Provider Directory Advisory Committee Meeting March 15 2017
















- Slides: 55

Provider Directory Advisory Committee Meeting March 15, 2017
Welcome! • Rollcall and agenda review (5 min) • PDAC introductions (10 min) • Charter and work plan (20 min) • Refresh on Provider Directory functions, features, and timeline and Introduction and discussion on risks, barriers, gaps (25 min) • HIT Portfolio update (10 min) • Common Credentialing update (20 min) • HIT Commons presentation (20 min) • Close (10 min)
Introductions • Name and where you’re from • Write down one word that you think of when you hear “Provider Directory” • Tell group your one word and why you chose to participate in the PDAC

PDAC Charter and Work Plan Karen Hale
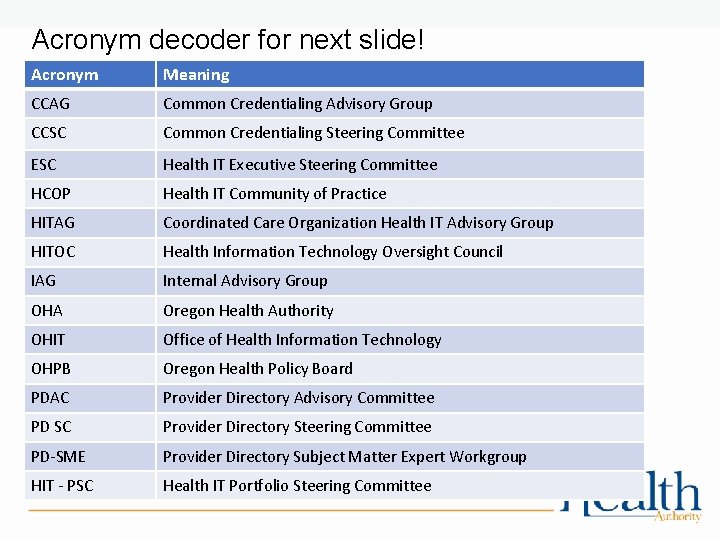
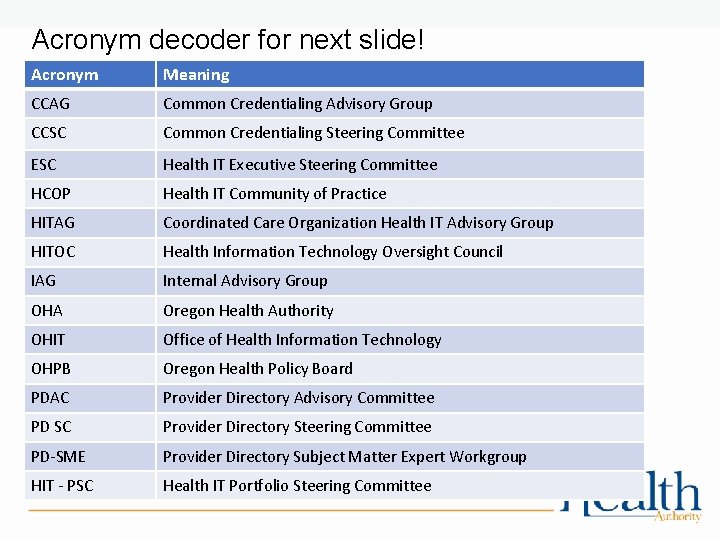
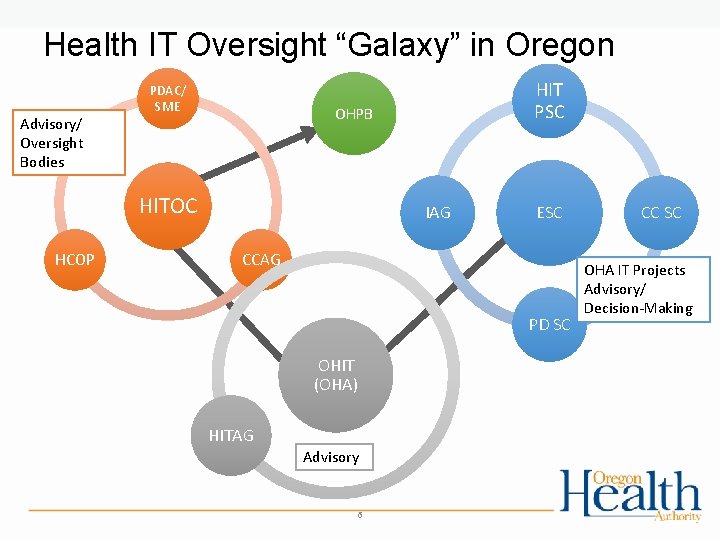
Acronym decoder for next slide! Acronym Meaning CCAG Common Credentialing Advisory Group CCSC Common Credentialing Steering Committee ESC Health IT Executive Steering Committee HCOP Health IT Community of Practice HITAG Coordinated Care Organization Health IT Advisory Group HITOC Health Information Technology Oversight Council IAG Internal Advisory Group OHA Oregon Health Authority OHIT Office of Health Information Technology OHPB Oregon Health Policy Board PDAC Provider Directory Advisory Committee PD SC Provider Directory Steering Committee PD-SME Provider Directory Subject Matter Expert Workgroup HIT - PSC Health IT Portfolio Steering Committee
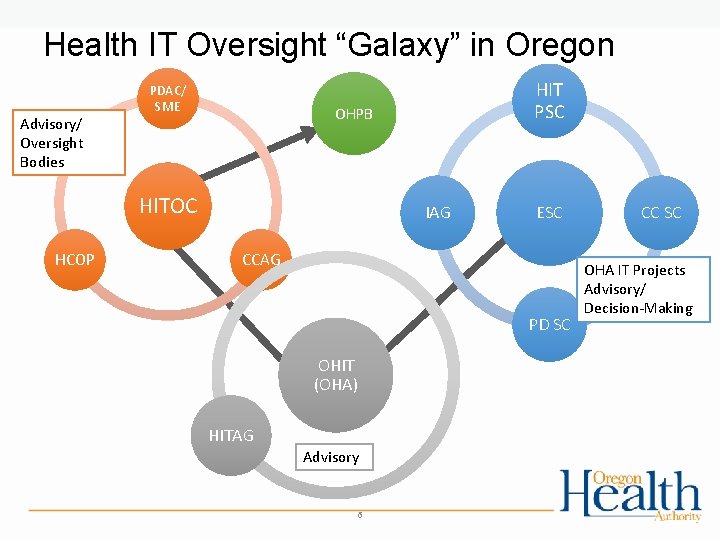
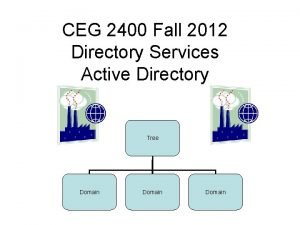
Health IT Oversight “Galaxy” in Oregon Advisory/ Oversight Bodies PDAC/ SME OHPB HITOC HCOP HIT PSC IAG ESC CCAG PD SC OHIT (OHA) HITAG Advisory 6 CC SC OHA IT Projects Advisory/ Decision-Making
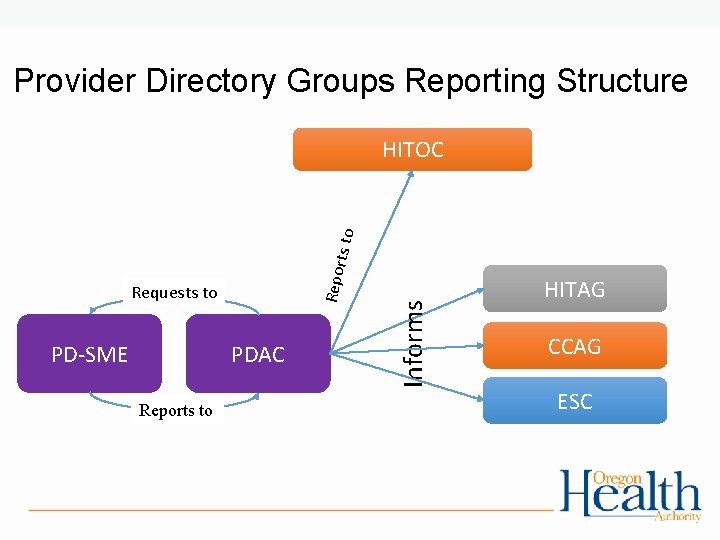
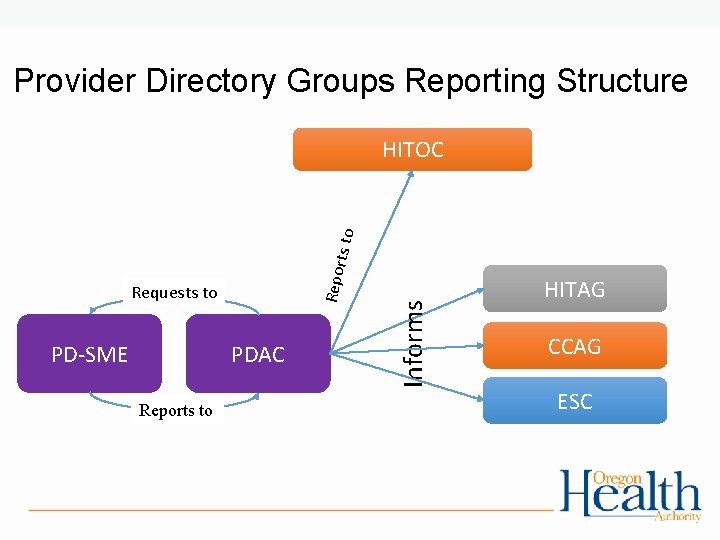
Provider Directory Groups Reporting Structure Requests to PD-SME PDAC Reports to Informs Repo rts to HITOC HITAG CCAG ESC
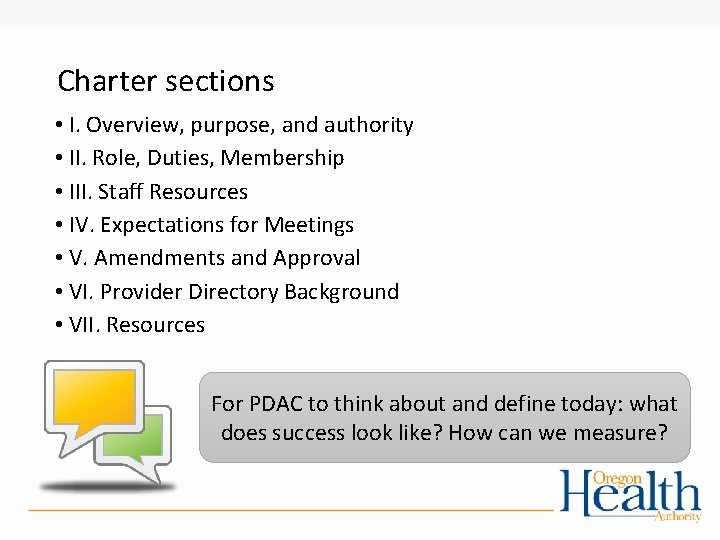
Charter sections • I. Overview, purpose, and authority • II. Role, Duties, Membership • III. Staff Resources • IV. Expectations for Meetings • V. Amendments and Approval • VI. Provider Directory Background • VII. Resources For PDAC to think about and define today: what does success look like? How can we measure?

