Principles of Nutrition and Fluid Balance Nutritional needs
Principles of Nutrition and Fluid Balance Nutritional needs and diet modifications
Nutrition • Process by which the body takes in food for growth and repair and uses it to maintain health.

Signs of Good Nutrition • • • Shiny hair clean skin and eyes well developed body alert expression pleasant disposition health sleep patterns appropriate appetite regular bowel habits body weight appropriate to height
Digestion • Process of breaking down foods into simple substances that can be used by the body for nourishment; the substances are call essential nutrients
Essential Nutrients • Body requires foods that: – supply heat and energy – build and repair body tissues – regulate body function y requires foods that • Six essential nutrients – – – proteins carbohydrates fats minerals vitamins water
Protein sources • • • Meat Poultry Eggs Milk cheese
Carbohydrates and fats • Energy foods-used to produce heat and energy • sources include – fruit – vegetables – foods made from grains
Fats • Plant and animal sources • Examples of food that are rich in fat include – pork – butter – nuts – egg yolk – cheese
Vitamins • Substances that regulate body processes • assist with…. – Building strong teeth and bones – promoting growth – aid normal body functioning – strengthening resistance to disease Vitamins used by the body
Minerals • Build body tissues especially bones and teeth • help regulate body fluids such as blood and digestive juices • Mineral needed daily are Calcium, phosphorus, iodine, iron, copper, potassium

Five Food Groups • US Department of Agriculture recommends – – – – Eating a variety of foods maintain a healthy body weight select foods low in fat, saturated fat and cholesterol select plenty of vegetables , fruits, and grain products use sugar in moderation use salt and sodium in moderation drink alcoholic beverages in moderation

Food Plate

Hospital Nutritional services • Meal trays prepared by dietary department • Includes essential nutrients • Meals prepared according to patients needs • Ordered by physician
Responsibilities during meals • Prepare the patient for the meal • Checking the food tray for correctness • Checking the tray card against the patients identification • Serving the tray to the patient • Assisting the patient with feeding if necessary
Diets • Regular- normal or full diet based on the food plate • Liquid diets – Clear liquids all components are clear i. e. tea, gelatin, or broth – Full liquids includes sherbet, eggnog, malted milk, milk and cream, plain ice cream • Soft diets are low residue, mildly flavored and requires minimal digestion. Foods included are soups, cottage cheese, crackers, fish, white meat of chicken and turkey

Special diets • Religious restricted • Therapeutic –prepared according to the patient’s individual health problem

Therapeutic Diets • Diabetic diet-prepared to maintain the patient’s blood sugar within normal limits • Sodium restricted • Calorie restricted • Low fat-limits cholesterol • Mechanically altered-consistency altered – Mechanical soft – pureed

Nutritional supplements • Used for patients with high nutritional demands • Provided between meals and are given for specific therapeutic purposes
Calorie Counts • Performed to assess a patients food intake • Food intake is recorded for three days or specified period analyzed for nutritional adequacy and calories consumed • Must accurate document food consumed • Dietician uses data to develop a specific nutritional plan.
