Prolonged Disorders of Consciousness A Wake Up Call


![Vegetative State [European : Unresponsive Wakefulness Syndrome(UWS) ; apallic syndrome] Usually: • Breathe spontaneously Vegetative State [European : Unresponsive Wakefulness Syndrome(UWS) ; apallic syndrome] Usually: • Breathe spontaneously](https://slidetodoc.com/presentation_image_h/274f4e3714644d38fb821dcacaec2c0e/image-16.jpg)








- Slides: 43
Prolonged Disorders of Consciousness A Wake Up Call
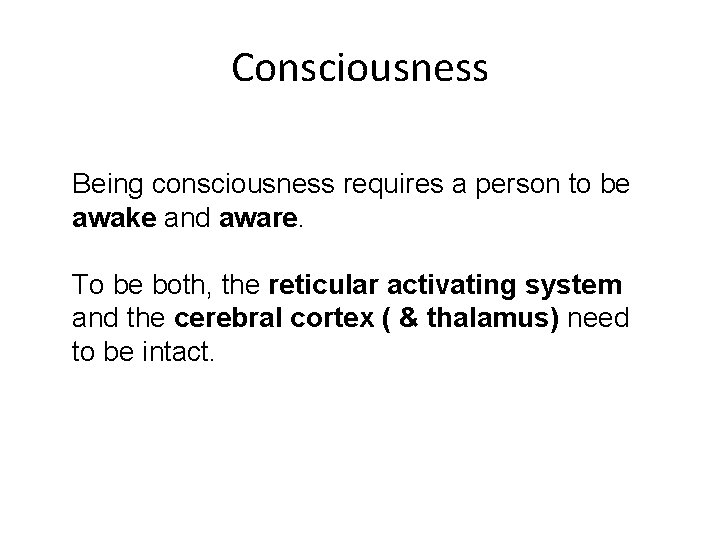
Consciousness • No clear agreed definition by neuroscientists • Generally accepted 2 components – Wakefulness – Awareness
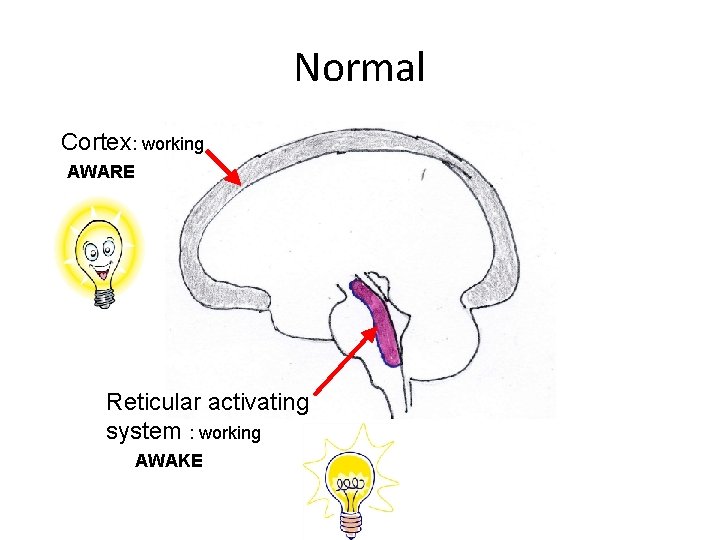
Neural Basis of Consciousness Reticular activating system in brain stem Cerebral cortex Thalamus AWAKE AWARE
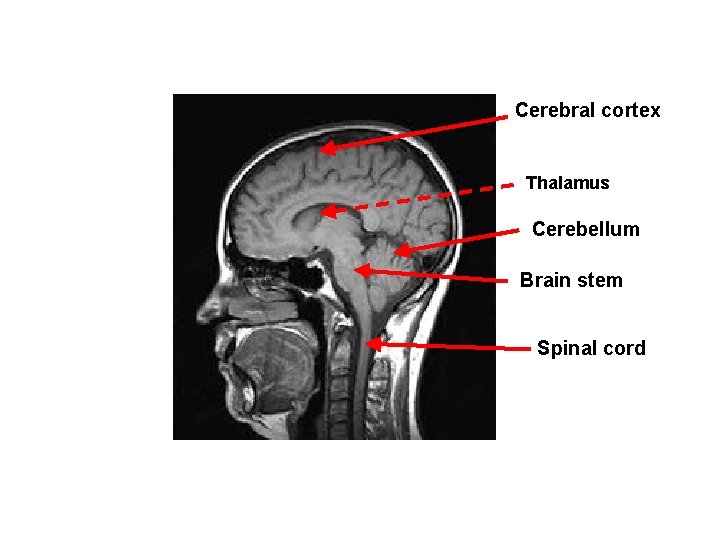
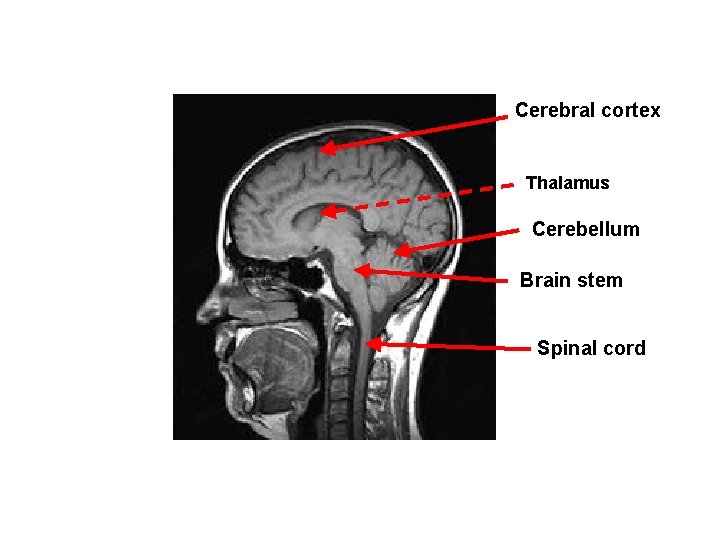
Cerebral cortex Thalamus Cerebellum Brain stem Spinal cord

Normal Cortex: working AWARE Reticular activating system : working AWAKE
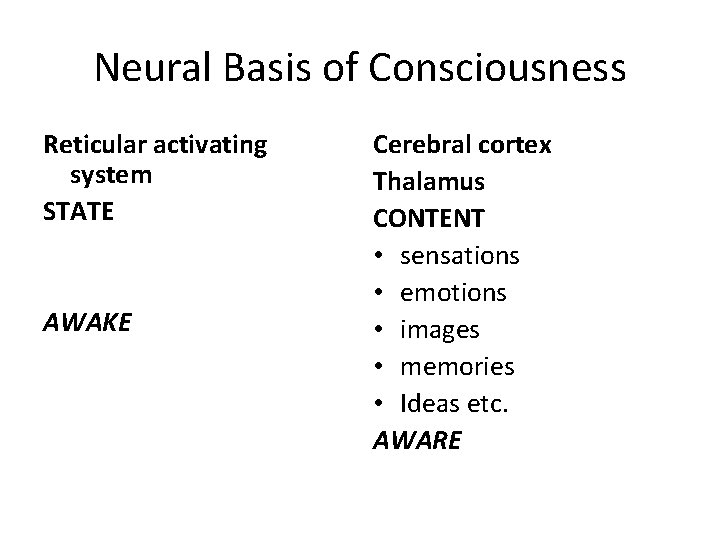
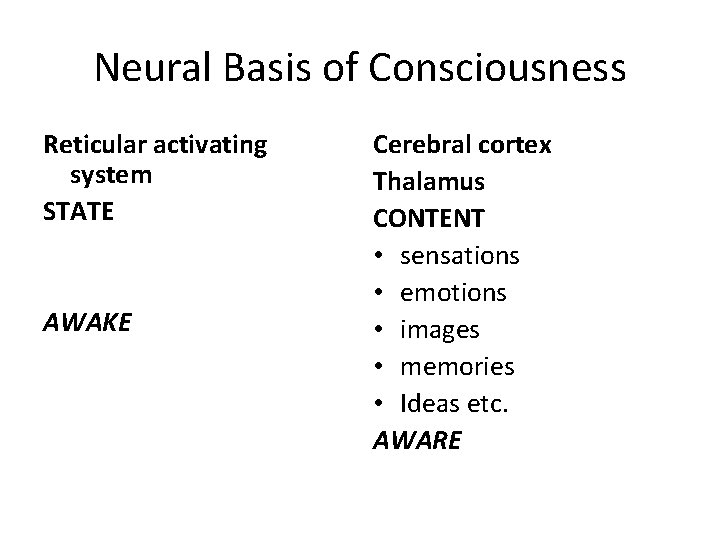
Neural Basis of Consciousness Reticular activating system STATE AWAKE Cerebral cortex Thalamus CONTENT • sensations • emotions • images • memories • Ideas etc. AWARE
Disturbance of consciousness

Common terms • Sleep: a state of reduced responsiveness to, and interaction with, the environment which is readily reversible • Confusional state: minor disorientation, faulty memory, short attention span, some difficulty following commands • Delirium: disorientation, irritability, restlessness, hallucinations • Stupor: unresponsive & only aroused by vigorous stimulation • Coma: unresponsive & unrousable
