Prior Authorization Trends 2020 Presented by Revenue Cycle

Prior Authorization Trends 2020 Presented by Revenue Cycle Advancement Center
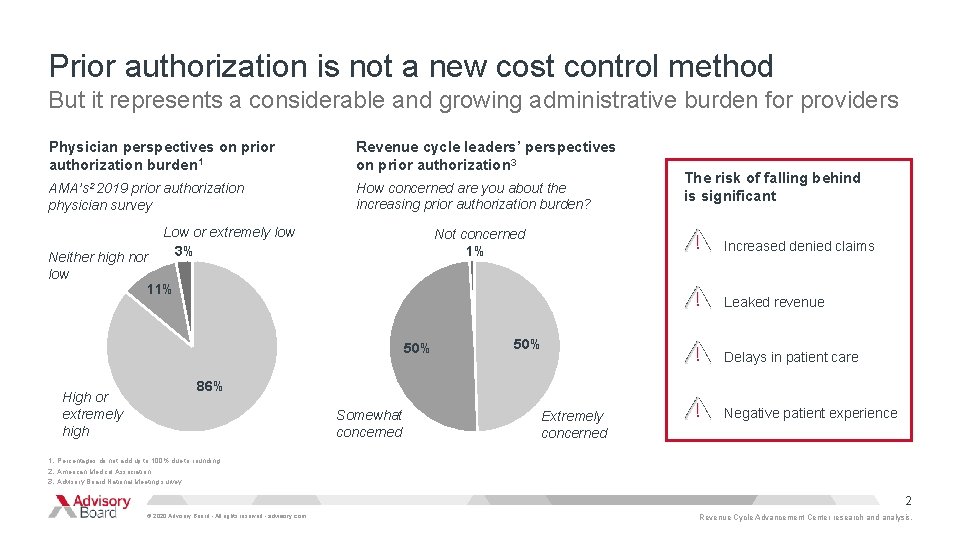
Prior authorization is not a new cost control method But it represents a considerable and growing administrative burden for providers Physician perspectives on prior authorization burden 1 Revenue cycle leaders’ perspectives on prior authorization 3 AMA’s 2 2019 prior authorization physician survey How concerned are you about the increasing prior authorization burden? Low or extremely low 3% Not concerned 1% Neither high nor low 11% Increased denied claims Leaked revenue 50% High or extremely high The risk of falling behind is significant 50% Delays in patient care 86% Somewhat concerned Extremely concerned Negative patient experience 1. Percentages do not add up to 100% due to rounding. 2. American Medical Association. 3. Advisory Board National Meeting survey. 2 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
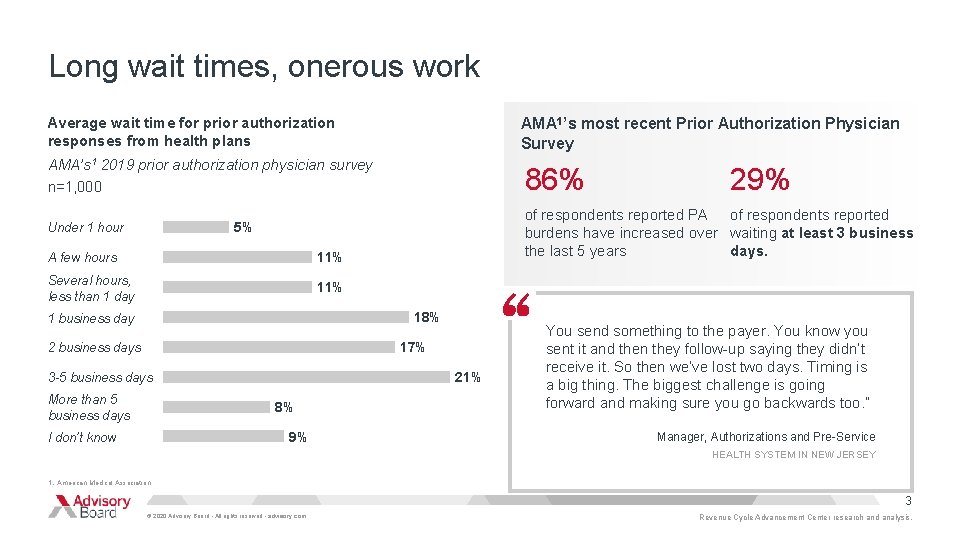
Long wait times, onerous work Average wait time for prior authorization responses from health plans AMA 1’s most recent Prior Authorization Physician Survey AMA’s 1 2019 prior authorization physician survey n=1, 000 86% of respondents reported PA of respondents reported burdens have increased over waiting at least 3 business the last 5 years days. 5% Under 1 hour A few hours 11% Several hours, less than 1 day 11% 18% 1 business day 17% 2 business days 21% 3 -5 business days More than 5 business days 8% 9% I don’t know 29% You send something to the payer. You know you sent it and then they follow-up saying they didn’t receive it. So then we’ve lost two days. Timing is a big thing. The biggest challenge is going forward and making sure you go backwards too. ” Manager, Authorizations and Pre-Service HEALTH SYSTEM IN NEW JERSEY 1. American Medical Association. 3 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
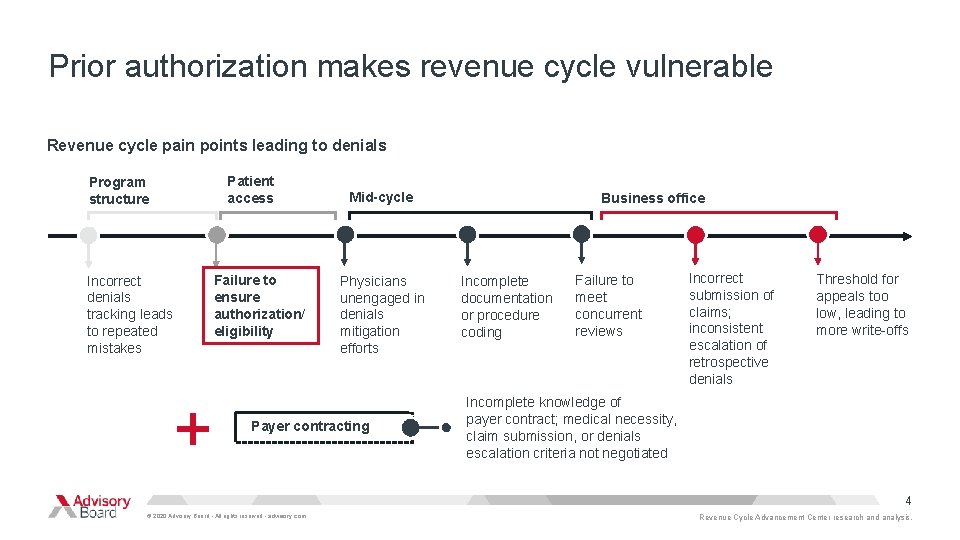
