Principles of Image Production Focusing cup Xray Tube
Principles of Image Production



Focusing cup
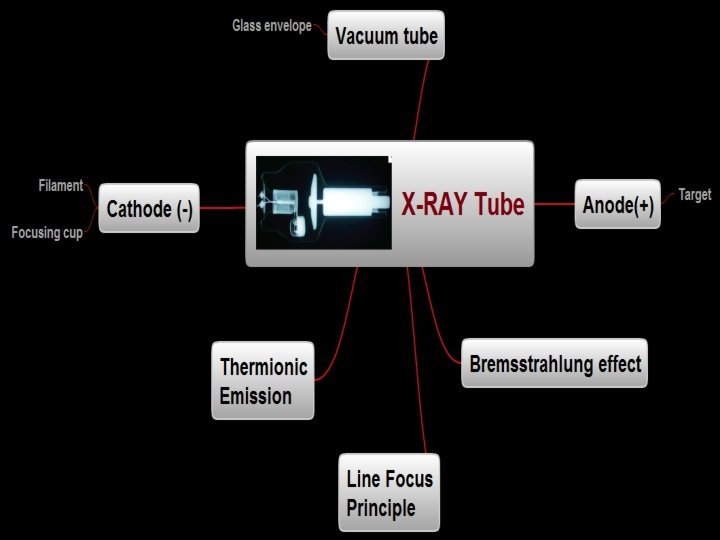
X-ray Tube • Vacuum tube – A device that relies on the flow of electric current through a vacuum • Glass envelope – Good insulator, vacuum tight, high melting point • Tube housing – Lined with 1. 5 mm of lead(pb) to prevent leakage radiation


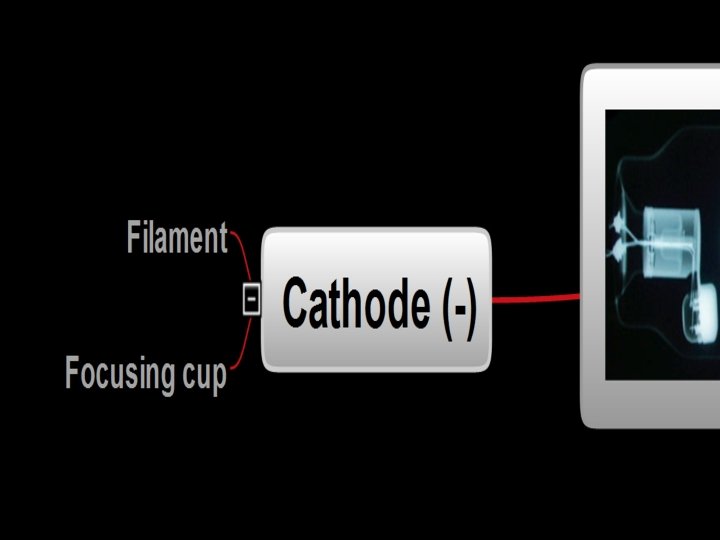
Cathode • Negative electrode • Contains – Focusing cup – Filament

Cathode • Focusing cup – Focuses the electrons on a smaller spot of the anode – Made of nickel, stainless steel or molybdenum – House the filaments
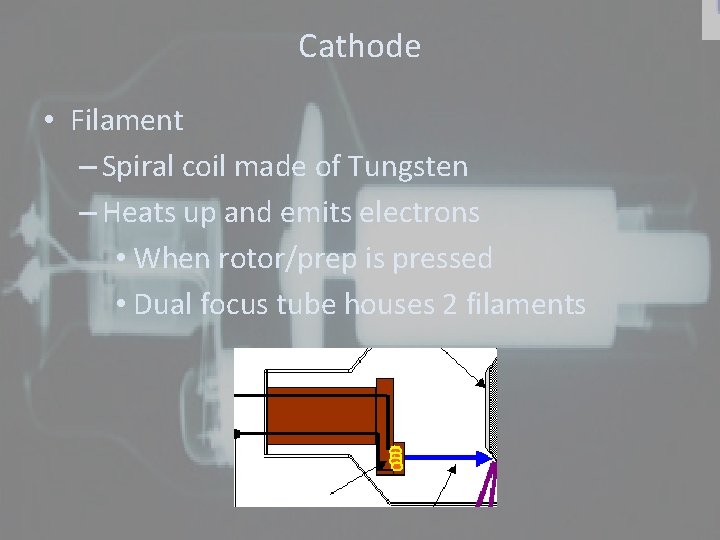
Cathode • Filament – Spiral coil made of Tungsten – Heats up and emits electrons • When rotor/prep is pressed • Dual focus tube houses 2 filaments
Apply your knowledge • What control setting does the radiographer set that would affect the number of electrons being released from the heating of the filament?