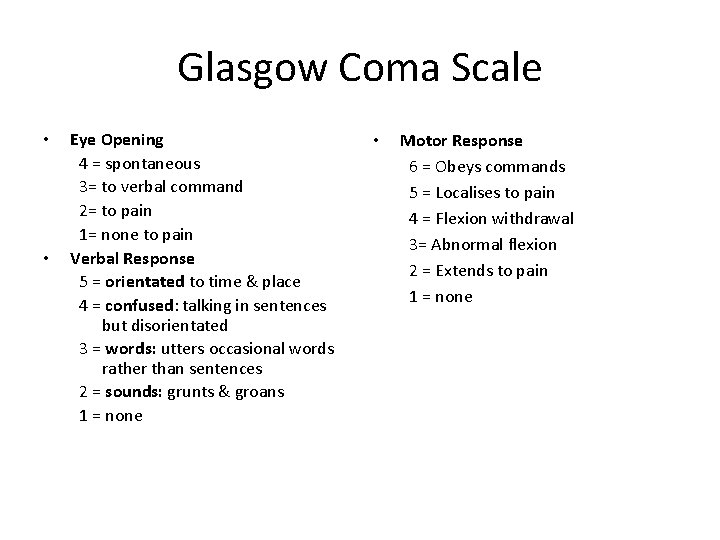
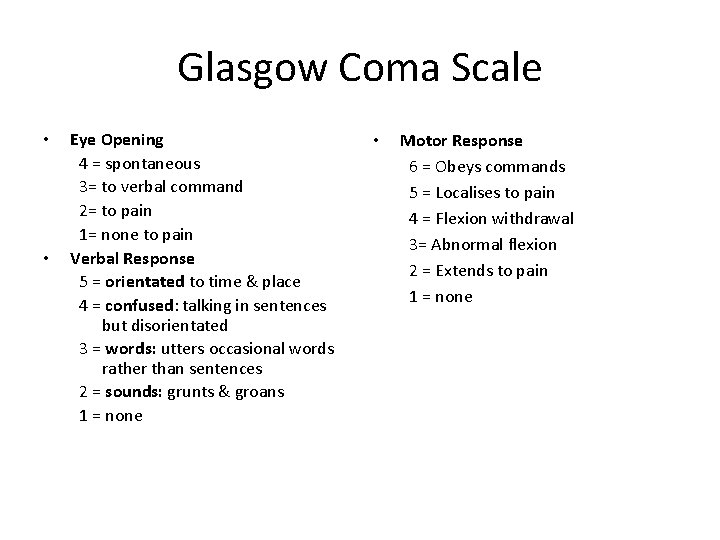
Glasgow Coma Scale • • Eye Opening 4 = spontaneous 3= to verbal command 2= to pain 1= none to pain Verbal Response 5 = orientated to time & place 4 = confused: talking in sentences but disorientated 3 = words: utters occasional words rather than sentences 2 = sounds: grunts & groans 1 = none • Motor Response 6 = Obeys commands 5 = Localises to pain 4 = Flexion withdrawal 3= Abnormal flexion 2 = Extends to pain 1 = none
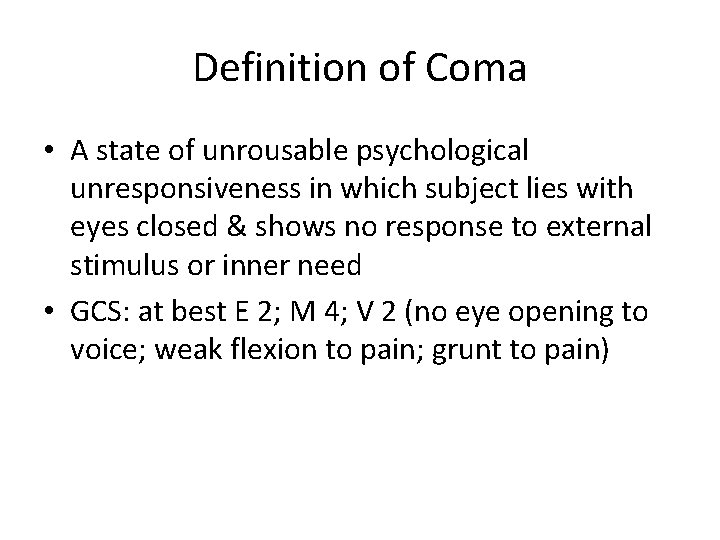
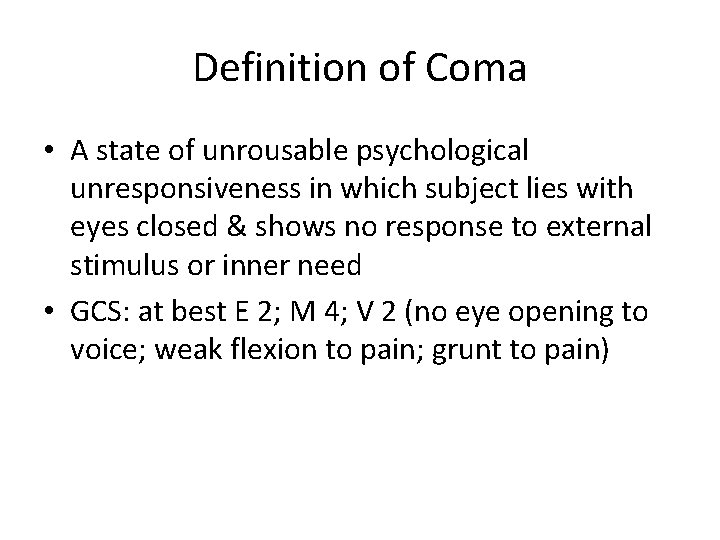
Definition of Coma • A state of unrousable psychological unresponsiveness in which subject lies with eyes closed & shows no response to external stimulus or inner need • GCS: at best E 2; M 4; V 2 (no eye opening to voice; weak flexion to pain; grunt to pain)
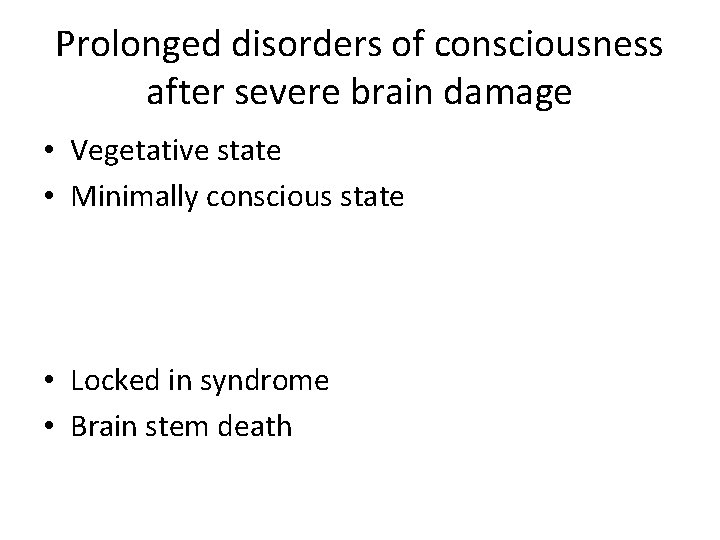
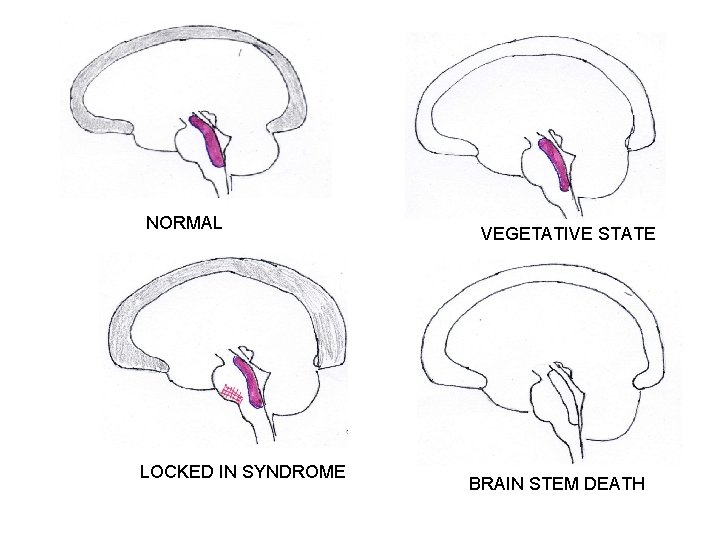
Prolonged disorders of consciousness after severe brain damage • Vegetative state • Minimally conscious state • Locked in syndrome • Brain stem death
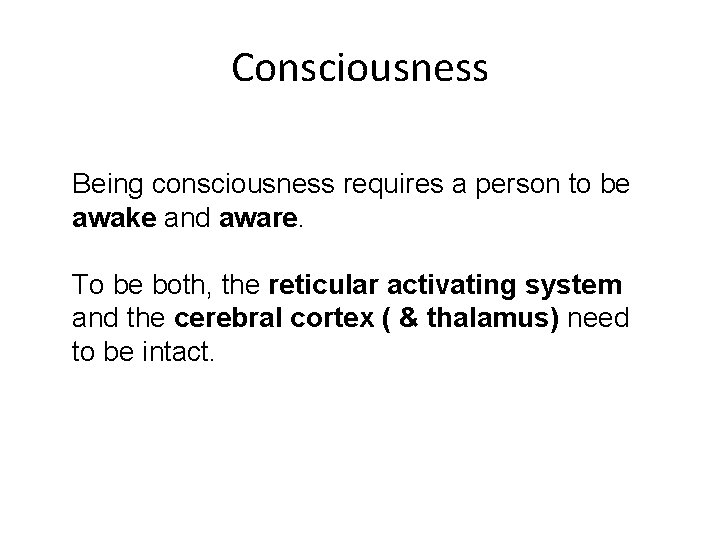
Consciousness Being consciousness requires a person to be awake and aware. To be both, the reticular activating system and the cerebral cortex ( & thalamus) need to be intact.
