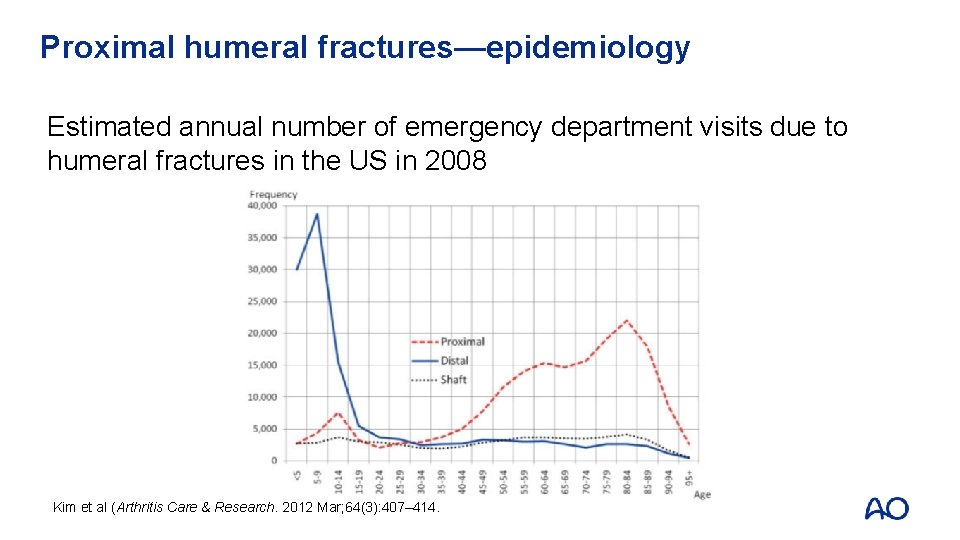
Proximal humeral fractures—epidemiology Estimated annual number of emergency department visits due to humeral fractures in the US in 2008 Kim et al (Arthritis Care & Research. 2012 Mar; 64(3): 407– 414.
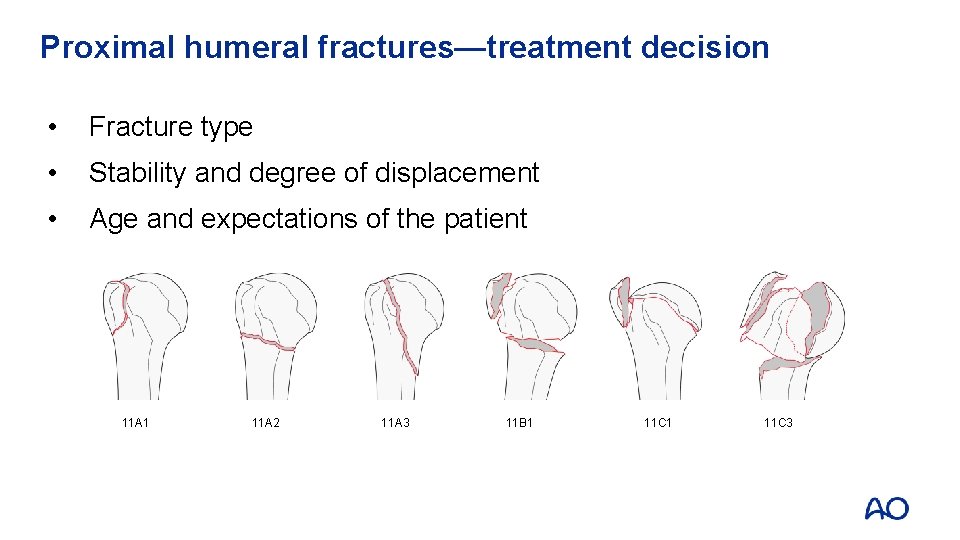
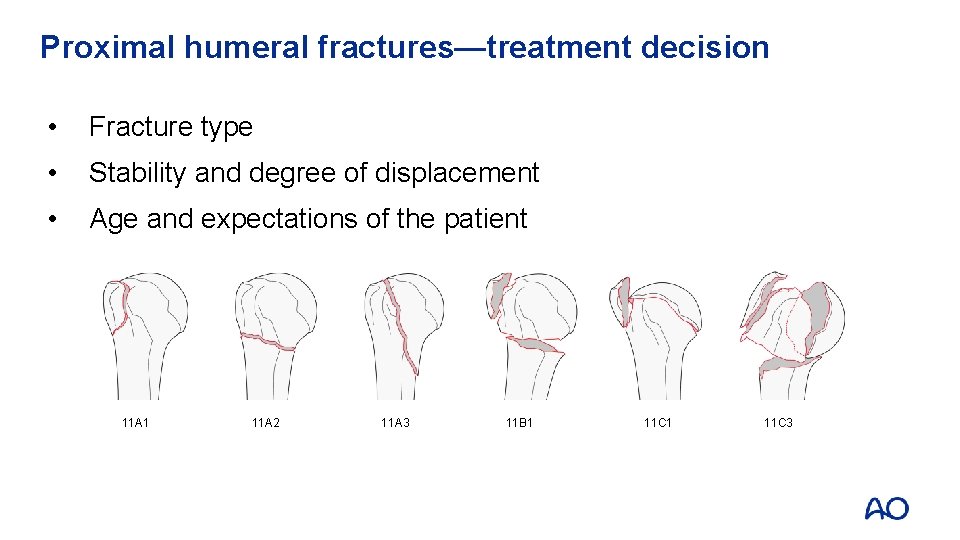
Proximal humeral fractures—treatment decision • Fracture type • Stability and degree of displacement • Age and expectations of the patient 11 A 1 11 A 2 11 A 3 11 B 1 11 C 3
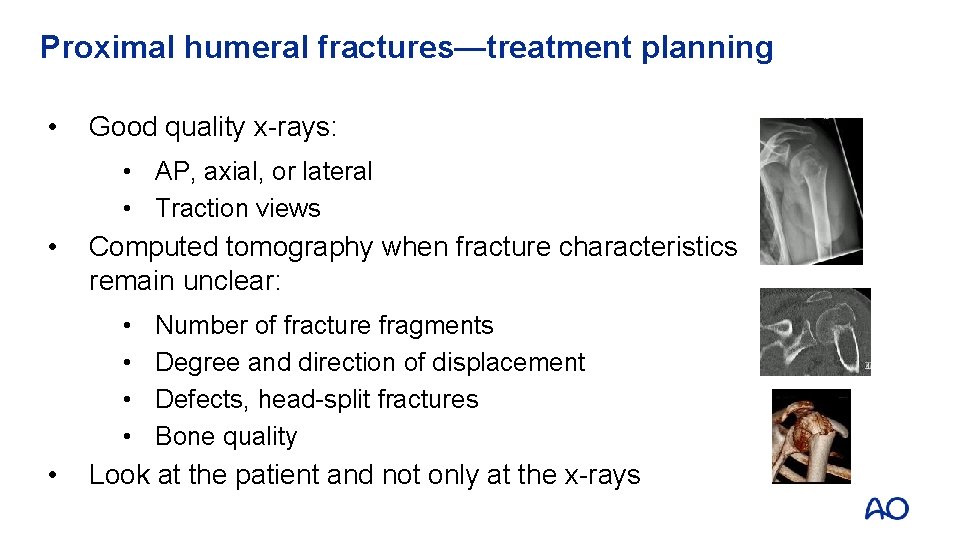
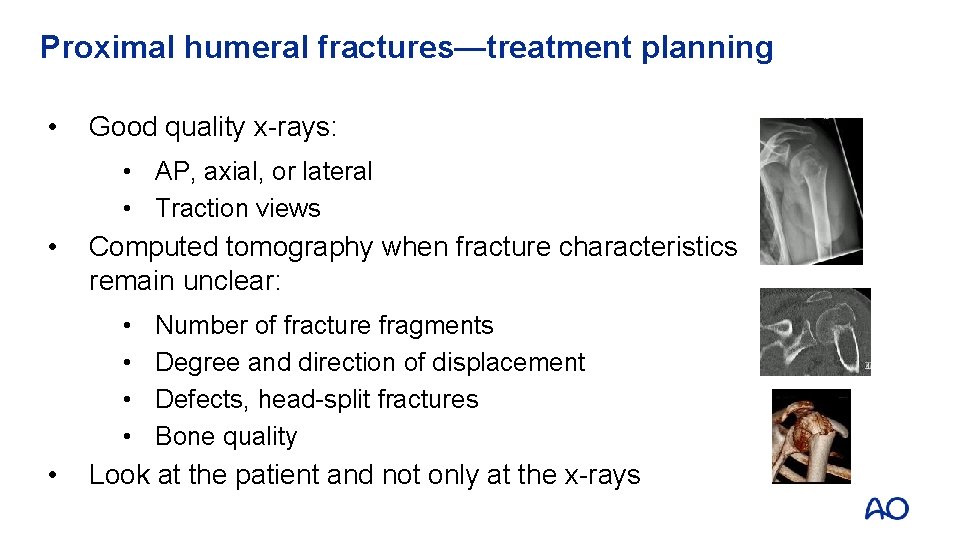
Proximal humeral fractures—treatment planning • Good quality x-rays: • AP, axial, or lateral • Traction views • Computed tomography when fracture characteristics remain unclear: • • • Number of fracture fragments Degree and direction of displacement Defects, head-split fractures Bone quality Look at the patient and not only at the x-rays
Proximal humeral fractures—treatment options • Nonoperative • Minimally invasive osteosynthesis • Plate osteosynthesis • Intramedullary (IM) osteosynthesis (IM nailing) • Endoprosthetic replacement
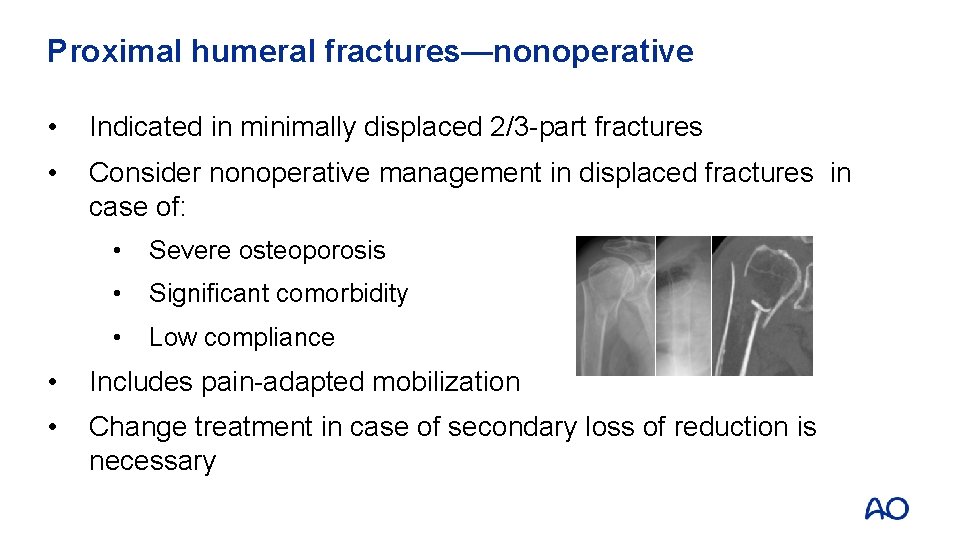
