Principles of Gynecological Procedures AMER SALAMAT OBJECTIVES AMER
Principles of Gynecological Procedures AMER SALAMAT
OBJECTIVES • AMER PART: Anatomical revision of female Genitalia , and Hysterectomy. • ALA’A PART: Cervical Conization, Cervical Cerclage, Colporaphy, Dilation & Curettage. • LEEN PART: Hysteroscopy, Laparoscopy Cystoscopy, Myotectomy, Hysterosalpingogram (HSG)
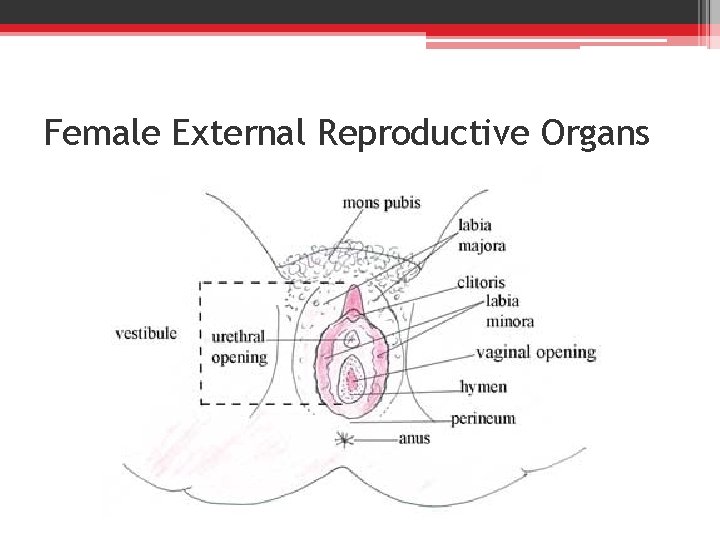
Female External Reproductive Organs
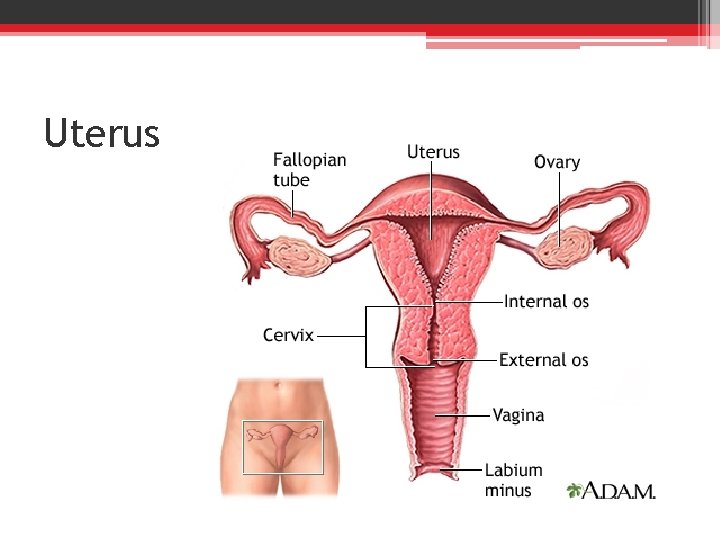
Uterus
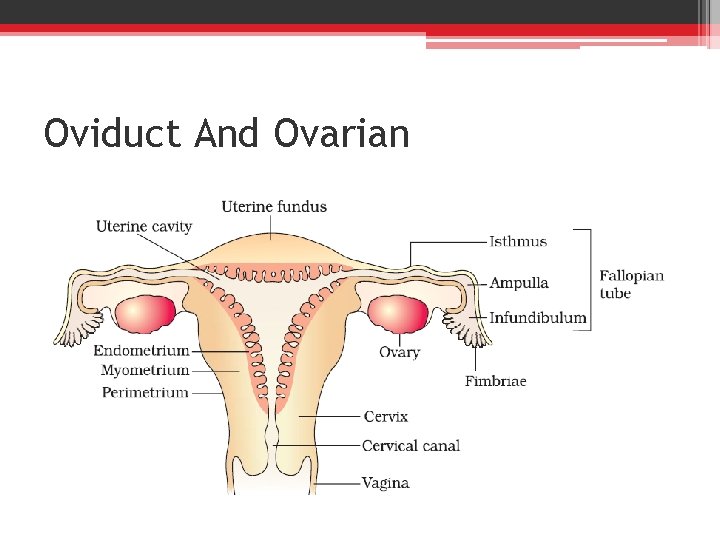
Oviduct And Ovarian
