Provider Revalidation Instructions Bulk Enrollment Tools 1 Agenda
Provider Revalidation Instructions – Bulk Enrollment Tools 1
Agenda • • • 2 Overview of Affordable Care Act (ACA) Provider Revalidation Cycle Assignments Revalidation Application Requirements Risk Category Assignments Provider Screening Requirements Surety Bond Requirements Application Fees Site Visits Non-billing, Ordering, Prescribing, or Referring (NOPR) Providers Health PAS Online Portal Changes Next Steps Stay Informed
Overview: ACA Provider Revalidation Section 6401 of the ACA establishes a requirement for Medicare and Medicaid to revalidate enrollment information under new screening criteria for all enrolled providers, regardless of provider type. All providers are required to revalidate with Maine. Care at least every five years - three years for Durable Medical Equipment (DME) providers - or upon the request of Maine. Care Services. In compliance with the ACA, Maine. Care Services began the revalidation process in the spring of 2017. Failure to revalidate will result in the termination of your enrollment with the Maine. Care program and denial of claims. 3
Overview: ACA Provider Revalidation • • • 4 Providers enrolled after January 17, 2017 are screened using the new requirements. Revalidation for providers enrolled after January 17, 2017 will be scheduled for every five years - three years for Durable Medical Equipment (DME) providers - or upon the request of Maine. Care Services. Providers enrolled prior to January 17, 2017 are required to submit a Maine. Care enrollment revalidation application using the online portal during one of thirteen, sixty-day cycles. The revalidation application will be available during your assigned sixty-day cycle. All Maine. Care providers must revalidate during their assigned cycle.
Revalidation Cycle Assignments The revalidation cycles will be implemented in the following manner: 5 • Cycle 1 was successfully completed with a small number of providers. • Providers will be distributed evenly across cycles 2 – 13, based on their current enrollment size. This is based on the number of rendering providers, service locations, and site visits affiliated to each Pay-To NPI. • All NPI’s associated to one federal ID number will be assigned within the same cycle.
Revalidation Cycle Assignments 6 • A letter will be sent to the Pay-To address 60 days, and again at 30 days prior to your revalidation start date. • A reminder email will be sent to the contact person identified on your current Provider Enrollment Application (PEA) 30 days after the start of your revalidation. • If you do not revalidate within the 60 day period, your claims will pend on day 61. • If you do not revalidate by day 90, your Maine. Care pended claims will be denied on day 91, and your enrollment terminated. • If you are assigned to the upcoming revalidation cycle, you should already have received your 60 day letter. • If you do not plan to revalidate, please submit a Disenrollment case using the online portal.
Revalidation Application Requirements 7 • Providers are required to supply the Social Security Number (SSN) and the date of birth (DOB) for board members, managing employees, rendering providers, and any person with ownership or controlling interest of 5% or more in the disclosing entity. • Providers also have to ensure that their National Provider Identifier (NPI), Internal Revenue Service (IRS), and Maine. Care information matches. • Some service locations are now subject to site visits. • Providers must continue to meet all licensure requirements for their provider type and specialty, as well as more stringent screening requirements that may result in some providers being terminated. • Background checks are required for providers, owners with 5% or greater direct or indirect ownership, managing employees, and board members.
Revalidation Application Requirements 8 • An application fee is required for certain providers types. • Organizations may enroll Non-billing, Ordering, Prescribing, or Rendering (NOPR) providers with their revalidation applications. • Surety bonds are required for DME providers and Home Health Agencies (HHA). • Any maintenance updates that need to be made to your enrollment may be made as part of the revalidation application. • Electronic Fund Transfer (EFT) will be required. • Each provider will be required to sign and submit a new provider agreement. A signed vendor form is required if changes are made to the Pay-To information. • Each provider will be required to have a trading partner account prior to submitting the revalidation application.
Risk Category Assignments 9 • Maine. Care providers have been assigned to risk categories of limited, moderate, or high. • The Centers for Medicare & Medicaid Services (CMS) assigned specific provider types to a risk level depending on how much of a risk these provider types pose to the medical billing practice. • Maine. Care assigned providers to a risk level based on CMS requirements and guidance. • Risk levels are assigned depending on the provider type and specialty of the service location.