Anode • Positive electrode • Electrons strike anode target – Target is made of Tungsten • Stationary or Rotating • Rotating (via induction motor) – Large copper rotor – Steel bearings – Avoids pitting
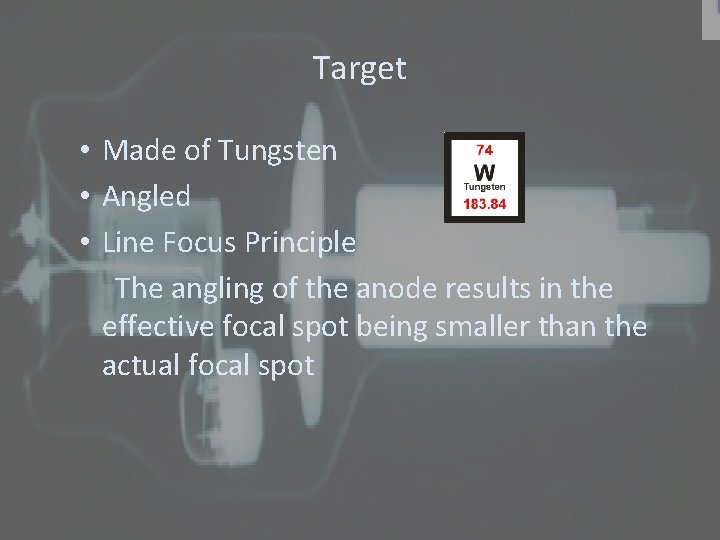
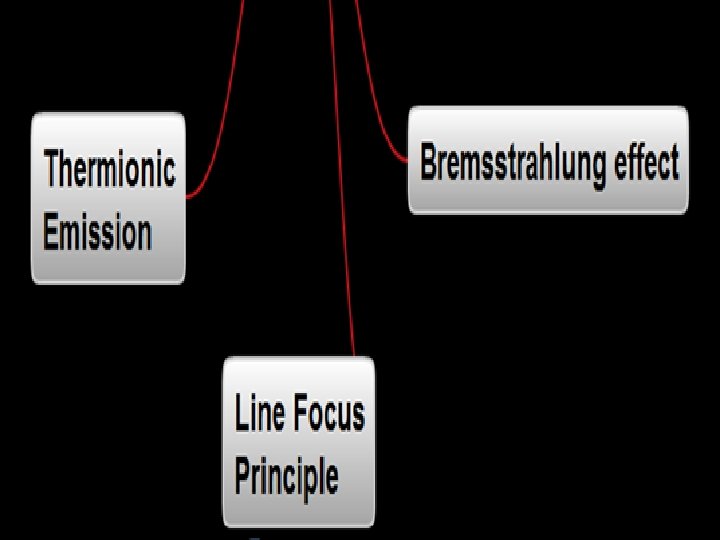
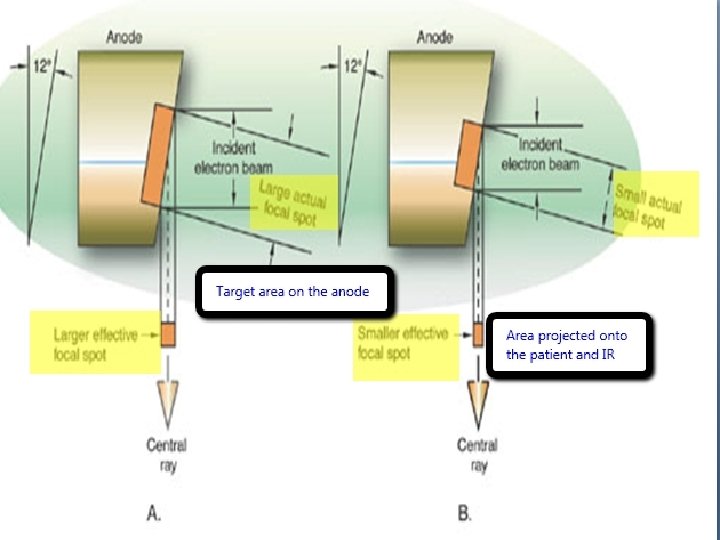
Target • Made of Tungsten • Angled • Line Focus Principle The angling of the anode results in the effective focal spot being smaller than the actual focal spot