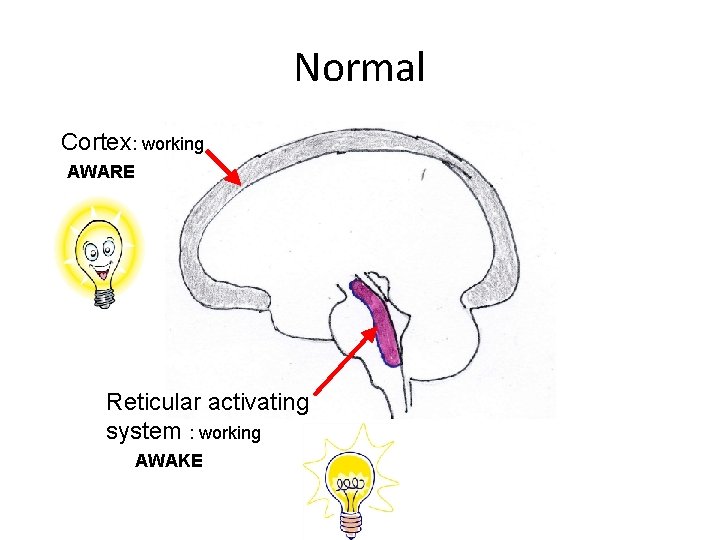
Normal Cortex: working AWARE Reticular activating system : working AWAKE
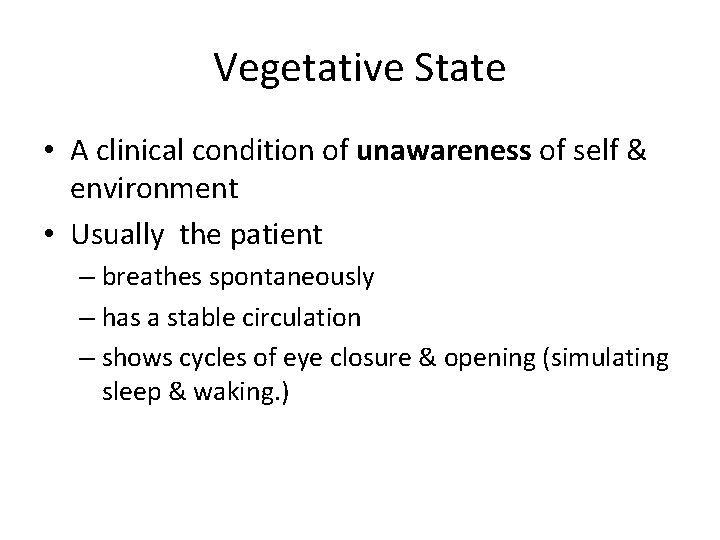
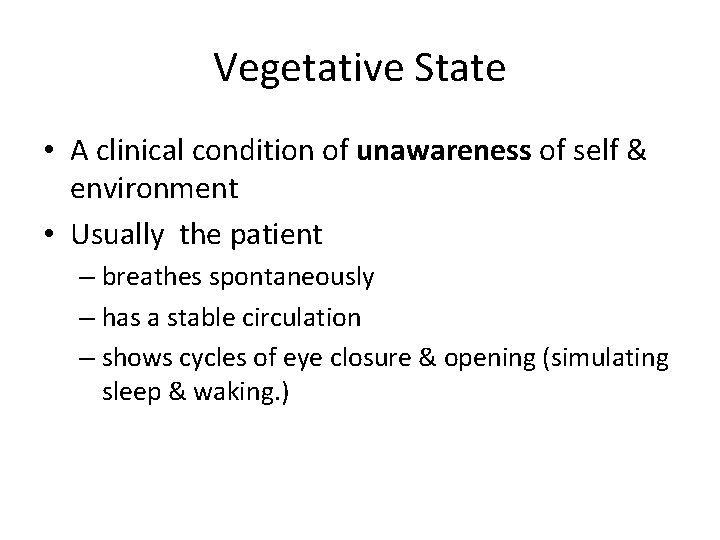
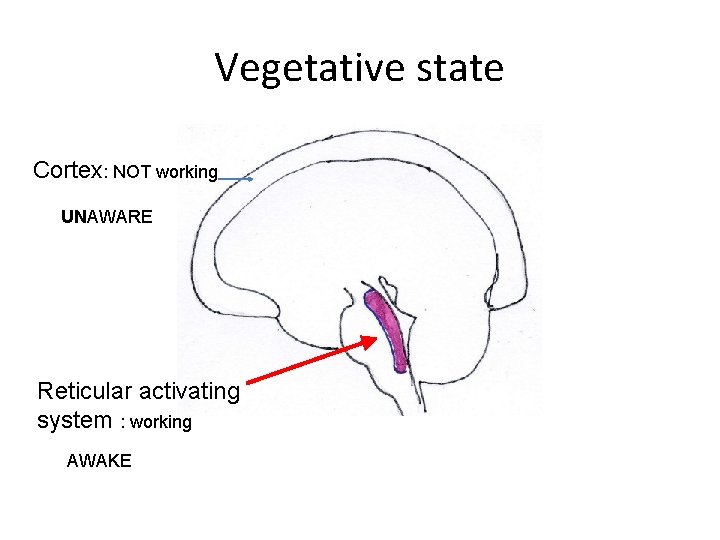
Vegetative State • A clinical condition of unawareness of self & environment • Usually the patient – breathes spontaneously – has a stable circulation – shows cycles of eye closure & opening (simulating sleep & waking. )
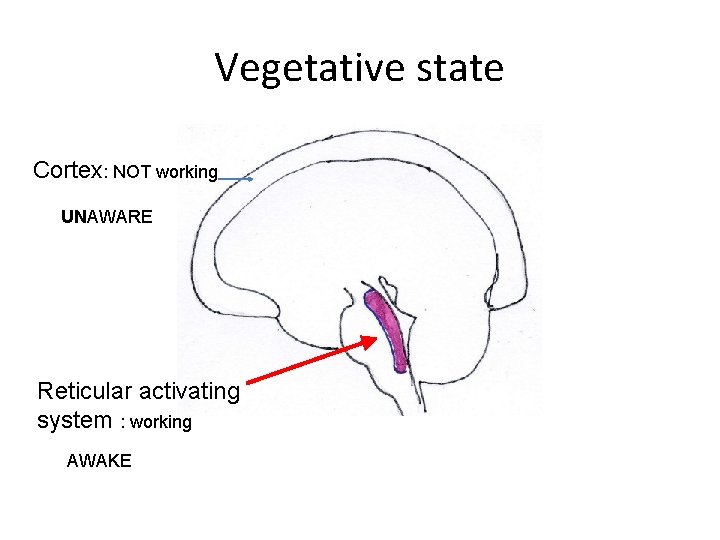
Vegetative state Cortex: NOT working UNAWARE Reticular activating system : working AWAKE
![Vegetative State European Unresponsive Wakefulness SyndromeUWS apallic syndrome Usually Breathe spontaneously Vegetative State [European : Unresponsive Wakefulness Syndrome(UWS) ; apallic syndrome] Usually: • Breathe spontaneously](https://slidetodoc.com/presentation_image_h/274f4e3714644d38fb821dcacaec2c0e/image-16.jpg)
Vegetative State [European : Unresponsive Wakefulness Syndrome(UWS) ; apallic syndrome] Usually: • Breathe spontaneously • Stable circulation • Cycles of eye closure/opening (like sleep/wake)

Observed Behaviours during VEGETATIVE STATE • • • Chewing; teeth grinding; tongue pumping Roving eye movements Non-purposeful limb movements Facial movements (e. g. smiles or grimaces) Shedding tears Grunts or groans
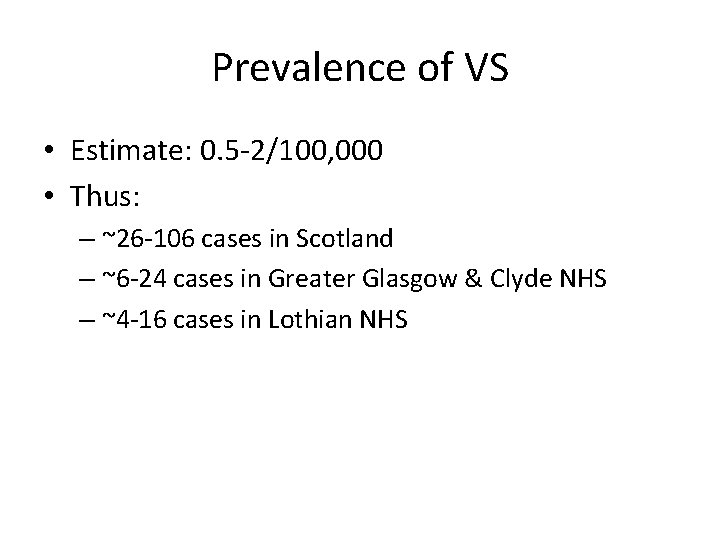
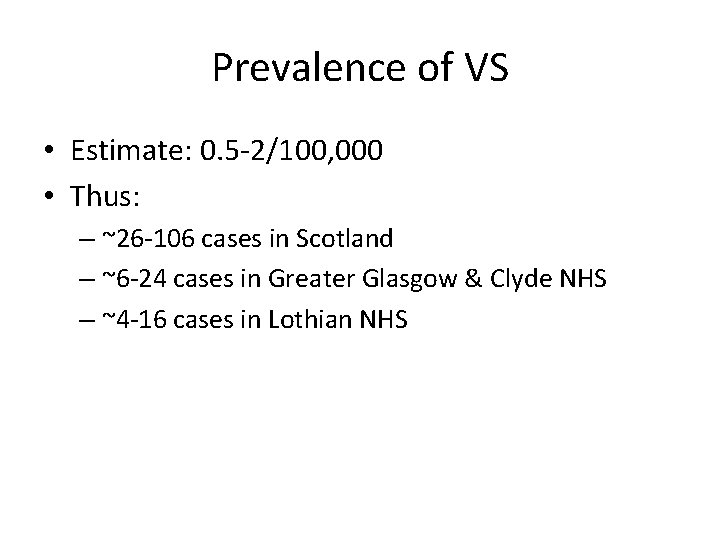
Prevalence of VS • Estimate: 0. 5 -2/100, 000 • Thus: – ~26 -106 cases in Scotland – ~6 -24 cases in Greater Glasgow & Clyde NHS – ~4 -16 cases in Lothian NHS

