Principles of Hemodynamics Relationship between pressure 2 flow
Principles of Hemodynamics ¤ Relationship between; pressure 2. flow 3. resistance in the circulatory system 1. ¤ It is important to focus on how these relationships interact with each other Cardiac output ¤ Systemic vascular resistance ¤ Blood pressure ¤
Hemodynamic Assessment • Catheter is a ‘hollow plastic tube’ so we can get. . – Pressure wave – Sa. O 2 by Oxymetry • Representative usefulness of cardiac cath in hemodynamic assessment – Pressure wave in each cardiac chamber – Cardiac output – Detection of cardiac shunt
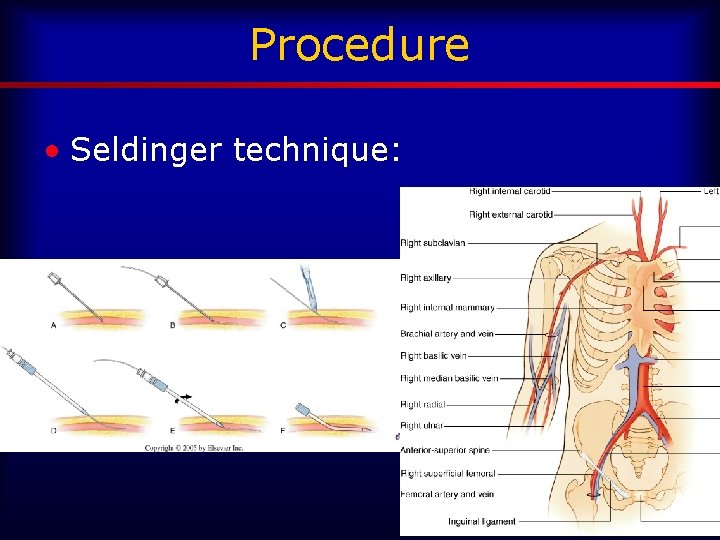
Procedure • Seldinger technique:
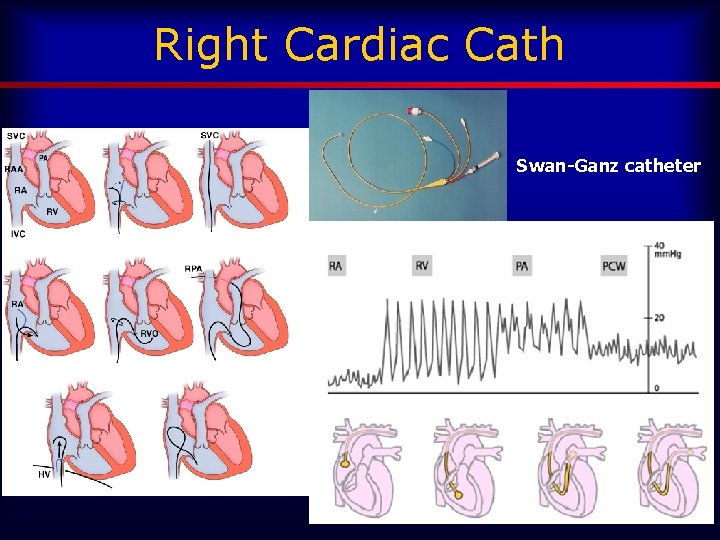
Right Cardiac Cath Swan-Ganz catheter
What is a Swan? Ø Full name: Swan-Ganz Catheter Ø Pulmonary Artery (PA) Catheter = right heart catheter
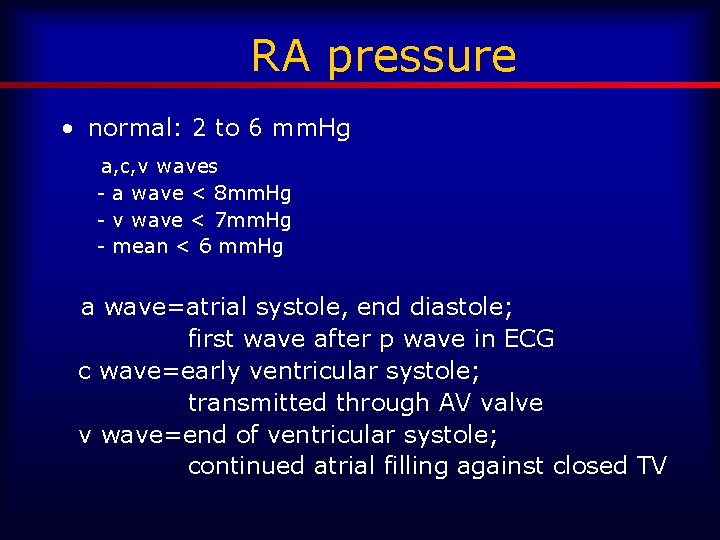