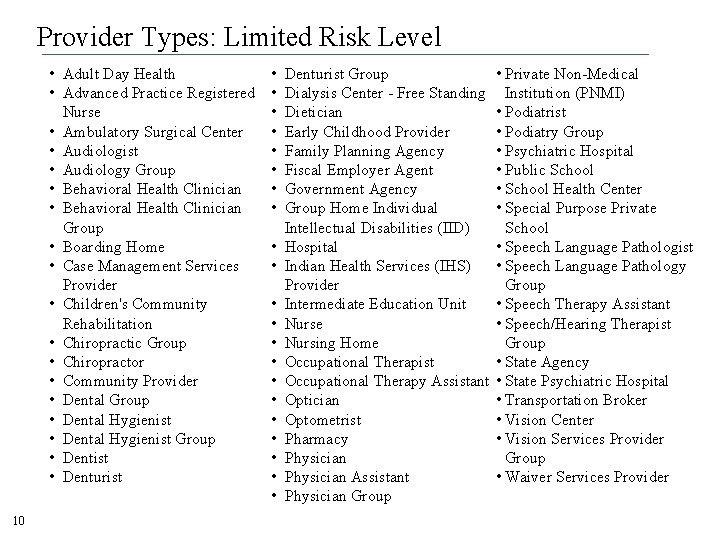
Provider Types: Limited Risk Level • Adult Day Health • Advanced Practice Registered Nurse • Ambulatory Surgical Center • Audiologist • Audiology Group • Behavioral Health Clinician Group • Boarding Home • Case Management Services Provider • Children's Community Rehabilitation • Chiropractic Group • Chiropractor • Community Provider • Dental Group • Dental Hygienist Group • Dentist • Denturist 10 • • • • • • Denturist Group Dialysis Center - Free Standing Dietician Early Childhood Provider Family Planning Agency Fiscal Employer Agent Government Agency Group Home Individual Intellectual Disabilities (IID) Hospital Indian Health Services (IHS) Provider Intermediate Education Unit Nurse Nursing Home Occupational Therapist Occupational Therapy Assistant Optician Optometrist Pharmacy Physician Assistant Physician Group • Private Non-Medical Institution (PNMI) • Podiatrist • Podiatry Group • Psychiatric Hospital • Public School • School Health Center • Special Purpose Private School • Speech Language Pathologist • Speech Language Pathology Group • Speech Therapy Assistant • Speech/Hearing Therapist Group • State Agency • State Psychiatric Hospital • Transportation Broker • Vision Center • Vision Services Provider Group • Waiver Services Provider
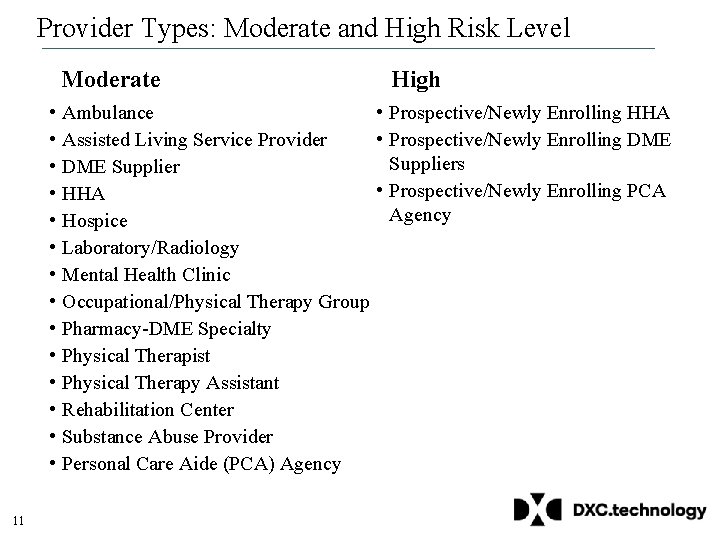
Provider Types: Moderate and High Risk Level Moderate • Ambulance • Assisted Living Service Provider • DME Supplier • HHA • Hospice • Laboratory/Radiology • Mental Health Clinic • Occupational/Physical Therapy Group • Pharmacy-DME Specialty • Physical Therapist • Physical Therapy Assistant • Rehabilitation Center • Substance Abuse Provider • Personal Care Aide (PCA) Agency 11 High • Prospective/Newly Enrolling HHA • Prospective/Newly Enrolling DME Suppliers • Prospective/Newly Enrolling PCA Agency
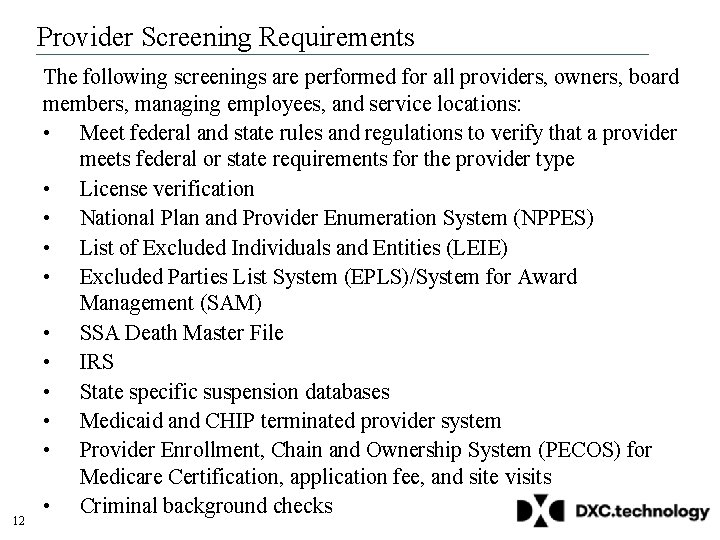
Provider Screening Requirements 12 The following screenings are performed for all providers, owners, board members, managing employees, and service locations: • Meet federal and state rules and regulations to verify that a provider meets federal or state requirements for the provider type • License verification • National Plan and Provider Enumeration System (NPPES) • List of Excluded Individuals and Entities (LEIE) • Excluded Parties List System (EPLS)/System for Award Management (SAM) • SSA Death Master File • IRS • State specific suspension databases • Medicaid and CHIP terminated provider system • Provider Enrollment, Chain and Ownership System (PECOS) for Medicare Certification, application fee, and site visits • Criminal background checks
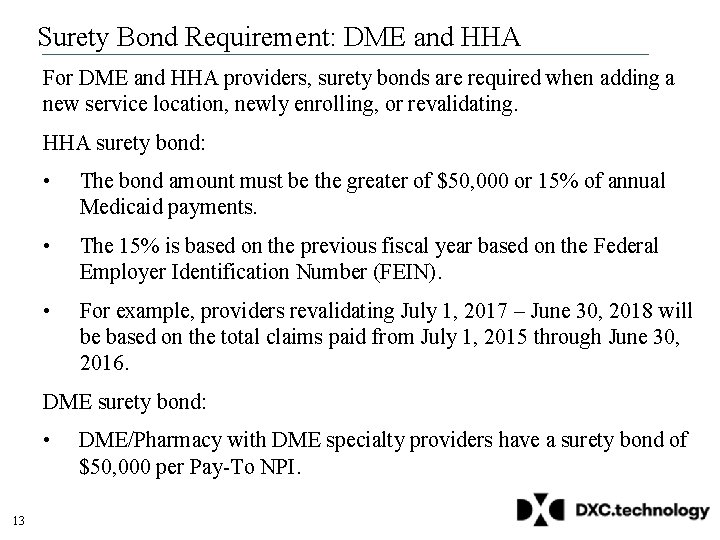
Surety Bond Requirement: DME and HHA For DME and HHA providers, surety bonds are required when adding a new service location, newly enrolling, or revalidating. HHA surety bond: • The bond amount must be the greater of $50, 000 or 15% of annual Medicaid payments. • The 15% is based on the previous fiscal year based on the Federal Employer Identification Number (FEIN). • For example, providers revalidating July 1, 2017 – June 30, 2018 will be based on the total claims paid from July 1, 2015 through June 30, 2016. DME surety bond: • 13 DME/Pharmacy with DME specialty providers have a surety bond of $50, 000 per Pay-To NPI.
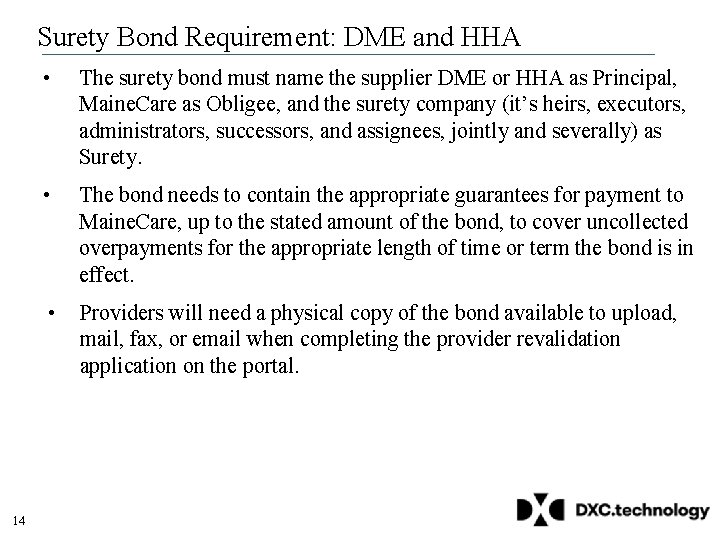
Surety Bond Requirement: DME and HHA 14 • The surety bond must name the supplier DME or HHA as Principal, Maine. Care as Obligee, and the surety company (it’s heirs, executors, administrators, successors, and assignees, jointly and severally) as Surety. • The bond needs to contain the appropriate guarantees for payment to Maine. Care, up to the stated amount of the bond, to cover uncollected overpayments for the appropriate length of time or term the bond is in effect. • Providers will need a physical copy of the bond available to upload, mail, fax, or email when completing the provider revalidation application on the portal.
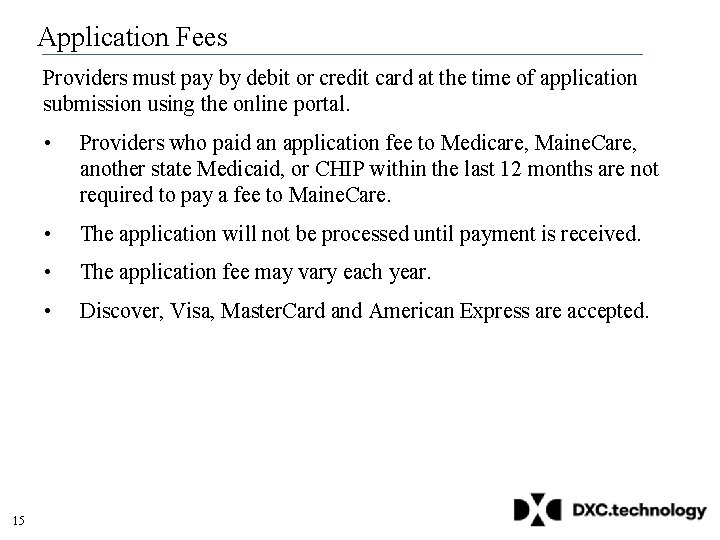
Application Fees Providers must pay by debit or credit card at the time of application submission using the online portal. 15 • Providers who paid an application fee to Medicare, Maine. Care, another state Medicaid, or CHIP within the last 12 months are not required to pay a fee to Maine. Care. • The application will not be processed until payment is received. • The application fee may vary each year. • Discover, Visa, Master. Card and American Express are accepted.