Minimally Conscious State One or more of following – follows simple commands – gestural or verbal yes/no responses – intelligible verbalization – stereotypical movements (e. g. blink, smile) in meaningful relationship to the eliciting stimulus & not reflexive – manipulation of objects
Minimally Conscious State(MCS) Crying, smiling, laughing in response to emotional stimuli Vocalisation or gestures to comments/questions Reaching for objects Touching/holding objects in a manner that accommodates the size & shape of object • Sustained fixation or pursuit eye movements in direct response to stimuli • Other localising or discriminating behaviours that constitute: • • – Movement towards a perceived object – Differential responses to different objects or people

Emergence from MCS Responses become RELIABLE & CONSISTENT • Functional Communication: verbal, written , using augmentative communication device ; or yes/no signals. +/or • Functional use of objects: discrimination between at least 2 different objects
Assessment tools • JFK Coma Recovery Scale-Revised (CRS-R) • Wessex Head Injury Matrix (WHIM) • Sensory Modality Assessment and Rehabilitation Technique (SMART) • Western Neuro Sensory Stimulation Profile (WNSSP) • Sensory Stimulation Assessment Measure (SSAM) • Disorders of Consciousness Scale (DOCS)
Investigative techniques • Functional MRI (f. MRI) scans • Electrophysiology – Sleep EEG – Evoked potentials

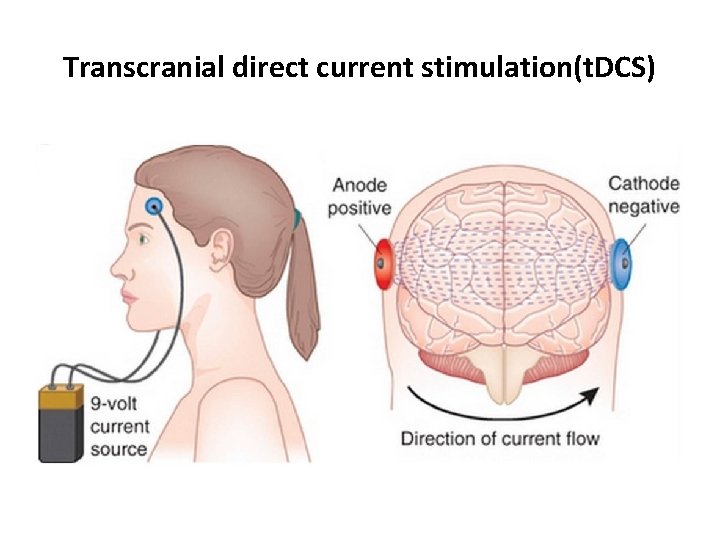
Treatment approaches • Medications: – Amantadine – Zolpidem – Methylphenidate • Neurostimulation: – Deep brain stimulation – Transcranial magnetic stimulation – Transcranial direct current stimulation • Sensory stimulation (Coma arousal programmes)