I. Overview, purpose, and authority Purpose • PDAC: • to provide guidance that ensure a successful Provider Directory implementation • PD-SME • to ensure the Provider Directory meets the needs for users Authority • Not decision-making bodies • PD-SME reports to PDAC • PDAC reports to Heath Information Technology Oversight Council (HITOC)
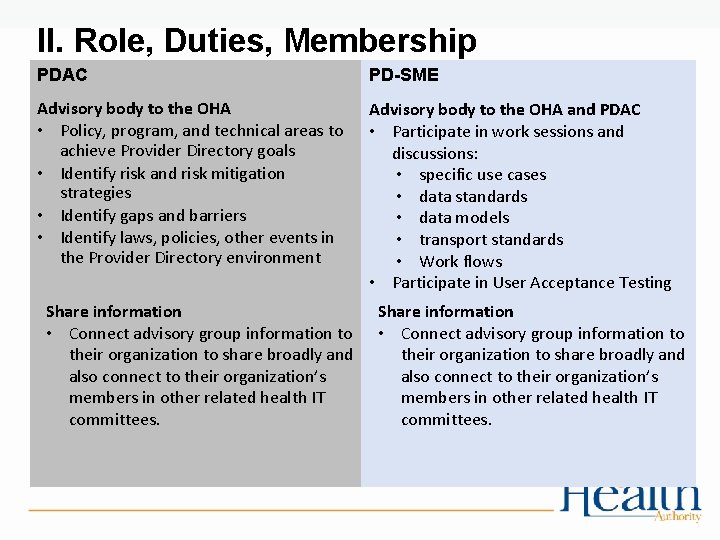
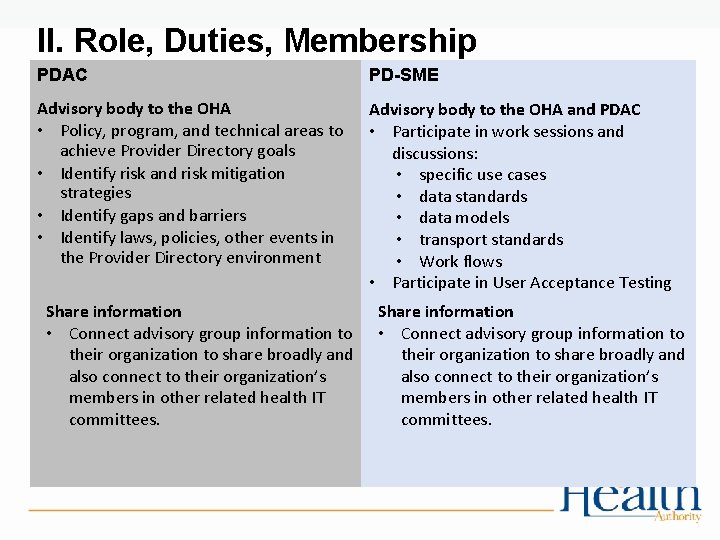
II. Role, Duties, Membership PDAC PD-SME Advisory body to the OHA • Policy, program, and technical areas to achieve Provider Directory goals • Identify risk and risk mitigation strategies • Identify gaps and barriers • Identify laws, policies, other events in the Provider Directory environment Advisory body to the OHA and PDAC • Participate in work sessions and discussions: • specific use cases • data standards • data models • transport standards • Work flows • Participate in User Acceptance Testing Share information • Connect advisory group information to their organization to share broadly and also connect to their organization’s members in other related health IT committees.