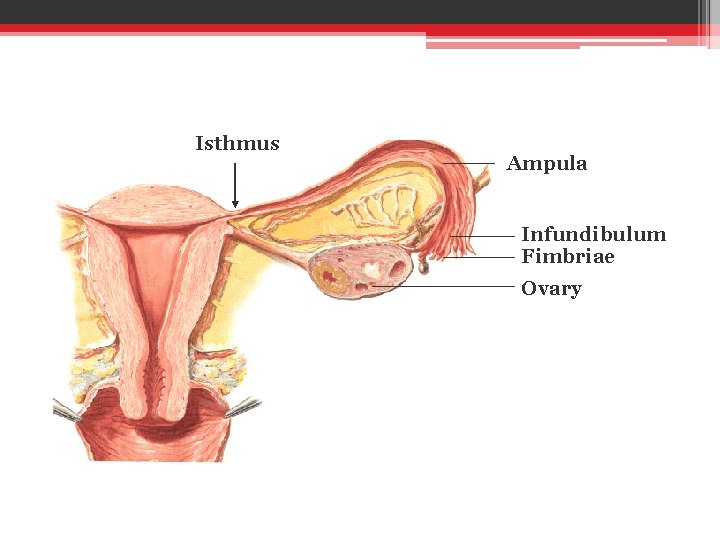
Isthmus Ampula Infundibulum Fimbriae Ovary
Hysterectomy
• Is an operation to remove a woman's uterus, and it is one of the commonest surgical procedures in gynaecology. • It is commonly performed for heavy or painful or irregular periods, when medical treatment or less invasive surgery such as endometrial ablation has failed.
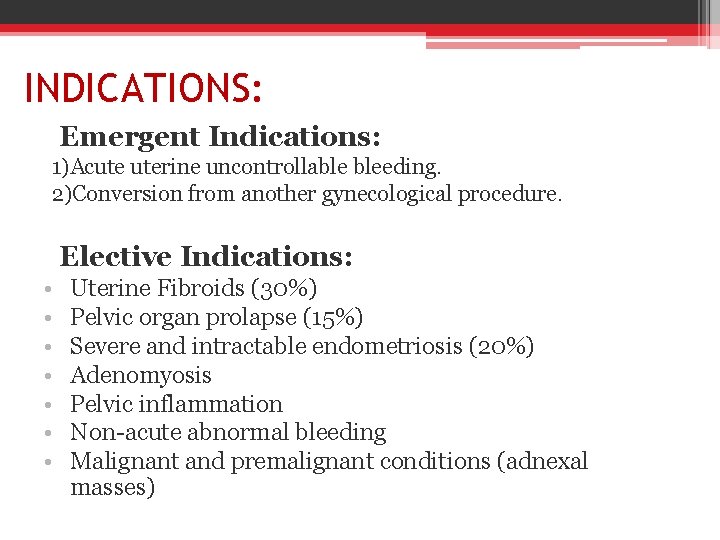
INDICATIONS: Emergent Indications: 1)Acute uterine uncontrollable bleeding. 2)Conversion from another gynecological procedure. Elective Indications: • • Uterine Fibroids (30%) Pelvic organ prolapse (15%) Severe and intractable endometriosis (20%) Adenomyosis Pelvic inflammation Non-acute abnormal bleeding Malignant and premalignant conditions (adnexal masses)
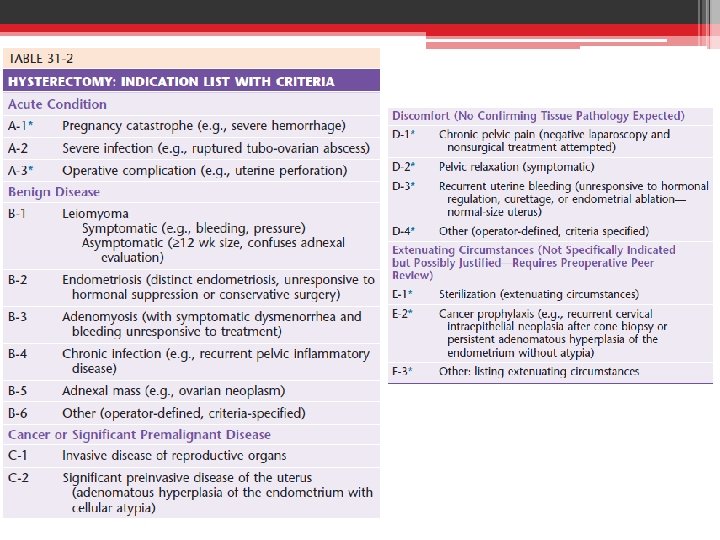
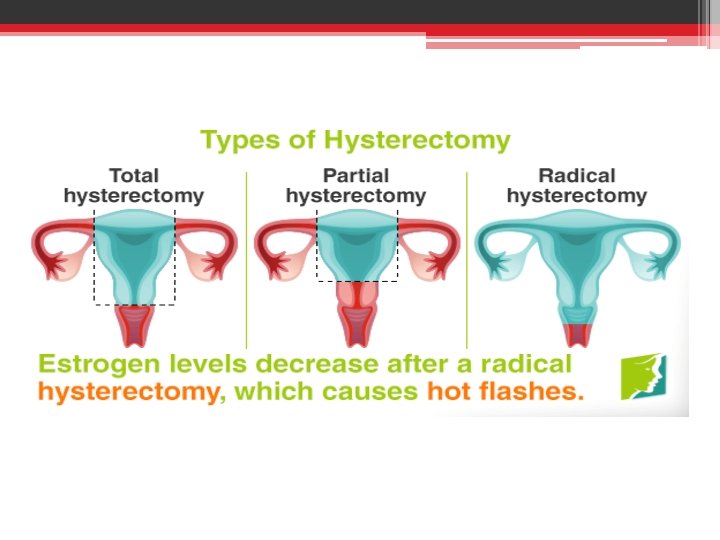
Types I. Subtotal (supracervical) II. Total(simple) III. Radical
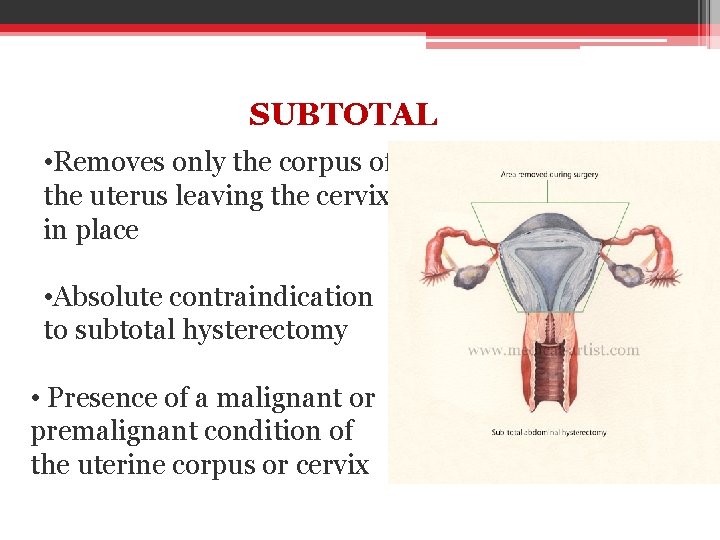
SUBTOTAL • Removes only the corpus of the uterus leaving the cervix in place • Absolute contraindication to subtotal hysterectomy • Presence of a malignant or premalignant condition of the uterine corpus or cervix