Deep brain stimulation (DBS)

Transcranial magnetic stimulation(TMS)
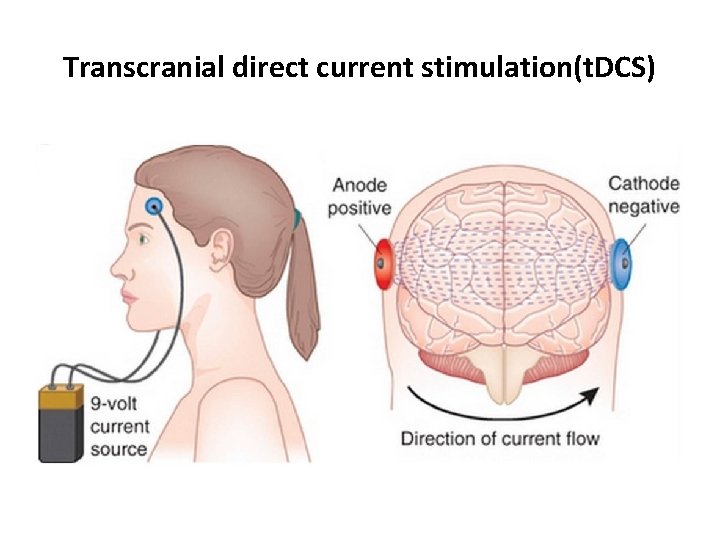
Transcranial direct current stimulation(t. DCS)
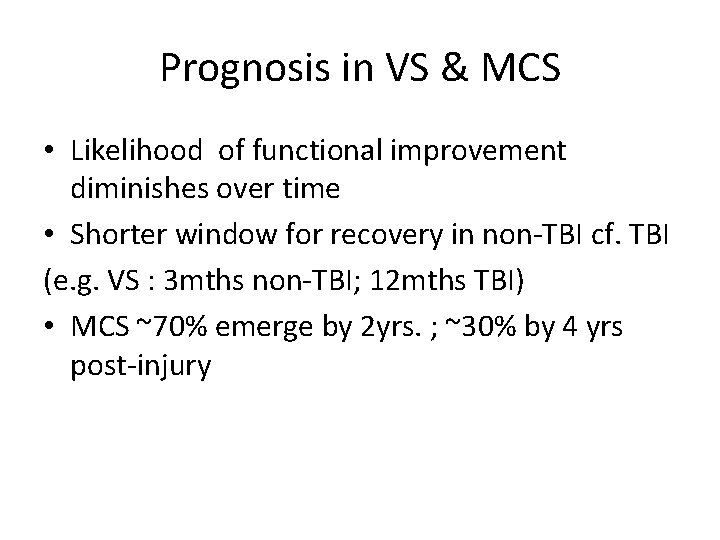
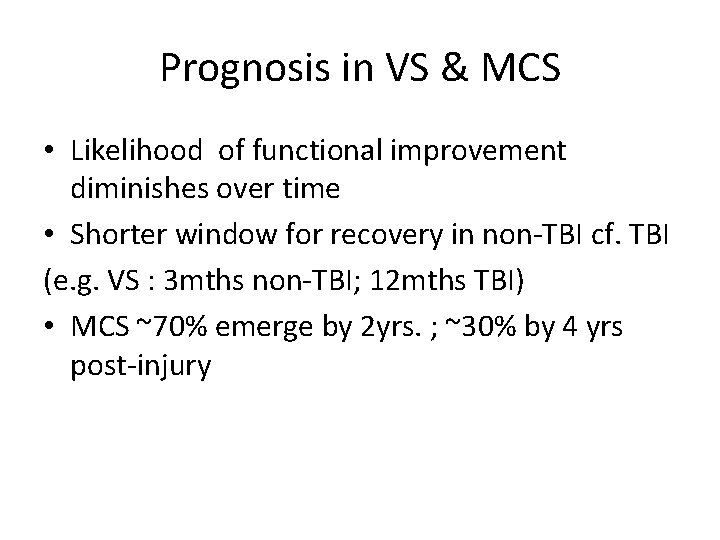
Prognosis in VS & MCS • Likelihood of functional improvement diminishes over time • Shorter window for recovery in non-TBI cf. TBI (e. g. VS : 3 mths non-TBI; 12 mths TBI) • MCS ~70% emerge by 2 yrs. ; ~30% by 4 yrs post-injury
Permanent Vegetative State • > 6 months after non-traumatic brain injury • > 1 year after traumatic brain injury
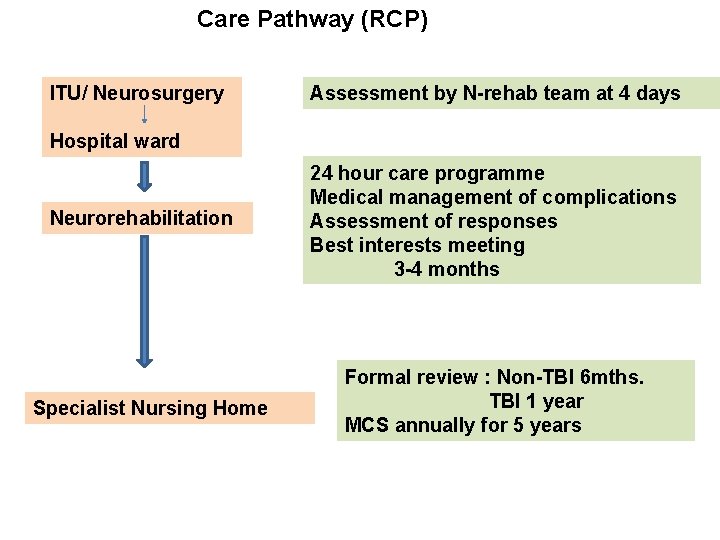
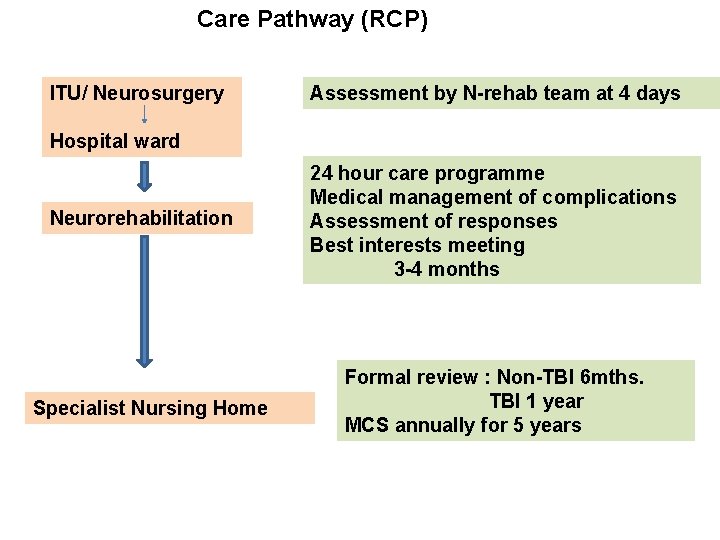
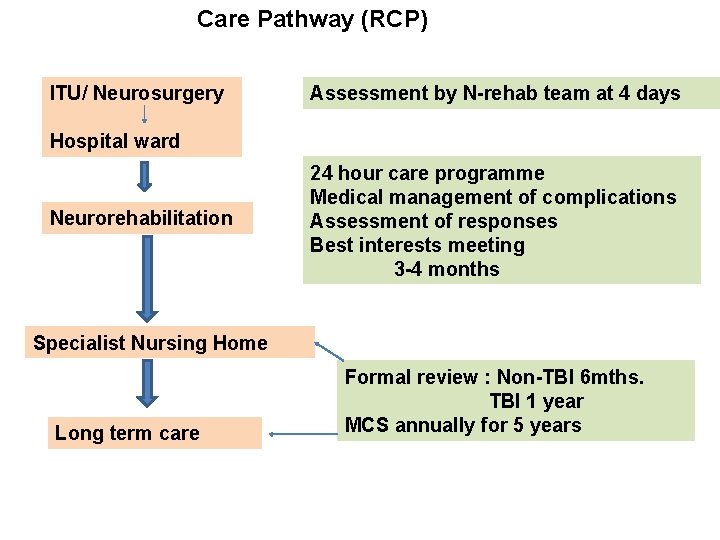
Care Pathway (RCP) ITU/ Neurosurgery Assessment by N-rehab team at 4 days Hospital ward Neurorehabilitation Specialist Nursing Home 24 hour care programme Medical management of complications Assessment of responses Best interests meeting 3 -4 months Formal review : Non-TBI 6 mths. TBI 1 year MCS annually for 5 years
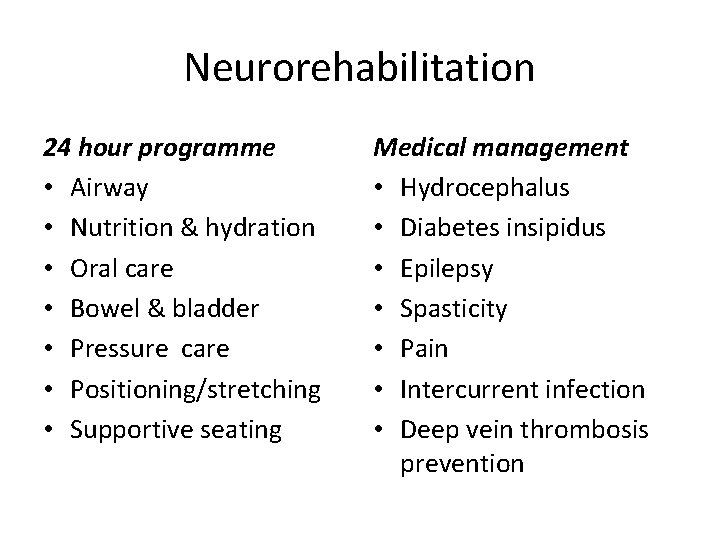
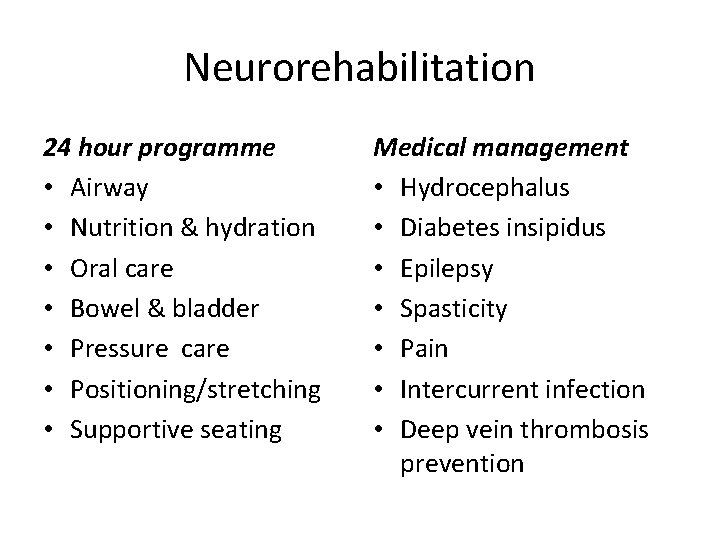
Neurorehabilitation 24 hour programme • Airway • Nutrition & hydration • Oral care • Bowel & bladder • Pressure care • Positioning/stretching • Supportive seating Medical management • Hydrocephalus • Diabetes insipidus • Epilepsy • Spasticity • Pain • Intercurrent infection • Deep vein thrombosis prevention