Line Focus Principle • Actual FSS – Target area on Anode that is exposed to electrons • Effective FSS – Directly under the anode target – Area projected onto patient and IR
Anode Heel Effect • X-rays are more intense on the cathode side of the tube and less intense toward the anode. • The lowering intensity on the anode side=lighter image on that end • Place thinner or less dense portion of the pts anatomy under anode end (scoliosis series)
Thermionic Emission • Heat induced flow of electrons • Heated filament emits electrons by thermionic emission • Occurs when you press the rotor/prep button

Apply your knowledge • What control setting does the radiographer set that would affect the energy of the electrons as they reach the anode?
X-ray Production • High speed electrons from Cathode, collide with anode target and loose energy • Xrays are produced • Happens when exposure button is pressed

Bremsstrahlung • Occurs when an incident electron interacts w/ the force field of an atomic nucleus. • The force of the nucleus causes the electron to slow down. • As the electron loses energy, it changes direction and the energy loss appears as an xray • 85% of the x-ray beam consists of this interaction
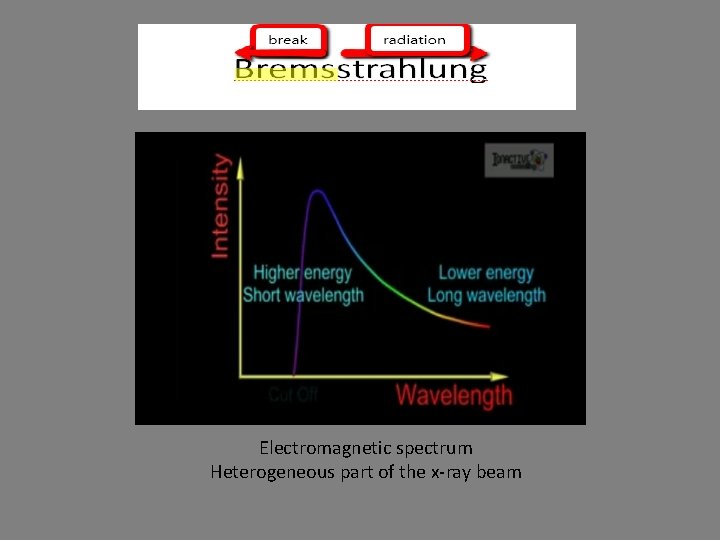
e Electromagnetic spectrum Heterogeneous part of the x-ray beam
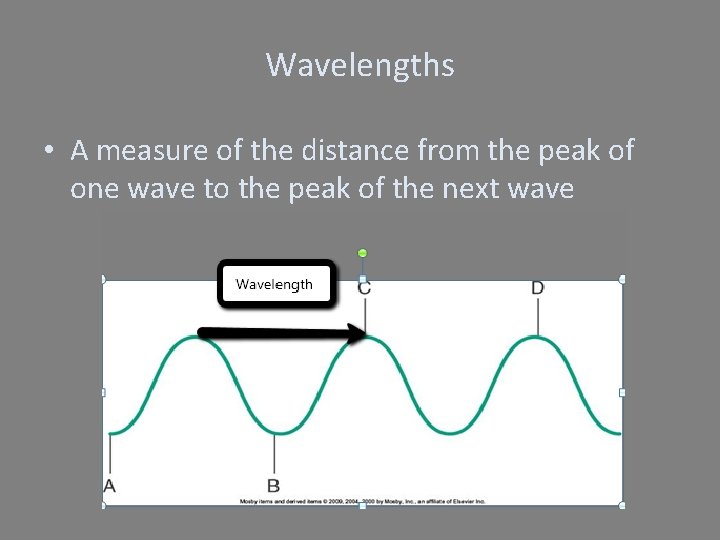
Wavelengths • A measure of the distance from the peak of one wave to the peak of the next wave
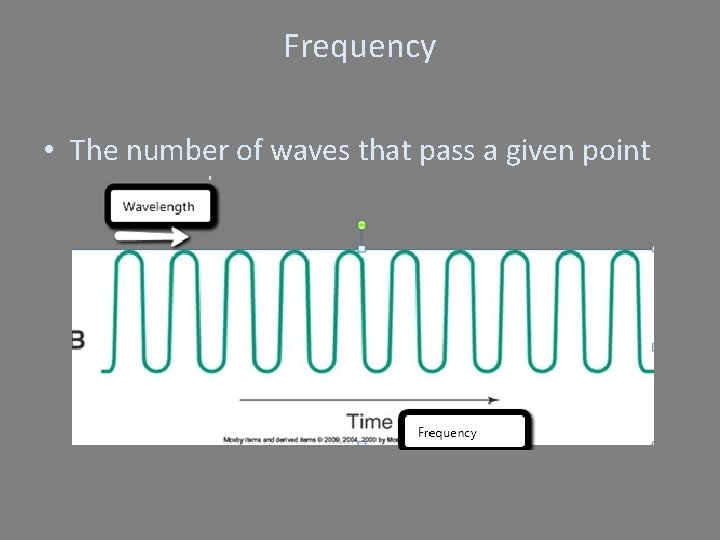
Frequency • The number of waves that pass a given point per second