II. Role, Duties, Membership • Decisions by the group will be made by consensus; PDAC and PD-SME are not decision making bodies but provide critical recommendations and advice to OHA for the implementation of the Provider Directory • Membership terms • 2017 -2018 • Membership Composition § Hospitals § Health Information Exchanges § Health Plans • Chair § CCOs § Long term care § Clinics and providers § Behavioral Health § Dental § Independent Physician Association § Healthcare Research • OHA will select the Chair from among the Members; Martinez has been selected to serve as the PDAC chair
III. Staff Resources • The Council is staffed by the Office of HIT, as led by the Director of HIT, for the Oregon Health Authority. Support will be provided by other OHA leaders, staff, and consultants as requested or needed. • Karen Hale, Provider Directory Program Manager • Stacey Weight, Business Analyst • Jason Miranda, Lead Implementation Analyst • Rachel Ostroy, Implementation Director • Susan Otter, Director and State Coordinator for Health Information Technology
IV. Expectations for Meetings • The PDAC and PD-SME will meet every other month in offsetting months beginning in March 2017; • Location of meetings will be in the Portland/Willamette Valley area; • A standard meeting time will be established; • Meeting materials and notes will be posted to the OHA’s Provider Directory website; • OHA may also call for member participation outside the regularly scheduled meetings if needed; • In-person attendance at the meetings is preferred; • Ad hoc meetings can be called; • All meetings will be public and documented on the Provider Directory website and meet requirements for public meetings: http: //www. oregon. gov/oha/OHIT/Pages/Provider-Directory-Advisory. aspx • Members are expected to review materials ahead of the meeting and come prepared to discuss and participate.
V. Amendments and Approval This charter may be amended. An amended charter requires approval by HITOC before it takes effect
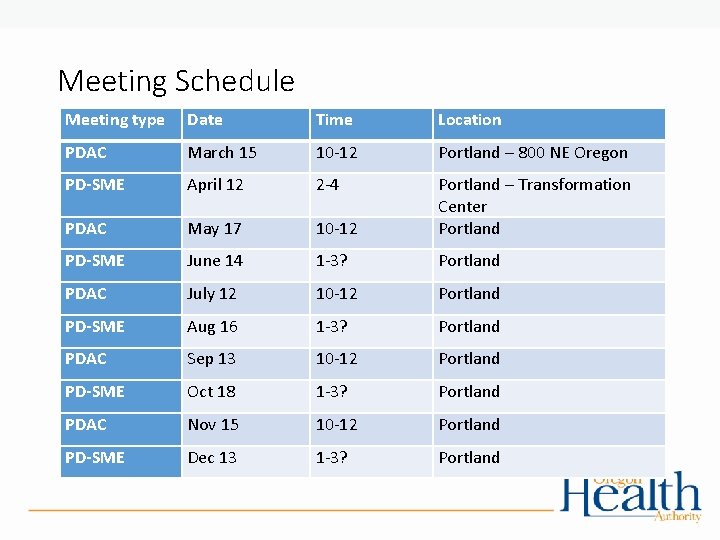
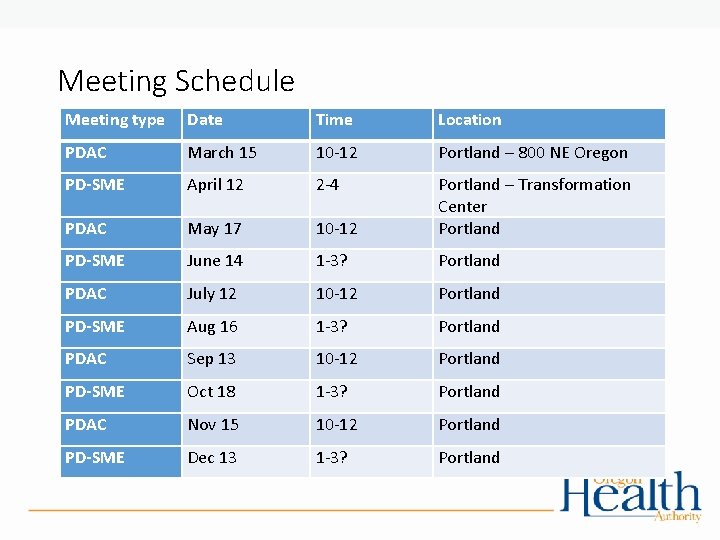
Meeting Schedule Meeting type Date Time Location PDAC March 15 10 -12 Portland – 800 NE Oregon PD-SME April 12 2 -4 PDAC May 17 10 -12 Portland – Transformation Center Portland PD-SME June 14 1 -3? Portland PDAC July 12 10 -12 Portland PD-SME Aug 16 1 -3? Portland PDAC Sep 13 10 -12 Portland PD-SME Oct 18 1 -3? Portland PDAC Nov 15 10 -12 Portland PD-SME Dec 13 1 -3? Portland
Priority buckets of work for the PDAC ØGovernance – policies/program/technical ØData governance ØProgram governance ØCommunications strategies ØMarketing and Outreach ØAdoption and uptake strategies ØFee structures and options Review work plan
Group discussion • What are the objectives PDAC wants to achieve? • What are measures that can be used to determine if we met our objectives?
Provider Directory Refresher, Critical Success Factors, and identification of risks, gaps, and barriers
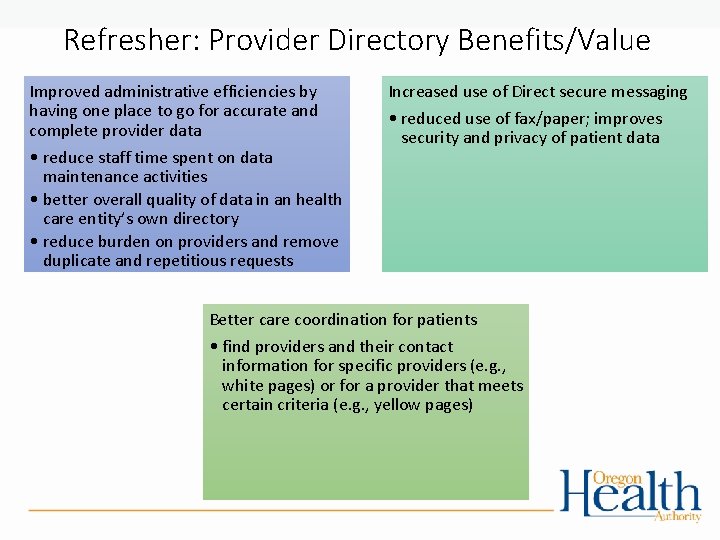
