Programme 1 Hematological malignancies acute leukemias lymphomas 2


- Slides: 64
Programme 1. Hematological malignancies: acute leukemias, lymphomas 2. Solid tumors, part I: Brain tumors, neuroblastoma, Wilms tumor, hepatoblastoma, germ cell tumors 3. Solid tumors, part II: soft tissue sarcomas, osteosarcoma, Ewing sarcoma, late effects after anticancer treatment 4. Anaemias 5. Coagulation disorders
Pediatric oncology and hematology Hematological malignancies: n Acute lymphoblastic leukemia n Acute non-lymphoblastic (myeloblastic) leukemia n Non-Hodgkin lymphoma n Hodgkin lymphoma
Childhood leukemia
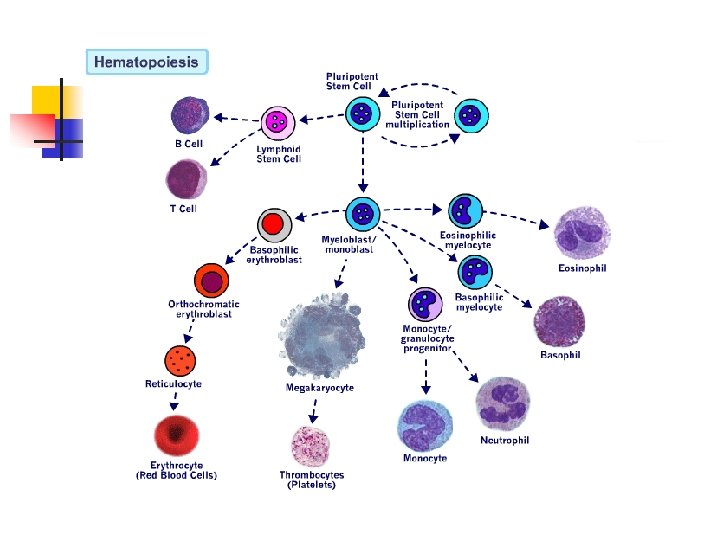
n n n Uncontrolled proliferation of immature blood cells with a different immunological subtypes which is lethal within 1 – 6 months without treatment The disorder starts in the bone marrow, where normal blood cells are replaced by leukemic cells Morphological (FAB), immunological, cytogenetic, biochemical, and molecular genetic factors characterize the subtypes with various response to treatment
Incidence n n Most frequent neoplasm in children (28 – 33%) 45/ 1 million children under the age of 16 years Incidence peak at 2 – 5 years 75 -80%- acute lymphoblastic leukemia -ALL 15 -20% - acute myelogenous (non-lymphoblastic) leukemia AML/ ANLL <5% - undifferentiated acute leukemia and chronic myelogenous leukemia -CML
Ethiology n n Unknown Higher risk in congenital disorders: -trisomy 21 (14 times higher) and other trisomies -Turner syndrome -Klinefelter syndrome -monosomy 7 -neurofibromatosis type 1 -Fanconi anemia (high fragility of chromosomes) -Bloom syndrome, Kostmann S. , Shwachman-Diamond S. , -ataxia- teleangiectasia -congenital agammaglobulinemia -Wiskott- Aldrich S.
n n Ionizing radiation (atomic bomb developed high incidence of leukemia) Chemical and drugs: -benzene -chloramphenicol -alkylating agents Infection (viral –HTLV, EBV, HIV) Immunodeficiency: agamma/hypogammaglobulinemia, Wiskott-Aldrich S, HIV infection
Acute lymphoblastic leukemia n n 80% of leukemias Girl – to- boy ratio is 1: 1. 2 Peak incidence 2 – 5 years Incidence in white children is twice as high as in nonwhite children