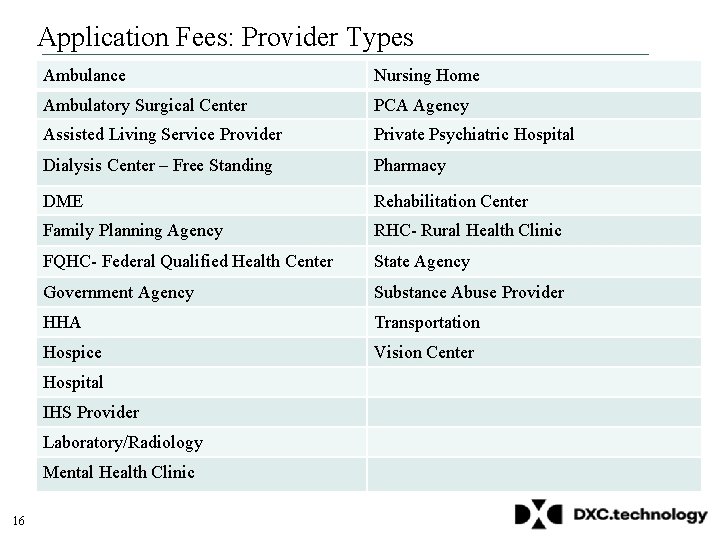
Application Fees: Provider Types Ambulance Nursing Home Ambulatory Surgical Center PCA Agency Assisted Living Service Provider Private Psychiatric Hospital Dialysis Center – Free Standing Pharmacy DME Rehabilitation Center Family Planning Agency RHC- Rural Health Clinic FQHC- Federal Qualified Health Center State Agency Government Agency Substance Abuse Provider HHA Transportation Hospice Vision Center Hospital IHS Provider Laboratory/Radiology Mental Health Clinic 16
Site Visits 17 • A site visit is conducted for any provider that is assigned to a moderate or high risk category. • Site visits are unannounced. • All moderate or high risk level providers will receive a Maine. Care site visit if they have not had a site visit with Medicare in the last 5 years. • If a provider fails a site visit, their Maine. Care enrollment is terminated or denied.
NOPR Providers 18 • Physicians and other practitioners who order, prescribe, or refer items or services for Maine. Care members, but who do not submit claims, are referred to as NOPR providers. • NOPR providers may enroll independently or as part of an organization that is enrolled in Maine. Care. If you belong to a group or are employed by a group, please discuss your enrollment with your group or organization. • Independent NOPR providers may enroll at any time after the system upgrade January 2017. • Organizations may enroll NOPRs as part of their revalidation application. • The NPI of the NOPR provider is required on claims and is validated against the Maine. Care provider enrollment file.
NOPR: Provider Type This list identifies the practitioner provider types that are required to be enrolled as a NOPR provider to order, prescribe, or refer services for Maine. Care members either independently or as part of a group or organization: • • 19 Advanced Practice Registered Nurse Chiropractor Dentist Optometrist Physician Assistant Podiatrist
NOPR: Independent NOPR providers enroll similar to an Individual provider, using the online portal PEA. • Independent NOPR providers are required to: o Register as a trading partner. o Complete an abbreviated PEA. o Read and acknowledge the online portal attestations. o Provide appropriate licensing and credentialing information and documentation. o Sign a provider agreement. o Screening as a limited risk category provider. • Once approved, independent NOPR providers have access to the PEA where they maintain their information, view member eligibility, and submit prior authorizations and referrals. • Their NPIs are used by billing providers for ordering, prescribing, or referring purposes. 20
NOPR: Organizations and Groups 21 • Some organizations that have not previously enrolled rendering providers are required to enroll NOPR providers with their revalidation application if the practitioners are not enrolled with Maine. Care as an individual, independent NOPR or as a rendering provider with other organizations. • Examples include Federally Qualified Health Centers (FQHC), Rural Health Centers (RHC), and Indian Health Services (IHS) providers. • Hospitals must ensure they have enrolled their 3 rd year residents that are licensed to practice as either a rendering or NOPR provider. • Hospitals must also ensure that all attending providers are enrolled in Maine. Care.
