PROFESSONAL INTERACTIONS WORKING AS A TEAM INTERACTIONS IFTS









- Slides: 59
PROFESSONAL INTERACTIONS WORKING AS A TEAM
INTERACTIONS IFTS 911
INTERACTIONS Like all of emergency services, you do not usually have the luxury of know the people you will interact with You are also dealing with people under trying circumstances. You also have to interact with numerous individuals who all have different functions Patient Family Nurses Doctors Etc……. .
INTERACTIONS AND THESE PEOPLE ALL HAVE TO DEAL WITH YOU!
RULES OF ENGAGEMENT Treat people the way you want to be treated. Always maintain the utmost professionalism.

RULES OF ENGAGEMENT And if the professionalism is not reciprocated. . .
RULES OF ENGAGEMENT SUCK IT UP. . . it's not about you, it is about providing the best patient care. And you never win this battle.
FIRST IMPRESSIONS PERCEPTION IS REALITY The first impression is the lasting one. How you project yourself is how people will respond to you. Confident or Arrogant? Professional or Uninterested? Well groomed or a slob?
EMT-STAFF INTERACTION Most common interaction is EMT-Nurse When arriving to pick up a patient, make it perfectly clear who you are and the patient you are here to care for. When arriving to drop off a patient, determine who is in charge and direct the conversation to that person or group of people.
EMT-STAFF INTERACTION Recognize that the staff can be stressed and spread thin. If possible pitch in.
EMT-STAFF INTERACTION Information needs to be gathered and given expeditiously. It should be geared to what is pertinent to the patient’s care. Don’t linger. If for any reason the interaction becomes heated or contentious, take it outside. NEVER ARGUE IN FRONT OF THE PATIENT OR FAMILY
EMT-STAFF INTERACTION “He said she said”. . “She said”. . . . “He said, he said”. . . . We said, she said”. . . . “We said, he said”. . . “He said, we said”. . . “She said, we said”. . . . “We said, they said”. . . . “They said, we said”. . . “He said, they said”. . . “She said, they said”. . . . “They said, he said”. . . . “They said, she said”. . . .
EMT-STAFF INTERACTION
EMT-FAMILY INTERACTION Introduce yourself and let them know what you are professionally; basic, paramedic… Gather some general information from them and confirm with them why you are there. Use them as a resource. They can give you valuable information. A small amount of interaction will put them all at ease

EMT-PATIENT INTERACTION DIGNITY AND DEFERENCE The elderly (and all your patients) deserve to be treated with the respect that comes from a long life. That elderly person may have been a wife, mother, retired military, lawyer, doctor or judge. While that person may now be feeble and demented, it does not mean we patronize them.
EMT-PATIENT INTERACTION �SIR MAM �MISTER MRS. • JUDGE � DOCTOR • CAPTAIN………. .
EMT-PATIENT INTERACTION DON’T USE…. HON DEAR SWEETHEART etc. • IT IS PATRONIZING AND

EMT-PATIENT INTERACTION YOU SOUND LIKE A D-BAG
ARRIVE PREPARED You must be prepared to practice at your licensed level when you arrive at the patients side. Arrive at the patient’s side with all the equipment you need to practice at your certified level Patients are presumed sick and do not walk to the stretcher. Care begins when you first interact with the patient. Don’t begin in the ambulance.
MOLST A MOLST OR Comfort Care order has to be with the patient and available in order to follow the directive You cannot accept a verbal from the staff or family member. The legal guardian cannot give a verbal directive in person or over the phone as well.
LEVEL OF CARE The level of care is determined by the facility request and/or dispatch. On arrival, the situation may have changed and a more advanced level of care should could be necessary.
LEVEL OF CARE DON’T BE SHY ABOUT ASKING FOR HELP. It’s not a sign of weakness. Your first priority is doing the right thing by the patient.
ITF TO 911 Patients from skilled care facilities are typically complex and at best in “stable disequilibrium”. These patients are best served at facilities that know them and have provided previous care. EVERY EFFORT SHOULD BE MADE TO GET THE PATIENT TO THE DESIGNATED FACILITY.