Refresher: Provider Directory Benefits/Value Improved administrative efficiencies by having one place to go for accurate and complete provider data • reduce staff time spent on data maintenance activities • better overall quality of data in an health care entity’s own directory • reduce burden on providers and remove duplicate and repetitious requests Increased use of Direct secure messaging • reduced use of fax/paper; improves security and privacy of patient data Better care coordination for patients • find providers and their contact information for specific providers (e. g. , white pages) or for a provider that meets certain criteria (e. g. , yellow pages)
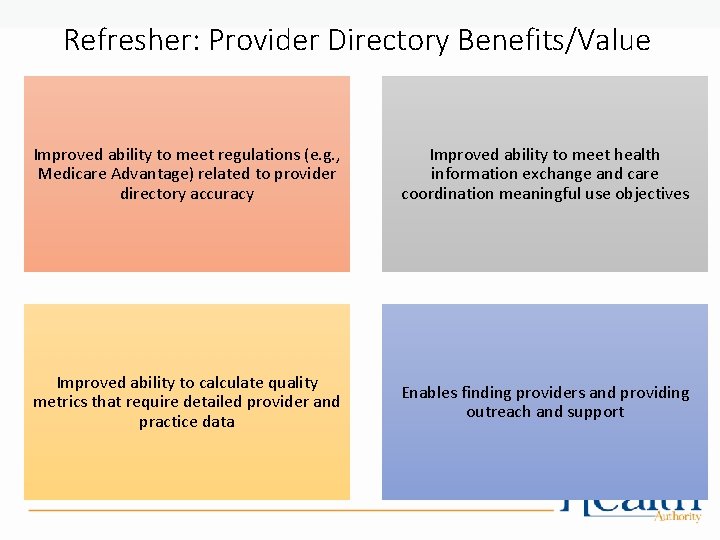
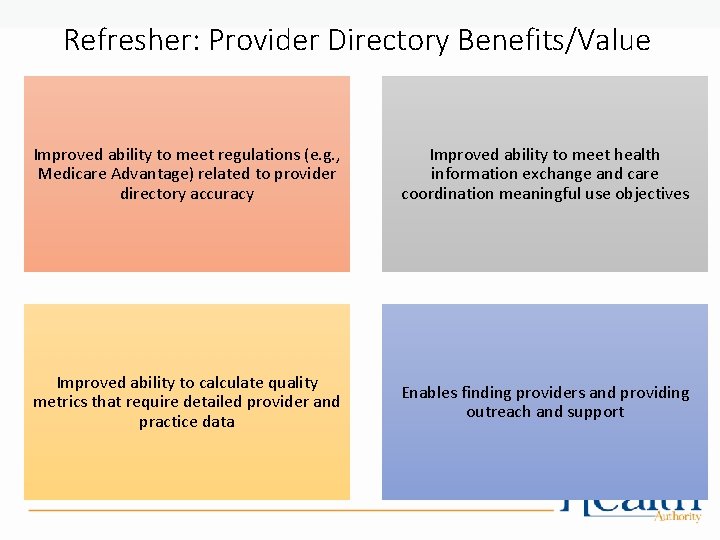
Refresher: Provider Directory Benefits/Value Improved ability to meet regulations (e. g. , Medicare Advantage) related to provider directory accuracy Improved ability to meet health information exchange and care coordination meaningful use objectives Improved ability to calculate quality metrics that require detailed provider and practice data Enables finding providers and providing outreach and support
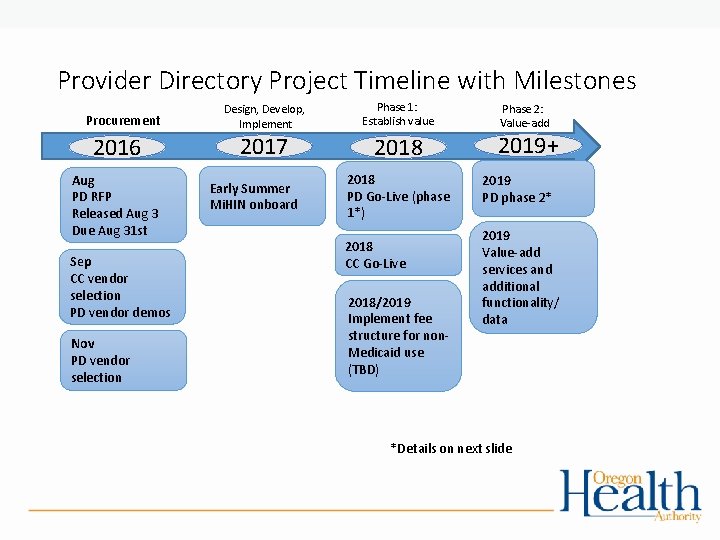
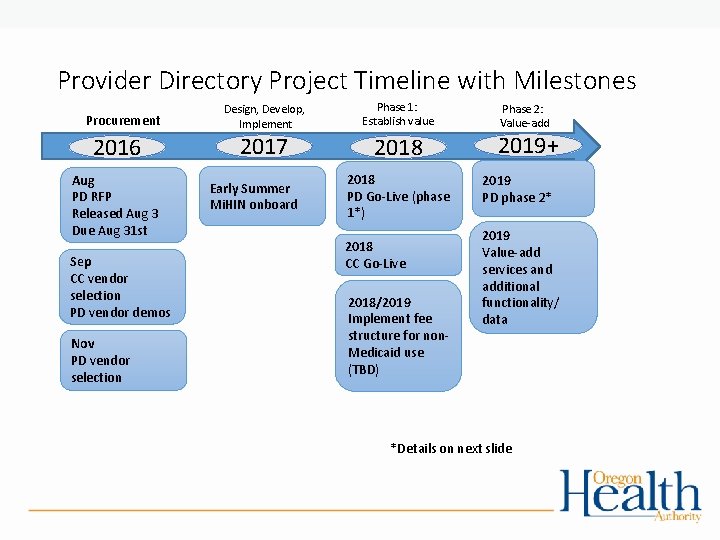
Provider Directory Project Timeline with Milestones Procurement 2016 Aug PD RFP Released Aug 3 Due Aug 31 st Sep CC vendor selection PD vendor demos Nov PD vendor selection Design, Develop, Implement Phase 1: Establish value 2017 2018 Early Summer Mi. HIN onboard 2018 PD Go-Live (phase 1*) 2018 CC Go-Live 2018/2019 Implement fee structure for non. Medicaid use (TBD) Phase 2: Value-add 2019+ 2019 PD phase 2* 2019 Value-add services and additional functionality/ data *Details on next slide
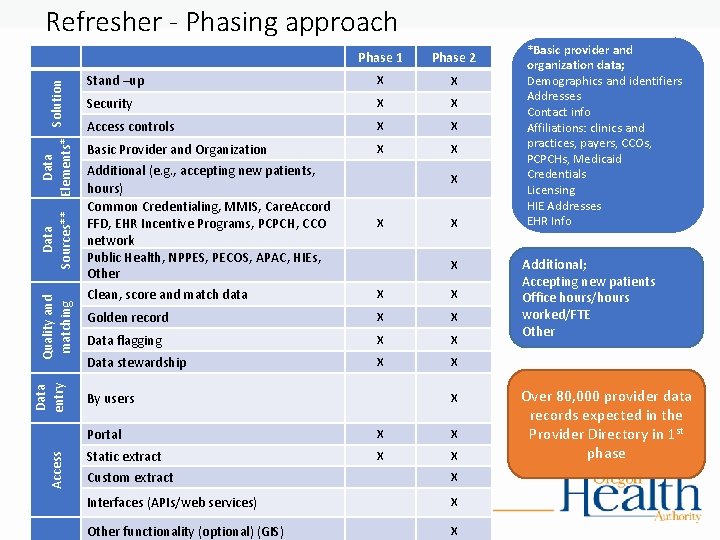
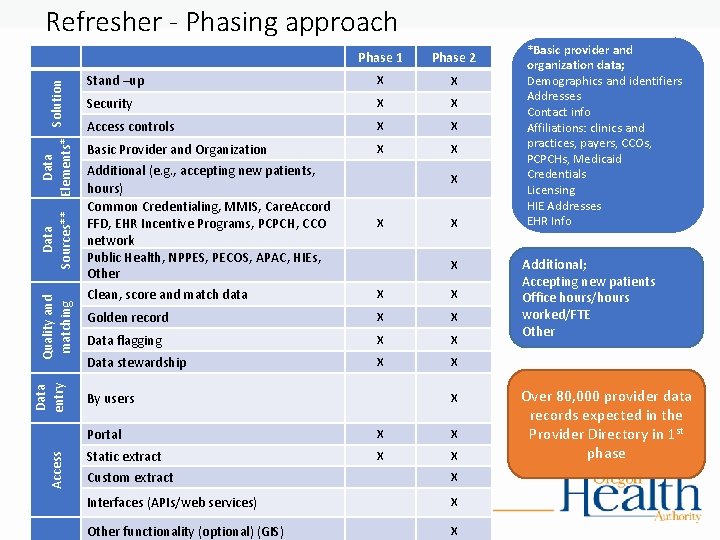
Access Data entry Quality and matching Data Solution Sources** Elements* Refresher - Phasing approach Phase 1 Phase 2 Stand –up X X Security X X Access controls X X Basic Provider and Organization X X Additional (e. g. , accepting new patients, hours) Common Credentialing, MMIS, Care. Accord FFD, EHR Incentive Programs, PCPCH, CCO network Public Health, NPPES, PECOS, APAC, HIEs, Other Clean, score and match data X X X Golden record X X Data flagging X X Data stewardship X X By users X Portal X X Static extract X X Custom extract X Interfaces (APIs/web services) X Other functionality (optional) (GIS) X *Basic provider and organization data; Demographics and identifiers Addresses Contact info Affiliations: clinics and practices, payers, CCOs, PCPCHs, Medicaid Credentials Licensing HIE Addresses EHR Info Additional; Accepting new patients Office hours/hours worked/FTE Other Over 80, 000 provider data records expected in the Provider Directory in 1 st phase
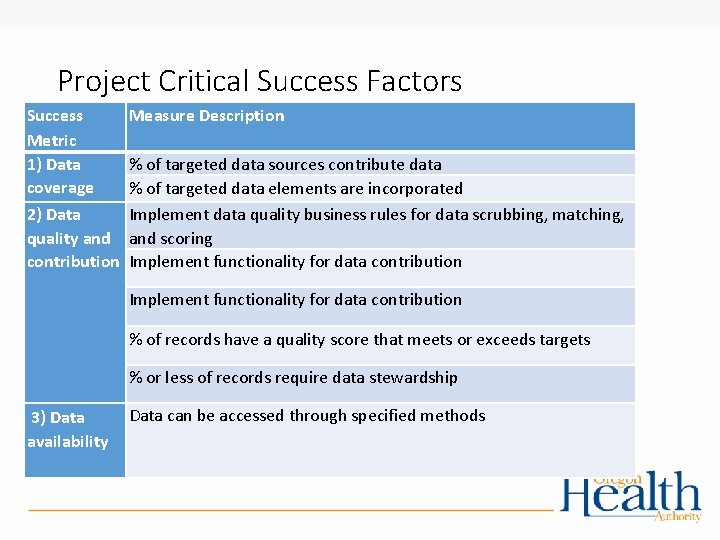
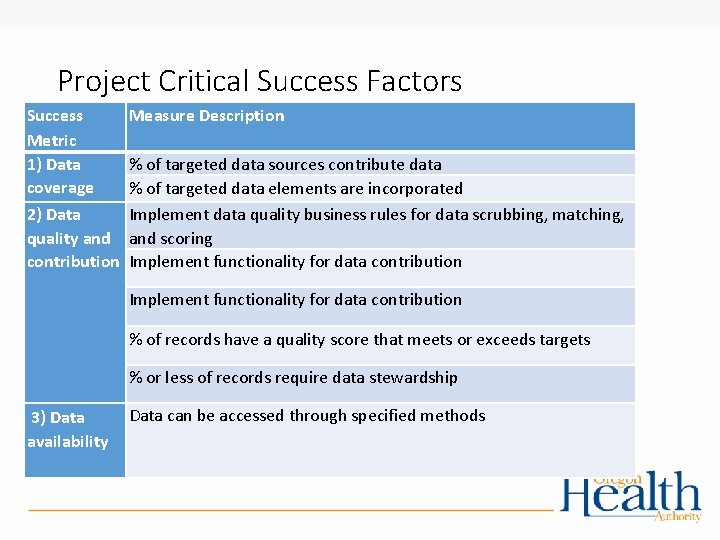
Project Critical Success Factors Success Metric 1) Data coverage Measure Description Implement functionality for data contribution % of targeted data sources contribute data % of targeted data elements are incorporated 2) Data Implement data quality business rules for data scrubbing, matching, quality and scoring contribution Implement functionality for data contribution % of records have a quality score that meets or exceeds targets % or less of records require data stewardship 3) Data availability Data can be accessed through specified methods

