Prof S Moied Ahmed Ph D MD FICCM


- Slides: 142
Prof. S Moied Ahmed Ph. D, MD, FICCM, FCCP, FIMSA Department of Anaesthesiology & Critical Care J N Medical College AMU, Aligarh
How we would proceed? • Discuss under two broad headings – Cases (3 -4 cases, according to availability time) – Algorithm with related equipment • Only on core airway problems • Question & answer based • Summarize at the end of each case • Leave it for you to read the part not discussed • Feel free to ask questions related to the topic.
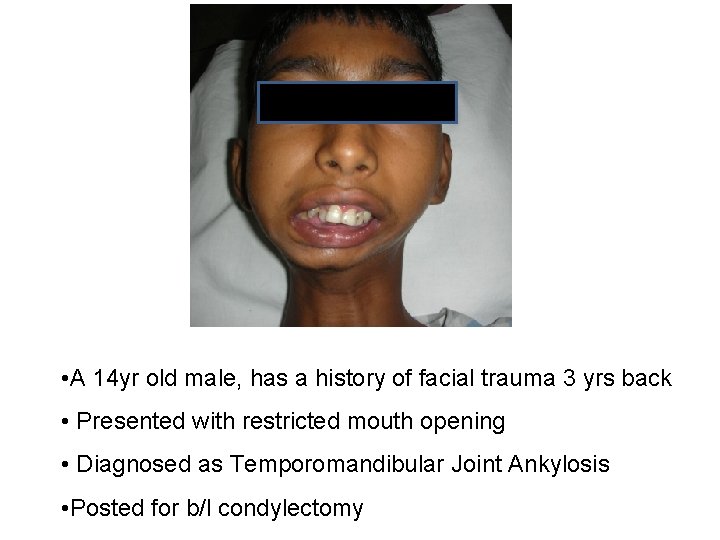
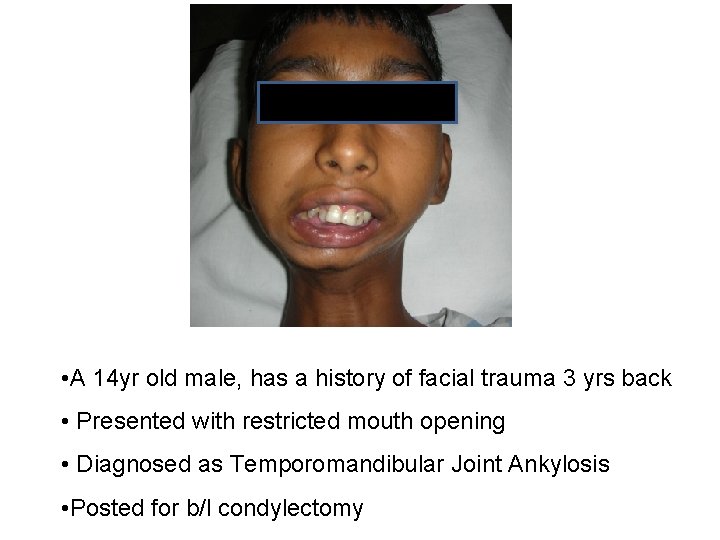
• A 14 yr old male, has a history of facial trauma 3 yrs back • Presented with restricted mouth opening • Diagnosed as Temporomandibular Joint Ankylosis • Posted for b/l condylectomy
• What do you mean by TM joint ankylosis?
• Ankylosis of the Temporomandibular joint, an arthrogenic disorder of the TMJ, refers to restricted mandibular movements (hypomobility) with deviation to the affected side on opening of the mouth.
• What is so peculiar about TM joint?
• Diarthrodial synovial joint with three different features – Both the joint functions as a single unit that is the craniomandibular articulation. – Articular surfaces are lined by fibrocartilage instead of hyaline – Articular discs – biconcave – separates into two compartments
• How much mouth opening does each joint contribute?
– Hinge joint: 2 – 3 cm – Sliding joint: 2 – 3 cm – A total of 6 cm when the mouth opens fully
• What are the clinical features of TMJ ankylosis?
• Inability to open the jaws • In unilateral ankylosis, the lower jaws shifts towards the affected side on opening of the mouth • In severe cases, there is complete immobilization • There may be abnormal forward protrusion of the mandible as the excess tissues occupies the space • Facial deformity
• What physical clinical features are of your concern? OR • What are the associated problems the patient can have?
• Restricted Joint movement in all directions (max inter incisor gap 4 -6 cm, lateral excursion 1 cm) • Facial asymmetry, hypoplastic and retrognathic mandible, bird-face deformity • Dentition problems – caries, abscess • OSA / increased airway obstruction • Corpulmonale
• What are your ANAESTHETIC considerations?
• Difficult airway • Associated OSA • Sensitive to central depressant drugs / sedatives • Poor nutrition • Poor dental hygiene / abscess • Post operative maintenance of airway • Paediatric age group
• Why do these patients have increased incidence of airway obstruction?
• Secondary to structural encroachment on pharyngeal and hypo pharyngeal lumen, • Subatmospheric intrapharyngeal pressure and hypotonocity of oropharyngeal muscles.
• During airway management when do you face difficulties? • Difficult mask ventilation - BONES • Difficult laryngoscopy and intubation - LEMON • Difficult supraglottic airway insertion – RODS /DROPS • Difficult extubation
• Why should there be difficult mask ventilation ?
• Difficult mask seal : small and receding mandible • Tongue fall – jaw thrust not possible
• Why should there be difficult laryngoscopy and intubation?
