Prostate Cancer Screening in the PostUSPSTF Era Alon




- Slides: 75
Prostate Cancer Screening in the Post-USPSTF Era Alon Z. Weizer, MD, MS Associate Professor of Urology Associate Chair, Surgical Services, Department of Urology, University of Michigan
Disclosures • Summus (e. Consult Platform): Advisory Board
Outline • Case presentation • US Preventative Services Task Force Recommendations as a Wake-Up Call • Goals of Cancer Screening • PSA and Prostate Cancer Basics • Impact of USPSTF on Screening • Improvements to Screening Process/Recommendations
Learning Objectives • Understand the rationale behind prostate cancer screening • Understand the implications of USPSTF recommendations on screening • Appreciate current recommendations and options to improve screening • Learn a proposed algorithm for appropriate screening for prostate cancer
Case Presentation • 54 year old Caucasian man presents to your office for annual health maintenance – On review of systems, he reports nocturia x 3 • Past medical history: hypertension controlled on lisinopril, mild obesity (BMI 31) • Past surgical history: right shoulder surgery, appendectomy as a child • Social history: machinist, married, 2 kids in college, quit smoking 10 years ago, minimal alcohol use • Medications: lisinopril, ibuprofen as needed • Allergies: none
Case Presentation • Physical examination: prostate 50 grams, no nodules but left lobe is larger than the right • Urinalysis, CBC, basic metabolic panel: normal • Next steps…
United States Preventative Services Task Force Recommendations • US Preventative Services Task Force recommendations: – 2008: Against PSA screening for men >75 years – October 2011: Draft recommendations against screening in all asymptomatic men – May 2012: Final recommendations of Grade D for PSA screening in all asymptomatic men – Why: Harms of Screening Outweigh the Benefits
What was the USPSTF’s Evidence? • Screening trials show increased diagnosis without improved overall or Ca. P-specific mortality • Treatment significantly impacts a man’s QOL – We have over-treated prostate cancer and likely still do today in several venues – The PCa screening trials were completed prior to AS – recent data: up to 50% of men diagnosed with localized prostate cancer go on AS – As RALP techniques mature, functional outcomes will continue to improve • Politically motivated? – Treatment costs $11 billion per year
American Urologic Association Early Detection of Prostate Cancer 2013 Guidelines • • No PSA screening in men under 40 No routine screening of men 40 -54 – Consider family history and African American race • Men 55 -69 have the greatest benefit from screening – – Shared decision making based on patients values and preferences Can increase screening interval to every 2 years • No routine screening for men 70+ or any man with <1015 year life expectancy – Consider population baseline age-adjusted life expectancy and adjust according to patient comorbidities
American Cancer Society Guidelines for Prostate Cancer Early Detection • Main emphasis: discuss the risks and uncertainties of screening to promote an informed decision: – Chance that cancer is diagnosed – We don’t know which low-risk cancers progress and pose a threat to a patient’s health – Diagnosis could compel the patient to undergo treatment that could ultimately be unnecessary – Treatments come with significant risks to quality of life (e. g. urinary incontinence, urinary and bowel symptoms, worsening erectile function)
