Problematic platelets Phase 2 a Lecture 11 th
Problematic platelets Phase 2 a Lecture 11 th December 2015 University of Sheffield Medical School Dr Stephanie Stone Spr Haematology Sheffield Teaching Hospitals www. ifm. liu. se
Overview • Normal physiology of platelets • Platelet abnormalities – focus on thrombocytopenia • Clinical features of thrombocytopenia and platelet disorders • Important causes of thrombocytopenia
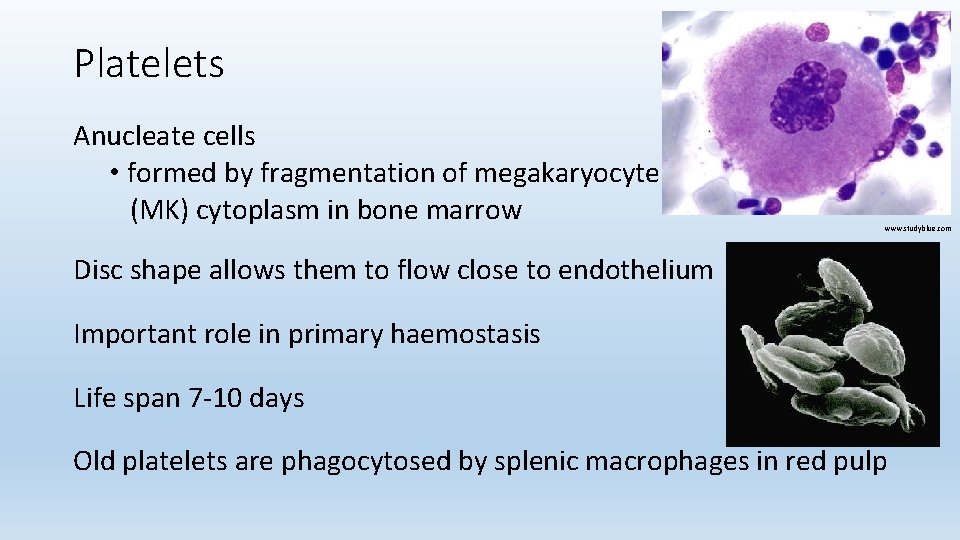
Platelets Anucleate cells • formed by fragmentation of megakaryocyte (MK) cytoplasm in bone marrow www. studyblue. com Disc shape allows them to flow close to endothelium Important role in primary haemostasis Life span 7 -10 days Old platelets are phagocytosed by splenic macrophages in red pulp

Control of platelet production TPO Thrombopoietin (TPO): produced mainly by liver TPO • Stimulates production of platelets by megakaryocytes • Binds to platelet and MK receptors • ↓plts = less bound TPO = ↑ free TPO able to bind to MK = ↑ Plt prodn www. studyblue. com

