Promoting Improvement PDSA Plan Do Study Act Agenda

- Slides: 30
Promoting Improvement PDSA Plan – Do – Study – Act
Agenda �Introductions �Course Objectives �The Model for Improvement at UNMH ◦ PDSA
Course Objectives Describe concepts of change and principles of PDSA as a systematic problem -solving model • List the steps in a PDSA cycle. • Applying insights gained from this interactive and fun exercise, participants will be energized to bring new Quality Improvement skills and knowledge back to their clinical settings to begin or enhance improvement efforts. •
What in the world is PDSA? “a cycle that can be used to turn ideas into action and connect action to learning” “a shorthand for testing a change” www. ihi. org
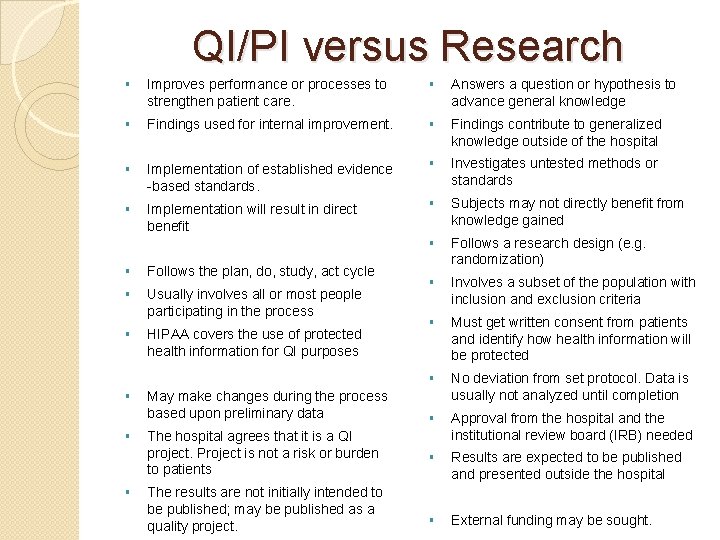
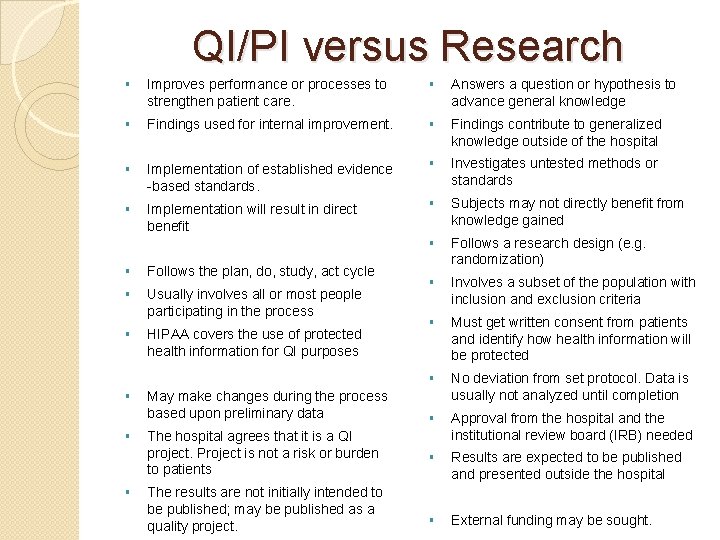
QI/PI versus Research § Improves performance or processes to strengthen patient care. § Answers a question or hypothesis to advance general knowledge § Findings used for internal improvement. § Findings contribute to generalized knowledge outside of the hospital § Implementation of established evidence -based standards. § Investigates untested methods or standards § Implementation will result in direct benefit § Subjects may not directly benefit from knowledge gained § Follows a research design (e. g. randomization) § Involves a subset of the population with inclusion and exclusion criteria § Must get written consent from patients and identify how health information will be protected § No deviation from set protocol. Data is usually not analyzed until completion § Approval from the hospital and the institutional review board (IRB) needed § Results are expected to be published and presented outside the hospital § External funding may be sought. § Follows the plan, do, study, act cycle § Usually involves all or most people participating in the process § HIPAA covers the use of protected health information for QI purposes § § § May make changes during the process based upon preliminary data The hospital agrees that it is a QI project. Project is not a risk or burden to patients The results are not initially intended to be published; may be published as a quality project.