Dysphagia • Difficulty swallowing food and liquids; occurs in patients with neurological problems and some other diagnoses such as cancer • Clients who have had a stroke
Signs and Symptoms of Dysphagia • Taking a long time before beginning to swallow • Swallowing three or four times with each bite of food • Frequent throat clearing or coughing • Lack of a gag reflex or weak cough • Difficulty controlling liquids and secretions in the mouth
Dysphagia continued • Wet, gurgling voice • Refusing to eat, spitting food out, or pocketing food in cheeks • Unintentional weight loss • Tightness in the throat or chest • Feeling as if food is sticking in the esophagus or sternal area
Aspiration Precautions • Positioning – Upright at 60 -90 degrees – Head and neck flexed at midline – Remain upright for at least 30 minutes after meals – Feeder at or below eye level of patient
Aspiration precautions • Environment – Minimize distractions, adequate lighting, comfort level • Amount and Rate – ½ to 1 teaspoon at a time, pause between spoonfuls, verbal cues for additional swallows, no straws, use thickening agents, may need to decrease rate and amount of food toward end of meal • Diet – Check diet order, if patient can not tolerate stop feeding, post aspiration sigh above bed
Aspiration precautions continued Other – Oral hygiene before meals, periodically throughout meal check to see if patient swallowing and can clear throat – Do Not mix textures together – Check mouth to see if pocketing food – Follow recommendations by speech pathologist– chin tuck, head turn, effortful swallow, head tilt to right or left, alternate textures

Alternative nutrition • Total parenteral nutrition • Enteral feedings
Disorders requiring TPN/Enteral nutrition • • Cancer Ulcerative Colitis Crohn’s Alzheimer’s Disease ALS MS/MD Parkinson’s Disease Aspiration risk
Disorders requiring tube feeding • • Cancer Ulcerative Colitis Crohn’s Alzheimer’s Disease ALS MS/MD Parkinson’s Disease Aspiration risk
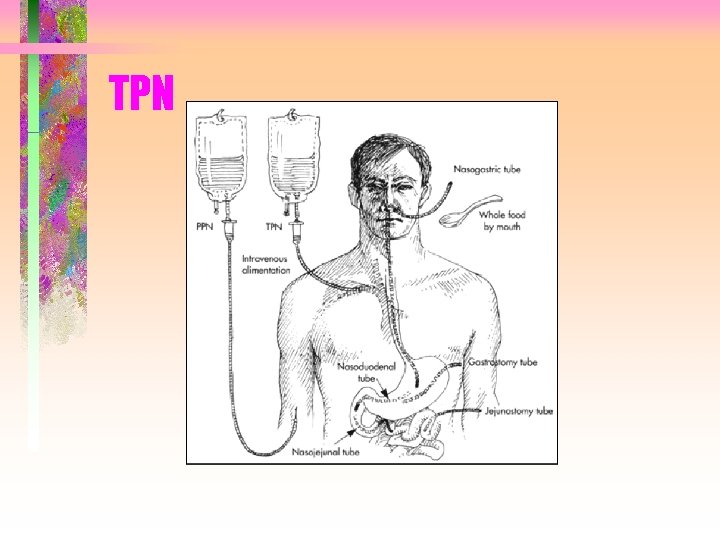
TPN
Total Parenteral Nutrition • Total parenteral nutrition (TPN) supplies all daily nutritional requirements. • TPN can be used in the hospital or at home • Because TPN solutions are concentrated and can cause thrombosis of peripheral veins, a central venous catheter is usually required.
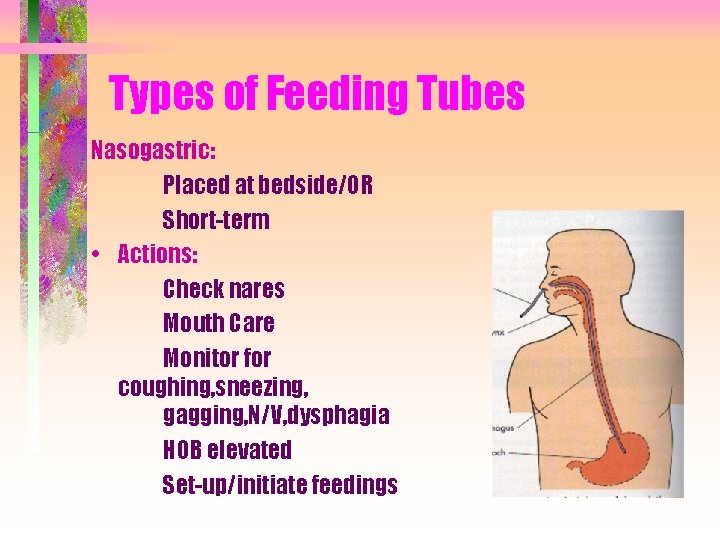
Types of Feeding Tubes Nasogastric: Placed at bedside/OR Short-term • Actions: Check nares Mouth Care Monitor for coughing, sneezing, gagging, N/V, dysphagia HOB elevated Set-up/initiate feedings