ITF TO 911 When assessing these patients, rely on the staff to gain a sense what is normal for them. The level of consciousness may be poor in an acute setting but normal for this patient. Abnormal vitals may be the norm for the patient. HYPOTENSION AND TACHYCARDIA ARE RARELY THE NORM! It’s your job to sort this out.
ITF TO 911 If you still feel uncomfortable about the destination Relay your concerns to the staff so they can address them. Consider upgrading the level of service if possible. i. e. basic to paramedic.
ITF TO 911 TRY NEVER TO UNILATERALLY CHANGE THE PATIENT’S DESTINATION. Contact medical control.
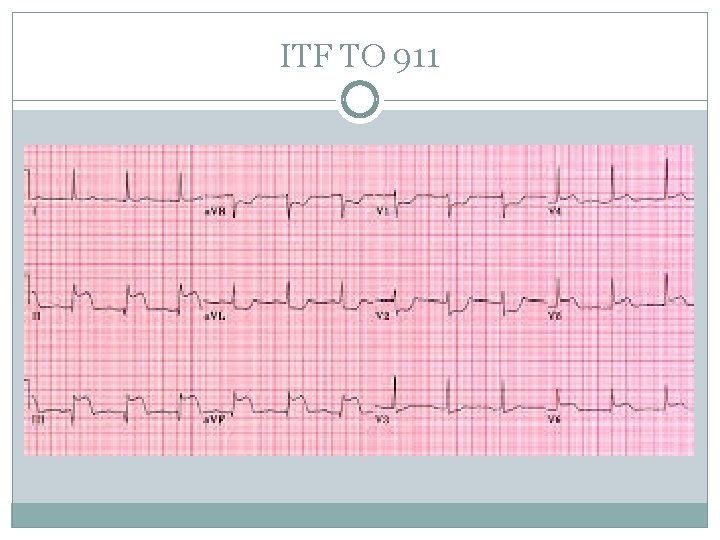
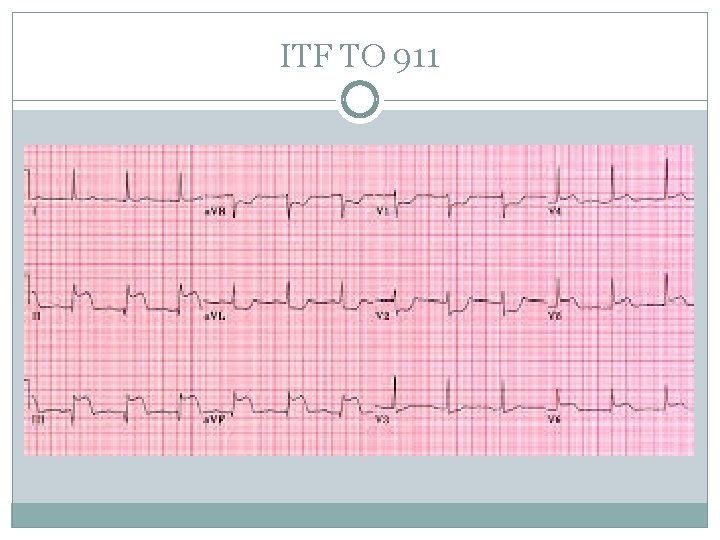
ITF TO 911 The decision to change an ITF to a 911 call occurs primarily because of a change in the patients condition. A “routine” chest pain now has an EKG which demonstrates a stemi. The TIA is now a CVA
ITF TO 911 When the interfaculty call becomes a 911…. FOLLOW THE STATE’S POINT OF ENTRY PROTOCOLS.
ITF TO 911 COMMUNICATE Let the patient, staff and family know of the change of condition and destination. Contact the destination hospital.
ITF TO 911 57 y/0 male with chest pain is going to the Morton Hospital in Taunton. He is pain free and the chest pain is reproducible. Vitals are normal and the EKG is normal. Except for getting an EKG and being given an aspirin at the office, nothing else has been done. How do you present yourself to the office?
ITF TO 911 You get into the ambulance and he now complains of severe chest pain and is diaphoretic. Now what?