RA pressure • normal: 2 to 6 mm. Hg a, c, v waves - a wave < 8 mm. Hg - v wave < 7 mm. Hg - mean < 6 mm. Hg a wave=atrial systole, end diastole; first wave after p wave in ECG c wave=early ventricular systole; transmitted through AV valve v wave=end of ventricular systole; continued atrial filling against closed TV
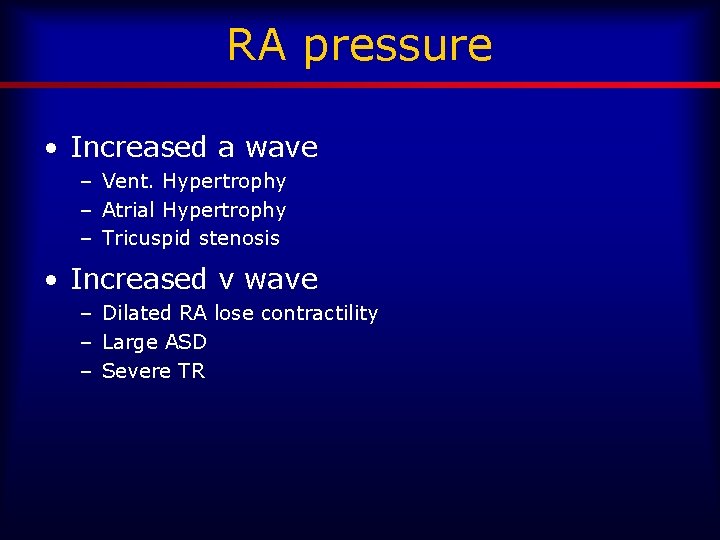
RA pressure • Increased a wave – Vent. Hypertrophy – Atrial Hypertrophy – Tricuspid stenosis • Increased v wave – Dilated RA lose contractility – Large ASD – Severe TR
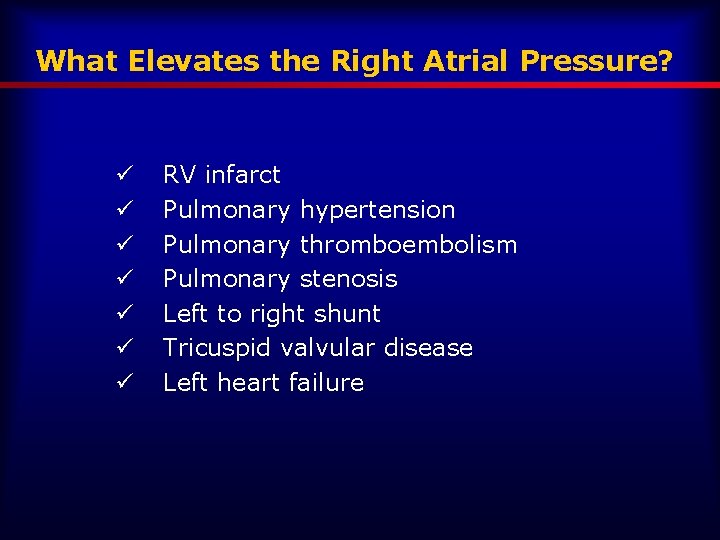
What Elevates the Right Atrial Pressure? ü ü ü ü RV infarct Pulmonary hypertension Pulmonary thromboembolism Pulmonary stenosis Left to right shunt Tricuspid valvular disease Left heart failure
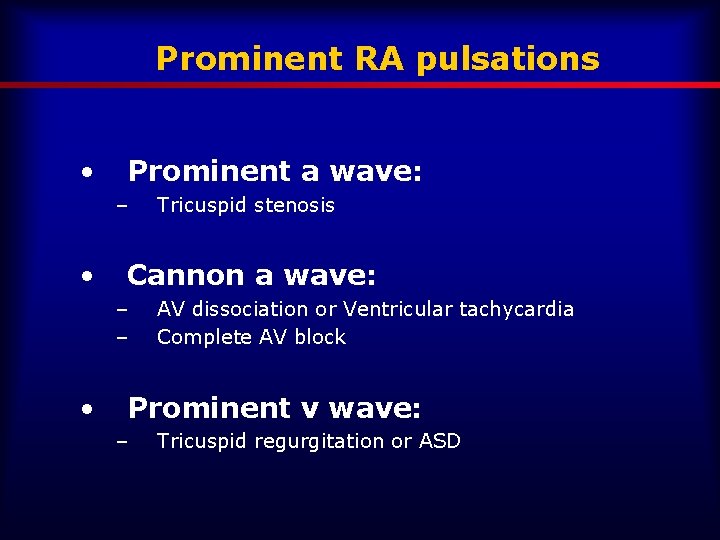
Prominent RA pulsations • Prominent a wave: – • Cannon a wave: – – • Tricuspid stenosis AV dissociation or Ventricular tachycardia Complete AV block Prominent v wave: – Tricuspid regurgitation or ASD
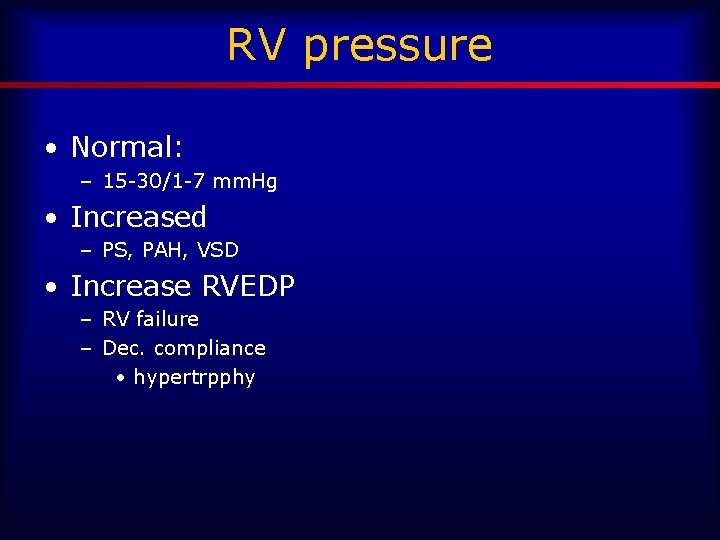