Who’s Right When it Comes to Screening? • Principles of Screening: – Disease should have a high incidence √ – Biological behavior and natural history of the disease should be known √ – Test should have high sensitivity, specificity, and positive predictive value ? – Test should be rapid, inexpensive, noninvasive, and acceptable to patients √ – Acceptable and efficacious method of treatment must exist for patients diagnosed with disease √ – Screening should lower the disease-specific morbidity and increase survival ?
Examining the Evidence • Understanding PSA • Prostate Cancer Incidence and Mortality over time • Randomized Controlled Trials of PSA Screening
PSA Facts • Discovered in 1970 • Most widely used oncologic biomarker • 3/4 men over 50 have had a PSA • Member of the human kallikrein family of glycoproteins
PSA Facts • • Produced by the glandular epithelium of the prostate Trace amounts in salivary, pancreatic and breast tissue Found in semen, urine and blood Serine protease that liquefies semen to improve sperm mobility • Found in 3 forms in serum: – – – Bound to α-1 -Antichymotrypsin Bound to α-2 -Macroglobulin Free PSA
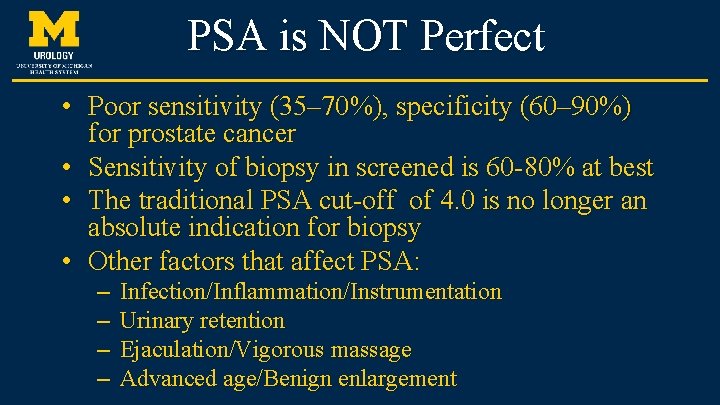
PSA is NOT Perfect • Poor sensitivity (35– 70%), specificity (60– 90%) for prostate cancer • Sensitivity of biopsy in screened is 60 -80% at best • The traditional PSA cut-off of 4. 0 is no longer an absolute indication for biopsy • Other factors that affect PSA: – – Infection/Inflammation/Instrumentation Urinary retention Ejaculation/Vigorous massage Advanced age/Benign enlargement
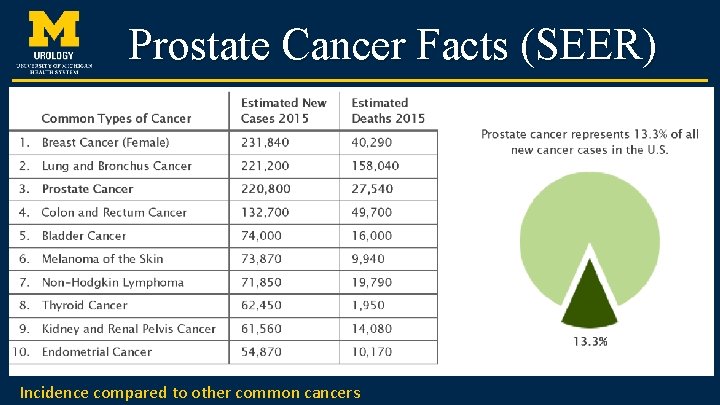
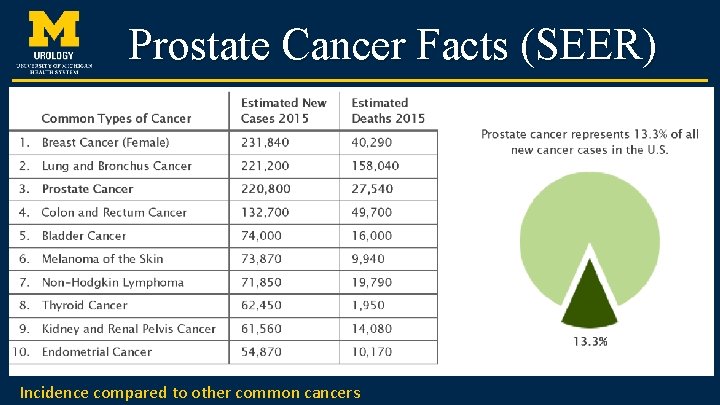
Prostate Cancer Facts (SEER) Incidence compared to other common cancers
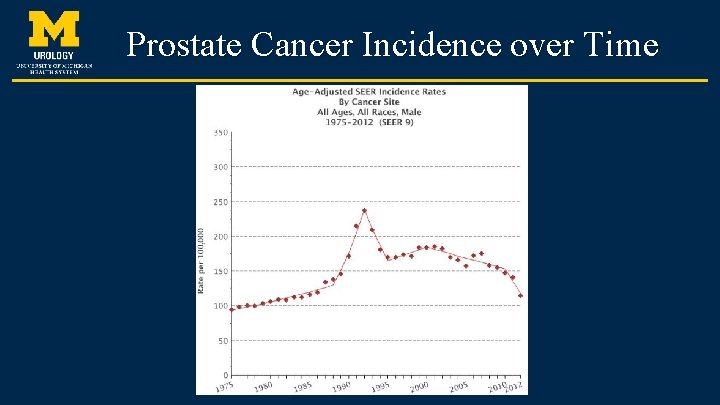
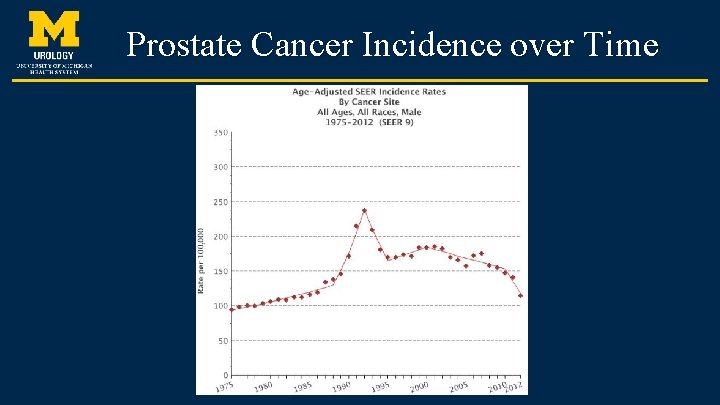
Prostate Cancer Incidence over Time
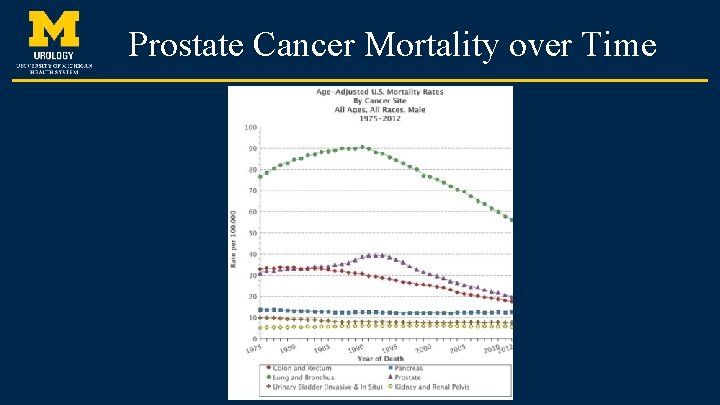
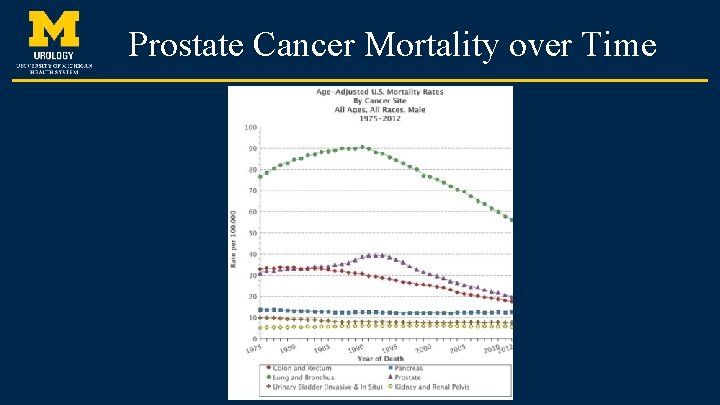
Prostate Cancer Mortality over Time
The screening studies • European Randomized Study of Screening for Prostate Cancer (Europe) • Goteborg Study (Sweden) • Prostate, Lung, Colon and Ovarian Cancer Screening trial (U. S. )

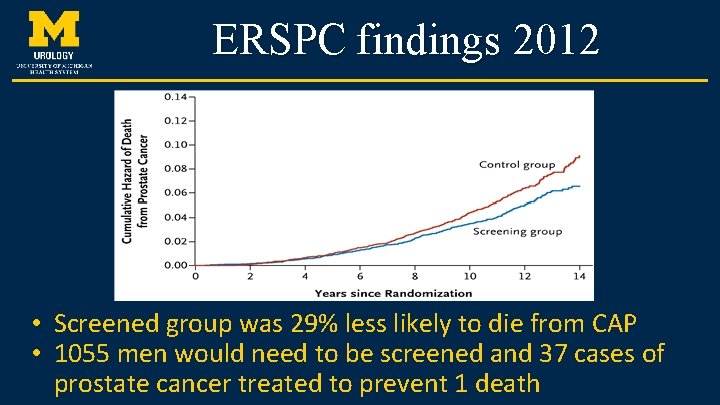
ERSPC: “The European study” • Random assignment of men between 50 and 74 in 7 European countries – 83, 000 in the screened group; 99, 000 in the control – PSA on average once every 4 years in screened cohort • During the median follow up of 11 years, PCa diagnosed in 9. 6% of the screened group and 6. 0% of controls Schröder FH, NEJM 2012
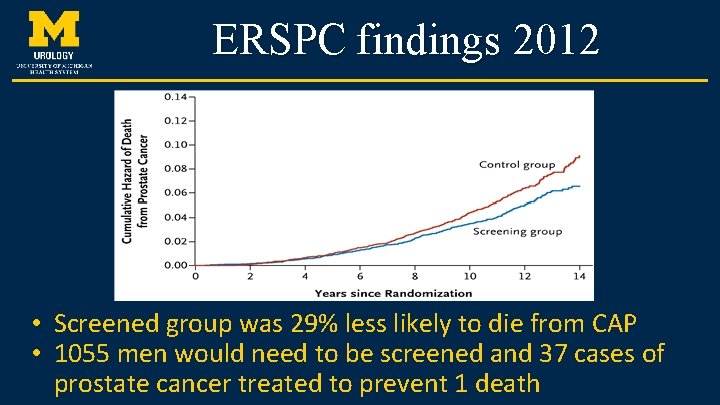
ERSPC findings 2012 • Screened group was 29% less likely to die from CAP • 1055 men would need to be screened and 37 cases of prostate cancer treated to prevent 1 death
Issues with this Study • • Positive PSA defined as 3. 0 ng/ml in most centers 6 -core biopsy used: prostate cancer diagnosis is up to 20% higher with an extended biopsy scheme (10 -18 cores) • Localized prostate cancer more common in the screened group A definite benefit of avoiding metastatic disease
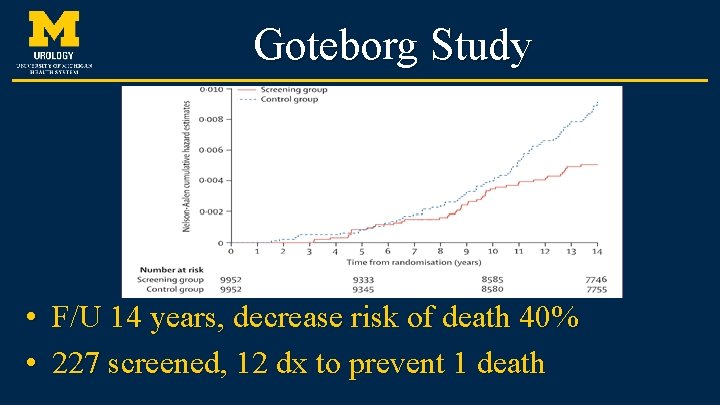
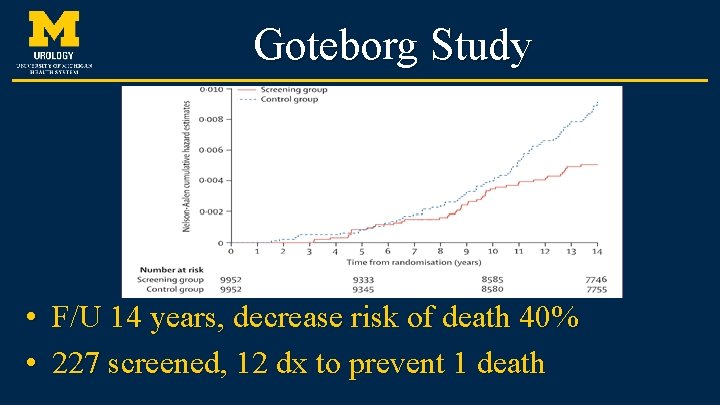
Goteborg Study • F/U 14 years, decrease risk of death 40% • 227 screened, 12 dx to prevent 1 death
PLCO: “The US trial” • 38, 000 men each randomly assigned to annual screening or “usual care” – Compliance rates for PSA and DRE were 85% and 86%, respectively – Usual care included up to 52% getting annual PSA and 46% getting yearly DRE – Follow up was for 7 to 10 years Andriole GL, NEJM 2009; 360: 1310 -1319
