Principles of Orthopaedic Trauma Care Compartment Syndrome Alison






- Slides: 20
Principles of Orthopaedic & Trauma Care Compartment Syndrome Alison Holman Faculty of Health & Life Sciences UWE March 2011
Learning Outcomes • • • Define Compartment Syndrome and identify underlying pathology & the main causes Explain principles of patient assessment and provide an evidence base Identify relevant investigations and the practitioners role in these Describe the conservative and surgical treatment options and the care management Explore the implications of compartment syndrome for the patient & families, carers
Compartment Syndrome is … • ‘ … an elevation of the interstitial pressure in a closed osseofascial compartment that results in microvascular compromise’ Mubarak & Hargens (1983, cited Edwards 2004: 32) • ‘ … a condition in which the circulation and function of tissues within a closed space are compromised by an increased pressure within that space’. Matsen (1975, cited Singh, Trikha & Lewis 2005: 468) CS originally described by Volkmann in 1872 with reference to the forearm.
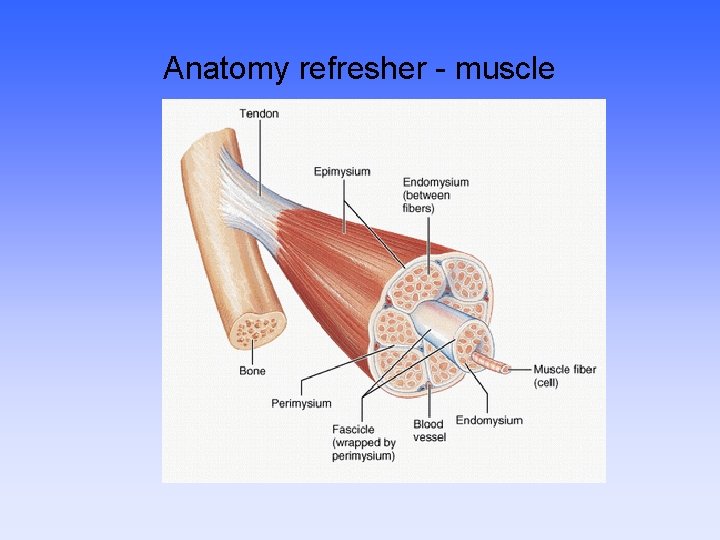
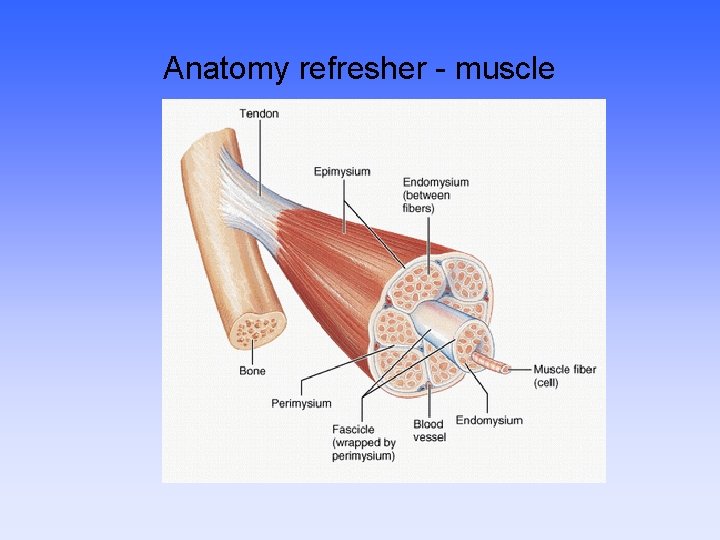
Anatomy refresher - muscle

Anatomy revision Key Compartment Syndrome sites 4 Lower limb compartments 3 Thigh compartments 2 Forearm compartments Normal Inter Compartmental Pressure (ICP) = 0 -8 mm. Hg (Edwards 2004)
Is compartment syndrome acute? • ACUTE follows traumatic event, commonly fractures, with worsening symptoms & irreversible tissue damage within hours • CHRONIC a recurrent syndrome occurring with exercise or work (microtrauma or repetitive overexertion). Symptoms often resolve with rest.