Clinical manifestation n 1. General aspects: - history and symptoms reflect: the degree of bone marrow infiltration by leukemic cells and 2. the extramedullary involvement of the disease - the duration of symptoms is days to several weeks, occasionally – several months - often: low –grade fever, signs of infection, fatigue, bleeding, pallor
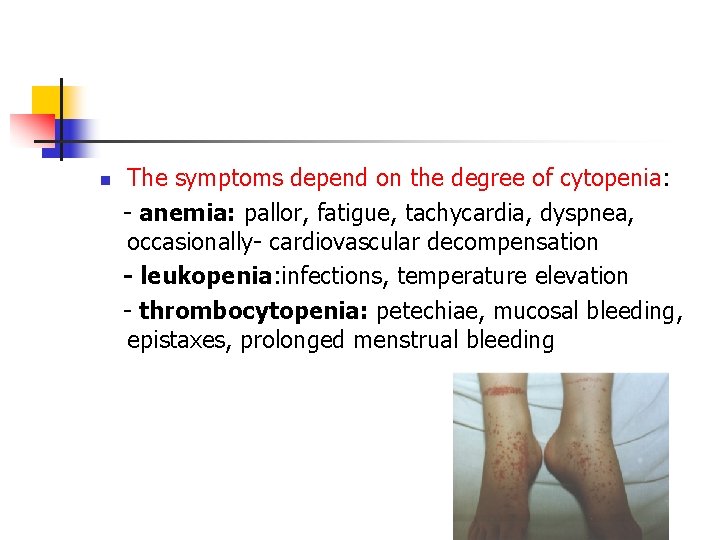
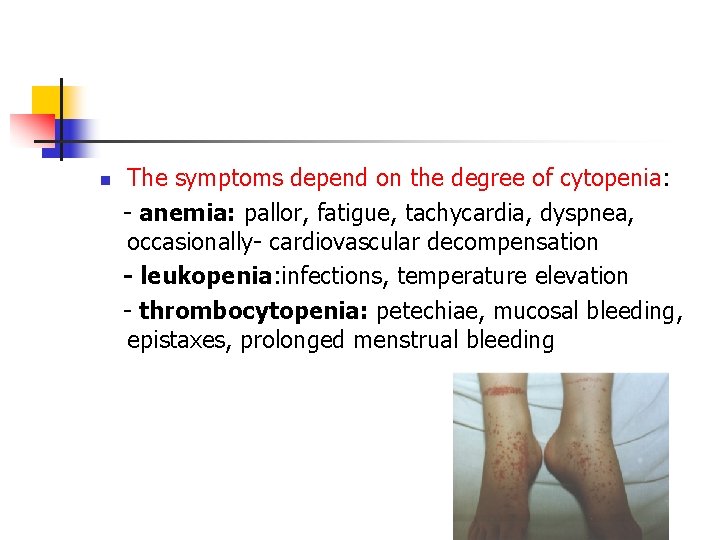
n The symptoms depend on the degree of cytopenia: - anemia: pallor, fatigue, tachycardia, dyspnea, occasionally- cardiovascular decompensation - leukopenia: infections, temperature elevation - thrombocytopenia: petechiae, mucosal bleeding, epistaxes, prolonged menstrual bleeding
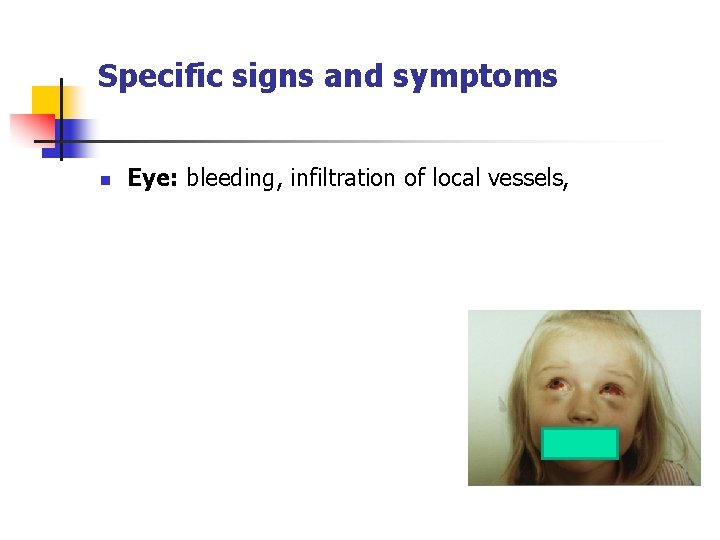
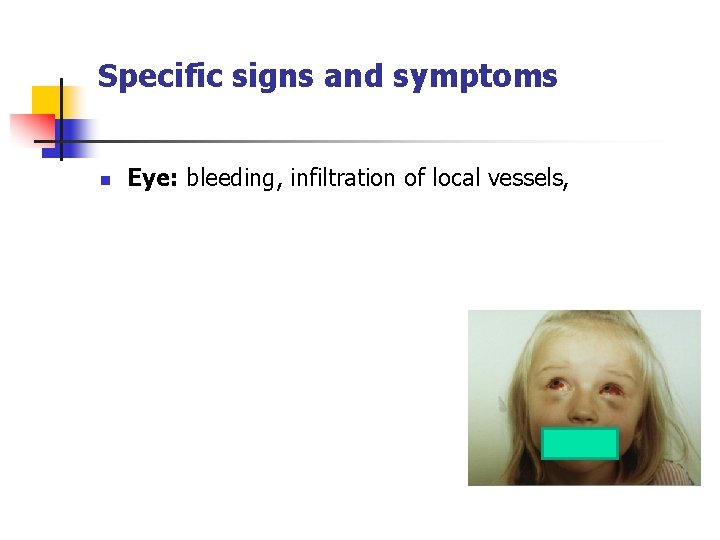
Specific signs and symptoms n Eye: bleeding, infiltration of local vessels,
CNS: at time of diagnosis less than 5% have CNS leukemia with meningeal signs (morning headache, vomiting, papilla edema, focal neurological signs)
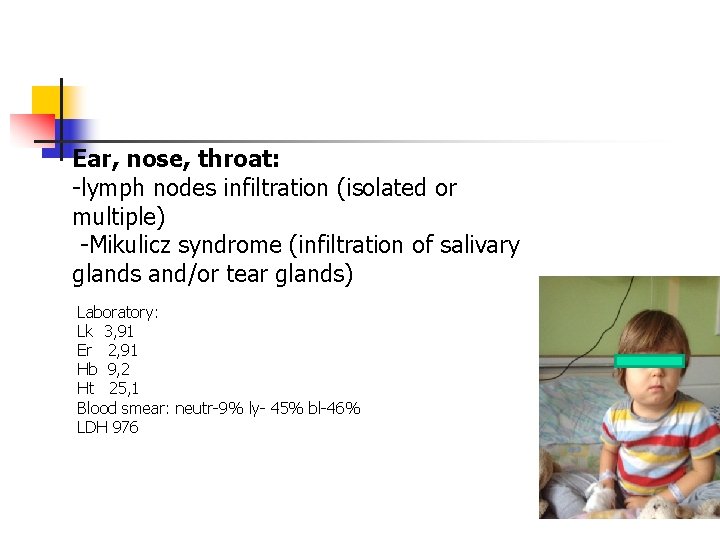
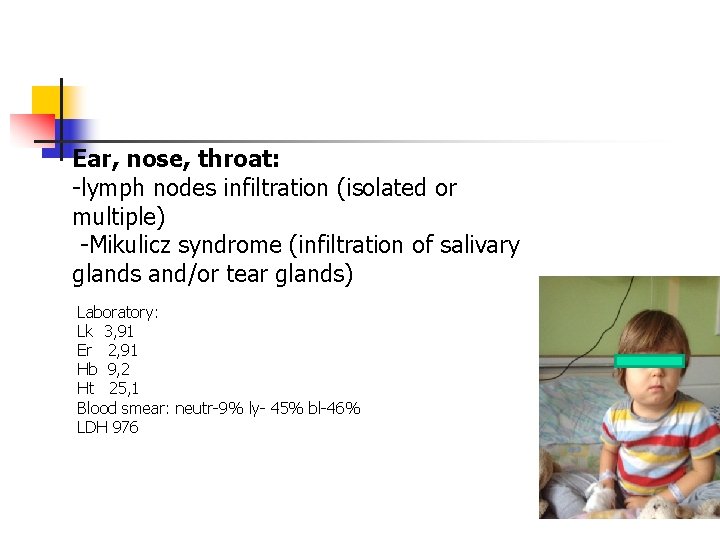
Ear, nose, throat: -lymph nodes infiltration (isolated or multiple) -Mikulicz syndrome (infiltration of salivary glands and/or tear glands) Laboratory: Lk 3, 91 Er 2, 91 Hb 9, 2 Ht 25, 1 Blood smear: neutr-9% ly- 45% bl-46% LDH 976

Skin: maculopapular skin infiltration, often of deep red color (infants)
n n Cardiac involvement: -leukemic infiltration or hemorrhage -occasionally cardiac tamponade due to pericardial infiltration -tachycardia, low blood pressure or other signs of cardiac insufficiency Mediastinum: -enlargement due to leukemic infiltration by lymph nodes and /or thymus (observed in T-cell leukemia) Pleura/and pericardium: effusion Kidney enlargement
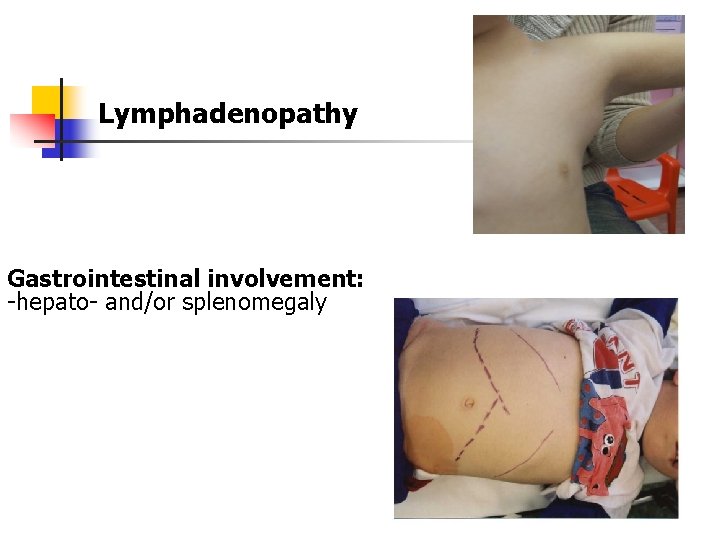
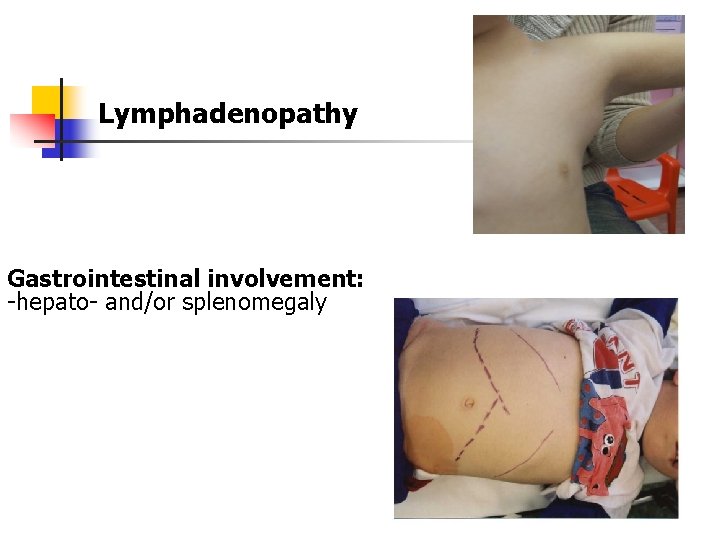
Lymphadenopathy Gastrointestinal involvement: -hepato- and/or splenomegaly
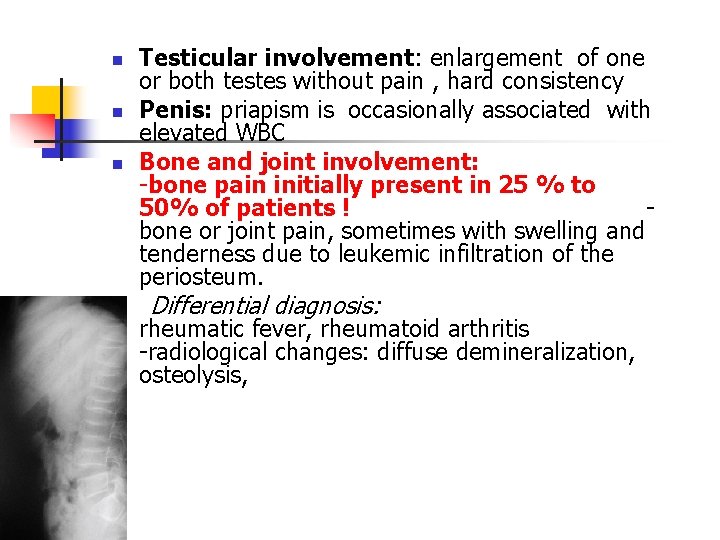