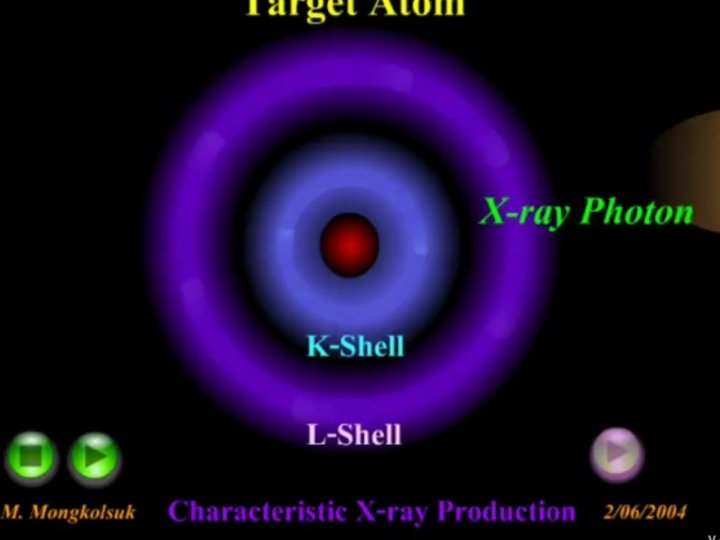
Characteristic Interactions • Projectile electron interacts w/ electron from inner shell(K) of target(tungsten) atom • An outer shell electron drops into the open position & creates an energy difference • The energy difference is emitted as an x-ray • Only K-shell x-rays are diagnostically useful.
X-ray Production 1. Source of free electrons (filament/m. A) set by m. A 1. Filament heats up based on the amount of current (m. A) 2. Thermionic Emission (step down transformer located in the filament circuit) 2. Acceleration of Electrons (k. Vp) Kilovoltage sent to the filament from the step up transformer 3. Focusing of electrons 4. Deceleration of Electrons

Apply Your Knowledge • What Happens When………… – The rotor/prep button is pressed? – When the exposure button is pressed?
Maximize Tube Life

• What are some of the ways a radiographer can help maximize the x-ray tubes life?

Maximize tube life • Use low m. A – Tube current/quantity of electrons – High filament current applied for too long will shorten filament life. – Tungsten from the filament is deposited on to the glass envelope.
Maximize tube life • Make sure tube is warmed up before using Warm up with low m. A exposures High m. A exposures on cold target will crack the target 100 m. A 1 sec 65 -70 k. Vp Large FS
Calculate Heat Unit Follow tube rating charts to prevent excessive heat damage to tube • k. Vp x m. A x T • 3 phase 6 pulse generator • 1. 35 x k. Vp x m. A x sec • 3 phase 12 pulse generator • 1. 41 x k. Vp x m. A x sec
What is the heat unit for a 6 pulse unit set at 70 k. Vp 100 m. A 1/2 sec
Beam Characteristics • Beam Quality- Refers to the penetrating(energy) power of the x-ray beam • Affected by k. Vp Beam filtration • Beam Quantity-Total number(intensity) of x -ray photons in a beam • Affected by m. As, k. Vp, Distance and Filtration
Beam Quality • Penetrating (energy/how fast) power of the beam • Affected by k. Vp and filtration • Directly proportional to k. Vp • k. Vp= beam penetration • High k. Vp=High quality or “Hard” beams • Low k. Vp=Low quality or “Soft” beams
Beam Quality • Filtration Removes the lower energy photons making the quality higher • Half-value layer Beam quality is measured by the half-value layer Thickness of absorbing material (AL) necessary to reduce the energy of the beam to ½ its original intensity