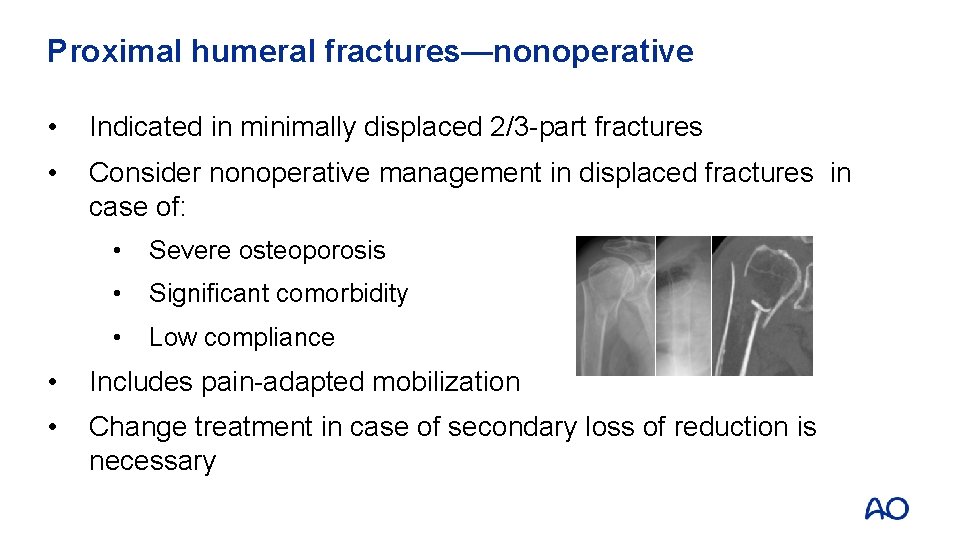
Proximal humeral fractures—nonoperative • Indicated in minimally displaced 2/3 -part fractures • Consider nonoperative management in displaced fractures in case of: • Severe osteoporosis • Significant comorbidity • Low compliance • Includes pain-adapted mobilization • Change treatment in case of secondary loss of reduction is necessary
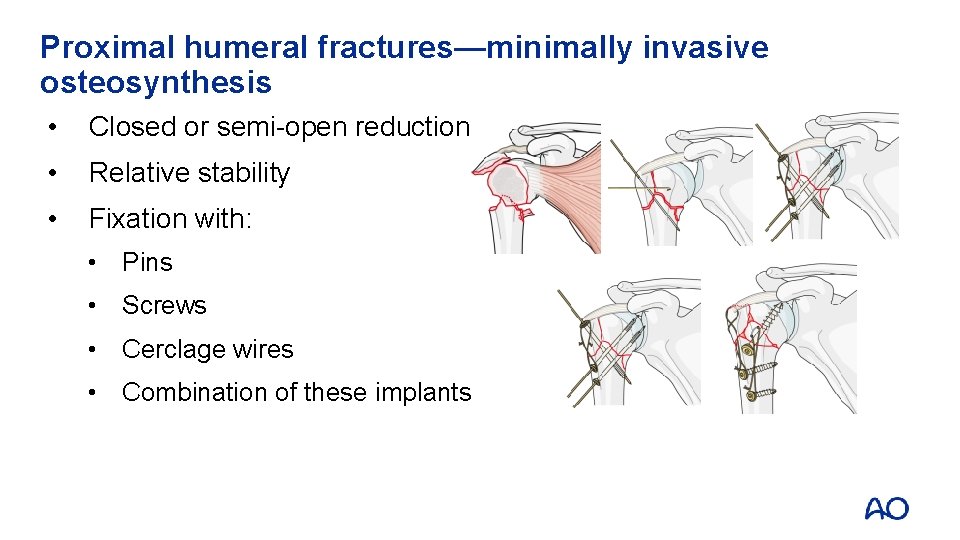
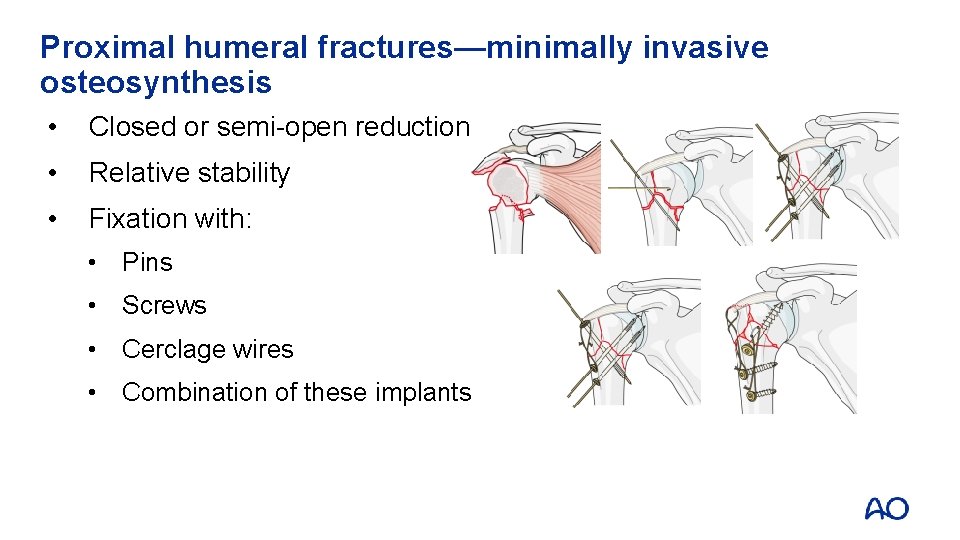
Proximal humeral fractures—minimally invasive osteosynthesis • Closed or semi-open reduction • Relative stability • Fixation with: • Pins • Screws • Cerclage wires • Combination of these implants
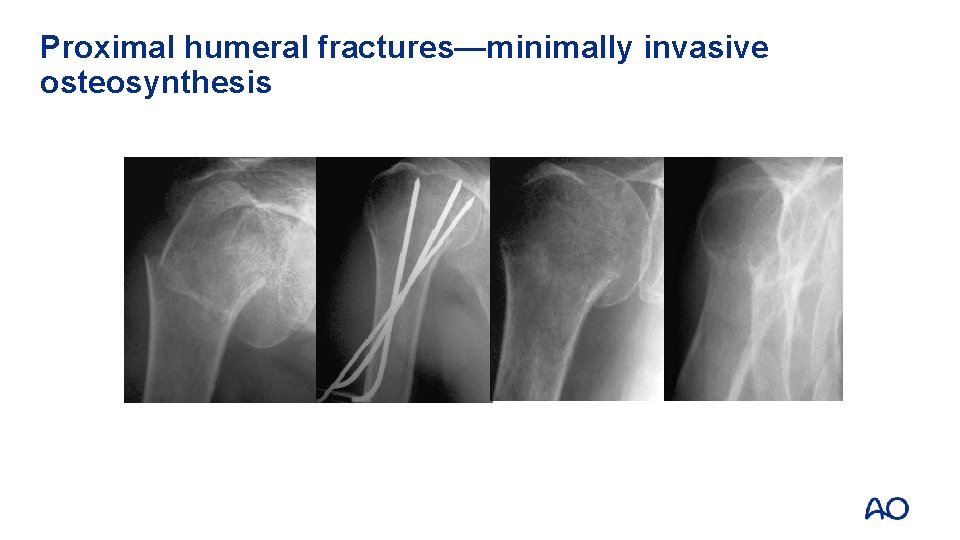
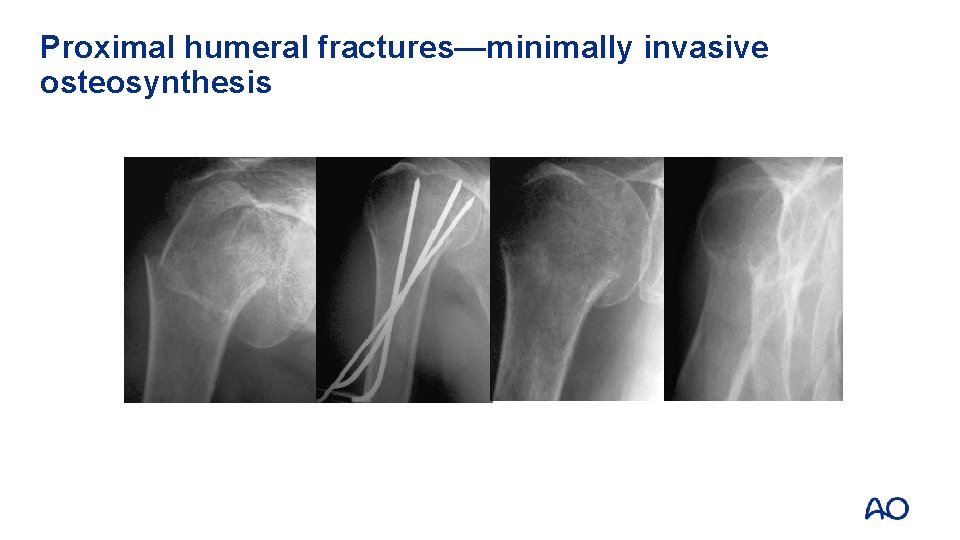
Proximal humeral fractures—minimally invasive osteosynthesis
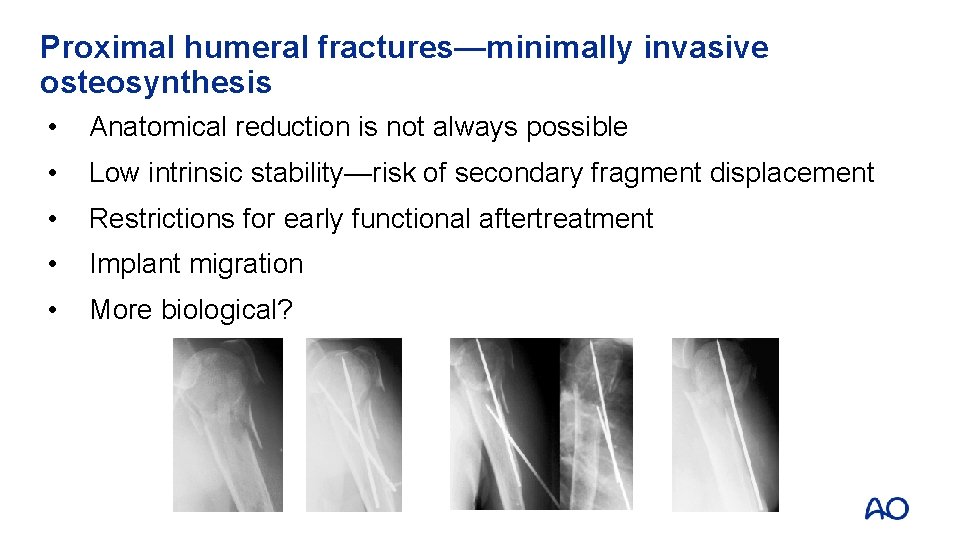
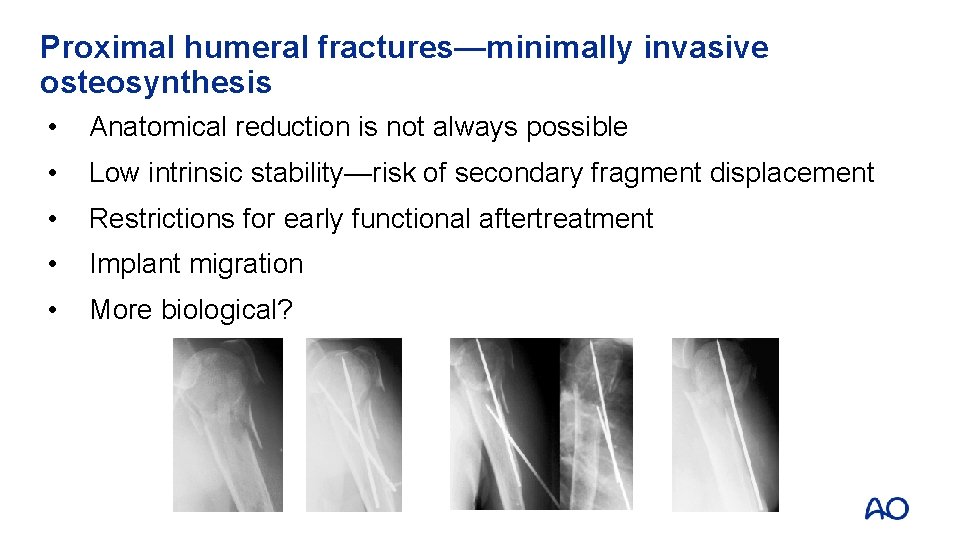
Proximal humeral fractures—minimally invasive osteosynthesis • Anatomical reduction is not always possible • Low intrinsic stability—risk of secondary fragment displacement • Restrictions for early functional aftertreatment • Implant migration • More biological?