Platelet activation & role in primary haemostasis Collagen v. WF Ca Spreading Release of granule contents n Xa-Va 2+ ge Ca AD P ino Fibrin clot r fib bin m o hr t www. ifm. liu. se Aggregation
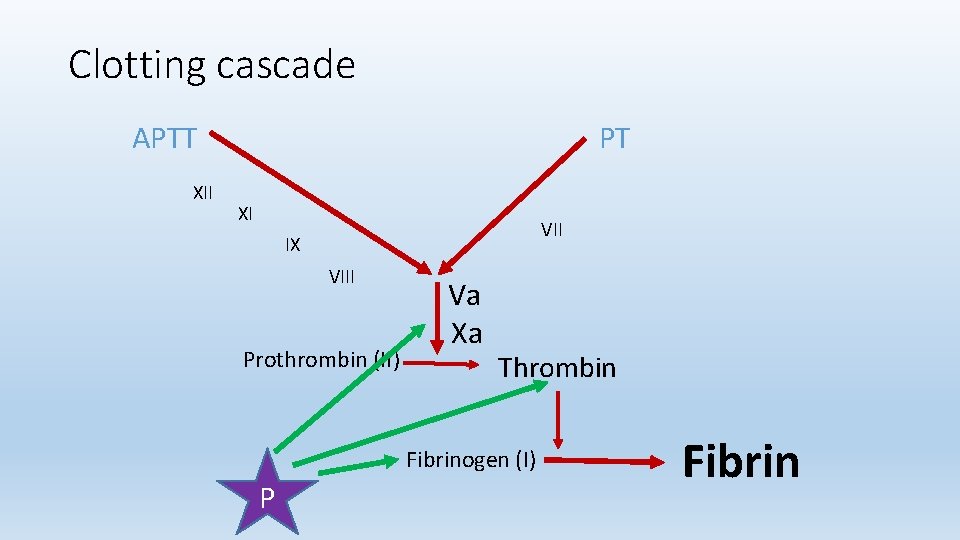
Clotting cascade APTT XII PT XI VII IX VIII Prothrombin (II) Va Xa Thrombin Fibrinogen (I) P Fibrin
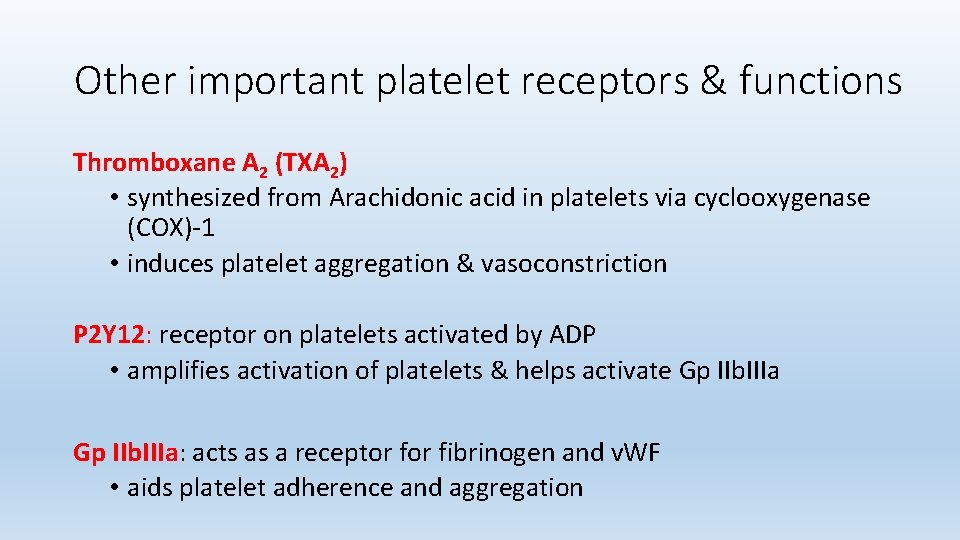
Other important platelet receptors & functions Thromboxane A 2 (TXA 2) • synthesized from Arachidonic acid in platelets via cyclooxygenase (COX)-1 • induces platelet aggregation & vasoconstriction P 2 Y 12: receptor on platelets activated by ADP • amplifies activation of platelets & helps activate Gp IIb. IIIa: acts as a receptor fibrinogen and v. WF • aids platelet adherence and aggregation
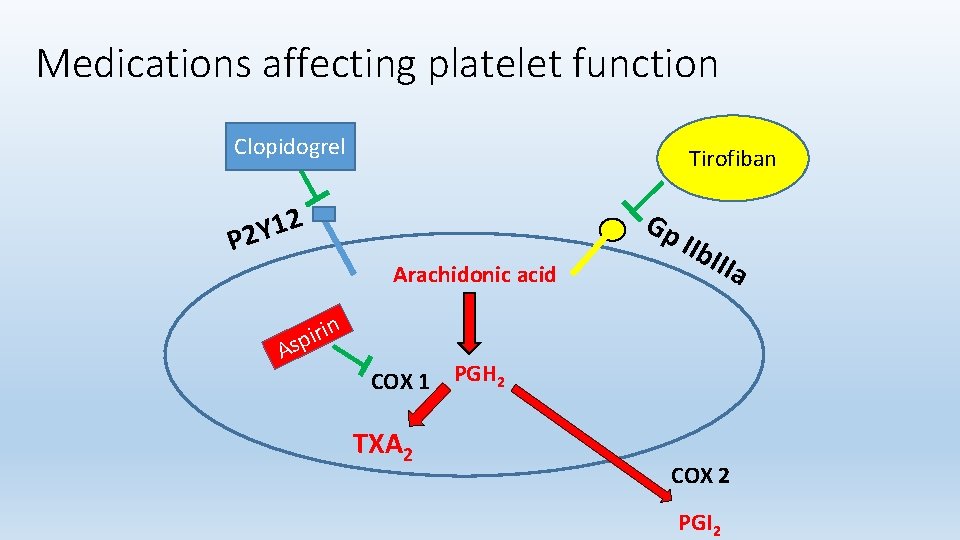
Medications affecting platelet function Clopidogrel Tirofiban 2 1 Y P 2 Gp Arachidonic acid A n i r i sp IIb IIIa COX 1 PGH 2 TXA 2 COX 2 PGI 2
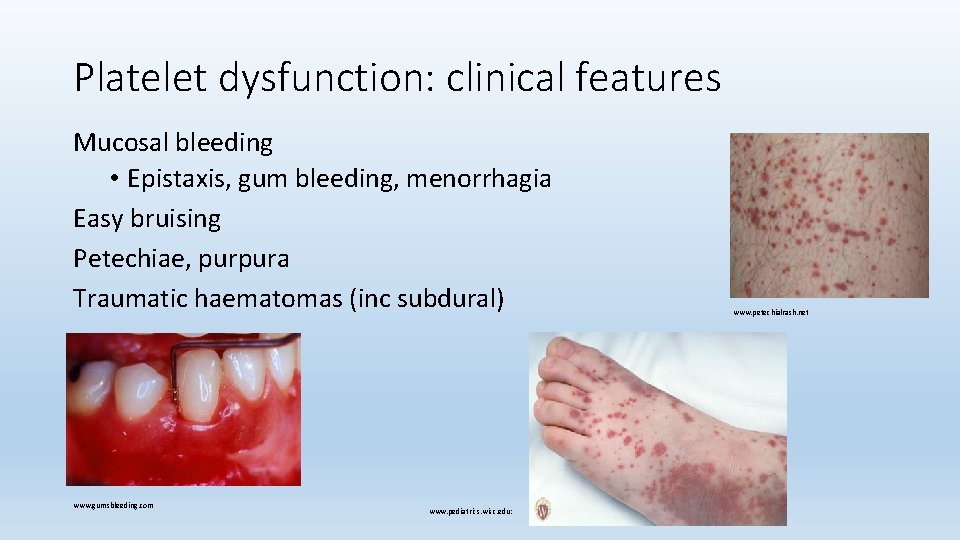
