Protracted vacuum extraction and neonatal intracranial hemorrhage among

- Slides: 11
Protracted vacuum extraction and neonatal intracranial hemorrhage among infants born at term: a nationwide case-control study Katarina Åberg 1 | Mikael Norman 2| Karin Pettersson 3| Hans Järnbert-Pettersson 3| Cecilia Ekéus 1 1: Department of Womenʹs and Childrenʹs Health, Division of Reproductive Health, Karolinska Institutet, Stockholm, Sweden; 2: Department of Clinical Science, Intervention and Technology, Karolinska Institutet , Stockholm, Sweden; 3: Department of Clinical Science and Education, Södersjukhuset Hospital, Karolinska Institutet, Stockholm, Sweden ACTA Obstetricia et Gynecologica Scandinavica Journal Club April 2019 Edited by Francesco D’Antonio
Introduction Ø Intracranial hemorrhage (ICH) is a rare but potentially life-threatening complication among term newborns, associated with increased risk of long-term neurological disability. Ø The risk of ICH has been shown to increase after all operative deliveries, except for elective cesarean section. Ø However, these studies were all limited by lack of information about the indications for operative delivery. Ø An excess risk for ICH after vacuum extraction (VE) has been reported by some authors. In particular, case reports suggest that difficult and protracted extractions may cause ICH, although this has not been confirmed in larger studies. Ø The maximum duration, number of pulls or detachments allowed to safely deliver the infant are not known and guidelines rely mainly on clinical experience. Previous recommendations were a maximum of 3 pulls. In recent years this policy has changed to reduce maternal perineal injuries and more updated recommendations are a maximum of 3 pulls for the descent to the pelvic floor and 3 additional pulls for the outlet phase
Aim of the study To investigate the impact of protracted vacuum extraction on the risk for neonatal intracranial hemorrhage in term infants.
Material and Methods Ø Study design: Nationwide case-control study. Ø Inclusion criteria: all live-born infants, delivered by VE at term (≥ 37 gestational weeks). The cases were all infants from the source population who were diagnosed with neonatal ICH (182 cases). For each case, 3 VE-delivered controls without a diagnosis of ICH were included. Controls were matched for hospital and year of birth and were randomly selected from term infants born by VE at the same hospital within a year before the case (546 controls). Ø Primary outcome: Neonatal ICH, was defined according to the Swedish version of the International Classification of Diseases, 10 th revision (ICD-10) and included the following ICDcodes: P 10. 0 -10. 4, P 10. 8 -10. 9 (Intracranial laceration and hemorrhage due to birth injury) and P 52. 0 -52. 6, P 52. 8 -52. 9 (Intracranial non-traumatic hemorrhage of fetus and newborn). All diagnoses were validated in the records. If ICH could not be confirmed, the case and its 3 matched controls, were excluded. Ø Main exposure: protracted VE defined as extractions exceeding safety recommendations for VE deliveries, and included: vacuum duration > 15 min, > 6 pulls or > 2 cup detachments. Vacuum duration, recorded in minutes, was defined as duration from vacuum application until delivery or cup removal and was categorized into ≤ 15 min and > 15 min. Number of pulls was categorized into ≤ 6 and > 6. Cup detachments, defined as involuntary detachment of the cup, were categorized into ≤ 2 and > 2.

Material and Methods Ø Statistical analysis: Chi-squared test with an α-level set to 0. 05 was used to test differences in proportions between categories. To study the association between protracted extraction and ICH, conditional logistic regression analysis by Cox regression was used. Thereafter, possible confounders (maternal height, parity, induction of labor, maternal fever, indication for VE, station before VE and birthweight) were added to the model and adjusted ORs were estimated.