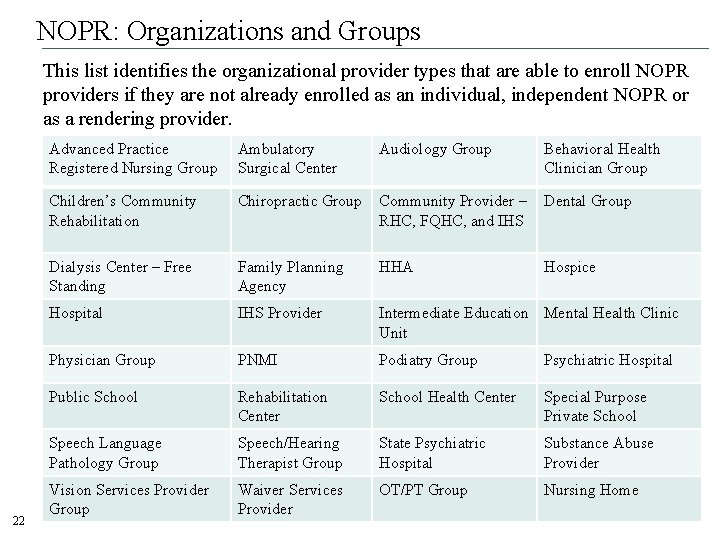
NOPR: Organizations and Groups This list identifies the organizational provider types that are able to enroll NOPR providers if they are not already enrolled as an individual, independent NOPR or as a rendering provider. 22 Advanced Practice Registered Nursing Group Ambulatory Surgical Center Audiology Group Behavioral Health Clinician Group Children’s Community Rehabilitation Chiropractic Group Community Provider – RHC, FQHC, and IHS Dental Group Dialysis Center – Free Standing Family Planning Agency HHA Hospice Hospital IHS Provider Intermediate Education Mental Health Clinic Unit Physician Group PNMI Podiatry Group Psychiatric Hospital Public School Rehabilitation Center School Health Center Special Purpose Private School Speech Language Pathology Group Speech/Hearing Therapist Group State Psychiatric Hospital Substance Abuse Provider Vision Services Provider Group Waiver Services Provider OT/PT Group Nursing Home
Health PAS Online Portal Changes The online portal is upgraded to support the revalidation process. The upgrade included improvements to the layout and navigation of the online portal, but the overall functionality does not change. Online portal enhancements include: • Redesigned homepage, using a tab layout instead of links. • Ability to view all letters and letter history. • New Enrollment Summary Report. • The ability to send secure emails