RV pressure • Normal: – 15 -30/1 -7 mm. Hg • Increased – PS, PAH, VSD • Increase RVEDP – RV failure – Dec. compliance • hypertrpphy
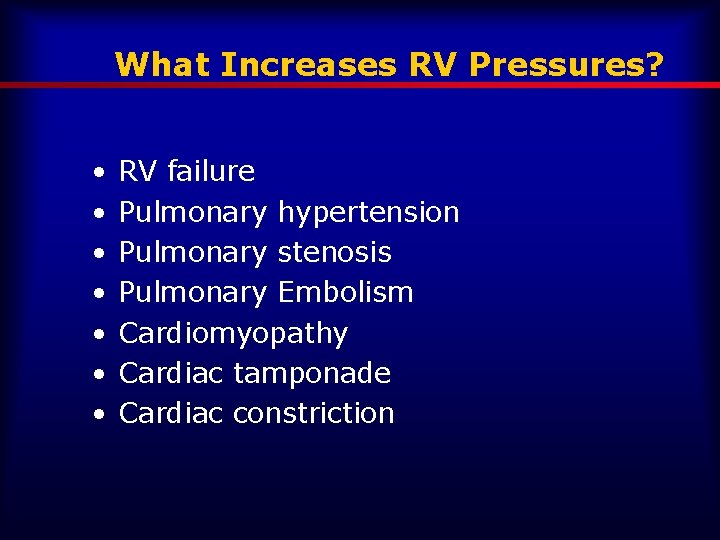
What Increases RV Pressures? • • RV failure Pulmonary hypertension Pulmonary stenosis Pulmonary Embolism Cardiomyopathy Cardiac tamponade Cardiac constriction
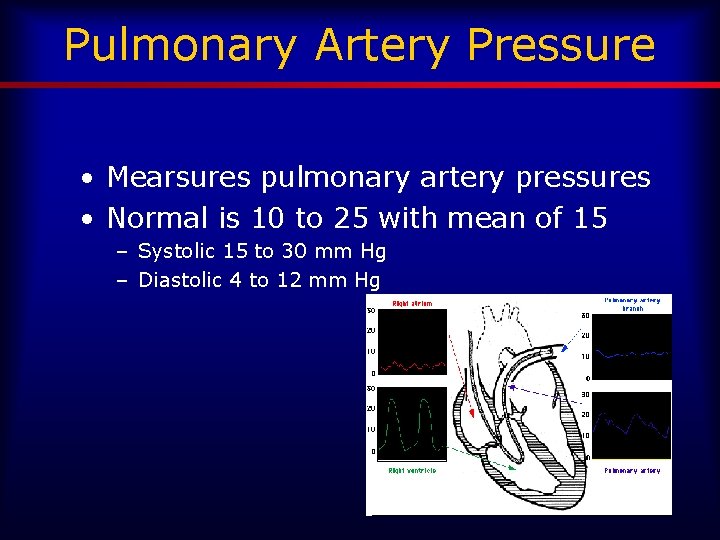
Pulmonary Artery Pressure • Mearsures pulmonary artery pressures • Normal is 10 to 25 with mean of 15 – Systolic 15 to 30 mm Hg – Diastolic 4 to 12 mm Hg
Left Cardiac Cath • LV pressure wave • Systemic vascular resistance
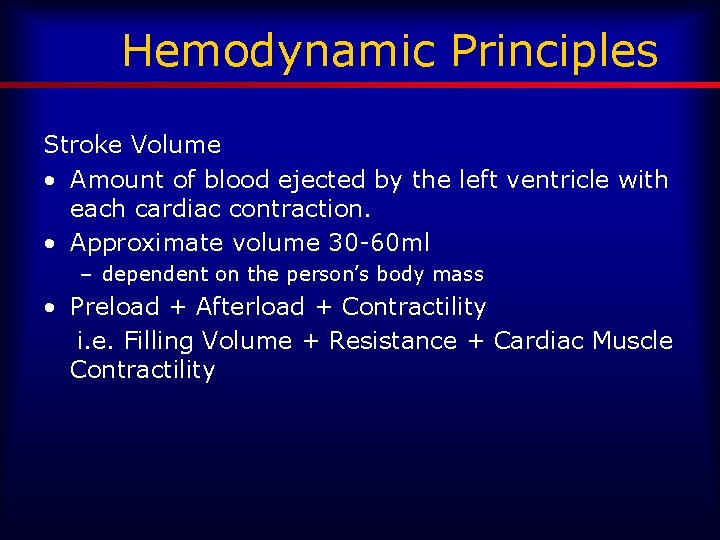
Hemodynamic Principles Stroke Volume • Amount of blood ejected by the left ventricle with each cardiac contraction. • Approximate volume 30 -60 ml – dependent on the person’s body mass • Preload + Afterload + Contractility i. e. Filling Volume + Resistance + Cardiac Muscle Contractility
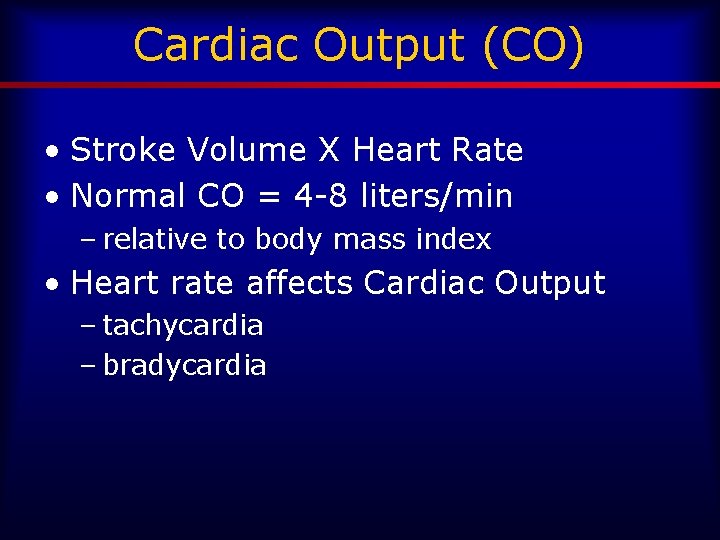
