Printing Color GUIDELINES FOR PRINTING AND COLOR REPRODUCTION
- Slides: 2
Printing & Color GUIDELINES FOR PRINTING AND COLOR REPRODUCTION NOTE: THE POSTER TEMPLATE IS BUILT 50% TO SCALE DUE TO POWERPOINT SIZE LIMITATIONS. Print at 200% for 42”x 60” Poster INTERMOUNTAIN RESEARCH POSTER COLOR PALETTE BREAKDOWN For Body Copy Primary Color Secondary Color Dark Gray R-68 G-68 B-68 C-0, M-0, Y-0, K-79 Midnight Blue R-0 G-51 B-102 C-100, M-69, Y-8, K-54 Medium Blue R-51 G-136 B-221 C-68, M-34, Y-0, K-0 Light Blue R-170 G-204 B-238 C-35, M-9, Y-0, K-0 Tan (40%) R-221 G-204 B-170 C-3, M-3, Y-15, K-5 Bright Green R-136 G-187 B-0 C-54, M-0, Y-100, K-0 Gold R-255 G-187 B-C-34 C-0, M-31, Y-100, K-0 TYPOGRAPHY Times New Roman — Title & affiliations section (serif) Secondary Color Orange Dark Green R-204 G-102 B-34 R-68 G-119 B-034 C-5, M-71, Y-100, K-23 C-71, M-4, Y-100, K-45 (FONTS) Calibri — Sub title, body copy, chart, & table copy (sans serif)
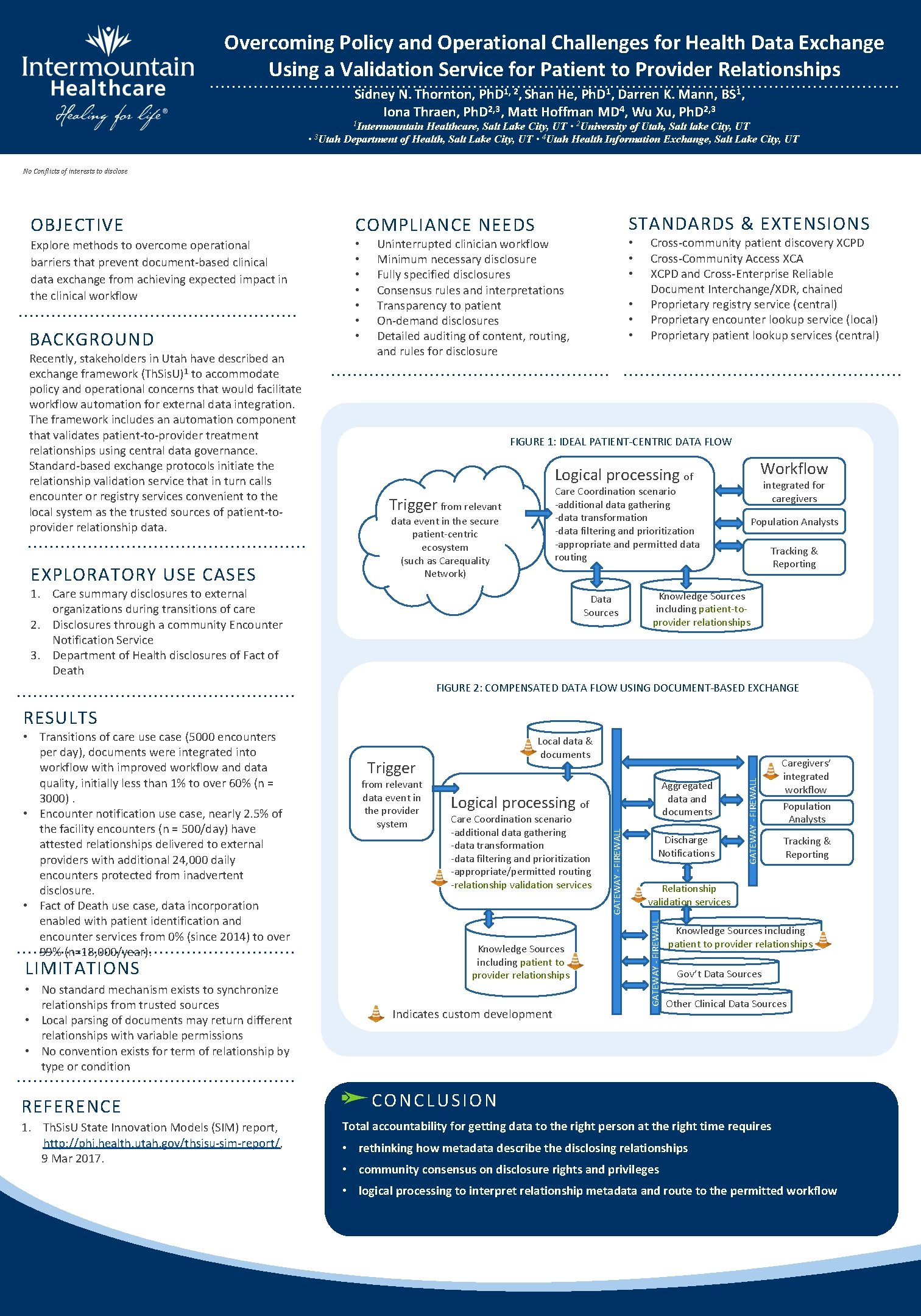
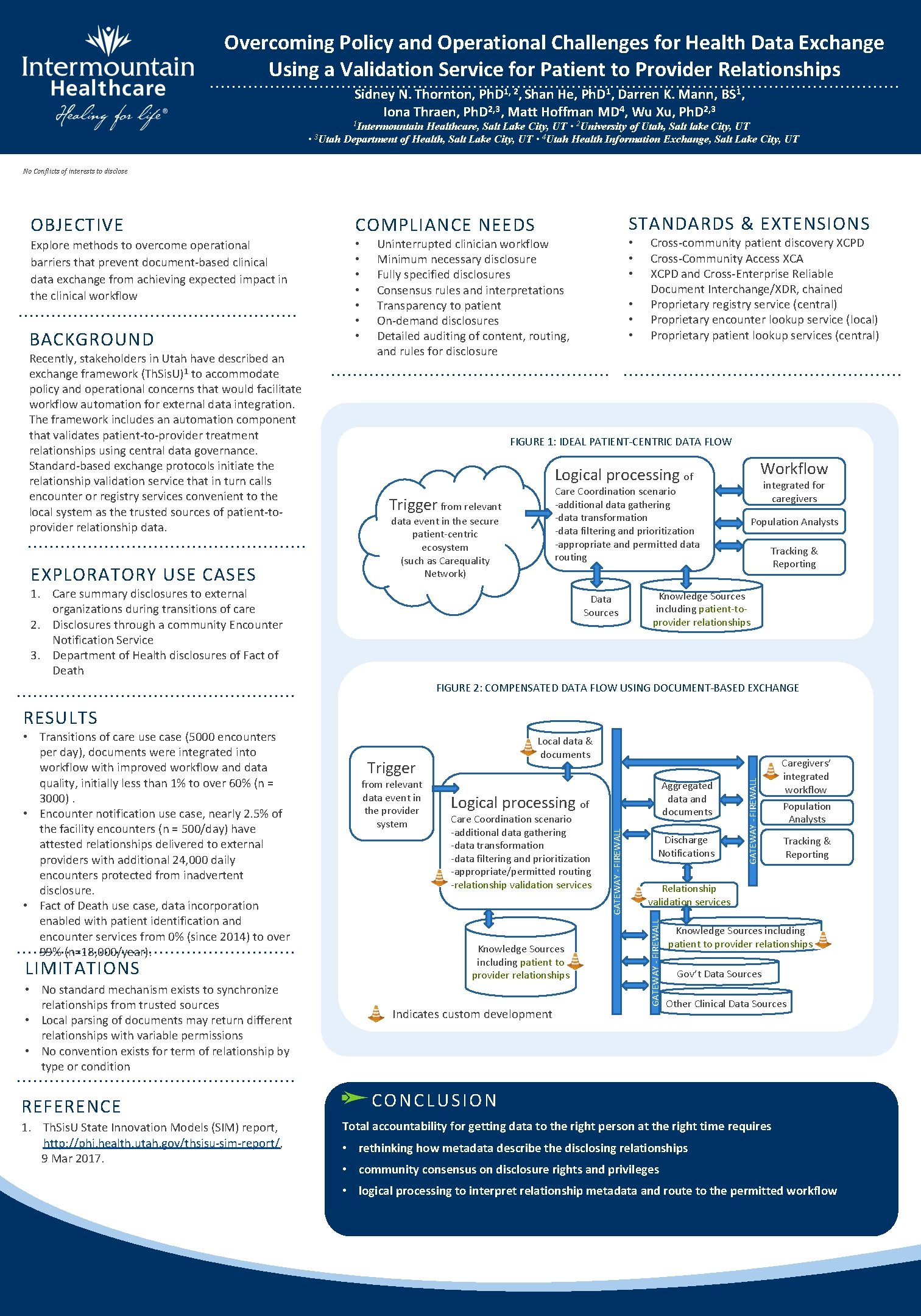
Overcoming Policy and Operational Challenges for Health Data Exchange Using a Validation Service for Patient to Provider Relationships Sidney N. Thornton, Ph. D 1, 2, Shan He, Ph. D 1, Darren K. Mann, BS 1, Iona Thraen, Ph. D 2, 3, Matt Hoffman MD 4, Wu Xu, Ph. D 2, 3 1 Intermountain Healthcare, Salt Lake City, UT • 2 University of Utah, Salt lake City, UT • 3 Utah Department of Health, Salt Lake City, UT • 4 Utah Health Information Exchange, Salt Lake City, UT No Conflicts of interests to disclose OBJECTIVE Explore methods to overcome operational barriers that prevent document-based clinical data exchange from achieving expected impact in the clinical workflow BACKGROUND Recently, stakeholders in Utah have described an exchange framework (Th. Sis. U)1 to accommodate policy and operational concerns that