Platelet dysfunction: clinical features Mucosal bleeding • Epistaxis, gum bleeding, menorrhagia Easy bruising Petechiae, purpura Traumatic haematomas (inc subdural) www. gumsbleeding. com www. pediatrics. wisc. edu: www. petechialrash. net
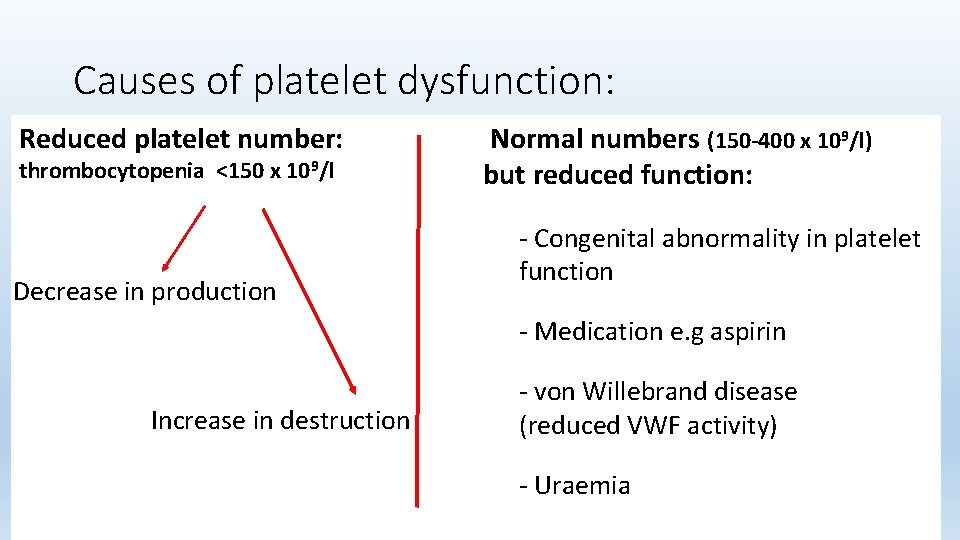
Causes of platelet dysfunction: Reduced platelet number: thrombocytopenia <150 x 109/l Decrease in production Normal numbers (150 -400 x 109/l) but reduced function: - Congenital abnormality in platelet function - Medication e. g aspirin Increase in destruction - von Willebrand disease (reduced VWF activity) - Uraemia
Thrombocytopenia: decreased production Congenital thrombocytopenia • Absent / reduced / malfunctioning megakaryocytes in BM Infiltration of bone marrow • Leukaemia, metastatic malignancy, lymphoma, myelofibrosis
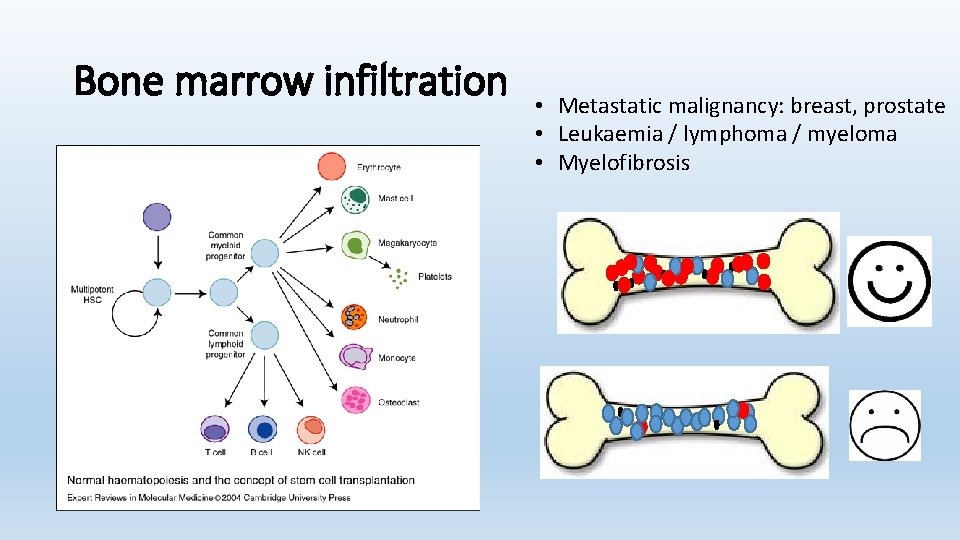
Bone marrow infiltration • Metastatic malignancy: breast, prostate • Leukaemia / lymphoma / myeloma • Myelofibrosis
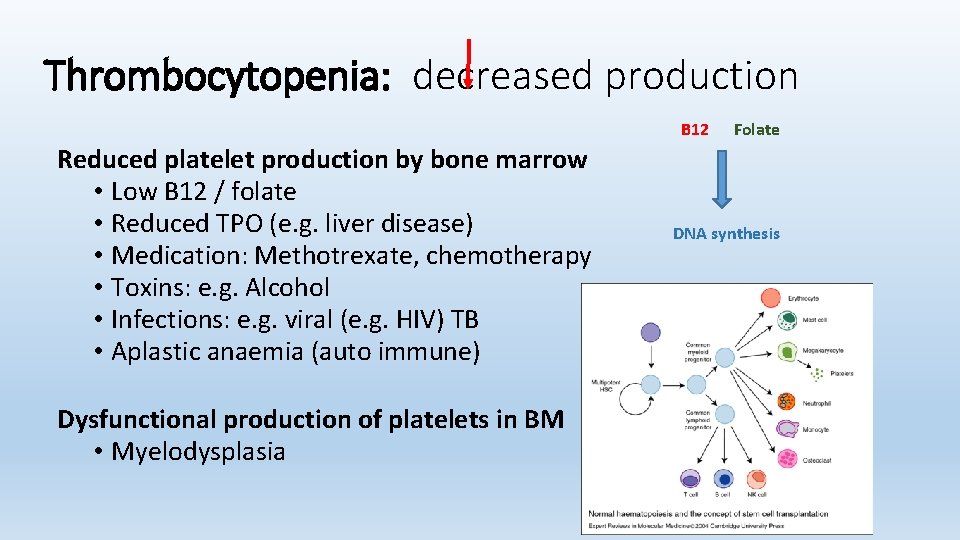