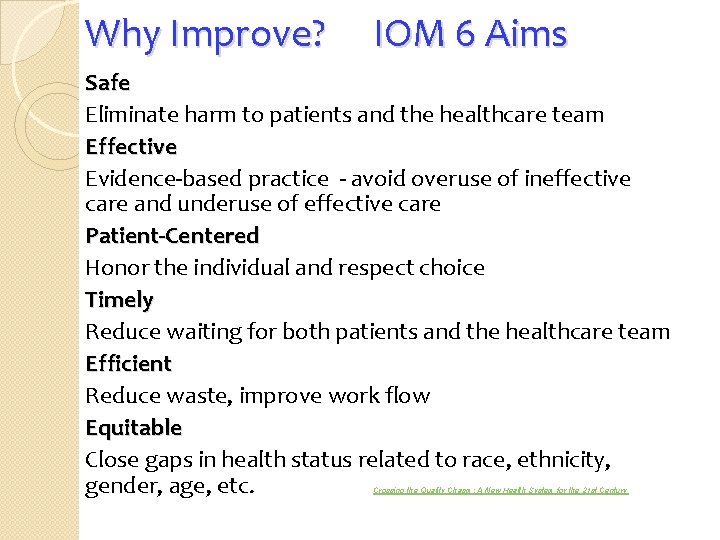
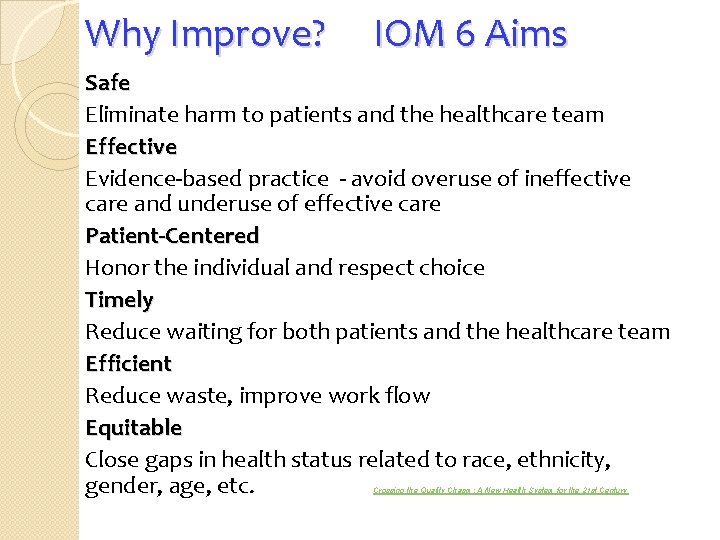
Why Improve? IOM 6 Aims Safe Eliminate harm to patients and the healthcare team Effective Evidence-based practice - avoid overuse of ineffective care and underuse of effective care Patient-Centered Honor the individual and respect choice Timely Reduce waiting for both patients and the healthcare team Efficient Reduce waste, improve work flow Equitable Close gaps in health status related to race, ethnicity, gender, age, etc. Crossing the Quality Chasm: A New Health System for the 21 st Century
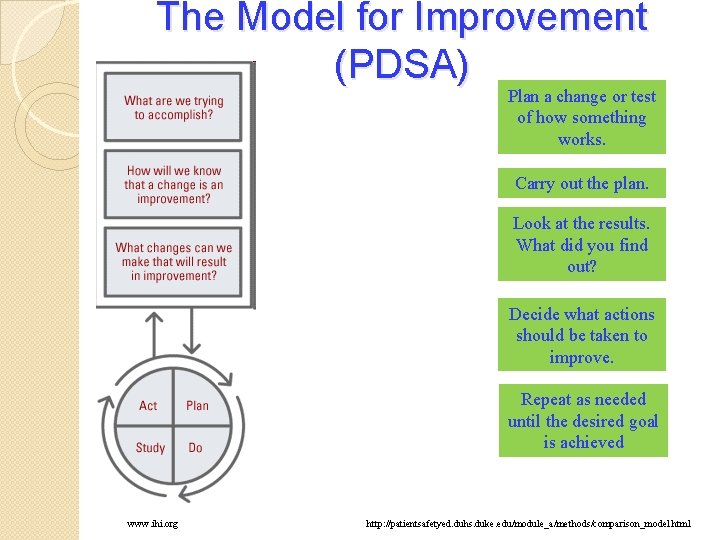
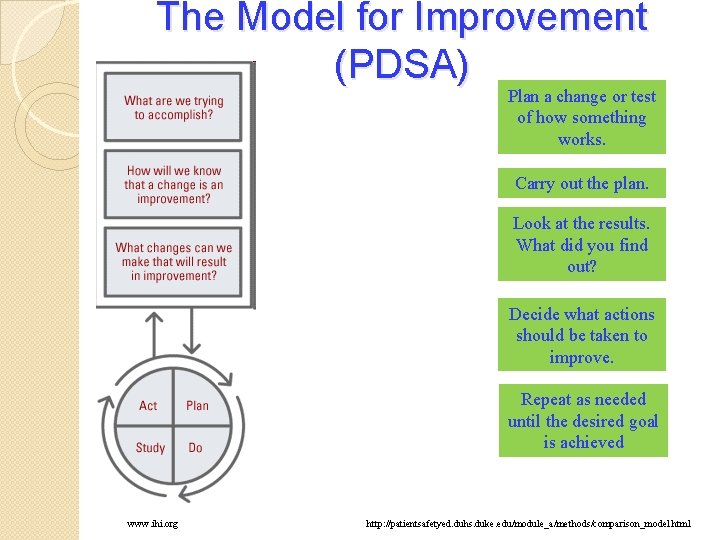
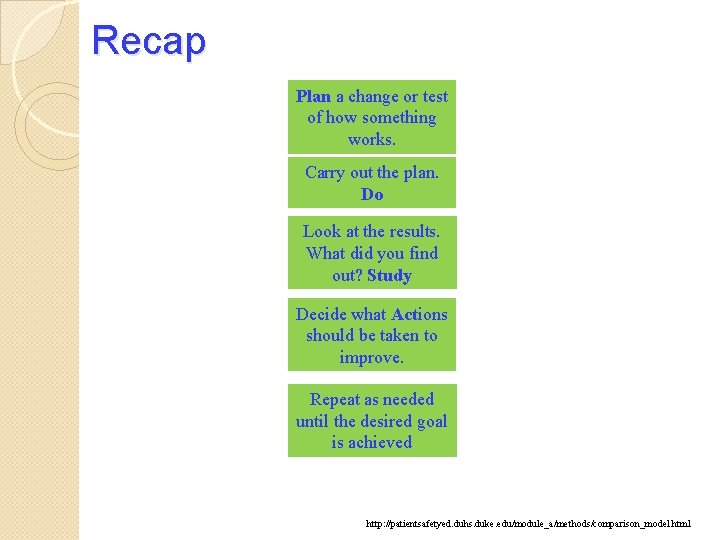
The Model for Improvement (PDSA) Plan a change or test of how something works. Carry out the plan. Look at the results. What did you find out? Decide what actions should be taken to improve. Repeat as needed until the desired goal is achieved www. ihi. org http: //patientsafetyed. duhs. duke. edu/module_a/methods/comparison_model. html
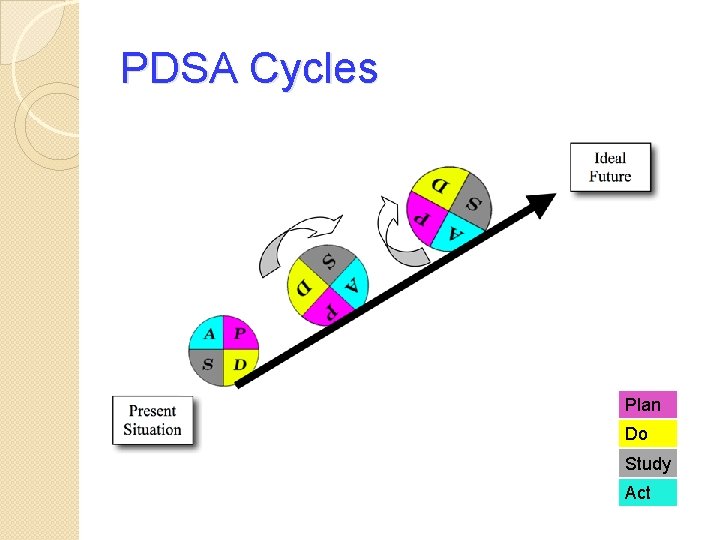
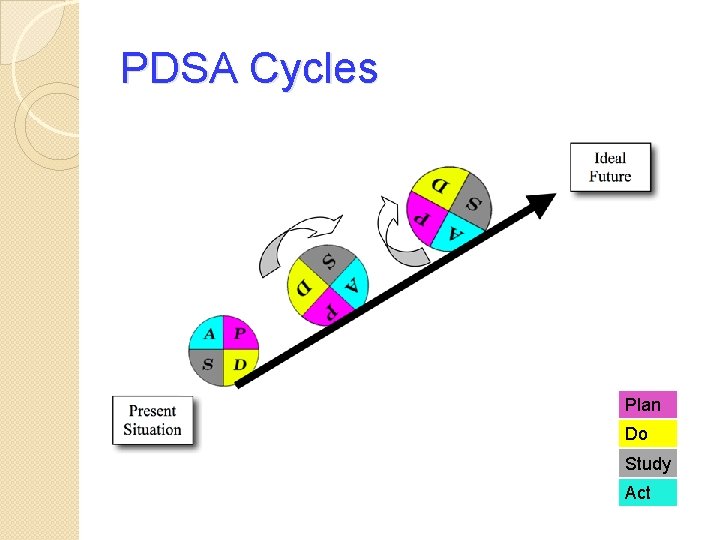
PDSA Cycles Plan Do Study Act
PDSA is a Team Effort! � Create a team to work on the project. ◦ Identify key stakeholders in the process – direct and indirect ◦ Always include frontline staff who will be affected by the change! � What are we trying to accomplish? Set Goals ◦ Clear determination of a specific goal ◦ Narrow focus � How will we know that a change is an improvement? ◦ Establish Measures ◦ Use SMART goals to make measures meaningful � What changes can we make that will result in improvement? ◦ Select Change(s) ◦ Test Change until the change is hardwired