would facilitate workflow automation for external data integration. The framework includes an automation component that validates patient-to-provider treatment relationships using central data governance. Standard-based exchange protocols initiate the relationship validation service that in turn calls encounter or registry services convenient to the local system as the trusted sources of patient-toprovider relationship data. EXPLORATORY USE CASES COMPLIANCE NEEDS STANDARDS & EXTENSIONS • • • • Uninterrupted clinician workflow Minimum necessary disclosure Fully specified disclosures Consensus rules and interpretations Transparency to patient On-demand disclosures Detailed auditing of content, routing, and rules for disclosure Cross-community patient discovery XCPD Cross-Community Access XCA XCPD and Cross-Enterprise Reliable Document Interchange/XDR, chained Proprietary registry service (central) Proprietary encounter lookup service (local) Proprietary patient lookup services (central) FIGURE 1: IDEAL PATIENT-CENTRIC DATA FLOW Workflow Logical processing of Care Coordination scenario -additional data gathering -data transformation -data filtering and prioritization -appropriate and permitted data routing Trigger from relevant data event in the secure patient-centric ecosystem (such as Carequality Network) 1. Care summary disclosures to external organizations during transitions of care 2. Disclosures through a community Encounter Notification Service 3. Department of Health disclosures of Fact of Death Data Sources integrated for caregivers Population Analysts Tracking & Reporting Knowledge Sources including patient-toprovider relationships FIGURE 2: COMPENSATED DATA FLOW USING DOCUMENT-BASED EXCHANGE RESULTS • No standard mechanism exists to synchronize relationships from trusted sources • Local parsing of documents