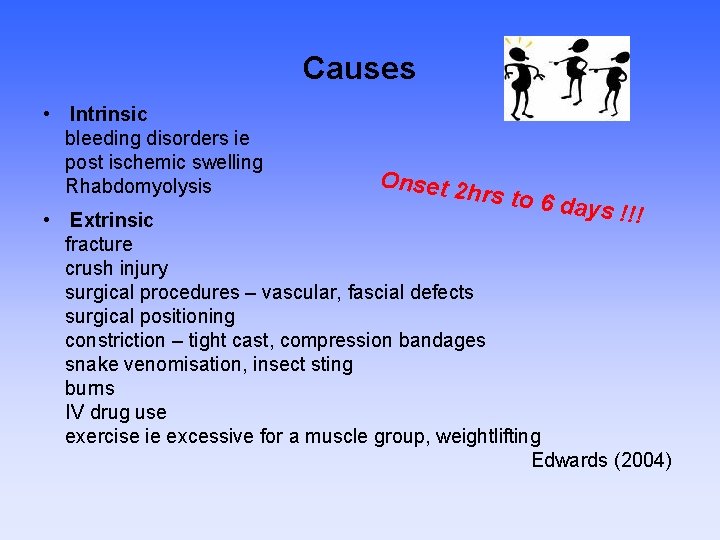
Causes • Intrinsic bleeding disorders ie post ischemic swelling Rhabdomyolysis Onset 2 hrs to 6 day s !!! • Extrinsic fracture crush injury surgical procedures – vascular, fascial defects surgical positioning constriction – tight cast, compression bandages snake venomisation, insect sting burns IV drug use exercise ie excessive for a muscle group, weightlifting Edwards (2004)
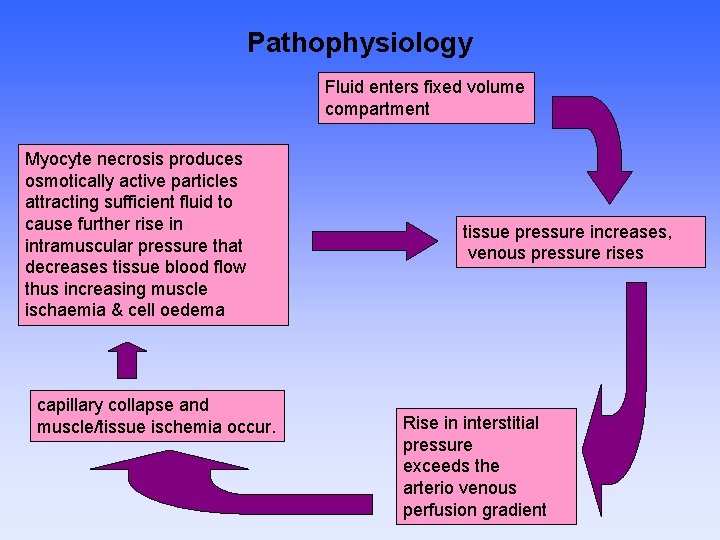
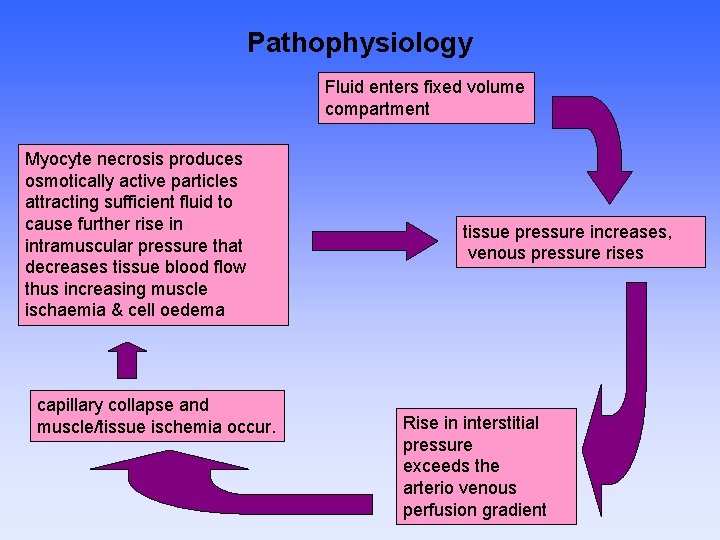
Pathophysiology Fluid enters fixed volume compartment Myocyte necrosis produces osmotically active particles attracting sufficient fluid to cause further rise in intramuscular pressure that decreases tissue blood flow thus increasing muscle ischaemia & cell oedema capillary collapse and muscle/tissue ischemia occur. tissue pressure increases, venous pressure rises Rise in interstitial pressure exceeds the arterio venous perfusion gradient
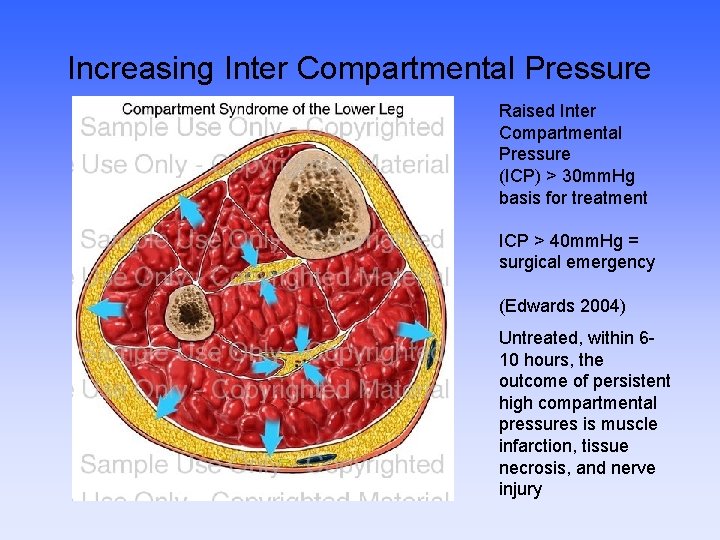
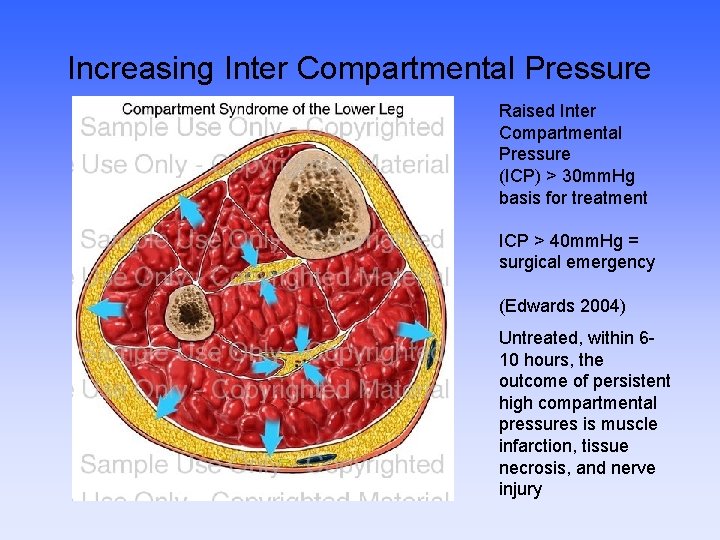