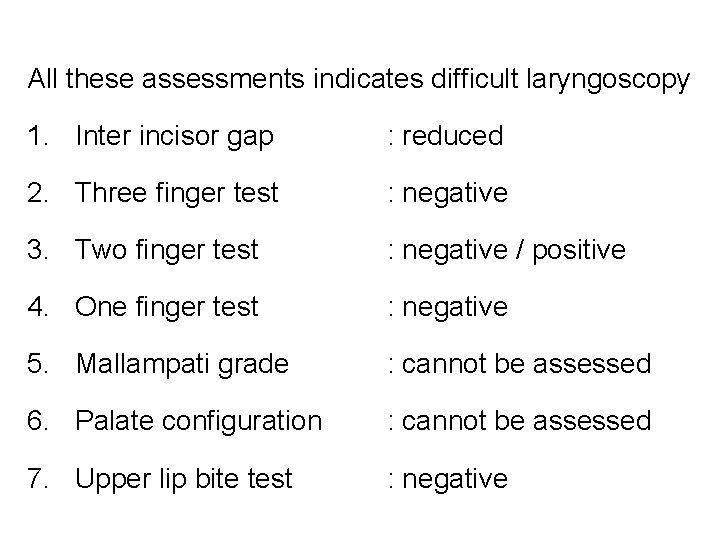
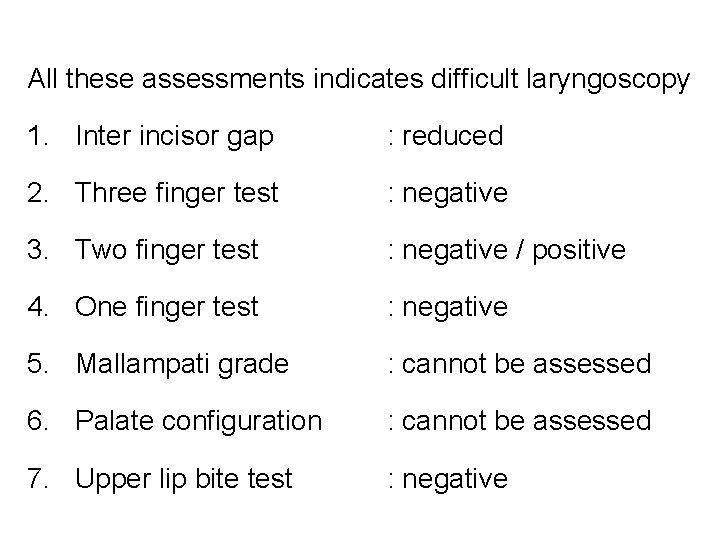
All these assessments indicates difficult laryngoscopy 1. Inter incisor gap : reduced 2. Three finger test : negative 3. Two finger test : negative / positive 4. One finger test : negative 5. Mallampati grade : cannot be assessed 6. Palate configuration : cannot be assessed 7. Upper lip bite test : negative
• Why difficult supraglottic device insertion?
• No mouth opening / < 1 cm
• What if there is partial restriction?
• Restriction of movement of tongue away from airway preventing tongue displacement • Hinders insertion of rigid laryngoscopy • Minimum mouth opening required for insertion of supraglottics is approx 2 cm
• Would you like to use sedatives?
• Sedatives best avoided in premedication : - reduce arousal and ventilatory responses to hypoxia and hypercapnia - worsen OSA by reducing pharyngeal muscle tone, thereby increasing the likelihood of upper airway collapse. • If associated with OSA, risk is increased : - increased sensitivity to central depressants - perioperative risk of apnoea and desaturation
• How will you deliver anaesthesia to this patient?
– Awake Nasal Fibre-optic guided intubation – gold standard – Followed by general anaesthesia
• What are your other airway management options?
• Trachlight nasal intubation • Seeing optic stylet (SOS) aided intubation • Flexible airway scope tool (FAST) aided intubation • Blind awake nasal intubation (Paediatric patient) • Retrograde nasotracheal intubation • Tracheostomy /tracheotomy
• How would you prepare him for awake nasal fibreoptic?
– Psychological preparation by explaining the technique, – Anxiolytics – Antisialogogues – Antiemetics – Nasal decongestants
• How would you obtain local anaesthesia?
– Spray as you go – Different blocks – Sprays, nebulisation, gargles
• What problem do you anticipate while intubating with fibreoptic?
– Fixed jaw deformity – Distorted soft tissue anatomy – Position of the larynx may be altered – No mouth opening – Inability to protrude the tongue and lift epiglottis – Inability to negotiate the tip of fiberoptic
• How would you solve your problem?
• Ask the patient to phonate
• What will you do if you encounter bleeding in the passage?
• Suction through other nostril • Withdraw the fiberscope and reinsert • Use light wand • Insert a ETT first till the end posterior nares or oropharynx and the pass the fibreoptic through the tube – could bypass the blood
• What would be your technique if this patient is uncooperative ?
• Under inhalational anaesthesia • Light sedation + lignocaine + propofol
• How would you manage if the patient sustains laryngospasm while intubating blindly?
• Bilateral Superior laryngeal nerve block would make mask ventilation possible
• What other technique would you keep ready before starting ?
• Cricothyrotomy with transtracheal jet ventilation would be safest • Fastest would be needle cricothyrotomy • Surgical tracheostomy should be the last option.
• How will you extubate this patient?
