PRINCIPLES OF MEDICAL ETHICS BASIC BIOMEDICAL PRINCIPLES Principle

PRINCIPLES OF MEDICAL ETHICS
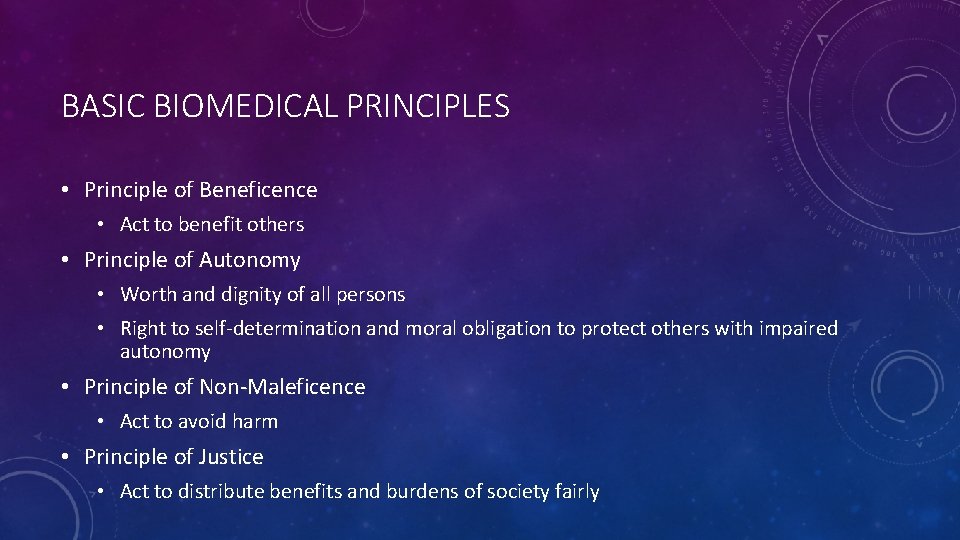
BASIC BIOMEDICAL PRINCIPLES • Principle of Beneficence • Act to benefit others • Principle of Autonomy • Worth and dignity of all persons • Right to self-determination and moral obligation to protect others with impaired autonomy • Principle of Non-Maleficence • Act to avoid harm • Principle of Justice • Act to distribute benefits and burdens of society fairly
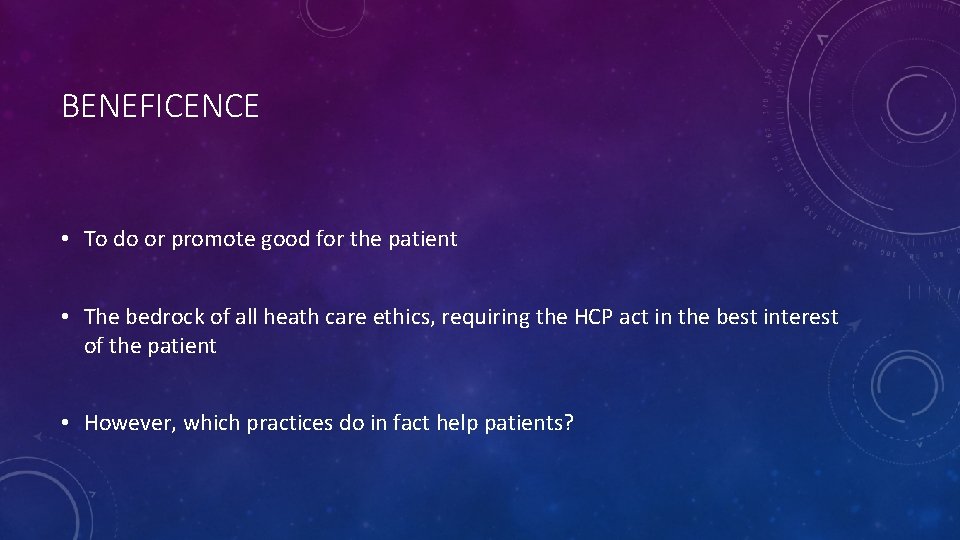
BENEFICENCE • To do or promote good for the patient • The bedrock of all heath care ethics, requiring the HCP act in the best interest of the patient • However, which practices do in fact help patients?