Beam Quantity • Total number of x-ray photons in beam • Affected by – m. As, k. Vp, distance and filtration • m. As is the primary factor • Directly proportional to m. As – Double the m. As=Double output • Square of k. Vp – Double k. Vp=increase quantity by factor of four

Inverse Square Law • Beam Quantity varies inversely as the square of the distance – Inverse Square Law- The intensity of the beam is inversely proportional to the square of the distance – The intensity quadruples if the distance is reduced to ½ of its original value
Apply your knowledge • What will the intensity of a beam be at 40 inches if it is 5 R at 80 inches? • A radiographer receives 120 mrem of exposure standing 5 feet from the radiation source. If the radiographer wants to decrease his exposure to 50 mrem, how far from the radiation source must he stand? • A chest radiograph is produced w/ sufficient optical density using 10 m. As at 72 inches. If the same radiograph is performed at 44 SID , what new m. As should be used to produce the radiograph with the same density?

X-ray Beam • Beam Quality k. Vp Filtration(Half Value Layer) • Beam Quantity m. As k. Vp Distance Filtration (Half Value Layer)
Beam Characteristics Primary vs. Remnant Primary radiation- useful radiation that consists of the x-ray photons directed through the x-ray tube window port “Incident Photons” Remnant radiation- “exit radiation” the portion of the attenuated(progressive absorption) x-ray beam that emerges from the patient and interacts with the image receptor
Fundamental Properties • X-ray is a form of electromagnetic energy • Heterogeneous and polyenergetic Wide variety of wavelengths and energies • X-rays travel in straight line at the speed of light • Ionize Matter Removal of an electron from an atom
Fundamental Properties • Ionize Matter – Removal of an electron from an atom • Ionization is the characteristic of x-rays that make them dangerous in general and harmful to the patient if misused • Damage molecules and DNA, cause chemical changes in cells
Photon Interactions with Matter Purpose: How X-ray photons interact w/ matter(human tissue) Reason: To minimize harm to the patient and produce a quality radiographic image
Compton Interaction • Scattering events that ionize the atom • Incident photon interacts w/ an outer- shell electron, producing a scatter photon and recoil electron • Problems Results in Image fog Adds to patient dose Major source of Occupational radiation dose

Photoelectric Interaction • Total absorption of the incident photon • The atom is ionized • A characteristic cascade producing secondary photon results • An ejected photoelectron exits the atom w/ enough energy to undergo many more interactions • Primary source of patient radiation exposure • Directly impacts contrast
Coherent (Classical) Interactions • AKA: Coherent Scattering or Thomson Scattering • No electron is removed, the atom absorbs the energy & then releases it in a new direction • Contribute only to patient skin exposure • Very low energy • Unmodified

Key Words for Interactions that are happening inside the tube Incident electrons (Bremsstrahlung/Characteristic) Interacts w/ force field (Bremsstrahlung) Dislodges a K-shell electron(Characteristic) Photon interactions w/ matter (human tissue) Incident photons Scatter photon (Compton)
Beam Attenuation

Beam Attenuation • Gradual loss of intensity • Affected by – Thickness of the anatomic part – Atomic number – Tissue density – Energy of the beam (Quality)

Beam Attenuation Tissue Thickness tissue thickness= beam attenuation More x-rays are absorbed or scattered by the tissue so more radiation is needed to produce an image
Beam Attenuation Atomic Number High atomic number (bone)= attenuation= bright image Lower atomic number (fat)= attenuation= light image
Beam Attenuation Tissue Density Compactness of the atomic particles in tissue density= attenuation Bone Muscle Fat Air
Beam Attenuation Quality of the beam Higher penetrating x-rays (shorter wavelength w/ higher frequency) =lower attenuation Lower penetrating x-rays (longer wavelength w/ lower frequency)=higher attenuation
- Slides: 60