Increasing Inter Compartmental Pressure Raised Inter Compartmental Pressure (ICP) > 30 mm. Hg basis for treatment ICP > 40 mm. Hg = surgical emergency (Edwards 2004) Untreated, within 610 hours, the outcome of persistent high compartmental pressures is muscle infarction, tissue necrosis, and nerve injury

Single-incision fasciotomy. Photographs courtesy of DG Smith, MD, Harborview Hospital, Seattle, WA
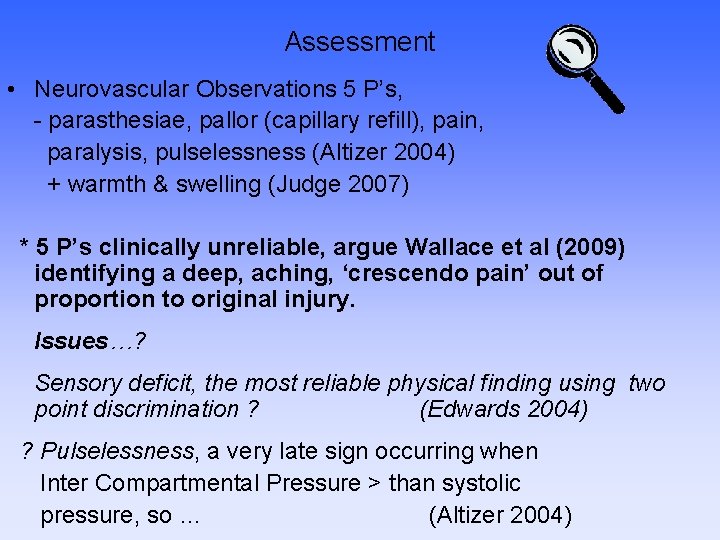
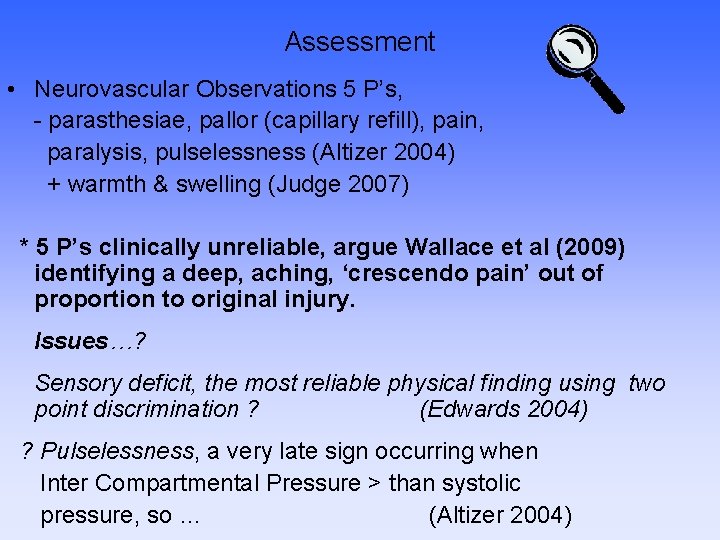
Assessment • Neurovascular Observations 5 P’s, - parasthesiae, pallor (capillary refill), pain, paralysis, pulselessness (Altizer 2004) + warmth & swelling (Judge 2007) * 5 P’s clinically unreliable, argue Wallace et al (2009) identifying a deep, aching, ‘crescendo pain’ out of proportion to original injury. Issues…? Sensory deficit, the most reliable physical finding using two point discrimination ? (Edwards 2004) ? Pulselessness, a very late sign occurring when Inter Compartmental Pressure > than systolic pressure, so … (Altizer 2004)