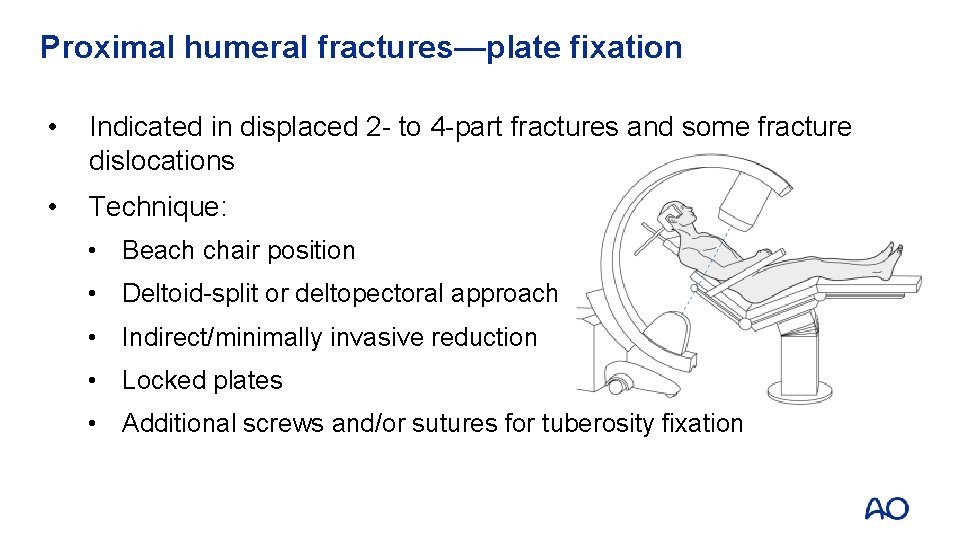
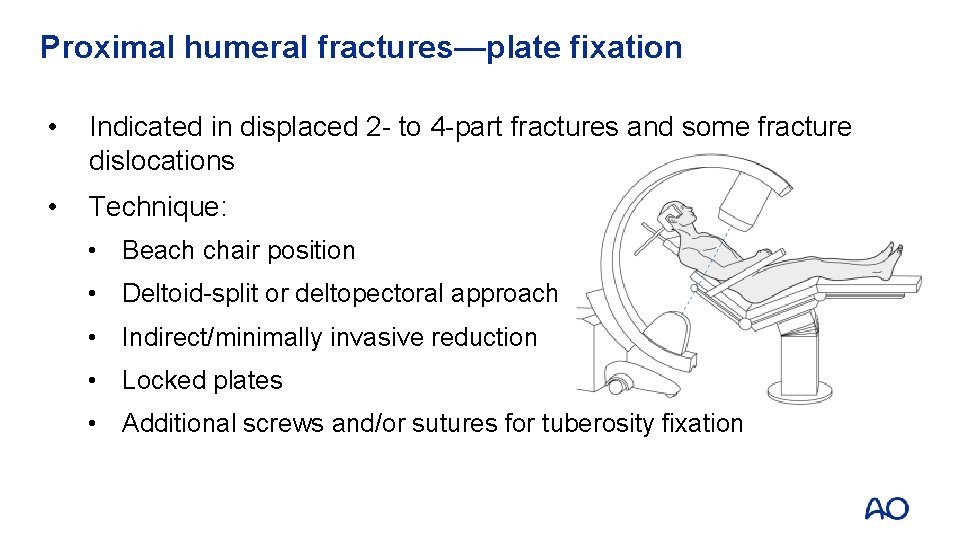
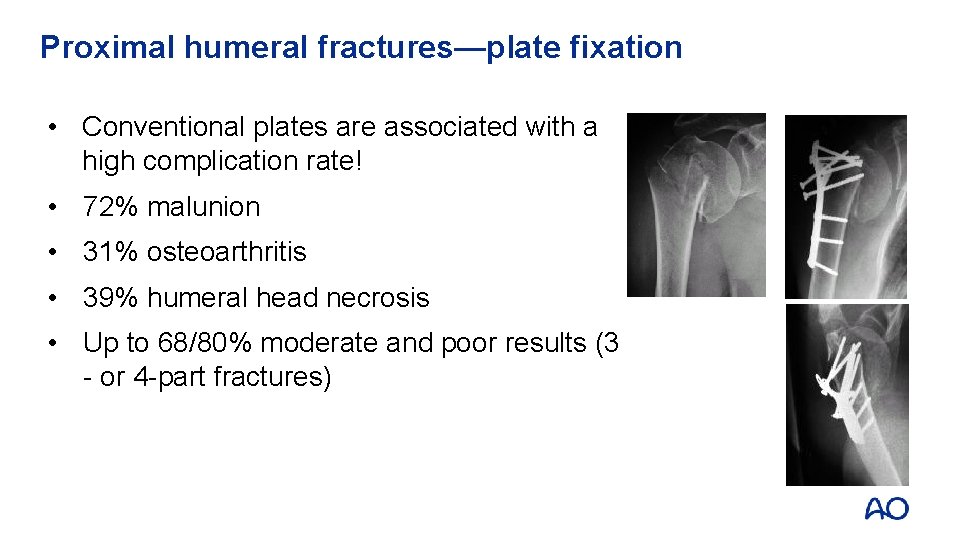
Proximal humeral fractures—plate fixation • Indicated in displaced 2 - to 4 -part fractures and some fracture dislocations • Technique: • Beach chair position • Deltoid-split or deltopectoral approach • Indirect/minimally invasive reduction • Locked plates • Additional screws and/or sutures for tuberosity fixation
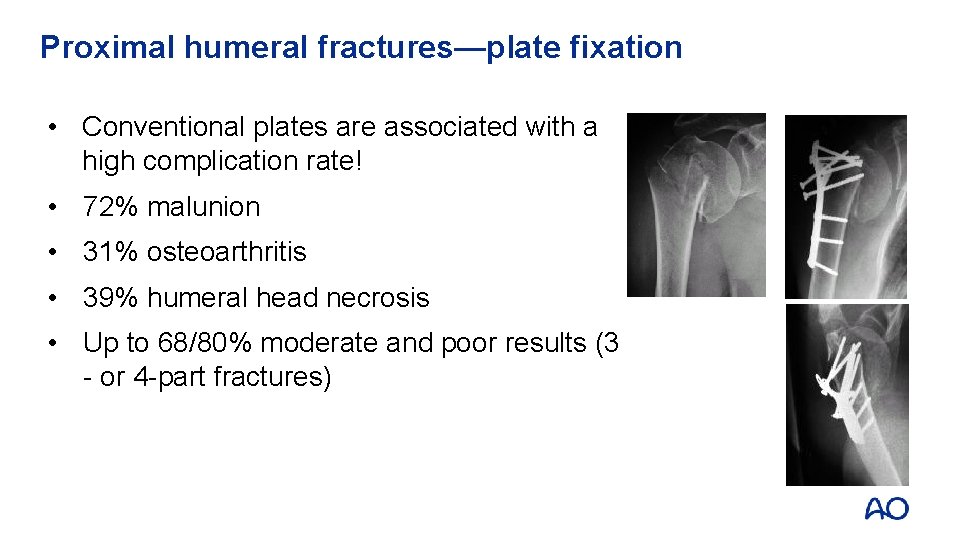
Proximal humeral fractures—plate fixation • Conventional plates are associated with a high complication rate! • 72% malunion • 31% osteoarthritis • 39% humeral head necrosis • Up to 68/80% moderate and poor results (3 - or 4 -part fractures)

Proximal humeral fractures—plate fixation Locked plates: • Biomechanically more stable • Better adapted to the anatomy But: • Bone-implant interface is more demanding • Implants have their specific complications
Proximal humeral fractures—locked plate fixation Outcomes: • Satisfactory to excellent results: 68– 87% • Constant scores: 60– 85/100 • Reoperation rate: 9– 25%