Thrombocytopenia: decreased production B 12 Reduced platelet production by bone marrow • Low B 12 / folate • Reduced TPO (e. g. liver disease) • Medication: Methotrexate, chemotherapy • Toxins: e. g. Alcohol • Infections: e. g. viral (e. g. HIV) TB • Aplastic anaemia (auto immune) Dysfunctional production of platelets in BM • Myelodysplasia Folate DNA synthesis
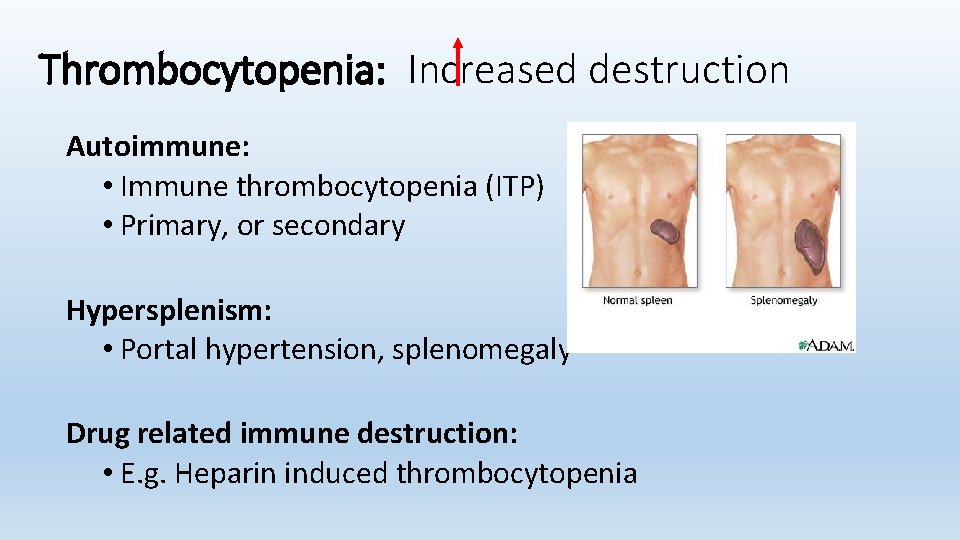
Thrombocytopenia: Increased destruction Autoimmune: • Immune thrombocytopenia (ITP) • Primary, or secondary Hypersplenism: • Portal hypertension, splenomegaly Drug related immune destruction: • E. g. Heparin induced thrombocytopenia

Thrombocytopenia: Increased destruction Consumption of platelets: • Disseminated intravascular coagulopathy (DIC) • Thrombotic thrombocytopenic purpura (TTP) • Haemolytic uraemic syndrome (HUS) • Haemolysis, elevated liver enzymes and low platelets (HELLP) • Major haemorrhage
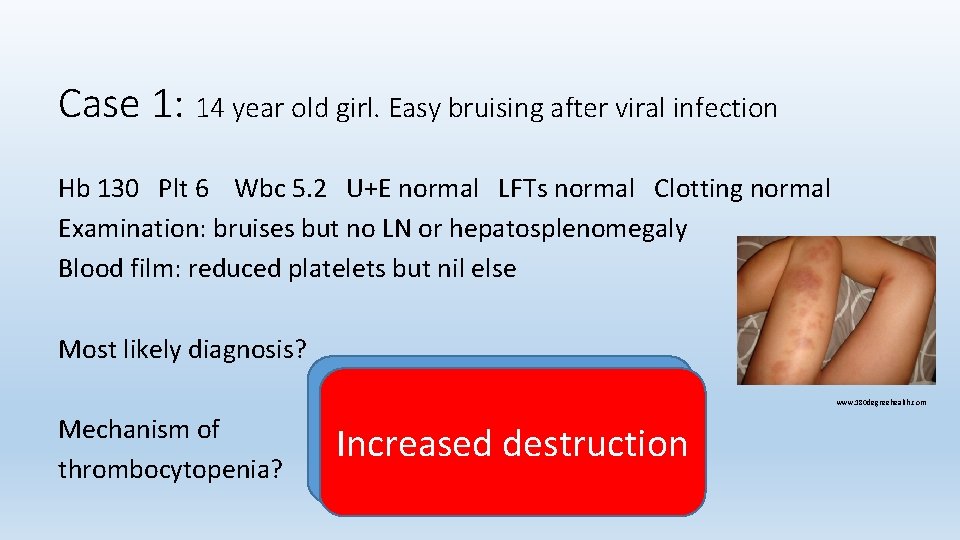