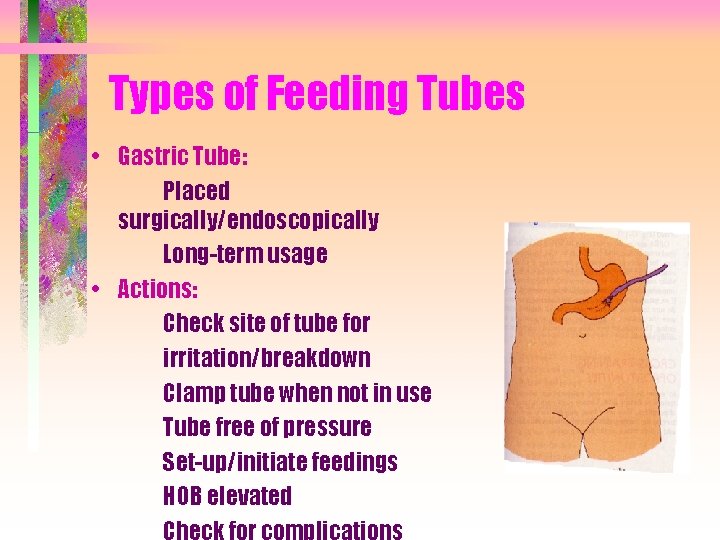
Types of Feeding Tubes • Gastric Tube: Placed surgically/endoscopically Long-term usage • Actions: Check site of tube for irritation/breakdown Clamp tube when not in use Tube free of pressure Set-up/initiate feedings HOB elevated Check for complications
Feeding Options • Continuous Feeding: – Feedings given via pump at controlled rate ordered by MD – Administration may be 24 hrs or throughout the night only – Tube feeding formula needs to be at adequate level to ensure continuous flow (No more than two cans in bag at once) – HOB elevated – Use appropriate tubing
Feeding Options • Bolus: – Large amount of formula administered as ordered-- q 3 - 4 hrs – Administered by staff – Accurate measurement of ordered formula – Administer at appropriate controlled rate – FINAL flush is critical – HOB elevated during and after feeding
Effects of Tube Feeding • Loss of dignity • Loss of sensation and texture of food • Inability to share social connection with family/friends • Inability to choose diet • Anger • Possible risk of aspiration/infection
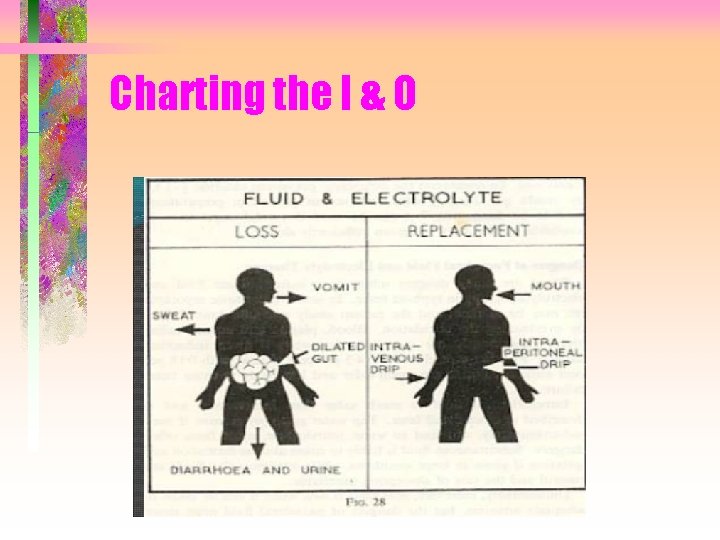
Charting the I & O
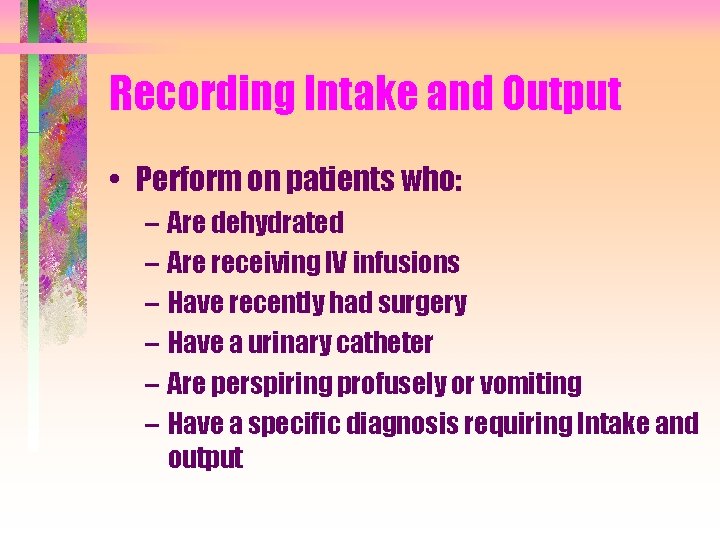
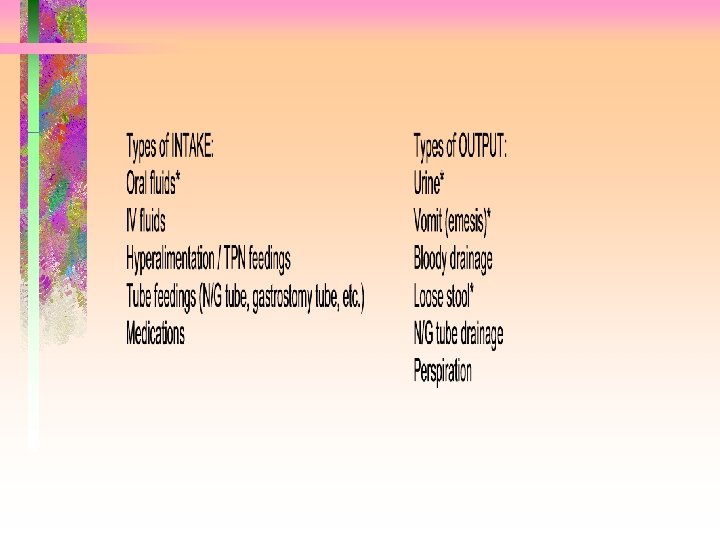
