PROSTATE CANCER AND BPH Prostate cancer The second
PROSTATE CANCER AND BPH
Prostate cancer • The second most common cancer diagnosed in men • The incidence increase with age very rare before age of 40, more in western countries particularly Scandinavian countries (low light exposure), and black men are at greatest risk • Family history: ptn with family history has increase incidence of prostate cancer and earlier onset
• The most common prostatic malignancy is adenocarcinoma of prostate acinar or ductal epithelium • 75% are in peripheral zone, and 85% are multifocal • 15% in transitional and 5% in central zone • Tumour may involve nearby structures (urethral sphincter, corpora of penis, trigon, seminal vesicle , unlikely the rectum because denonvilliers fascia
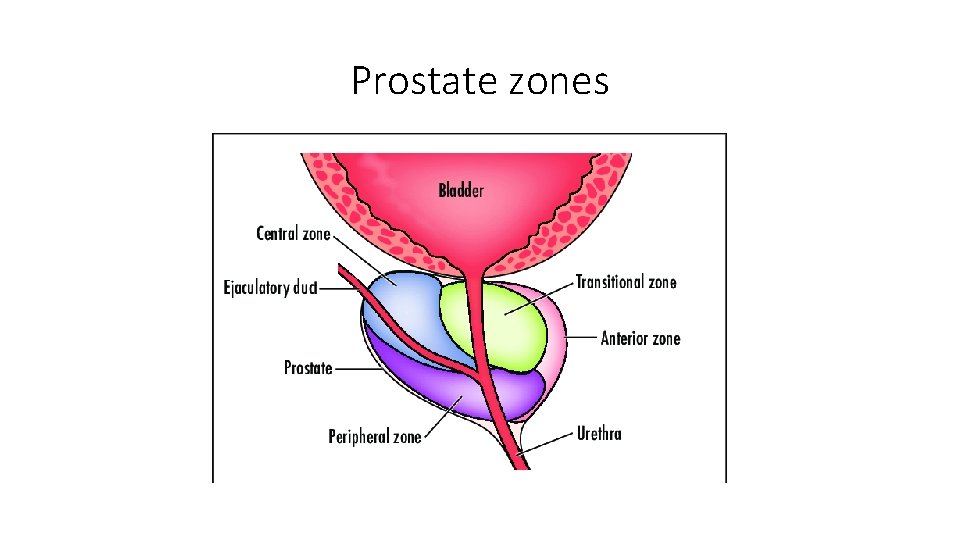
Prostate zones

Grading • It is graded by gleason system • Using low power microscope adenocarcinoma is graded into 1 -5 according to gland forming differentiation • Because the PC is multiple we add the two dominant grade • 2 -6 is well differentiated, 7 moderate differentiated, 8 -10 poorly differentiated • It correlate well with prognosis
• Cytologic features play no part in this grading system
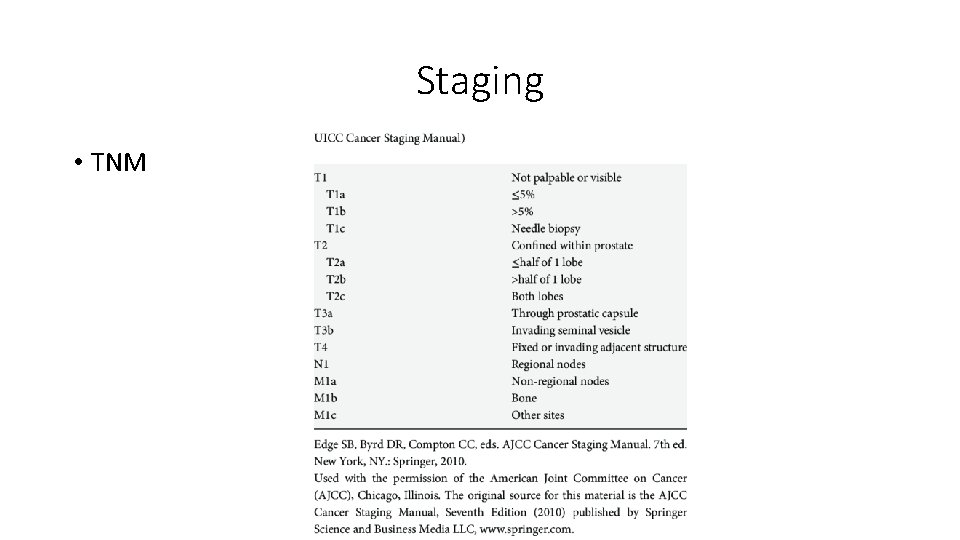
Staging • TNM
• T stage assessed by DRE, TRUS, and MRI • N stage assessed by MRI or during pelvic lymphadenectomy • M stage by CT scan and bone scan
Presentation • Screening refers to testing for disease in healthy, asymptomatic populations, whereas diagnosis is the identification of disease among individuals with signs or symptoms. • prostate cancer rarely causes symptoms at an early stage. The presence of symptoms suggests locally advanced or metastatic disease. • Manifestations of locally advanced prostate cancer include urinary symptoms, ureteral obstruction causing renal failure, hematospermia or decreased ejaculate volume, • Manifestations of metastatic disease include bone pain, pathologic fractures, anemia, and lower extremity edema, and, less commonly, malignant retroperitoneal fibrosis, paraneoplastic syndromes, and disseminated intravascular coagulation (DIC).