Case 1: 14 year old girl. Easy bruising after viral infection Hb 130 Plt 6 Wbc 5. 2 U+E normal LFTs normal Clotting normal Examination: bruises but no LN or hepatosplenomegaly Blood film: reduced platelets but nil else Most likely diagnosis? Mechanism of thrombocytopenia? Immune Increased destruction thrombocytopenia www. 180 degreehealth. com
Immune thrombocytopenia Ig. G antibodies form to platelet and megakaryocyte surface glycoproteins Opsonized platelets are removed by reticuloendothelial system Primary: • May follow viral infection / immunisation esp in children Secondary: • Occurs in association with some • Malignancies, such as Chronic Lymphocytic Leukaemia (CLL) • Infections e. g. HIV / Hep C
Immune thrombocytopenia Investigations: • • Any underlying cause? Diagnosis of exclusion Treatment: • • Immunosuppression e. g. steroids / IVIG Treat underlying cause If bleeding – give platelets - but will disappear quickly Tranexamic acid • • Inhibits breakdown of fibrin Good for mucosal bleeding but NOT if urinary tract bleeding (clot retention)
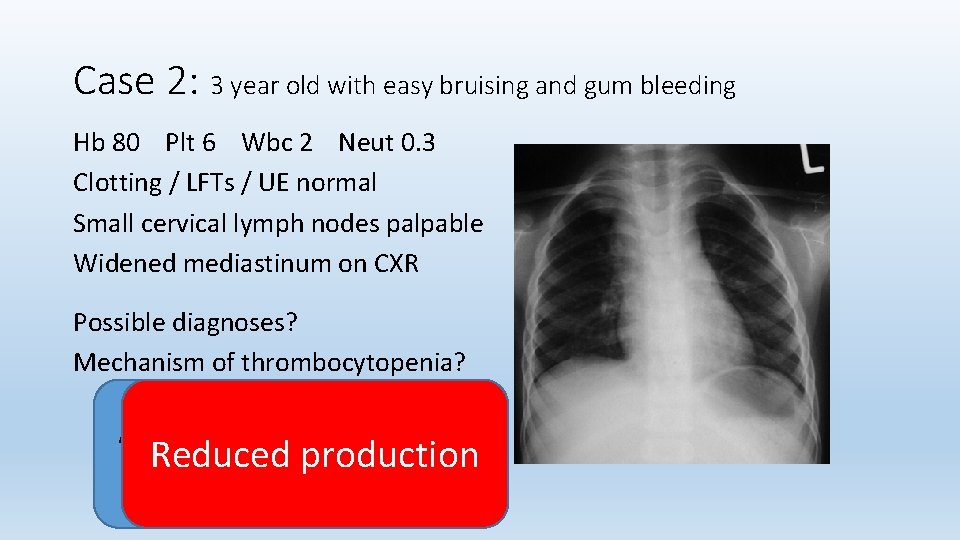
