Provider Update HIV Safer Conception Clinical Updates on

- Slides: 39
Provider Update: HIV & Safer Conception: Clinical Updates on Pr. EP, Tas. P & Assisted Reproductive Technologies 4/23/2018 - UCSF Mission Bay Monica Hahn & Guy Vandenberg
Outline • Overview of preconception health for serodifferent couples • Cases: – Pr. EP (Pre-Exposure Prophylaxis) – Tas. P (Treatment as Prevention) – Assisted Reproductive Options • Low Tech • High Tech (AKA Assisted Reproductive Technologies) • Bonus case (extra credit) • Resources • Q&A and Discussion
Poll: True or False? 1. If you ARE living with HIV and are pregnant, your baby will always be born with HIV (unless your viral load is undetectable) 2. If you are NOT living with HIV and you are pregnant, your baby can be born with HIV if your partner or sperm donor is living with HIV
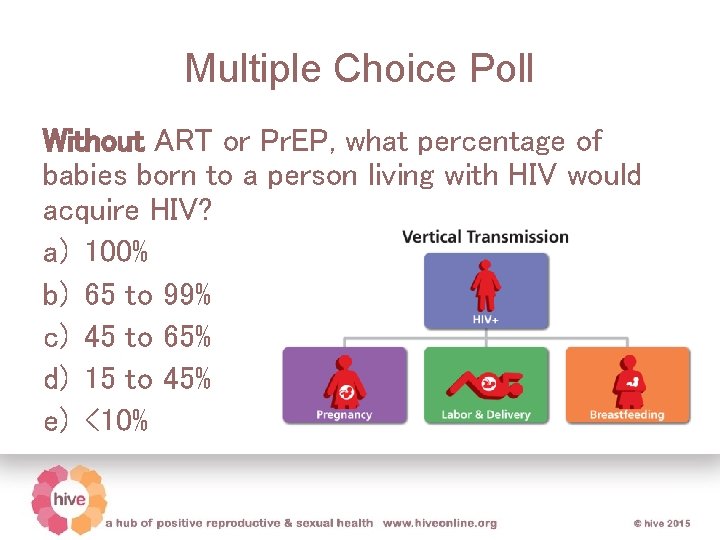
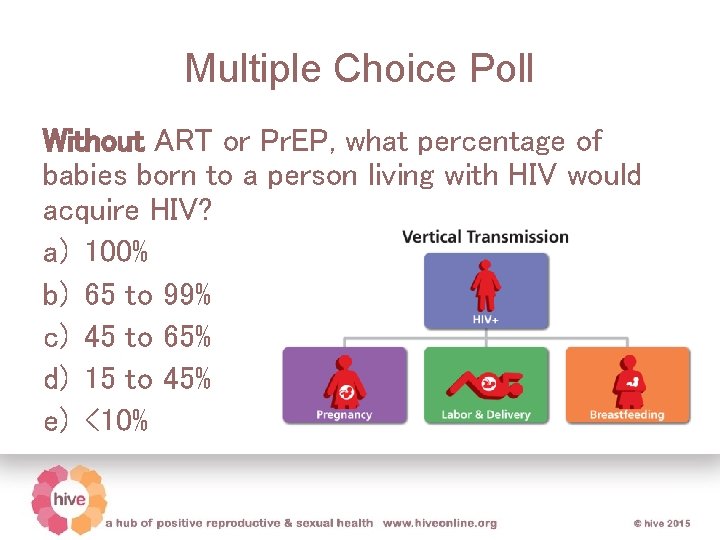
Multiple Choice Poll Without ART or Pr. EP, what percentage of babies born to a person living with HIV would acquire HIV? a) 100% b) 65 to 99% c) 45 to 65% d) 15 to 45% e) <10%
Framing: Reproductive Justice and Sex Positivity • Reproductive Justice: The human right to maintain personal bodily autonomy, have children, not have children, and parent the children we have in safe and sustainable communities. (Sister. Song) • Sex positivity: Simply the idea that all sex, as long as it is healthy and explicitly consensual, is a positive thing. (Women and Gender Advocacy Center)
Goals of HIV-centered preconception health • Optimize overall health for everyone: Healthy diet, exercise, vaccines, avoid tobacco • Screen for, reduce risk for, treat STIs • Reduce exposure to potentially harmful medications and substances – Check on Reprotox, Lactmed • Take prenatal vitamin/folic acid • Prevent HIV transmission to partner and infant ACOG Practice Bulletin No 117; December, 2010
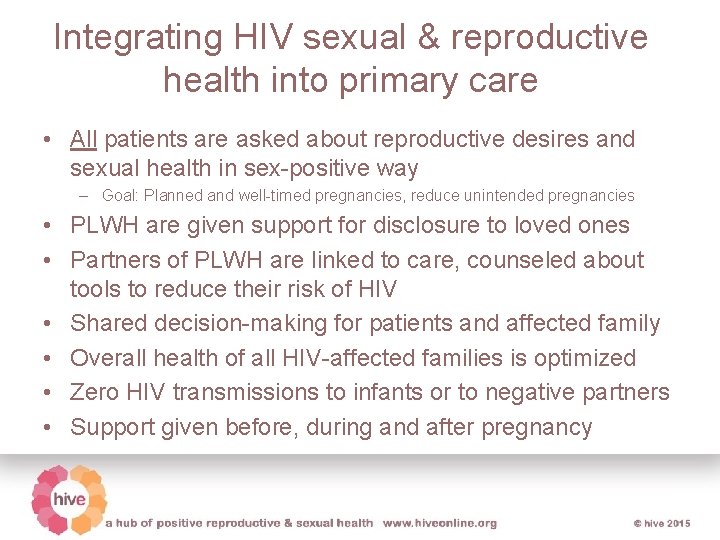
Integrating HIV sexual & reproductive health into primary care • All patients are asked about reproductive desires and sexual health in sex-positive way – Goal: Planned and well-timed pregnancies, reduce unintended pregnancies • PLWH are given support for disclosure to loved ones • Partners of PLWH are linked to care, counseled about tools to reduce their risk of HIV • Shared decision-making for patients and affected family • Overall health of all HIV-affected families is optimized • Zero HIV transmissions to infants or to negative partners • Support given before, during and after pregnancy
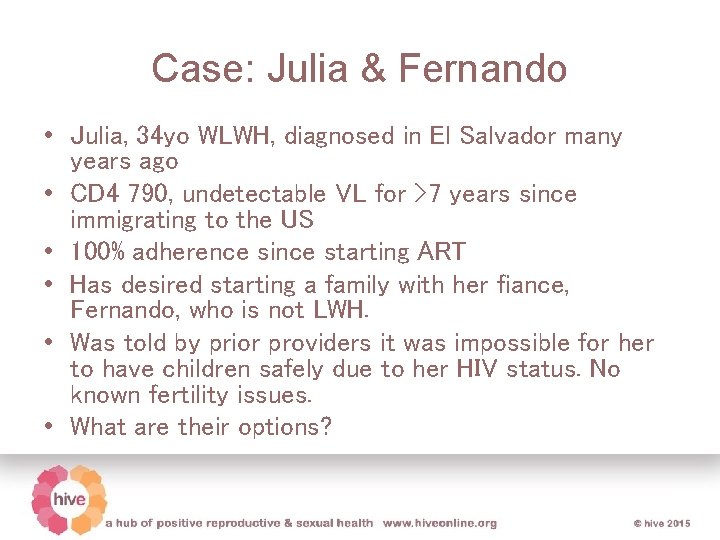