ITF TO 911
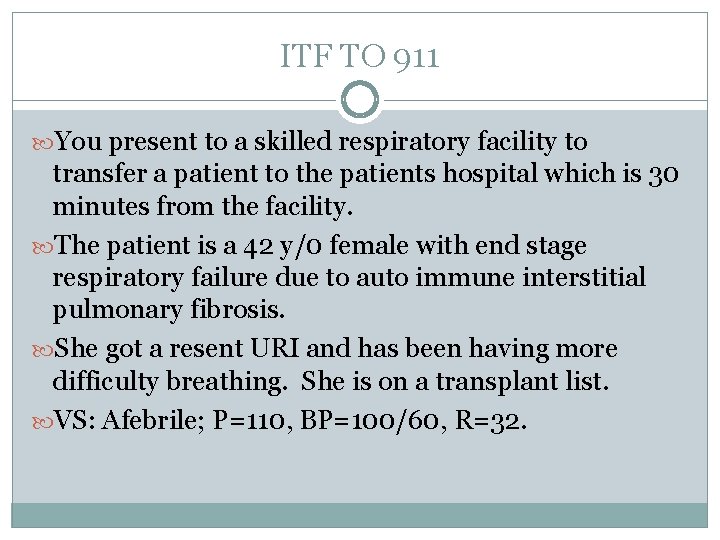
ITF TO 911 You present to a skilled respiratory facility to transfer a patient to the patients hospital which is 30 minutes from the facility. The patient is a 42 y/0 female with end stage respiratory failure due to auto immune interstitial pulmonary fibrosis. She got a resent URI and has been having more difficulty breathing. She is on a transplant list. VS: Afebrile; P=110, BP=100/60, R=32.
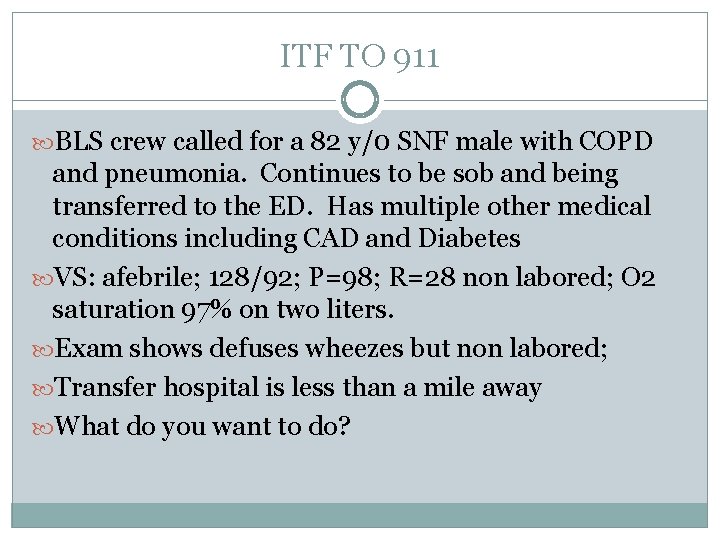
ITF TO 911 BLS crew called for a 82 y/0 SNF male with COPD and pneumonia. Continues to be sob and being transferred to the ED. Has multiple other medical conditions including CAD and Diabetes VS: afebrile; 128/92; P=98; R=28 non labored; O 2 saturation 97% on two liters. Exam shows defuses wheezes but non labored; Transfer hospital is less than a mile away What do you want to do?

ITF TO 911 Transfer hospital is 20 miles away and minimum of 25 -30 minutes. This change anything?
ITF PROTOCOLS STAFFING Staffing must meet the medical needs of the patient. Minimum staffing is Intermediate/Basic; Paramedic/Basic; Basic/Basic
ITF PROTOCOLS SCOPE OF PRACTICE EMT’s must never practice beyond their scope of practice Section 170. 360(A) of the EMS Regulations states, “No ambulance service or agent thereof shall transport a patient between health care facilities who is receiving medical treatment that is beyond the training and certification capabilities of the EMTs staffing the ambulance unless an additional health care professional with that capability accompanies the patient. . . ”
ITF PROTOCOLS SCOPE OF PRACTICE In the even a specialist travels with the crew, that specialist must contact medical control.