Case 2: 3 year old with easy bruising and gum bleeding Hb 80 Plt 6 Wbc 2 Neut 0. 3 Clotting / LFTs / UE normal Small cervical lymph nodes palpable Widened mediastinum on CXR Possible diagnoses? Mechanism of thrombocytopenia? Acute Lymphoblastic Reduced production Leukaemia
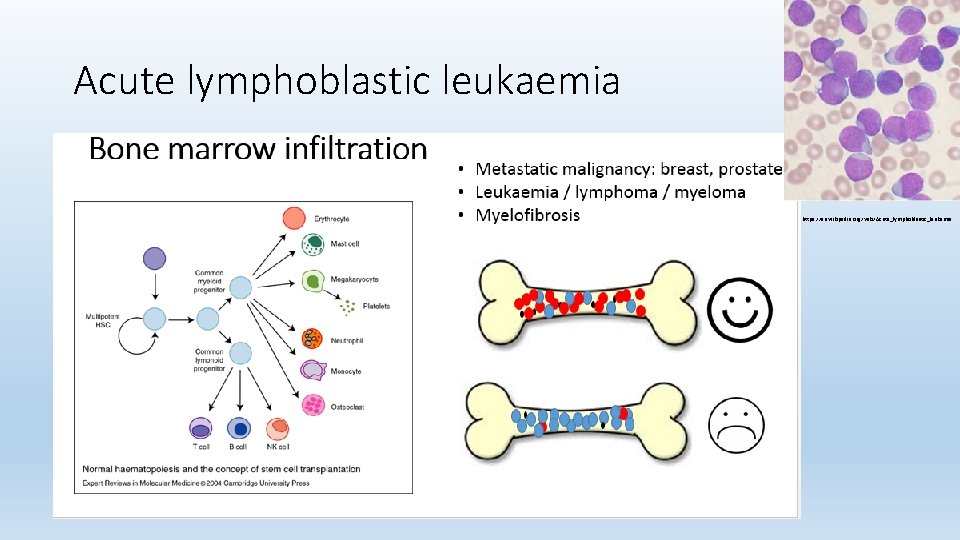
Acute lymphoblastic leukaemia https: //en. wikipedia. org/wiki/Acute_lymphoblastic_leukemia
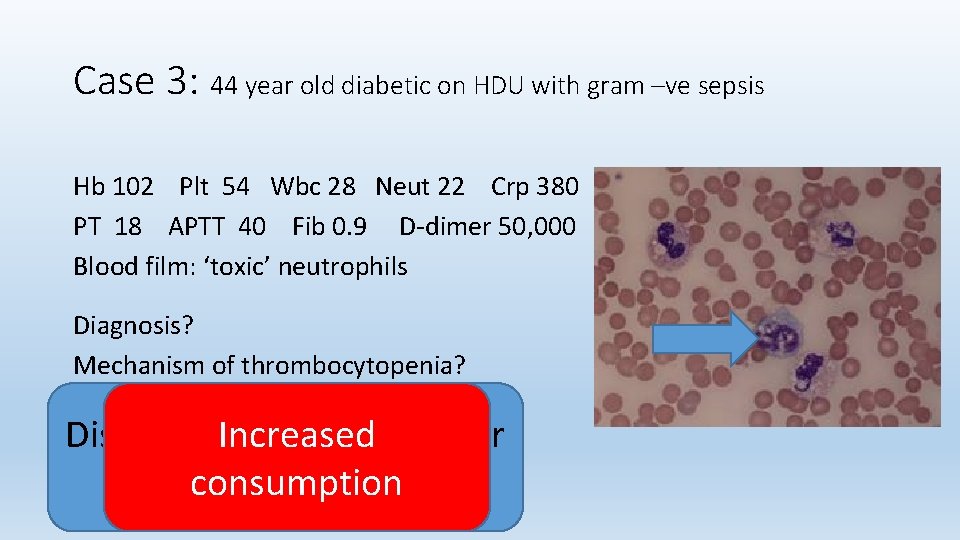
Case 3: 44 year old diabetic on HDU with gram –ve sepsis Hb 102 Plt 54 Wbc 28 Neut 22 Crp 380 PT 18 APTT 40 Fib 0. 9 D-dimer 50, 000 Blood film: ‘toxic’ neutrophils Diagnosis? Mechanism of thrombocytopenia? Disseminated Increased Intravascular Coagulopathy consumption
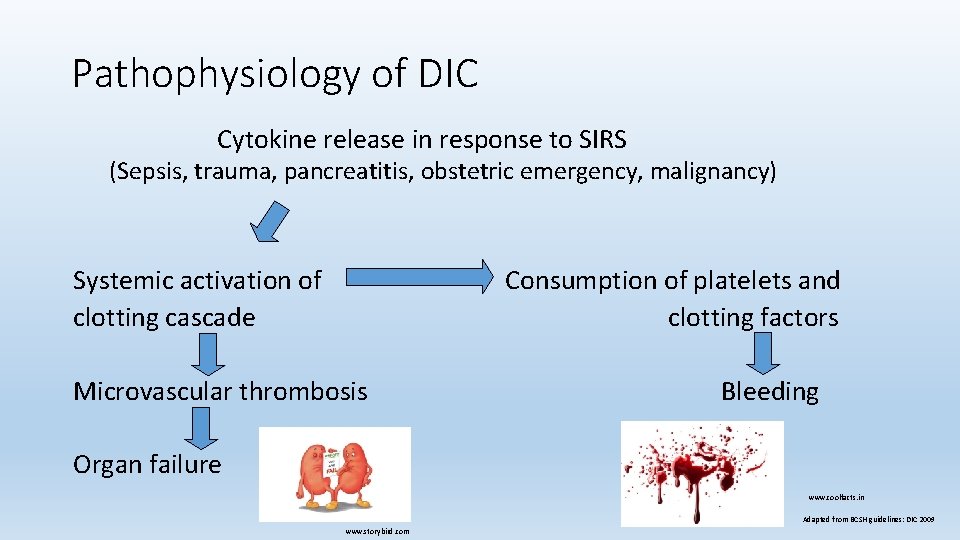
Pathophysiology of DIC Cytokine release in response to SIRS (Sepsis, trauma, pancreatitis, obstetric emergency, malignancy) Systemic activation of clotting cascade Consumption of platelets and clotting factors Microvascular thrombosis Bleeding Organ failure www. coolfacts. in Adapted from BCSH guidelines: DIC 2009 www. storybird. com