Prior authorization makes revenue cycle vulnerable Revenue cycle pain points leading to denials Patient access Program structure Failure to ensure authorization/ eligibility Incorrect denials tracking leads to repeated mistakes + Mid-cycle Physicians unengaged in denials mitigation efforts Payer contracting Business office Incomplete documentation or procedure coding Failure to meet concurrent reviews Incorrect submission of claims; inconsistent escalation of retrospective denials Threshold for appeals too low, leading to more write-offs Incomplete knowledge of payer contract; medical necessity, claim submission, or denials escalation criteria not negotiated 4 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
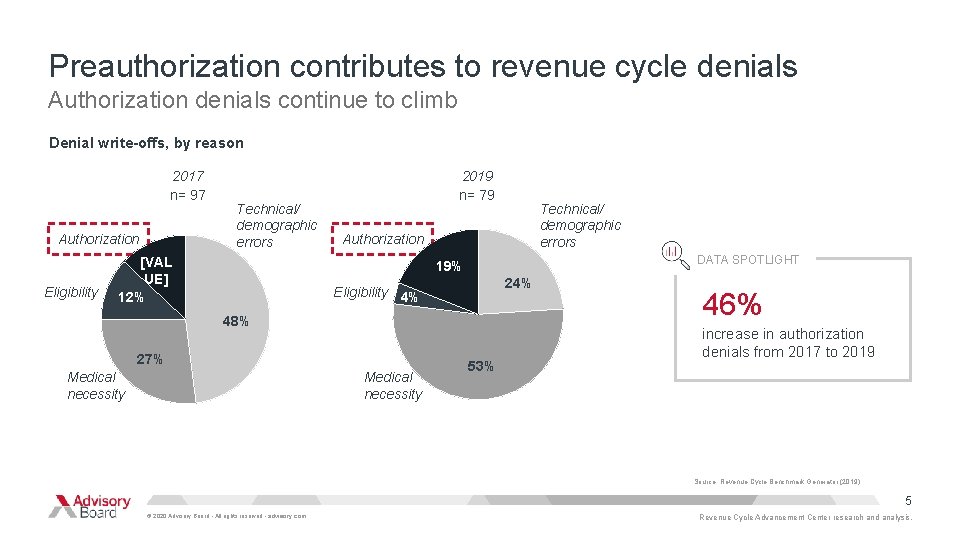
Preauthorization contributes to revenue cycle denials Authorization denials continue to climb Denial write-offs, by reason 2017 n= 97 Authorization Eligibility Technical/ demographic errors [VAL UE] 12% 2019 n= 79 Technical/ demographic errors Authorization DATA SPOTLIGHT 19% 24% Eligibility 4% 48% 27% Medical necessity 53% 46% increase in authorization denials from 2017 to 2019 Source: Revenue Cycle Benchmark Generator (2019) 5 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
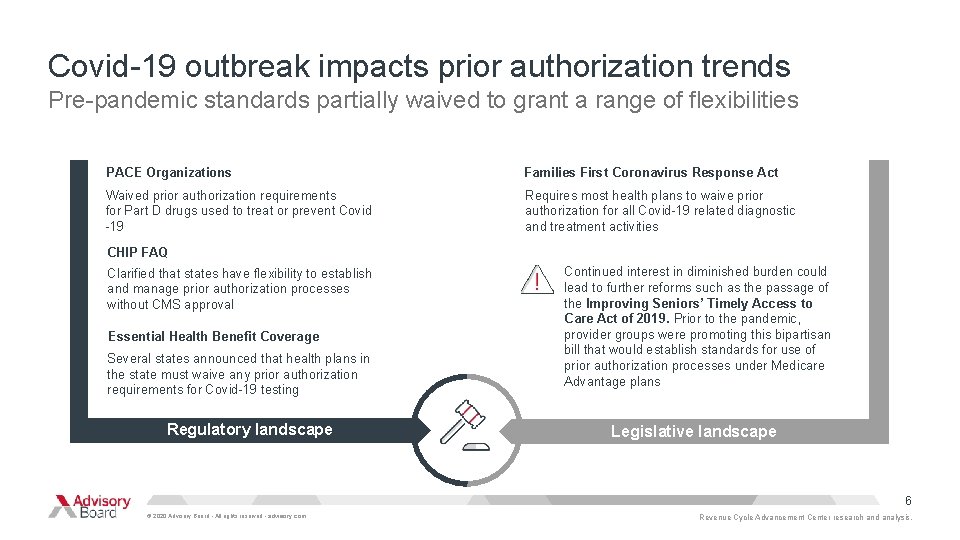
Covid-19 outbreak impacts prior authorization trends Pre-pandemic standards partially waived to grant a range of flexibilities PACE Organizations Families First Coronavirus Response Act Waived prior authorization requirements for Part D drugs used to treat or prevent Covid -19 Requires most health plans to waive prior authorization for all Covid-19 related diagnostic and treatment activities CHIP FAQ Clarified that states have flexibility to establish and manage prior authorization processes without CMS approval Essential Health Benefit Coverage Several states announced that health plans in the state must waive any prior authorization requirements for Covid-19 testing Regulatory landscape Continued interest in diminished burden could lead to further reforms such as the passage of the Improving Seniors’ Timely Access to Care Act of 2019. Prior to the pandemic, provider groups were promoting this bipartisan bill that would establish standards for use of prior authorization processes under Medicare Advantage plans Legislative landscape 6 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