n n n Testicular involvement: enlargement of one or both testes without pain , hard consistency Penis: priapism is occasionally associated with elevated WBC Bone and joint involvement: -bone pain initially present in 25 % to 50% of patients ! bone or joint pain, sometimes with swelling and tenderness due to leukemic infiltration of the periosteum. Differential diagnosis: rheumatic fever, rheumatoid arthritis -radiological changes: diffuse demineralization, osteolysis,
Laboratory findings n n n Red cells: -hemoglobin – normal/ moderate /markedly low -low number of reticulocytes White blood cell : - normal/ low/ high -in children with high WBC- leukemic blast cells present Platelets: -usually low
n n Coagulopathy: -in children with hyperleukocytosis -more common in AML -low levels of prothrombin, fibrinogen, factors V, IX, and X may be present Chemistry: -the serum uric acid is often high initially - the serum potassium level may be high (cell lysis) -serum hypocalcemia or hypercalcemia (in marked leukemic bone infiltration) abnormal liver function > increased level of transaminases
n Bone marrow analysis: >25% blasts -characterize the blast cells -determine the degree of reduction of normal hematopoiesis -morphological, immunological, biochemical, and cytogenetic analyses Differential diagnosis: aplastic anemia, myelodysplastic syndrome, neoplastic infiltrations (neuroblastoma, NHL)
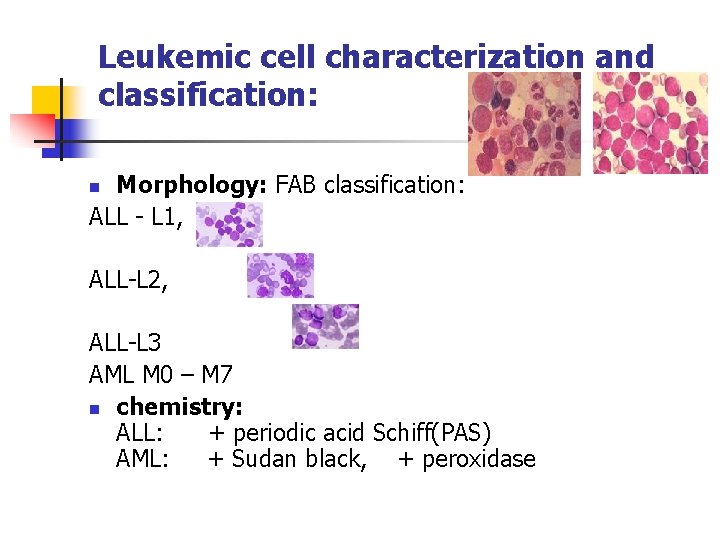
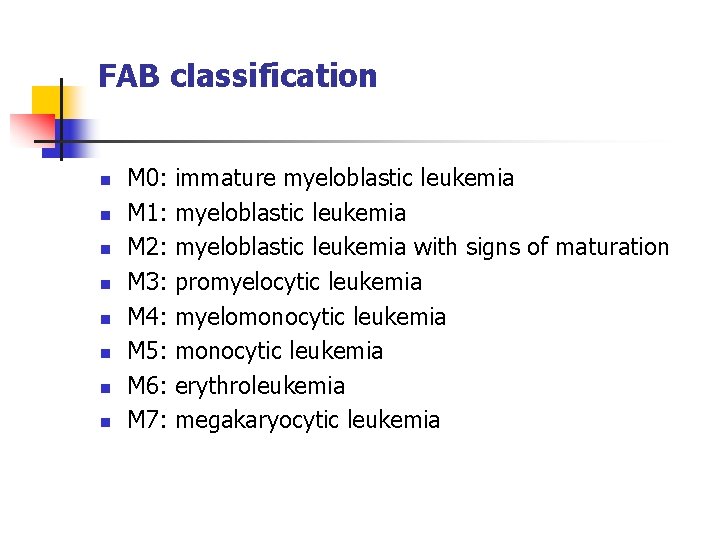
Leukemic cell characterization and classification: Morphology: FAB classification: ALL - L 1, n ALL-L 2, ALL-L 3 AML M 0 – M 7 n chemistry: ALL: + periodic acid Schiff(PAS) AML: + Sudan black, + peroxidase
Immunological characterization: -monoclonal antibodies to leukemia-associated antigens differentiate between types of leukemic cells: * lympoid stem cells: CD 19, HLA-DR, CD 24 (+/-) * early pre-B cells: CD 19, HLA-DR, CD 24 * pre-B cells: CD 19, HLA-DR, CD 24, CD 10, CD 20(+/ -) * B-precursors cell: CD 19, HLA-DR, CD 24, CD 10, CD 20 * T-cell lineage: CD 7, CD 2, CD 1, CD 4, CD 8, CD 3
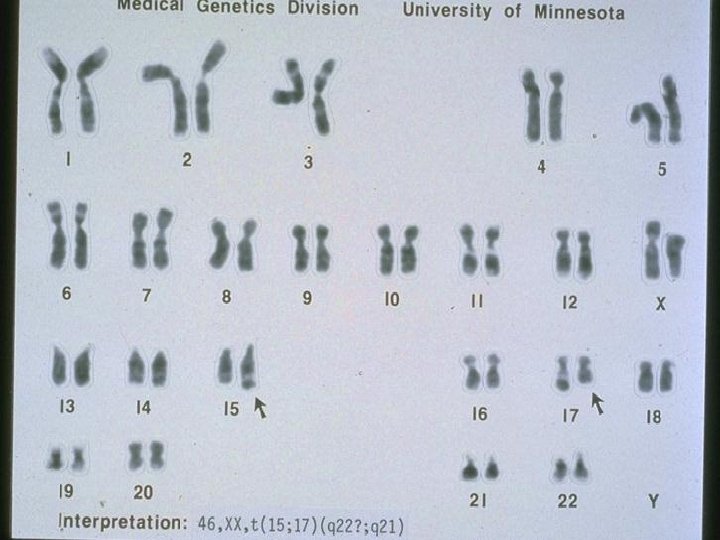
n Cytogenetic characterization: - in 85% of children abnormal karyotype in the malignant clone *t(9; 22) (BCR-ABL) –unfavorable prognosis *t (4; 11) in infants , poor prognosis -ploidy and structure of chromosomes (rearrangements) -hypoploidy- poor prognosis -DNA index (DI)