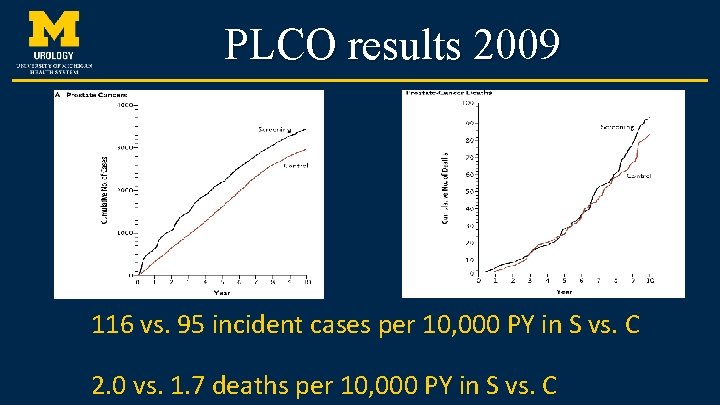
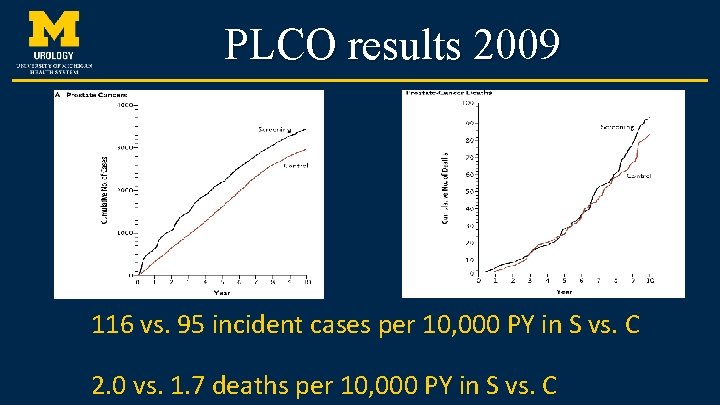
PLCO results 2009 116 vs. 95 incident cases per 10, 000 PY in S vs. C 2. 0 vs. 1. 7 deaths per 10, 000 PY in S vs. C
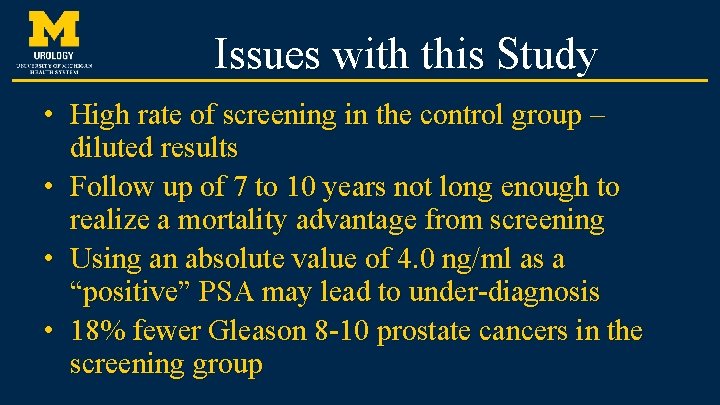
Issues with this Study • High rate of screening in the control group – diluted results • Follow up of 7 to 10 years not long enough to realize a mortality advantage from screening • Using an absolute value of 4. 0 ng/ml as a “positive” PSA may lead to under-diagnosis • 18% fewer Gleason 8 -10 prostate cancers in the screening group
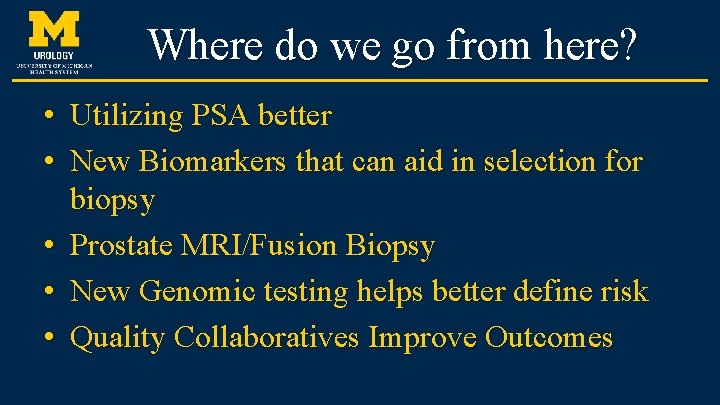
Where do we go from here? • Utilizing PSA better • New Biomarkers that can aid in selection for biopsy • Prostate MRI/Fusion Biopsy • New Genomic testing helps better define risk • Quality Collaboratives Improve Outcomes
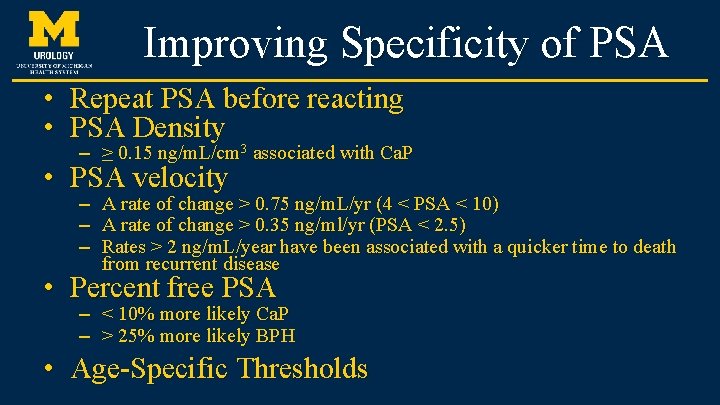
Improving Specificity of PSA • Repeat PSA before reacting • PSA Density – ≥ 0. 15 ng/m. L/cm 3 associated with Ca. P • PSA velocity – A rate of change > 0. 75 ng/m. L/yr (4 < PSA < 10) – A rate of change > 0. 35 ng/ml/yr (PSA < 2. 5) – Rates > 2 ng/m. L/year have been associated with a quicker time to death from recurrent disease • Percent free PSA – < 10% more likely Ca. P – > 25% more likely BPH • Age-Specific Thresholds
Biomarkers
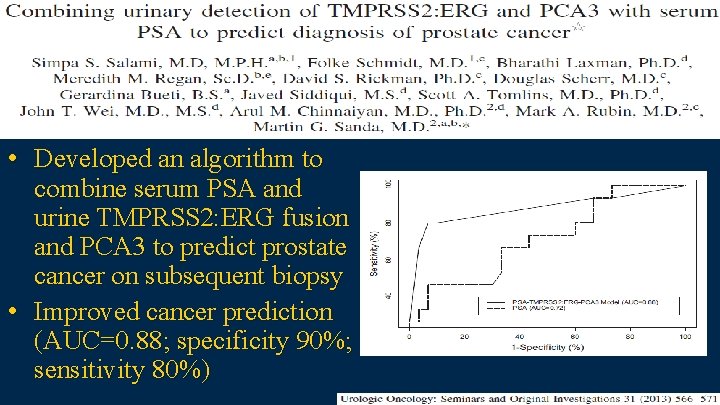
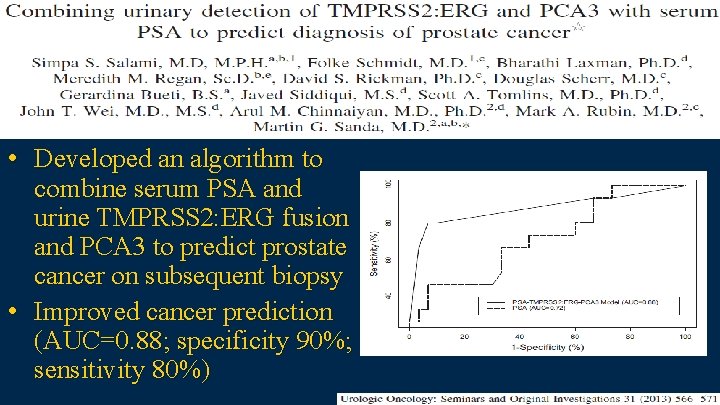
• Developed an algorithm to combine serum PSA and urine TMPRSS 2: ERG fusion and PCA 3 to predict prostate cancer on subsequent biopsy • Improved cancer prediction (AUC=0. 88; specificity 90%; sensitivity 80%)
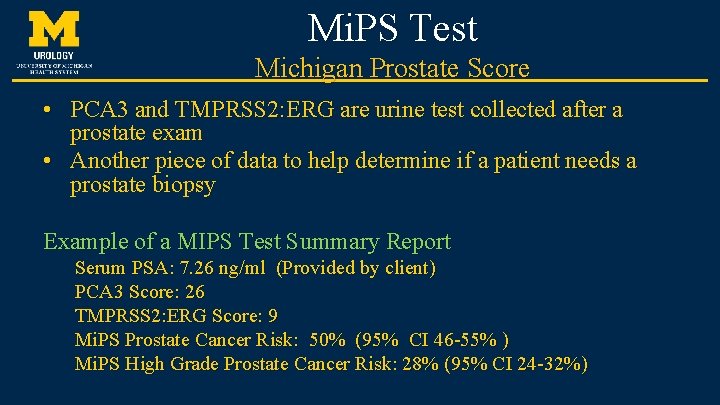
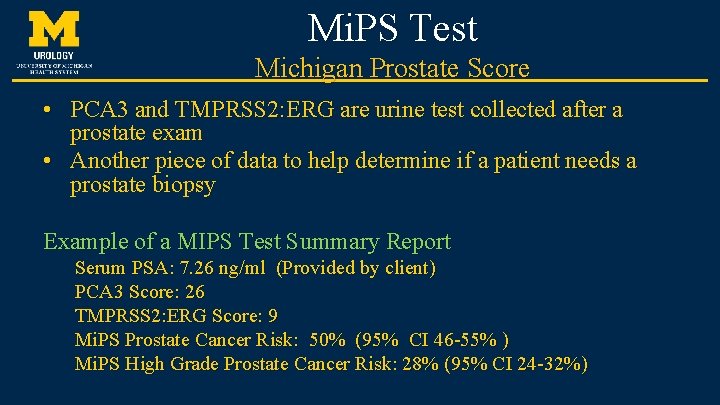
Mi. PS Test Michigan Prostate Score • PCA 3 and TMPRSS 2: ERG are urine test collected after a prostate exam • Another piece of data to help determine if a patient needs a prostate biopsy Example of a MIPS Test Summary Report Serum PSA: 7. 26 ng/ml (Provided by client) PCA 3 Score: 26 TMPRSS 2: ERG Score: 9 Mi. PS Prostate Cancer Risk: 50% (95% CI 46 -55% ) Mi. PS High Grade Prostate Cancer Risk: 28% (95% CI 24 -32%)
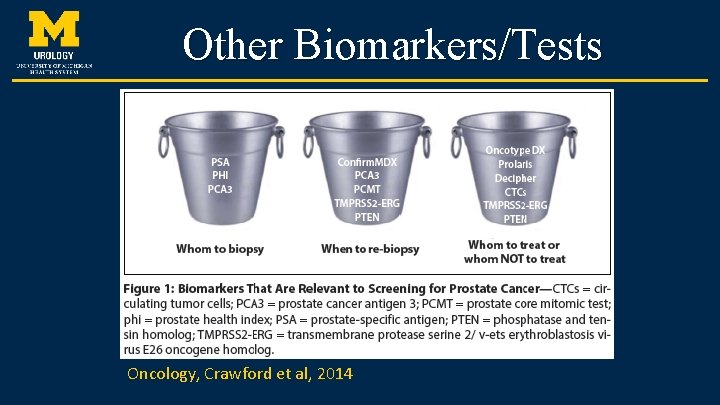
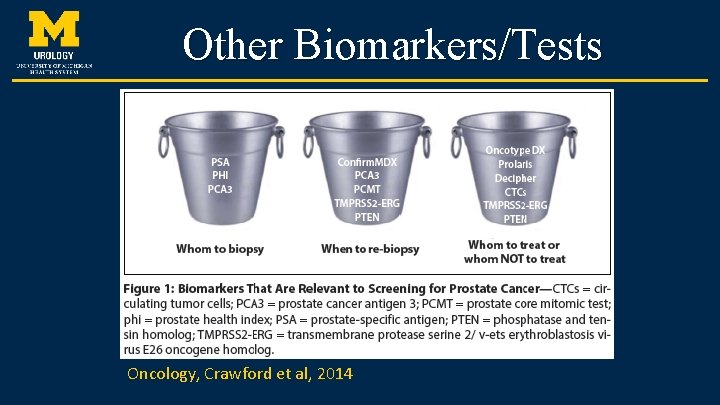
Other Biomarkers/Tests Oncology, Crawford et al, 2014
Imaging
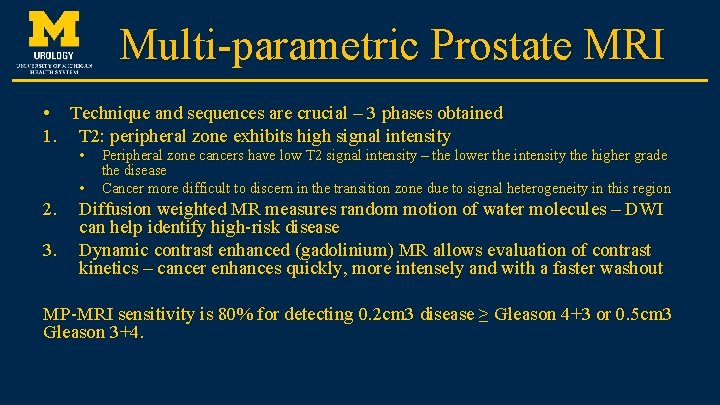
Multi-parametric Prostate MRI • Technique and sequences are crucial – 3 phases obtained 1. T 2: peripheral zone exhibits high signal intensity • • 2. 3. Peripheral zone cancers have low T 2 signal intensity – the lower the intensity the higher grade the disease Cancer more difficult to discern in the transition zone due to signal heterogeneity in this region Diffusion weighted MR measures random motion of water molecules – DWI can help identify high-risk disease Dynamic contrast enhanced (gadolinium) MR allows evaluation of contrast kinetics – cancer enhances quickly, more intensely and with a faster washout MP-MRI sensitivity is 80% for detecting 0. 2 cm 3 disease ≥ Gleason 4+3 or 0. 5 cm 3 Gleason 3+4.
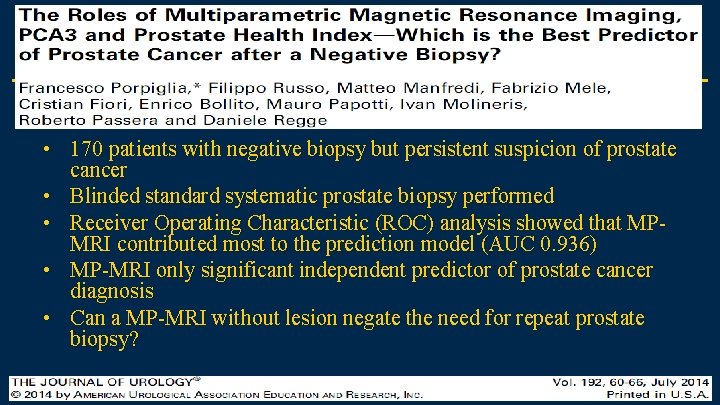
• 170 patients with negative biopsy but persistent suspicion of prostate cancer • Blinded standard systematic prostate biopsy performed • Receiver Operating Characteristic (ROC) analysis showed that MPMRI contributed most to the prediction model (AUC 0. 936) • MP-MRI only significant independent predictor of prostate cancer diagnosis • Can a MP-MRI without lesion negate the need for repeat prostate biopsy?