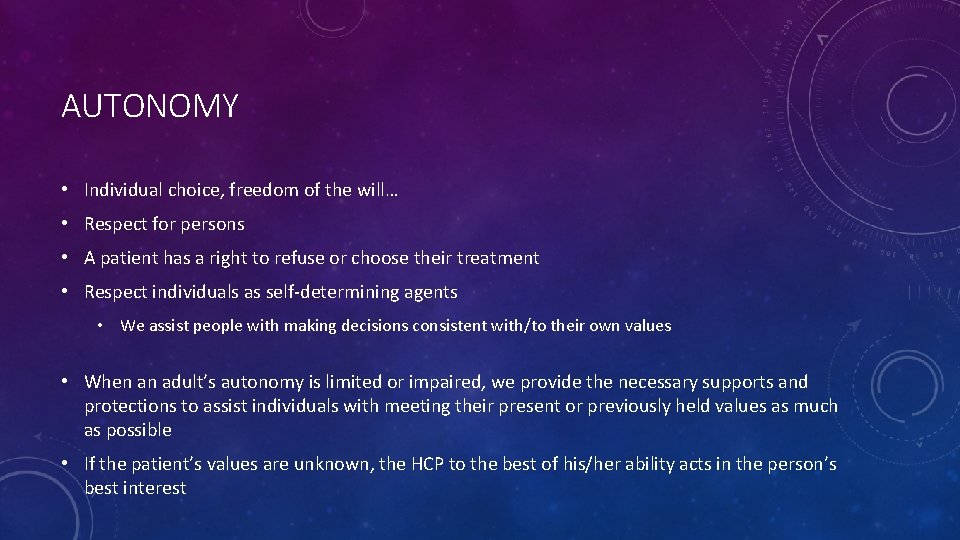
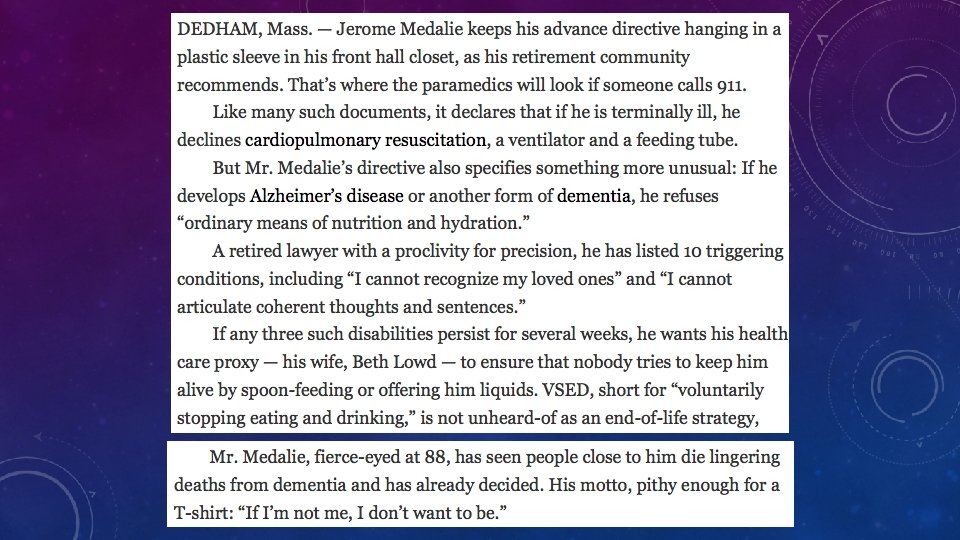
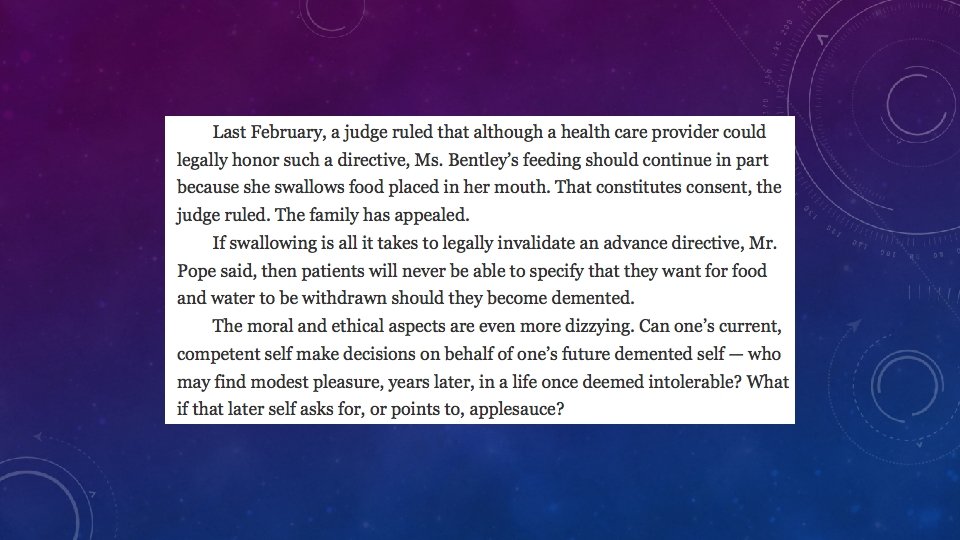
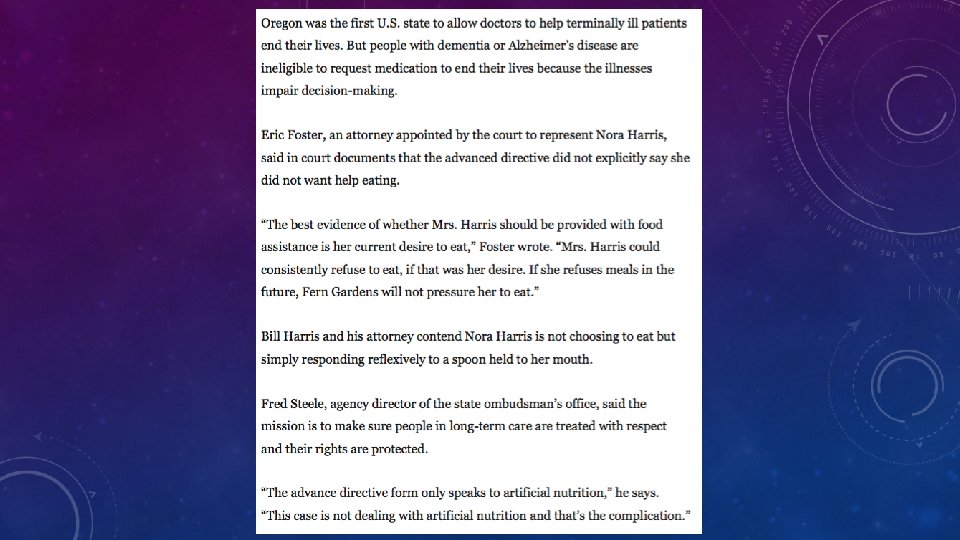
AUTONOMY • Individual choice, freedom of the will… • Respect for persons • A patient has a right to refuse or choose their treatment • Respect individuals as self-determining agents • We assist people with making decisions consistent with/to their own values • When an adult’s autonomy is limited or impaired, we provide the necessary supports and protections to assist individuals with meeting their present or previously held values as much as possible • If the patient’s values are unknown, the HCP to the best of his/her ability acts in the person’s best interest
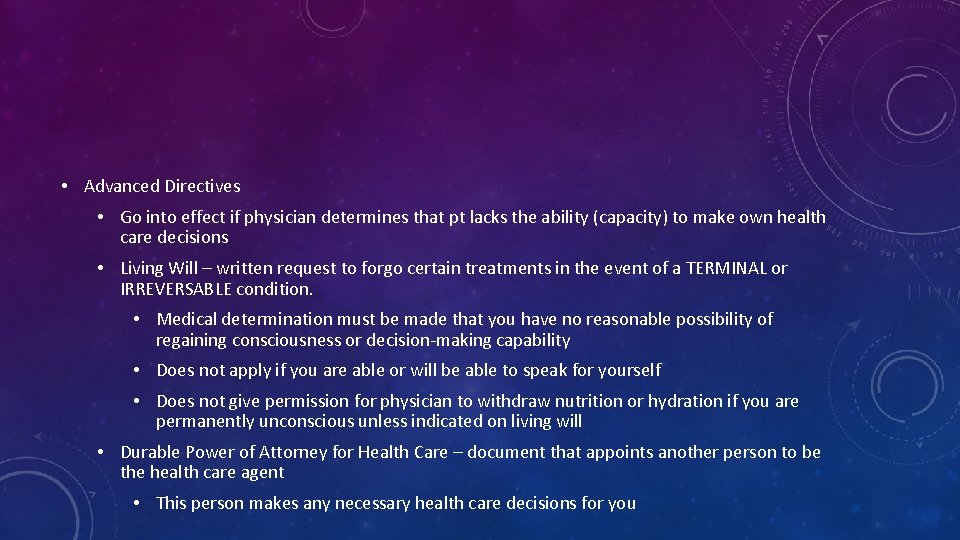
• Advanced Directives • Go into effect if physician determines that pt lacks the ability (capacity) to make own health care decisions • Living Will – written request to forgo certain treatments in the event of a TERMINAL or IRREVERSABLE condition. • Medical determination must be made that you have no reasonable possibility of regaining consciousness or decision-making capability • Does not apply if you are able or will be able to speak for yourself • Does not give permission for physician to withdraw nutrition or hydration if you are permanently unconscious unless indicated on living will • Durable Power of Attorney for Health Care – document that appoints another person to be the health care agent • This person makes any necessary health care decisions for you
NON-MALEFICENCE • “First, do no harm” • Must balance not harming a patient with the belief of doing them good • Treatments believed to do good may result in harm • Important to know how likely it is that a treatment will harm a patient • Double effect: non-maleficence + beneficence • Two types of consequences that may be produced by a single action
JUSTICE • Demands that we act fairly when dealing with patients • We are required to: • Seek an equitable relationship between risk and benefits • Create a fair distribution of the goods of health care
Do you agree with these principles?