Project Critical Success Factors Success Metric 4) User satisfaction Measure Description Satisfaction surveys have scores that meet targets and has a response rate of at least 10% Help desk ticket resolution scores meet targets % on-boarded users log in to the PD 5) User adoption and uptake 6) Cost Coverage O&M costs are covered by fees

Risks, Barriers, Gaps When implementing the Provider Directory, 1) What are some of the risks that may impact success? • On a scale from 1 -10 • What is the likelihood that will happen? • How much could it impact the Provider Directory? • What strategies can be used to mitigate risks? 2) What are some of the barriers? gaps? countermeasures?

Risks, Barriers, Gaps Group Discussion Risk analysis Risk Probability Severity Score Mitigation Low adoption 5 8 40 Implement strong communication strategy Set adoption targets Check in with stakeholders “ruthlessly” to ensure cost/benefits are understood Ensure data can be trusted Additional items from group

Risks, Barriers, Gaps Group Discussion Gaps Countermeasures Accepting new patients is not in phase 1 Clear communication on what will be available and when Analyze work arounds Additional items from group Barriers Barrier Countermeasures Timing for the provider directory to become live and contractor onboard due to state and federal contract processes Research methods to potentially speed up the approval process Additional items from group

HIT Portfolio Update Rachel Ostroy Implementation Director
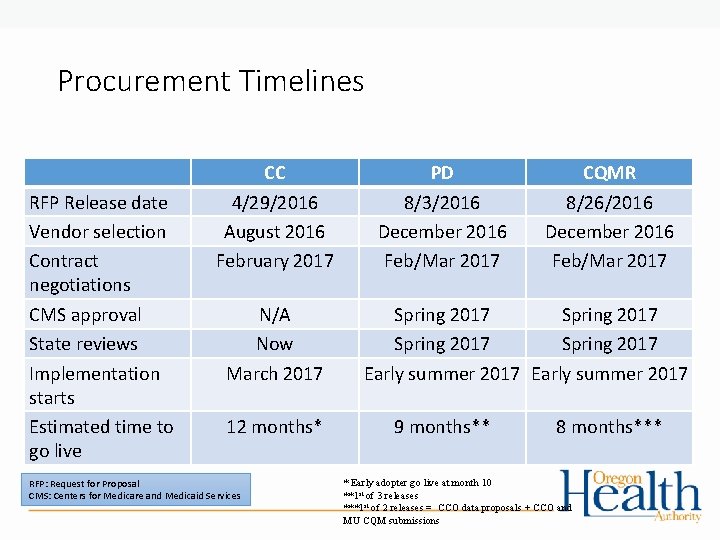
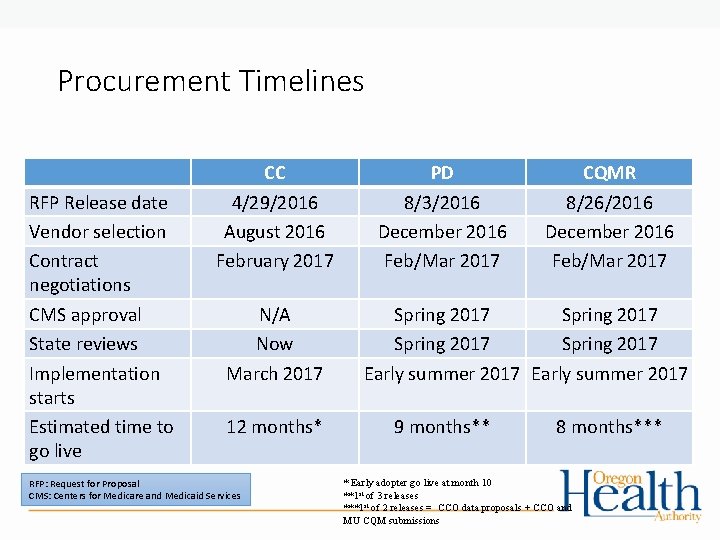
Procurement Timelines RFP Release date Vendor selection Contract negotiations CMS approval State reviews Implementation starts Estimated time to go live CC 4/29/2016 August 2016 February 2017 N/A Now March 2017 12 months* RFP: Request for Proposal CMS: Centers for Medicare and Medicaid Services PD 8/3/2016 December 2016 Feb/Mar 2017 CQMR 8/26/2016 December 2016 Feb/Mar 2017 Spring 2017 Early summer 2017 9 months** 8 months*** * Early adopter go live at month 10 **1 st of 3 releases ***1 st of 2 releases = CCO data proposals + CCO and MU CQM submissions
PD Implementation Next Steps üFinalize PD Implementation Statement of Work (SOW) Review • OHA and Harris Team complete contract negotiations • Complete State approval process (Stage Gate) for Implementation Phase • Receive approval from Centers for Medicare and Medicaid Services (CMS) • Execute Harris contract amendment • Execute Mi. HIN subcontract; One. Health. Port (OHP) and Fiscal Services subcontracts • Mi. HIN Implementation Phase Kickoff – Estimated early summer 2017 Parallel tasks
The Oregon Common Credentialing Program March 15, 2017 Melissa Isavoran, Program Manager Health Policy & Analytics Office of Health Information Technology
Common Credentialing Overview “A centralized system that collects and verify health care practitioner credentials can provide efficiencies in the credentialing process across multiple entities and attribute to greater patient safety due to collective assurances of credentials. ” 32
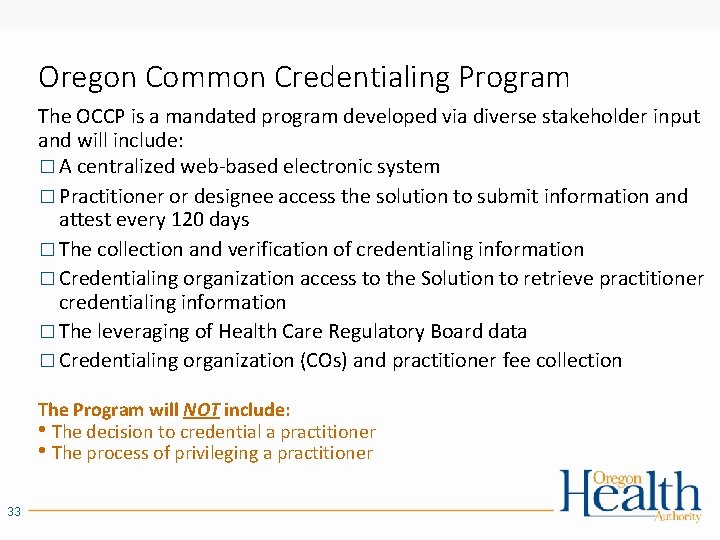
Oregon Common Credentialing Program The OCCP is a mandated program developed via diverse stakeholder input and will include: � A centralized web-based electronic system � Practitioner or designee access the solution to submit information and attest every 120 days � The collection and verification of credentialing information � Credentialing organization access to the Solution to retrieve practitioner credentialing information � The leveraging of Health Care Regulatory Board data � Credentialing organization (COs) and practitioner fee collection The Program will NOT include: • The decision to credential a practitioner • The process of privileging a practitioner 33
OCCP User Value 34
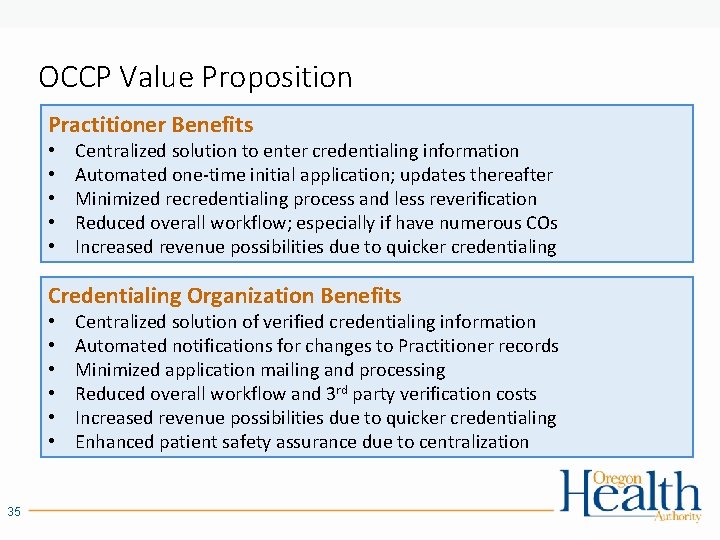
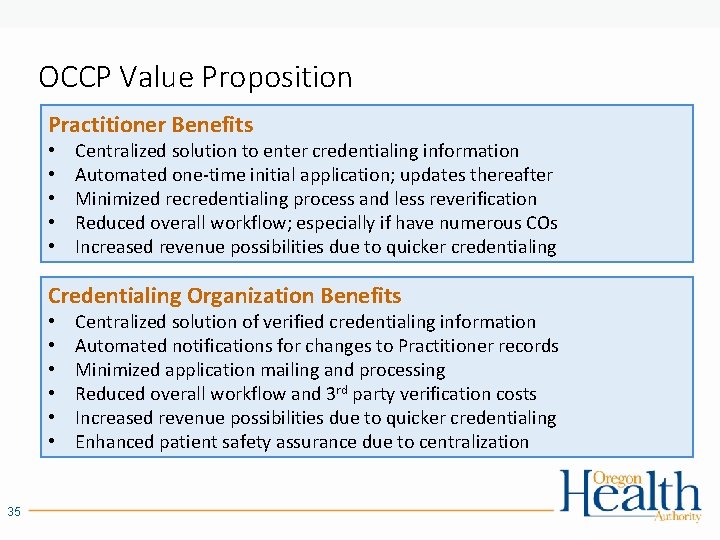
OCCP Value Proposition Practitioner Benefits • • • Centralized solution to enter credentialing information Automated one-time initial application; updates thereafter Minimized recredentialing process and less reverification Reduced overall workflow; especially if have numerous COs Increased revenue possibilities due to quicker credentialing Credentialing Organization Benefits • • • 35 Centralized solution of verified credentialing information Automated notifications for changes to Practitioner records Minimized application mailing and processing Reduced overall workflow and 3 rd party verification costs Increased revenue possibilities due to quicker credentialing Enhanced patient safety assurance due to centralization

Practitioner Value Credentialing process Submitting initial applications Submitting supporting documentation HCP current workflow Submittal to each new CO Ensure application completeness Submittal to each CO Submittal to each requesting CO Coordination with each CO Submitting recredentialing applications Submittal to each CO Submitting CO specific documentation HCP post OCCP workflow One time initial submittal to OCCP Submittal to each requesting CO Coordination with OCCP Attest to OCCP every 120 days Notes: • While the recredentialing process will continue to exist, the recredentialing application will no longer be necessary as COs will be able to access the OCCP system to retrieve a current Oregon Practitioner Credentialing Application with updated attestations/verifications for the practitioners in which they have access. • Practitioners credentialed with one or fewer COs will be excluded from 120 day attestation requirement. 36
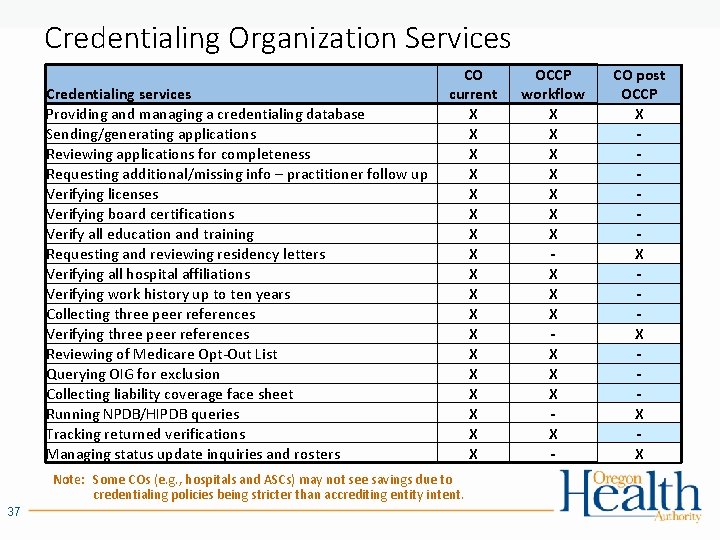
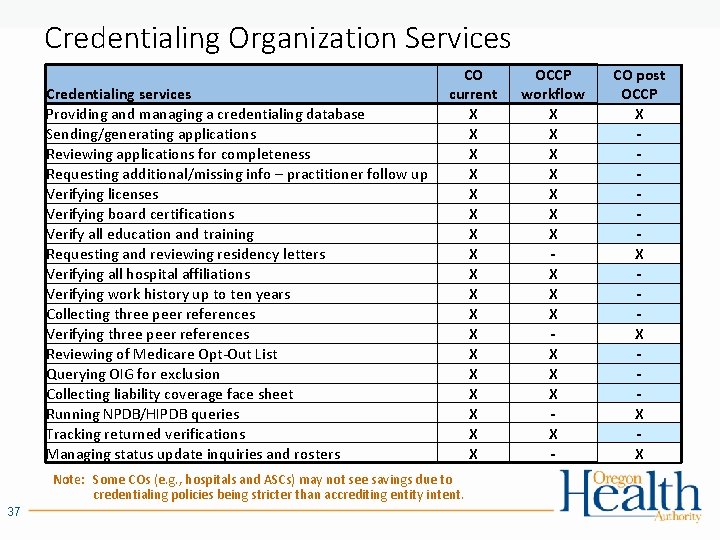
Credentialing Organization Services Credentialing services Providing and managing a credentialing database Sending/generating applications Reviewing applications for completeness Requesting additional/missing info – practitioner follow up Verifying licenses Verifying board certifications Verify all education and training Requesting and reviewing residency letters Verifying all hospital affiliations Verifying work history up to ten years Collecting three peer references Verifying three peer references Reviewing of Medicare Opt-Out List Querying OIG for exclusion Collecting liability coverage face sheet Running NPDB/HIPDB queries Tracking returned verifications Managing status update inquiries and rosters CO current X X X X X Note: Some COs (e. g. , hospitals and ASCs) may not see savings due to credentialing policies being stricter than accrediting entity intent. 37 OCCP workflow X X X X - CO post OCCP X X X