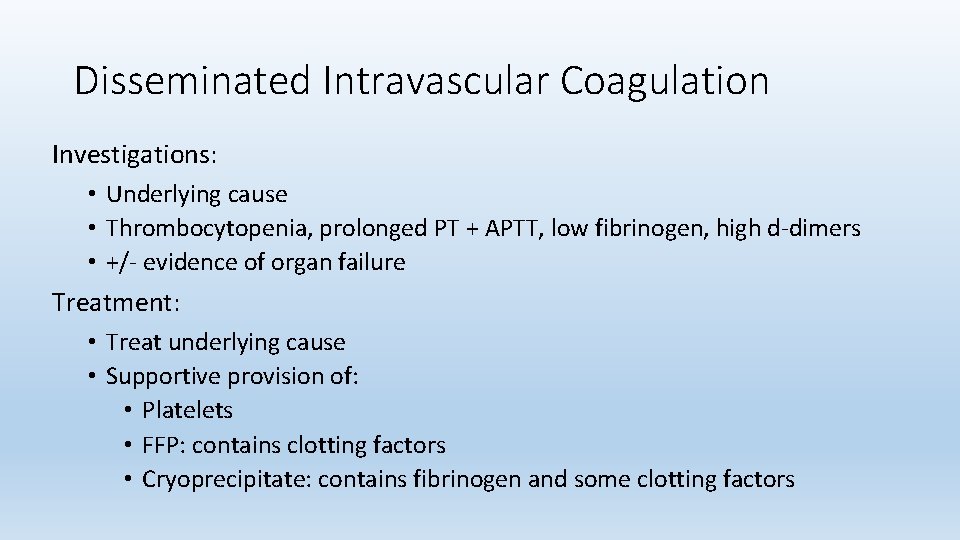
Disseminated Intravascular Coagulation Investigations: • Underlying cause • Thrombocytopenia, prolonged PT + APTT, low fibrinogen, high d-dimers • +/- evidence of organ failure Treatment: • Treat underlying cause • Supportive provision of: • Platelets • FFP: contains clotting factors • Cryoprecipitate: contains fibrinogen and some clotting factors
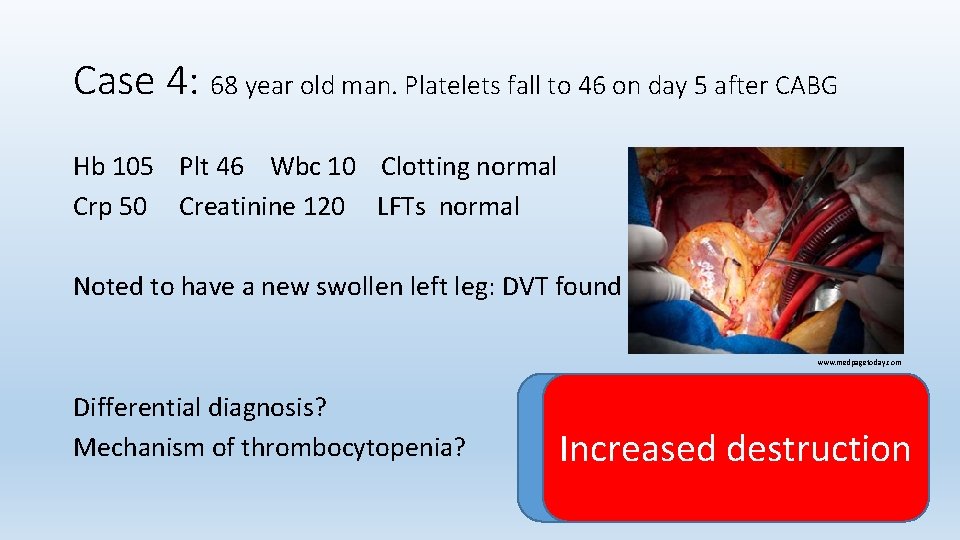
Case 4: 68 year old man. Platelets fall to 46 on day 5 after CABG Hb 105 Plt 46 Wbc 10 Clotting normal Crp 50 Creatinine 120 LFTs normal Noted to have a new swollen left leg: DVT found www. medpagetoday. com Differential diagnosis? Mechanism of thrombocytopenia? Heparin Induced Increased destruction Thrombocytopenia
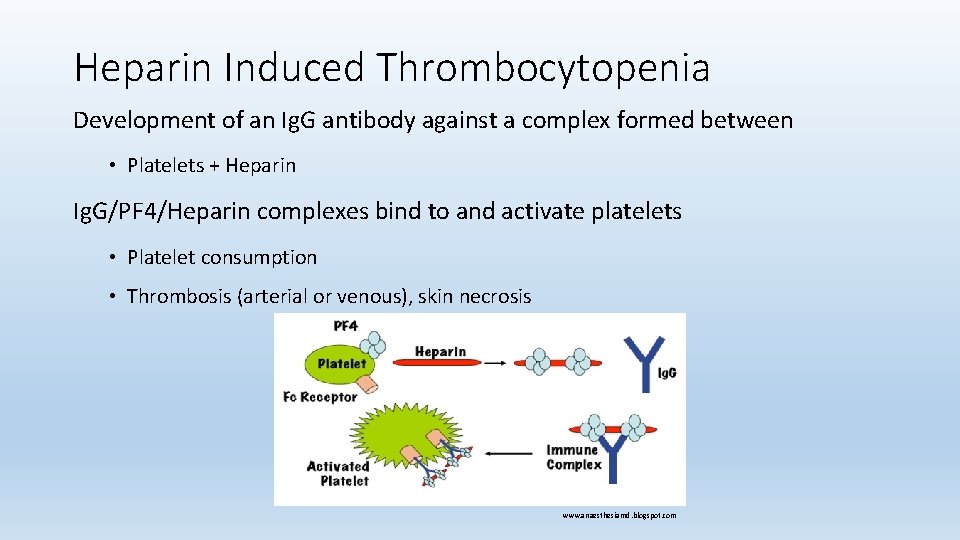
Heparin Induced Thrombocytopenia Development of an Ig. G antibody against a complex formed between • Platelets + Heparin Ig. G/PF 4/Heparin complexes bind to and activate platelets • Platelet consumption • Thrombosis (arterial or venous), skin necrosis www. anaesthesiamd. blogspot. com