ITF PROTOCOLS BASIC STAFFING “Clearly stable for transport” and all devices are “off” No airway issues All lines such as nasogastric tubes, picc lines, feeding tubes, bladder irrigations, etc. are clamped May transport a “stable” patient who has a maintenance IV running
ITF PROTOCOLS INTERMEDIATE STAFFING Patient with an acute or sub acute problem Has been stabilized to the best of the facilities abilities and has the potential of decompensating. “Instrumentation or medication running must be consistent with the Interfacility Transfer Guidelines. ”

ITF PROTOCOLS PARAMEDIC STAFFING Patient with an acute problem Has been stabilized to the best of the facilities abilities and has “high potential” of decompensating. “Critical care patient with any other instrumentation or medication running that is not included in the Interfacility Transfer Guidelines. ”
ITF PROTOCOLS CRITICAL CARE TRANSPORT “Under no circumstances shall EMTs function or be assigned to transfers beyond, or potentially beyond, the scope of their training and level of certification. ”
ITF PROTOCOLS CRITICAL CARE TRANSPORT CCT should be used when management of the patient is beyond the EMT’s scope of practice. CCT may be a designated truck that has the appropriate medical staff; i. e. Tufts Floating CCT may be the appropriate level of EMT’s along with additional hospital staff. CCT may be an air ambulance.