Cardiac Output (CO) • Stroke Volume X Heart Rate • Normal CO = 4 -8 liters/min – relative to body mass index • Heart rate affects Cardiac Output – tachycardia – bradycardia
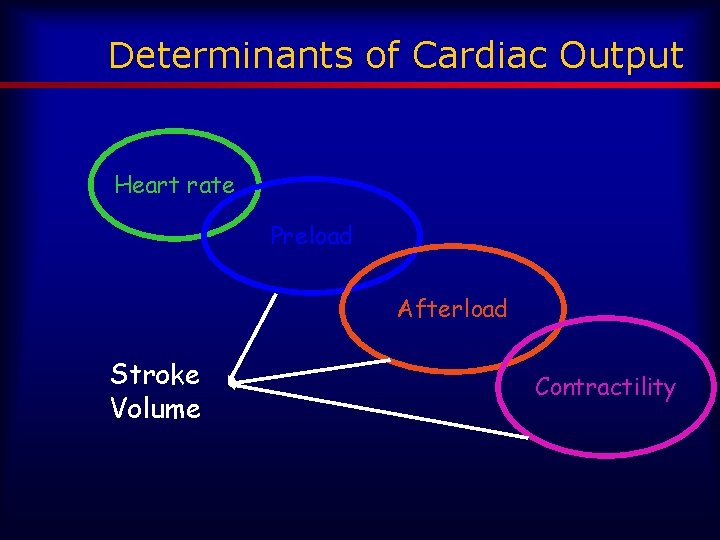
Determinants of Cardiac Output Heart rate Preload Afterload Stroke Volume Contractility
Preload • Central Venous Pressure (CVP) measures from the venous system (superior & inferior vena cava entering the right atrium) • Normal is 0 -8 mm. Hg • Pulmonary Artery Wedge Pressure (PAWP) estimates LA pressure
Low Central Venous Pressure • Indicates – decreased venous return – hypovolemia
Elevated Central Venous Pressure • Indicates: – fluid overload – right-sided heart failure – increased venous return
Correlation • Decreased CVP= decreased CO (decreased volume/preload) • Increased CVP=increased CO (increased preload)
