Provider Adherence to Oral Chemotherapy Dose Adjustment Guidelines

- Slides: 21
Provider Adherence to Oral Chemotherapy Dose Adjustment Guidelines UT Clinical Safety & Effectiveness Conference San Antonio, TX October 27 -28, 2011 Amy Fowler, MD Alexis Kennedy, CPNP Naomi Winick, MD
The Team • Team Members • CS&E Participants • Amy Fowler, MD, Project Leader • Alexis Kennedy, CPNP, Project Champion • Team Members • • • Naomi Winick, MD, Physician Champion Gretchen Hirschey, RN, Nursing Champion Jessica Rajian, RN, EPIC Champion Christian Tellinghuisen, Database support All the pediatric hematology/oncology fellows • Facilitator - Pat Griffith, BS, MT, MBA
Childhood Acute Lymphoblastic Leukemia (ALL) • Most common malignancy of childhood – 50 -60 new cases annually in Dallas – About 150 children treated for ALL at any given time • Current survival rates vastly improved • Oral chemotherapy – – Important component of therapy 6 -mercaptopurine (6 MP) and methotrexate (MTX) Given daily, at home, for ~ 2 -3 years Dosed based on degree of bone marrow suppression • Published dosing guidelines for providers • Specific rules for when to hold doses or dose escalate • Target absolute neutrophil count (ANC): 500 – 1, 500/μL
Clinical importance of dosing guidelines • Degree of bone marrow suppression – Lower ANC Improved survival • Dose intensity of oral chemotherapy – Greater dose intensity Improved survival • Problem with excessive neutropenia (ANC <500) • Risk of serious infections increases • Results in held doses (chemo interruptions) • Decreases dose intensity due to breaks in therapy • Dose interruptions – Greater dose interruptions Inferior survival • Provider adherence impacts all of the above