• Awake • Complete reversal of NMD • Extubate over ventilating stylet
Summarize • TMJ ankylosis patients have limited mouth opening and facial deformity • Usually associated with OSA • This leads to DMV, DL & I, DSI • Awake fiberoptic is the technique of choice • Fiberoptic technique could be difficult because of limited mouth opening and relatively large tongue • Alternative technique could be inhalational + sedation • Extubation should be awake

PBC neck 28 year male posted for contracture release and skin grafting
Questions could be: • Related to – acute burn injury: types, phases, assessment, organs affected, resuscitation with fluids, effects of drugs, electrolyte imbalances, surgery needed – read it yourself • Related to Airway injury: – ACUTE – POST BURN (Contracture)
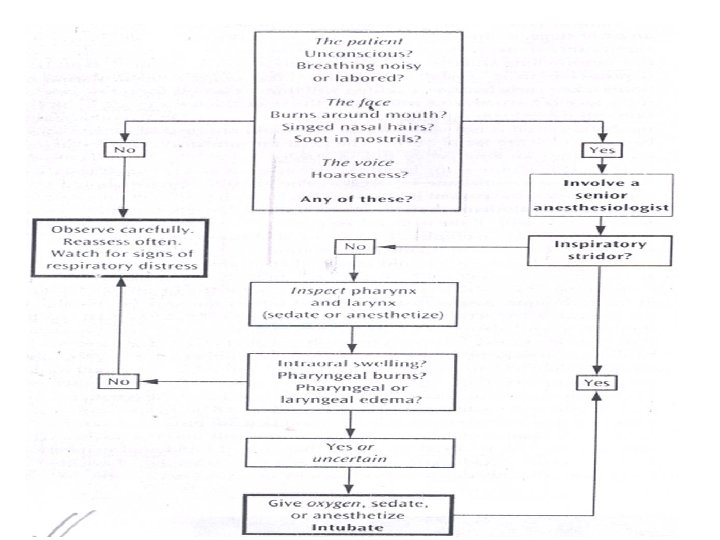
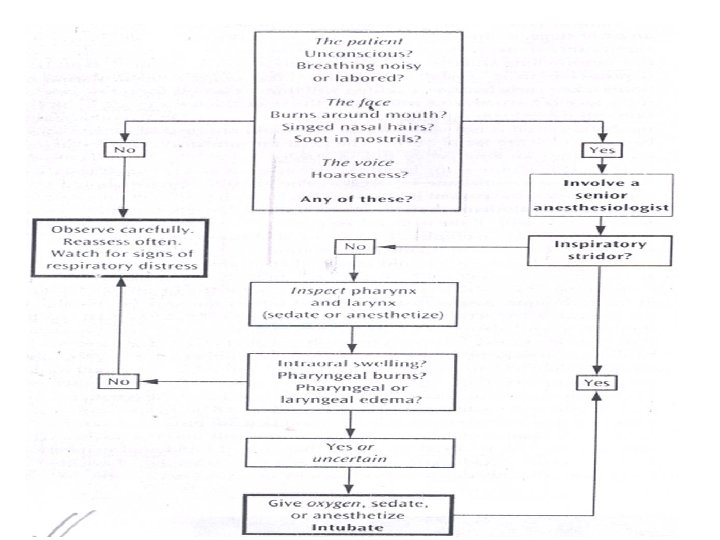
• When do you suspect airway injury?
• if burns in closed space - facial / oral burns - carbonaceous sputum - wheezing / tachypnoea - stridor / hoarseness - singed nasal hairs
• What are the characteristics of acute airway injury?
• Rapid deterioration • Worsens 8 -12 hrs post burn • Aggravated by fluid resuscitation • Sudden severe complete obstruction
• What should be your airway management strategy?
• What are the problems you anticipate while delivering anaesthesia?
• Securing IV lines • Monitoring • Administration of muscle relaxants – Depolarizing – Non-depolarizing • Securing Airway • Positioning the patient
• What are the problems you anticipate while securing airway
• Difficult mask ventilation • Difficult laryngoscopy & intubation • Difficult insertion of supraglottic device • Difficult surgical airway
• Why DMV?
• Reduced mouth opening – difficulty in introducing oral airways • Restricted head & neck movement – limiting sniffing position • Limited jaw movement – unable to lift the mandible • Facial contracture – prevents adequate mask seal over the face Role of using pneumonics? BONES? ? ? ? MOANS
• Why Difficult laryngoscopy and intubation?
• MP grading? ? ? • LEMON • Sniffing position • Inadequate mouth opening • Non-compliant submandibular space • Anterior larynx • Larynx shifted from midline • Inability to apply BURP, OELM
• Why Difficult insertion of supraglottics?
• Restricted mouth opening • Distorted pharyngeal and laryngeal anatomy • Inadequate head extension (< 90 between oral and pharyngeal axes, Ishimura, 1994)
• Why difficult surgical airway?
• Scar in the anterior aspect of neck • Anatomical landmark – site cannot be located • Extension not possible – inadequate space • Thick scar anterior aspect of neck – identification of structures not possible • Fibrotic scar - Incision leads excessive bleading
• How would you intubate?
• Awake Fibreoptic intubation (nasal & oral) • If mouth opening > 2 fingers and definitive airway is needed - ILMA aided intubation, Airtraq, Video laryngoscopes (Mcgrarth, C-Mac, PCD, Kings Vision, etc) • If mouth opening > 2 fingers and definitive airway not needed, LMA could be a choice • If mouth opening < 2 fingers and definitive airway not needed, Combitube, LTS, could be a choice • Contracture release followed by ETI, LMA, ILMA etc
• Remember the option that can never be a choice - ?
• Why difficult Extubation – Any patients with difficult intubation should be considered as difficult extubation
Summarize • Early definitive airway in acute airway burn injury • Could have difficult MV, ETI, SG, EXT • Causcious with muscle relaxants • Awake intubation – technique of choice • Awake extubation

MAXILLOFACIAL INJURY • A 28 year old male patient was involved in a motor vehicle accident and sustained maxillary and mandibular # posted for dental wiring
1. Anticipation of difficult airway / assessment of difficult airway 2. Difficulties expected while proceeding with the technique 3. How do you prepare the patient 4. What is the technique of choice 5. How would you overcome those trouble shooting / difficulties 6. Alternative techniques available / could be undertaken 7. How would you fix the ET tube 8. What precautions would you take while extubation.