Effective Teams – Key Stakeholders P L A N � System Leadership ◦ Teams need someone with enough authority in the organization to institute a change that has been suggested and to overcome barriers that arise. � Clinical/Technical Expertise ◦ A content expert is someone who knows the subject intimately and who understands the processes of care. (Frontline staff, physicians, LIPs) � Day-to-Day Leadership ◦ A day-to-day leader is the driver of the project, assuring that tests are implemented and overseeing data collection. � Facilitator ◦ Objective process expert. Makes recommendations and keeps the project moving
What is process? �Process P L A N is a structured set of activities that transform inputs into outputs. �A “process map” visually describes the flow of activities of a process. A process flow can be defined as the sequence and interactions of related process steps, activities or tasks that make up an individual process, from beginning to end. A process map is read from left to right or from top to bottom. �Process mapping is about communicating your process to others so that you achieve your management objectives.
What is your current process? Mapping �How are you doing ◦ Use flow diagrams the process now? �Be realistic in how you describe what you are doing. ◦ List Actual process, not what is in policy or the ideal P L A N �Include all the embedded work-around steps. �This may take several meetings, but will be the starting point to see if your change makes a difference.
Goals - Examples �Reduce P L A N waiting time to see a urologist by 50% within 9 months �Reduce linen waste/re-processing by 20% within 9 months �Improve glycemic control in hospitalized patients within 1 year by reducing the number of severe hypoglycemic (<60) by 10% �Improve Hand Hygiene compliance by providers to 90% within 3 months �Reduce scanned document turn around time by 50% within 9 months �Improve compliance of correct document in correct location (currently at 89%) by 10% in next 2 months.
Establishing Measures – How will we know that a change is an improvement? Measures tell a team whether the changes they are making actually lead to improvement. ü Effective measurements require a baseline. ü P L A N There are 2 basic types of measure in healthcare: Outcome Measures What is the result? ◦ For diabetes: Average hemoglobin A 1 c level for population of patients with diabetes ◦ For access: Number of days to appointment Process Measures Are the parts/steps in the system performing as planned? ◦ For diabetes: Percentage of patients with hemoglobin A 1 c level measured twice in the past year ◦ For access: Average daily clinician hours available for appointments
Selecting Changes – What changes can we make that will result in improvement? �All P L A N improvement requires making changes, but not all changes result in improvement. �Therefore we must identify the changes that are most likely to result in � Eliminate Waste improvement. � Manage Time � Improve Work Flow � Optimize Inventory � Change the Work Environment � Producer/Customer Interface � Focus on Variation � Error Proofing � Focus on the Product or Service
Implement the Change - Do ü Pilot changes on a smaller scale, when possible, before replicating the change to the entire system. ü Consider D O and assess whether the changes may improve one part of the system while causing new problems in other parts of the system. ü Communicate and collaborate with all areas that may be impacted by the change. Involve them in the project from the beginning, if appropriate.