Recording Intake and Output • Perform on patients who: – Are dehydrated – Are receiving IV infusions – Have recently had surgery – Have a urinary catheter – Are perspiring profusely or vomiting – Have a specific diagnosis requiring Intake and output
Fluid intake • May be either encouraged or restricted depending on patient condition • Estimate intake by knowing liquid container amounts
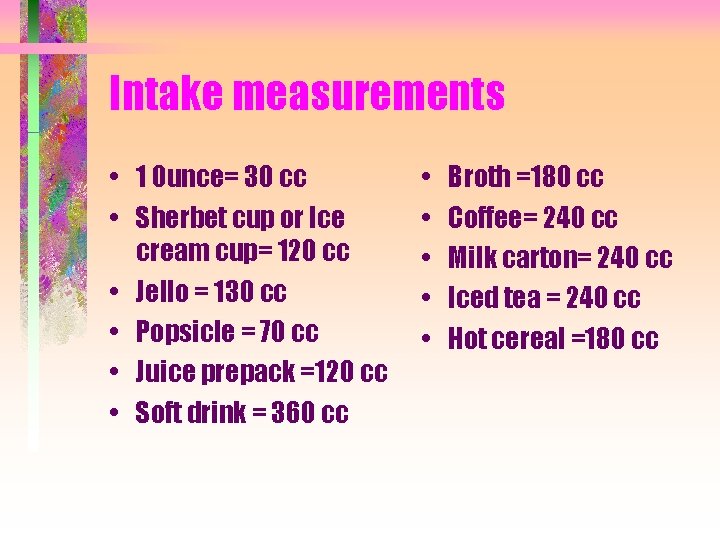
Intake measurements • 1 0 unce= 30 cc • Sherbet cup or Ice cream cup= 120 cc • Jello = 130 cc • Popsicle = 70 cc • Juice prepack =120 cc • Soft drink = 360 cc • • • Broth =180 cc Coffee= 240 cc Milk carton= 240 cc Iced tea = 240 cc Hot cereal =180 cc
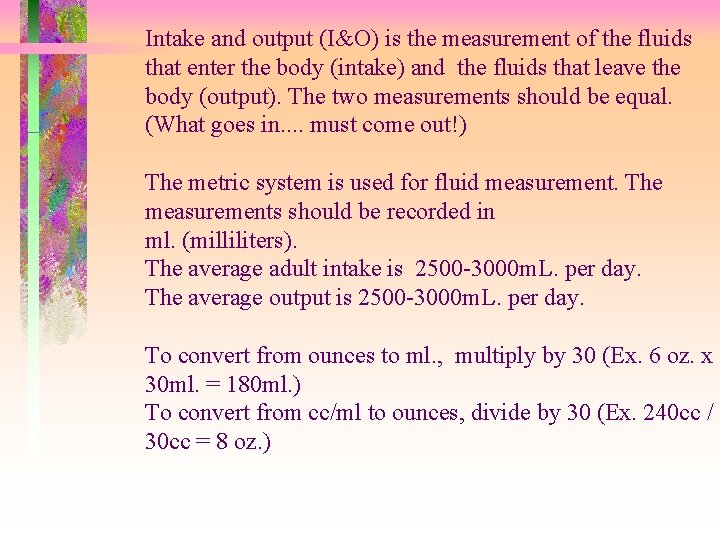
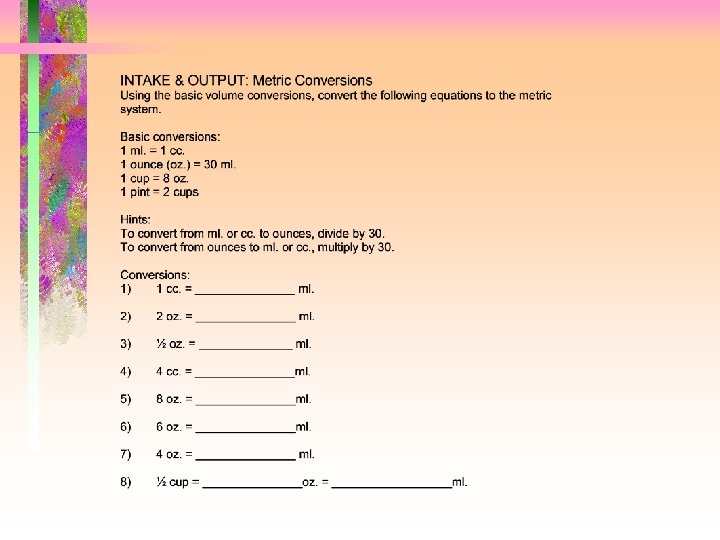
Intake and output (I&O) is the measurement of the fluids that enter the body (intake) and the fluids that leave the body (output). The two measurements should be equal. (What goes in. . must come out!) The metric system is used for fluid measurement. The measurements should be recorded in ml. (milliliters). The average adult intake is 2500 -3000 m. L. per day. The average output is 2500 -3000 m. L. per day. To convert from ounces to ml. , multiply by 30 (Ex. 6 oz. x 30 ml. = 180 ml. ) To convert from cc/ml to ounces, divide by 30 (Ex. 240 cc / 30 cc = 8 oz. )
- Slides: 42