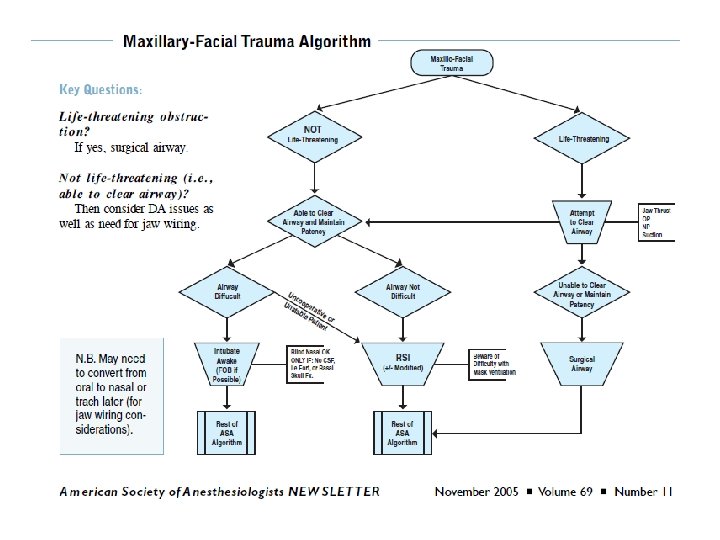
• Is the patient conscious? • Is he/she breathing spontaneously? • What is the extent, composition and the anatomy of the airway? • How extensive is the damage to the bony structures of the face? • Is there a limitation in mouth opening? Is that limitation the result of pain & after sedation the mouth could be opened wider? • Is there soft tissue edema & pressure on the airway?
• L-E-M-O-N: – Look externally – Evaluate 3 -3 -2 rule – Mallampati classification – Obstruction – Neck mobility
1. Anticipation of difficult airway / assessment of difficult airway 2. Difficulties expected while proceeding with the technique 3. How do you prepare the patient 4. What is the technique of choice 5. How would you overcome those trouble shooting / difficulties 6. Alternative techniques available / could be undertaken 7. How would you fix the ET tube 8. What precautions would you take while extubation.
1. Postero-inferior displacement of a fractured maxilla parallel to the inclined plane of the skull base. 2. A bilateral fracture of the anterior mandible. 3. Haemorrhage. 4. Soft tissue swelling and edema. 5. Trauma to the larynx and trachea. 6. Foreign bodies- dentures, debris, shrapnel, exfoliated teeth, bone fragments. 7. C-spine injury 8. Full stomach
1. Anticipation of difficult airway / assessment of difficult airway 2. Difficulties expected while proceeding with the technique 3. How do you prepare the patient 4. What is the technique of choice 5. How would you overcome those trouble shooting / difficulties 6. Alternative techniques available / could be undertaken 7. How would you fix the ET tube 8. What precautions would you take while extubation.
• Monitoring equipments • Oxygenation equipments • Wide bore Suction catheter (Yankauer) • I. V. access & premedication • Intubation equipments • Gum elastic bougie • Surgical or needle cricothyrodotomy kit • Equipments for checking tube position • Prevention of gastric aspiration • Patient positioning
1. Anticipation of difficult airway / assessment of difficult airway 2. Difficulties expected while proceeding with the technique 3. How do you prepare the patient 4. What is the technique of choice 5. How would you overcome those trouble shooting / difficulties 6. Alternative techniques available / could be undertaken 7. How would you fix the ET tube 8. What precautions would you take while extubation.
• The approach depends upon the patient’s • injuries, • airway status and • the care provider’s experience with such equipment & procedures. • There is no single universal technique of intubation which may be favorable in all circumstances.
• Regardless of the associated injuries, the primary means of securing the airway in the vast majority of acutely desaturating patients with maxillofacial trauma is awake orotracheal intubation via direct laryngoscopy.
• What are the key questions?
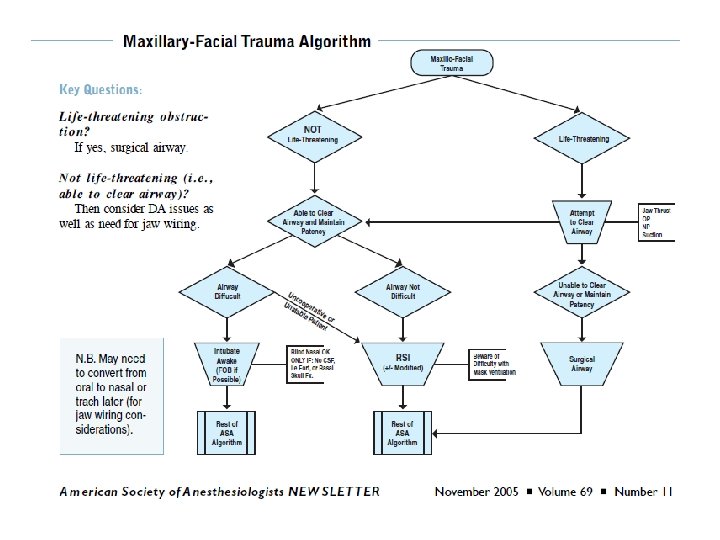
• What are the problems associated?
• Uncooperative patient. • Local anaesthetic preparation is time consuming, may increase the risk of aspiration and constant bleeding into the airway is likely to prevent effective local anaesthesia. • During routine laryngoscopy and intubation, presence of blood would interfere with the visibility of glottis. • ? Associated Cervical fracture
What next? • Intubation attempts under induction of General anesthesia is the next step. • Induce with inhalational anaesthetic. • Do not give muscle relaxant. • Now, attempt with Routine laryngoscopy.