• Locally advanced and metastatic disease are uncommon presentations due to widespread screening with prostate-specific antigen (PSA) and digital rectal examination(DRE). A histologic diagnosis of prostate cancer is typically madeby prostate needle biopsy using transrectal ultrasound guidance(TRUS biopsy).
Clinical diagnosis • It is usually suspected in the basis of DRE or PSA • Abnormal digital examination isassociate with higher grade , and indication of bx • PSA it is organ specific not disease specific, may be elevated in different prostate disease such as BPH, prostatitis, cancer, prostate calculi • There is no agreed standard for measuring PSA, higher level increase the chance of prostate cancer, and the level depend on the age
PSA • PSA density : the level divided by TRUS prostate volume the higher the density more chance of malignancy • Free/total ratio: decrease the ratio increase the posibility of prostate cancer, no clinical use if PSA more than 10 • PS velocity : absolute annual increase in PSA per year and PSA doubling time: exponential increase in PSA over time, has prognostic role but limited diagnostic role.
TRUS and multiparametric MRI are imaging study that can be used to detect PC Prostate bx: can be done transrectal or transperineal, at least 8 bx for prostate 30 cc and 10 -12 for larger prostate Complication include hematospermia , hematurea, prostatitis , retention, rectal bleeding -
• Assessing the risk category into: • 1 - low risk with PSA< 10, gleason score <7 and stage T 1 -T 2 a • 2 - intermediate risk with PSA 10 -20, gleason 7 and T 2 b-T 2 c • 3 -High risk with PSA >20, gleason 8 -10 and T 3 -T 4
1 -Watchful waiting • It is suitable for ptn with health problem and life expectancy less than 10 years • Ptn watched if develop local or distant progression • If disease progress… palliative treatment for cancer and symptom Mx
2 -Active surveillance • In low risk pt to avoid overtreatment • Do serial DRE, PSA and TRUS biopsy, if disease progress aim to cure it
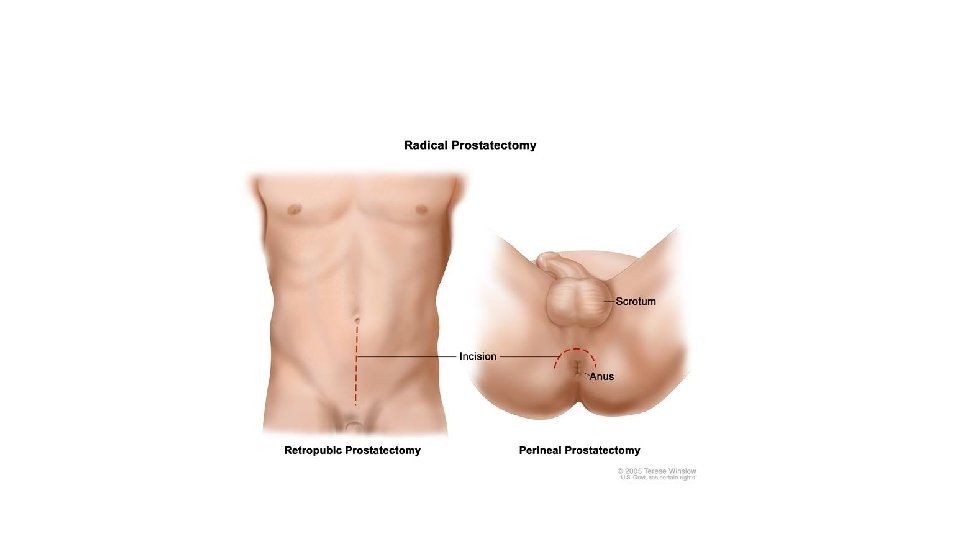
3 - Radical prostatectomy • Best option for localized and locally advanced disease • Either retropubic or perineal approaches….