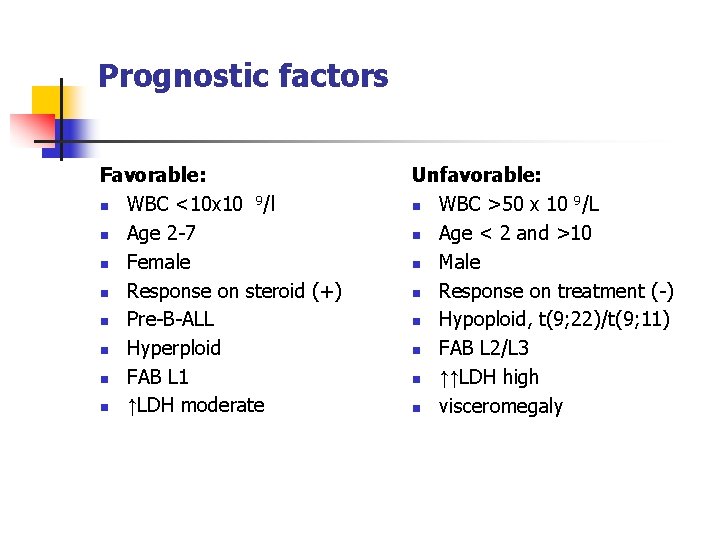
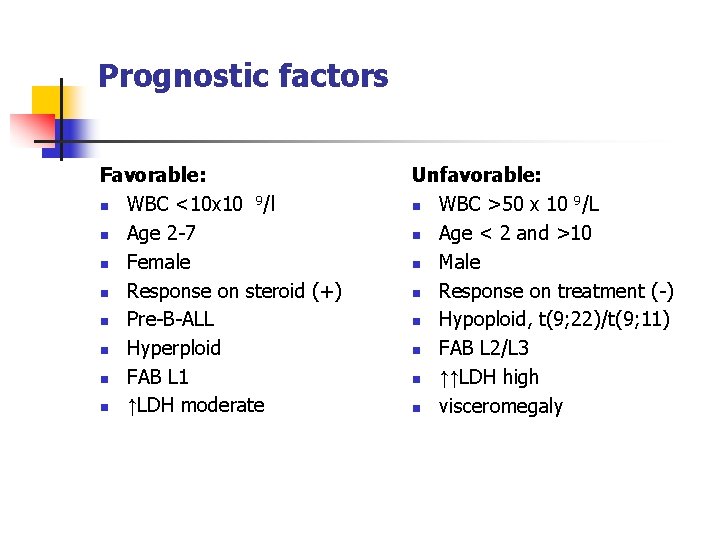
Prognostic factors Favorable: n WBC <10 x 10 9/l n Age 2 -7 n Female n Response on steroid (+) n Pre-B-ALL n Hyperploid n FAB L 1 n ↑LDH moderate Unfavorable: n WBC >50 x 10 9/L n Age < 2 and >10 n Male n Response on treatment (-) n Hypoploid, t(9; 22)/t(9; 11) n FAB L 2/L 3 n ↑↑LDH high n visceromegaly
Differential diagnosis n n n n Leukemic reaction in bacterial infection, acute hemolysis, tuberculosis, sarcoidosis, histoplasmosis Lymphocytosis: pertussis Infectious mononucleosis Aplastic anemia Idiopathic thrombocytopenia Bone marrow infiltration by a solid tumor (NBL, NHL, RMS) Rheumatoid arthritis, rheumatoid fever
Therapy n n In experienced center Subdivided into: -remission induction -consolidation with CNS prophylaxis -maintenance phase Prognosis n n Rate of first remission in ALL: more than 90% 80% of children survive without relapse
Response on treatment n n n Reaction on steroids (7. day) Reaction on chemotherapy (15. and 33. day) Minimal residual disease - MRD (-)
Acute myelogenous leukemia n n Heterogeneous group of malignant hematological precursor cells of the myeloid, monocytic, erythroid or megakaryocytic cell lineage Epidemiology: 15 -20% of all leukemias in children Frequency remains stable throughout childhood with slight increase during adolescence No difference in incidence between boys and girls
FAB classification n n n n M 0: M 1: M 2: M 3: M 4: M 5: M 6: M 7: immature myeloblastic leukemia with signs of maturation promyelocytic leukemia myelomonocytic leukemia erythroleukemia megakaryocytic leukemia
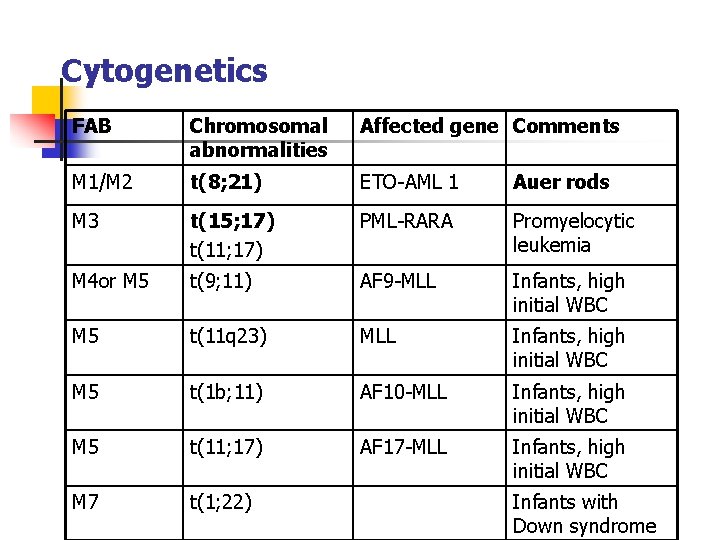
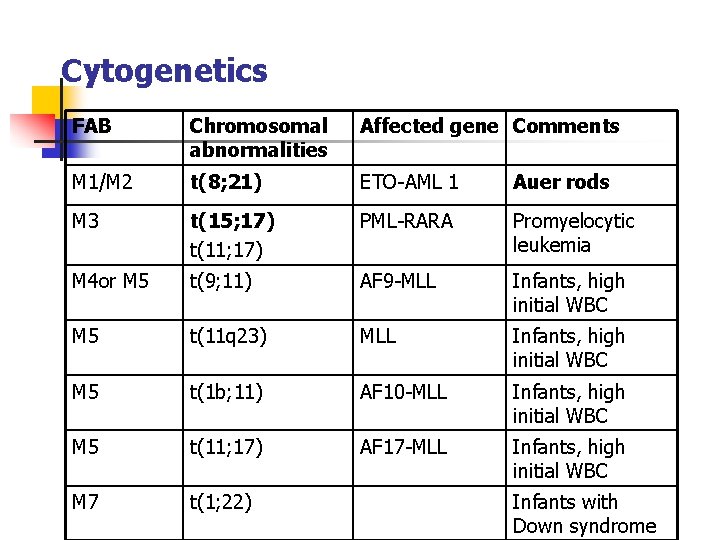
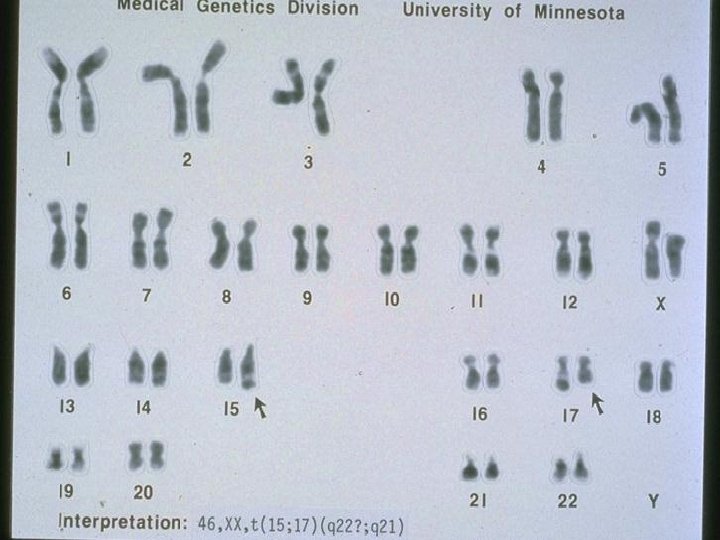
Cytogenetics FAB Chromosomal abnormalities Affected gene Comments M 1/M 2 t(8; 21) ETO-AML 1 Auer rods M 3 t(15; 17) t(11; 17) PML-RARA Promyelocytic leukemia M 4 or M 5 t(9; 11) AF 9 -MLL Infants, high initial WBC M 5 t(11 q 23) MLL Infants, high initial WBC M 5 t(1 b; 11) AF 10 -MLL Infants, high initial WBC M 5 t(11; 17) AF 17 -MLL Infants, high initial WBC M 7 t(1; 22) Infants with Down syndrome
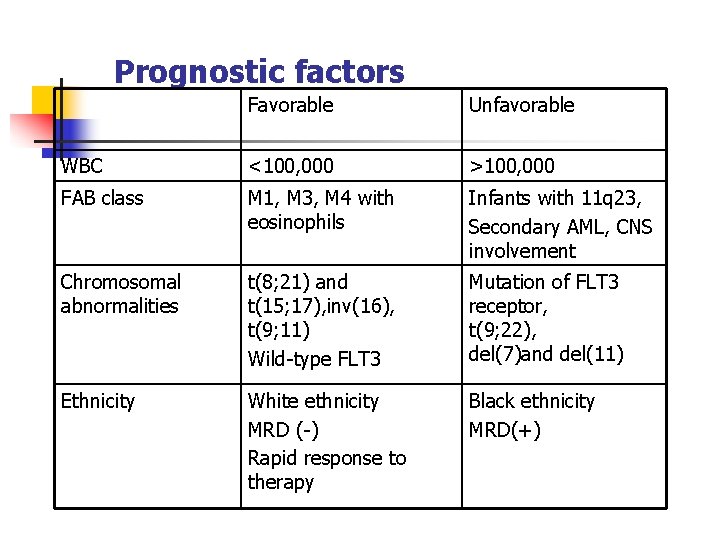