Afterload • Systemic Vascular Resistance (SVR) – Measures resistance (impedance) met from blood entering the arterial bed from the left side of the heart • Pulmonary Vascular Resistance (PVR) – Measures resistance (impedance) met from the blood entering the arterial bed of the pulmonary vasculature from the right side of the heart. • Increased SVR & PVR - increases myocardial workload and myocardial oxygen consumption
Systemic Vascular Resistance (SVR) • Mechanisms that cause vasoconstriction increase SVR, and those mechanisms that cause vasodilation decrease SVR. • SVR can be calculated if cardiac output (CO), mean arterial pressure (MAP), and central venous pressure (CVP) are known. • SVR = 80 X (MAP - CVP) ÷ CO • Normal Systemic Vascular Resistance is 800 -1200 (dynexsec)/cm 5
Correlation • Increased Cardiac Output= Decreased SVR – Fever – Septic Shock – Anemia – Aortic Regurgitation
Correlation • Decreased Cardiac Output= Increased SVR – Hypertension – Hypovolemia – Cardiogenic Shock – Hypothermia
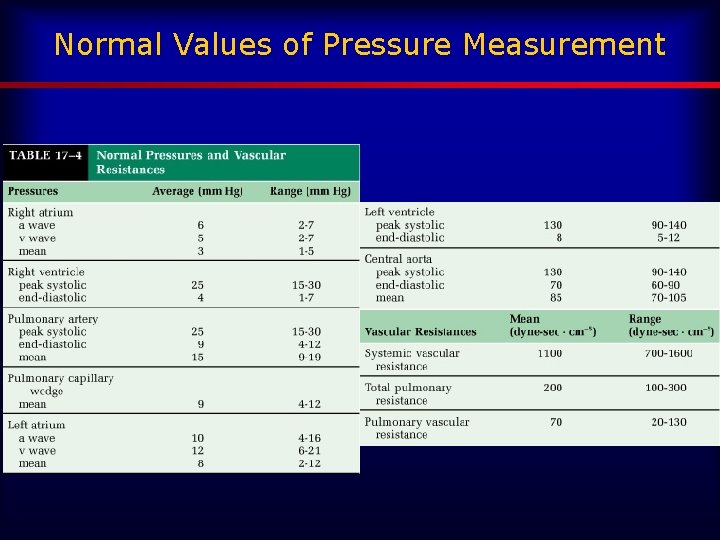
Normal Values of Pressure Measurement