4 - EBRT • For localized and locally advanced disease • C. I. in : - severe LUTS and IBD • S. E. : - LUTS, GI symptoms, hematuria and ED
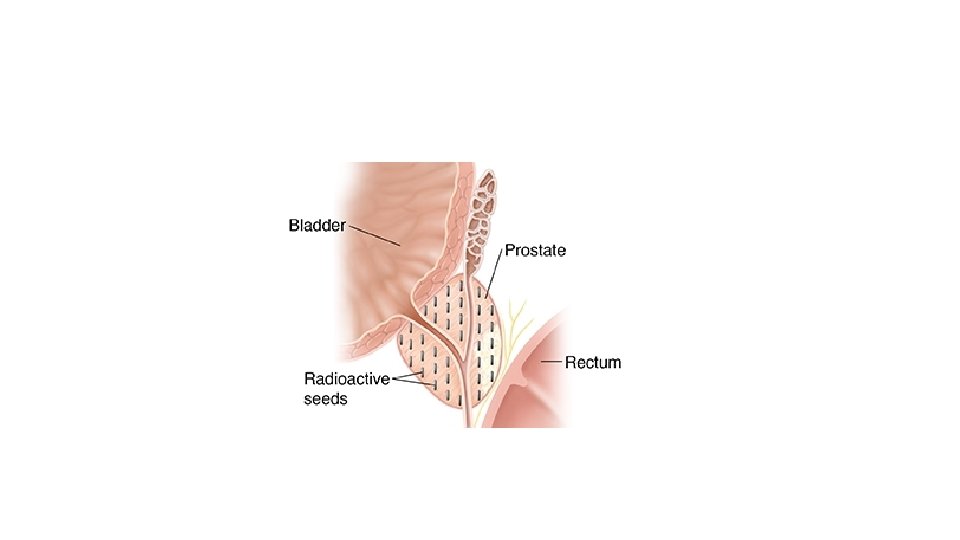
5 - Brachytherapy • C. I. : -previous TURP, prostate volume >60 ml and severe LUTS
6 - Hormonal therapy • In metastatic disease • Types: - surgical castration… • medical castration ( LHRH antagonist , LHRH agonist and antiandrogens)…. . • S. E. : - ED, hot flushes, weight gain, depression, gynecomastia, osteoporosis ( andropause)
BPH Prostate is one of sex accessory gland that derived from urogenital sinus Swelling of terminal part of hindgut result in formation of cloaca, which later on divided by urogenital septum into anorectal sinus and urogenital sinus The urogenital sinus is differentiated into bladder , urethra , and prostate Prostate development from urogenital sinus is under dihydrotestosteron stimulation
Function of prostate • Prostate with other sex accessory gland secrete seminal plasma which provide suitable environment for survival and function of sperm. • SAG include seminal vesicle, prostate, epididymis, cowper gland • Prostate form 16 of seminal fluid volume while the sperm only 1% of seminal fluid, the majority comes from seminal vesicle • Prostate seretes zinc, citric acid , and psa • Psa is important for liquifaction of semen
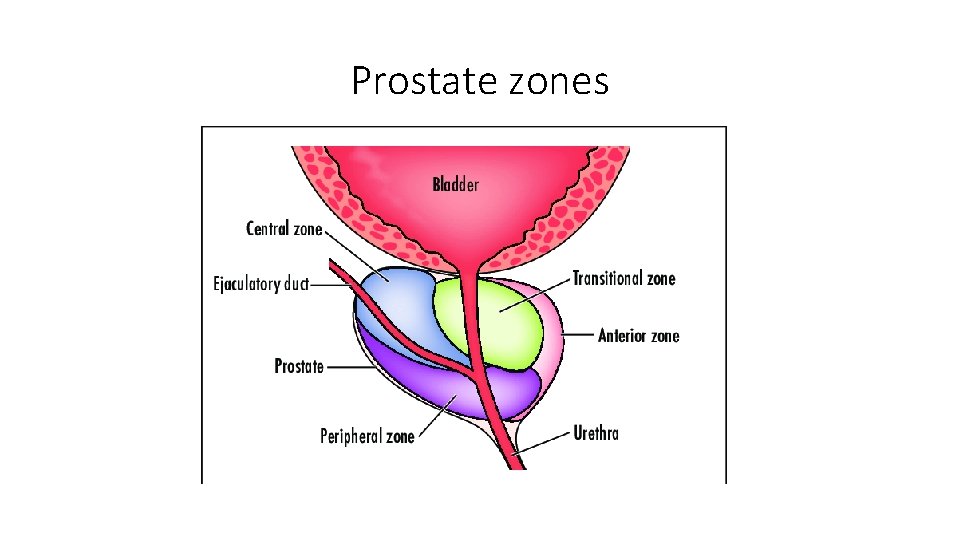
Prostate zones