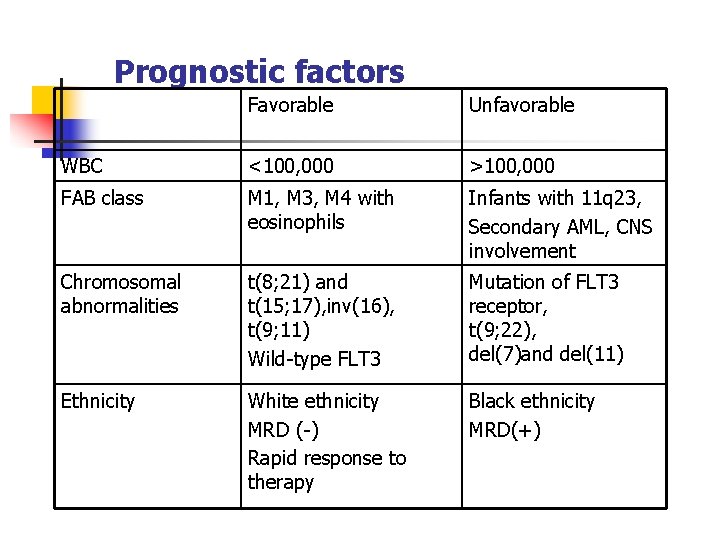
Prognostic factors Favorable Unfavorable WBC <100, 000 >100, 000 FAB class M 1, M 3, M 4 with eosinophils Infants with 11 q 23, Secondary AML, CNS involvement Chromosomal abnormalities t(8; 21) and t(15; 17), inv(16), t(9; 11) Wild-type FLT 3 Mutation of FLT 3 receptor, t(9; 22), del(7)and del(11) Ethnicity White ethnicity MRD (-) Rapid response to therapy Black ethnicity MRD(+)
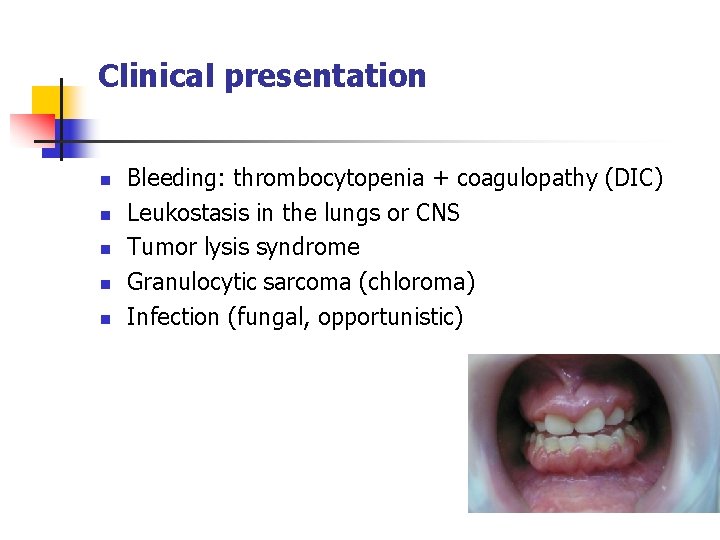
Clinical presentation n n Bleeding: thrombocytopenia + coagulopathy (DIC) Leukostasis in the lungs or CNS Tumor lysis syndrome Granulocytic sarcoma (chloroma) Infection (fungal, opportunistic)
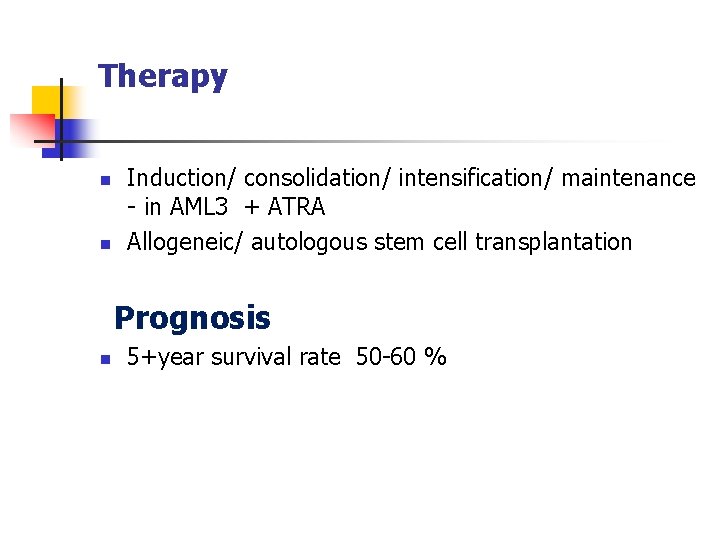
Therapy n n Induction/ consolidation/ intensification/ maintenance - in AML 3 + ATRA Allogeneic/ autologous stem cell transplantation Prognosis n 5+year survival rate 50 -60 %
Non-Hodgkin lymphoma (NHL)
n n n Neoplasia of the lymphatic system and its precursor cells with genetically disturbed regulation, differentiation and apoptosis If marked bone marrow involvement is present the clinical condition is equal of leukemia Incidence 5 – 7 % of all neoplasias in childhood Peak incidence between 5 and 15 years Ratio of boys to girls 2: 1 Burkitt lymphoma (BL): endemic form in Africa 10: 100, 000 children and sporadic form in Europe and USA
Etiology, pathogenesis and molecular genetics Often chromosomal alterations are detecable: in B-cell NHL translocation of chromosome 14 - t(18; 14) Predisposing factors for NHL: n Acquired immunodeficiency: autoimmune disorders, HIV infection n EBV infection n Congenital B-cell defect, congenital T-cell defect with thymus hyperplasia n Bloom syndrome, Chedak-Higashi syndrome, SCID, ataxia teleangiectasia, Wiskott-Aldrich syndrome n Exposure to irradiation n Drug induced, after immunosuppressive treatment
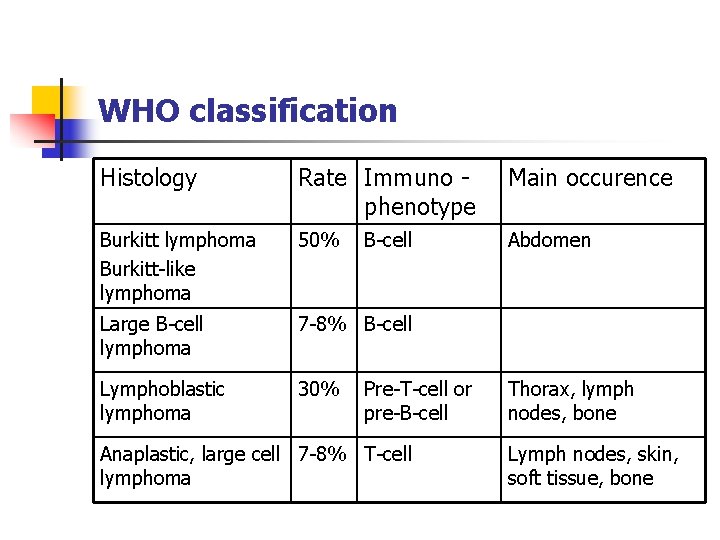
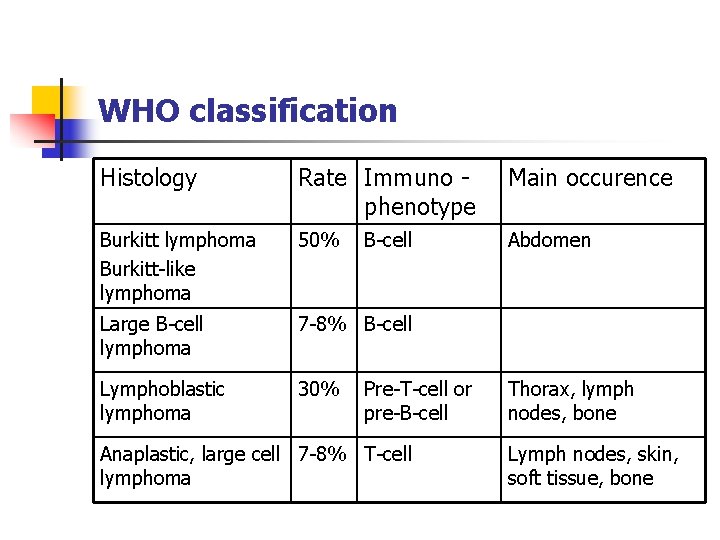
WHO classification Histology Rate Immuno phenotype Main occurence Burkitt lymphoma Burkitt-like lymphoma 50% Abdomen Large B-cell lymphoma 7 -8% B-cell Lymphoblastic lymphoma 30% B-cell Pre-T-cell or pre-B-cell Anaplastic, large cell 7 -8% T-cell lymphoma Thorax, lymph nodes, bone Lymph nodes, skin, soft tissue, bone