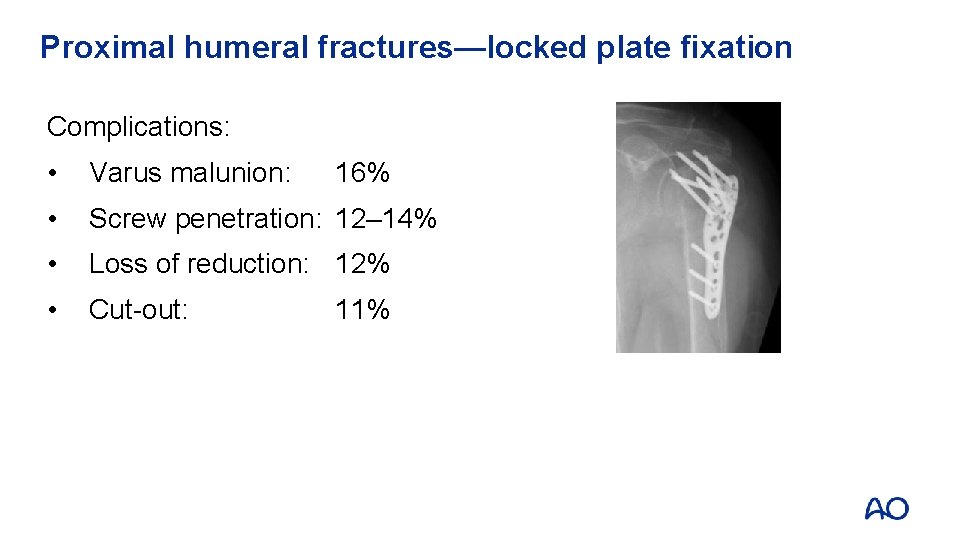
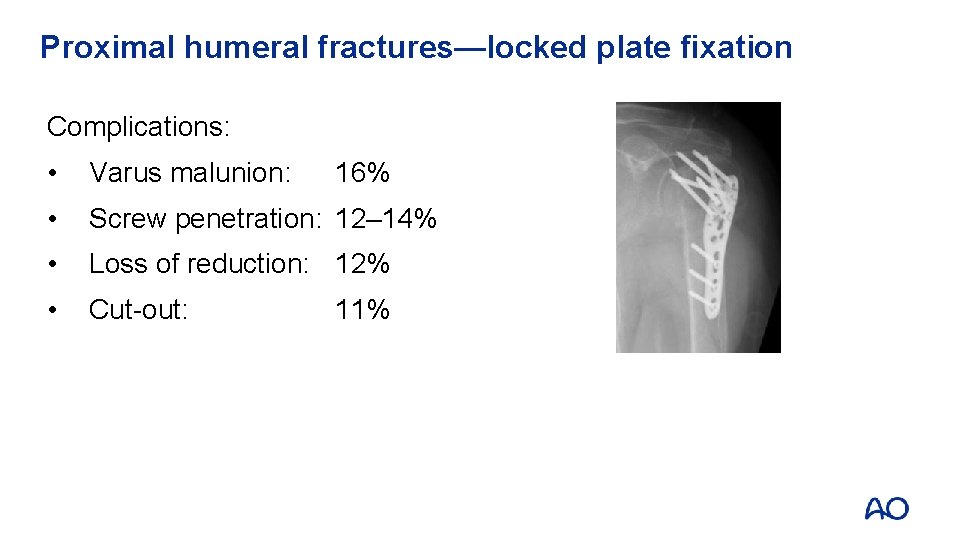
Proximal humeral fractures—locked plate fixation Complications: • Varus malunion: • Screw penetration: 12– 14% • Loss of reduction: 12% • Cut-out: 16% 11%
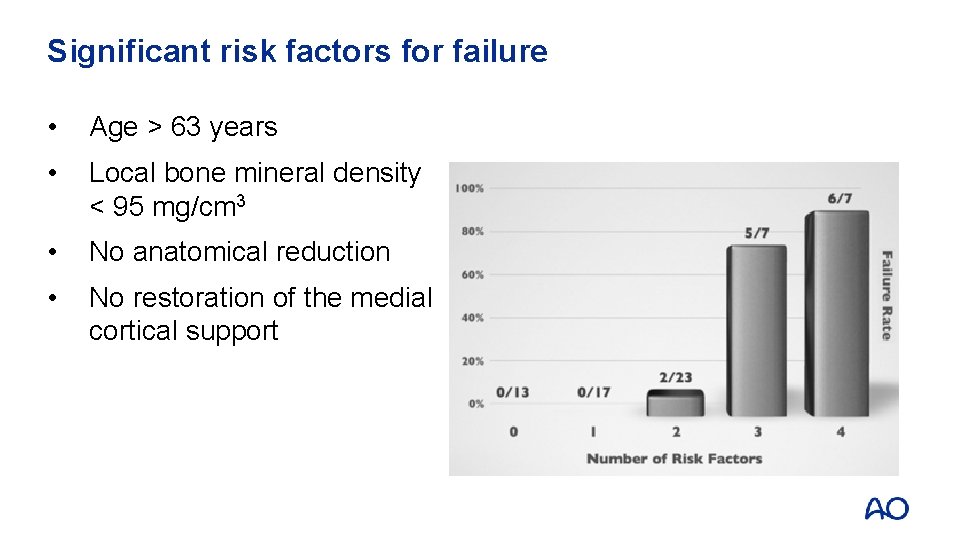
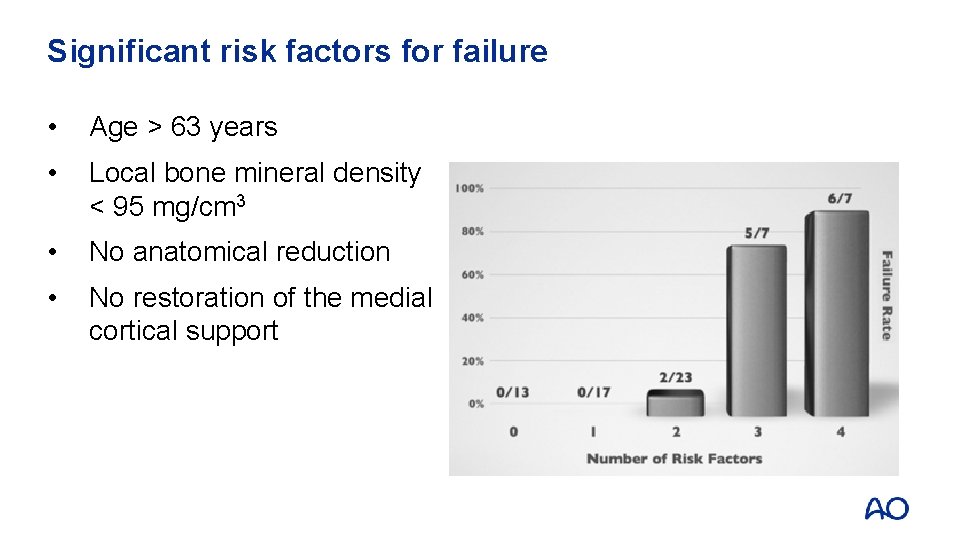
Significant risk factors for failure • Age > 63 years • Local bone mineral density < 95 mg/cm 3 • No anatomical reduction • No restoration of the medial cortical support
Factors for functional outcome • Significant determinants: • Age • Gender • Treatment • Intra-/postoperative complications • Anatomical restoration • Prevention of local complications, in particular those leading to severe varus deviation, appears essential to improving shoulder function
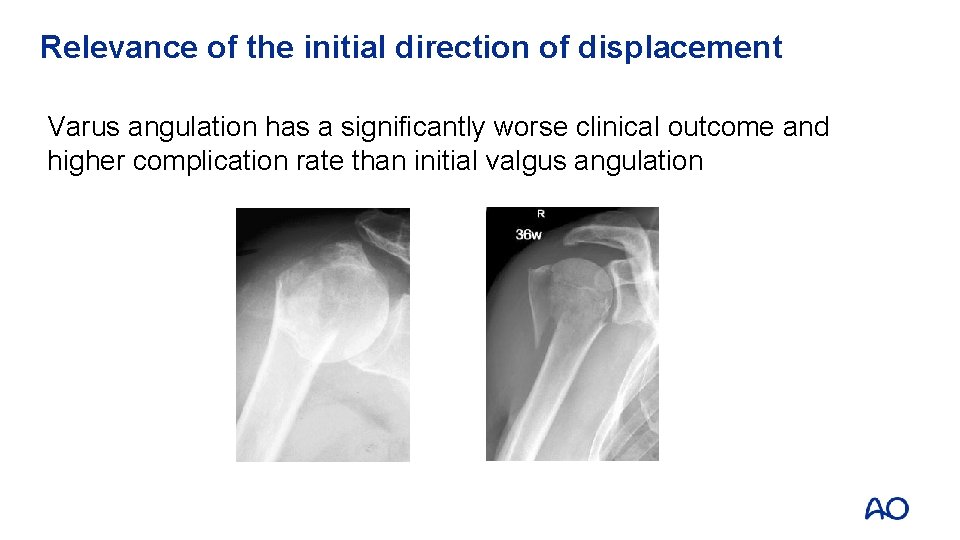
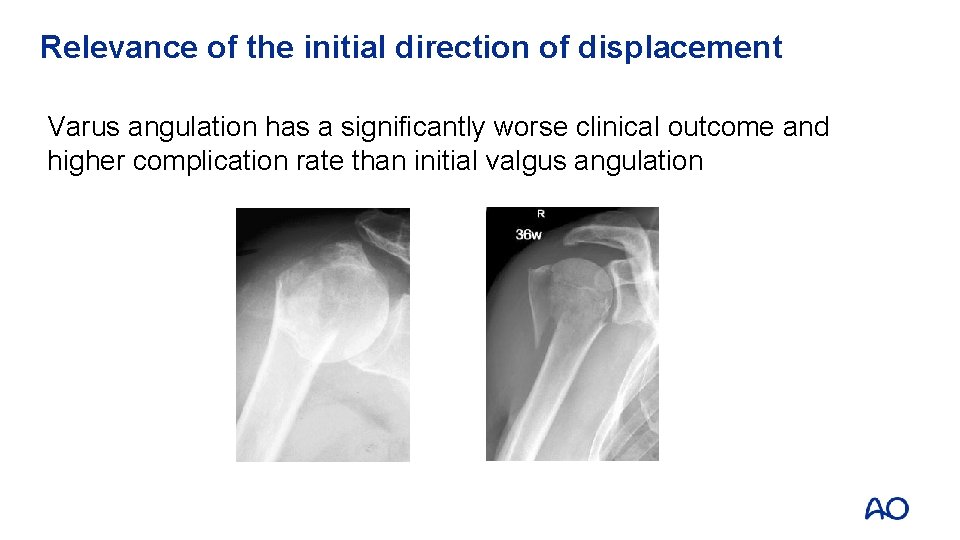
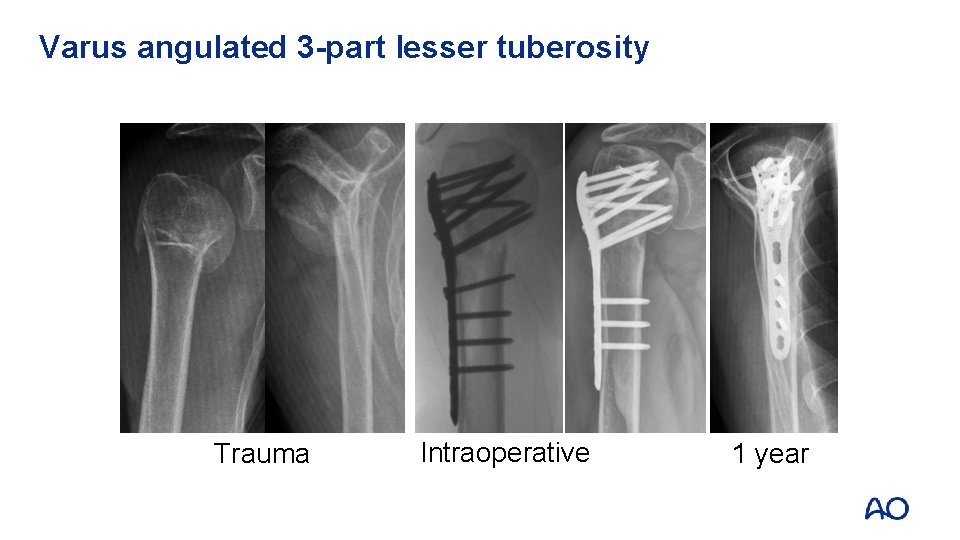
Relevance of the initial direction of displacement Varus angulation has a significantly worse clinical outcome and higher complication rate than initial valgus angulation
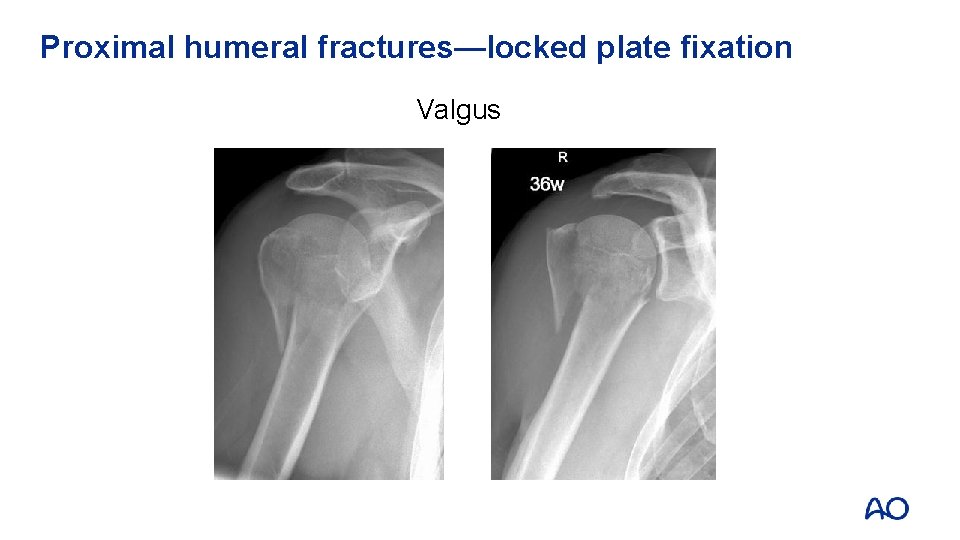