Case: Julia & Fernando • Julia, 34 yo WLWH, diagnosed in El Salvador many years ago • CD 4 790, undetectable VL for >7 years since immigrating to the US • 100% adherence since starting ART • Has desired starting a family with her fiance, Fernando, who is not LWH. • Was told by prior providers it was impossible for her to have children safely due to her HIV status. No known fertility issues. • What are their options?
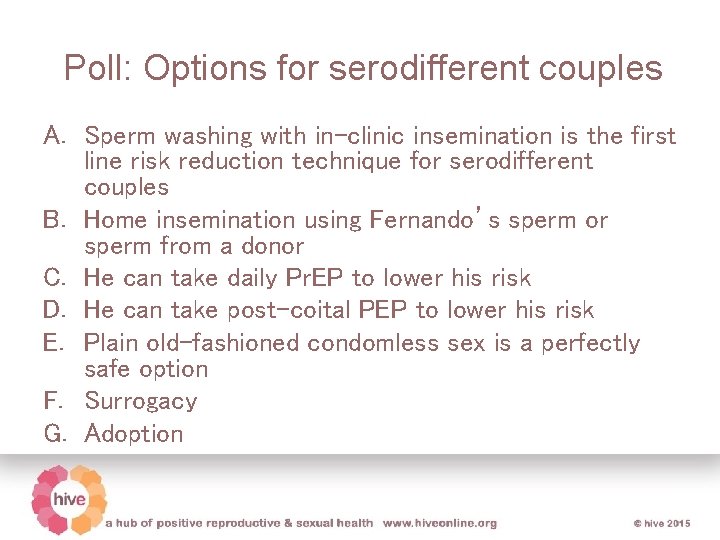
Poll: Options for serodifferent couples A. Sperm washing with in-clinic insemination is the first line risk reduction technique for serodifferent couples B. Home insemination using Fernando’s sperm or sperm from a donor C. He can take daily Pr. EP to lower his risk D. He can take post-coital PEP to lower his risk E. Plain old-fashioned condomless sex is a perfectly safe option F. Surrogacy G. Adoption
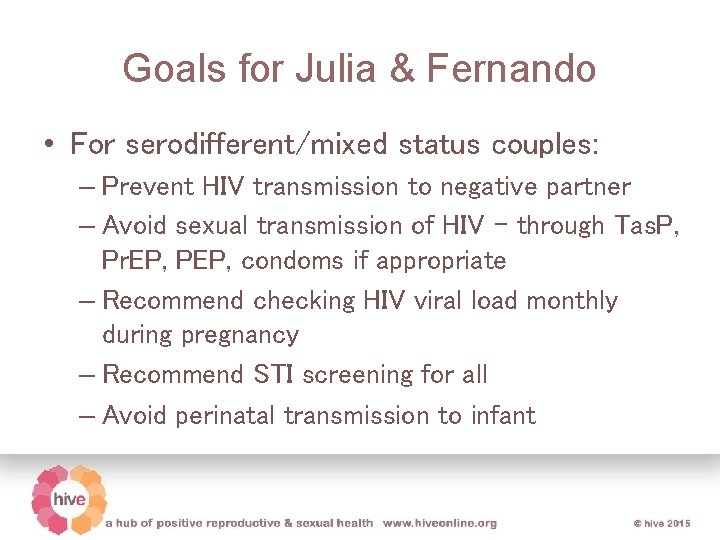
Goals for Julia & Fernando • For serodifferent/mixed status couples: – Prevent HIV transmission to negative partner – Avoid sexual transmission of HIV – through Tas. P, Pr. EP, PEP, condoms if appropriate – Recommend checking HIV viral load monthly during pregnancy – Recommend STI screening for all – Avoid perinatal transmission to infant
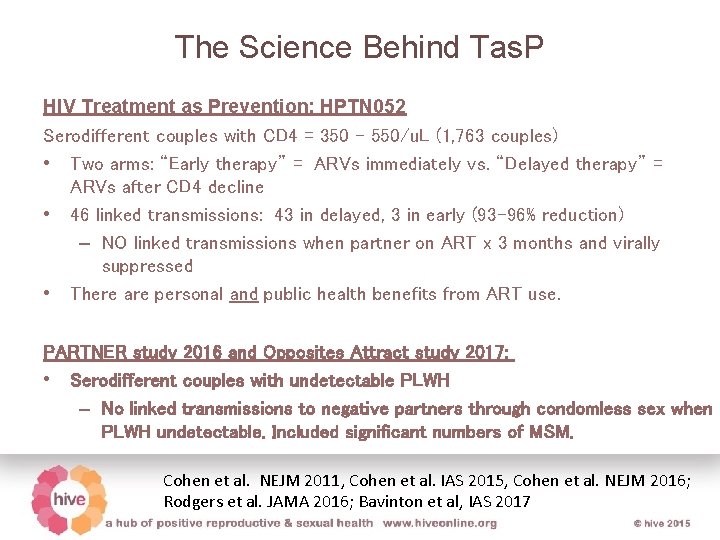
The Science Behind Tas. P HIV Treatment as Prevention: HPTN 052 Serodifferent couples with CD 4 = 350 - 550/u. L (1, 763 couples) • Two arms: “Early therapy” = ARVs immediately vs. “Delayed therapy” = ARVs after CD 4 decline • 46 linked transmissions: 43 in delayed, 3 in early (93 -96% reduction) – NO linked transmissions when partner on ART x 3 months and virally suppressed • There are personal and public health benefits from ART use. PARTNER study 2016 and Opposites Attract study 2017: • Serodifferent couples with undetectable PLWH – No linked transmissions to negative partners through condomless sex when PLWH undetectable. Included significant numbers of MSM. Cohen et al. NEJM 2011, Cohen et al. IAS 2015, Cohen et al. NEJM 2016; Rodgers et al. JAMA 2016; Bavinton et al, IAS 2017
#Uequals. U ”People who take ART daily as prescribed and achieve and maintain an undetectable viral load have effectively no risk of sexually transmitting the virus to an HIV-negative partner. ” CDC (September, 2017) “HIV stigma is a public health crisis, and yet many people in positions of power are still sitting on their hands, overstating risk and not sharing this life changing information! We need people to move away from controlling people with HIV and toward trusting people with HIV. ” (Bruce Richman, Prevention Access Campaign 2017)