Testing Change - Study S T U D Y Set aside time to analyze the data and study the results o Complete the analysis of the data o Compare the data to your predictions o Summarize and reflect on what was learned
Act Refine the change, based on what was learned from the test. ◦ Determine what modifications should be made ◦ Prepare a plan for the next test ◦ Celebrate successes! A C T Are changes designed to improve one part of the system causing new problems in other parts of the system? ◦ For reducing time patients spend on a ventilator after surgery: Make sure re-intubation rates are not increasing ◦ For reducing patients' length of stay in the hospital: Make sure readmission rates are not increasing ◦ For improving clinic access: Be sure satisfaction is not decreasing
Share and Spread • Share your findings with area leadership, S P R E A D • • physician and provider partners, executive leadership, and in area/department meetings. Offer your expertise in the process. Provide tools and other outcomes of the PDSA to other areas with the same issues.
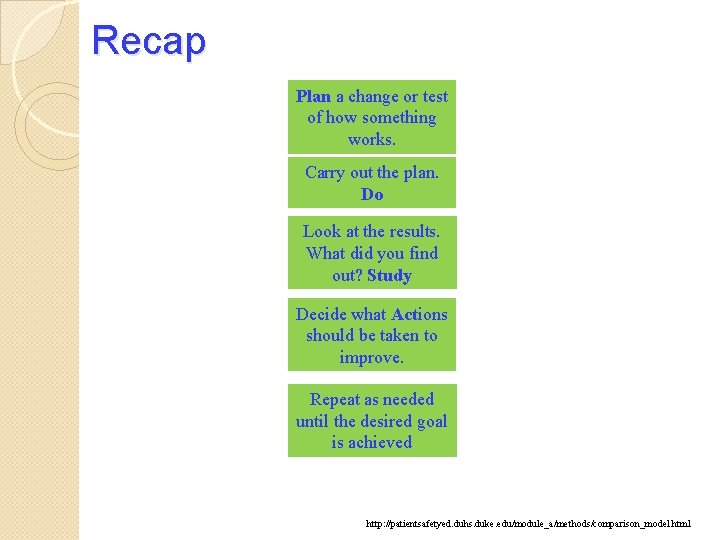
Recap Plan a change or test of how something works. Carry out the plan. Do Look at the results. What did you find out? Study Decide what Actions should be taken to improve. Repeat as needed until the desired goal is achieved http: //patientsafetyed. duhs. duke. edu/module_a/methods/comparison_model. html
Putting It Together Table Exercise

Breaking News: Health Care Teams Working to Improve Care of Multiple Bus Crash Victims! A bus filled with Potato Head family members has been in a terrible crash! At the scene of the accident, Emergency Medical Services arrives to find only scattered body parts. There were men, women, and children on the bus. Luckily, one of the uninjured family members was carrying a photo album with a photo of each family member.
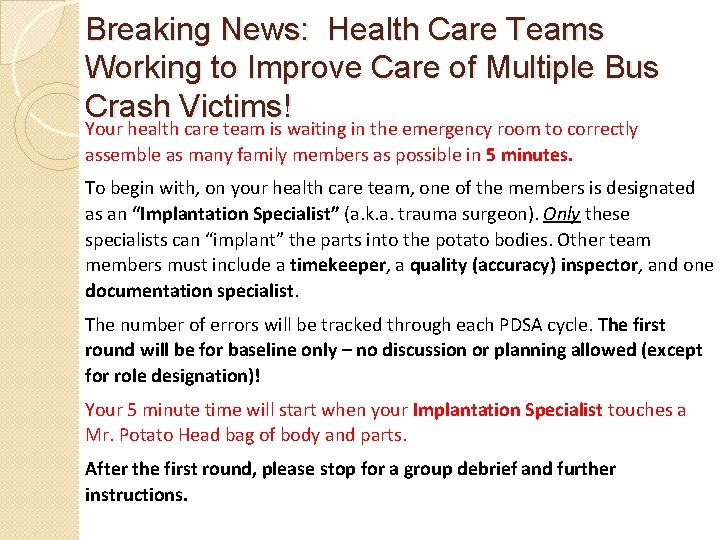
Breaking News: Health Care Teams Working to Improve Care of Multiple Bus Crash Victims! Your health care team is waiting in the emergency room to correctly assemble as many family members as possible in 5 minutes. To begin with, on your health care team, one of the members is designated as an “Implantation Specialist” (a. k. a. trauma surgeon). Only these specialists can “implant” the parts into the potato bodies. Other team members must include a timekeeper, a quality (accuracy) inspector, and one documentation specialist. The number of errors will be tracked through each PDSA cycle. The first round will be for baseline only – no discussion or planning allowed (except for role designation)! Your 5 minute time will start when your Implantation Specialist touches a Mr. Potato Head bag of body and parts. After the first round, please stop for a group debrief and further instructions.