from your Trading Partner Account (TPA). • Updated PEA to support new requirements under ACA. • The ability to upload documents within the PEA. • Minor navigational changes to access information. • Bulk upload and bulk update for service locations, rendering providers, and ordering/referring providers. 23
Health PAS Online Portal: New Sign In and Registration 24
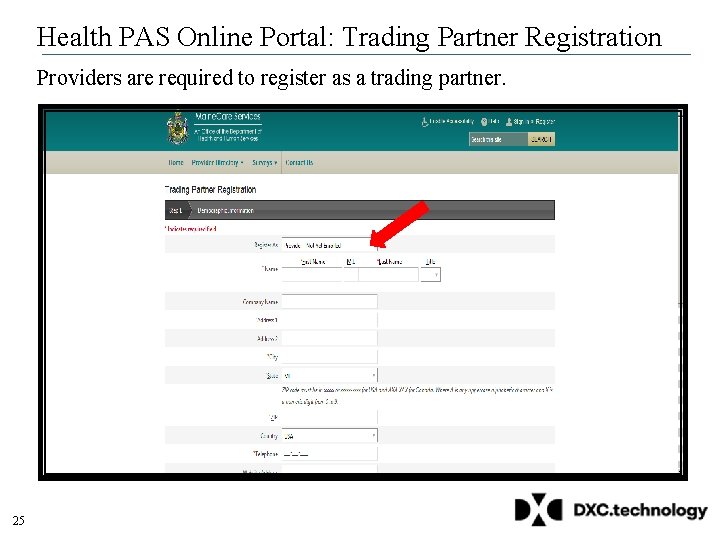
Health PAS Online Portal: Trading Partner Registration Providers are required to register as a trading partner. 25
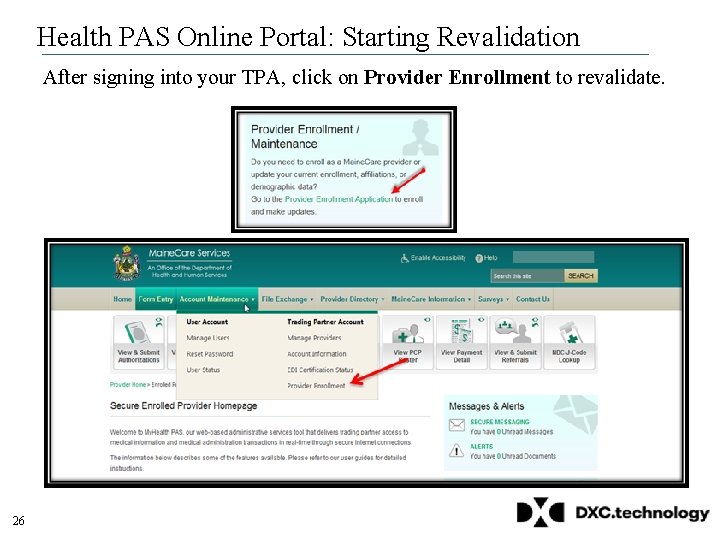
Health PAS Online Portal: Starting Revalidation After signing into your TPA, click on Provider Enrollment to revalidate. 26
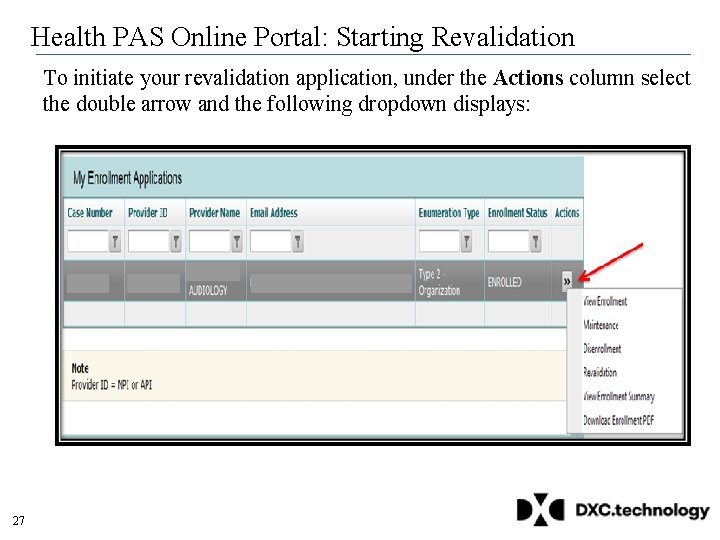
Health PAS Online Portal: Starting Revalidation To initiate your revalidation application, under the Actions column select the double arrow and the following dropdown displays: 27
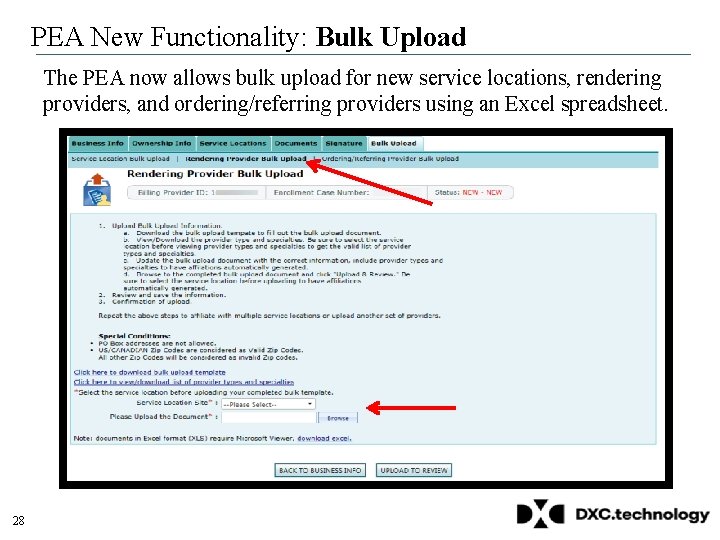
PEA New Functionality: Bulk Upload The PEA now allows bulk upload for new service locations, rendering providers, and ordering/referring providers using an Excel spreadsheet. 28
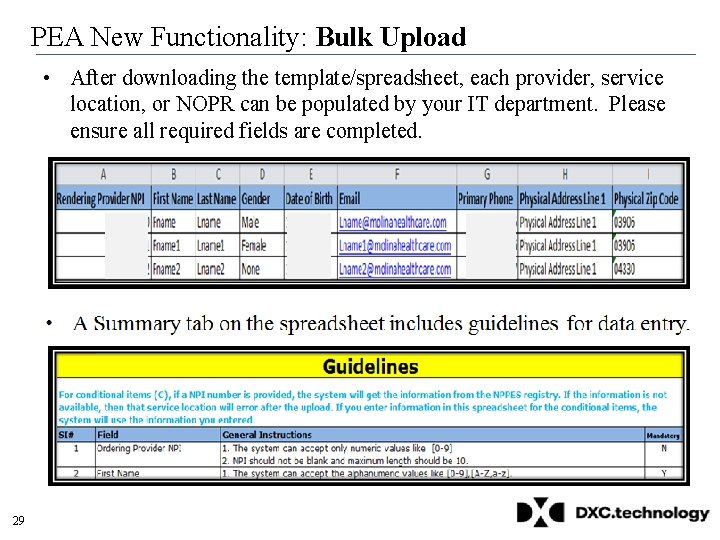
PEA New Functionality: Bulk Upload • After downloading the template/spreadsheet, each provider, service location, or NOPR can be populated by your IT department. Please ensure all required fields are completed. 29
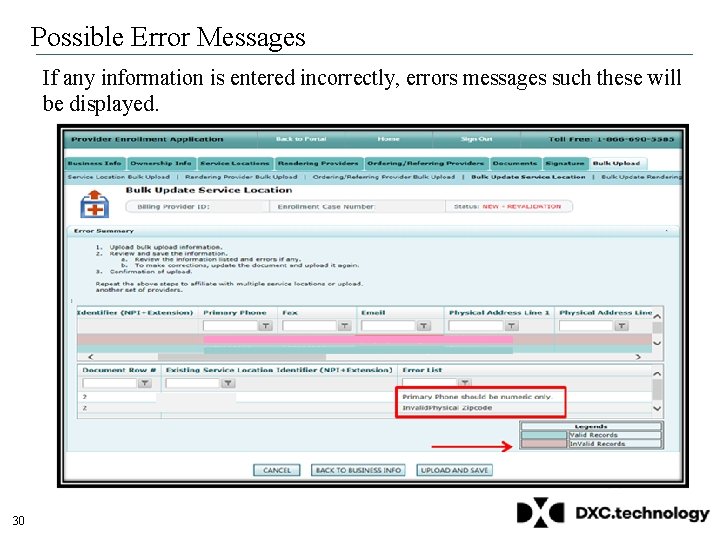