HIV & Pregnancy Taking ART, maintaining an undetectable viral load before conception and throughout pregnancy, avoiding breastfeeding, and giving the infant medicine as prescribed, virtually eliminates the risk of HIV transmission. (Mandelbrot 2015)
Case: Janet & James • Janet: 23 yo F with no significant PMHx and no primary care home • Hopes to start a family with James, her male partner LWH, taking ARVs and has undetectable viral load in the past year, with some past difficulty with adherence in setting of alcohol and substance use disorder, now in recovery • She has been told by providers that she would be irresponsible to consider having a child with this partner due to HIV risk to herself and her potential child, and should never have sex without condoms.
Poll: What do you recommend for this couple? A. Sperm washing with in-clinic insemination B. Just have plain old-fashioned condom-less sex – no need for anything else! C. She should always use condoms, and use PEP if the condom breaks D. She can add taking Pr. EP to lower her risk E. I’m not sure. I need more information
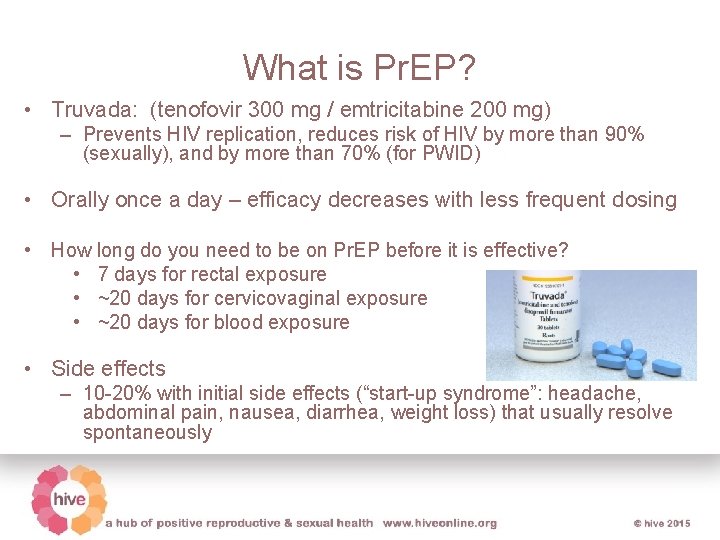
What is Pr. EP? • Truvada: (tenofovir 300 mg / emtricitabine 200 mg) – Prevents HIV replication, reduces risk of HIV by more than 90% (sexually), and by more than 70% (for PWID) • Orally once a day – efficacy decreases with less frequent dosing • How long do you need to be on Pr. EP before it is effective? • 7 days for rectal exposure • ~20 days for cervicovaginal exposure • ~20 days for blood exposure • Side effects – 10 -20% with initial side effects (“start-up syndrome”: headache, abdominal pain, nausea, diarrhea, weight loss) that usually resolve spontaneously
Safety of Pr. EP in preconception/pregnancy • Thought to be safe in preconception, pregnancy and breast/chestfeeding • Antiretroviral Pregnancy Registry: No evidence of adverse effects or birth defects among fetuses exposed to Pr. EP • Studies of women who took Pr. EP around preconception period: No adverse events and no HIV transmissions to negative partners • Possible association with decreased infant head circumference – unlikely to be clinically significant • US Perinatal Guidelines and British HIV Association statements defend safety of tenofovir in pregnancy da. Costa, Machado et al. 2011, Watts, Huang et al. 2011, Knapp, Brogly et al. 2012; Floridia, Mastroiacovo et al. 2013; Siberry, 2012; Mugo, 2012; Vernazza et al, 2011; Seidman et al, 2016; Siberry et al, 2012; Fowler et al 2016.