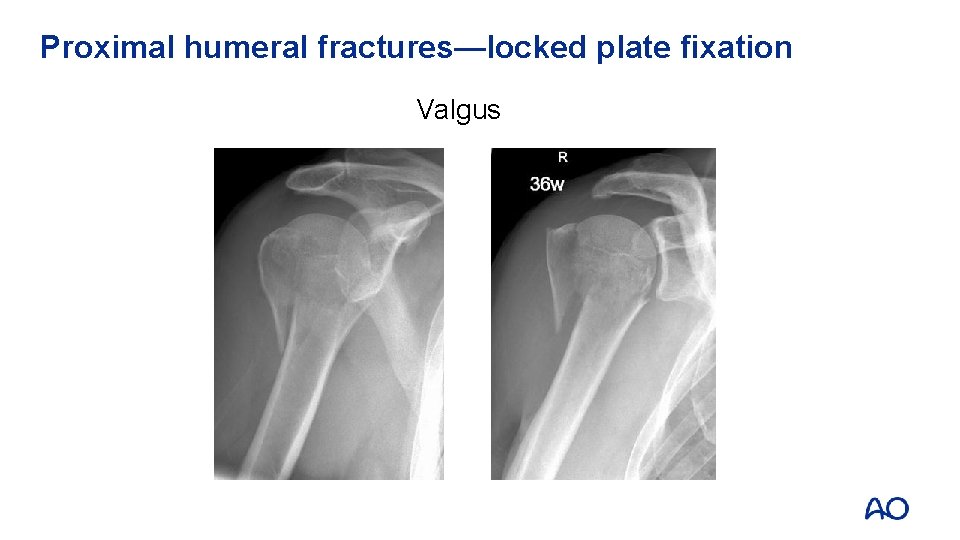
Proximal humeral fractures—locked plate fixation Valgus
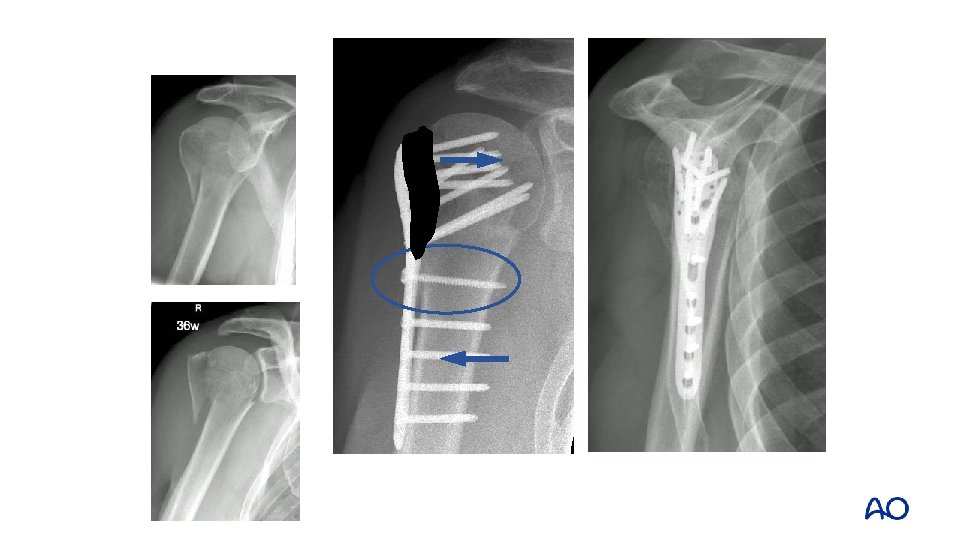
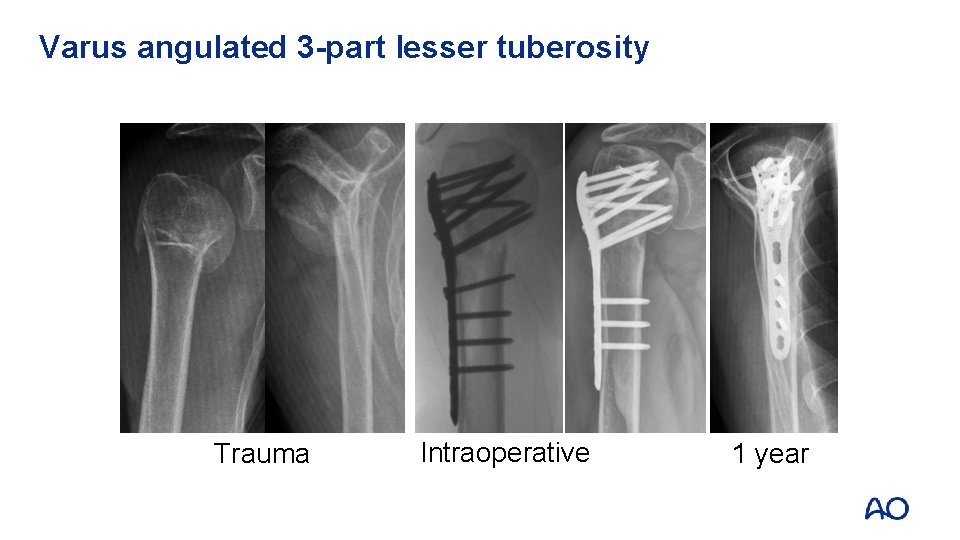
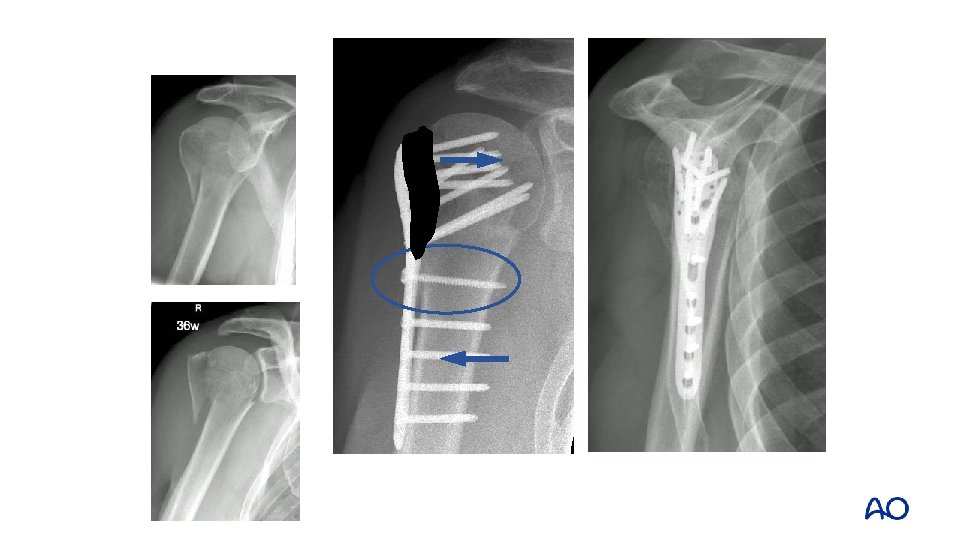
Varus angulated 3 -part lesser tuberosity Trauma Intraoperative 1 year
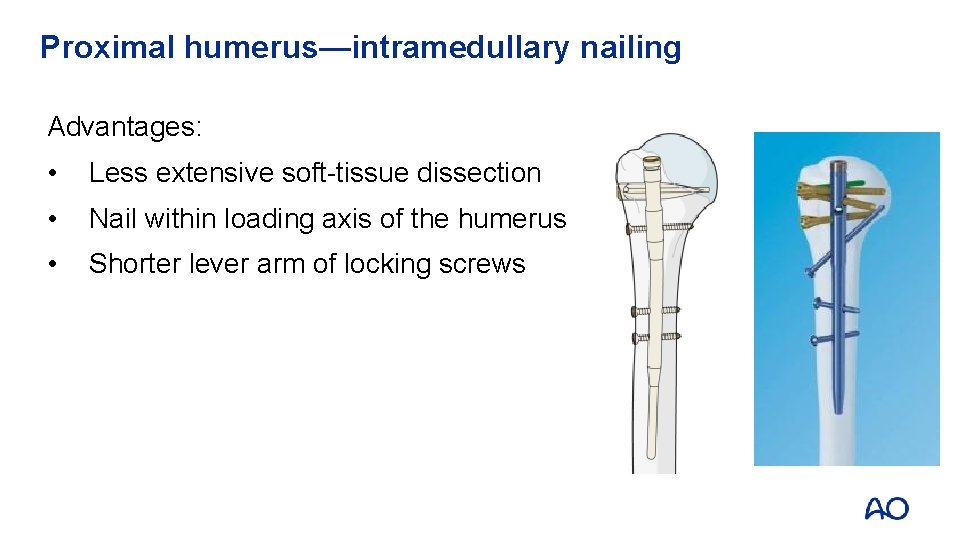
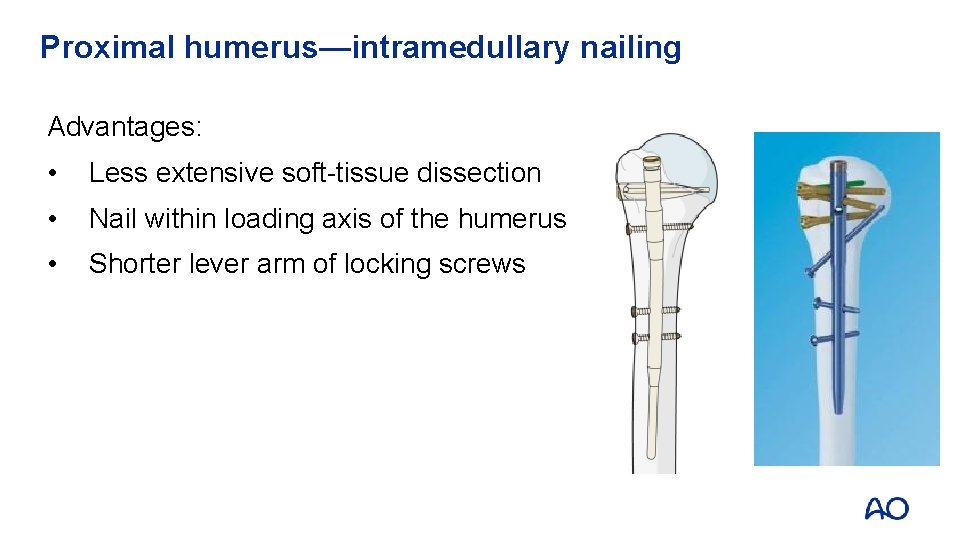
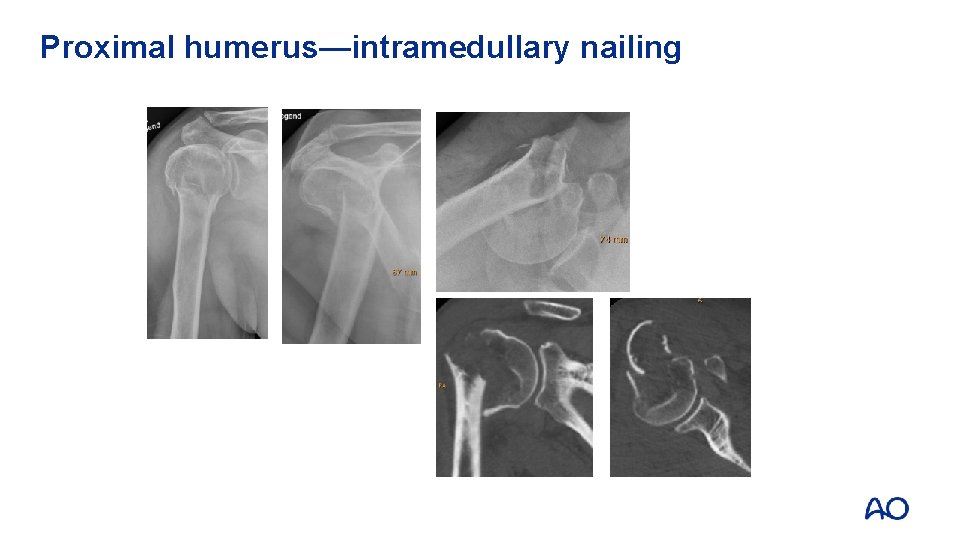
Proximal humerus—intramedullary nailing Advantages: • Less extensive soft-tissue dissection • Nail within loading axis of the humerus • Shorter lever arm of locking screws
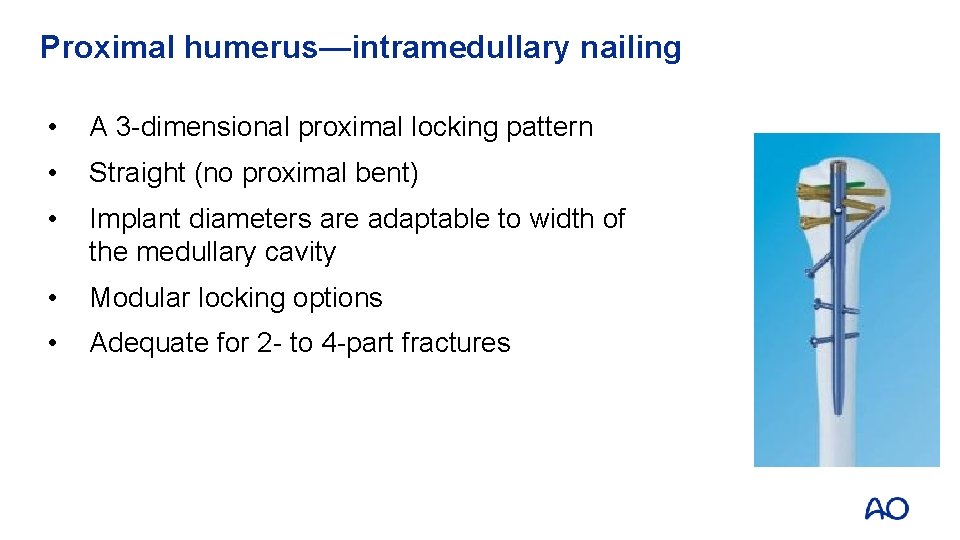
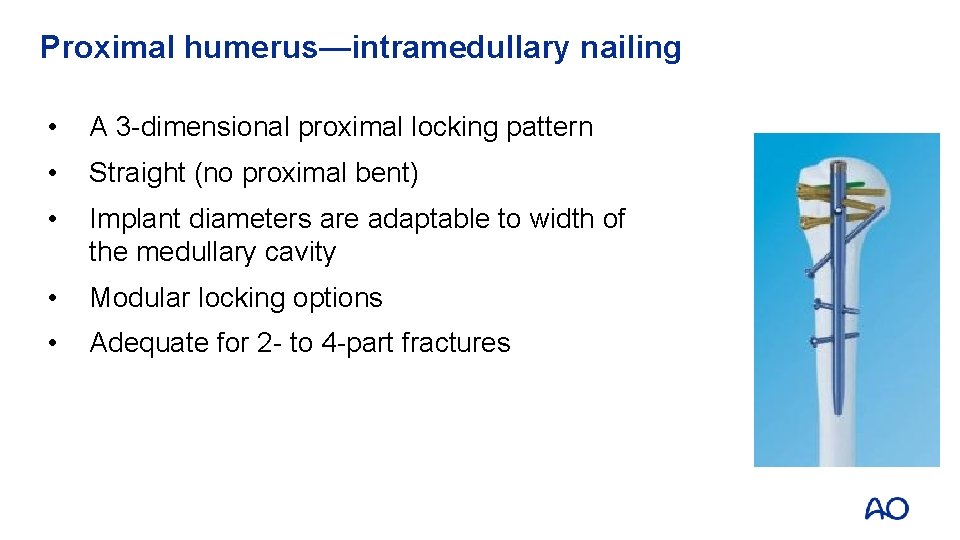
Proximal humerus—intramedullary nailing • A 3 -dimensional proximal locking pattern • Straight (no proximal bent) • Implant diameters are adaptable to width of the medullary cavity • Modular locking options • Adequate for 2 - to 4 -part fractures
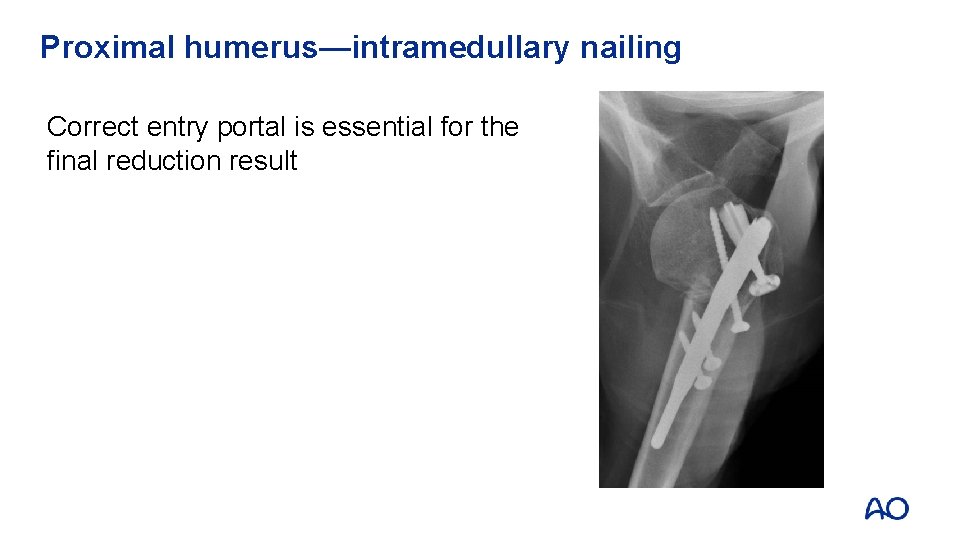
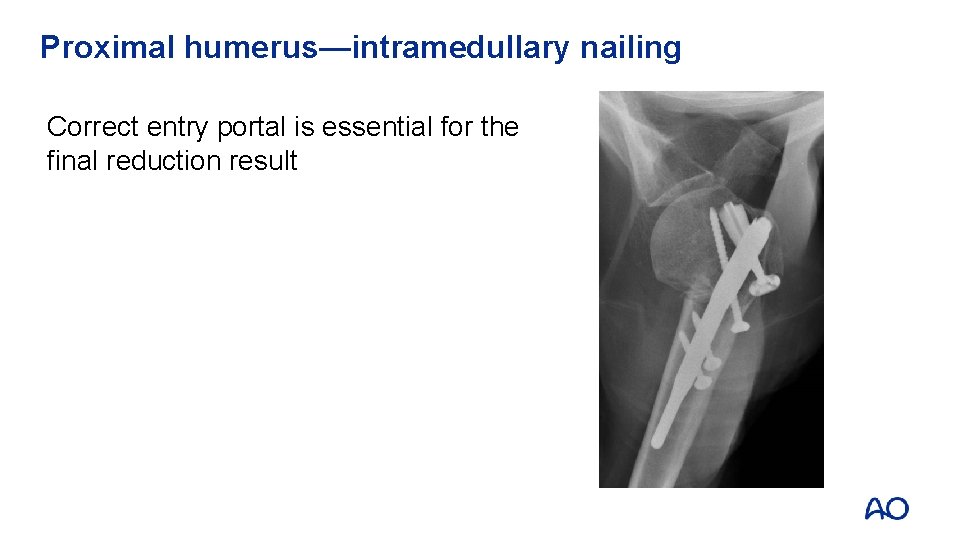
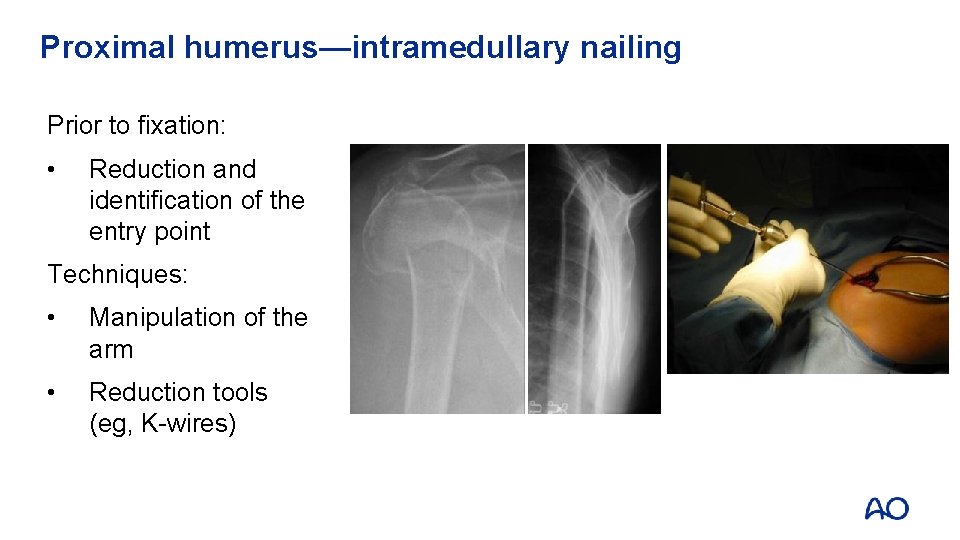
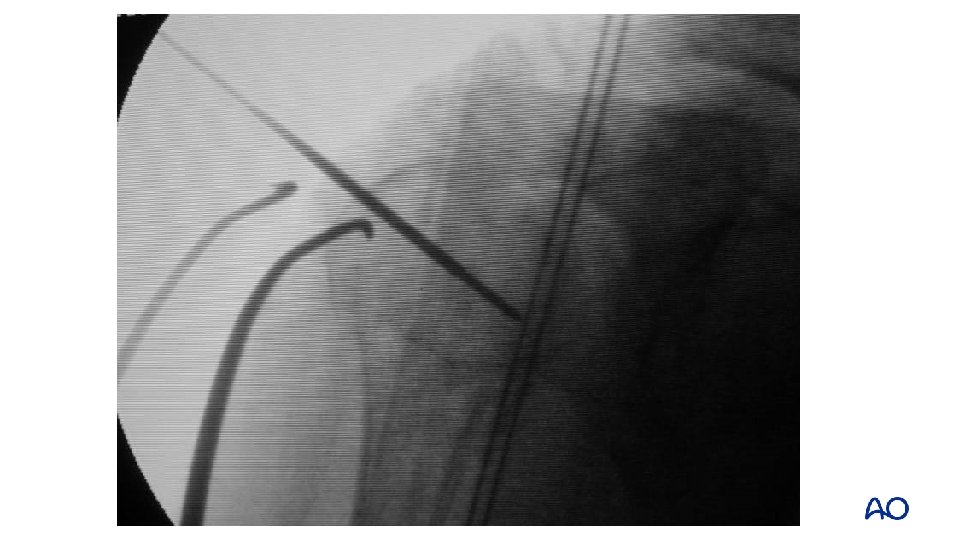
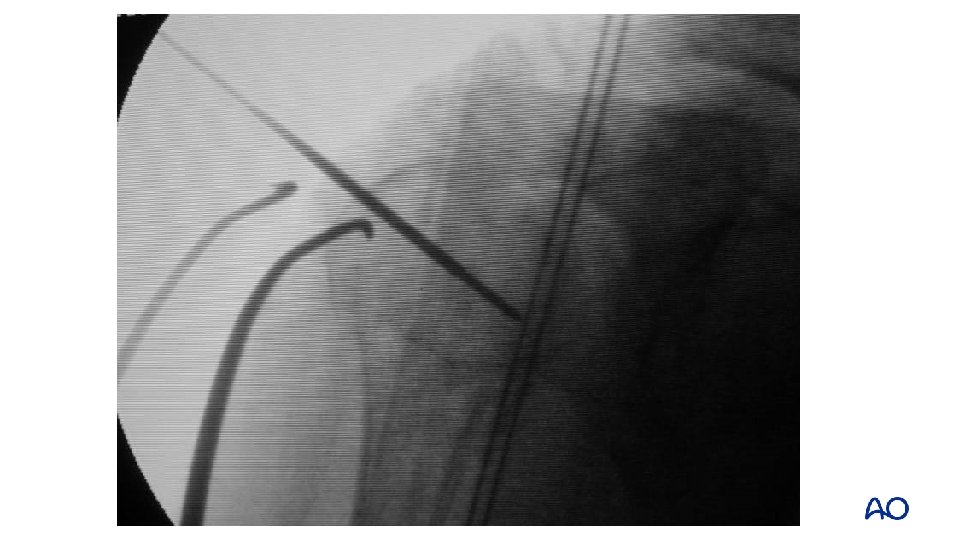