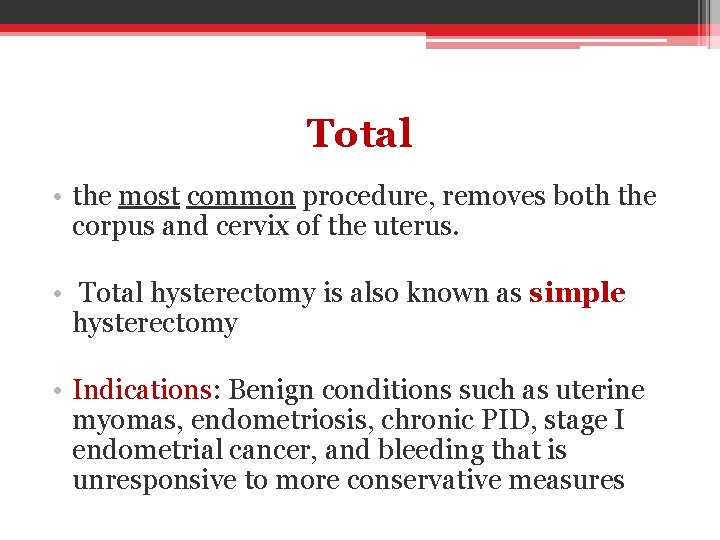
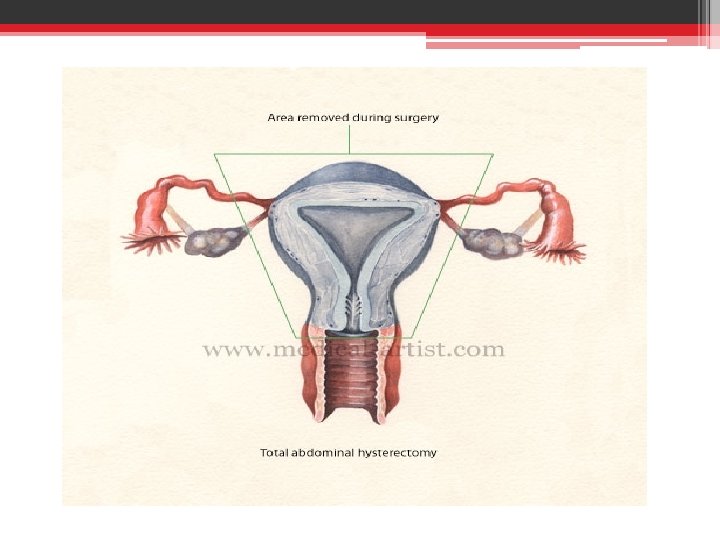
Total • the most common procedure, removes both the corpus and cervix of the uterus. • Total hysterectomy is also known as simple hysterectomy • Indications: Benign conditions such as uterine myomas, endometriosis, chronic PID, stage I endometrial cancer, and bleeding that is unresponsive to more conservative measures
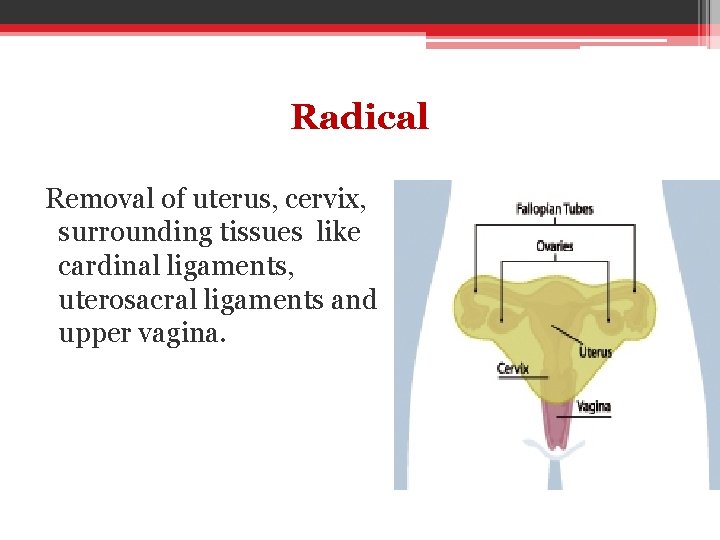
Radical Removal of uterus, cervix, surrounding tissues like cardinal ligaments, uterosacral ligaments and upper vagina.