may return different relationships with variable permissions • No convention exists for term of relationship by type or condition REFERENCE 1. Th. Sis. U State Innovation Models (SIM) report, http: //phi. health. utah. gov/thsisu-sim-report/, 9 Mar 2017. from relevant data event in the provider system Aggregated data and documents Logical processing of Care Coordination scenario -additional data gathering -data transformation -data filtering and prioritization -appropriate/permitted routing -relationship validation services Knowledge Sources including patient to provider relationships Indicates custom development Discharge Notifications GATEWAY - FIREWALL Trigger Caregivers’ integrated workflow Population Analysts Tracking & Reporting Relationship validation services GATEWAY - FIREWALL LIMITATIONS Local data & documents GATEWAY - FIREWALL • Transitions of care use case (5000 encounters per day), documents were integrated into workflow with improved workflow and data quality, initially less than 1% to over 60% (n = 3000). • Encounter notification use case, nearly 2. 5% of the facility encounters (n = 500/day) have attested relationships delivered to external providers with additional 24, 000 daily encounters protected from inadvertent disclosure. • Fact of Death use case, data incorporation enabled with patient identification and encounter services from 0% (since 2014) to over 99% (n=18, 000/year). Knowledge Sources including patient to provider relationships Gov’t Data Sources Other Clinical Data Sources CONCLUSION Total accountability for getting data to the right person at the right time requires • rethinking how metadata describe the disclosing relationships • community consensus on disclosure rights and privileges • logical processing to interpret relationship metadata and route to the permitted workflow