Proximal humerus—intramedullary nailing Correct entry portal is essential for the final reduction result
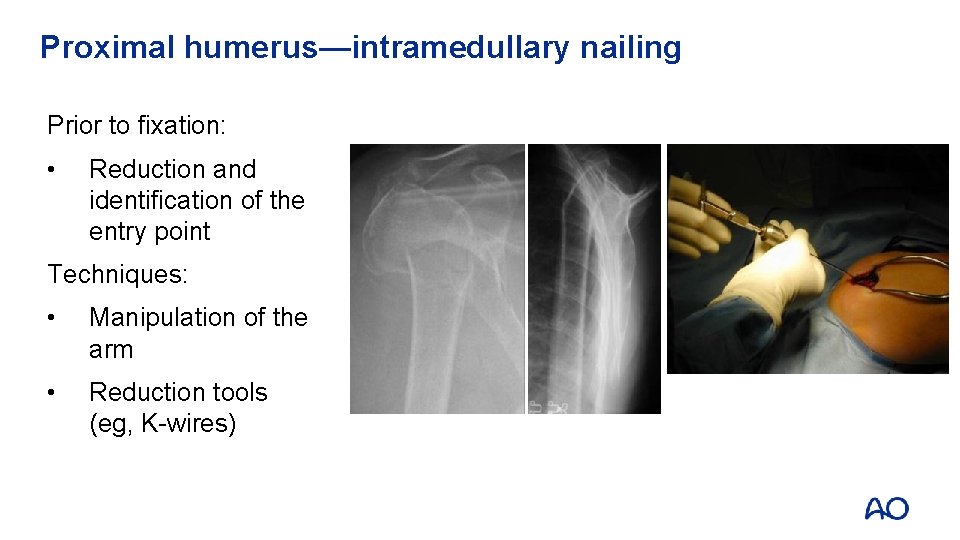
Proximal humerus—intramedullary nailing Prior to fixation: • Reduction and identification of the entry point Techniques: • Manipulation of the arm • Reduction tools (eg, K-wires)
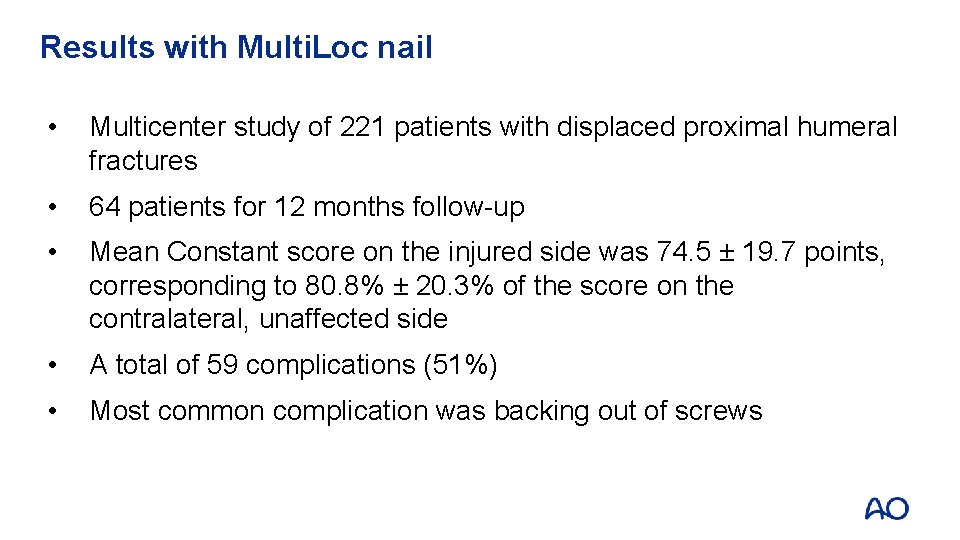
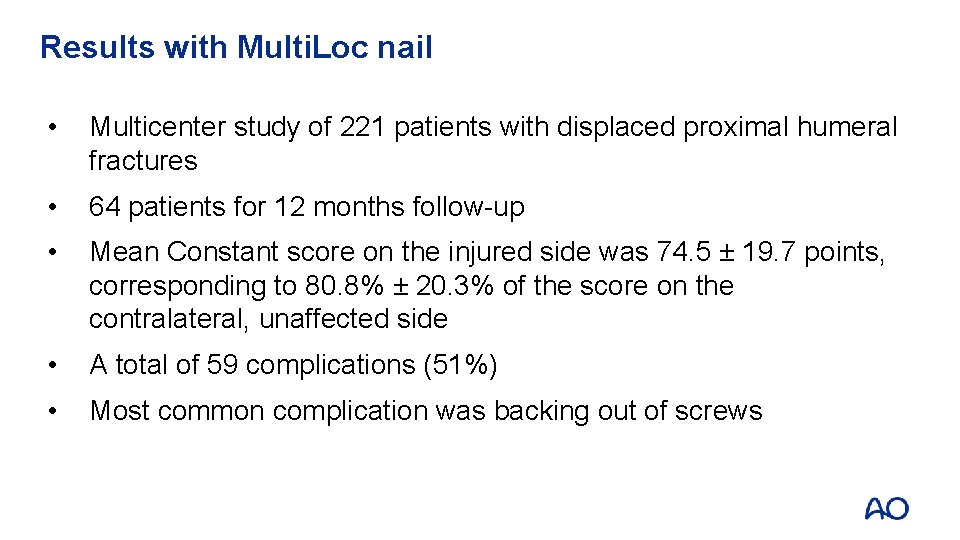
Results with Multi. Loc nail • Multicenter study of 221 patients with displaced proximal humeral fractures • 64 patients for 12 months follow-up • Mean Constant score on the injured side was 74. 5 ± 19. 7 points, corresponding to 80. 8% ± 20. 3% of the score on the contralateral, unaffected side • A total of 59 complications (51%) • Most common complication was backing out of screws back-out: 26 patients (22. 6%)
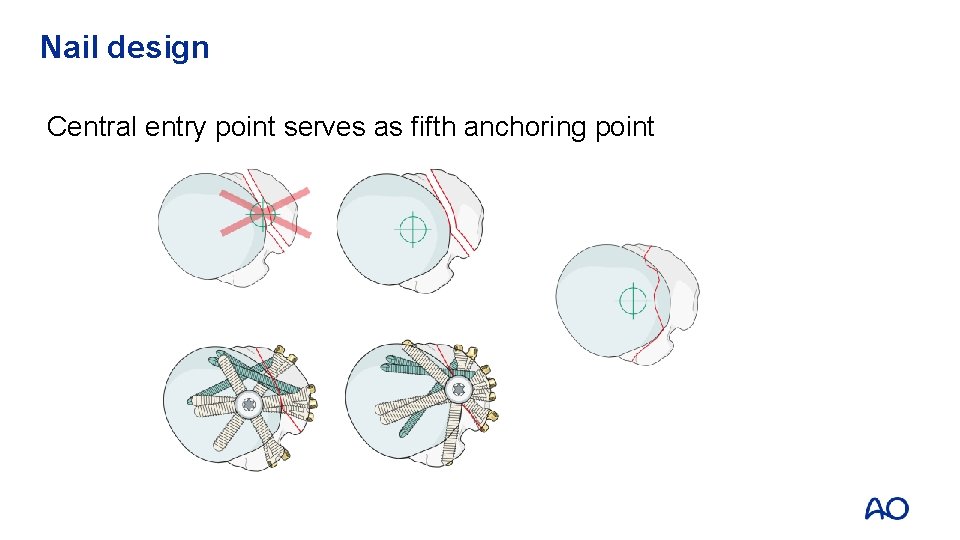
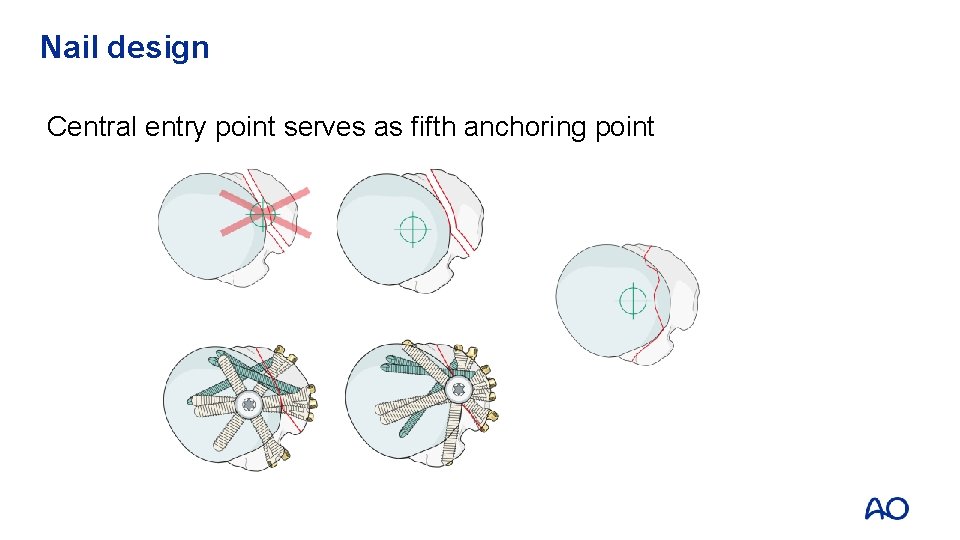
Nail design Central entry point serves as fifth anchoring point
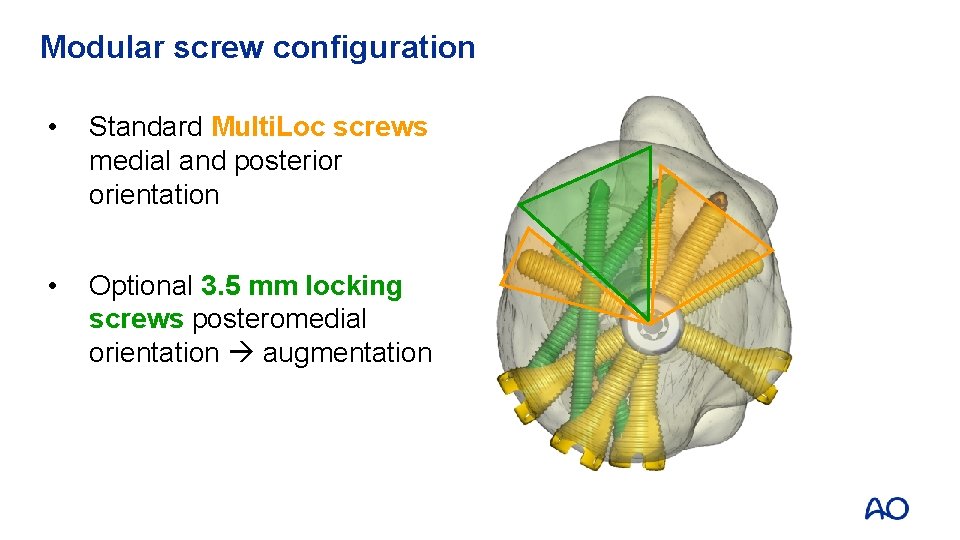
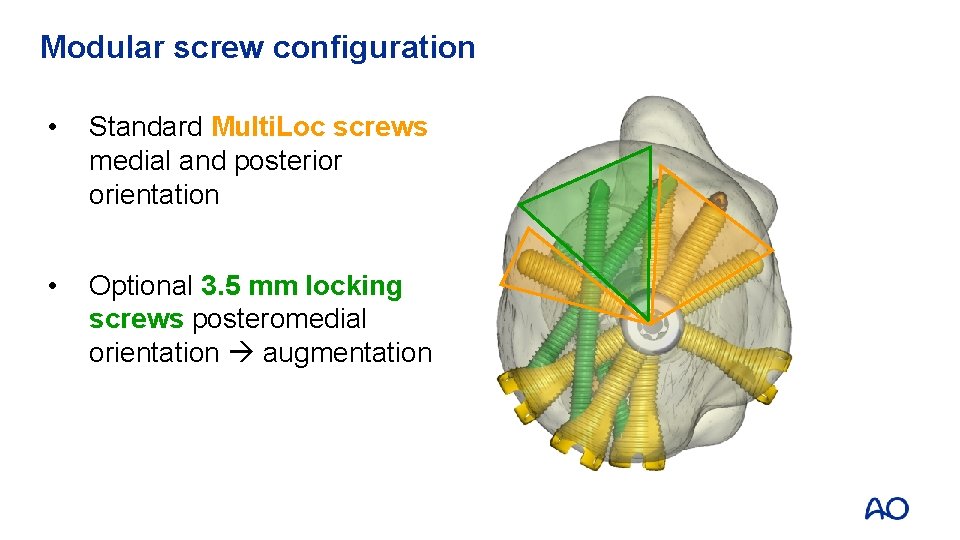