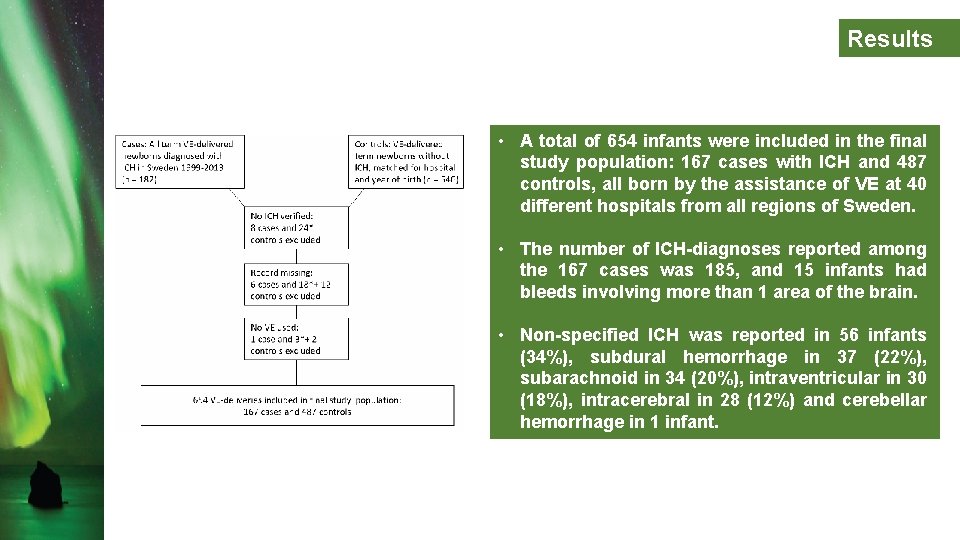
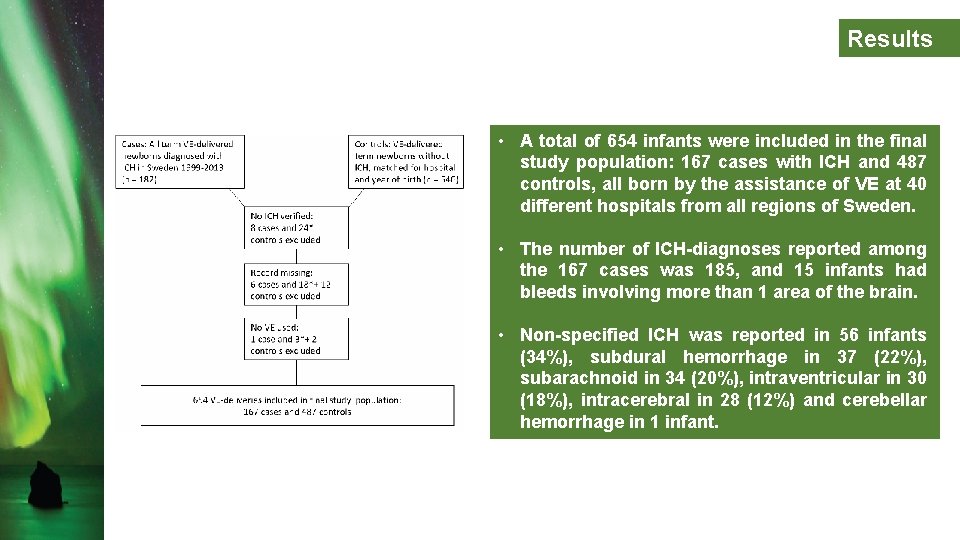
Results • A total of 654 infants were included in the final study population: 167 cases with ICH and 487 controls, all born by the assistance of VE at 40 different hospitals from all regions of Sweden. • The number of ICH-diagnoses reported among the 167 cases was 185, and 15 infants had bleeds involving more than 1 area of the brain. • Non-specified ICH was reported in 56 infants (34%), subdural hemorrhage in 37 (22%), subarachnoid in 34 (20%), intraventricular in 30 (18%), intracerebral in 28 (12%) and cerebellar hemorrhage in 1 infant.