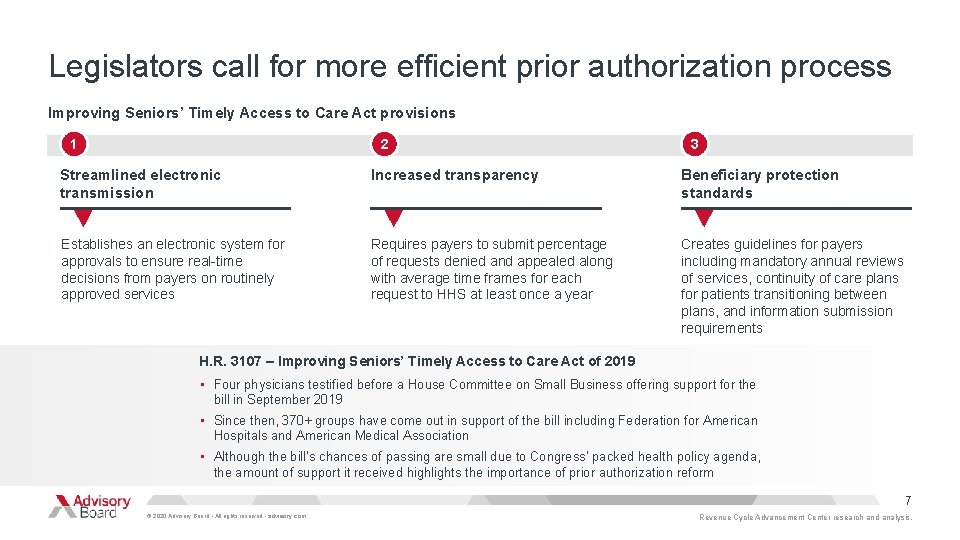
Legislators call for more efficient prior authorization process Improving Seniors’ Timely Access to Care Act provisions 1 2 3 Streamlined electronic transmission Increased transparency Beneficiary protection standards Establishes an electronic system for approvals to ensure real-time decisions from payers on routinely approved services Requires payers to submit percentage of requests denied and appealed along with average time frames for each request to HHS at least once a year Creates guidelines for payers including mandatory annual reviews of services, continuity of care plans for patients transitioning between plans, and information submission requirements H. R. 3107 – Improving Seniors’ Timely Access to Care Act of 2019 • Four physicians testified before a House Committee on Small Business offering support for the bill in September 2019 • Since then, 370+ groups have come out in support of the bill including Federation for American Hospitals and American Medical Association • Although the bill’s chances of passing are small due to Congress’ packed health policy agenda, the amount of support it received highlights the importance of prior authorization reform 7 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
Is automation the path forward? Unmet automation needs Providers often report working with vendors who are not advanced enough to meet their needs or who cannot interface with the number of payers necessary “I’m still looking for an authorization process that works like a claims adjudication process. The authorization piece is still very manual and paper driven. ” Director of Revenue Cycle Management Health System in New Jersey Director of Revenue Cycle Management Health system in New Jersey 8 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
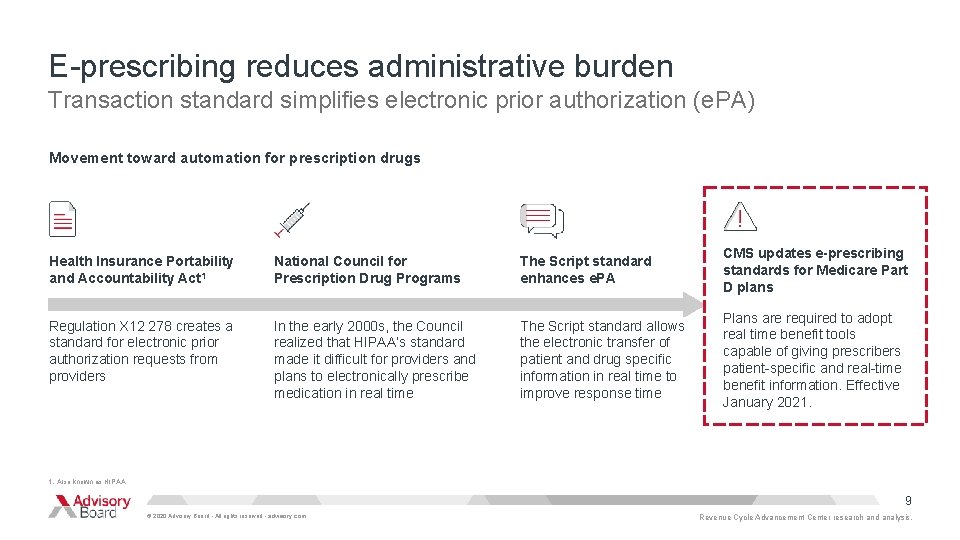