Modular screw configuration • Standard Multi. Loc screws medial and posterior orientation • Optional 3. 5 mm locking screws posteromedial orientation augmentation
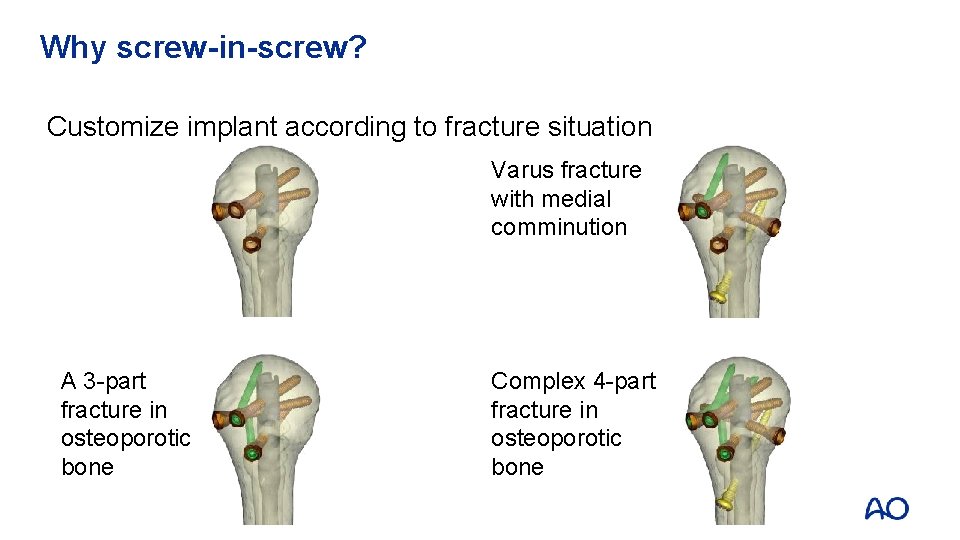
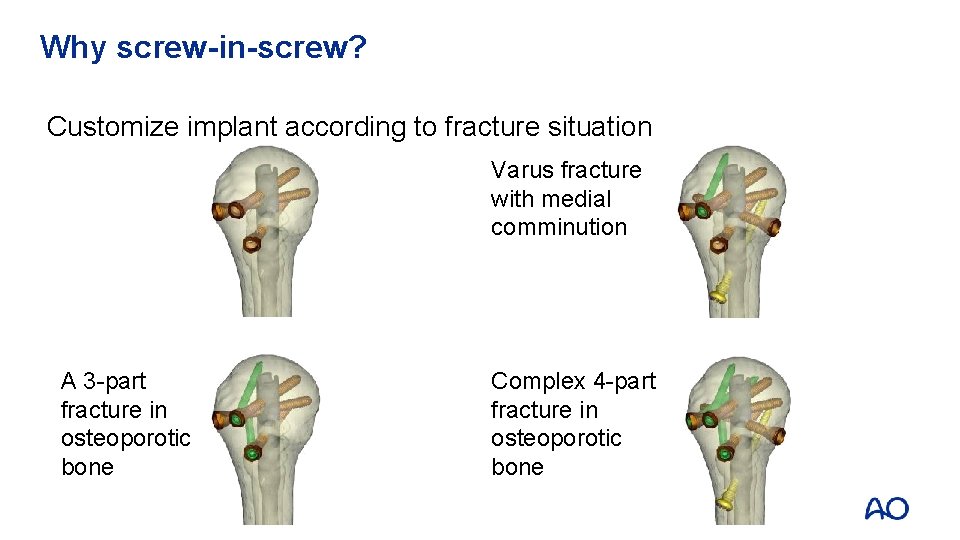
Why screw-in-screw? Customize implant according to fracture situation : 26 patients (22. 6%) A 3 -part fracture in osteoporotic bone Varus fracture with medial comminution Complex 4 -part fracture in osteoporotic bone
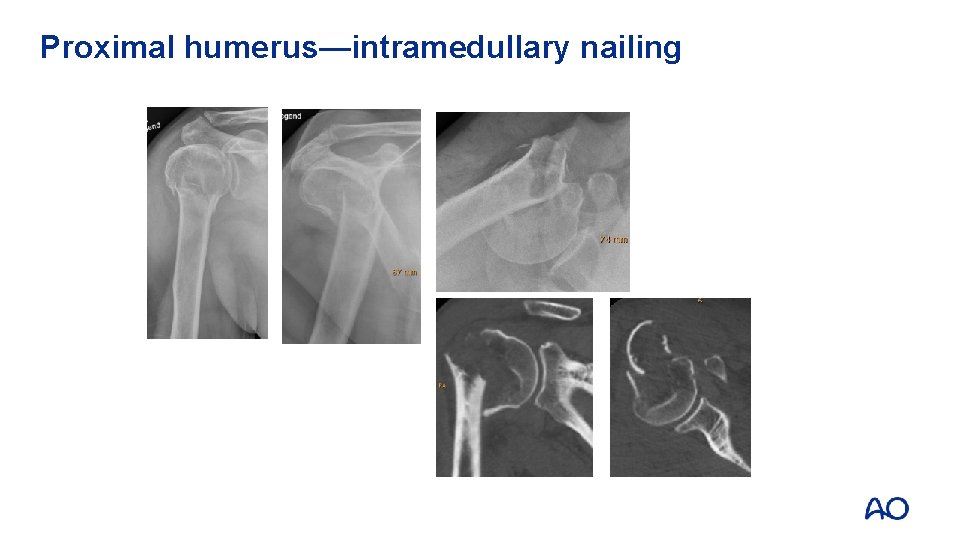
Proximal humerus—intramedullary nailing
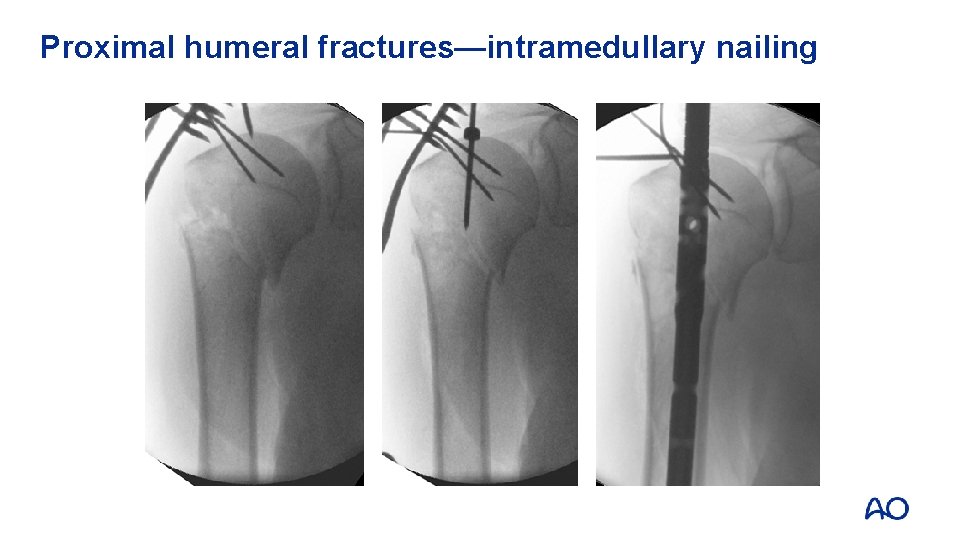
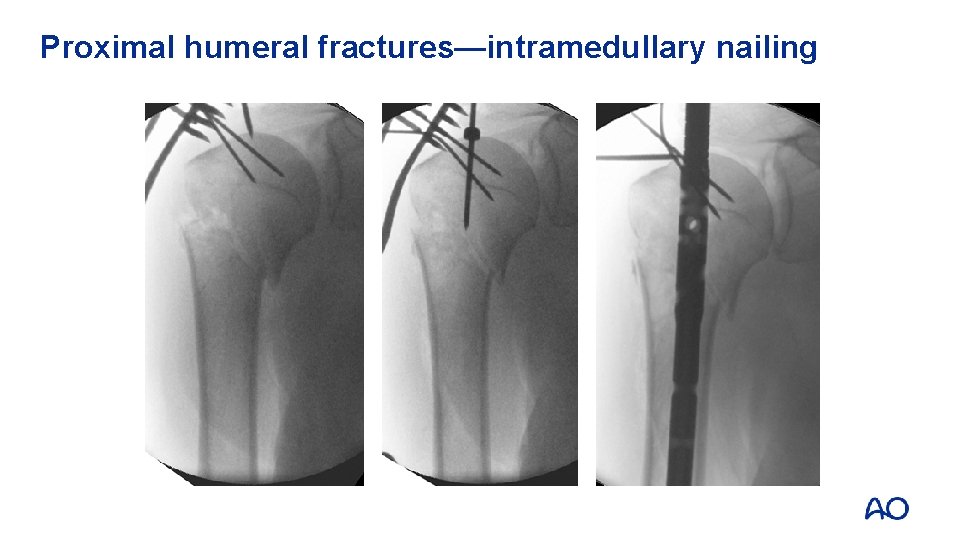
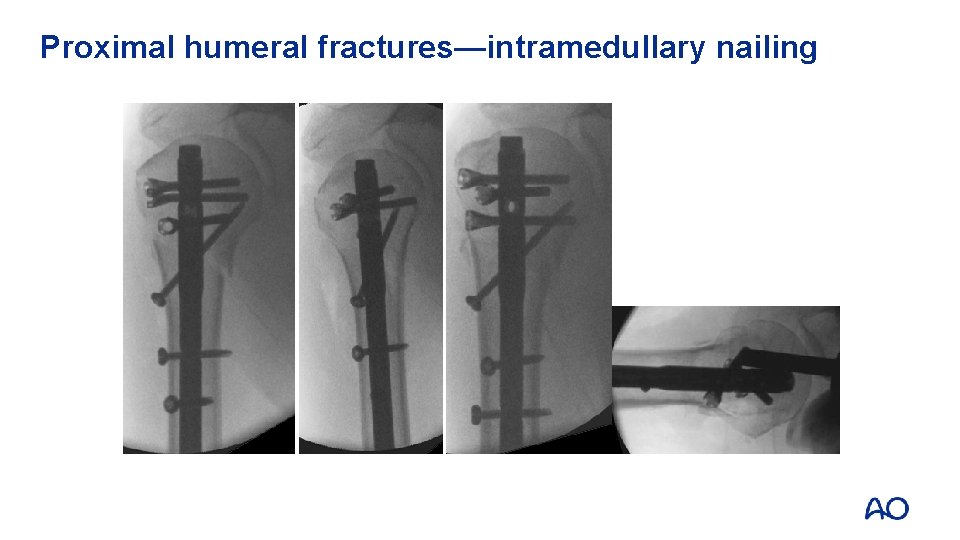
Proximal humeral fractures—intramedullary nailing
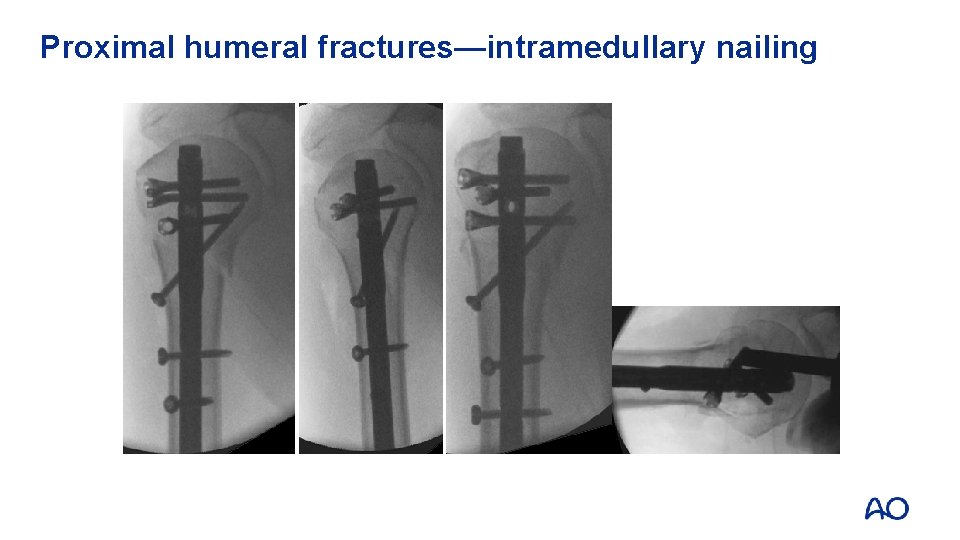
Proximal humeral fractures—intramedullary nailing Synthes Multilock Nail
Proximal humeral fractures—nailing or plating? • Functional results are similar • Number of complications are similar • Trend towards better results with nails in 2 - and 3 -part fractures • Trend towards better shoulder function in 4 -part fractures with plates
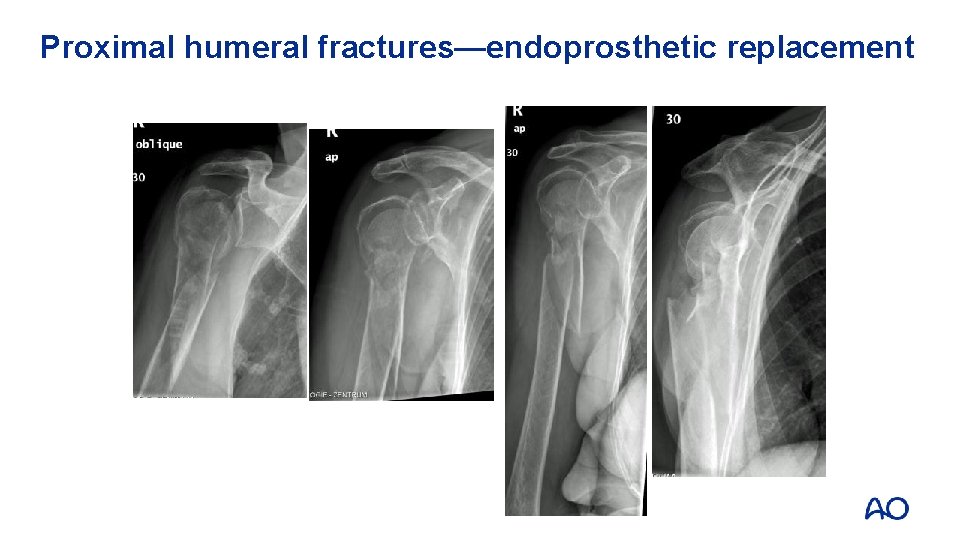
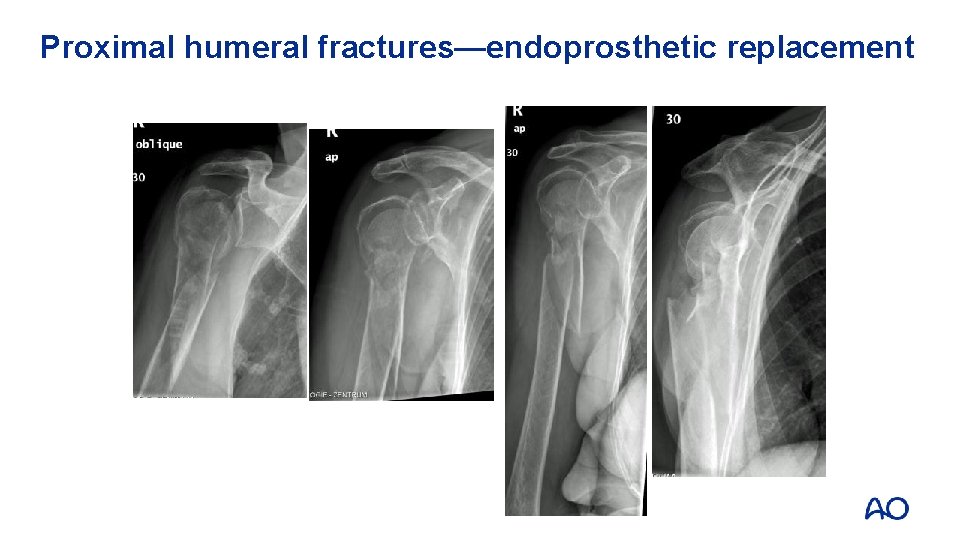