Patient education materials
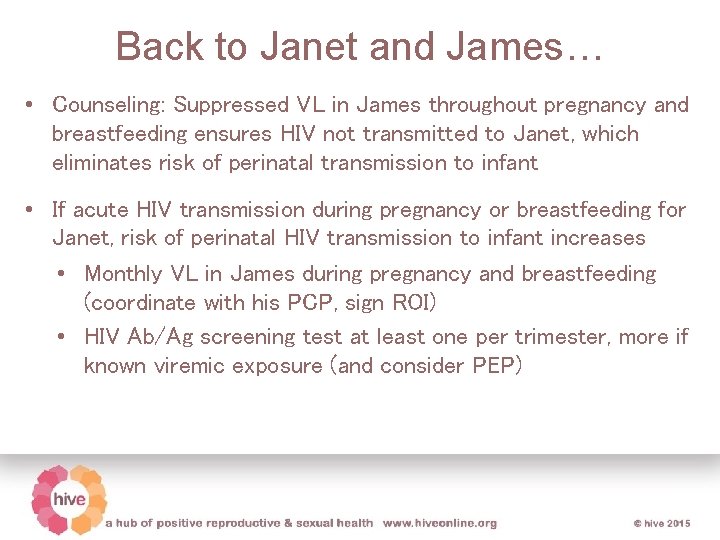
Back to Janet and James… • Counseling: Suppressed VL in James throughout pregnancy and breastfeeding ensures HIV not transmitted to Janet, which eliminates risk of perinatal transmission to infant • If acute HIV transmission during pregnancy or breastfeeding for Janet, risk of perinatal HIV transmission to infant increases • Monthly VL in James during pregnancy and breastfeeding (coordinate with his PCP, sign ROI) • HIV Ab/Ag screening test at least one per trimester, more if known viremic exposure (and consider PEP)
Is there any added benefit to Pr. EP if already using Tas. P? • Pr. EP provides little added benefit when: – The partner living with HIV is on ART and consistently undetectable – There are no other outside partners contributing risk for HIV Heffron 2016
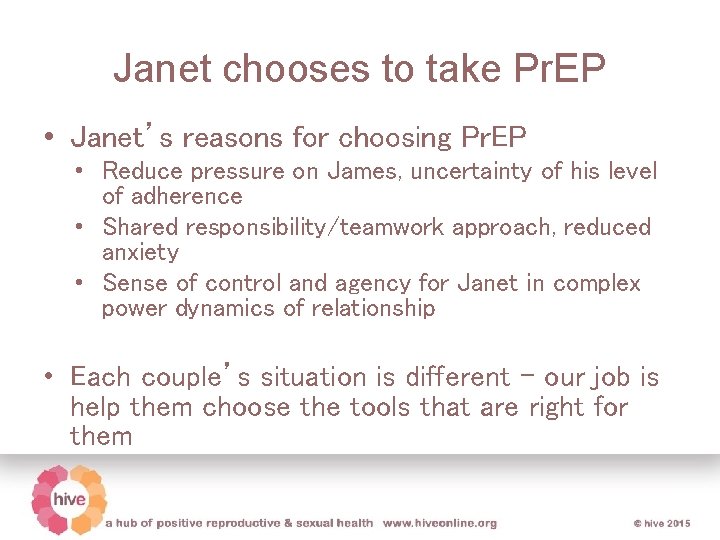