ITF PROTOCOLS INTERFACILITY TRANSFER CHECKLISTS SORTED BY PATIENT CONDITION/DIAGNOSIS D 1 Aortic Disection D 2 Blood Transfusion Reactions D 3 Cerebrovascular Accident (Post-t. Pa) D 4 Post-Arrest Induced Hypothermia D 5 Pregnancy-Related D 6 ST-Segment Elevation Myocardial Infarction (STEMI)
ITF PROTOCOLS GENERAL GUIDELINES FOR MEDICATION ADMINISTRATION “The transport paramedic must be familiar or become familiar through consultation (i. e. , with a drug reference or discussion with hospital staff) on the attributes of each drug the patient has received prior to and will receive during transport. ”
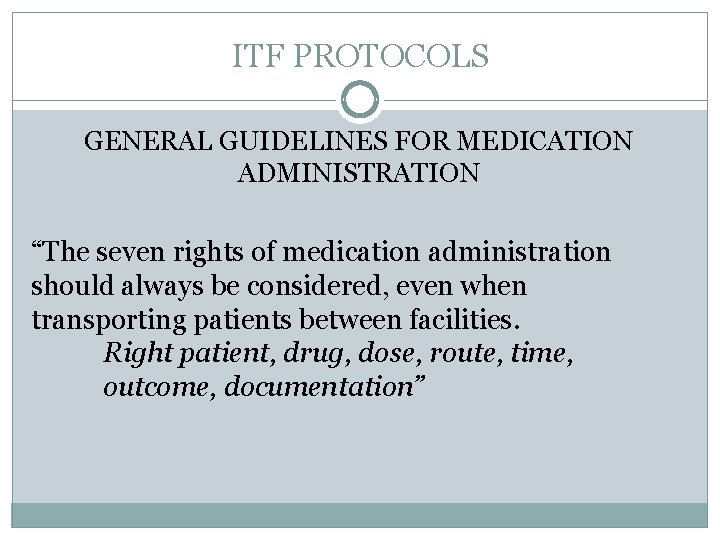
ITF PROTOCOLS GENERAL GUIDELINES FOR MEDICATION ADMINISTRATION “The seven rights of medication administration should always be considered, even when transporting patients between facilities. Right patient, drug, dose, route, time, outcome, documentation”

ITF PROTOCOLS GENERAL GUIDELINES FOR MEDICATION ADMINISTRATION “Paramedics may not accept any medications from the sending facility for the purposes of bolus administration during transport. ”

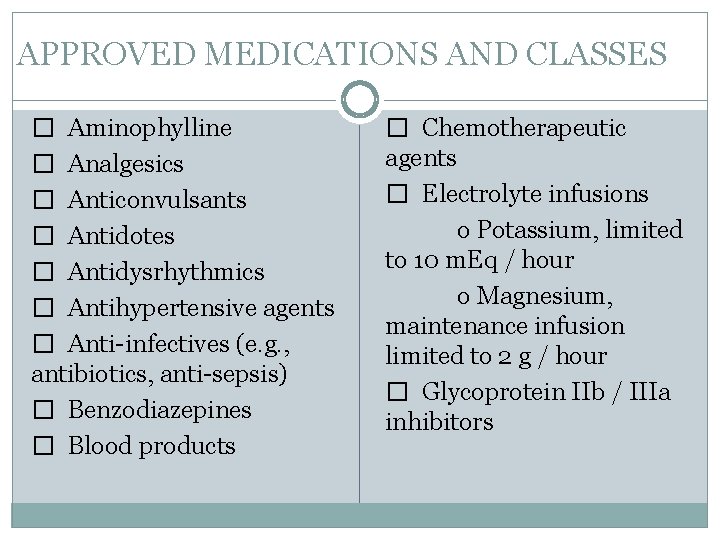
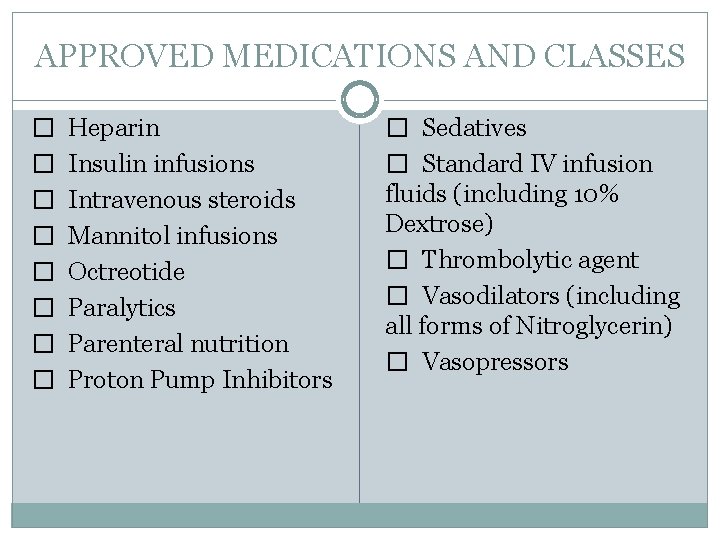
ITF PROTOCOLS APPROVED MEDICATIONS AND CLASSES “Any of the following medications or medication classes, not currently part of the EMT Paramedic Statewide Treatment Protocols, may be maintained if initiated at the sending facility, and can only be titrated through specific IFT protocols and by on-line MEDICAL CONTROL. ”