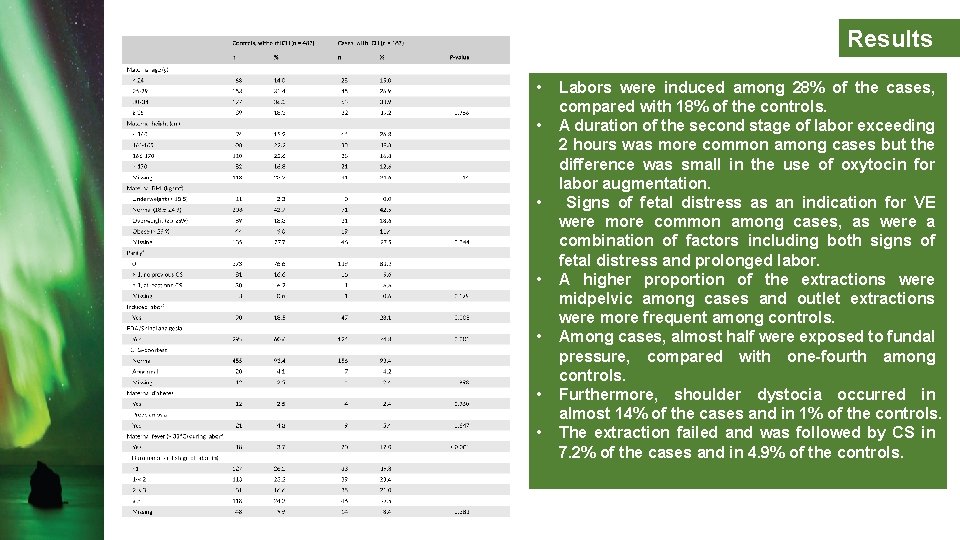
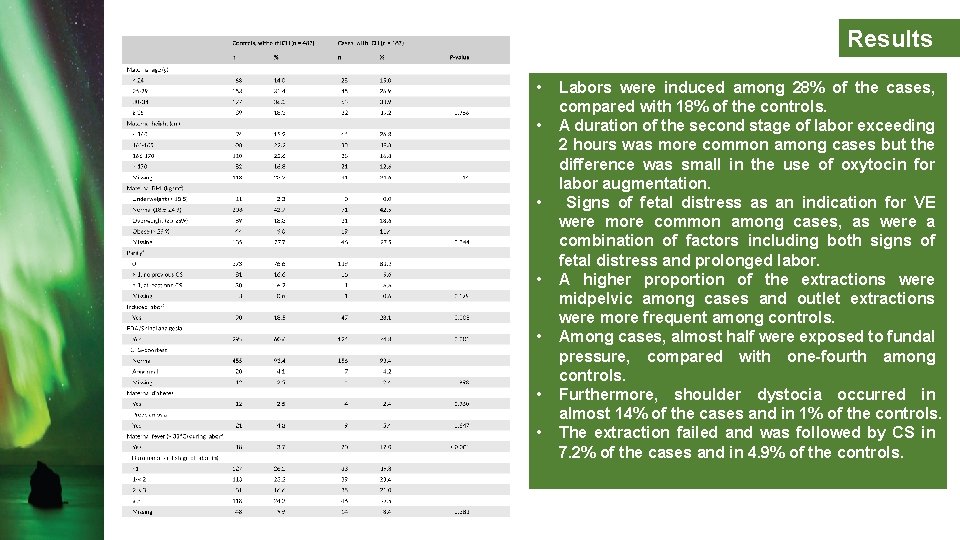
Results • • Labors were induced among 28% of the cases, compared with 18% of the controls. A duration of the second stage of labor exceeding 2 hours was more common among cases but the difference was small in the use of oxytocin for labor augmentation. Signs of fetal distress as an indication for VE were more common among cases, as were a combination of factors including both signs of fetal distress and prolonged labor. A higher proportion of the extractions were midpelvic among cases and outlet extractions were more frequent among controls. Among cases, almost half were exposed to fundal pressure, compared with one-fourth among controls. Furthermore, shoulder dystocia occurred in almost 14% of the cases and in 1% of the controls. The extraction failed and was followed by CS in 7. 2% of the cases and in 4. 9% of the controls.