Possible Error Messages If any information is entered incorrectly, errors messages such these will be displayed. 30
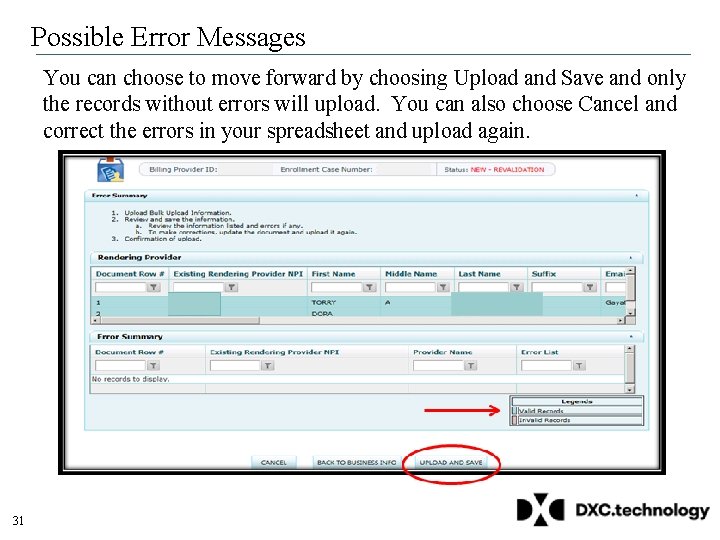
Possible Error Messages You can choose to move forward by choosing Upload and Save and only the records without errors will upload. You can also choose Cancel and correct the errors in your spreadsheet and upload again. 31
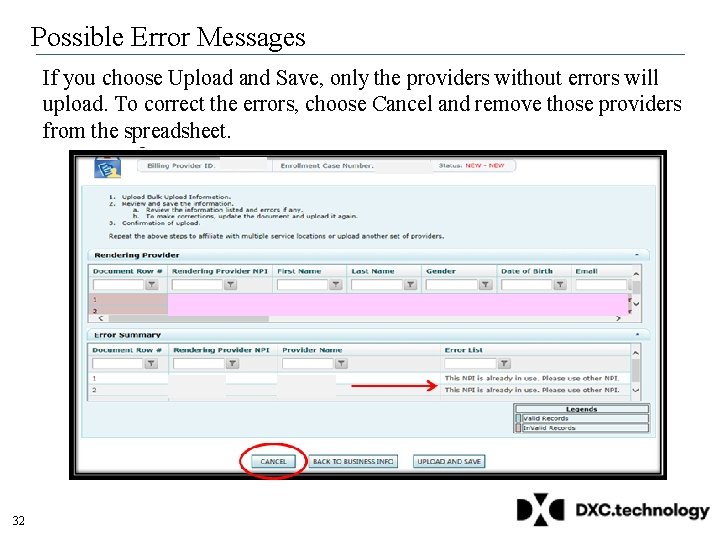
Possible Error Messages If you choose Upload and Save, only the providers without errors will upload. To correct the errors, choose Cancel and remove those providers from the spreadsheet. 32
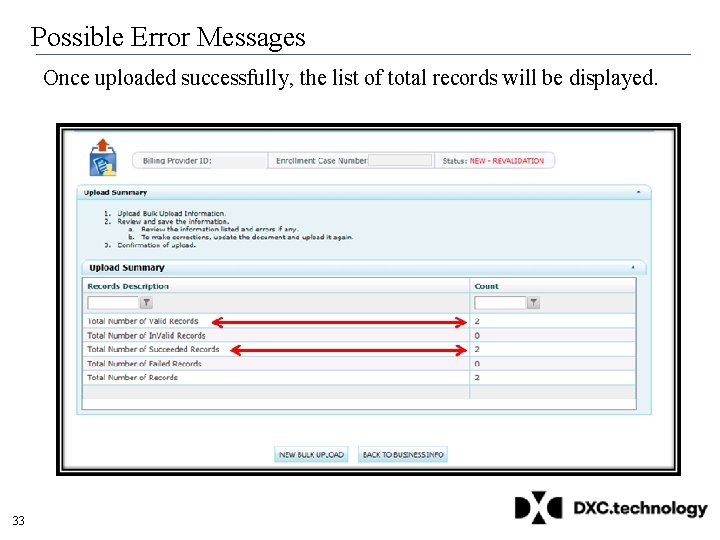
Possible Error Messages Once uploaded successfully, the list of total records will be displayed. 33
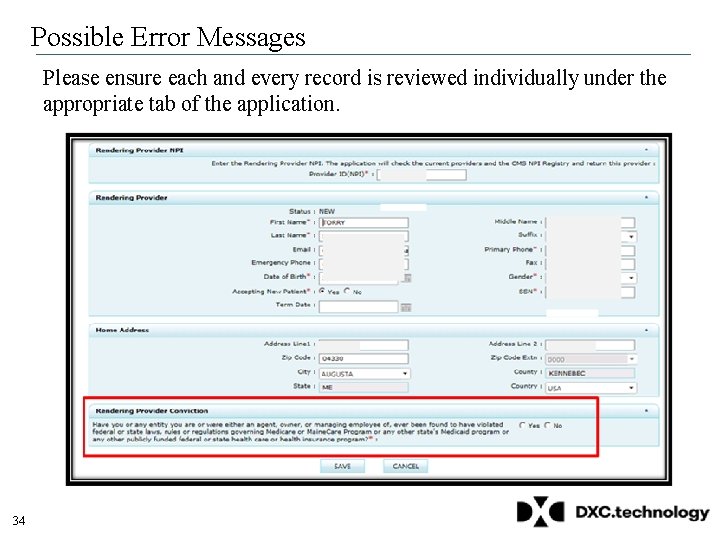
Possible Error Messages Please ensure each and every record is reviewed individually under the appropriate tab of the application. 34
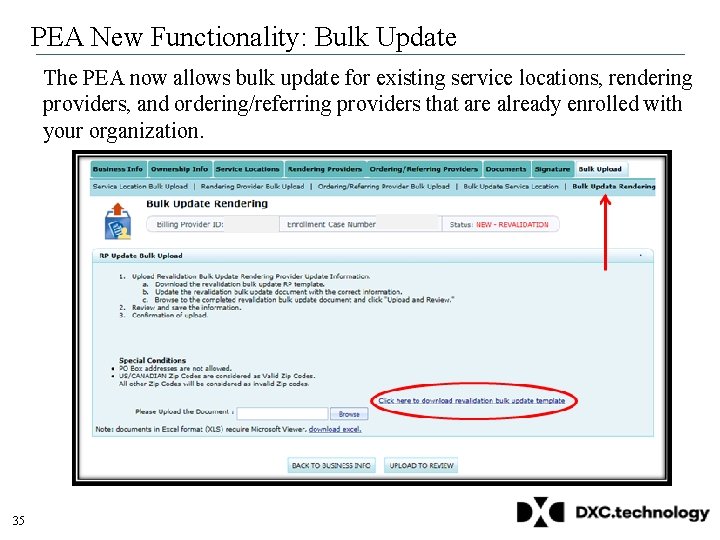
PEA New Functionality: Bulk Update The PEA now allows bulk update for existing service locations, rendering providers, and ordering/referring providers that are already enrolled with your organization. 35
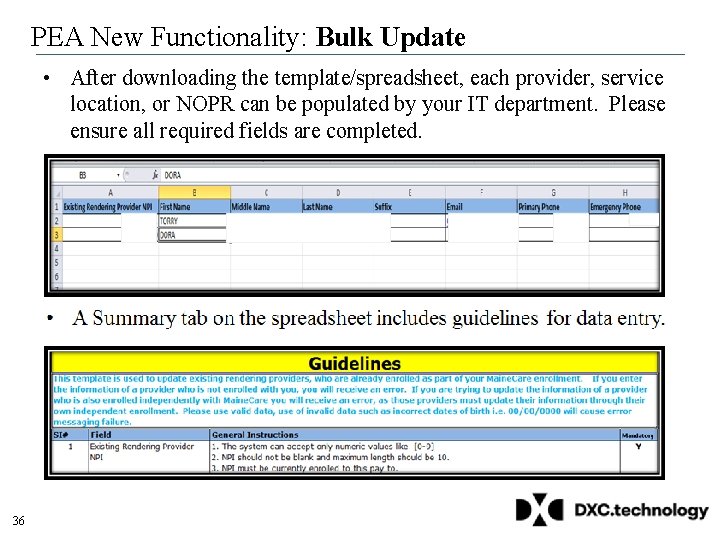
PEA New Functionality: Bulk Update • After downloading the template/spreadsheet, each provider, service location, or NOPR can be populated by your IT department. Please ensure all required fields are completed. 36
Next Steps • Please begin preparing so you are ready to submit your revalidation application and supporting documentation. • Know which revalidation cycle you are assigned. • Identify the individual within your organization who is submitting the application. • Begin gathering the information needed to update the application which includes owner, board member, and managing employee information, including their SSNs and DOBs. • Obtain license and certification information for service locations and practitioners required for your provider type and specialty. • Review your Enrollment Summary available online in the PEA. • Provider enrollment guides and checklists are available on the Health PAS Online Portal to assist you with preparing for revalidation. 37
Stay Informed The following resources are available to assist with the ACA provider revalidation project: • Maine. Care Provider Enrollment Webpage http: //www. maine. gov/dhhs/oms/enrollment. shtml • Maine. Care Revalidation Email Box Maine. Care. ACARevalidation@Molina. Healthcare. com • Maine. Care Provider Enrollment Frequently Asked Questions http: //www. maine. gov/dhhs/oms/enrollment-faq. shtml • Provider Enrollment Guides and Checklists https: //mainecare. maine. gov/Provider Enrollment Guides/Forms/On. Line Display View. aspx • Provider Services Call Center: 1 -866 -690 -5585, Option 7; TTY users dial 711 38
- Slides: 38