Fee Development and Draft Model Review 38
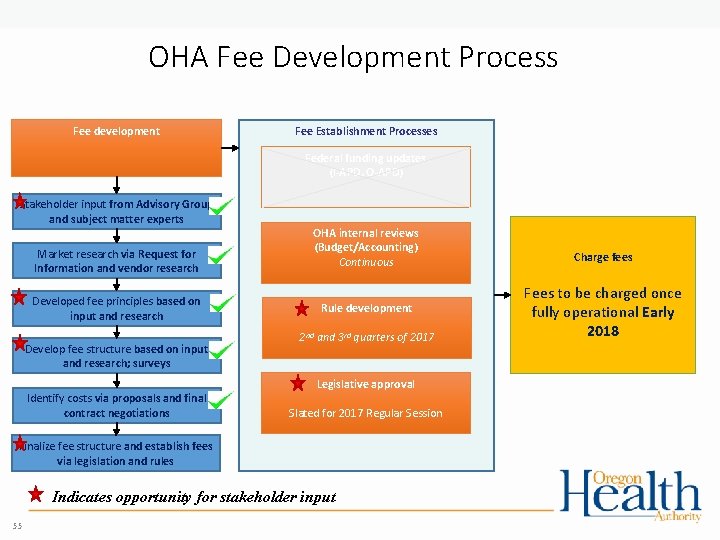
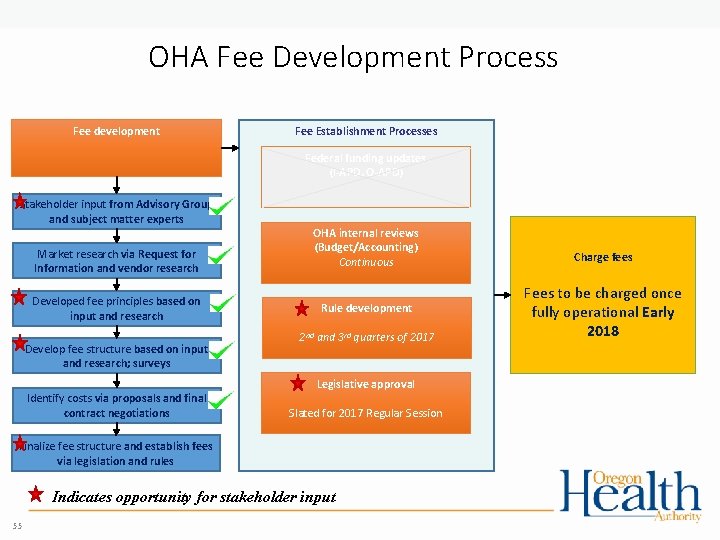
OHA Fee Development Process Fee development Fee Establishment Processes Federal funding updates (I-APD, O-APD) Stakeholder input from Advisory Group and subject matter experts Market research via Request for Information and vendor research Developed fee principles based on input and research Develop fee structure based on input and research; surveys OHA internal reviews (Budget/Accounting) Continuous Rule development 2 nd and 3 rd quarters of 2017 Legislative approval Identify costs via proposals and final contract negotiations Slated for 2017 Regular Session Finalize fee structure and establish fees via legislation and rules Indicates opportunity for stakeholder input 55 Charge fees Fees to be charged once fully operational Early 2018
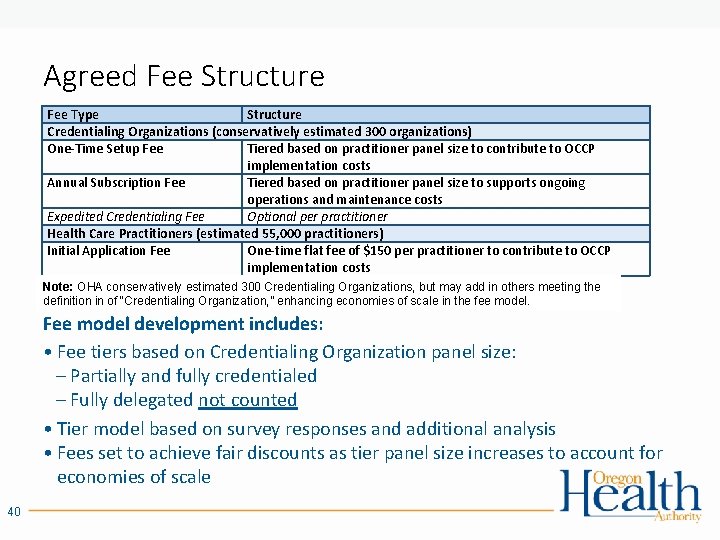
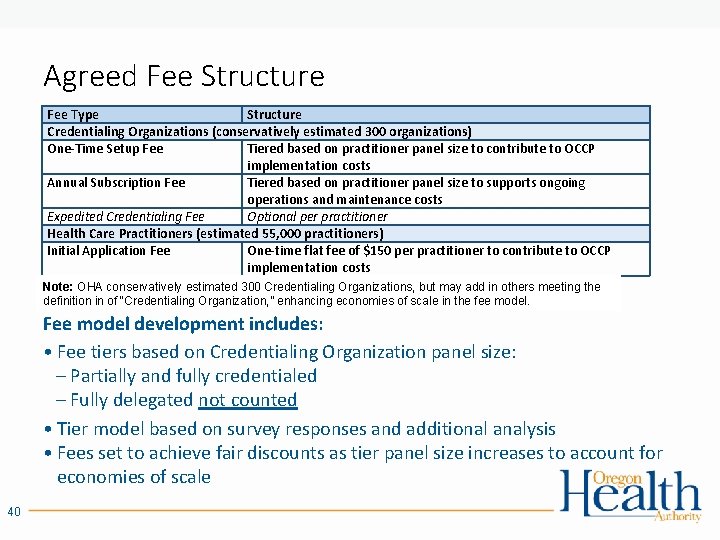
Agreed Fee Structure Fee Type Structure Credentialing Organizations (conservatively estimated 300 organizations) One-Time Setup Fee Tiered based on practitioner panel size to contribute to OCCP implementation costs Annual Subscription Fee Tiered based on practitioner panel size to supports ongoing operations and maintenance costs Expedited Credentialing Fee Optional per practitioner Health Care Practitioners (estimated 55, 000 practitioners) Initial Application Fee One-time flat fee of $150 per practitioner to contribute to OCCP implementation costs Note: OHA conservatively estimated 300 Credentialing Organizations, but may add in others meeting the definition in of “Credentialing Organization, ” enhancing economies of scale in the fee model. Fee model development includes: • Fee tiers based on Credentialing Organization panel size: – Partially and fully credentialed – Fully delegated not counted • Tier model based on survey responses and additional analysis • Fees set to achieve fair discounts as tier panel size increases to account for economies of scale 40
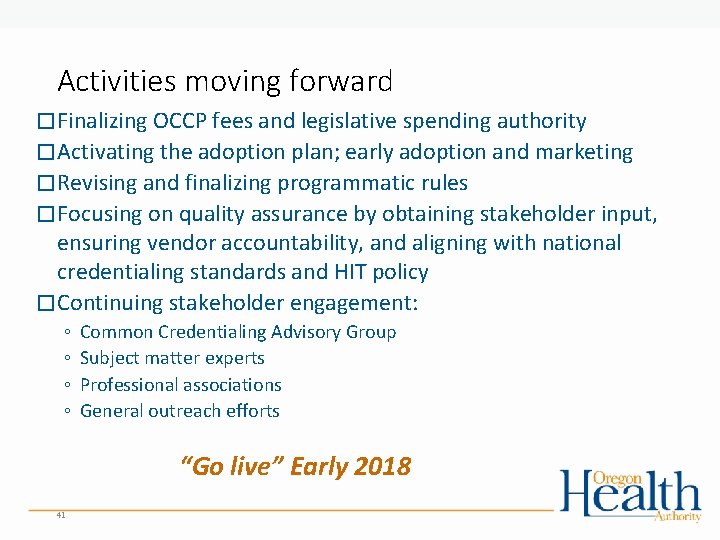
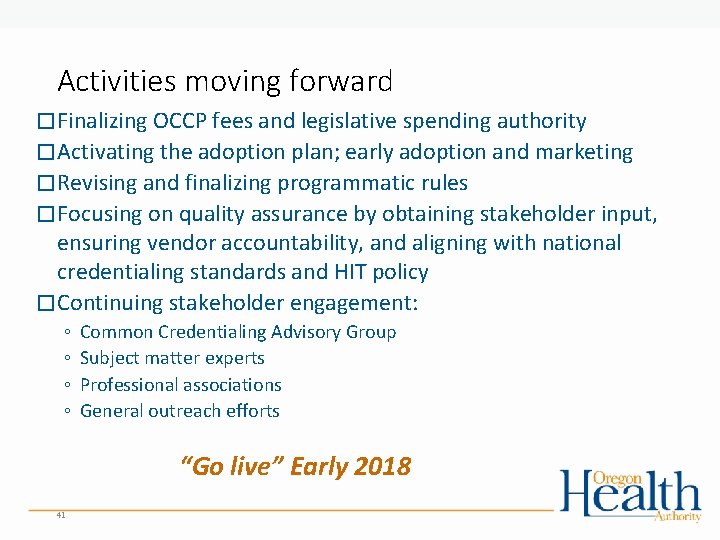
Activities moving forward � Finalizing OCCP fees and legislative spending authority � Activating the adoption plan; early adoption and marketing � Revising and finalizing programmatic rules � Focusing on quality assurance by obtaining stakeholder input, ensuring vendor accountability, and aligning with national credentialing standards and HIT policy � Continuing stakeholder engagement: ◦ ◦ Common Credentialing Advisory Group Subject matter experts Professional associations General outreach efforts “Go live” Early 2018 41
Questions? Send questions, comments, or volunteer interests to: credentialing@state. or. us More information can be found at: www. oregon. gov/oha/OHIT/occp 42