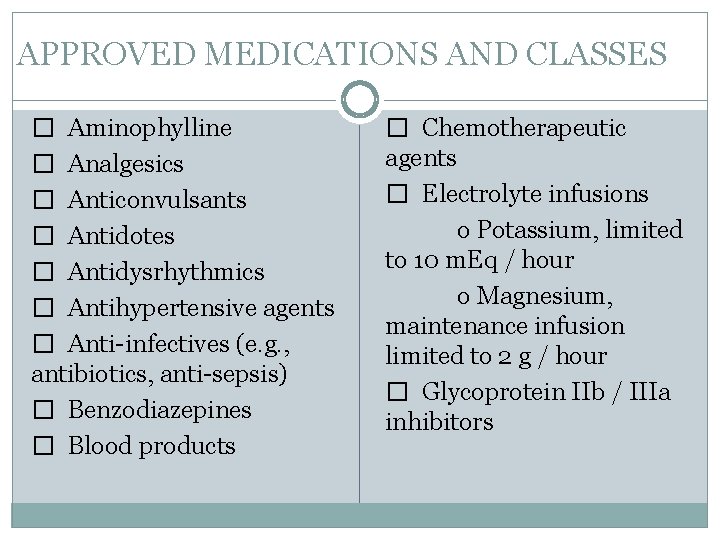
APPROVED MEDICATIONS AND CLASSES � Aminophylline � Analgesics � Anticonvulsants � Antidotes � Antidysrhythmics � Antihypertensive agents � Anti-infectives (e. g. , antibiotics, anti-sepsis) � Benzodiazepines � Blood products � Chemotherapeutic agents � Electrolyte infusions o Potassium, limited to 10 m. Eq / hour o Magnesium, maintenance infusion limited to 2 g / hour � Glycoprotein IIb / IIIa inhibitors
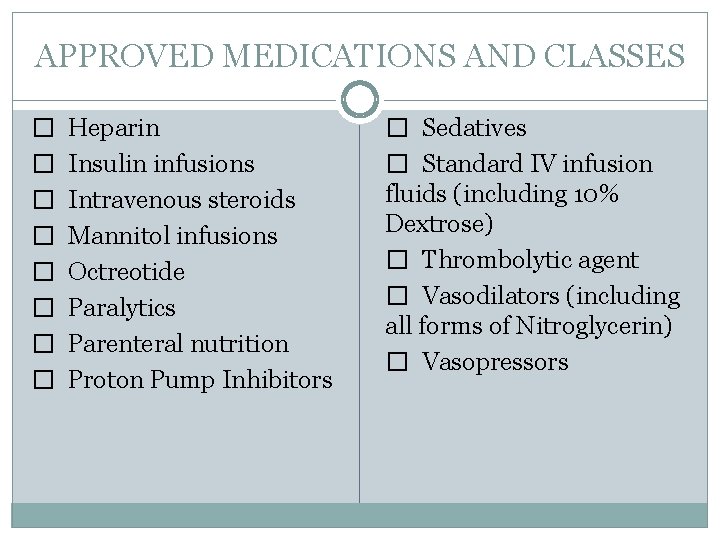
APPROVED MEDICATIONS AND CLASSES � Heparin � Insulin infusions � Intravenous steroids � Mannitol infusions � Octreotide � Paralytics � Parenteral nutrition � Proton Pump Inhibitors � Sedatives � Standard IV infusion fluids (including 10% Dextrose) � Thrombolytic agent � Vasodilators (including all forms of Nitroglycerin) � Vasopressors
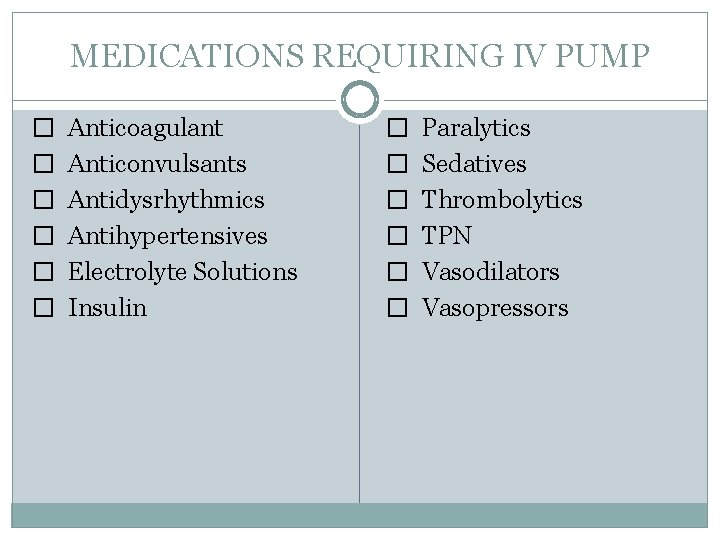
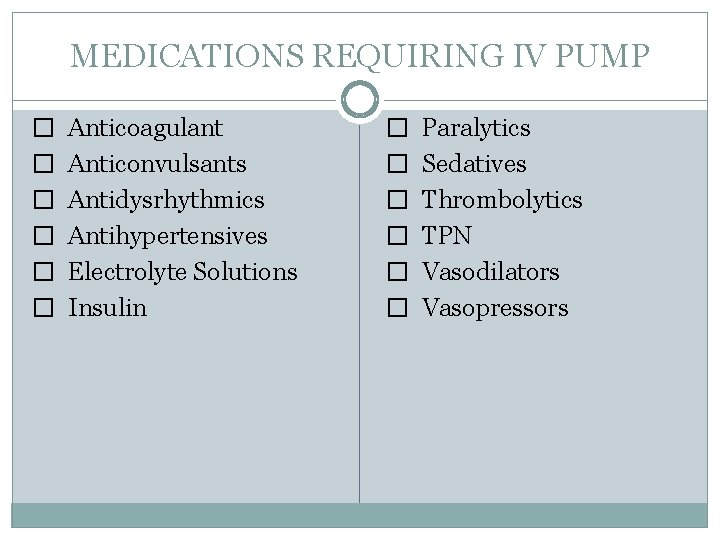
MEDICATIONS REQUIRING IV PUMP � Anticoagulant � Anticonvulsants � Antidysrhythmics � Antihypertensives � Electrolyte Solutions � Insulin � Paralytics � Sedatives � Thrombolytics � TPN � Vasodilators � Vasopressors
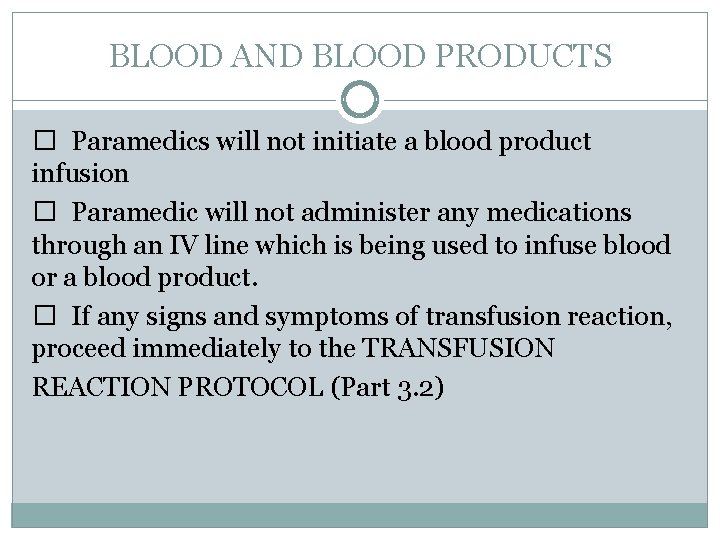
BLOOD AND BLOOD PRODUCTS � Paramedics will not initiate a blood product infusion � Paramedic will not administer any medications through an IV line which is being used to infuse blood or a blood product. � If any signs and symptoms of transfusion reaction, proceed immediately to the TRANSFUSION REACTION PROTOCOL (Part 3. 2)