Heparin Induced Thrombocytopenia Most at risk: • After cardiac bypass surgery • Unfractionated Heparin treatment • Usual presentation: • Sharp fall in platelets 5 -10 days after starting Heparin treatment Life threatening – need to stop UFH / LMWH Heparin immediately • Alternative anticoagulation (even if platelets low) • Never re-expose patient to Heparin
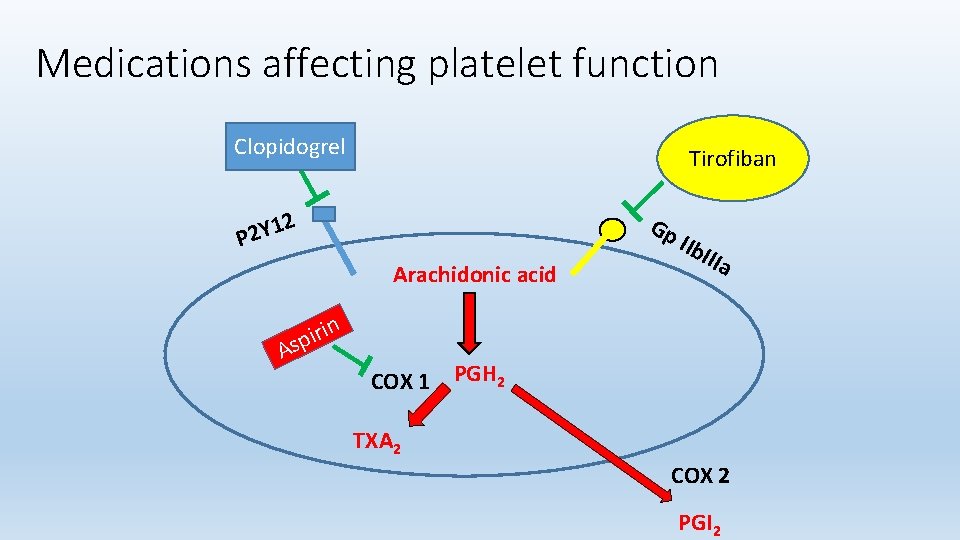
Medications affecting platelet function Clopidogrel Tirofiban 2 Gp 1 P 2 Y Arachidonic acid A n i r i sp IIb IIIa COX 1 PGH 2 TXA 2 COX 2 PGI 2
Summary Platelets – highly active cells • Life cycle: BM - circulation - spleen • Production under influence of TPO Dysfunction in platelet activity: • Too few around: thrombocytopenia • Decreased production • Increased consumption or destruction • Reduced function: • E. g. Aspirin www. ftalk. us
Any Questions? www. fbnotebook. com www. doccartoon. blogspot. com www. fbnotebook. com
- Slides: 29