HIT Commons Sean Carey Lead Policy Analyst 43
Background for Collaboration • Oregon HIT strategy development in 2013 • • • IT infrastructure support for healthcare transformation Patient and family Providers Coordinated Care stakeholders Policy makers • Envisioned "Commons" approach to community wide access to essential information • "Democratization" of essential information • Governance structure to reflect interests of common good 44

Early Successes • One. Health. Port single sign on: voluntary, informal, standardize • EDIE / Pre. Manage: formal state/private "co-sponsorship" with common governance structure • State financial support for Medicaid share of infrastructure, and support for high priority Medicaid users of Pre. Manage (CCOs, behavioral health teams) • Private financial support/sponsorship for primary care clinics • Standard vendor contracts, data use agreements, research and analytic support, and decision making policies • Prescription Drug Monitoring Program – HIT Gateway • Coordinated legislative strategy • Coordinated technology solutions (e. g. , Gateway) • Potential for shared funding for infrastructure and operations that leverages federal, state and private funding 45
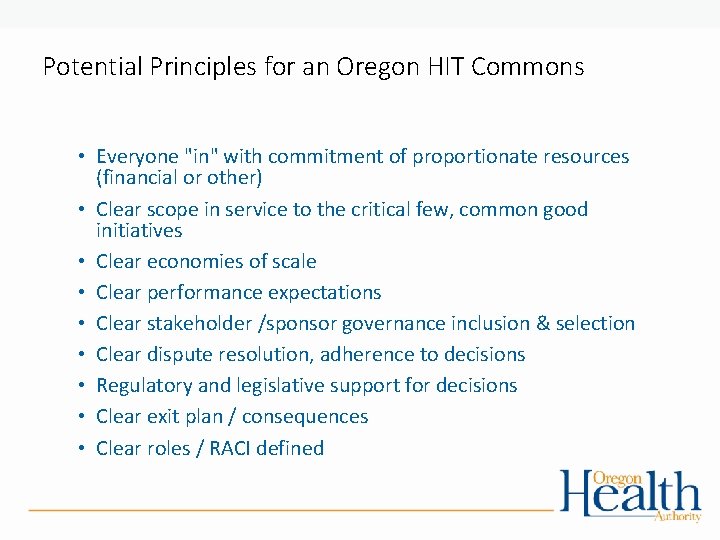
Potential Principles for an Oregon HIT Commons • Everyone "in" with commitment of proportionate resources (financial or other) • Clear scope in service to the critical few, common good initiatives • Clear economies of scale • Clear performance expectations • Clear stakeholder /sponsor governance inclusion & selection • Clear dispute resolution, adherence to decisions • Regulatory and legislative support for decisions • Clear exit plan / consequences • Clear roles / RACI defined
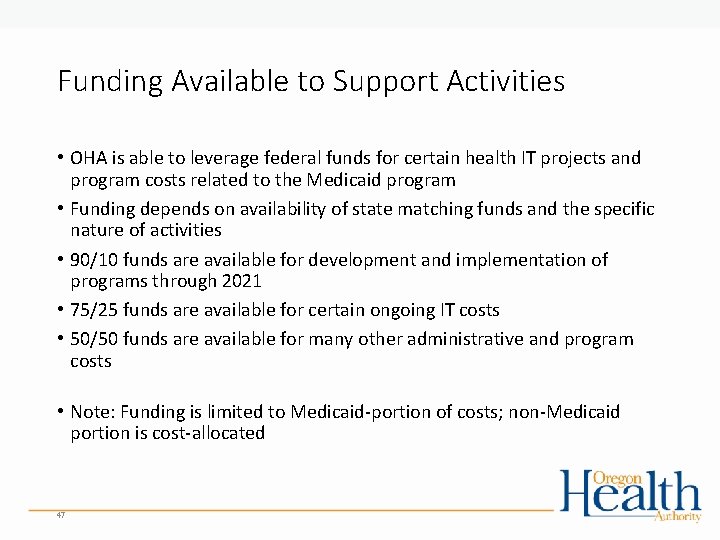
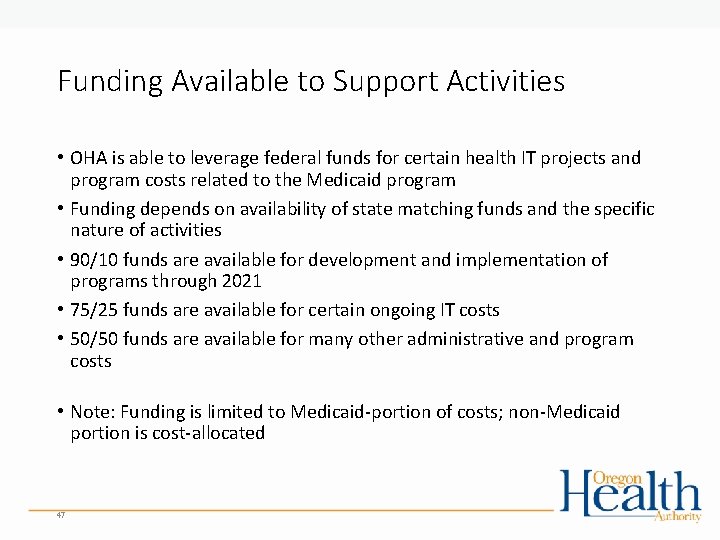
Funding Available to Support Activities • OHA is able to leverage federal funds for certain health IT projects and program costs related to the Medicaid program • Funding depends on availability of state matching funds and the specific nature of activities • 90/10 funds are available for development and implementation of programs through 2021 • 75/25 funds are available for certain ongoing IT costs • 50/50 funds are available for many other administrative and program costs • Note: Funding is limited to Medicaid-portion of costs; non-Medicaid portion is cost-allocated 47
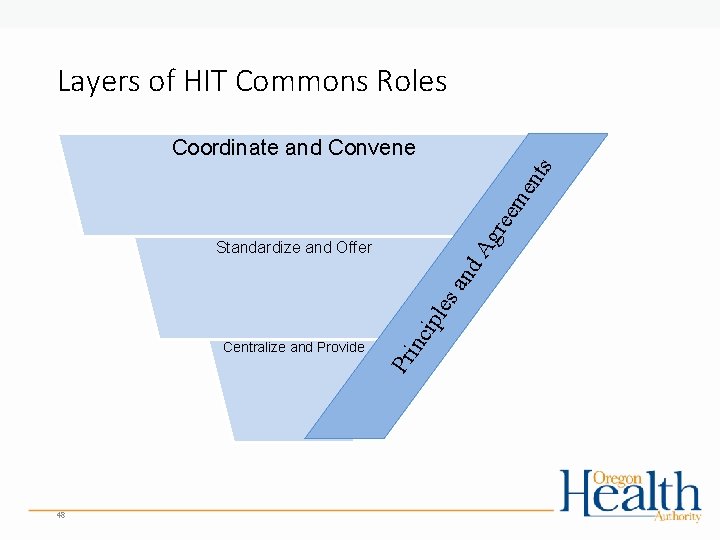
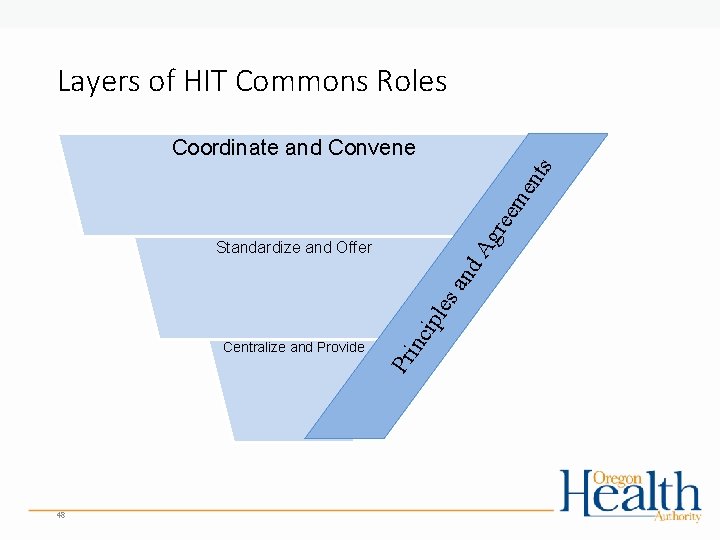
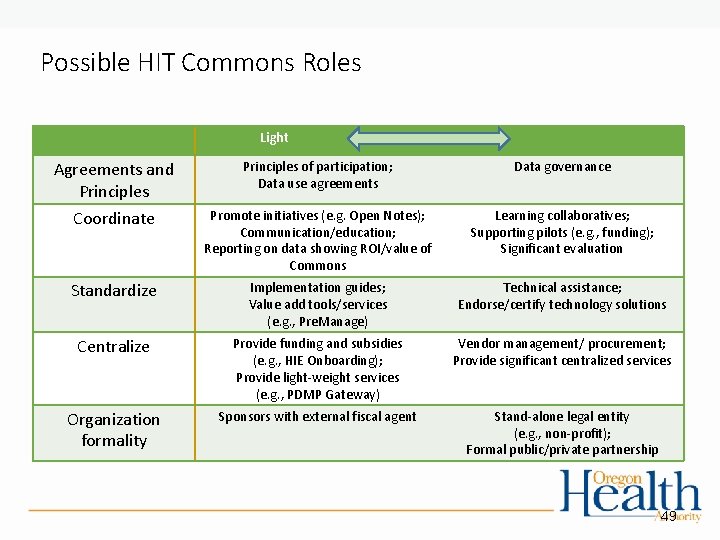
Layers of HIT Commons Roles Ag ree me n ts Coordinate and Convene Pr Centralize and Provide inc ipl es an d Standardize and Offer 48
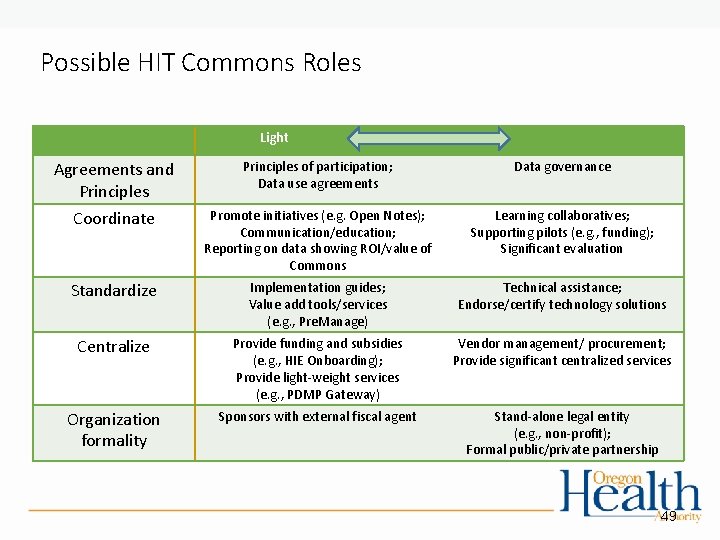
Possible HIT Commons Roles Light Robust Agreements and Principles Coordinate Principles of participation; Data use agreements Data governance Promote initiatives (e. g. Open Notes); Communication/education; Reporting on data showing ROI/value of Commons Learning collaboratives; Supporting pilots (e. g. , funding); Significant evaluation Standardize Implementation guides; Value add tools/services (e. g. , Pre. Manage) Technical assistance; Endorse/certify technology solutions Centralize Provide funding and subsidies (e. g. , HIE Onboarding); Provide light-weight services (e. g. , PDMP Gateway) Vendor management/ procurement; Provide significant centralized services Organization formality Sponsors with external fiscal agent Stand-alone legal entity (e. g. , non-profit); Formal public/private partnership 49