Routes: 1. Abdominal 2. Vaginal. 3. Laproscopic 4. Laproscopic-assisted -Performed either under Regional or General Anaesthesia.
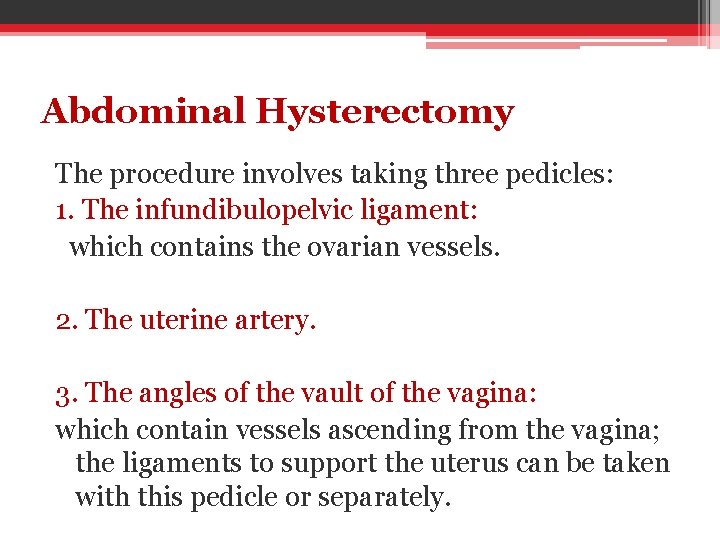
Abdominal Hysterectomy The procedure involves taking three pedicles: 1. The infundibulopelvic ligament: which contains the ovarian vessels. 2. The uterine artery. 3. The angles of the vault of the vagina: which contain vessels ascending from the vagina; the ligaments to support the uterus can be taken with this pedicle or separately.
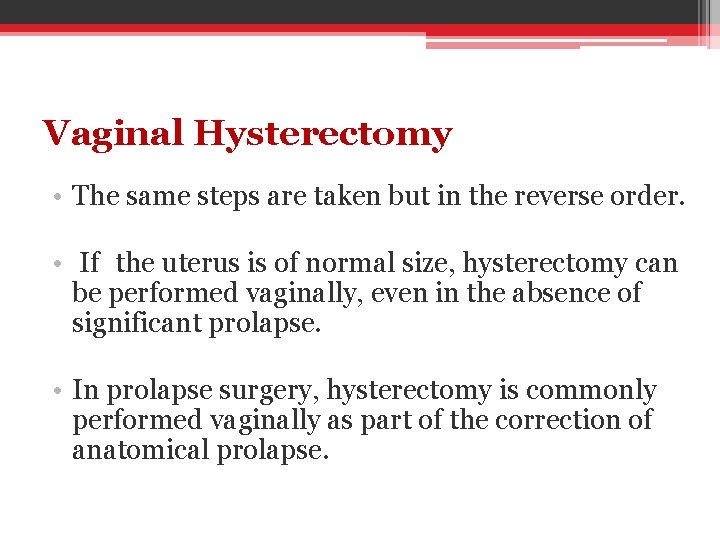
Vaginal Hysterectomy • The same steps are taken but in the reverse order. • If the uterus is of normal size, hysterectomy can be performed vaginally, even in the absence of significant prolapse. • In prolapse surgery, hysterectomy is commonly performed vaginally as part of the correction of anatomical prolapse.