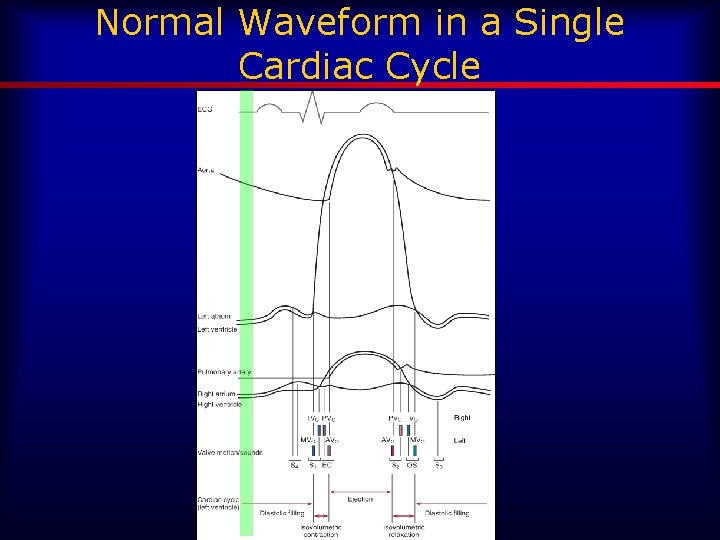
Normal Waveform in a Single Cardiac Cycle
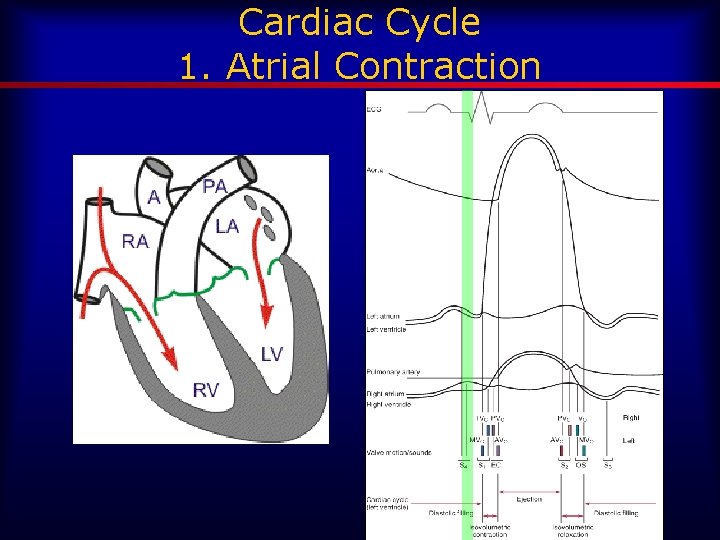
Cardiac Cycle 1. Atrial Contraction
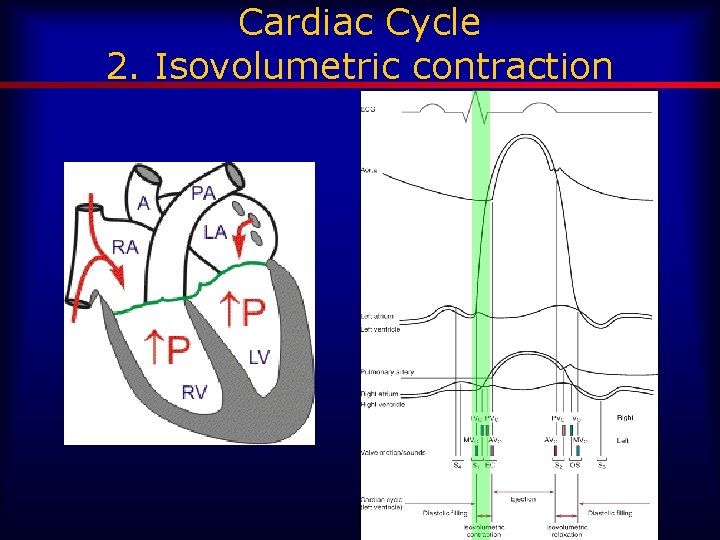
Cardiac Cycle 2. Isovolumetric contraction
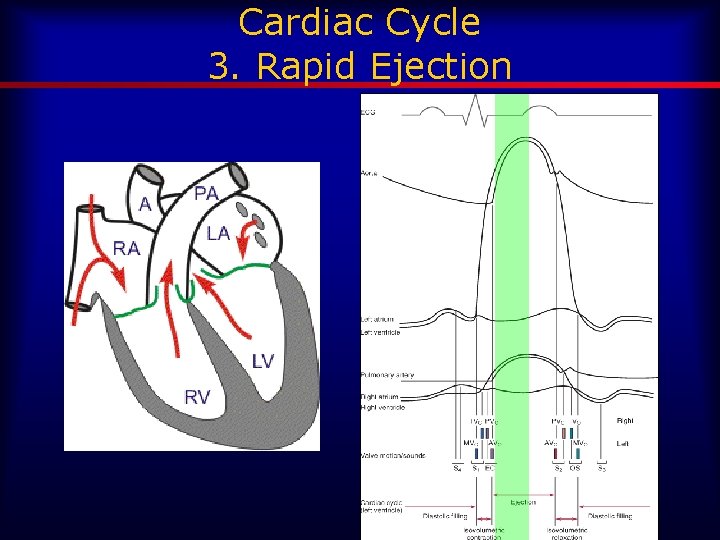
Cardiac Cycle 3. Rapid Ejection
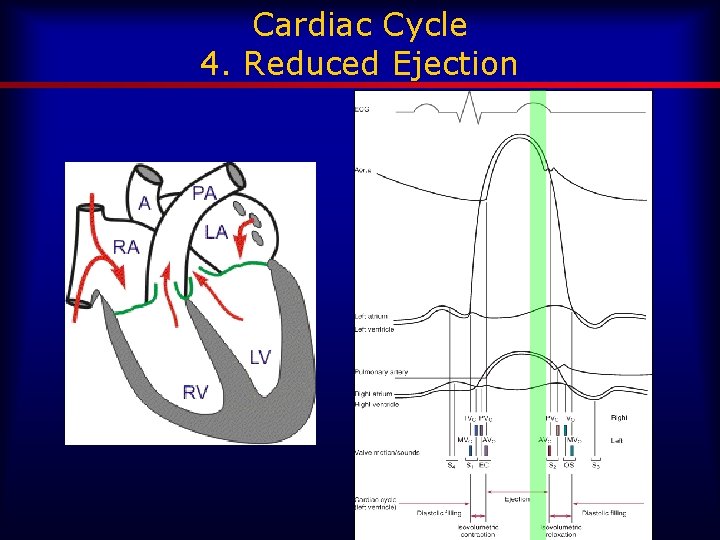
Cardiac Cycle 4. Reduced Ejection
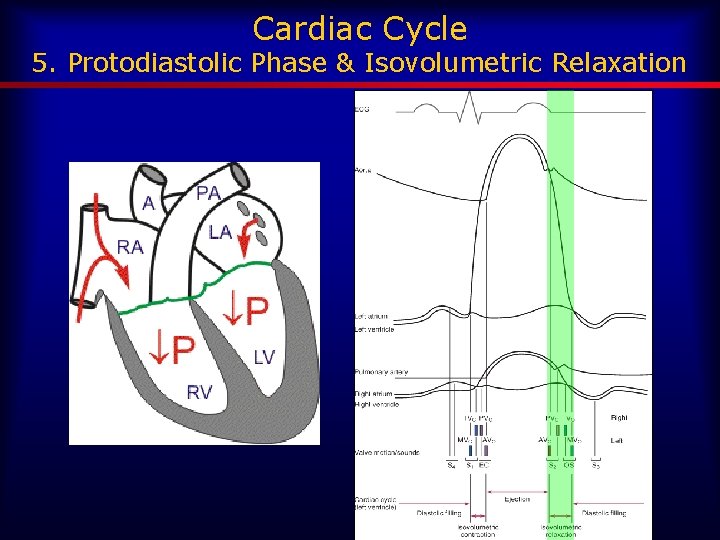
Cardiac Cycle 5. Protodiastolic Phase & Isovolumetric Relaxation
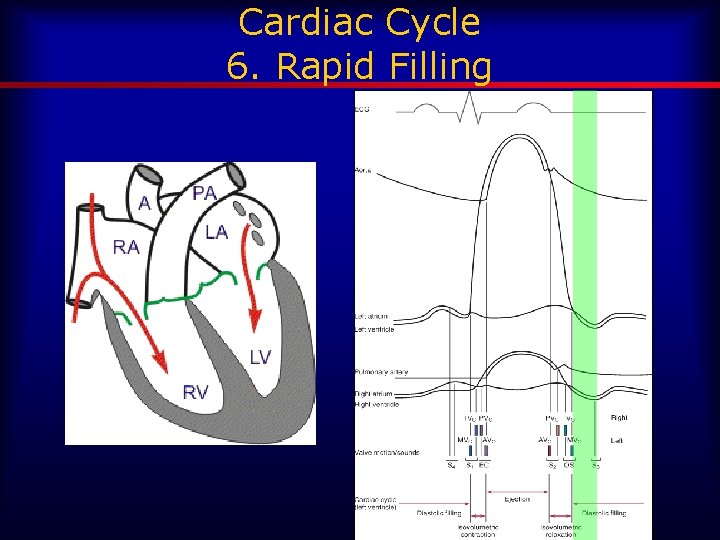
Cardiac Cycle 6. Rapid Filling
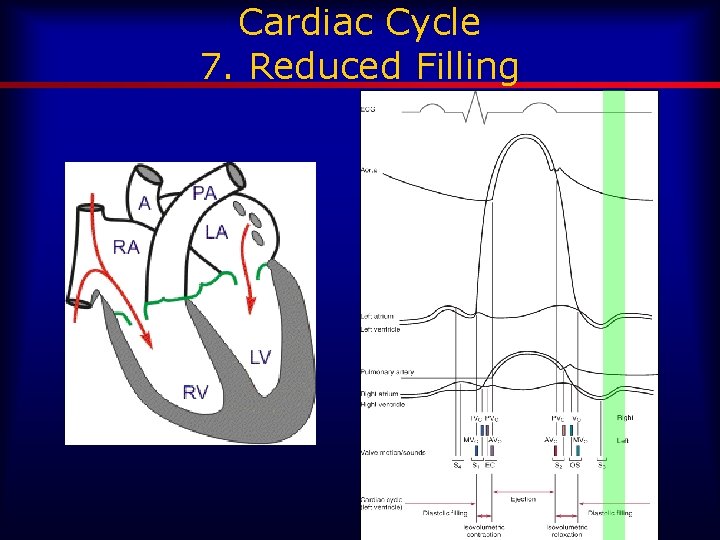
Cardiac Cycle 7. Reduced Filling
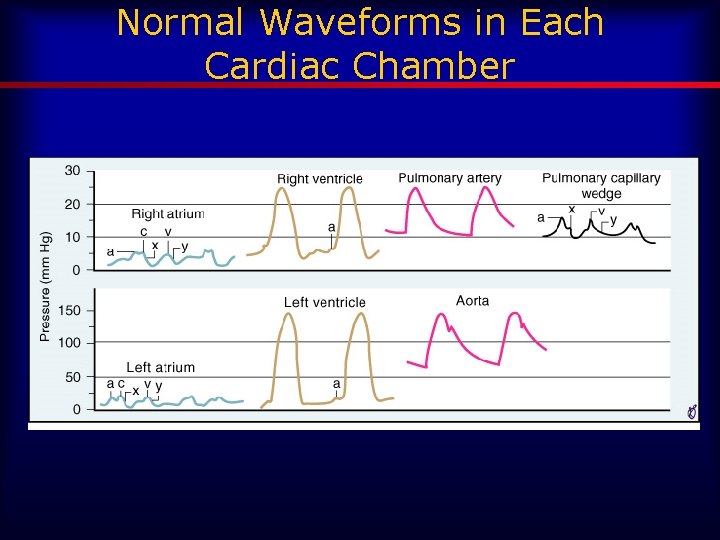
Normal Waveforms in Each Cardiac Chamber
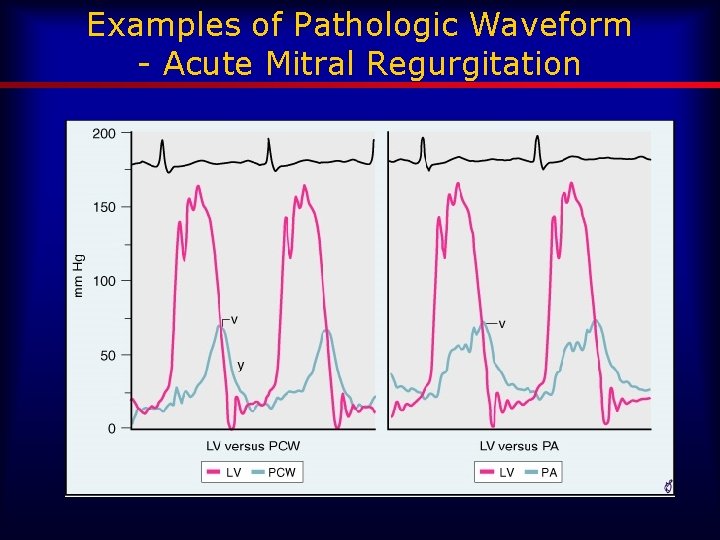
Examples of Pathologic Waveform - Acute Mitral Regurgitation
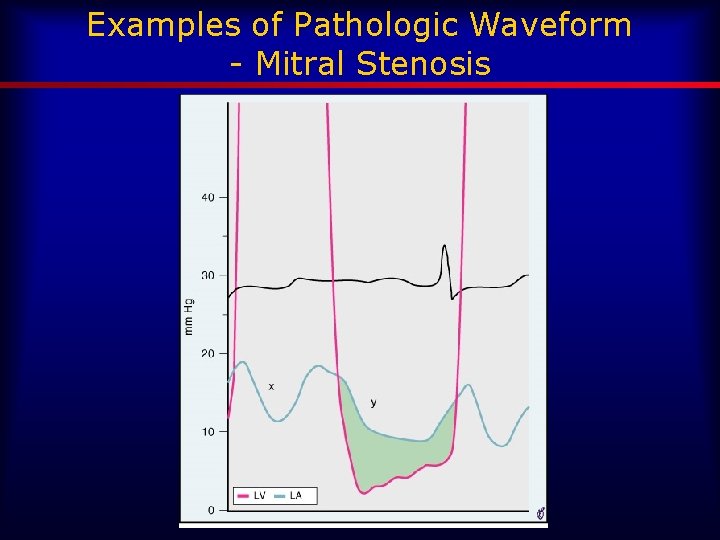
Examples of Pathologic Waveform - Mitral Stenosis
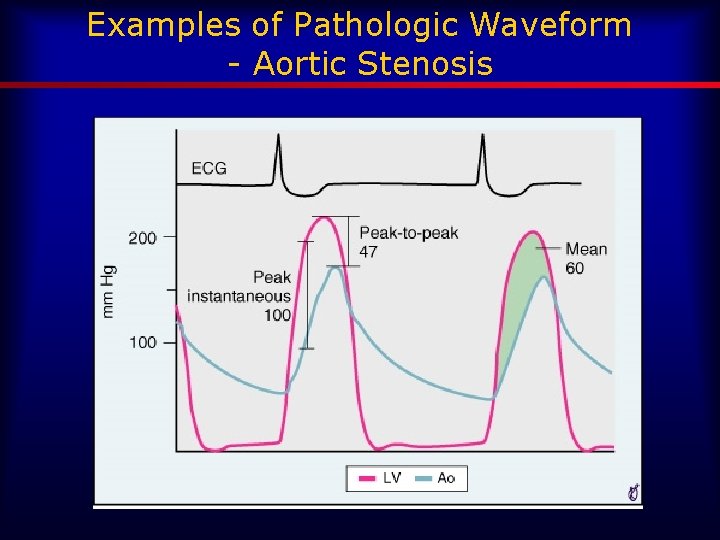