Burkitt lymphoma Burkit-like lymphoma n n About 50% of NHL Localization: abdomen, lymphatic tissue of adenoids and tonsils 80% with translocation t(8; 14) or t(8; 2) and t(22; 8) with c-MYC on chromosome 8 q 24 which stimulates proliferation 40% with a p 53 mutation
Large B-cell lymphoma n n 7 -8% of NHL Localization: abdomen, peripheral lymph nodes, skin, bone Lymphoblastic lymphoma n n 30% of NHL Usually mediastinal localization Anaplastic Large Cell Lymphoma n 7 -8% of NHL
Clinical manifestations Duration of symptoms: usually a few days to weeks Non-specific symptoms: fatigue, nausea, anorexia, loss of weigth and/or fever In relation to localisation of NHL: n Abdomen: n especially the ileocecal region, mesentery, retroperitoneum, ovaries > painfull, spasms, vomiting n Obstipation, intussusception n Apendicitis-like n Ileus, ascites
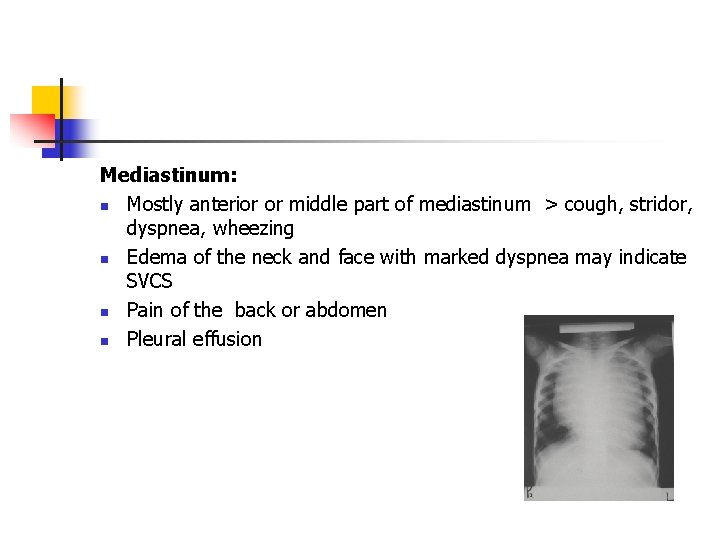
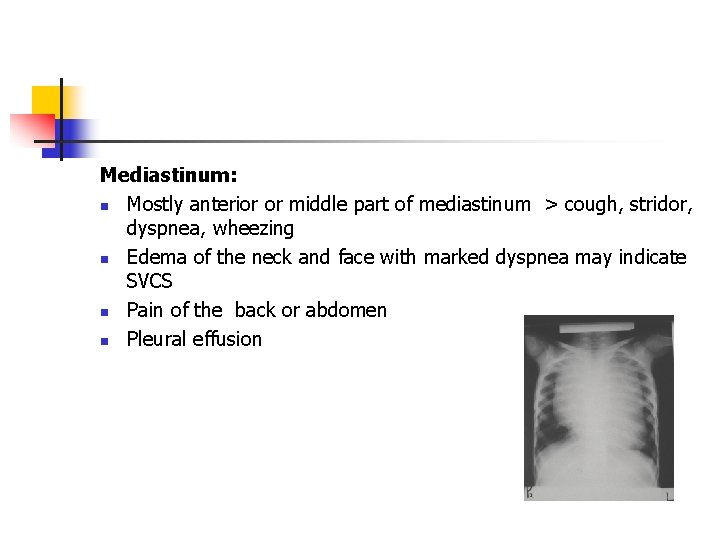
Mediastinum: n Mostly anterior or middle part of mediastinum > cough, stridor, dyspnea, wheezing n Edema of the neck and face with marked dyspnea may indicate SVCS n Pain of the back or abdomen n Pleural effusion
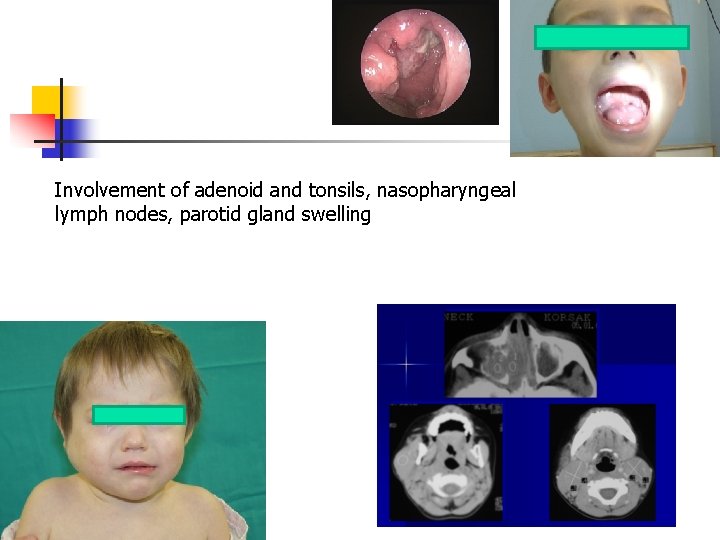
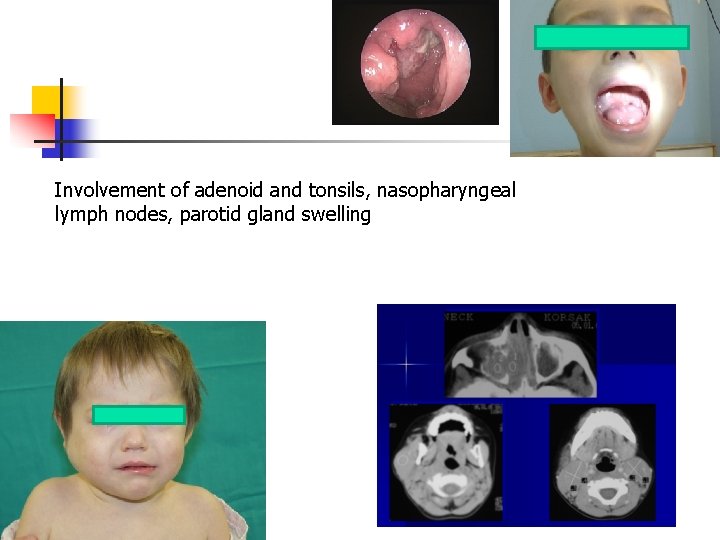
Involvement of adenoid and tonsils, nasopharyngeal lymph nodes, parotid gland swelling
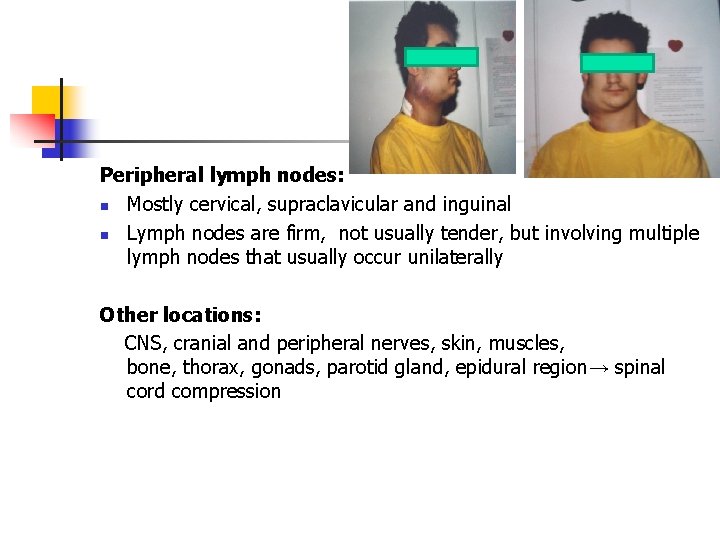
Peripheral lymph nodes: n Mostly cervical, supraclavicular and inguinal n Lymph nodes are firm, not usually tender, but involving multiple lymph nodes that usually occur unilaterally Other locations: CNS, cranial and peripheral nerves, skin, muscles, bone, thorax, gonads, parotid gland, epidural region→ spinal cord compression
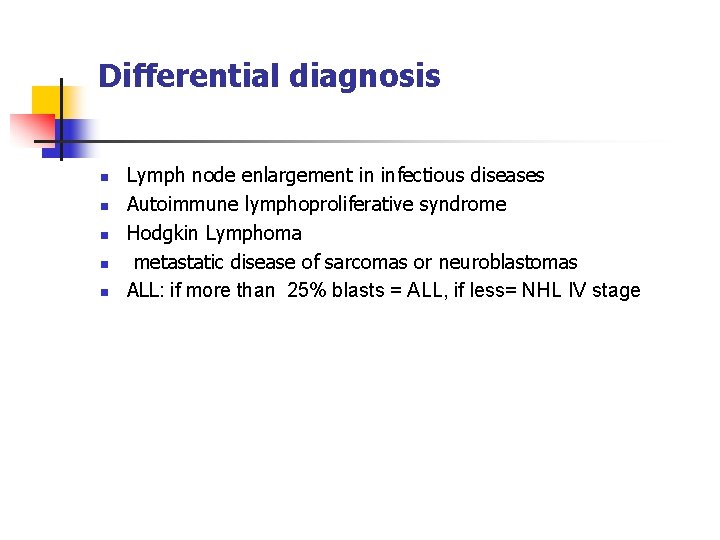
Differential diagnosis n n n Lymph node enlargement in infectious diseases Autoimmune lymphoproliferative syndrome Hodgkin Lymphoma metastatic disease of sarcomas or neuroblastomas ALL: if more than 25% blasts = ALL, if less= NHL IV stage
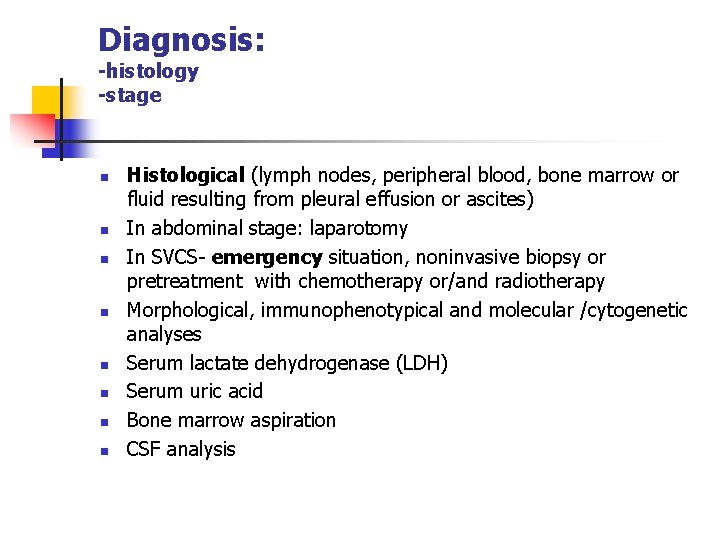