Janet chooses to take Pr. EP • Janet’s reasons for choosing Pr. EP • Reduce pressure on James, uncertainty of his level of adherence • Shared responsibility/teamwork approach, reduced anxiety • Sense of control and agency for Janet in complex power dynamics of relationship • Each couple’s situation is different – our job is help them choose the tools that are right for them
Switching Gears
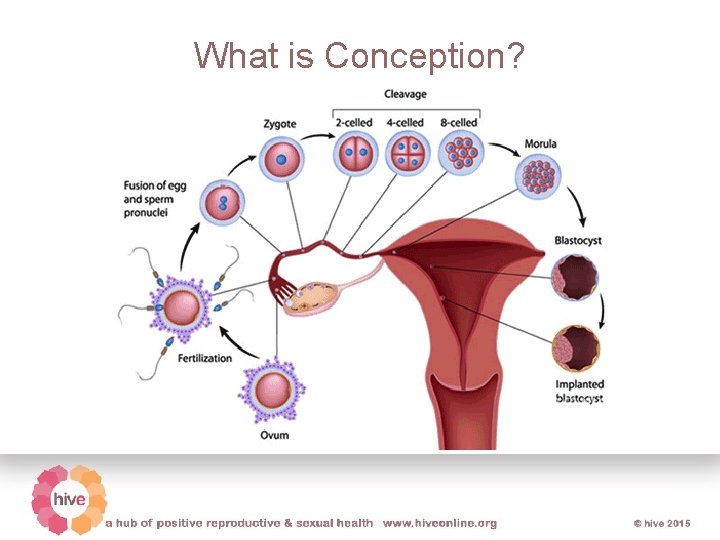
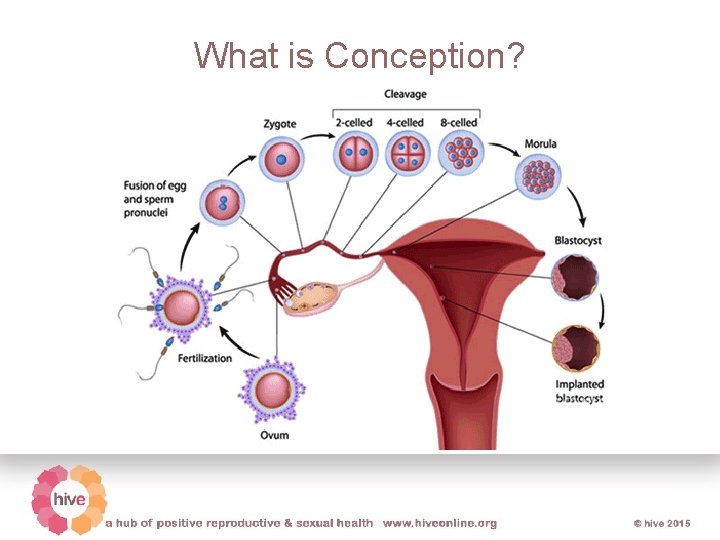
What is Conception?
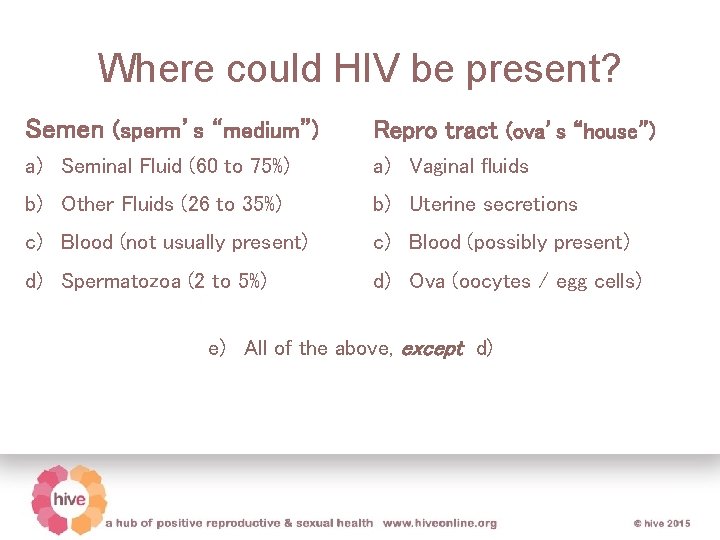
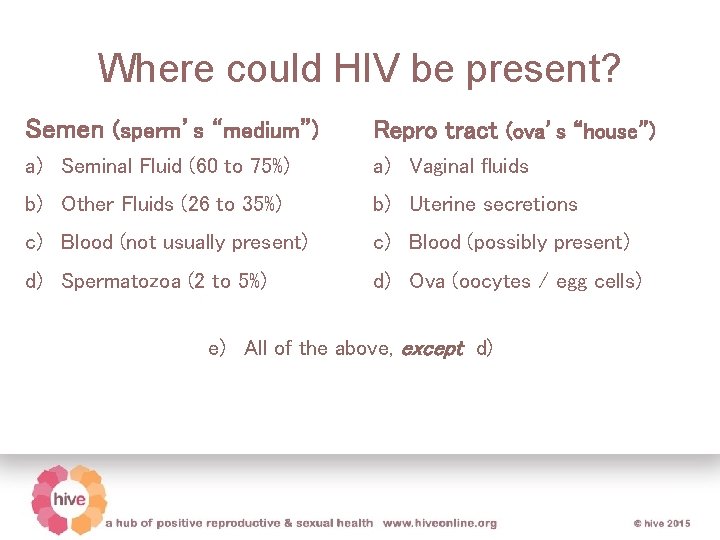
Where could HIV be present? Semen (sperm’s “medium”) Repro tract (ova’s “house”) a) Seminal Fluid (60 to 75%) a) Vaginal fluids b) Other Fluids (26 to 35%) b) Uterine secretions c) Blood (not usually present) c) Blood (possibly present) d) Spermatozoa (2 to 5%) d) Ova (oocytes / egg cells) e) All of the above, except d)
How to Increase Your Chances of Conception • Timed coitus: Coitus during windows of peak fertility (around ovulation) – Ovulation predictor kit – Apps for menses tracking • Definition of infertility: 1 year trying with frequent coitus/timed coitus if under age 35, or 6 months trying if over age 35.