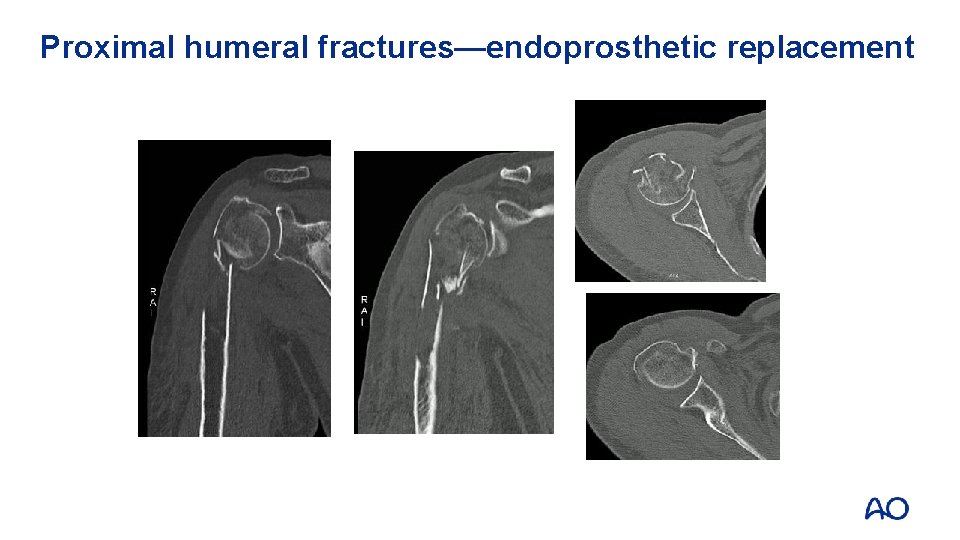
Proximal humeral fractures—endoprosthetic replacement
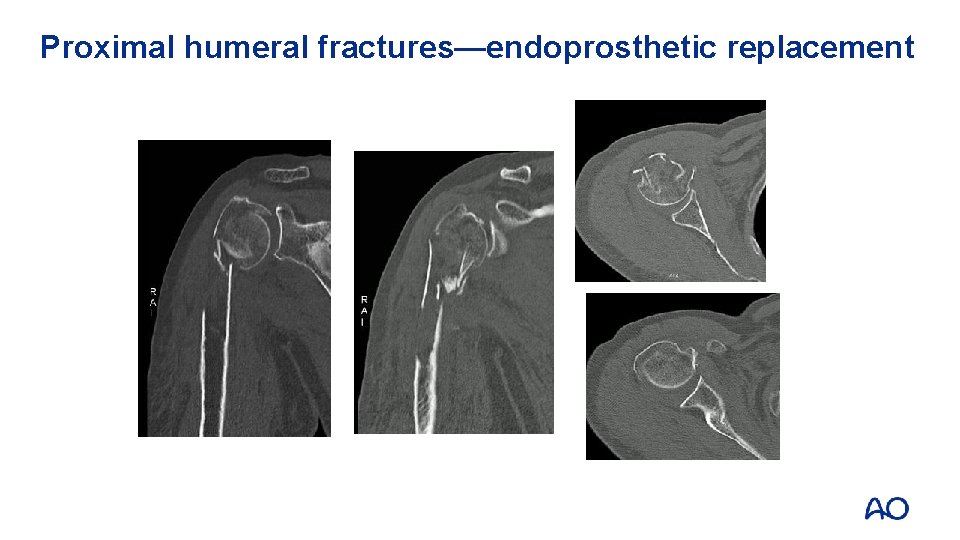
Proximal humeral fractures—endoprosthetic replacement
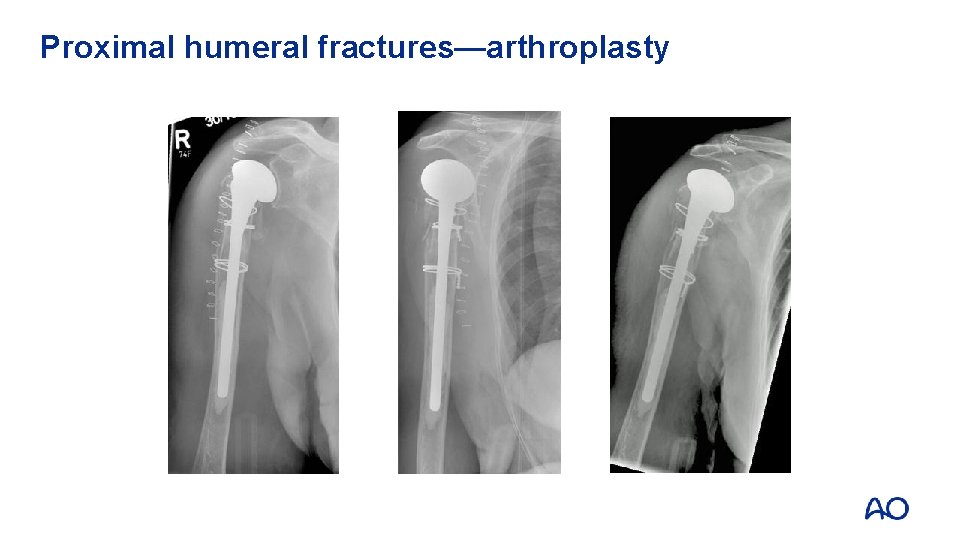
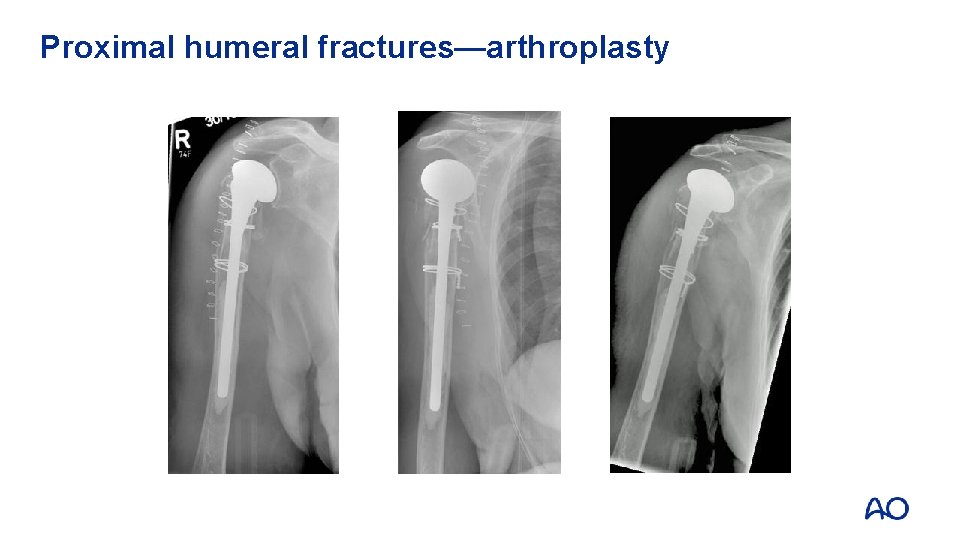
Proximal humeral fractures—arthroplasty
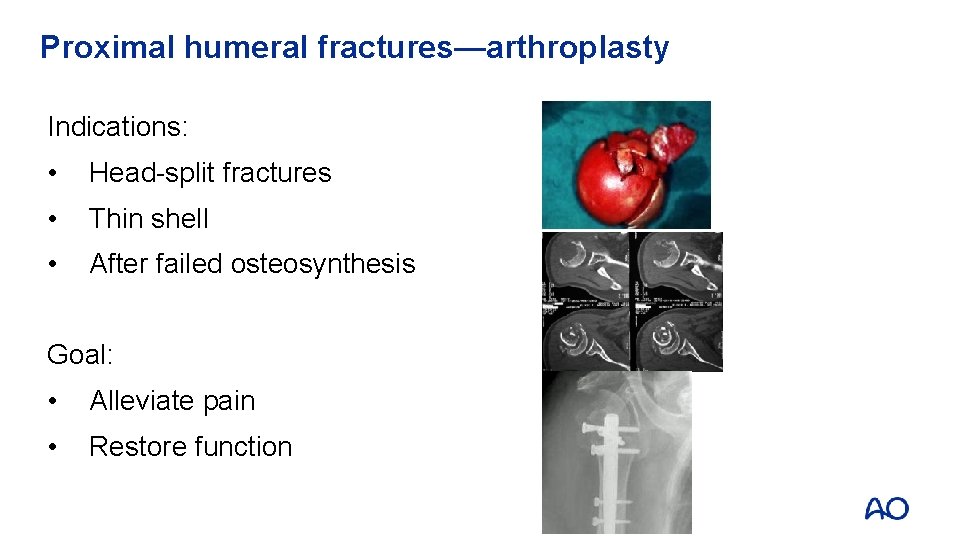
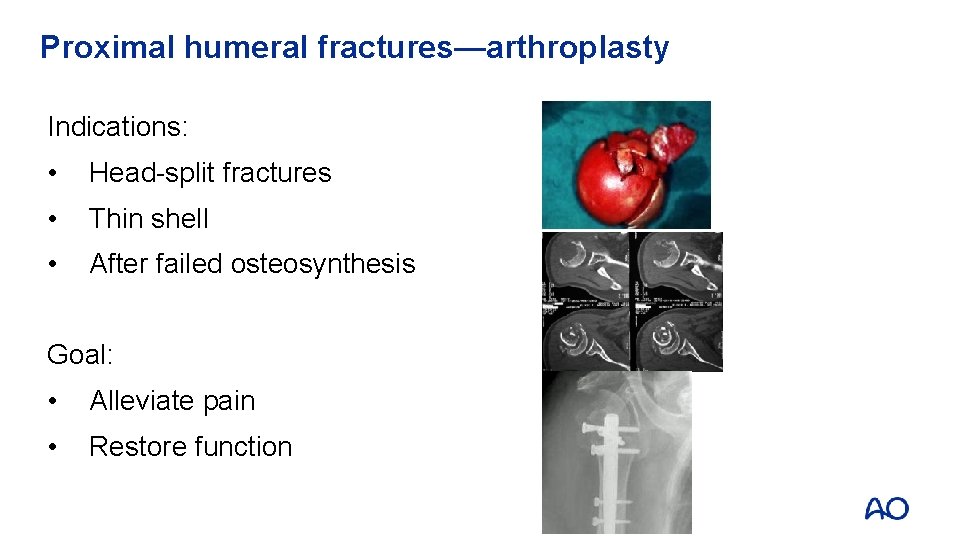
Proximal humeral fractures—arthroplasty Indications: • Head-split fractures • Thin shell • After failed osteosynthesis Goal: • Alleviate pain • Restore function
Arthroplasty versus nonoperative • Study results demonstrated a significant advantage in quality of life in favor of hemiarthroplasty in elderly patients with a displaced 4 -part fracture • Main advantage appeared to be less pain with no difference in range of motion
Take-home messages • Typical fracture in old patients • Decision on treatment depends upon high quality x-rays and careful planning • Plate fixation and IM nailing are treatment alternatives • Quality of the surgery is essential for good outcome and low complication rate