Neurorehabilitation (Cont. ) • Assessment of responses • Family communication re: diagnosis & prognosis • Best interest meeting – Resuscitation – Use of antibiotics etc. • Discharge planning
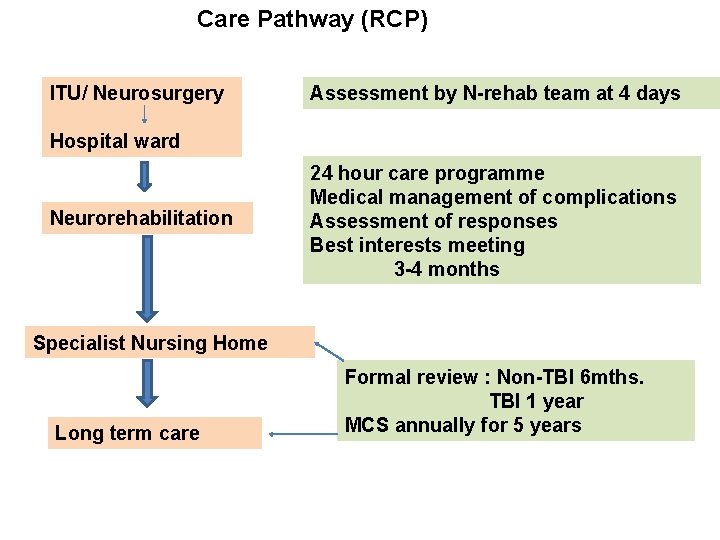
Care Pathway (RCP) ITU/ Neurosurgery Assessment by N-rehab team at 4 days Hospital ward Neurorehabilitation 24 hour care programme Medical management of complications Assessment of responses Best interests meeting 3 -4 months Specialist Nursing Home Long term care Formal review : Non-TBI 6 mths. TBI 1 year MCS annually for 5 years
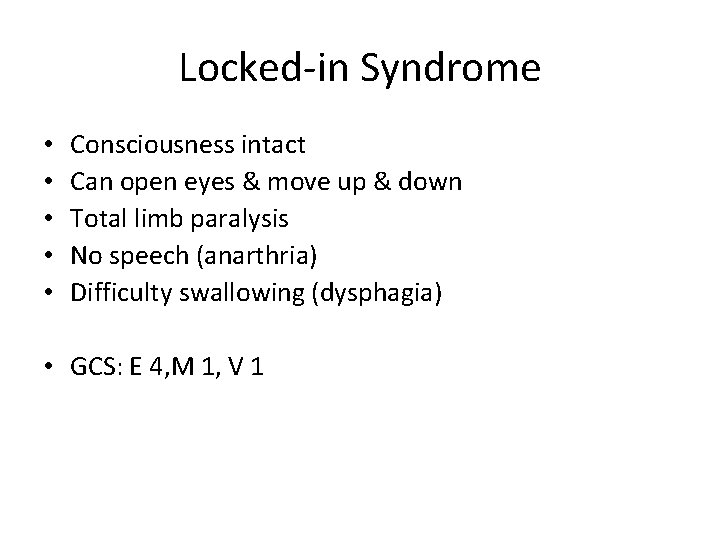
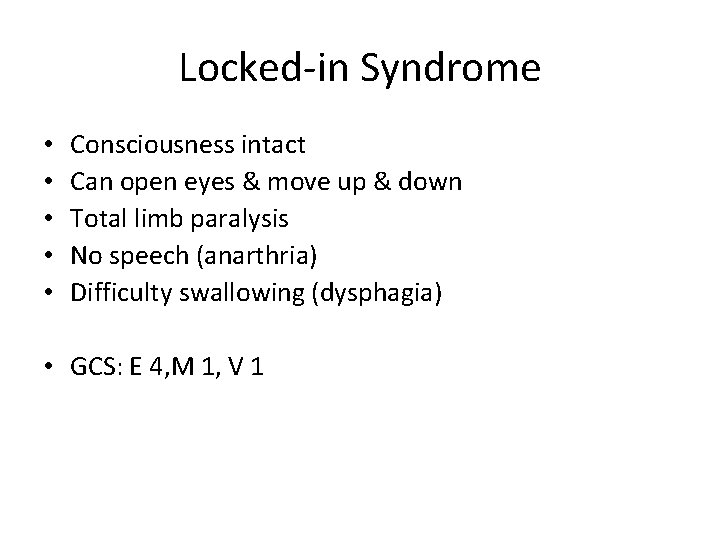
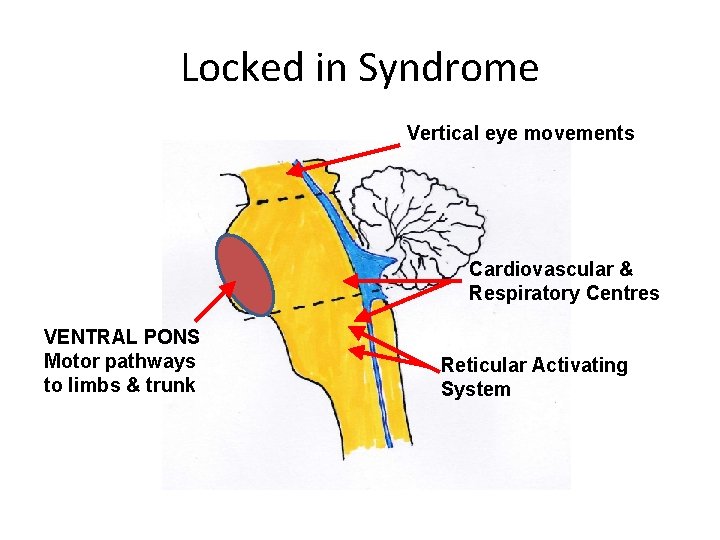
Locked-in Syndrome • • • Consciousness intact Can open eyes & move up & down Total limb paralysis No speech (anarthria) Difficulty swallowing (dysphagia) • GCS: E 4, M 1, V 1
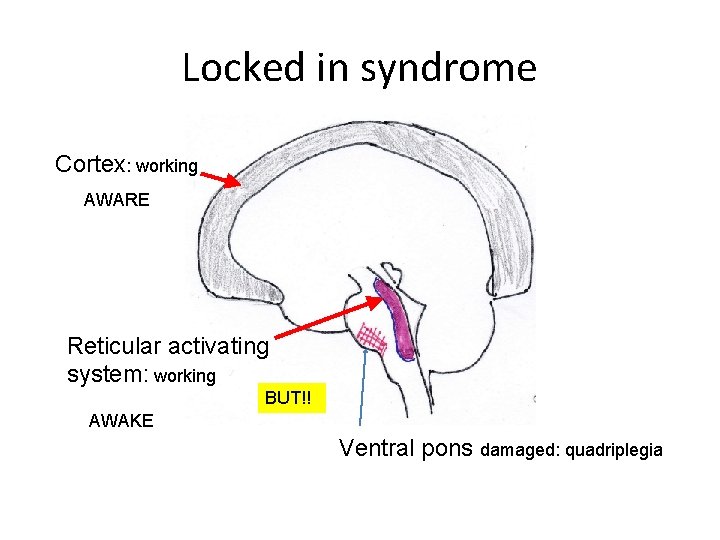
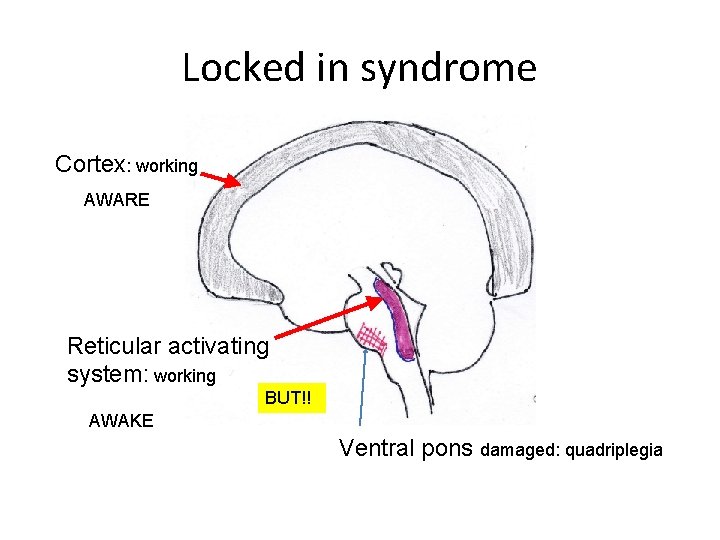
Locked in syndrome Cortex: working AWARE Reticular activating system: working BUT!! AWAKE Ventral pons damaged: quadriplegia
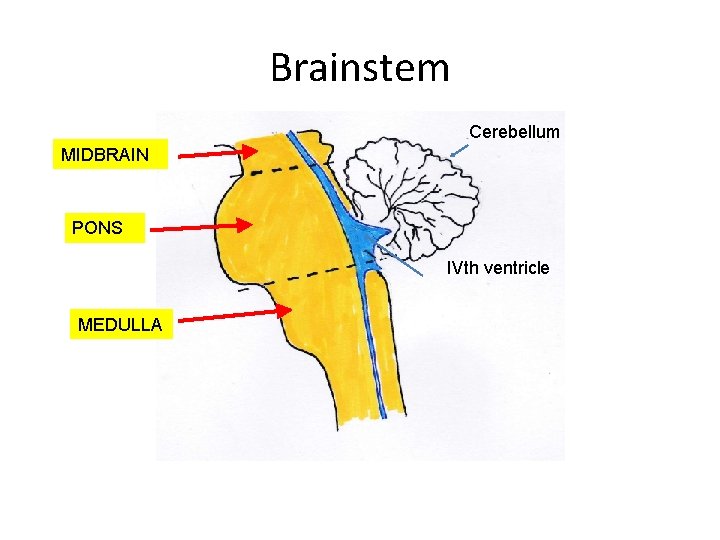
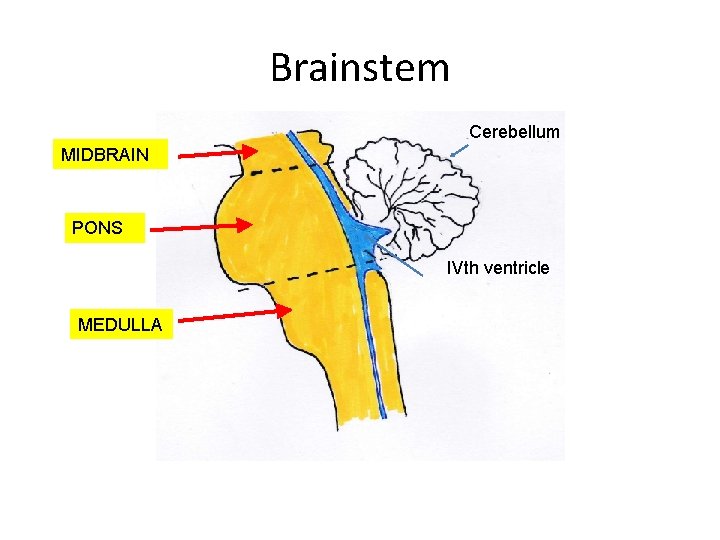
Brainstem Cerebellum MIDBRAIN PONS IVth ventricle MEDULLA
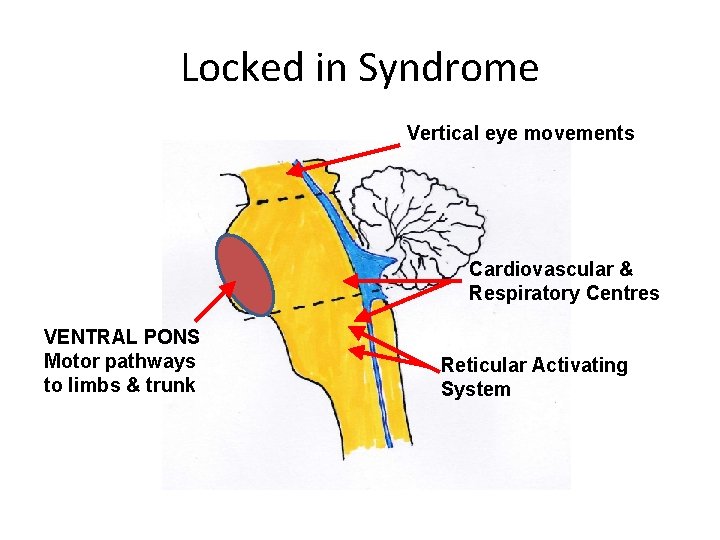
Locked in Syndrome Vertical eye movements Cardiovascular & Respiratory Centres VENTRAL PONS Motor pathways to limbs & trunk Reticular Activating System
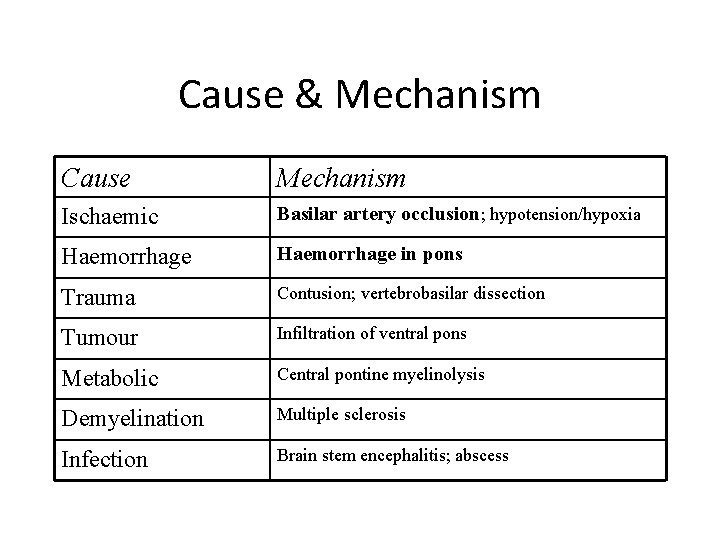
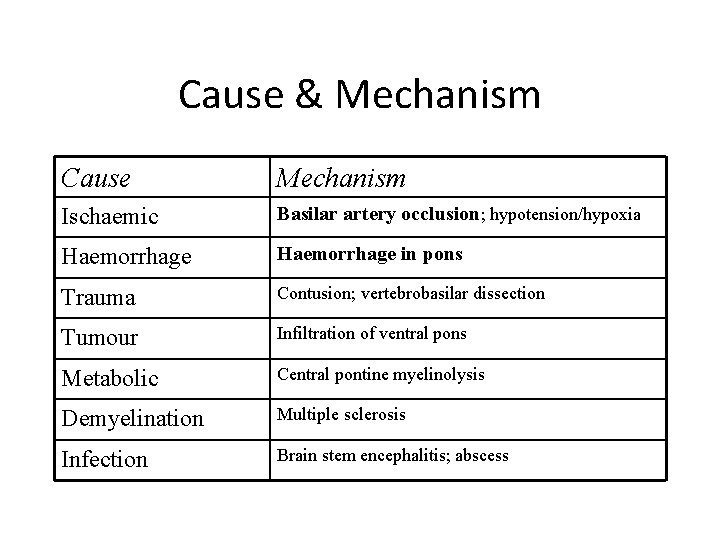
Cause & Mechanism Cause Mechanism Ischaemic Basilar artery occlusion; hypotension/hypoxia Haemorrhage in pons Trauma Contusion; vertebrobasilar dissection Tumour Infiltration of ventral pons Metabolic Central pontine myelinolysis Demyelination Multiple sclerosis Infection Brain stem encephalitis; abscess