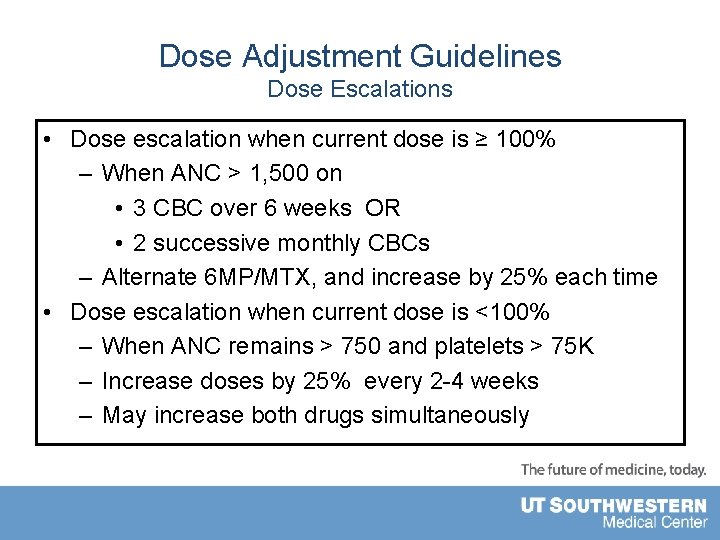
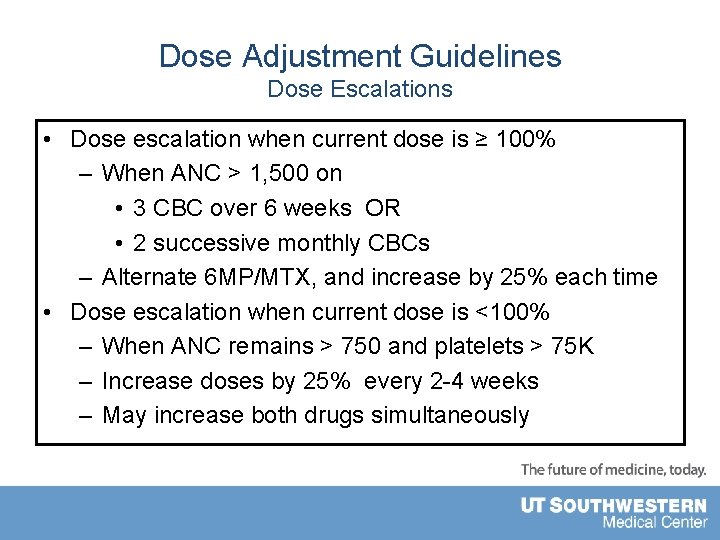
Dose Adjustment Guidelines Dose Escalations • Dose escalation when current dose is ≥ 100% – When ANC > 1, 500 on • 3 CBC over 6 weeks OR • 2 successive monthly CBCs – Alternate 6 MP/MTX, and increase by 25% each time • Dose escalation when current dose is <100% – When ANC remains > 750 and platelets > 75 K – Increase doses by 25% every 2 -4 weeks – May increase both drugs simultaneously
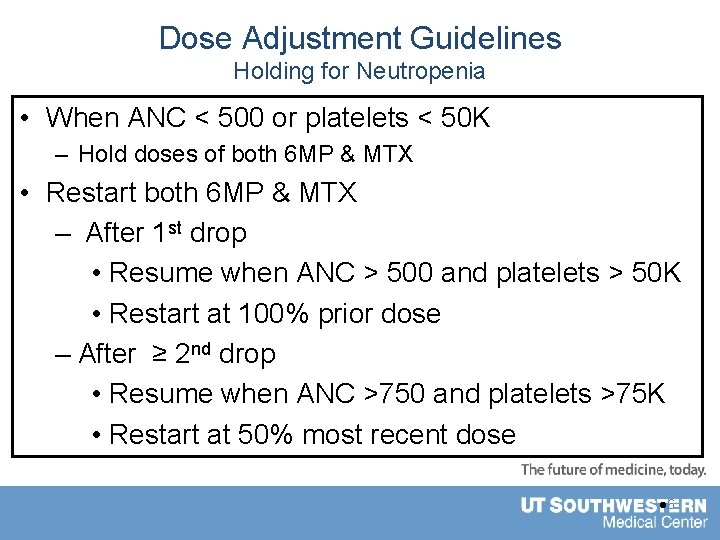
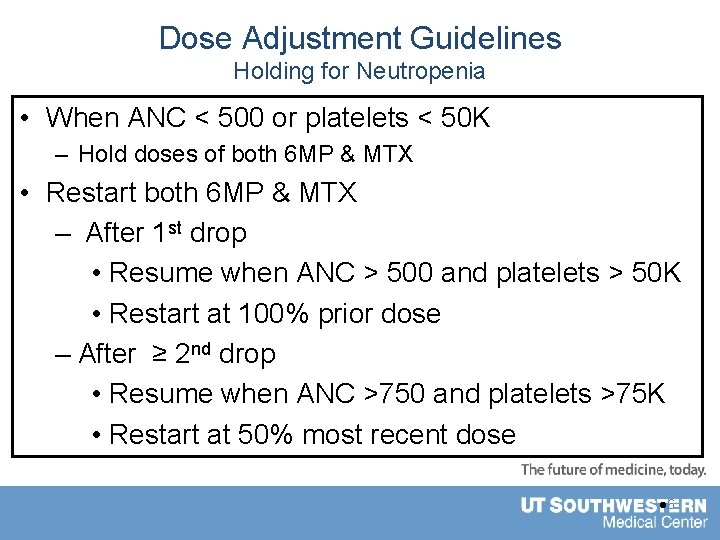
Dose Adjustment Guidelines Holding for Neutropenia • When ANC < 500 or platelets < 50 K – Hold doses of both 6 MP & MTX • Restart both 6 MP & MTX – After 1 st drop • Resume when ANC > 500 and platelets > 50 K • Restart at 100% prior dose – After ≥ 2 nd drop • Resume when ANC >750 and platelets >75 K • Restart at 50% most recent dose l 6
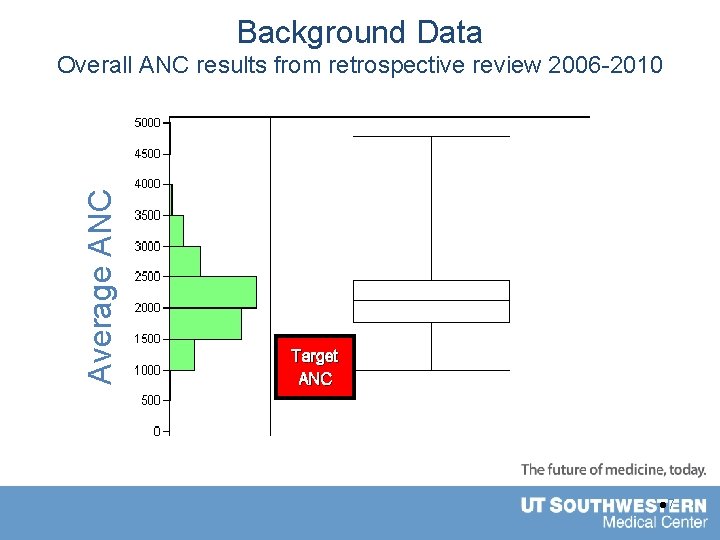
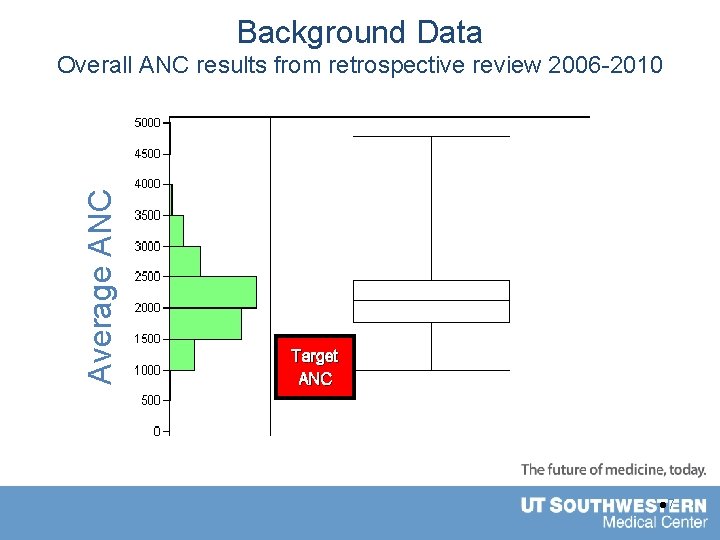
Background Data Average ANC Overall ANC results from retrospective review 2006 -2010 Target ANC l 7
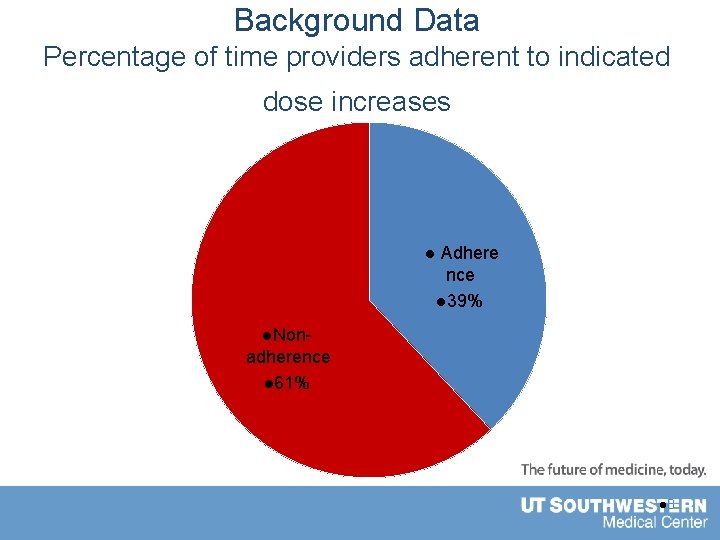
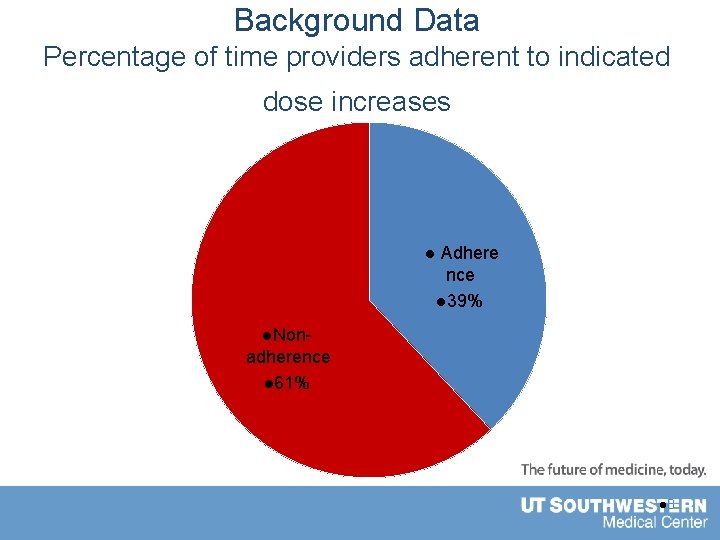
Background Data Percentage of time providers adherent to indicated dose increases l Adhere nce l 39% l. Non- adherence l 61% l 8
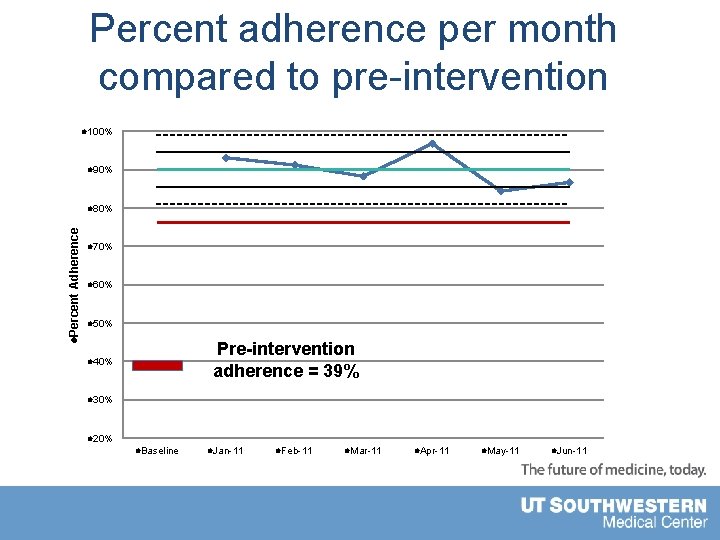
Aim Statement • Improve percentage of time that providers modify chemotherapy doses as indicated by protocol guidelines in children with ALL from 39% to over 75% – From January 1, 2011 to May 31, 2011.