Examples of Pathologic Waveform - Aortic Stenosis
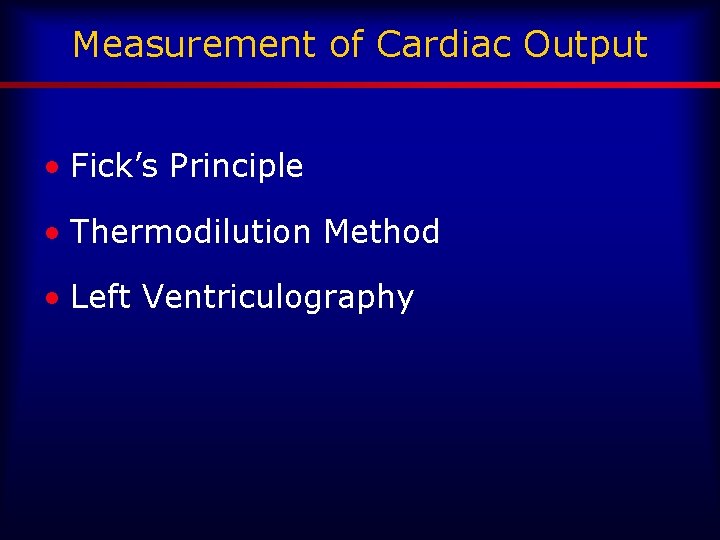
Measurement of Cardiac Output • Fick’s Principle • Thermodilution Method • Left Ventriculography
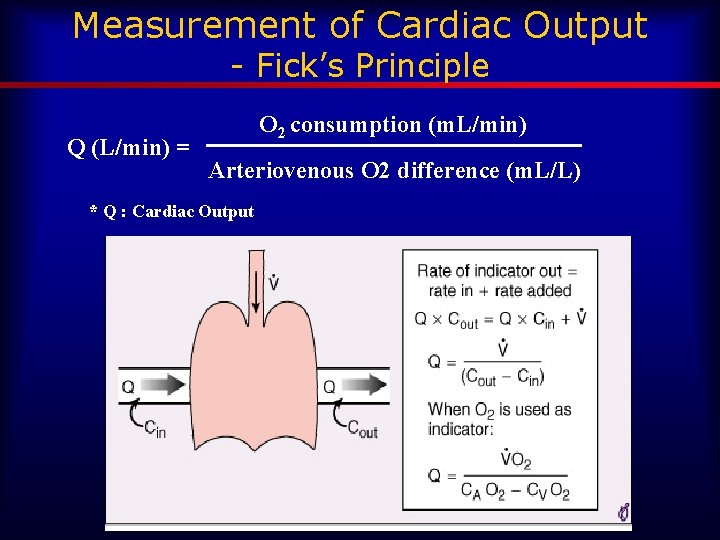
Measurement of Cardiac Output - Fick’s Principle Q (L/min) = O 2 consumption (m. L/min) Arteriovenous O 2 difference (m. L/L) * Q : Cardiac Output
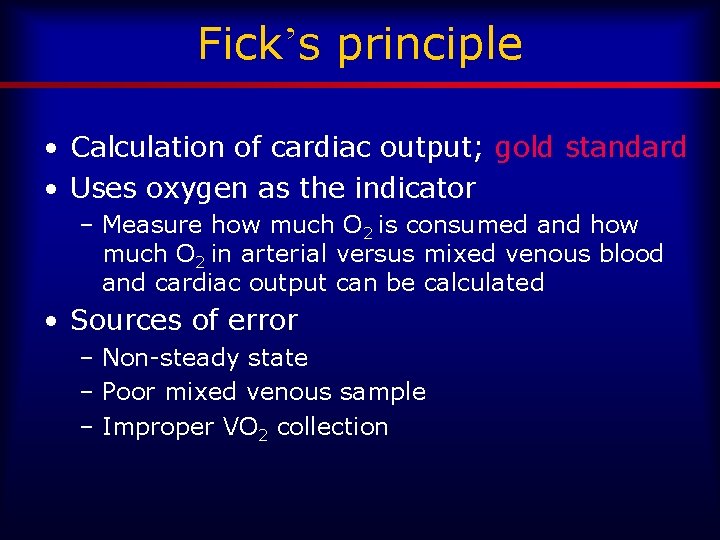
Fick’s principle • Calculation of cardiac output; gold standard • Uses oxygen as the indicator – Measure how much O 2 is consumed and how much O 2 in arterial versus mixed venous blood and cardiac output can be calculated • Sources of error – Non-steady state – Poor mixed venous sample – Improper VO 2 collection
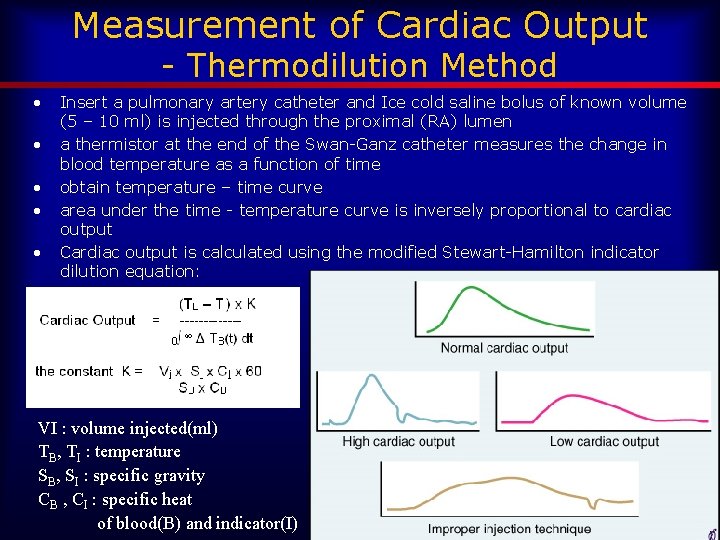
Measurement of Cardiac Output - Thermodilution Method • • • Insert a pulmonary artery catheter and Ice cold saline bolus of known volume (5 – 10 ml) is injected through the