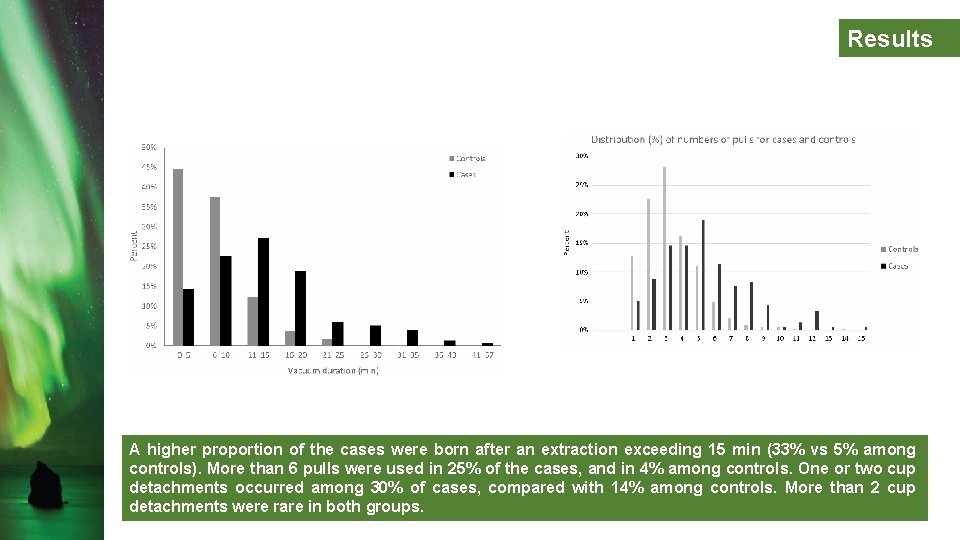
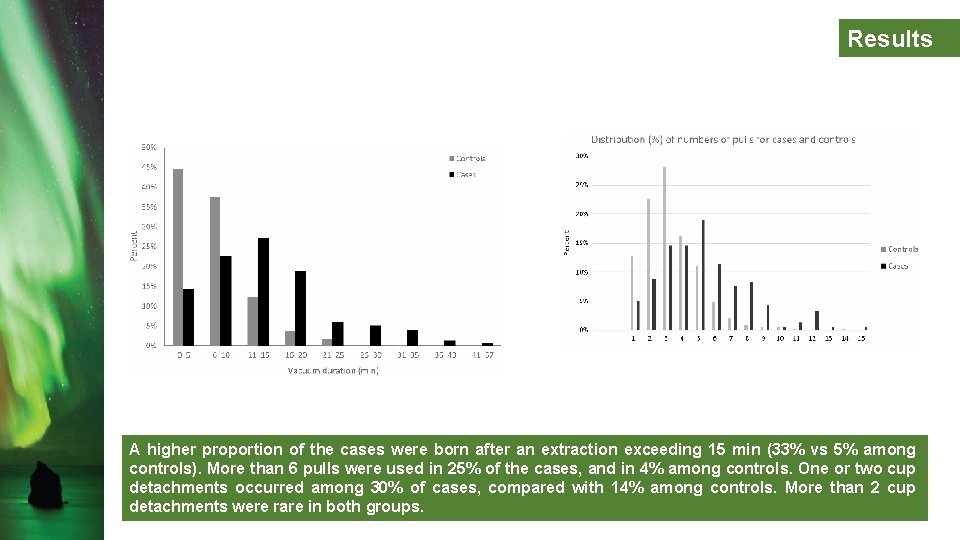
Results A higher proportion of the cases were born after an extraction exceeding 15 min (33% vs 5% among controls). More than 6 pulls were used in 25% of the cases, and in 4% among controls. One or two cup detachments occurred among 30% of cases, compared with 14% among controls. More than 2 cup detachments were rare in both groups.