1. Anticipation of difficult airway / assessment of difficult airway 2. Difficulties expected while proceeding with the technique 3. How do you prepare the patient 4. What is the technique of choice 5. How would you overcome those trouble shooting / difficulties 6. Alternative techniques available / could be undertaken 7. How would you fix the ET tube 8. What precautions would you take while extubation.
• Patients with bilateral mandibular body fractures are especially at risk for tongue base prolapse • Tongue retraction with a heavy suture or towel clamp will allow oxygenation until a definitive airway is secured.
• Suction is often necessary to clear pharyngeal secretions and bleeding. • Visualization of the larynx may be improved with cricoid pressure by an assistant.
• In patients where visualization of the true vocal cords is still difficult, some have described the use of a gum elastic bougie.
• Many level 1 trauma centers immobilize the entire spine in all blunt trauma patients until spinal injury can be disproved clinically and/or radiographically.
• RSI for full stomach. • Magill’s forceps to remove foreign bodies.
1. Anticipation of difficult airway / assessment of difficult airway 2. Difficulties expected while proceeding with the technique 3. How do you prepare the patient 4. What is the technique of choice 5. How would you overcome those trouble shooting / difficulties 6. Alternative techniques available / could be undertaken 7. How would you fix the ET tube 8. What precautions would you take while extubation.
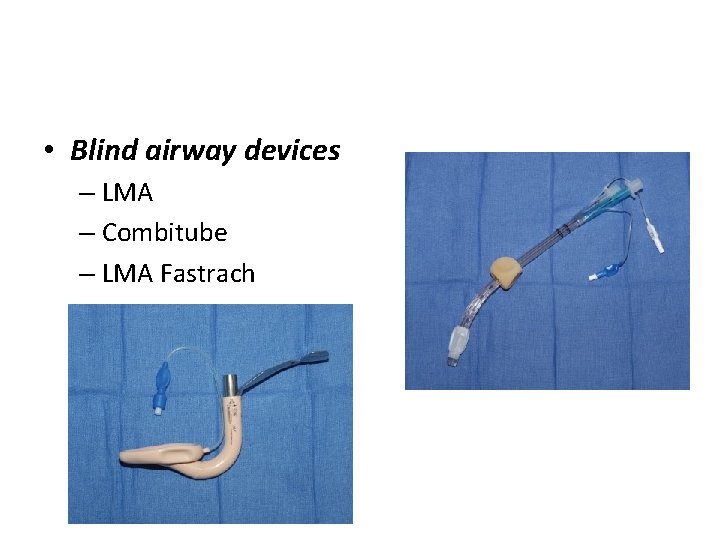
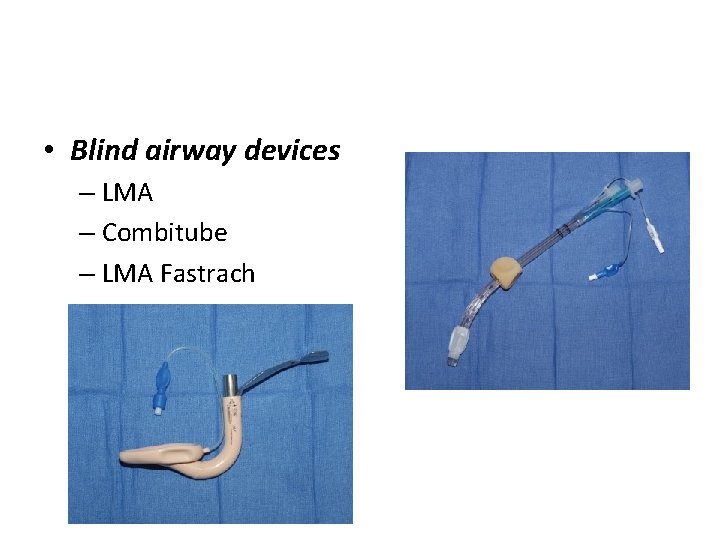
• Blind airway devices – LMA – Combitube – LMA Fastrach
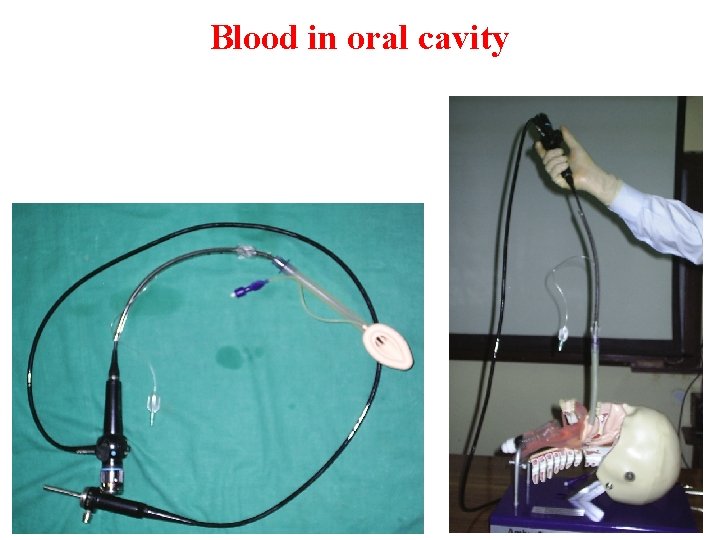
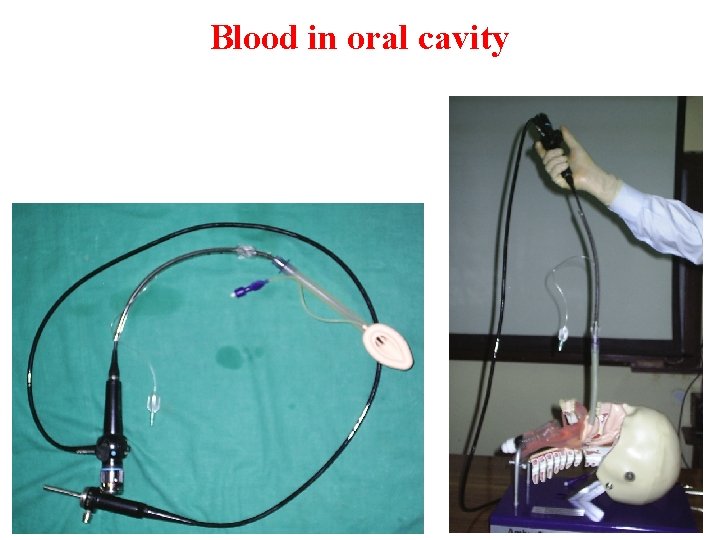
Blood in oral cavity
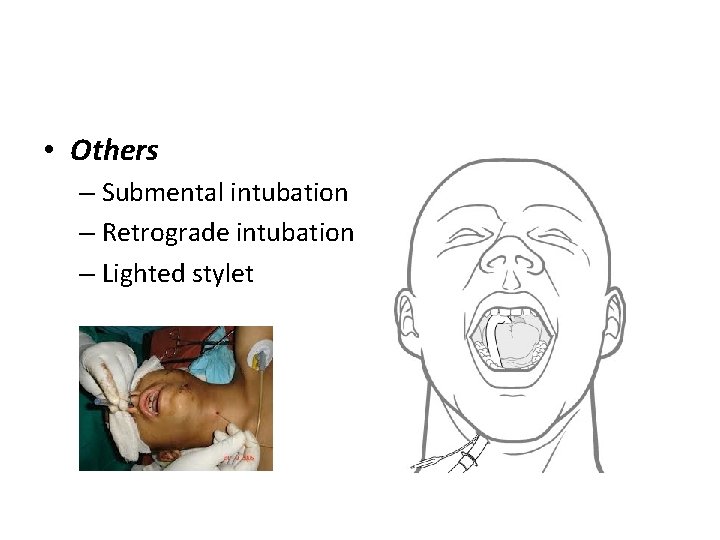
• Others – Submental intubation – Retrograde intubation – Lighted stylet
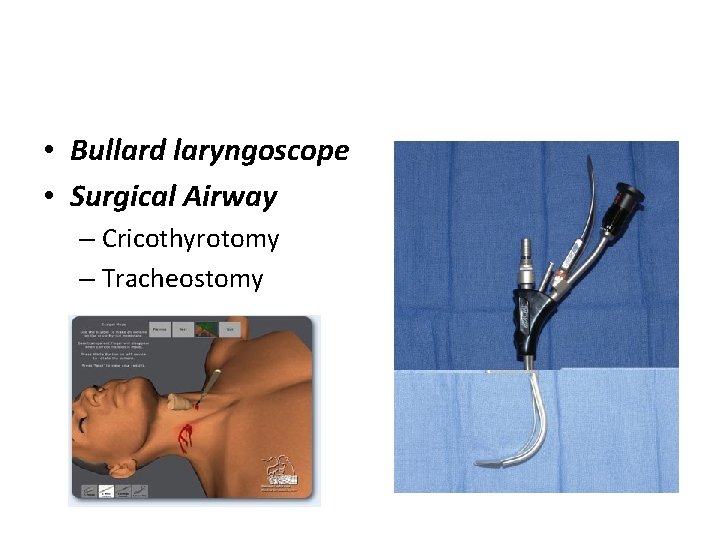
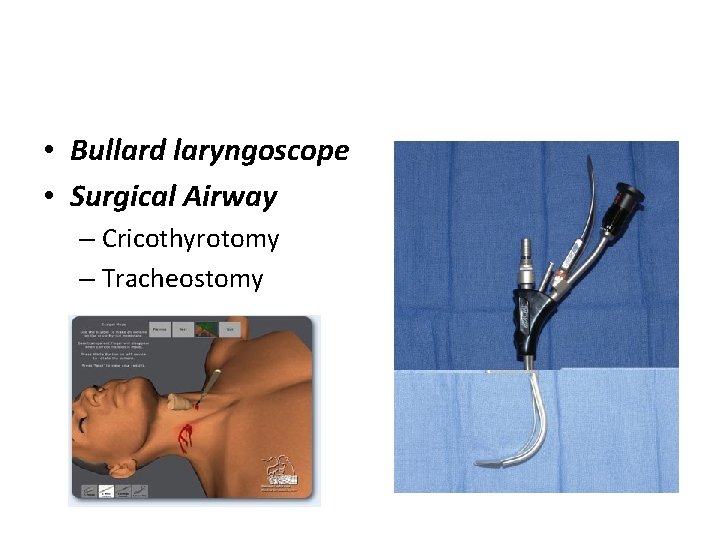
• Bullard laryngoscope • Surgical Airway – Cricothyrotomy – Tracheostomy
1. Anticipation of difficult airway / assessment of difficult airway 2. Difficulties expected while proceeding with the technique 3. How do you prepare the patient 4. What is the technique of choice 5. How would you overcome those trouble shooting / difficulties 6. Alternative techniques available / could be undertaken 7. How would you fix the ET tube 8. What precautions would you take while extubation.