Diagnostics Assessment… ? Frequency, ? By who, ? Recording, Action? Professional Accountability by ‘act or omission’, NMC 2009 Investigations: X-ray, MRI, CT, Ultra sound Intercompartmental measuring using, wick catheter, simple needle manometry, infusion technique, Slit catheter, CVP manometer, side ported needle, fibreoptic transducer (Edwards 2004) Care management issues: aseptic technique, equipment, location, who performs it, consent, analgesia, timing, parameters
Conservative management • Cast care management – split or wait for Dr? • Elevate ? ? ? • I/V Infusion
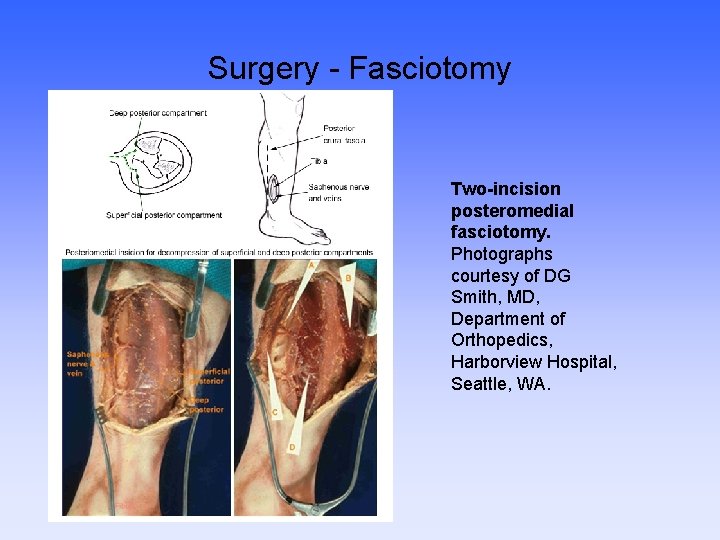
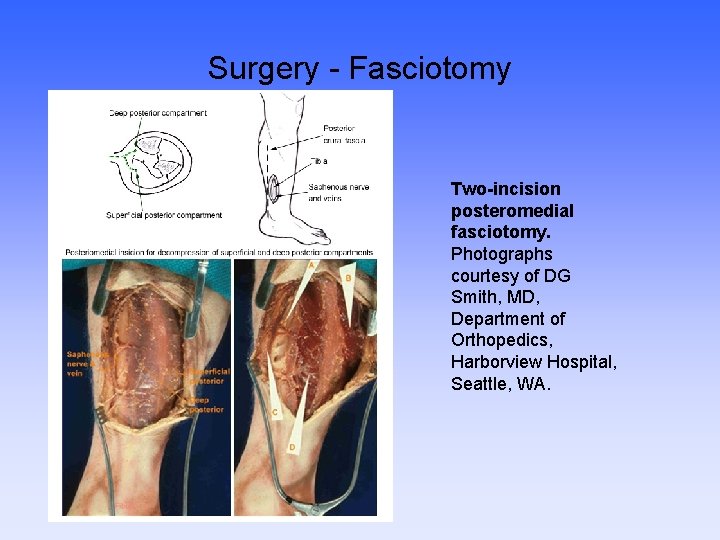
Surgery - Fasciotomy Two-incision posteromedial fasciotomy. Photographs courtesy of DG Smith, MD, Department of Orthopedics, Harborview Hospital, Seattle, WA.


Post-op fasciotomy & external fixation

Skin Grafting
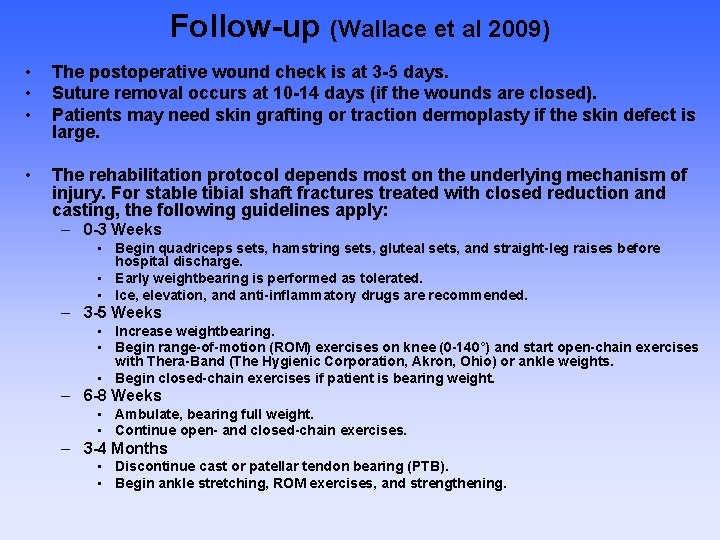
Follow-up (Wallace et al 2009) • • • The postoperative wound check is at 3 -5 days. Suture removal occurs at 10 -14 days (if the wounds are closed). Patients may need skin grafting or traction dermoplasty if the skin defect is large. • The rehabilitation protocol depends most on the underlying mechanism of injury. For stable tibial shaft fractures treated with closed reduction and casting, the following guidelines apply: – 0 -3 Weeks • Begin quadriceps sets, hamstring sets, gluteal sets, and straight-leg raises before hospital discharge. • Early weightbearing is performed as tolerated. • Ice, elevation, and anti-inflammatory drugs are recommended. – 3 -5 Weeks • Increase weightbearing. • Begin range-of-motion (ROM) exercises on knee (0 -140°) and start open-chain exercises with Thera-Band (The Hygienic Corporation, Akron, Ohio) or ankle weights. • Begin closed-chain exercises if patient is bearing weight. – 6 -8 Weeks • Ambulate, bearing full weight. • Continue open- and closed-chain exercises. – 3 -4 Months • Discontinue cast or patellar tendon bearing (PTB). • Begin ankle stretching, ROM exercises, and strengthening.