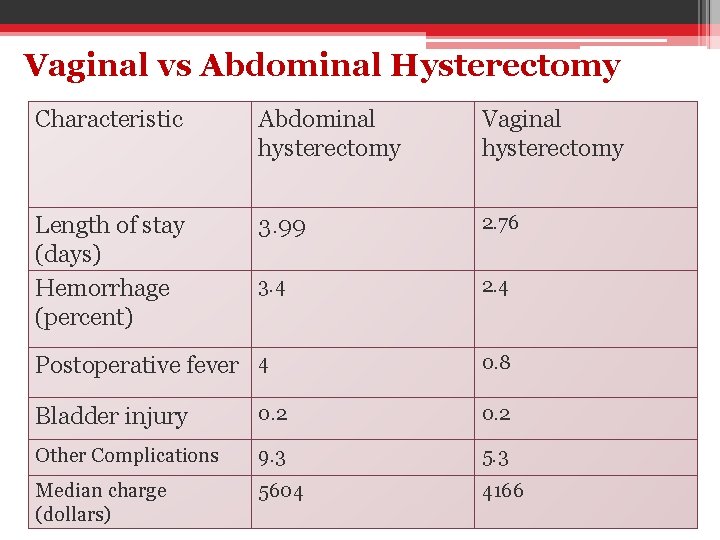
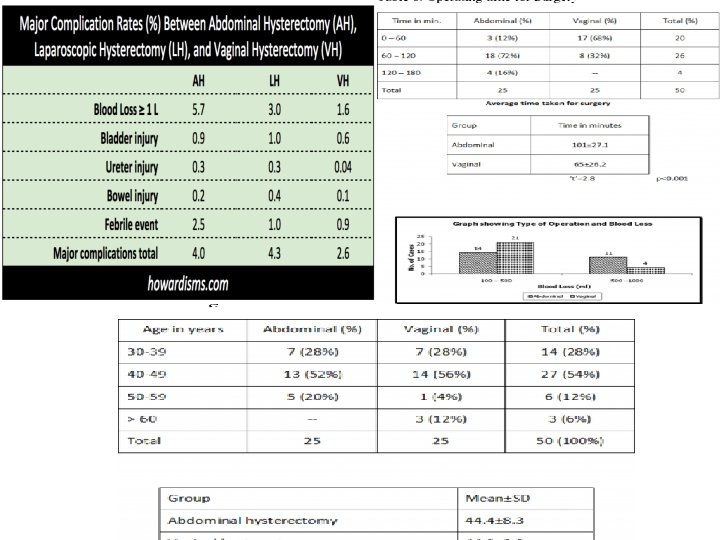
Vaginal vs Abdominal Hysterectomy Characteristic Abdominal hysterectomy Vaginal hysterectomy Length of stay (days) Hemorrhage (percent) 3. 99 2. 76 3. 4 2. 4 Postoperative fever 4 0. 8 Bladder injury 0. 2 Other Complications 9. 3 5. 3 Median charge (dollars) 5604 4166

LAVH, laparoscopic-aided vaginal hysterectomy; TLH, total laparoscopic hysterectomy.
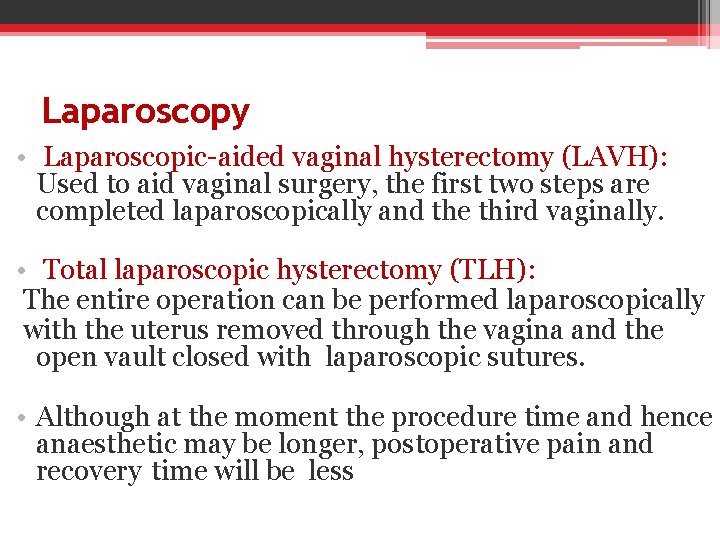
Laparoscopy • Laparoscopic-aided vaginal hysterectomy (LAVH): Used to aid vaginal surgery, the first two steps are completed laparoscopically and the third vaginally. • Total laparoscopic hysterectomy (TLH): The entire operation can be performed laparoscopically with the uterus removed through the vagina and the open vault closed with laparoscopic sutures. • Although at the moment the procedure time and hence anaesthetic may be longer, postoperative pain and recovery time will be less
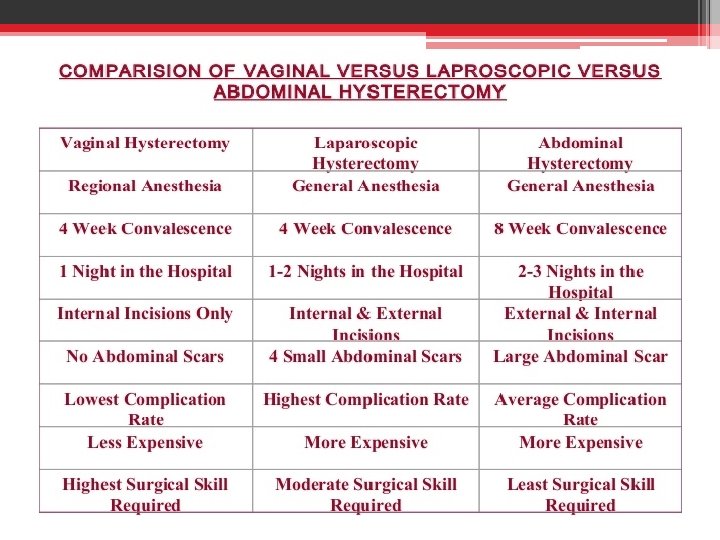