Prostate Biopsy
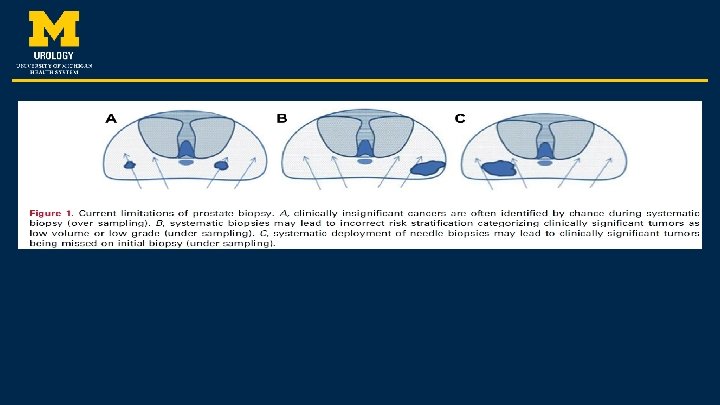
Prostate Biopsy • > 1. 2 million prostate biopsies are performed yearly in the US • Elevated PSA most frequently triggers biopsy • 30% of men referred for biopsy are diagnosed with prostate cancer • Relies on random sampling

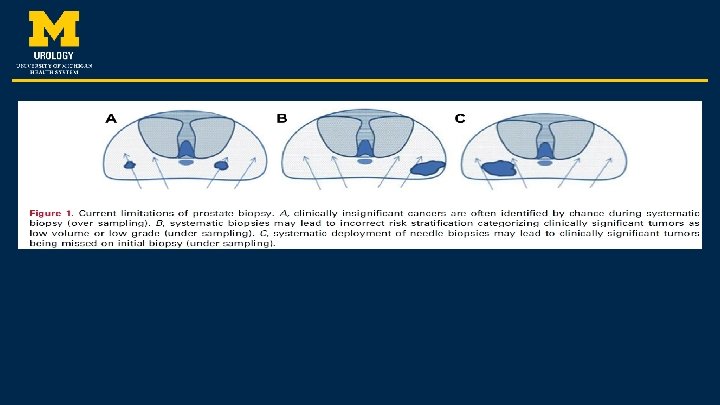
Shortcomings of Standard Systematic Prostate Biopsy • • • False-negative rate Incorrect risk stratification (up to 45%) Detection of clinically insignificant disease Need for repeat biopsy Disease overtreatment Increasing the core number (saturation or repeat biopsy) does not significantly reduce the risk of under sampling and incorrect risk stratification More biopsy episodes increases the risk of detecting indolent cancers Goal: Detect high-grade disease while avoiding low risk disease
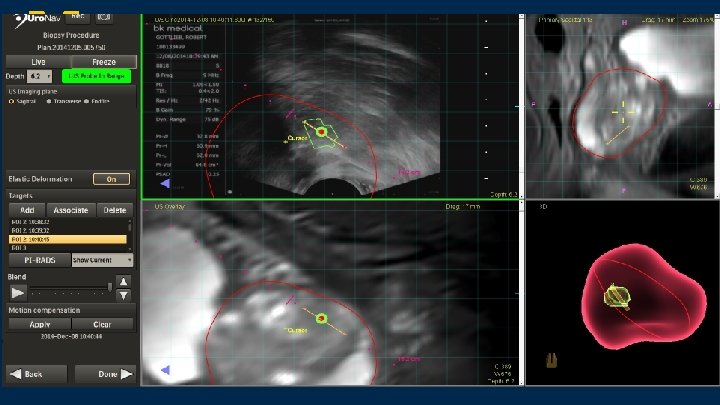
Types of MRI-Guided Prostate Biopsies • • • Cognitive In-bore Co-registered fusion biopsy
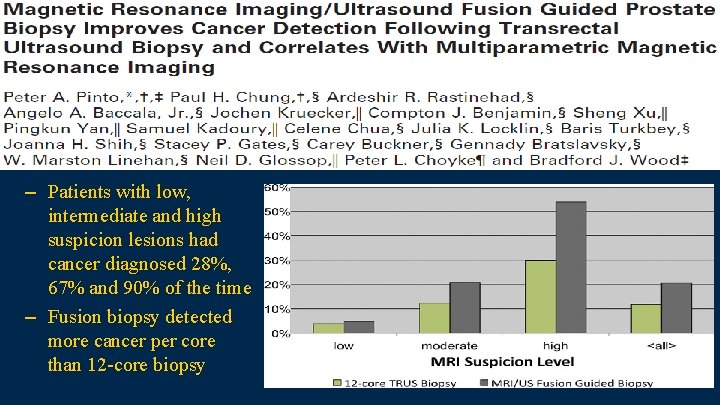
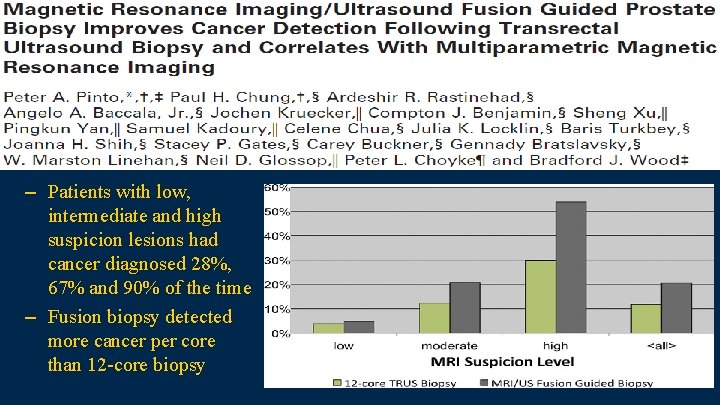
– Patients with low, intermediate and high suspicion lesions had cancer diagnosed 28%, 67% and 90% of the time – Fusion biopsy detected more cancer per core than 12 -core biopsy
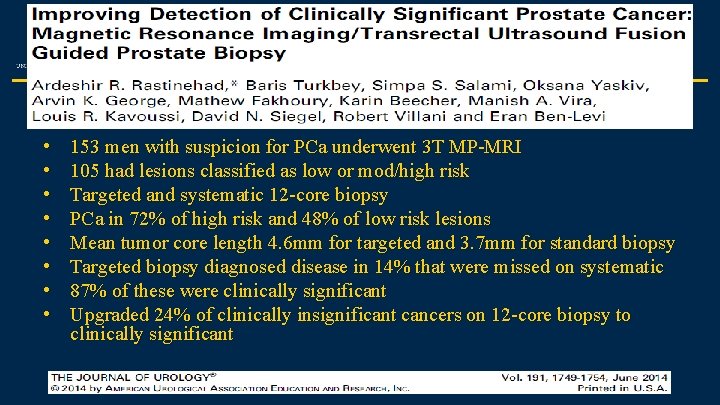
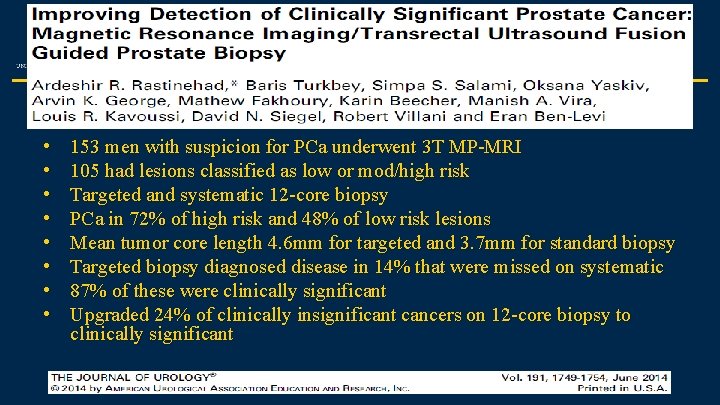
• • 153 men with suspicion for PCa underwent 3 T MP-MRI 105 had lesions classified as low or mod/high risk Targeted and systematic 12 -core biopsy PCa in 72% of high risk and 48% of low risk lesions Mean tumor core length 4. 6 mm for targeted and 3. 7 mm for standard biopsy Targeted biopsy diagnosed disease in 14% that were missed on systematic 87% of these were clinically significant Upgraded 24% of clinically insignificant cancers on 12 -core biopsy to clinically significant
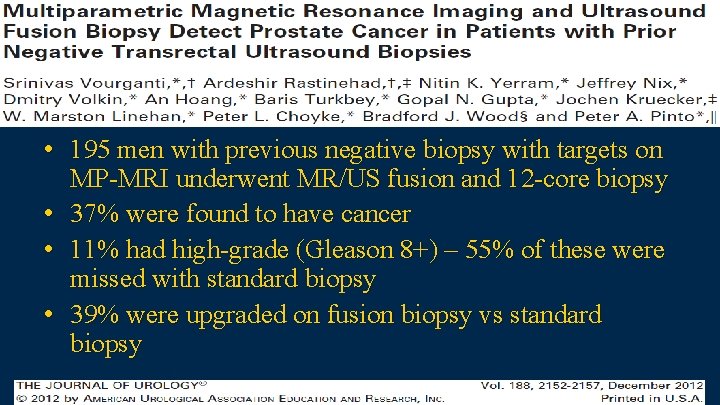
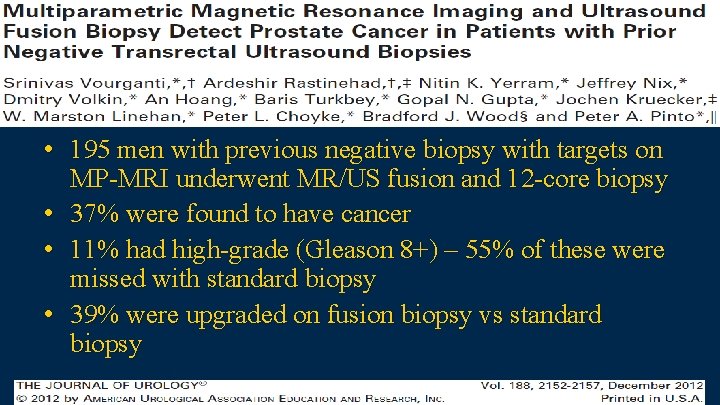