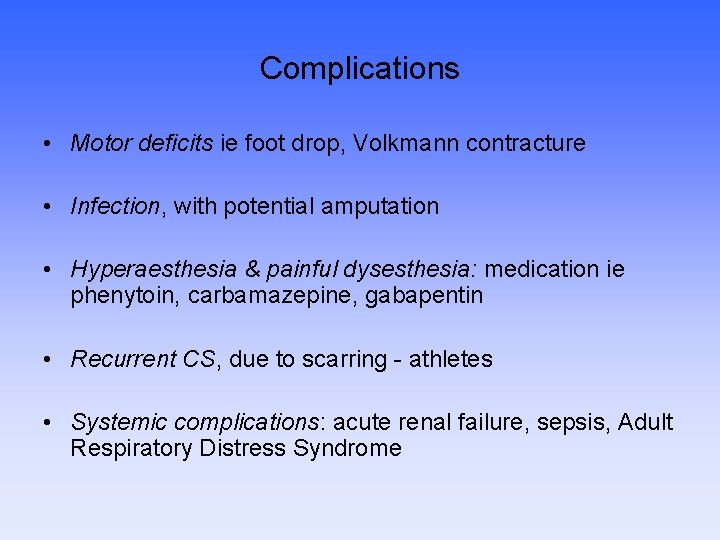
Complications • Motor deficits ie foot drop, Volkmann contracture • Infection, with potential amputation • Hyperaesthesia & painful dysesthesia: medication ie phenytoin, carbamazepine, gabapentin • Recurrent CS, due to scarring - athletes • Systemic complications: acute renal failure, sepsis, Adult Respiratory Distress Syndrome
Some psychosocial considerations … • • Work, transport Social activities Relationships Clothing Holidays Body image Self esteem Gender issues
 Compartment syndrome 7p
Compartment syndrome 7p Traction nursing interventions
Traction nursing interventions Mobile wad of henry
Mobile wad of henry Orthopaedic surgery south east london
Orthopaedic surgery south east london Sally tennant orthopaedic
Sally tennant orthopaedic Peter worlock
Peter worlock Rch fracture guidelines
Rch fracture guidelines Hospital
Hospital Stephen brennan bon secours
Stephen brennan bon secours Oncology gpo landscape
Oncology gpo landscape Charcot joints
Charcot joints Professor abudu royal orthopaedic hospital
Professor abudu royal orthopaedic hospital Dime sign ankle
Dime sign ankle Primary secondary and tertiary care
Primary secondary and tertiary care 4 r's trauma informed care
4 r's trauma informed care Lgbt trauma informed care
Lgbt trauma informed care Dr anita ravi
Dr anita ravi Pillars of trauma informed care
Pillars of trauma informed care 4 r's trauma informed care
4 r's trauma informed care Libby bergman
Libby bergman Tina champagne
Tina champagne