Brain stem death 1. Irremediable brain damage of known cause 2. Deep coma: effects of drugs & potentially reversible metabolic/endocrine disturbances excluded 3. Ventilator dependent
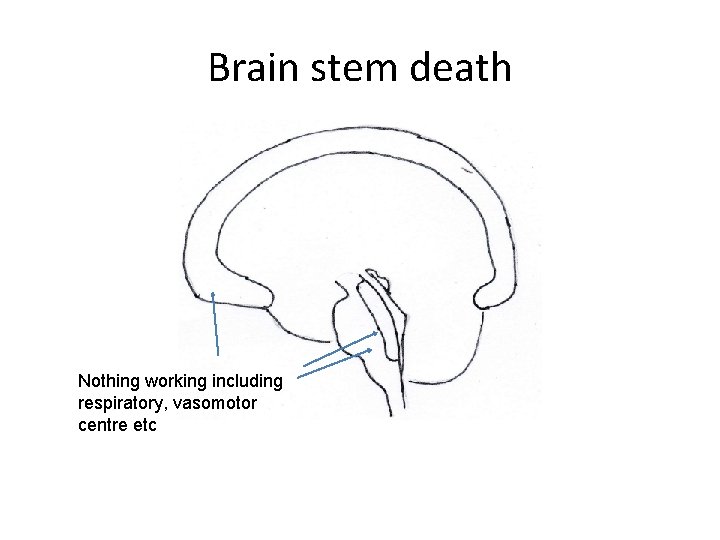
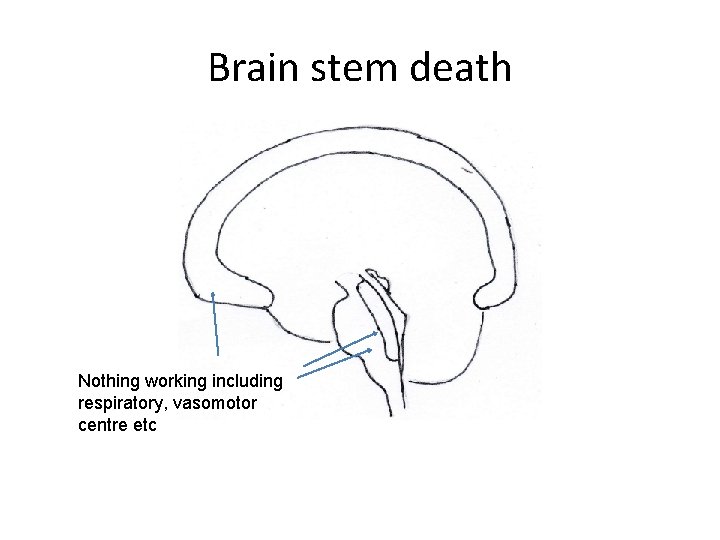
Brain stem death Nothing working including respiratory, vasomotor centre etc
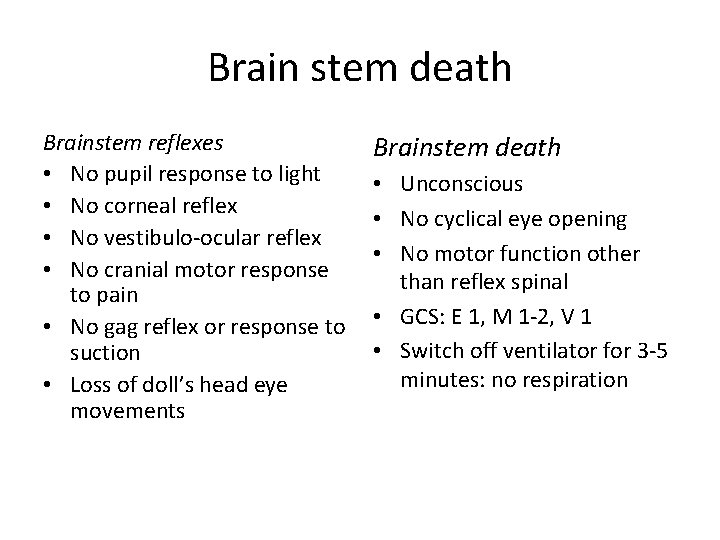
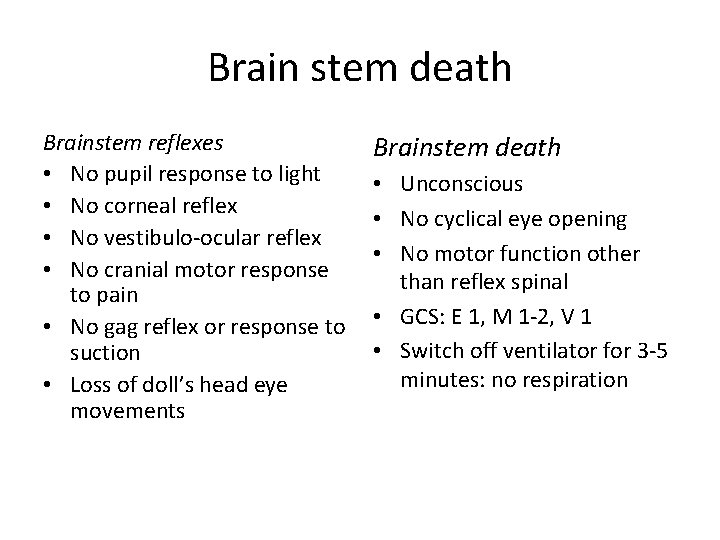
Brain stem death Brainstem reflexes • No pupil response to light • No corneal reflex • No vestibulo-ocular reflex • No cranial motor response to pain • No gag reflex or response to suction • Loss of doll’s head eye movements Brainstem death • Unconscious • No cyclical eye opening • No motor function other than reflex spinal • GCS: E 1, M 1 -2, V 1 • Switch off ventilator for 3 -5 minutes: no respiration
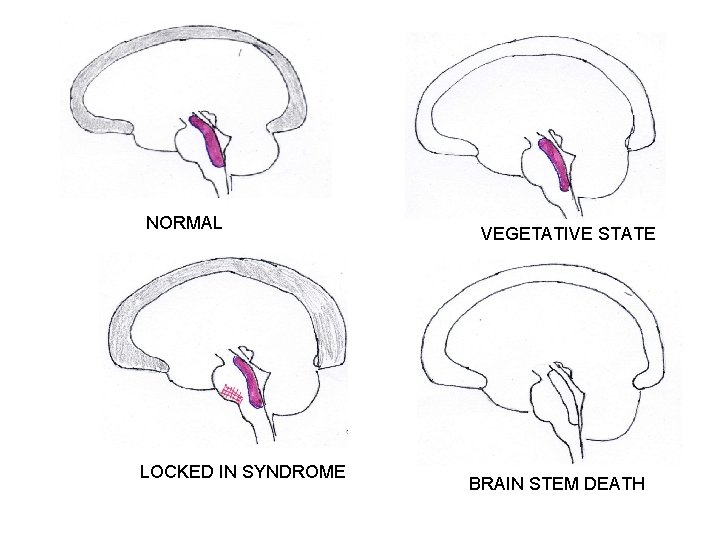
NORMAL LOCKED IN SYNDROME VEGETATIVE STATE BRAIN STEM DEATH

 Class consciousness vs false consciousness
Class consciousness vs false consciousness Bleeding time test procedure
Bleeding time test procedure Second stage of labor
Second stage of labor Obstructed labour causes
Obstructed labour causes Extended metaphor about family
Extended metaphor about family Prolonged pt
Prolonged pt Pt aptt
Pt aptt Box spread
Box spread Long call short call
Long call short call Gartner call recording magic quadrant
Gartner call recording magic quadrant Wake turbulence avoidance