Diagnosis: -histology -stage n n n n Histological (lymph nodes, peripheral blood, bone marrow or fluid resulting from pleural effusion or ascites) In abdominal stage: laparotomy In SVCS- emergency situation, noninvasive biopsy or pretreatment with chemotherapy or/and radiotherapy Morphological, immunophenotypical and molecular /cytogenetic analyses Serum lactate dehydrogenase (LDH) Serum uric acid Bone marrow aspiration CSF analysis
n n n n Radiological diagnosis Ultrasound Conventional X-ray CT of the thoracic, abdomen and skeletal disease MRI for CNS PET (positron –emmision tomography) Bone scan
Staging ( Murphy/St. Jude) n n I- a single tumor (extranodal) or single anatomical area (nodal), excluding mediastinum or abdomen II- a single tumor (extranodal) with regional involvement On same side of diaphragm a/ two or more nodal areas b/ two single (extranodal) tumors with or without regional node involvement A primary gastrointestinal tract tumor (usually ileocecal) with or without associated mesenteric node involvement; gross complete resection
n n III- On both sides of the diaphragm: a/two single tumors (extranodal) b/two or more nodal areas ALL primary intrathoracic tumors (mediastinal, pleural, thymic) All extensive primary intra-abdominal disease, unresectable All primary paraspinal or epidural tumors regardless of other sites IV- Any of the above with initial CNS or bone marrow involvement (less than 25%)
n n Stages I + II: 10 – 20% of all NHL Stages III+ IV: 80 – 90% of all NHL
Treatment n n n Induction therapy should be begun as soon as possible! Tumor lysis syndrome prophylaxis or treatment Chemotherapy (in Poland -according to BFM protocols) Surgical procedure: total resection in I or II stage with localized masses only BMT ( auto) Overall long-term survival >80%
Hodgkin Disease
n n n Progressive, painless enlargement of lymph nodes with continuous extension between lymph node region Pathogmonic histologically : Reed-Sternberg cells Incidence: 5 -7% of all neoplasia in childhood Boys more than girls Rare before 5 years; increasing until the age of 11 years Peak incidence between 15 and 35 years of age