• 195 men with previous negative biopsy with targets on MP-MRI underwent MR/US fusion and 12 -core biopsy • 37% were found to have cancer • 11% had high-grade (Gleason 8+) – 55% of these were missed with standard biopsy • 39% were upgraded on fusion biopsy vs standard biopsy
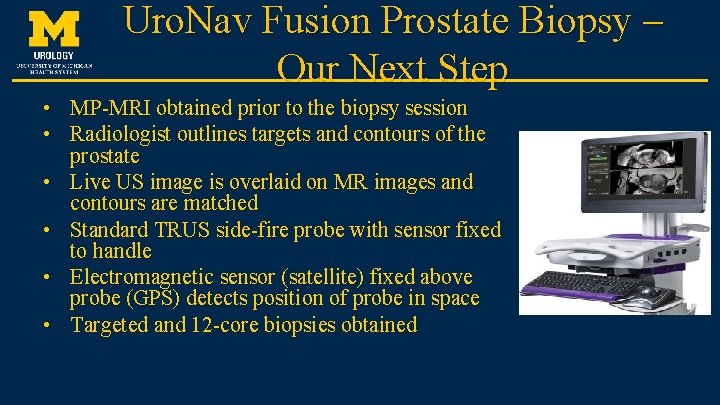
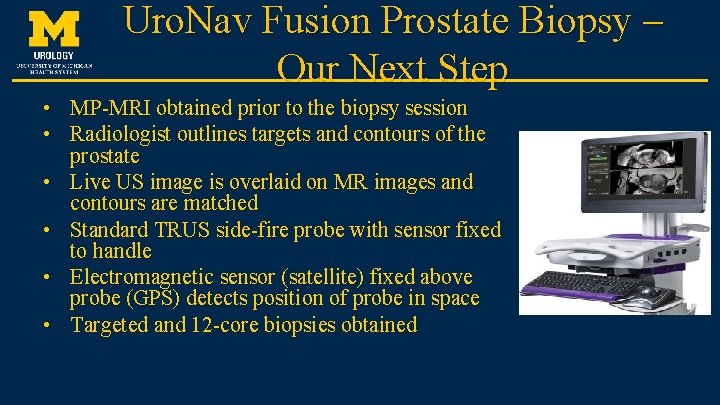
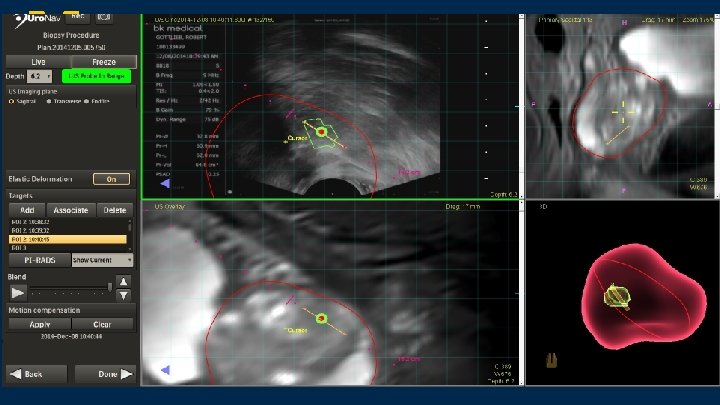
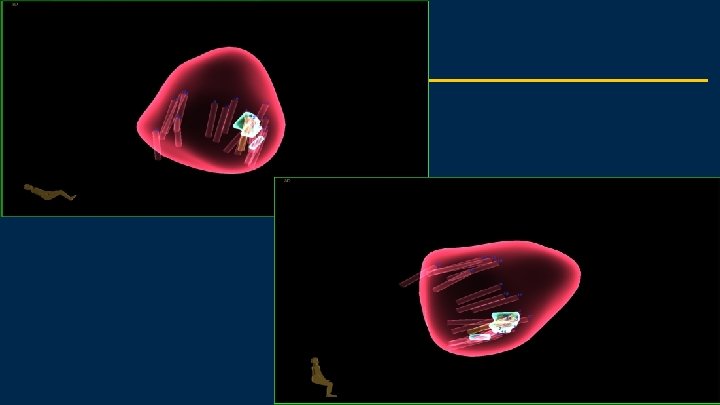
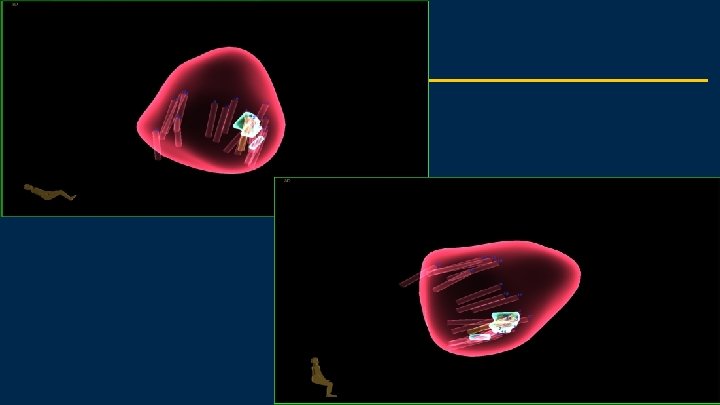
Uro. Nav Fusion Prostate Biopsy – Our Next Step • MP-MRI obtained prior to the biopsy session • Radiologist outlines targets and contours of the prostate • Live US image is overlaid on MR images and contours are matched • Standard TRUS side-fire probe with sensor fixed to handle • Electromagnetic sensor (satellite) fixed above probe (GPS) detects position of probe in space • Targeted and 12 -core biopsies obtained
Genetic Profiling
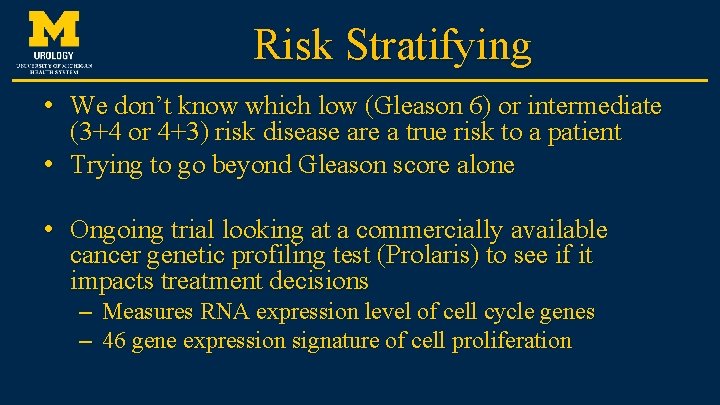
Risk Stratifying • We don’t know which low (Gleason 6) or intermediate (3+4 or 4+3) risk disease are a true risk to a patient • Trying to go beyond Gleason score alone • Ongoing trial looking at a commercially available cancer genetic profiling test (Prolaris) to see if it impacts treatment decisions – Measures RNA expression level of cell cycle genes – 46 gene expression signature of cell proliferation


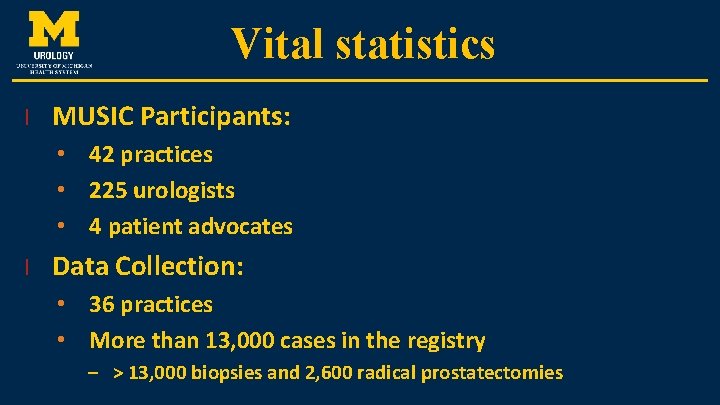
MUSIC Michigan Urologic Surgery Improvement Collaborative
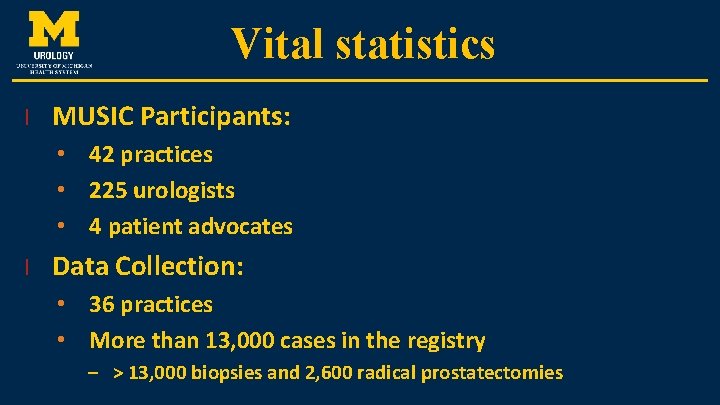
Vital statistics l MUSIC Participants: • 42 practices • 225 urologists • 4 patient advocates l Data Collection: • 36 practices • More than 13, 000 cases in the registry – > 13, 000 biopsies and 2, 600 radical prostatectomies
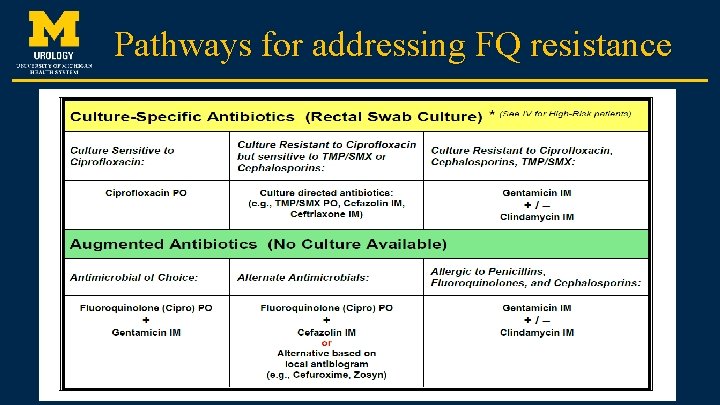
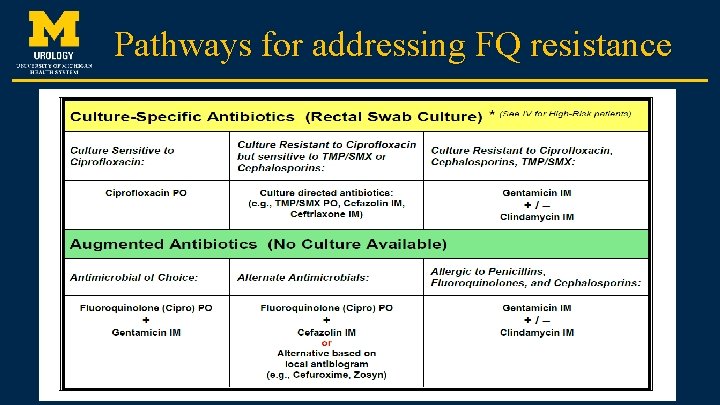
Pathways for addressing FQ resistance
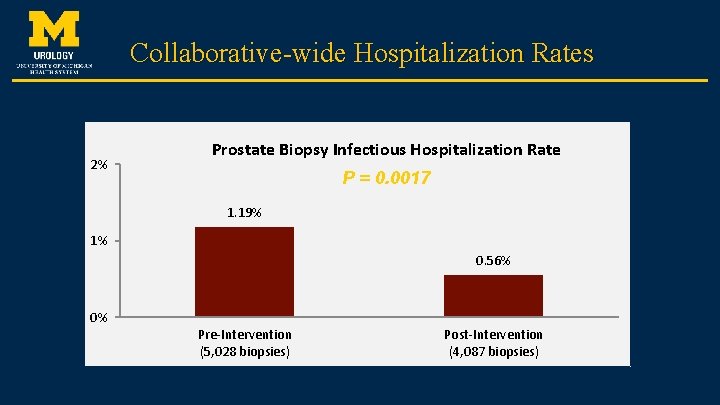
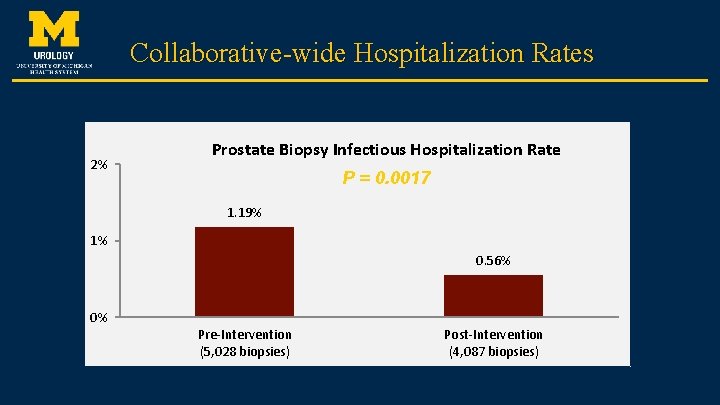
Collaborative-wide Hospitalization Rates 2% Prostate Biopsy Infectious Hospitalization Rate P = 0. 0017 1. 19% 1% n = 65 0. 56% n n= =2525 0% Pre-Intervention (5, 028 biopsies) Post-Intervention (4, 087 biopsies)