So. . The choice of abdominal or vaginal route for hysterectomy has to balance the benefits and risks of each approach. It is now generally agreed that vaginal surgery requires a shorter time in hospital and less recovery time before full mobility and activity is resumed.

Pre and post Operative Assessment • Preoperative Care: 1. 2. 3. 4. 5. Full History and Physical Examination. Investigation. Counseling and acquiring an informed consent. Psychological preparation. Medical consultation.
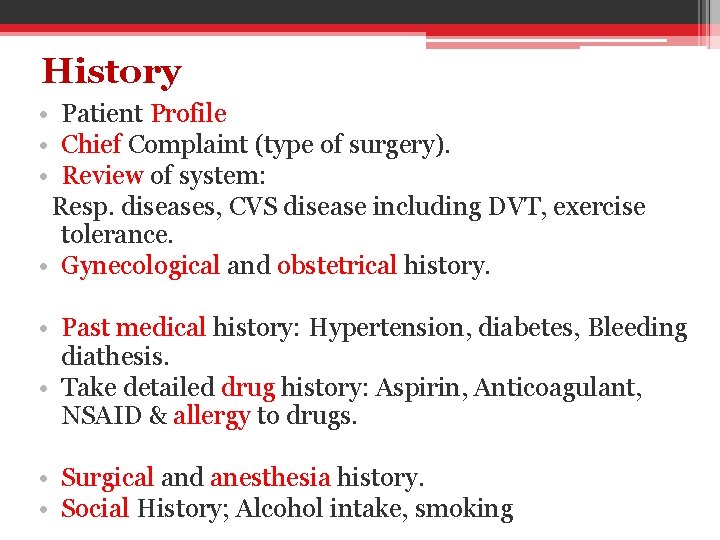
History • Patient Profile • Chief Complaint (type of surgery). • Review of system: Resp. diseases, CVS disease including DVT, exercise tolerance. • Gynecological and obstetrical history. • Past medical history: Hypertension, diabetes, Bleeding diathesis. • Take detailed drug history: Aspirin, Anticoagulant, NSAID & allergy to drugs. • Surgical and anesthesia history. • Social History; Alcohol intake, smoking
Physical Examination • Build on the information gathered during the history. -Pre-anesthesia physical examination : ( an assessment of the airway, lungs and heart, with documentation of vital signs) -Unexpected abnormal findings investigated before elective surgery.