Etiology and pathogenesis n n Correlation with EBV infection, genetic predisposition, disturbed humoral and cellular immune response High incidence in patients with LE, rheumatoid disorders, ataxia teleangiectasia, agammaglobulinemia
Clinical presentation n n Painless enlargement of lymph nodes, mostly in the cervical and supraclavicular regions Swollen lymph nodes are firm, not inflammatory and painfull to palpation Most common involved lymph nodes: cervical (75%), supraclavicular(25%), axillary, infradiaphragmatic Extranodal involvement: lung, bone, liver In mediastinal involvement: a cough, sometimes with dyspnea, dysphagia and enlargement of the vessels of the neck (SVCS)
B symptoms (in 20 -30%) n Fever higher than 38° C n Night sweats n Loss of more than 10% body weight n Sometimes: pruritus and/or nausea

Open biopsy Not fine-nedle biopsy!!! Histological classification: n Lymphocyte predominance n Nodular sclerosing n Lymphocyte-depleted n Mixed cellular
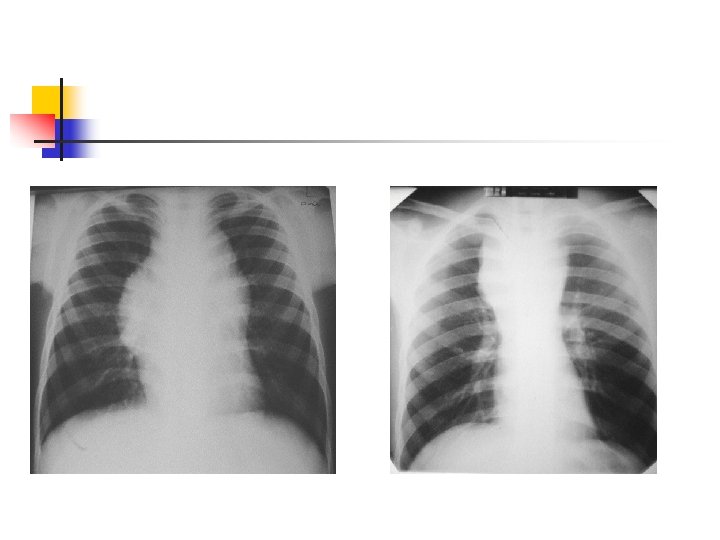
Laboratory analyses n n Blood Bone marrow Ferritin, LDH Immunological analyses Stagen n Radiological evaluation Chest (x-ray, CT) Abdomen (usg, CT) Bone scintigraphy PET-CT
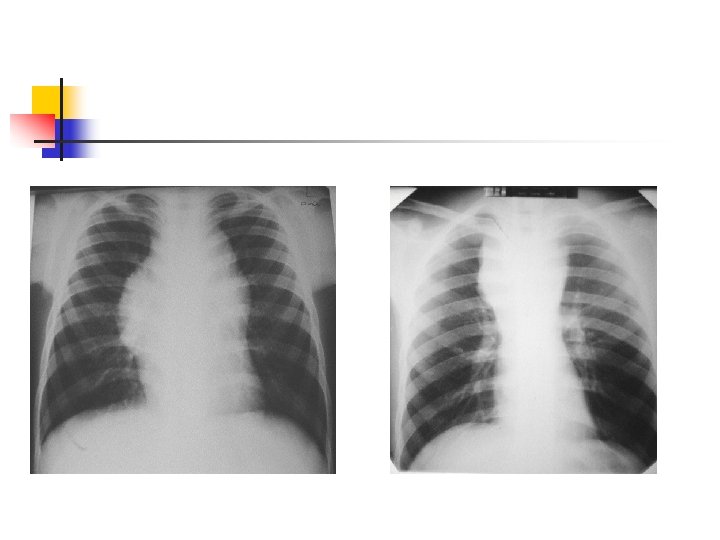
HL
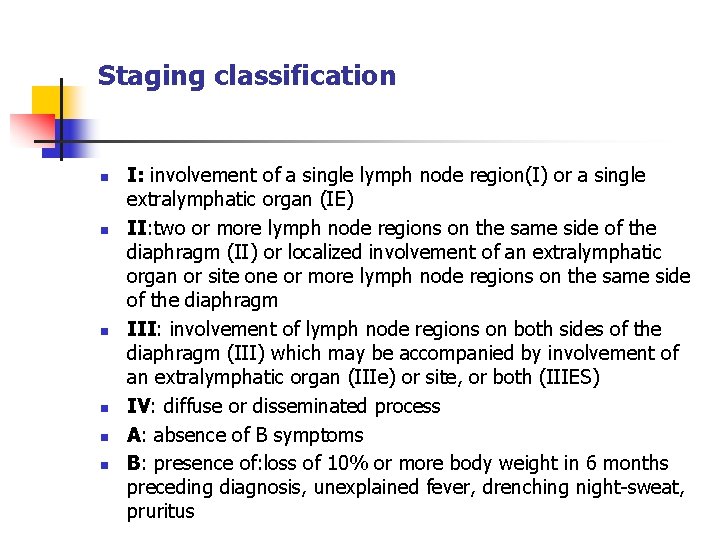
Staging classification n n n I: involvement of a single lymph node region(I) or a single extralymphatic organ (IE) II: two or more lymph node regions on the same side of the diaphragm (II) or localized involvement of an extralymphatic organ or site one or more lymph node regions on the same side of the diaphragm III: involvement of lymph node regions on both sides of the diaphragm (III) which may be accompanied by involvement of an extralymphatic organ (IIIe) or site, or both (IIIES) IV: diffuse or disseminated process A: absence of B symptoms B: presence of: loss of 10% or more body weight in 6 months preceding diagnosis, unexplained fever, drenching night-sweat, pruritus
Differential diagnosis n n n n Toxoplasmosis, tuberculosis, atypical infections NHL Mononucleosis Metastatic disease Thymus hyperplasia Rheumatoid arthritis, LE Sarcoidosis
Treatment n n Procedure depends on stage and histopathology Chemo- and radiotherapy (Euro. Net protocol) Prognosis n Stage I/II EFS >90% n Stage III/IV EFS 70 -80%