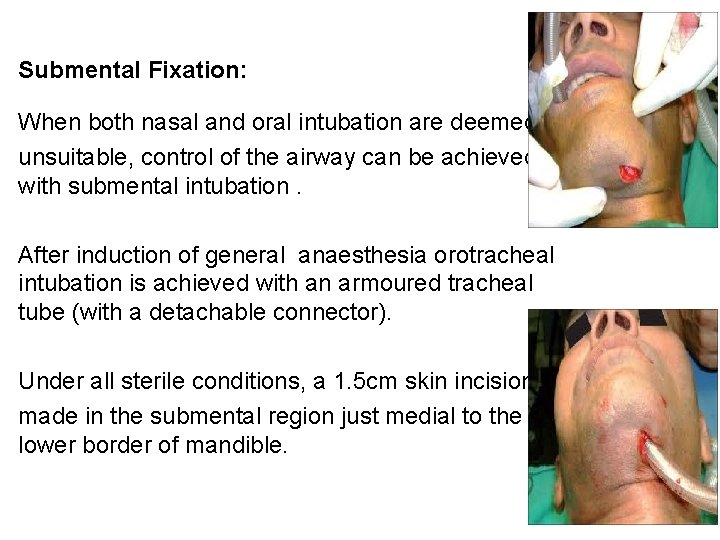
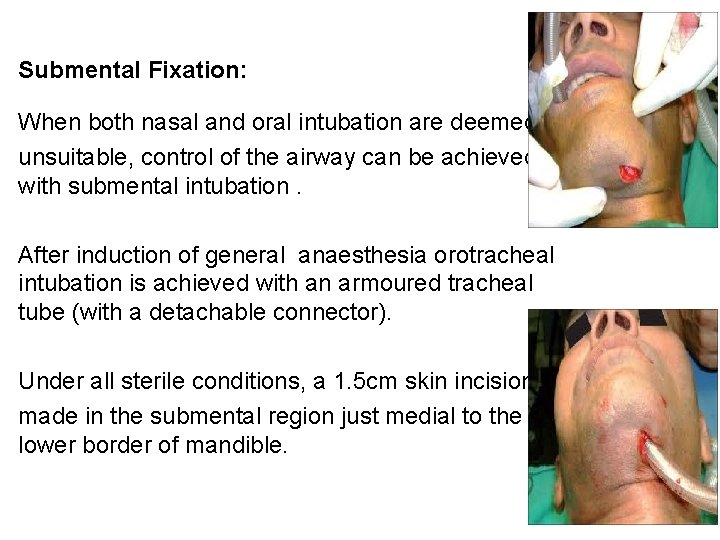
Submental Fixation: When both nasal and oral intubation are deemed unsuitable, control of the airway can be achieved with submental intubation. After induction of general anaesthesia orotracheal intubation is achieved with an armoured tracheal tube (with a detachable connector). Under all sterile conditions, a 1. 5 cm skin incision is made in the submental region just medial to the lower border of mandible.
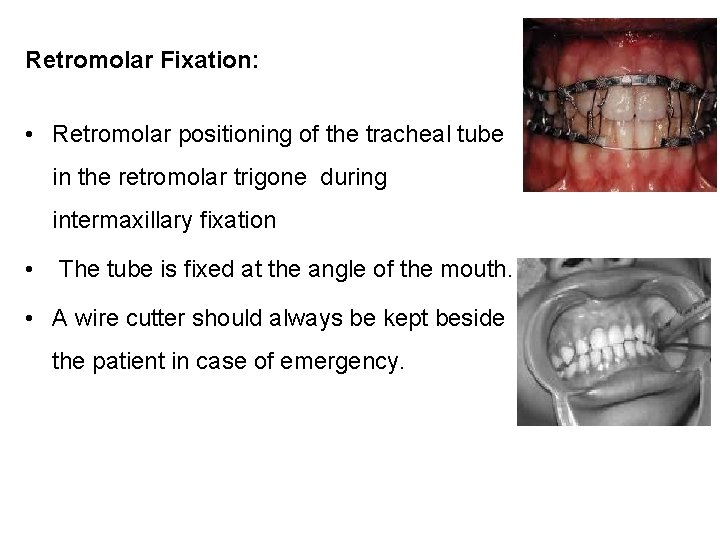
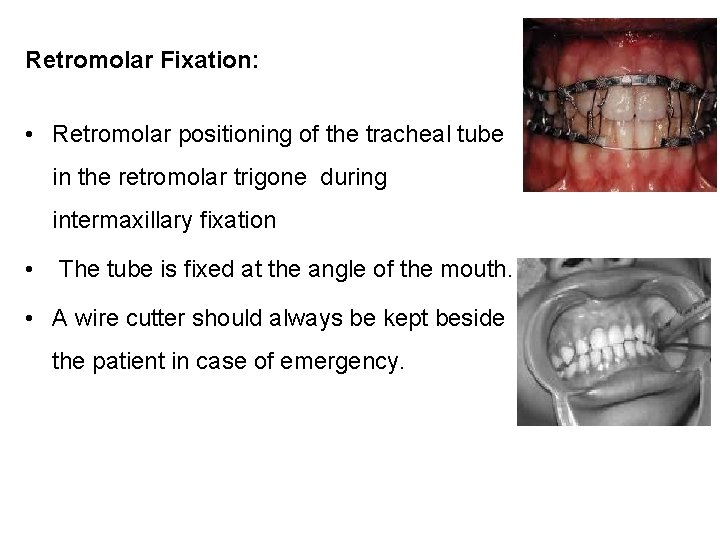
Retromolar Fixation: • Retromolar positioning of the tracheal tube in the retromolar trigone during intermaxillary fixation • The tube is fixed at the angle of the mouth. • A wire cutter should always be kept beside the patient in case of emergency.
1. Anticipation of difficult airway / assessment of difficult airway 2. Difficulties expected while proceeding with the technique 3. How do you prepare the patient 4. What is the technique of choice 5. How would you overcome those trouble shooting / difficulties 6. Alternative techniques available / could be undertaken 7. How would you fix the ET tube 8. What precautions would you take while extubation.
• Extubation should be deferred until normal anatomy is restored or at least until the edema subsides. • Close and continuous monitoring. • Preparation for re-intubation. • Steroids. • Wire cutters.