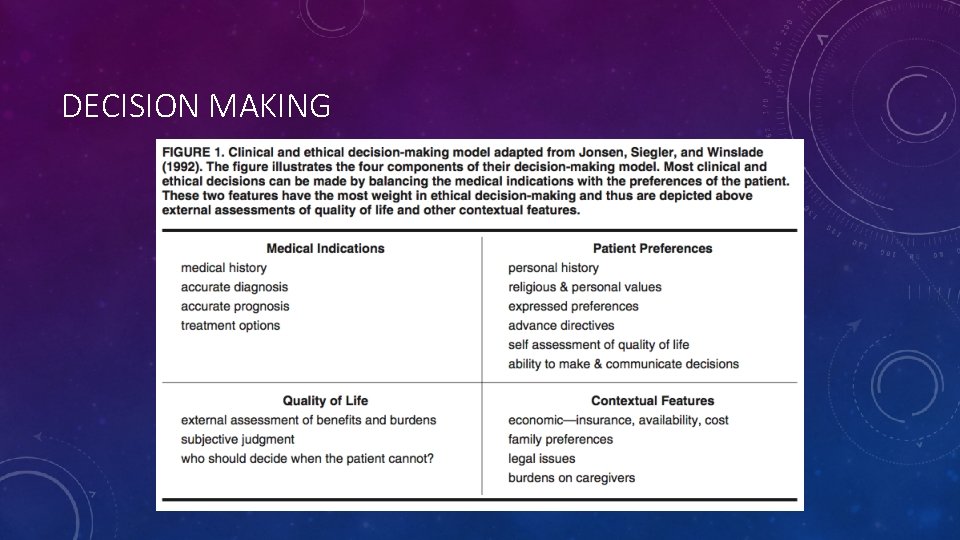
DECISION MAKING
INTERPRETING THE ETHICAL DECISION-MAKING MODEL • Medical indications and patient preferences are considered to be higher priority • Usually these are the basis on which medical and ethical decisions are made • When these are clear, ethical conflicts rarely arise: A competent adult almost universally has the right to accept or refuse a proposed recommendation • However, more often, in ethical conflicts, the medical diagnosis or prognosis and/or patient preferences are unclear or unknown.

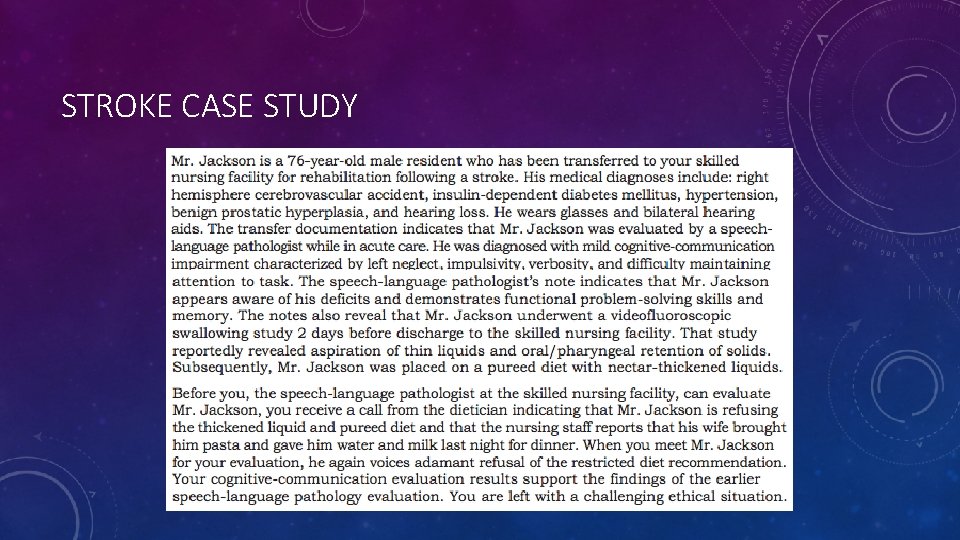
STROKE CASE STUDY
- Slides: 15