Patient Reported Outcomes (PRO) A statewide infrastructure for measuring and improving functional outcomes after radical prostatectomy Patients Providers Practices Collaborative 54
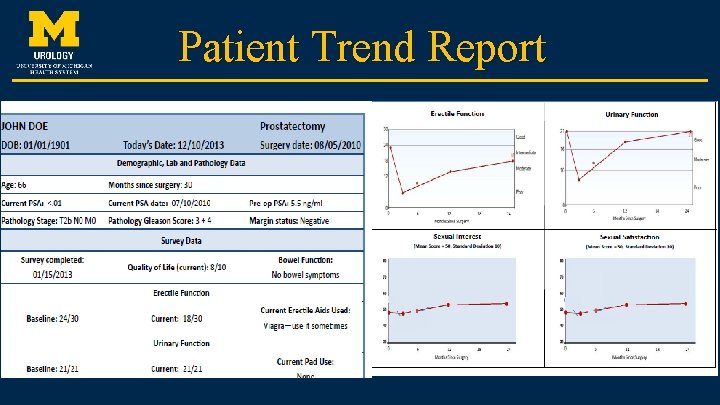
Patient Trend Report
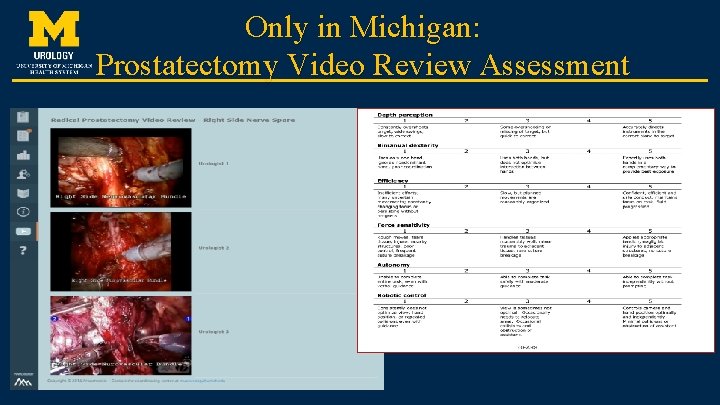
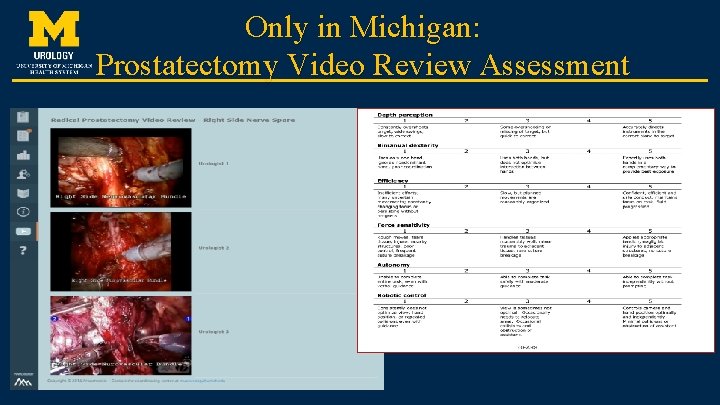
Only in Michigan: Prostatectomy Video Review Assessment
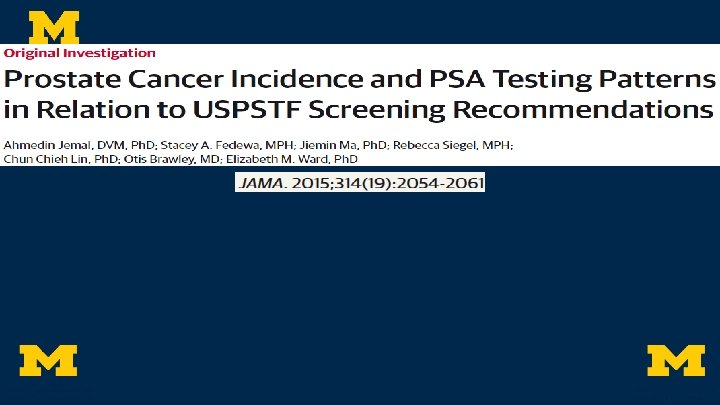
Methods-Incidence • Ecological study using SEER cancer registry – Data from 2005 -2012 • N = 446, 009 – Identified incident cases of local/regional or distant prostate cancer – Merged SEER data with CDC data to examine changes in incidence by age – Incidence Rations (IR) • Compare relative change in incidence between consecutive years for age standardized rates
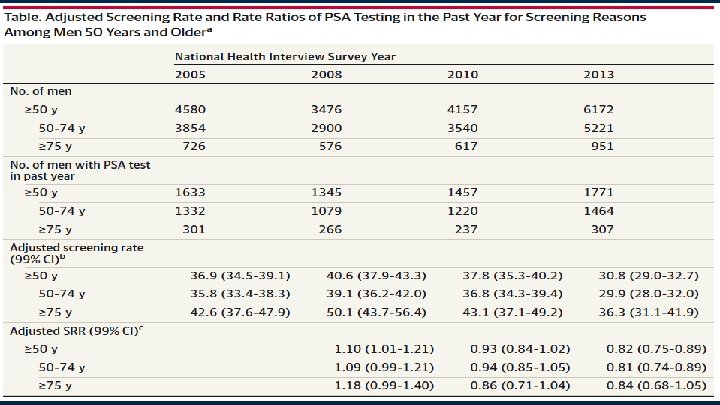
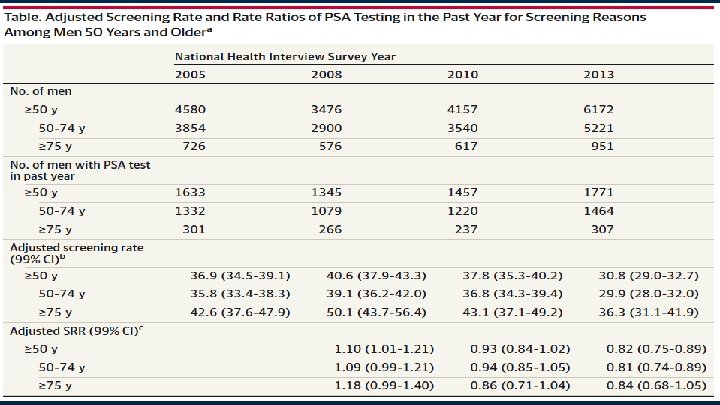
Methods-PSA testing • National Health Interview Surveys (NHIS) data – Nationally representative household cross-sectional sample – Collected 2005, 2008, 2010, 2013 • N = 18, 385 – Rate of self-reported PSA testing in past year – Screening Rate Ratios (SRR) • Age and Race adjusted comparison of relative change in screening between years
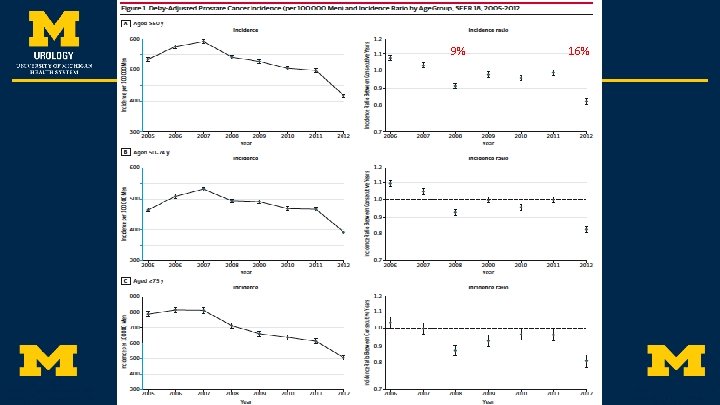
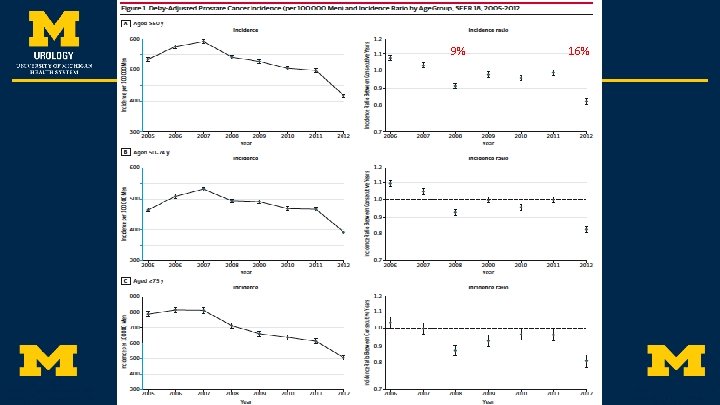
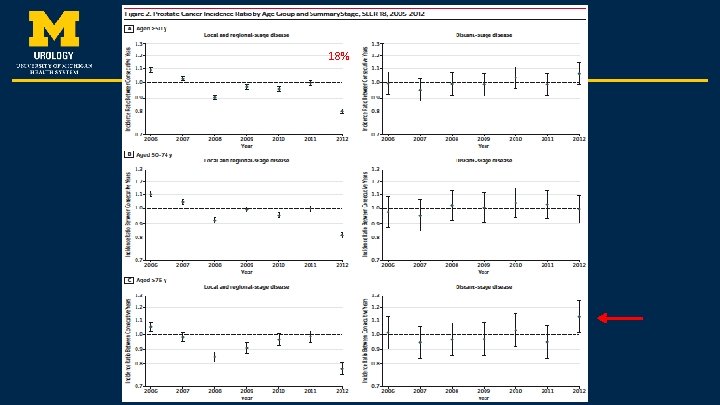
9% 16%
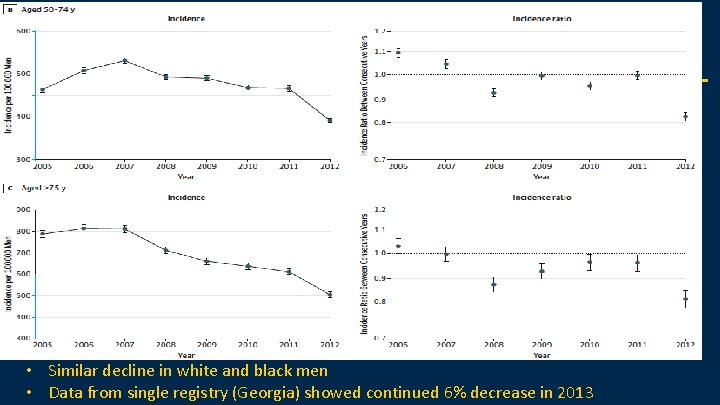
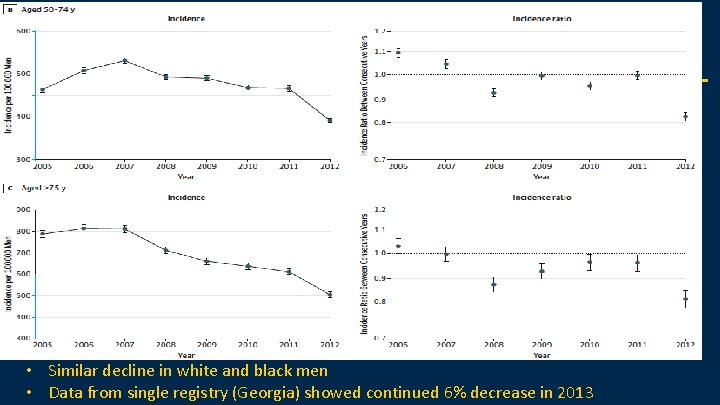
• Similar decline in white and black men • Data from single registry (Georgia) showed continued 6% decrease in 2013
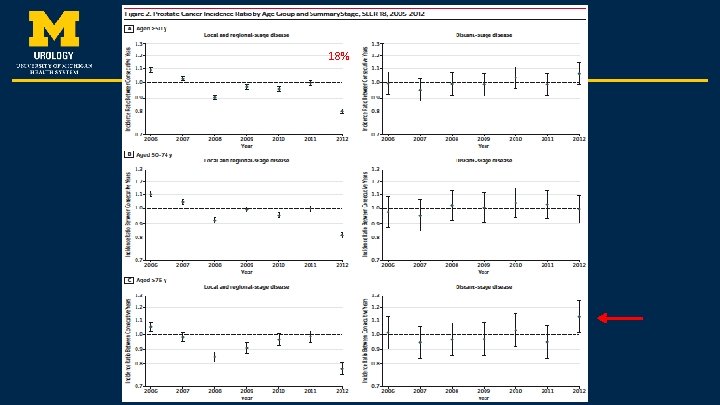
18%
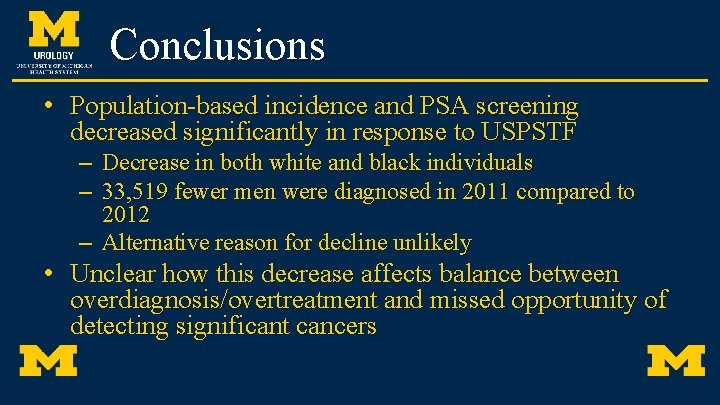
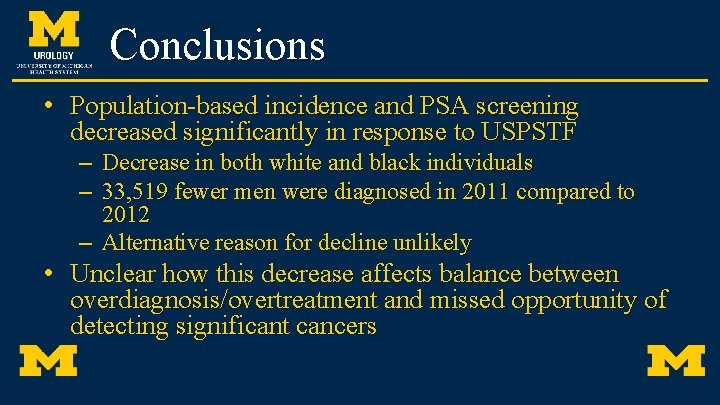
Conclusions • Population-based incidence and PSA screening decreased significantly in response to USPSTF – Decrease in both white and black individuals – 33, 519 fewer men were diagnosed in 2011 compared to 2012 – Alternative reason for decline unlikely • Unclear how this decrease affects balance between overdiagnosis/overtreatment and missed opportunity of detecting significant cancers