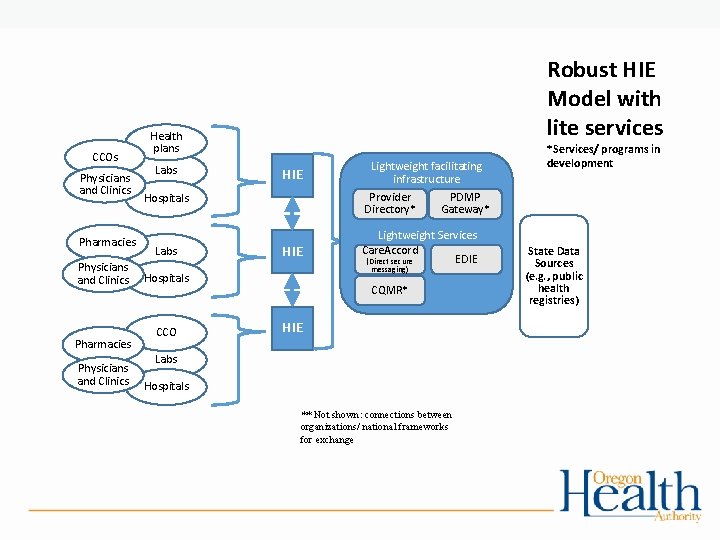
Example Problem to Solve Statewide HIE Network of Networks • Goal to have minimum core data available wherever Oregonians receive care or services across the state • Current environment: Basic movement of health information is improving but significant gaps and white spaces remain • Barriers to HIE include technology, organizational culture, trust • Ensuring HIE is meaningful and tools are used can be complex • “Raising all boats” to connect providers across the state can best be accomplished together • Shared governance can play a significant role
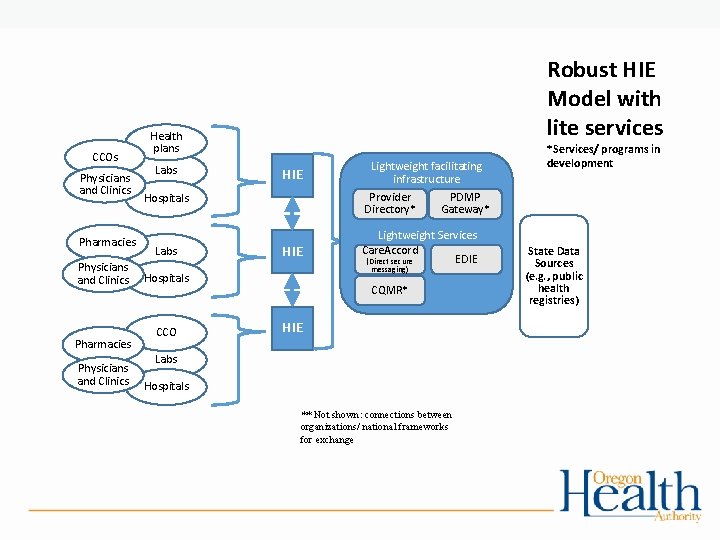
CCOs Physicians and Clinics Pharmacies Physicians and Clinics Robust HIE Model with lite services Health plans Labs HIE Provider Directory* Hospitals Labs HIE PDMP Gateway* Lightweight Services Care. Accord EDIE (Direct secure messaging) Hospitals CCO Lightweight facilitating infrastructure *Services/ programs in development CQMR* HIE Labs Hospitals ** Not shown: connections between organizations/ national frameworks for exchange State Data Sources (e. g. , public health registries)

Timeline • January – March: Initial Input and Research • • February 16 sensing session February 23 HIT Advisory Group meeting for CCO input Individual 1: 1 sensing sessions with additional stakeholders Research and reflection on other states’ models, successes, and challenges • Starting in April: Interim advisory group meets to help formulate business plan • April - June: Draft business plan input • OHLC, OHPB, HITOC, HITAG • Summer 2017: Final business plan released
Questions? 53

Close
Q & A/Close • For this meeting, what worked well? • What could we do better next time? • What questions do you have?
 Didd guidelines
Didd guidelines Hcsis
Hcsis Didd provider directory
Didd provider directory March march dabrowski
March march dabrowski Nasa astrophysics advisory committee
Nasa astrophysics advisory committee Aviation rulemaking advisory committee
Aviation rulemaking advisory committee Education without burden
Education without burden Trade union advisory committee
Trade union advisory committee Federal advisory committee on insurance
Federal advisory committee on insurance Pa safety committee certification
Pa safety committee certification Tcm technical committee meeting
Tcm technical committee meeting Bsa committee meeting agenda
Bsa committee meeting agenda Steering committee meeting agenda sample
Steering committee meeting agenda sample American epilepsy society annual meeting 2017
American epilepsy society annual meeting 2017 Job meeting bari 2017
Job meeting bari 2017 Joanne chien
Joanne chien Nrg oncology meeting 2017
Nrg oncology meeting 2017 Nrg oncology meeting 2016
Nrg oncology meeting 2016 Nrg oncology conference
Nrg oncology conference What is meeting and types of meeting
What is meeting and types of meeting Types of meeting
Types of meeting For todays meeting
For todays meeting Today meeting or today's meeting
Today meeting or today's meeting Active directory site topology
Active directory site topology Walsall community living directory
Walsall community living directory Nih enterprise directory
Nih enterprise directory Ibm tivoli directory integrator
Ibm tivoli directory integrator Jndi name
Jndi name Competency directory
Competency directory Usb root directory
Usb root directory Ad disaster recovery
Ad disaster recovery Active directory cleanup
Active directory cleanup Active directory alapok
Active directory alapok Ado net active directory
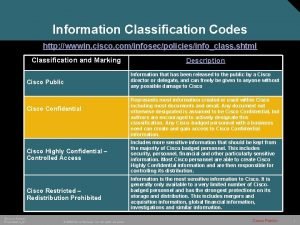
Ado net active directory Cisco data taxonomy categories
Cisco data taxonomy categories Manajemen file pada unix
Manajemen file pada unix Linux copy directory
Linux copy directory Pada sabtu
Pada sabtu Active directory fundamentals
Active directory fundamentals Advantages and disadvantages of active directory
Advantages and disadvantages of active directory Philippine national police organizational structure
Philippine national police organizational structure Active directory replication troubleshooting
Active directory replication troubleshooting What was directory
What was directory Ospital ng maynila emergency number
Ospital ng maynila emergency number Restic dry run
Restic dry run Unix directory tree
Unix directory tree Grouper active directory
Grouper active directory Napster directory
Napster directory Microsoft virtual academy active directory
Microsoft virtual academy active directory Advantages of two level directory
Advantages of two level directory Iowa nrcs directory
Iowa nrcs directory Brc global standards directory
Brc global standards directory Horizon nj health appeal form
Horizon nj health appeal form General graph directory
General graph directory Active directory two way trust
Active directory two way trust 389 directory
389 directory