E-prescribing reduces administrative burden Transaction standard simplifies electronic prior authorization (e. PA) Movement toward automation for prescription drugs Health Insurance Portability and Accountability Act 1 National Council for Prescription Drug Programs The Script standard enhances e. PA CMS updates e-prescribing standards for Medicare Part D plans Regulation X 12 278 creates a standard for electronic prior authorization requests from providers In the early 2000 s, the Council realized that HIPAA’s standard made it difficult for providers and plans to electronically prescribe medication in real time The Script standard allows the electronic transfer of patient and drug specific information in real time to improve response time Plans are required to adopt real time benefit tools capable of giving prescribers patient-specific and real-time benefit information. Effective January 2021. 1. Also known as HIPAA. 9 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
The script standard moves automation further Express Scripts adopts the standard to save physician time What the Script standard means for automation Express Scripts, a pharmacy benefit management organization, is working to adopt the Script standard with 55 -60% of its prior authorizations currently being done electronically. The organization’s goal is to grow its database to eventually extract all the necessary information for a prior authorization from a physician’s EHR without having to contact the physician directly. A change like this would save physicians considerable time given the 40% of physicians who report prescribing drugs that do not require prior authorization. 1 1. According to Express Scripts. Source: Modern Healthcare, “Why drug prior authorization has made more progress toward automation, ” https: //www. modernhealthcare. com/insurance/why-drug-prior -authorization-has-made-more-progress-toward-automation; Rev Cycle Intelligence, “CMS Seeks Electronic Prior Authorization for Medicare Part D Drugs, ” https: //revcycleintelligence. com/news/cms-seeks-electronic-prior-authorization-for-medicare-part-d-drugs; Revenue Cycle Advancement Center research and analysis. 10 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