Etiology • BPH is characterized by increase in the number of epithelial and stromal cell • The development of BPH requires androgen • In prostate the testosterone is converted into DHT by 5 alpha reductase, which is 5 times more potent than testosterone • There are two types of this enzyme , type 1 which is extraprostatic and type 2 which found in prostate • The process of BPH suggests reawakening of embryonic process of prostate development • Familial factors of BPH
pathophisiology • BPH develpes in transitional zone • Prostate hyperplasia-BOO-detruser response-LUTS • The size of prostate doesnot correlate with degree of obstruction • Static vs dynamic obstruction • Adrenergic nervous system –alpha 1 receipter-smooth muscle contraction-increase prostatic urethral resistance • Bladder response to obstruction includes hypertrophy (detrusal instability) by modulation of neural detrusal response • Deposition of collagen which affect the compliance
Symptoms of BPH • Symptoms can be obstructive or irritative symptoms or hematuria • Complication includes bladder stones , infections , hematurea, urinary retention,
assesment • History and physical examination • Serum creatinine and urine test • psa • Uroflowmetry and PVR • Renal / TRUS
Management • BPH vs BPE vs clinical BPH(LUTS) • Watchful waiting(simple measures such as decrease fluid intake , moderate intake of caffiene, time voiding, avoide constipation) • Medical management symptoms that cause bothering to the patient • Or patient with moderate to severe IPSS score • Surgical option if failed medical management or complication
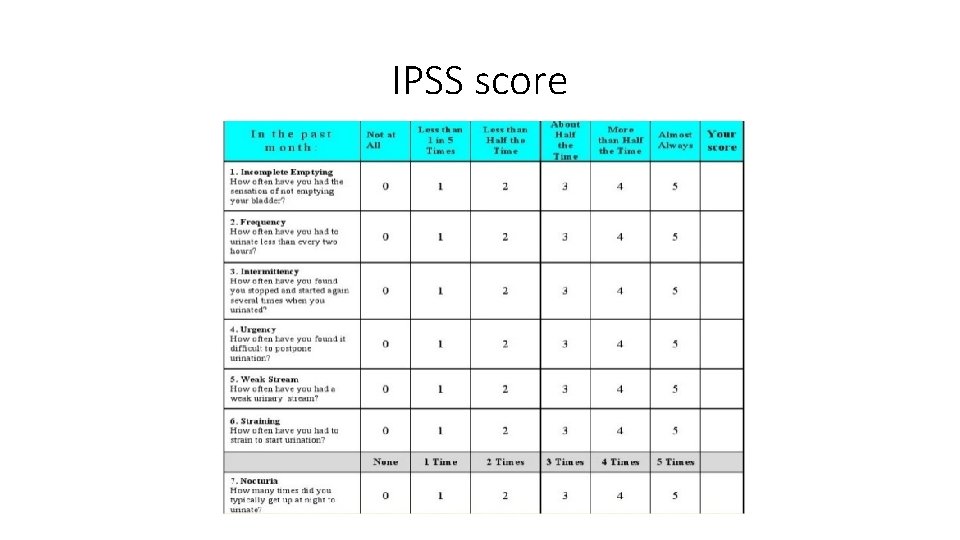
IPSS score
• Mild (symptom score less than of equal to 7) • Moderate (symptom score range 8 -19) • Severe (symptom score range 20 -35)