Preparing for Conception Women: • Hormone level tests (3 rd day of cycle) • And/or hysterosalpingogram Men: • Semen analysis
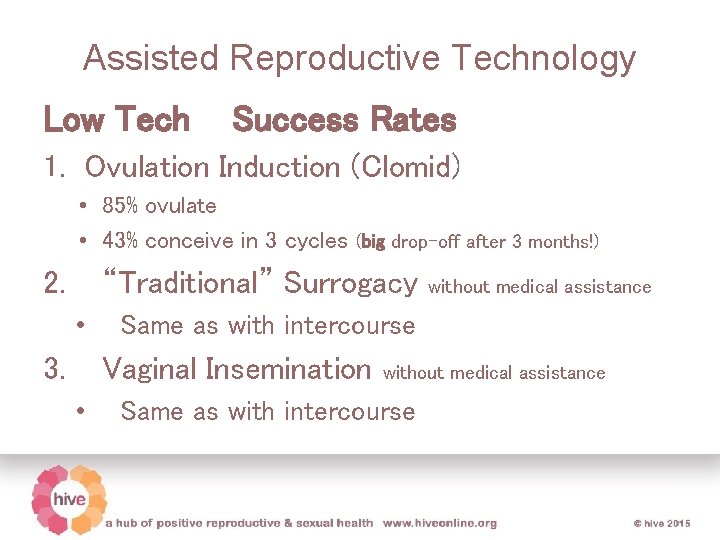
Assisted Reproductive Technology Low Tech Success Rates 1. Ovulation Induction (Clomid) • 85% ovulate • 43% conceive in 3 cycles (big drop-off after 3 months!) 2. “Traditional” Surrogacy • 3. Same as with intercourse Vaginal Insemination • without medical assistance Same as with intercourse
Low Tech Case: Miriam & Rashid • • • F & M couple, trying to conceive x 3 years Miriam is on ART, undetectable VL Tried herbals and Clomid w/o success (Sub-standard) semen analysis is unhelpful After considering other options, Miriam and Rashid decide to ask Rashid’s (twin-) brother Musa to donate sperm. He agrees • One year later: Miriam gives birth - to twins!
Note: The people in this picture are not Miriam & Rashid
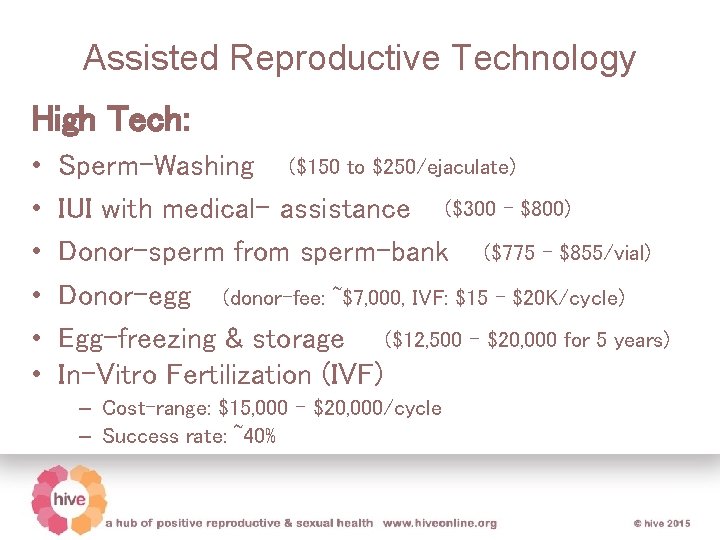
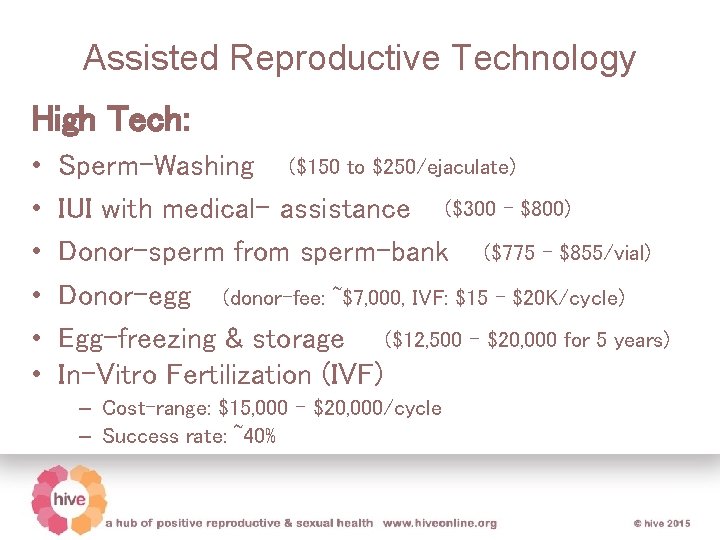
Assisted Reproductive Technology High Tech: • • • Sperm-Washing ($150 to $250/ejaculate) IUI with medical- assistance ($300 - $800) Donor-sperm from sperm-bank ($775 - $855/vial) Donor-egg (donor-fee: ~$7, 000, IVF: $15 – $20 K/cycle) Egg-freezing & storage ($12, 500 - $20, 000 for 5 years) In-Vitro Fertilization (IVF) – Cost-range: $15, 000 - $20, 000/cycle – Success rate: ~40%
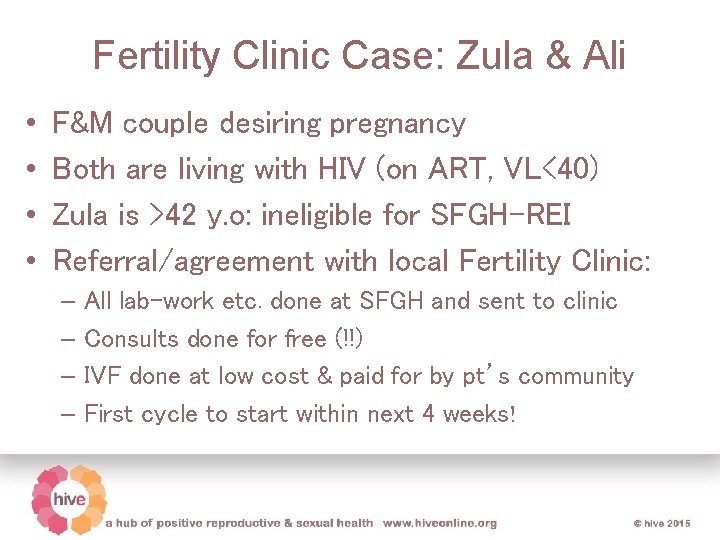
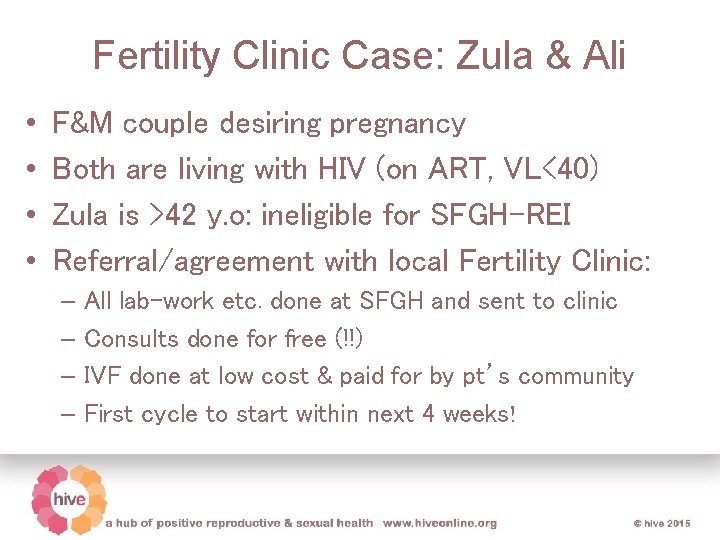
Fertility Clinic Case: Zula & Ali • • F&M couple desiring pregnancy Both are living with HIV (on ART, VL<40) Zula is >42 y. o: ineligible for SFGH-REI Referral/agreement with local Fertility Clinic: – All lab-work etc. done at SFGH and sent to clinic – Consults done for free (!!) – IVF done at low cost & paid for by pt’s community – First cycle to start within next 4 weeks!
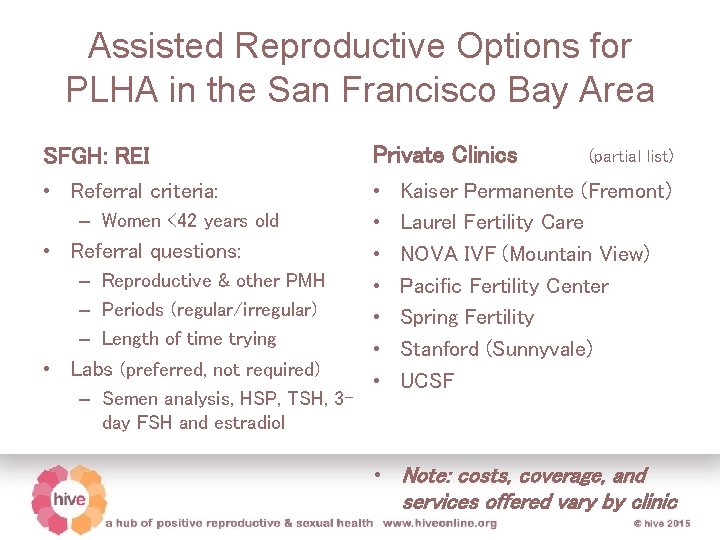
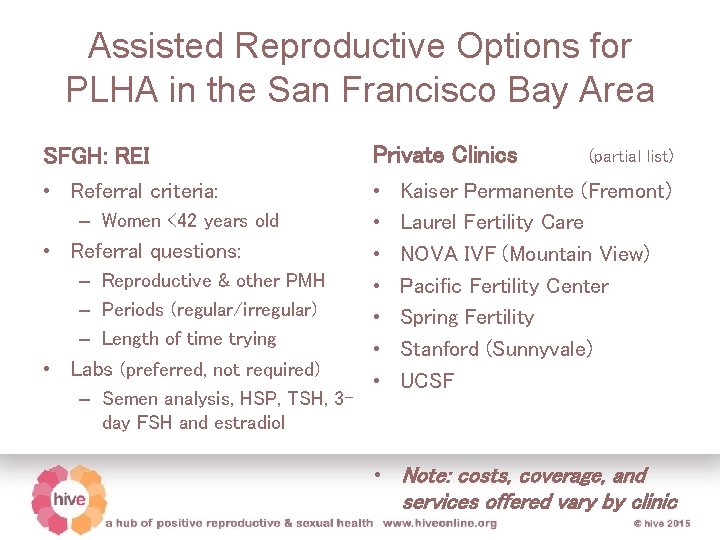
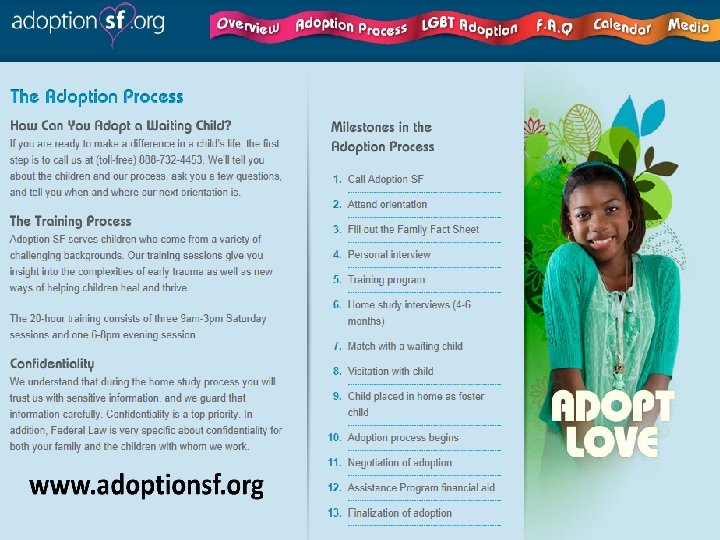
Assisted Reproductive Options for PLHA in the San Francisco Bay Area SFGH: REI Private Clinics • Referral criteria: • • – Women <42 years old • Referral questions: – Reproductive & other PMH – Periods (regular/irregular) – Length of time trying • Labs (preferred, not required) – Semen analysis, HSP, TSH, 3 day FSH and estradiol (partial list) Kaiser Permanente (Fremont) Laurel Fertility Care NOVA IVF (Mountain View) Pacific Fertility Center Spring Fertility Stanford (Sunnyvale) UCSF • Note: costs, coverage, and services offered vary by clinic