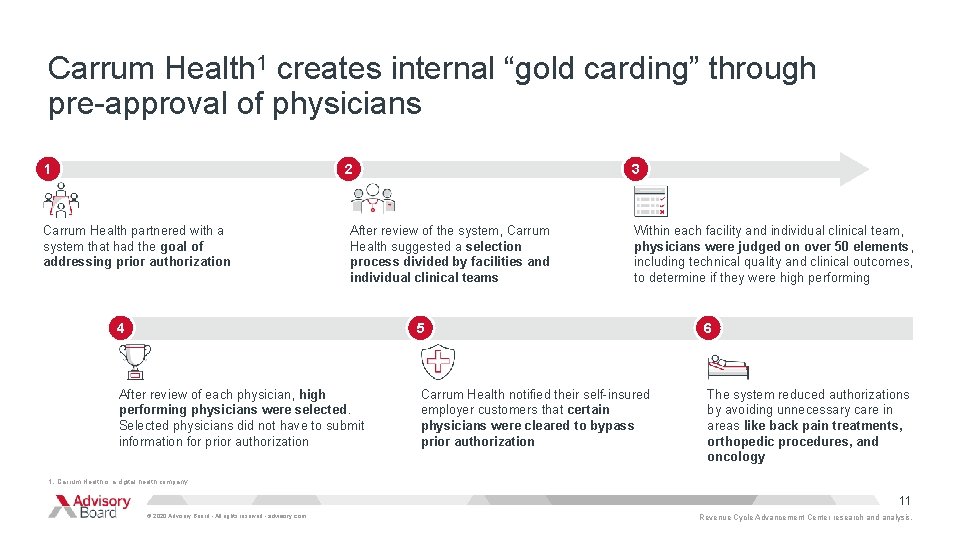
Carrum Health 1 creates internal “gold carding” through pre-approval of physicians 1 2 Carrum Health partnered with a system that had the goal of addressing prior authorization 3 After review of the system, Carrum Health suggested a selection process divided by facilities and individual clinical teams Within each facility and individual clinical team, physicians were judged on over 50 elements, including technical quality and clinical outcomes, to determine if they were high performing 4 5 6 After review of each physician, high performing physicians were selected. Selected physicians did not have to submit information for prior authorization Carrum Health notified their self-insured employer customers that certain physicians were cleared to bypass prior authorization The system reduced authorizations by avoiding unnecessary care in areas like back pain treatments, orthopedic procedures, and oncology 1. Carrum Health is a digital health company. 11 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
Case in brief Carrum Health San Francisco, CA • Carrum Health is a private firm that connects self-insured employers to regional health care providers through a bundled payment solution • One of the firm’s benefits for health care providers with considerable prior authorization burden—through their bundled payment solution, prior authorization was eliminated for select physicians • Physicians that eliminated prior authorization reported higher satisfaction with their work 12 © 2020 Advisory Board • All rights reserved • advisory. com
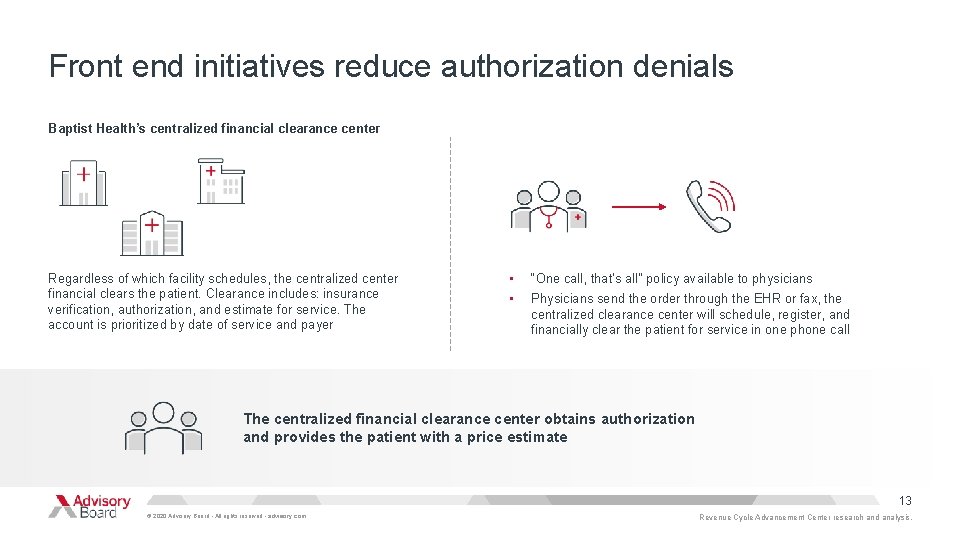