Wake turbulence avoidance Why does nwakibie trust okonkwo to farm his yam seeds?
Why does nwakibie trust okonkwo to farm his yam seeds? Sail strung
Sail strung Waiting line manament
Waiting line manament Wake turbulence avoidance
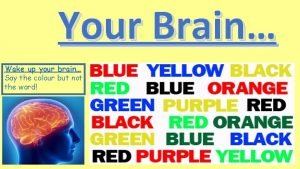
Wake turbulence avoidance Wake up my brain
Wake up my brain Wake forest symplicity
Wake forest symplicity Eog grading scale 1-5 nc
Eog grading scale 1-5 nc Vanderbilt neurology residents
Vanderbilt neurology residents Sleeping in my orchard a serpent stung me
Sleeping in my orchard a serpent stung me Everyday activities esl
Everyday activities esl Did paris love juliet give evidence
Did paris love juliet give evidence A lion laughing
A lion laughing Aig wake county
Aig wake county Karl bane
Karl bane True terror is to wake up
True terror is to wake up Simple present verbs
Simple present verbs Wake tech orientation
Wake tech orientation Wake forest opcd
Wake forest opcd Wake up past simple form
Wake up past simple form Wake up london
Wake up london Wake turbulence
Wake turbulence The wake-sleep algorithm for unsupervised neural networks
The wake-sleep algorithm for unsupervised neural networks Keep the soul alive
Keep the soul alive Icao doc 9966
Icao doc 9966 Wake tech data science
Wake tech data science Wakebi
Wakebi Bill wake
Bill wake Wake county economic development
Wake county economic development Deink en pasado simple
Deink en pasado simple Wake tech business analytics
Wake tech business analytics Wake sleep
Wake sleep Wake county ems membership
Wake county ems membership Get up verb 2
Get up verb 2