Measures of Success • Provider adherence – Proportion of times dose escalation made when indicated by the guidelines. – Followed specific rules based on guidelines • Used consistent and trained set of providers to make decision on appropriateness of dose escalations • Goal to minimize variation in interpretation • Goal to improve from 39% to >75% l 10
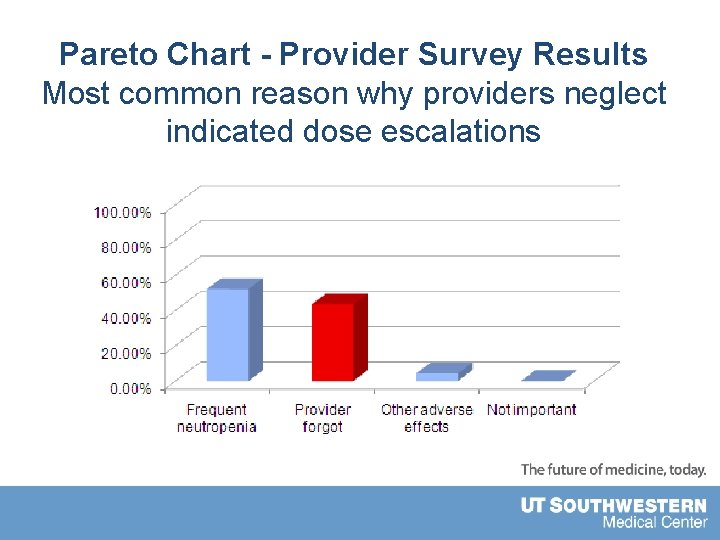
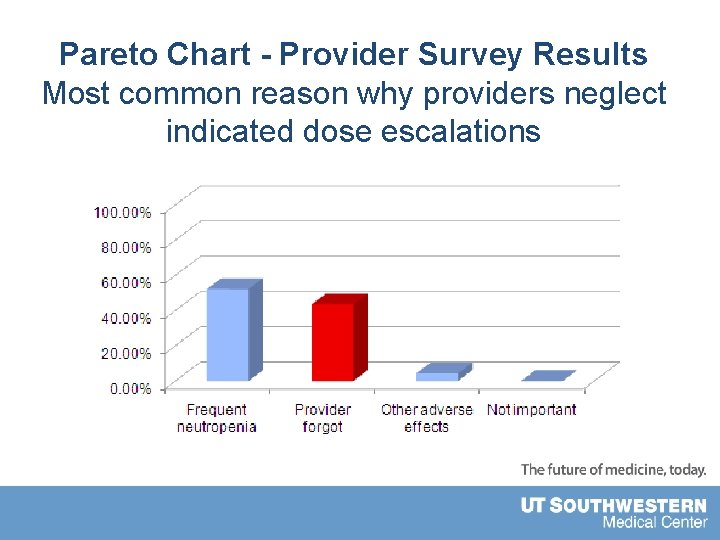
Pareto Chart - Provider Survey Results Most common reason why providers neglect indicated dose escalations
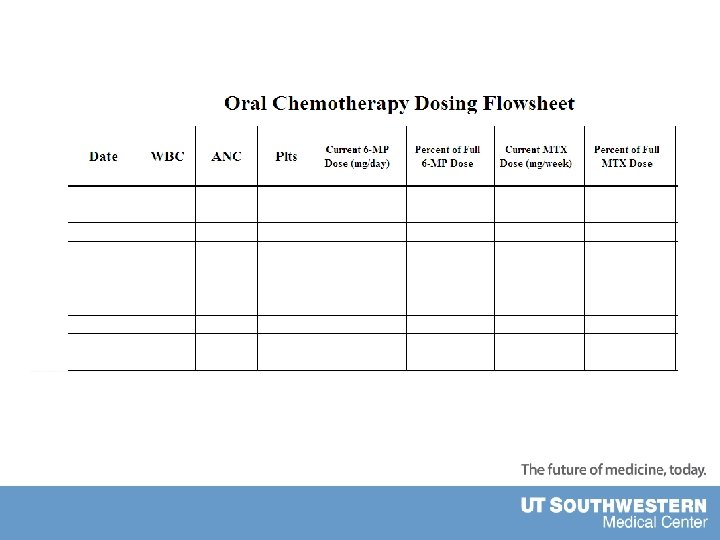
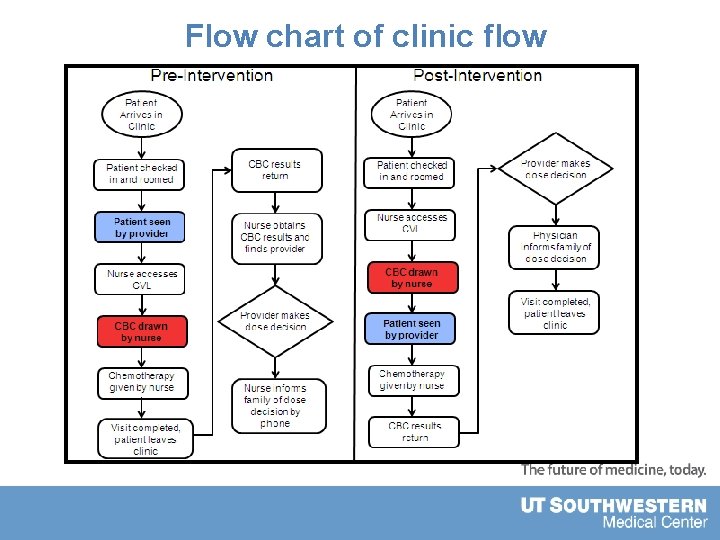
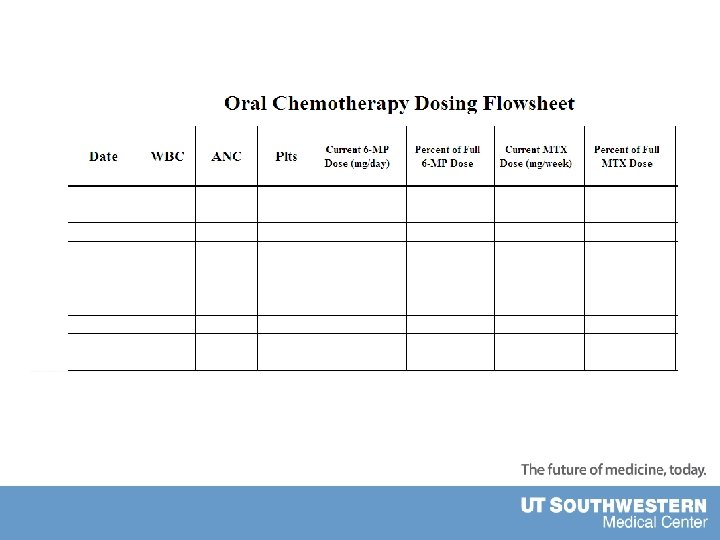