Summarize • • • Could be routine or emergency presentation Anticipated difficult airway No definite technique of choice If not bleeding orally fiberoptic Variety of alternative techniques Scope of Submental / Retromolar intubation Fixation of tube could be difficult Plan for extubation / keep wire cutter ready
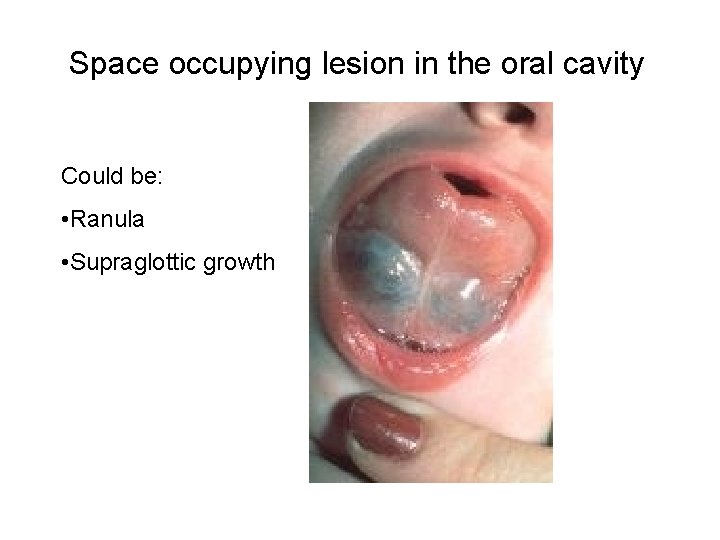
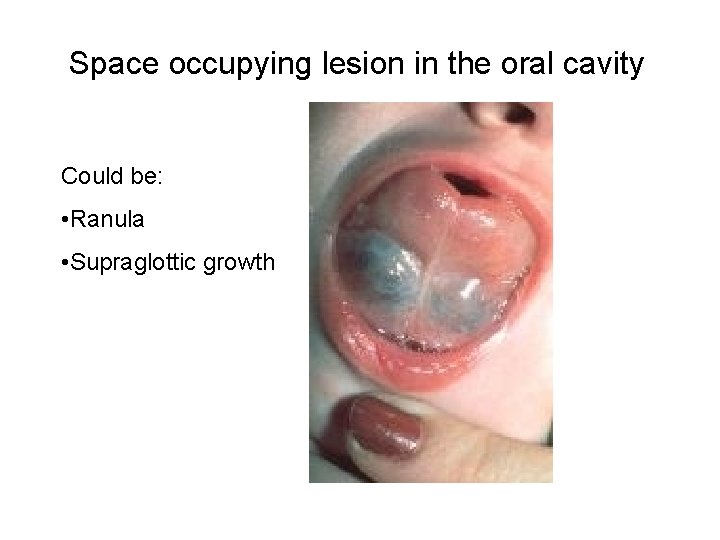
Space occupying lesion in the oral cavity Could be: • Ranula • Supraglottic growth
• What are the anatomical considerations one should enquire
• Size • Location • Extension
• What specific history you would like to elicit?
• Change in voice • H/O of sleep apnea • Position one is comfortable during sleep
• What specific examinations are important for you?
• Size, location of growth • Mouth opening • Distortion of the lower jaw • Indirect larygoscopy • Pliability of submandibular space
• Specific investigations you would advice preoperatively?
• X-Ray Neck – AP, lateral • CT neck • Indirect laryngoscopy
• What are the challenges faced by an anaesthetist
• Optimisation of disease (malnutrition, infection • Previous surgery distorting the airway anatomy • Radiotherapy and chemo therapy can lead to fibrosis of oral tissues and restricting movements /reduce compliance • Friable growth leading to sudden uncontrolled bleeding • Aspiration of blood / tumor debris
• What are the difficulties you anticipate while maintaining airway?
• Difficult mask ventilation • Prolonged laryngoscopy time • Difficulty in placement of ETT
• Does previous uneventful airway management guarantee subsequent smooth airway management?
• Anatomy may be changed due growth or surgery • Post surgical healing with fibrosis • Post operative radiation induced fibrosis
• What are the implications of non-compliant submandibular space?
• Non-compliant sub-mandibular space will not allow the base of the tongue to be depressed during laryngoscopy. • Patient will present anterior / superior larynx
• What will be your intubation technique?
• Awake fiberoptic technique of choice • Trachlight aided intubation (Ranula) • Retrograde intubation • Direct laryngoscopy intubation
• How will you prepare this patient for awake intubation?
• Psychological preparation • Premedication with mild sedation + analgesic + anti-sialogogue • Instillation of vasoconstrictor • Topical administration of local anaesthetic to the airway using 4% xylocaine, 4% xylocaine gargle • “Spray-as-you-go” with local anaesthetic?
• Will you perform nerve blocks?
• Best to avoid because – Could cause direct extension of the tumor secondary to trauma from needle passing through the tumor – Normal anatomy could be distorted
• What will you do if you lose control of airway in this case?
• Emergency transtracheal jet ventilation • Needle cricothyrotomy and oxygenation
• Do you anticipate any problem during extubation of the trachea
• Yes, because of the following reasons – – surgical manipulation can lead to edema of the airway causing post extubation obstruction – Damage of recurrent laryngeal nerve / vocal cord paralysis if neck dissection
• What precaution will you take prior to and after extubation
• Use of intraoperative dexamethasone to reduce edema formation • Awaken the patient prior to extubation • Wait for complete reversal of NMB • Extubate over jet stylet • Nurse the patient postoperative in head-up position for 12 – 24 hours • Keep a tracheostomy kit ready
Summarize Assessment of the growth Previous history is important Investigations before deciding for technique Technique to be decided on the basis of the growth • Avoid nerve blocks • No supraglotics • Extubation should be with caution • •
• • • Bubbling with questions? ? ?
• Thank you for asking • At least you were awake