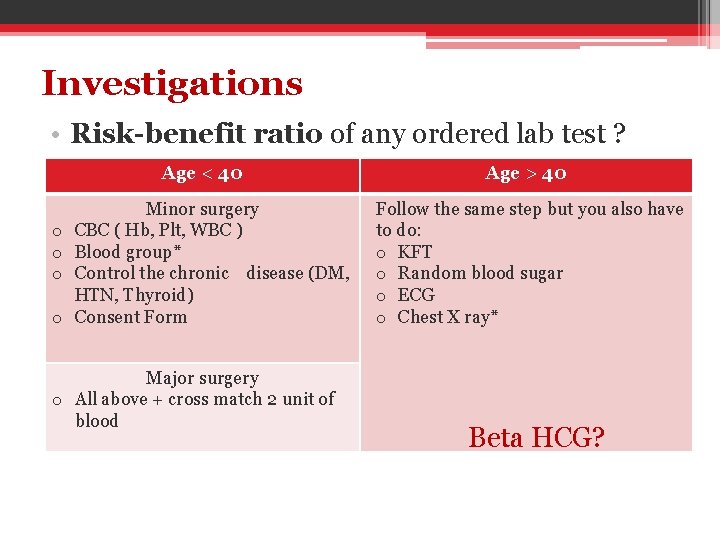
Investigations • Risk-benefit ratio of any ordered lab test ? Age < 40 o o Minor surgery CBC ( Hb, Plt, WBC ) Blood group* Control the chronic disease (DM, HTN, Thyroid) Consent Form Major surgery o All above + cross match 2 unit of blood Age > 40 Follow the same step but you also have to do: o KFT o Random blood sugar o ECG o Chest X ray* Beta HCG?
Drugs? When to stop before the operation! 1. Anti-platelet (Aspirin): 7 -10 days prior to surgery. 2. Oral contraceptive: 2 -3 month prior to surgery. 3. Anticoagulants: Warfarin: Stop the drug, Daily INR* until normal (target 1. 5), then give LMWH*: must be stopped 12 hrs prior to surgery
Preoperative Care Counseling is considered an important part of preoperative care… The PREPARED Checklist: • The procedure • The Reason or indication • Our Expectations • The preference that the patient may have • The Alternatives or options • The Risks and possible complication • The Expense • The Decision to perform or not to perform the procedure.
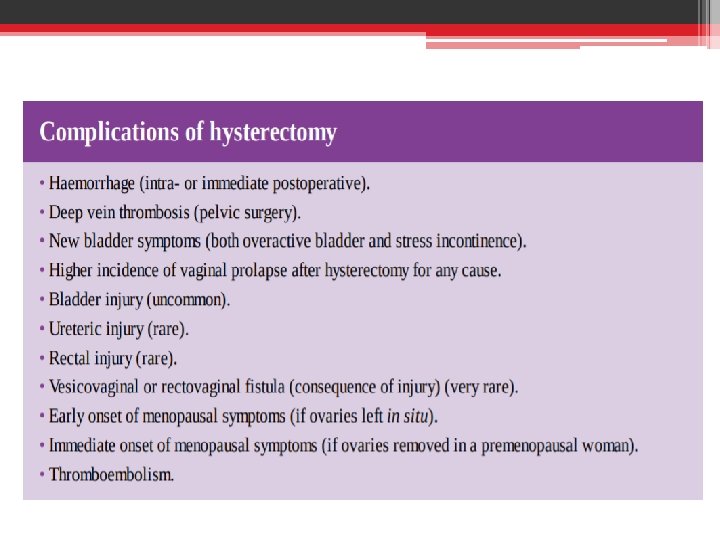
Intraoperative risks: Include: 1. Anesthetic complications. 2. Intra op. bleeding. 3. Unintended damage to organs or tissue.
Smile. . Take A Breath To Be Continued…
- Slides: 34