Prometheus CIK liver Dr Priya Rogers Dr Katherine

- Slides: 3

Prometheus’ CIK liver Dr Priya Rogers, Dr Katherine Hickman, Dr David Bowden Addenbrooke’s Hospital, Cambridge University Hospitals, Cambridge, UK.
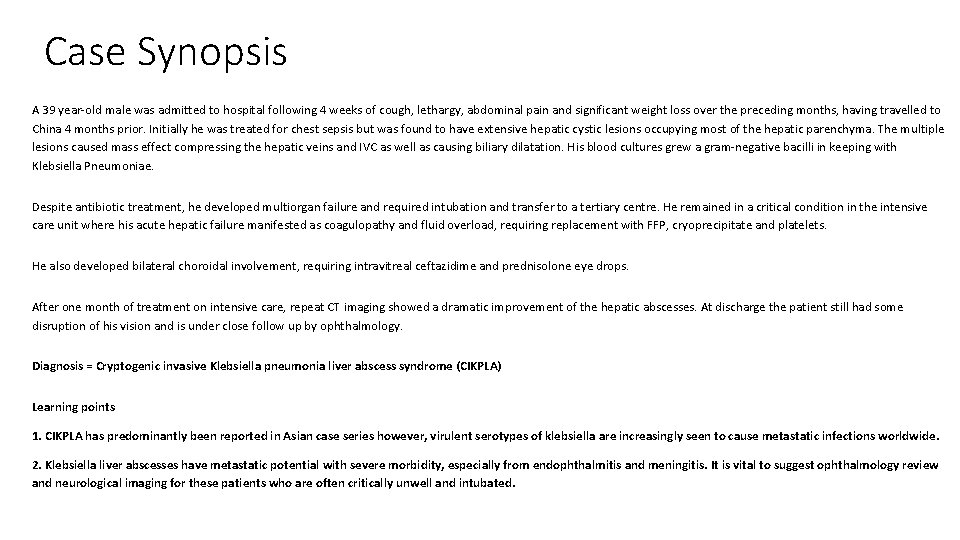
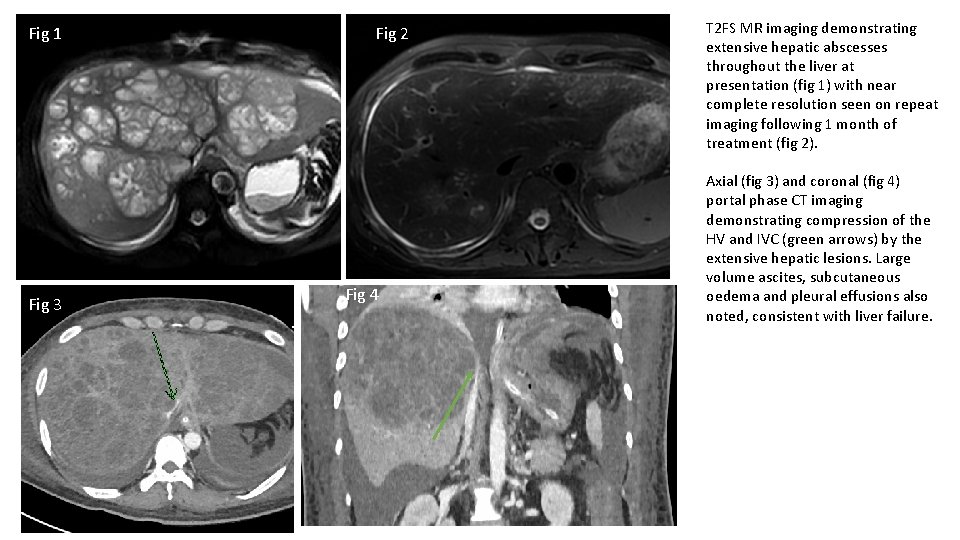
Case Synopsis A 39 year-old male was admitted to hospital following 4 weeks of cough, lethargy, abdominal pain and significant weight loss over the preceding months, having travelled to China 4 months prior. Initially he was treated for chest sepsis but was found to have extensive hepatic cystic lesions occupying most of the hepatic parenchyma. The multiple lesions caused mass effect compressing the hepatic veins and IVC as well as causing biliary dilatation. His blood cultures grew a gram-negative bacilli in keeping with Klebsiella Pneumoniae. Despite antibiotic treatment, he developed multiorgan failure and required intubation and transfer to a tertiary centre. He remained in a critical condition in the intensive care unit where his acute hepatic failure manifested as coagulopathy and fluid overload, requiring replacement with FFP, cryoprecipitate and platelets. He also developed bilateral choroidal involvement, requiring intravitreal ceftazidime and prednisolone eye drops. After one month of treatment on intensive care, repeat CT imaging showed a dramatic improvement of the hepatic abscesses. At discharge the patient still had some disruption of his vision and is under close follow up by ophthalmology. Diagnosis = Cryptogenic invasive Klebsiella pneumonia liver abscess syndrome (CIKPLA) Learning points 1. CIKPLA has predominantly been reported in Asian case series however, virulent serotypes of klebsiella are increasingly seen to cause metastatic infections worldwide. 2. Klebsiella liver abscesses have metastatic potential with severe morbidity, especially from endophthalmitis and meningitis. It is vital to suggest ophthalmology review and neurological imaging for these patients who are often critically unwell and intubated.
Fig 1 Fig 3 Fig 2 Fig 4 T 2 FS MR imaging demonstrating extensive hepatic abscesses throughout the liver at presentation (fig 1) with near complete resolution seen on repeat imaging following 1 month of treatment (fig 2). Axial (fig 3) and coronal (fig 4) portal phase CT imaging demonstrating compression of the HV and IVC (green arrows) by the extensive hepatic lesions. Large volume ascites, subcutaneous oedema and pleural effusions also noted, consistent with liver failure.