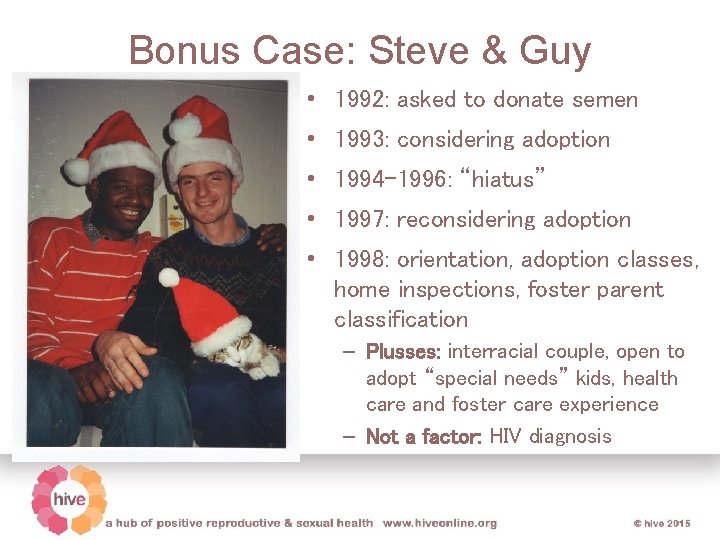
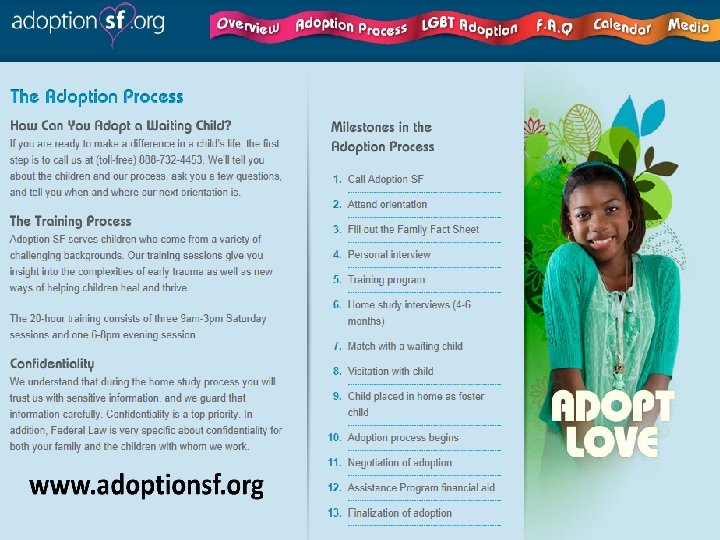
Bonus Case: Steve & Guy • 1992: asked to donate semen • 1993: considering adoption • 1994 -1996: “hiatus” • 1997: reconsidering adoption • 1998: orientation, adoption classes, home inspections, foster parent classification – Plusses: interracial couple, open to adopt “special needs” kids, health care and foster care experience – Not a factor: HIV diagnosis
• 2016: settled into “unclehood”
Thank you! • Please contact us with any questions! • Monica Hahn: • monica. hahn@ucsf. edu • Guy Vandenberg: guy. vandenberg@ucsf. edu
HIVEonline. org Resources for providers v Integrated resources on sexual & reproductive health v Videos of how to counsel patients v Sample order sheets Resources for patients v Information sheets on prevention options in and around pregnancy (Spanish & English) v Videos of patient experiences

Reproductive Health Clinic at SFGH Ward 86. Call: 415 -206 -2482 or email: guy. vandenberg@ucsf. edu