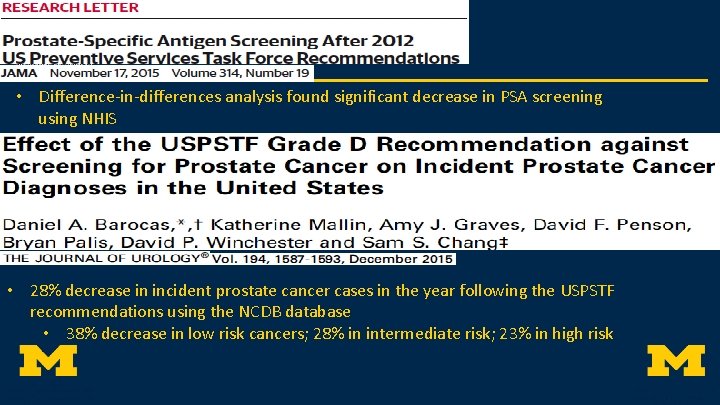
• Difference-in-differences analysis found significant decrease in PSA screening using NHIS • 28% decrease in incident prostate cancer cases in the year following the USPSTF recommendations using the NCDB database • 38% decrease in low risk cancers; 28% in intermediate risk; 23% in high risk
How do we improve screening • Shared decision making around screening in men 50/55 -69 years old • Obtain a confirmatory test prior to proceeding with biopsy to help refine risk • Obtain MRI to help improve the yield of biopsy • Promote active surveillance as front line treatment in appropriate patients – Consider use of genomic tests to better define risk
Treatment Appropriateness Rationale: great concern regarding overtreatment Variation is appropriate when it can be explained by factors that are considered relevant in treatment decisions Variation is inappropriate when based on ethnicity, insurance, choice of doctor, ancillary profit, etc
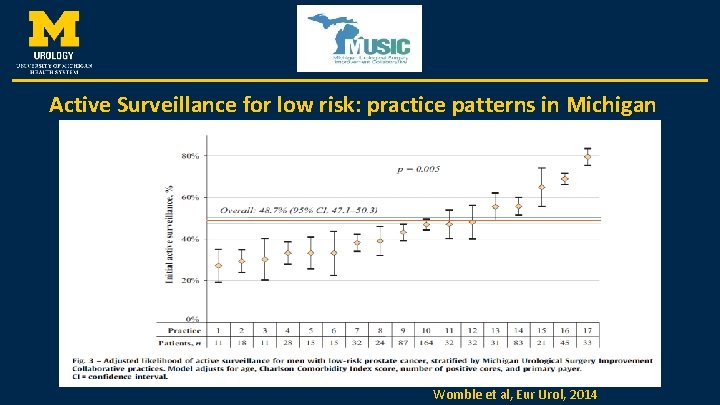
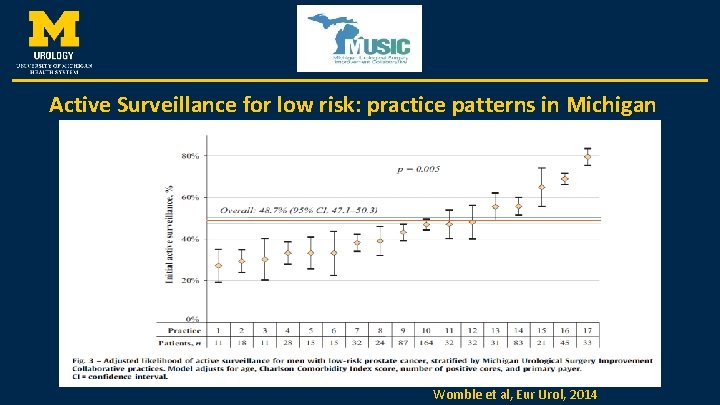
Active Surveillance for low risk: practice patterns in Michigan Womble et al, Eur Urol, 2014
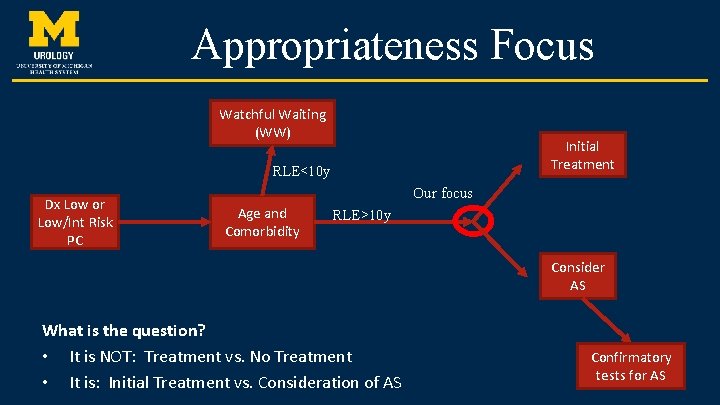
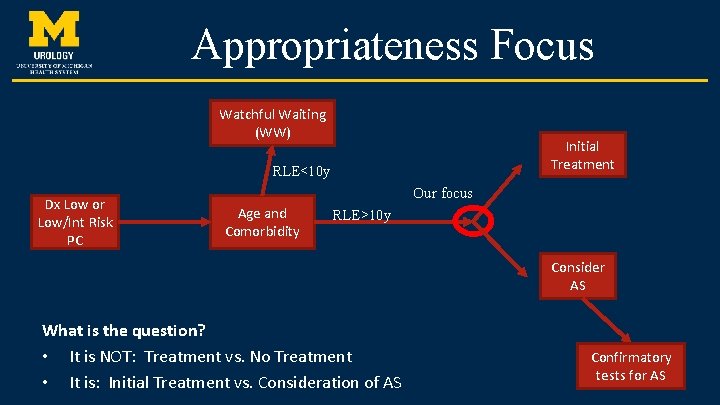
Appropriateness Focus Watchful Waiting (WW) Initial Treatment RLE<10 y Dx Low or Low/Int Risk PC Our focus Age and Comorbidity RLE>10 y Consider AS What is the question? • It is NOT: Treatment vs. No Treatment • It is: Initial Treatment vs. Consideration of AS Confirmatory tests for AS
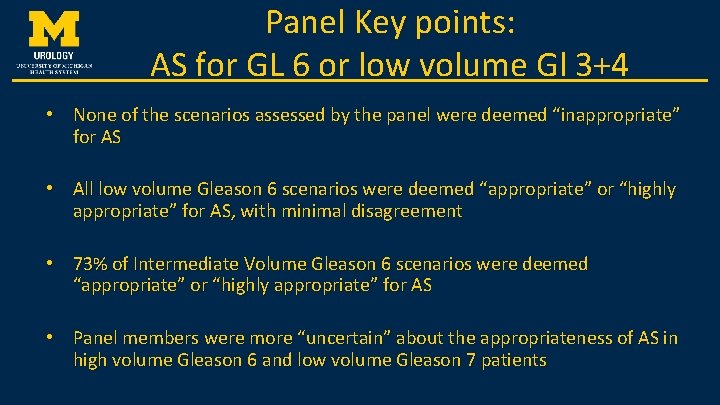
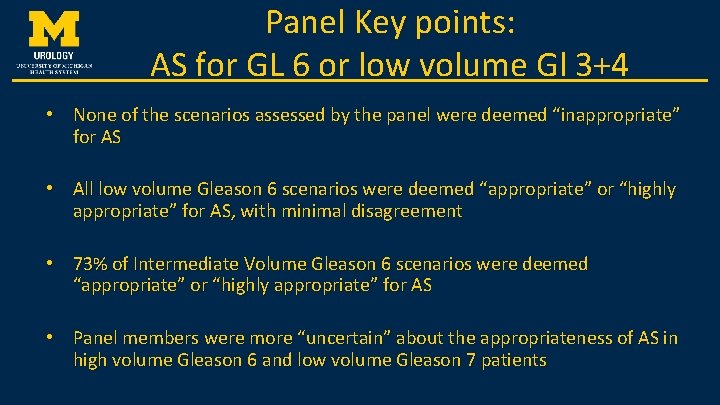
Panel Key points: AS for GL 6 or low volume Gl 3+4 • None of the scenarios assessed by the panel were deemed “inappropriate” for AS • All low volume Gleason 6 scenarios were deemed “appropriate” or “highly appropriate” for AS, with minimal disagreement • 73% of Intermediate Volume Gleason 6 scenarios were deemed “appropriate” or “highly appropriate” for AS • Panel members were more “uncertain” about the appropriateness of AS in high volume Gleason 6 and low volume Gleason 7 patients