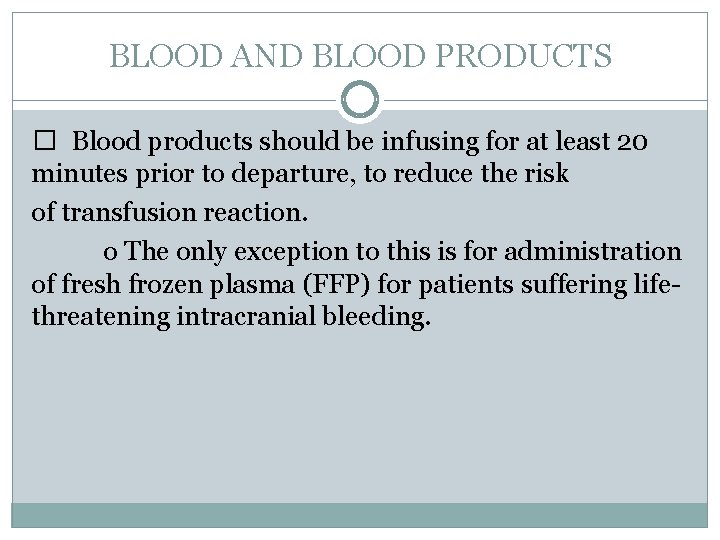
BLOOD AND BLOOD PRODUCTS � Blood products should be infusing for at least 20 minutes prior to departure, to reduce the risk of transfusion reaction. o The only exception to this is for administration of fresh frozen plasma (FFP) for patients suffering lifethreatening intracranial bleeding.
MECHANICAL VENTILATION � Unless the transfer is time sensitive in nature (e. g. , STEMI, aortic dissection, acute CVA, unstable trauma, etc. ), the following requirements apply to ventilator use and / or adjustment: o Patients must be observed, by the sending facility, for a minimum of 20 minutes after any adjustment in ventilator settings. o Patients should be on the transport ventilator for 20 minutes prior to departure.
SUMMARY WE ARE ALL ON THE SAME TEAM. Our goal is the best patient care we ALL can afford to give.
SUMMARY ACT PROFESSIONAL AT ALL TIMES Perception is reality. You will be assessed within the first few minutes. After that you have to live with it!
SUMMARY REACH OUT AND HELP Patient care carries with it high level of stresses. Everyone should do whatever they can to prioritize and expedite the care of the patient.
SUMMARY COMMUNICATE Communication will prevent and clear most issues before they become substantial. And just remember…. .
SUMMARY Pissing contests hinder the best care we can give and in the end hurt the reputation of everyone and every entity involved.