Front end initiatives reduce authorization denials Baptist Health’s centralized financial clearance center Regardless of which facility schedules, the centralized center financial clears the patient. Clearance includes: insurance verification, authorization, and estimate for service. The account is prioritized by date of service and payer • “One call, that’s all” policy available to physicians • Physicians send the order through the EHR or fax, the centralized clearance center will schedule, register, and financially clear the patient for service in one phone call The centralized financial clearance center obtains authorization and provides the patient with a price estimate 13 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
Address authorization changes mid-care Baptist Heath prioritizes same day follow-up Implement effective work queues Pre-service review for high-dollar cases • • The revenue integrity team checks on all “big ticket, ” clinically complex services in what they call “pre-service high-dollar review. ” • During this stage, clinical nurses complete frontend service review to ensure that appropriate authorization is secured and that documentation supports medical necessity. • If the authorization is missing or the case does not meet medical necessity the Revenue Integrity staff will obtain the authorization or work with the physician/physician’s office to obtain additional information for the authorization or medical necessity. To address authorization changes mid-care, the center manages a work queue that notifies staff when service changes will likely require follow-up with the payer. • The center’s goal is to follow-up on the same day as the change. • For example, if a radiologist determines a different type of scan is needed, the center will reach out to the payer within the same day and ask for authorization for the new scan. 14 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
Prior authorization is a hurdle for providers Prior authorization has turned into an absolute nightmare. I work with provider representatives more than I do anyone else…There are so many inconsistencies with payers…everyone has their own separate rules. Director of Authorization Management Health System in the South 15 © 2020 Advisory Board • All rights reserved • advisory. com Revenue Cycle Advancement Center research and analysis.