• Medical management includes alpha adrenergic blocker • Like tamsulosin alfuzosin doxazosin terazosin • Side effect include dizziness , postural hypotension, retrograde ejaculation, intraoperative floppy iris syndrome(tamsulosin impaire iris dilatation which is important for safe cataract surgery • 5 alpha reductase inhibiters such as finasteride and dutasteride If prostate size more than 40 ml , <decrease the size by 20 %, the effect appear after 3 -6 monthes Mainly sexual side effect ED decrease libido • Anticholinergic. PDEI good option in ptn of ED and LUTS
• Combination treatement of alpha 1 blocker and anti muscarinic in ptn with significant irritative symptom. • No anti muscarinic if PVR more than 150 ml
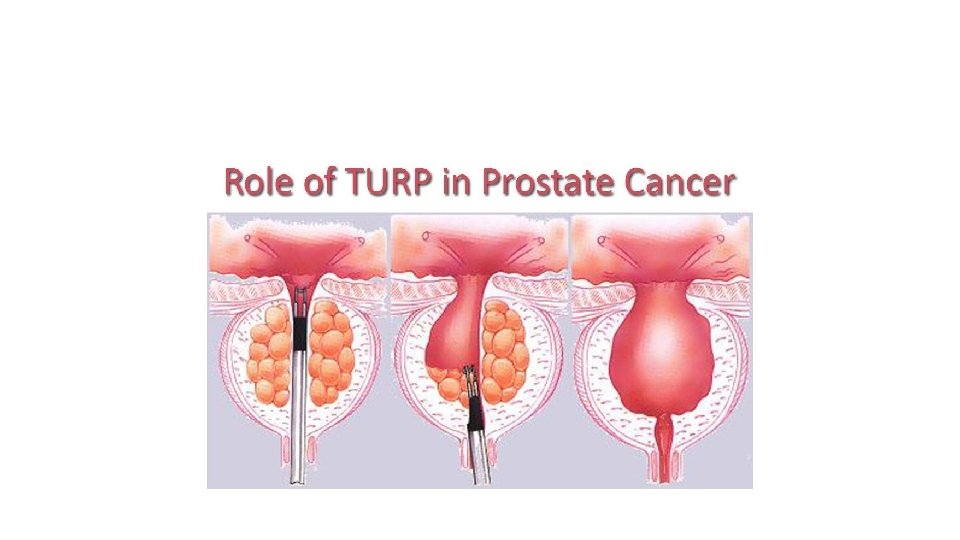
• Surgical like TURP (electrified wire loop, TUIP, laser prostatectomy or open prostatectomy • Indications: • Failure of medical Tx • Recurrent UTI • Renal impairment • Recurrent hematuria • Bladder stones
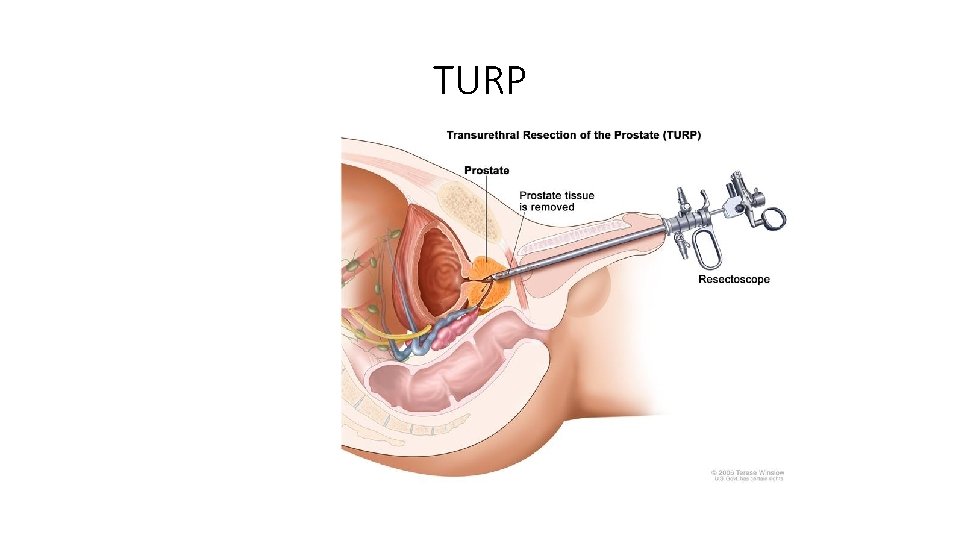
TURP
• Indications for open rather than endoscopic procedure: • Large prostate size (>80 g) • severe Urethral stricture • Difficult lithotomy position • Large bladder stones
• TUR syndrome: fluid absorption of hypotonic fluid which lead to dilutional hyponatremia with resulting neurologic change , bradycardia , and hypertension. • Early vs late complication of TURP • Early like infection, hemorrhage, TUR syndrome, or bladder perforation • Late like retrograde ejaculation , incontinence, failure of surgery
- Slides: 39