proximal (RA) lumen a thermistor at the end of the Swan-Ganz catheter measures the change in blood temperature as a function of time obtain temperature – time curve area under the time - temperature curve is inversely proportional to cardiac output Cardiac output is calculated using the modified Stewart-Hamilton indicator dilution equation: VI : volume injected(ml) TB, TI : temperature SB, SI : specific gravity CB , CI : specific heat of blood(B) and indicator(I)
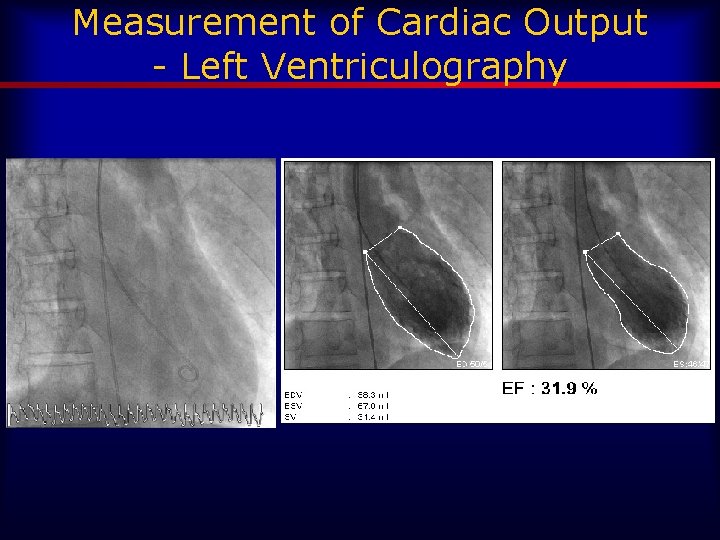
Measurement of Cardiac Output - Left Ventriculography
Vascular Resistance • From Left and Right heart catheterization • SVR = 80 x (MAP – RA) / SBF PVR = 80 x (PA – PCW or LA) / PBF
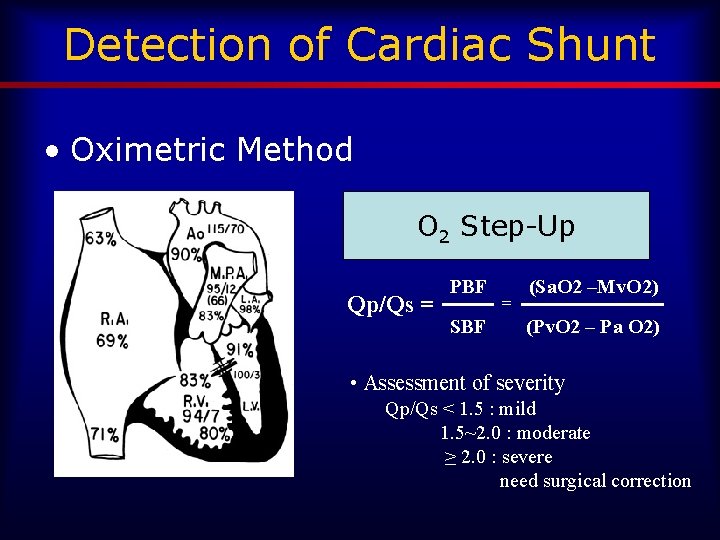
Detection of Cardiac Shunt • Oximetric Method O 2 Step-Up Qp/Qs = PBF SBF = (Sa. O 2 –Mv. O 2) (Pv. O 2 – Pa O 2) • Assessment of severity Qp/Qs < 1. 5 : mild 1. 5~2. 0 : moderate ≥ 2. 0 : severe need surgical correction
- Slides: 45