Targets for Intervention • Provider and nursing education – Awareness of the clinical importance – Review of guideline content • Created flow-sheet – Easy access to pertinent labs and dosing • Posters with guidelines placed in provider work areas • Change in process of clinic flow – Timing of lab draws – Results return prior to patient leaving clinic
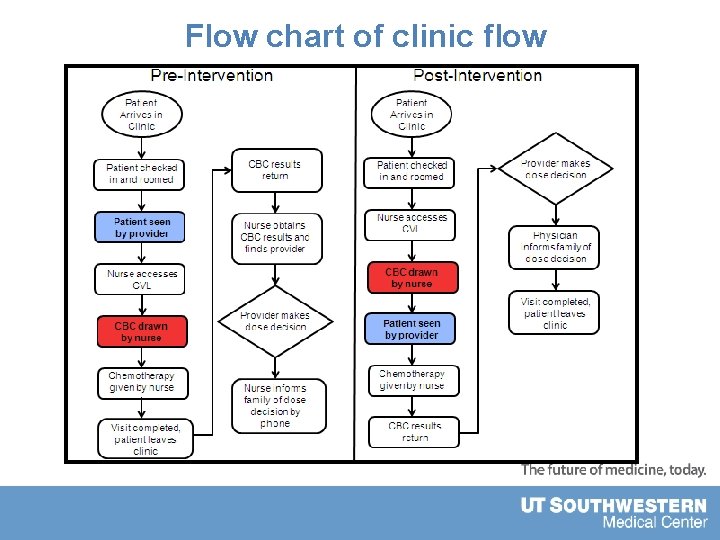
Flow chart of clinic flow
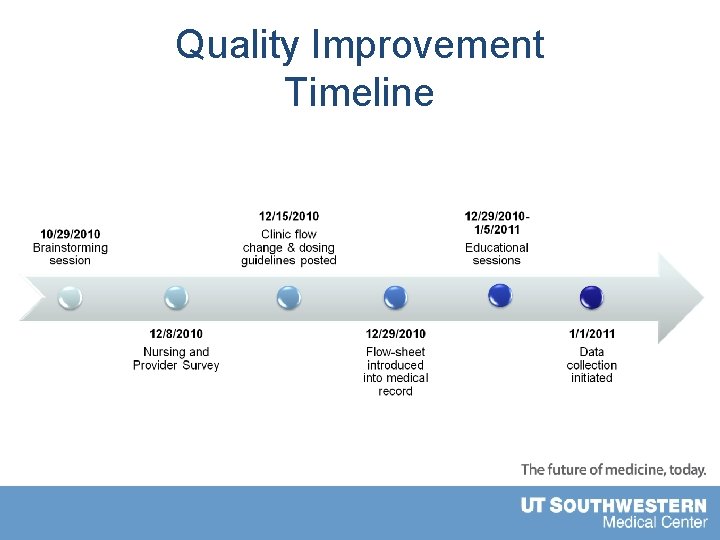
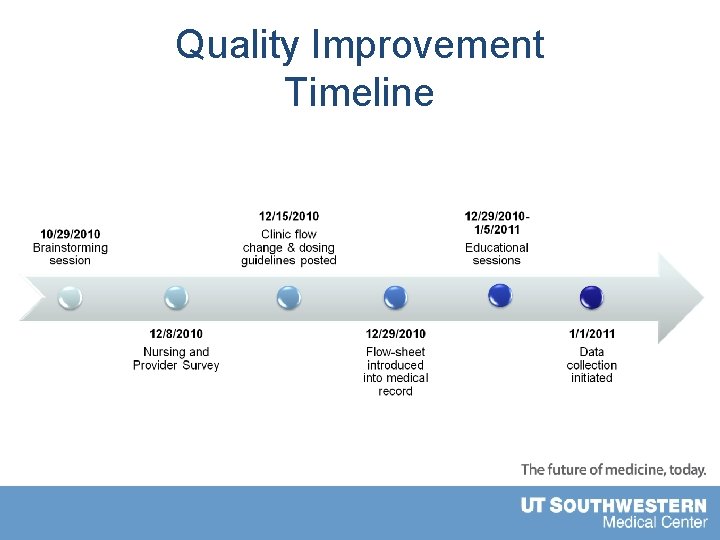
Quality Improvement Timeline
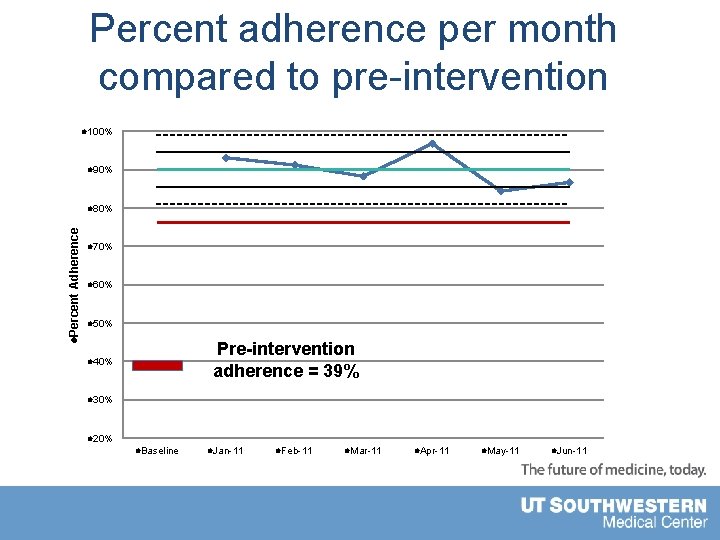
Percent adherence per month compared to pre-intervention l 100% l 90% l. Percent Adherence l 80% l 70% l 60% l 50% Pre-intervention adherence = 39% l 40% l 30% l 20% l. Baseline l. Jan-11 l. Feb-11 l. Mar-11 l. Apr-11 l. May-11 l. Jun-11
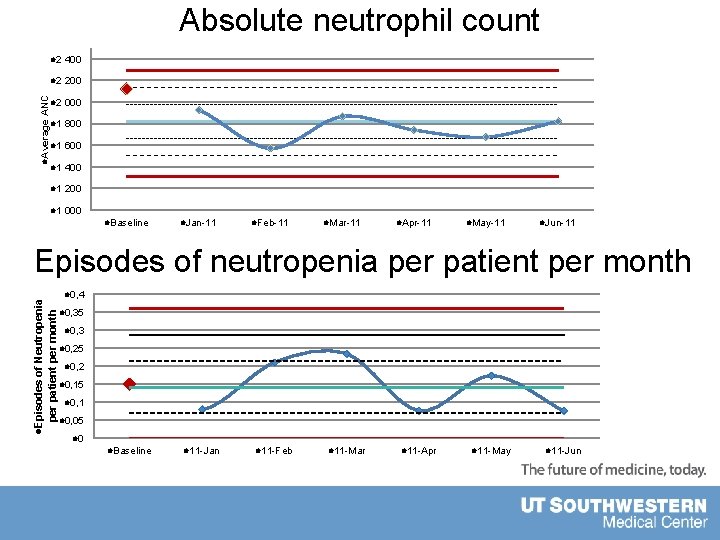