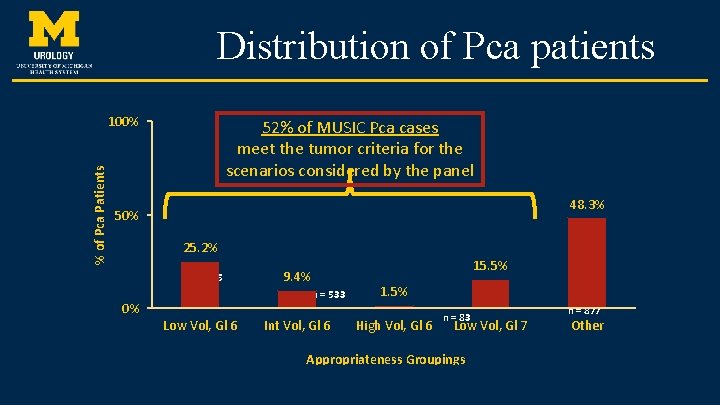
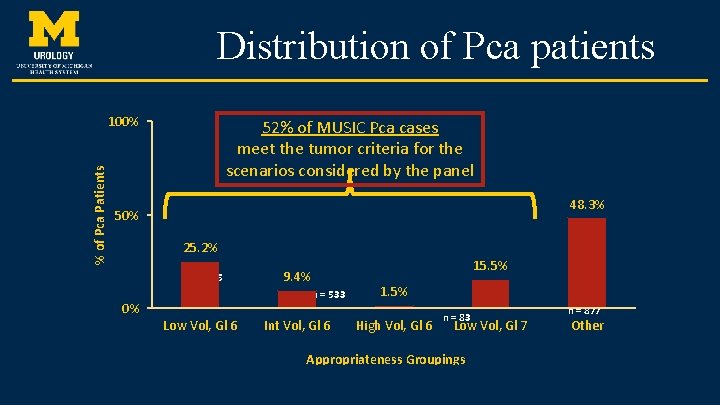
Distribution of Pca patients % of Pca Patients 100% 52% of MUSIC Pca cases meet the tumor criteria for the scenarios considered by the panel 48. 3% 50% 25. 2% n = 1, 425 15. 5% 9. 4% n = 533 0% Low Vol, Gl 6 Int Vol, Gl 6 1. 5% High Vol, Gl 6 n = 83 Low Vol, Gl 7 Appropriateness Groupings n = 877 Other
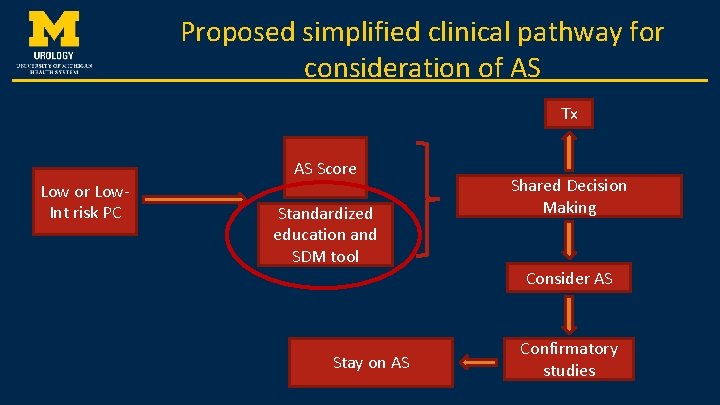
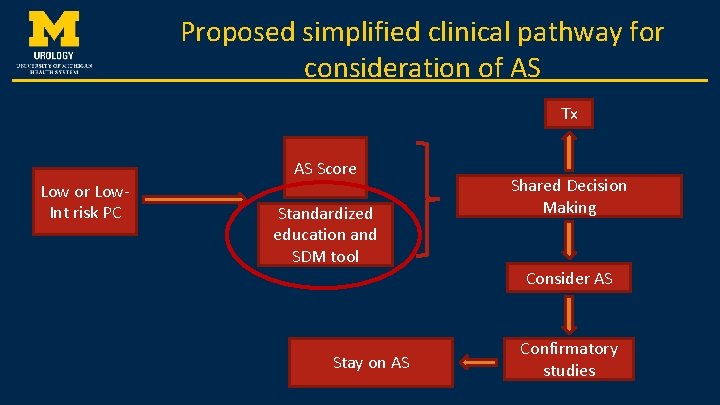
Proposed simplified clinical pathway for consideration of AS Tx AS Score Low or Low. Int risk PC Standardized education and SDM tool Stay on AS Shared Decision Making Consider AS Confirmatory studies
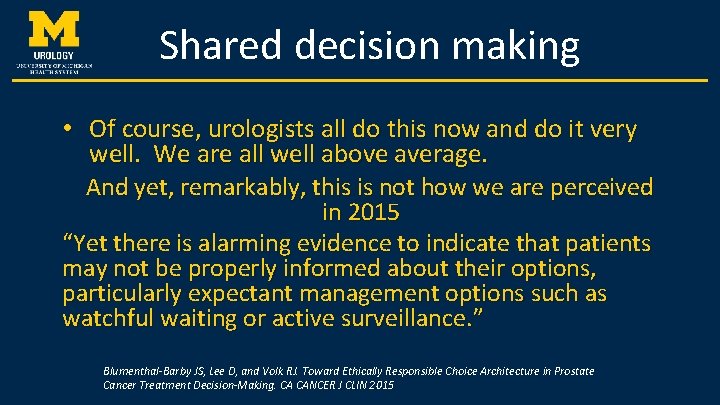
Shared decision making • Of course, urologists all do this now and do it very well. We are all well above average. And yet, remarkably, this is not how we are perceived in 2015 “Yet there is alarming evidence to indicate that patients may not be properly informed about their options, particularly expectant management options such as watchful waiting or active surveillance. ” Blumenthal-Barby JS, Lee D, and Volk RJ. Toward Ethically Responsible Choice Architecture in Prostate Cancer Treatment Decision-Making. CA CANCER J CLIN 2015
Shared decision making • In 2015, the Movember Foundation reviewed PCa treatment SDM web-based tools and recognized 2 instruments as ideal 1. Wiser. Care 2. Prostate Personal Patient Profile (“P 3 P”) • In Jan 2016, the MUSIC AS working group reviewed both of these and selected P 3 P Implementation next challenge!!
Final Word • Case: to screen or not to screen? Getting a PSA for symptoms is not screening • While better treatments exist for advanced/metastatic disease, no one has examined QOL/morbidity/cost compared to early treatment • Questions?