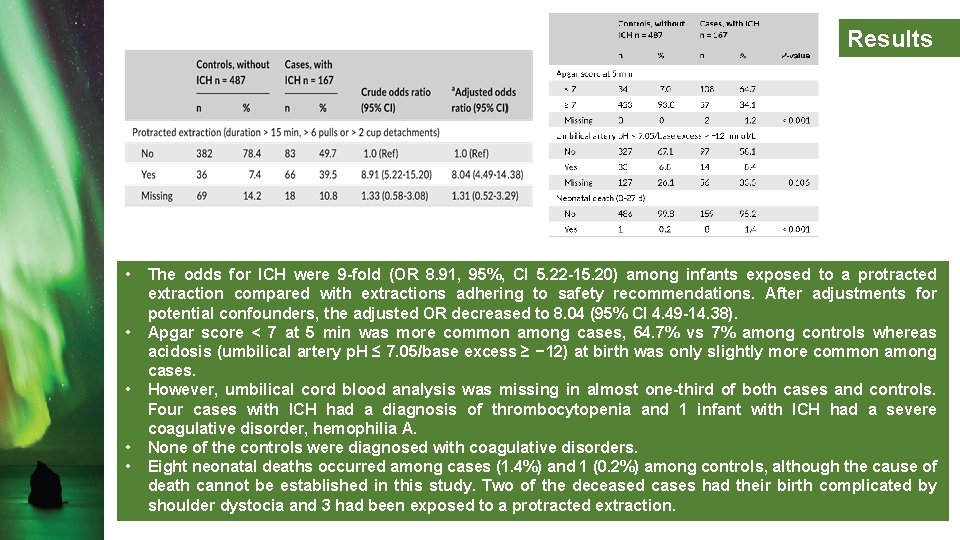
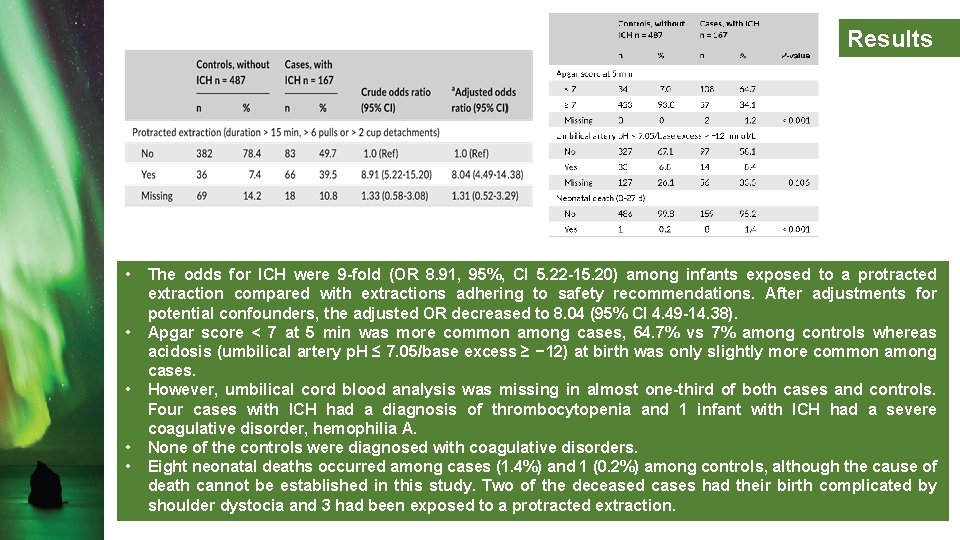
Results • • • The odds for ICH were 9 -fold (OR 8. 91, 95%, CI 5. 22 -15. 20) among infants exposed to a protracted extraction compared with extractions adhering to safety recommendations. After adjustments for potential confounders, the adjusted OR decreased to 8. 04 (95% CI 4. 49 -14. 38). Apgar score < 7 at 5 min was more common among cases, 64. 7% vs 7% among controls whereas acidosis (umbilical artery p. H ≤ 7. 05/base excess ≥ − 12) at birth was only slightly more common among cases. However, umbilical cord blood analysis was missing in almost one-third of both cases and controls. Four cases with ICH had a diagnosis of thrombocytopenia and 1 infant with ICH had a severe coagulative disorder, hemophilia A. None of the controls were diagnosed with coagulative disorders. Eight neonatal deaths occurred among cases (1. 4%) and 1 (0. 2%) among controls, although the cause of death cannot be established in this study. Two of the deceased cases had their birth complicated by shoulder dystocia and 3 had been exposed to a protracted extraction.
Limitations Ø Retrospective design. Ø Some delivery information (urgency to deliver, traction force and technique) were not reported. Ø Authors did not have access to the complete neonatal records and were unable to assess the exact type of hemorrhage for 56 cases with a diagnostic code for nonspecified ICH. Ø Furthermore, there was a large proportion of missing values for some variables, due to incomplete records. Unfortunately, information was missing also for the exposure to protracted extraction for 10% of the cases and 14% of the controls. For most variables the proportion of missing values was equal between cases and controls. Ø t. The diagnostic procedure for suspected ICH was not standardized and there have been changes in the diagnostic management during the study period.
Conclusion The strong association between protracted extraction and intracranial hemorrhage suggests that adherence to safety recommendations may reduce the risk for intracranial hemorrhage in infants delivered by vacuum extraction. However, safe limits for vacuum duration and number of pulls are still unknown and intracranial hemorrhage may occur even when performed in accordance with safety recommendations.