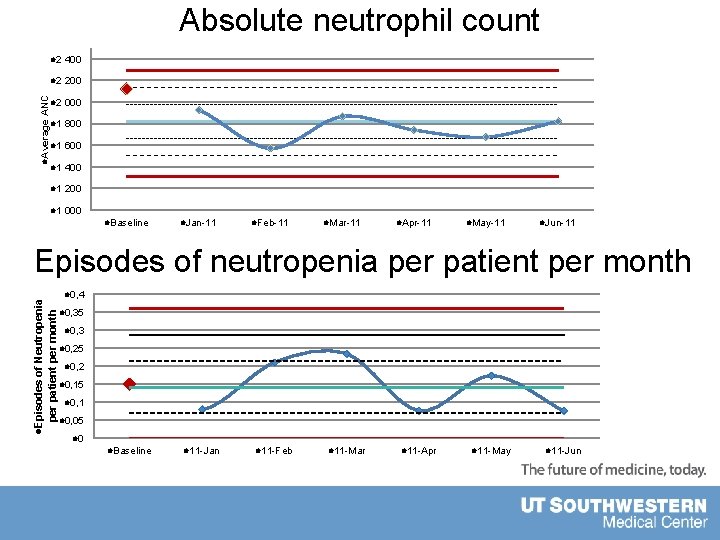
l 2 400 l 2 200 ANC l 2 000 l. Average Absolute neutrophil count l 1 800 l 1 600 l 1 400 l 1 200 l 1 000 l. Baseline l. Jan-11 l. Feb-11 l. Mar-11 l. Apr-11 l. May-11 l. Jun-11 l. Episodes of Neutropenia per patient per month Episodes of neutropenia per patient per month l 0, 4 l 0, 35 l 0, 3 l 0, 25 l 0, 2 l 0, 15 l 0, 1 l 0, 05 l 0 l. Baseline l 11 -Jan l 11 -Feb l 11 -Mar l 11 -Apr l 11 -May l 11 -Jun
Conclusions • Exceeded goal with 90% adherence • Increased bone marrow suppression (ANC) • No change in frequency of neutropenic episodes • May increase length of dose interruptions • Longer dose interruptions Theoretical risk of negative influence on survival rates • Must weigh risks and benefits of improved adherence • Universal buy-in • Nursing staff • Families • Administration • Providers (Mid-level and physician)
Challenges • Data collection – Very labor and time intensive – Complex spreadsheets – Clinical expertise needed for data evaluation • Commitment from providers “set in their ways” • Guidelines leaving room for interpretation • Difficult to put $$ value on results
Next Steps • Clinic to continue the interventions • Continued monitoring • Quarterly chart audits • Introduce into EMR system • Build reminders and flow sheets electronically • Large scale, multi-institution collaborative • Need to look at effect on survival rates • Publish results • Influence the Children’s Oncology Group, organization creating new versions of guidelines