Credits Revenue Cycle Advancement Center Project director Research team Lauren Robinson Sophia Duke-Mosier Anoop Mehendale robinsolau@advisory. com (202) 266 -5398 Program leadership Rob Lazerow Robin Brand Emily Connelly 16 © 2020 Advisory Board • All rights reserved • advisory. com
LEGAL CAVEAT Advisory Board has made efforts to verify the accuracy of the information it provides to members. This report relies on data obtained from many sources, however, and Advisory Board cannot guarantee the accuracy of the information provided or any analysis based thereon. In addition, Advisory Board is not in the business of giving legal, medical, accounting, or other professional advice, and its reports should not be construed as professional advice. In particular, members should not rely on any legal commentary in this report as a basis for action, or assume that any tactics described herein would be permitted by applicable law or appropriate for a given member’s situation. Members are advised to consult with appropriate professionals concerning legal, medical, tax, or accounting issues, before implementing any of these tactics. Neither Advisory Board nor its officers, directors, trustees, employees, and agents shall be liable for any claims, liabilities, or expenses relating to (a) any errors or omissions in this report, whether caused by Advisory Board or any of its employees or agents, or sources or other third parties, (b) any recommendation or graded ranking by Advisory Board, or (c) failure of member and its employees and agents to abide by the terms set forth herein. Advisory Board and the “A” logo are registered trademarks of The Advisory Board Company in the United States and other countries. Members are not permitted to use these trademarks, or any other trademark, product name, service name, trade name, and logo of Advisory Board without prior written consent of Advisory Board. All other trademarks, product names, service names, trade names, and logos used within these pages are the property of their respective holders. Use of other company trademarks, product names, service names, trade names, and logos or images of the same does not necessarily constitute (a) an endorsement by such company of Advisory Board and its products and services, or (b) an endorsement of the company or its products or services by Advisory Board is not affiliated with any such company. IMPORTANT: Please read the following. Advisory Board has prepared this report for the exclusive use of its members. Each member acknowledges and agrees that this report and the information contained herein (collectively, the “Report”) are confidential and proprietary to Advisory Board. By accepting delivery of this Report, each member agrees to abide by the terms as stated herein, including the following: 1. Advisory Board owns all right, title, and interest in and to this Report. Except as stated herein, no right, license, permission, or interest of any kind in this Report is intended to be given, transferred to, or acquired by a member. Each member is authorized to use this Report only to the extent expressly authorized herein. 2. Each member shall not sell, license, republish, or post online or otherwise this Report, in part or in whole. Each member shall not disseminate or permit the use of, and shall take reasonable precautions to prevent such dissemination or use of, this Report by (a) any of its employees and agents (except as stated below), or (b) any third party. 3. Each member may make this Report available solely to those of its employees and agents who (a) are registered for the workshop or membership program of which this Report is a part, (b) require access to this Report in order to learn from the information described herein, and (c) agree not to disclose this Report to other employees or agents or any third party. Each member shall use, and shall ensure that its employees and agents use, this Report for its internal use only. Each member may make a limited number of copies, solely as adequate for use by its employees and agents in accordance with the terms herein. 4. Each member shall not remove from this Report any confidential markings, copyright notices, and/or other similar indicia herein. 5. Each member is responsible for any breach of its obligations as stated herein by any of its employees or agents. 6. If a member is unwilling to abide by any of the foregoing obligations, then such member shall promptly return this Report and all copies thereof to Advisory Board. © 2020 Advisory Board • All rights reserved • advisory. com 17
655 New York Avenue NW, Washington DC 20001 202 -266 -5600 │ advisory. com
- Slides: 18