Breaking News: Health Care Teams Working to Improve Care of Multiple Bus Crash Victims! Round 1 – Establishing a baseline Each team will build their first Mr. Potato Heads and record their time and accuracy. This is an important benchmark for what will follow – assembling Mr. Potato Heads as quickly and accurately as possible.
Breaking News: Health Care Teams Working to Improve Care of Multiple Bus Crash Victims! Round 2 – 1 st PDSA Considering your baseline, your team will set out on your first PDSA, agreeing to a theory or a hypothesis for what time and accuracy you can achieve together, BEFORE testing your theory. Record the outcomes in both time and accuracy. Discuss if your hypothesis was confirmed or refuted.
Breaking News: Health Care Teams Working to Improve Care of Multiple Bus Crash Victims! Round 3 – PDSA Cycle Each round, your team should identify a theory or hypothesis that can be tested to improve on accuracy and/or time of the task. Results from each round should be recorded and plotted on your chart. Discuss if your hypothesis was confirmed or refuted.
Debrief �Talk vs Test �Time vs Accuracy �Collaboration �Documentation �Competency �Testing Considerations �Was this an effective method for learning PDSA?
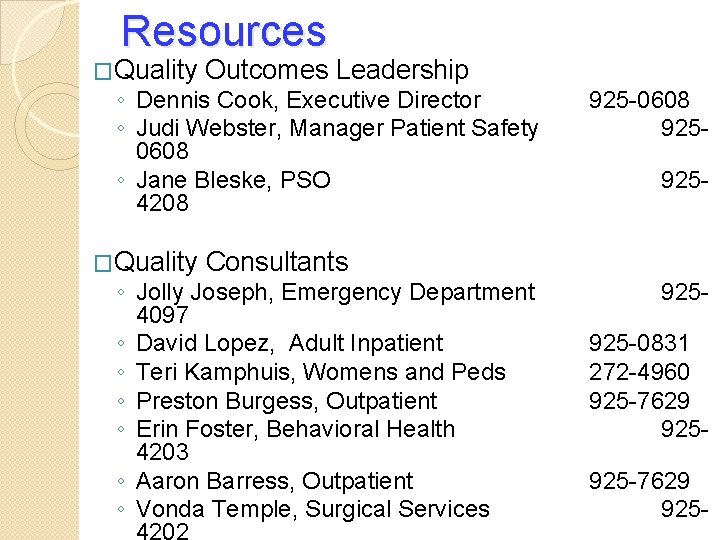
Resources �Quality Outcomes Leadership ◦ Dennis Cook, Executive Director ◦ Judi Webster, Manager Patient Safety 0608 ◦ Jane Bleske, PSO 4208 �Quality 925 -0608 925925 - Consultants ◦ Jolly Joseph, Emergency Department 4097 ◦ David Lopez, Adult Inpatient ◦ Teri Kamphuis, Womens and Peds ◦ Preston Burgess, Outpatient ◦ Erin Foster, Behavioral Health 4203 ◦ Aaron Barress, Outpatient ◦ Vonda Temple, Surgical Services 925925 -0831 272 -4960 925 -7629 925 -
Additional Resources �Office of Quality & Safety �PDSA form ◦ ◦ Quality Central (from intranet Home page) Patient Safety (top tab) Patient Safety Tools (right side) PDSA Template (first choice) https: //hospitals. health. unm. edu/intranet/qc/pt-safetytools. shtml
Questions? Thank you! Please complete your evaluation so we can learn and grow!