PRINCIPLES OF FRACTURE MANAGEMENT ESSIEN U NITMED TUTORIALS

- Slides: 63
PRINCIPLES OF FRACTURE MANAGEMENT ESSIEN, U © NITMED TUTORIALS
OUTLINE • INTRODUCTION • • DEFINATION STATEMENT OF SURGICAL IMPORTANCE CLASSIFICATION PATHOPHYSIOLOGY/CLINICAL FEATURES • PRINCIPLES • • • RESUSCITATION REDUCTION HOLD REDUCTON REHABILITATION COMPLICATION OF TREATMENT FUTURE TRENDS PECULIARTIES TO OUR ENVIRONMENT CONCLUSION REFERENCES
INTRODUCTION • A fracture is a break in the structural continuity of a living bone • Usually due to failure of skeleton to cope with the load put upon it. • The WHO declared the decade 2000 -2010 as bone and joint decade.
EPIDEMIOLOGY • Trauma is a common cause of fracture and it causes 140, 000 death/yr in US. • It is the leading cause of morbidity in people 134 years • Causes more years of lost productivity years than coronary artery disease, cancer and stroke combined.
• Incidence and severity is influenced by age, sex, co-morbidity, lifestyle and occupation. • Its incidence on Nigeria is about 1. 5 million per year
STATEMENT OF SURGICAL IMPORTANCE • The knowledge of fracture management has remained important in surgical practice • More so as its occurrence or complications affects greatly the productive life of individuals affected • It then becomes pertinent for the surgeon to arm himself with the principles of its management
CLASSIFICATION • Base on communication with external environment – Open – Closed
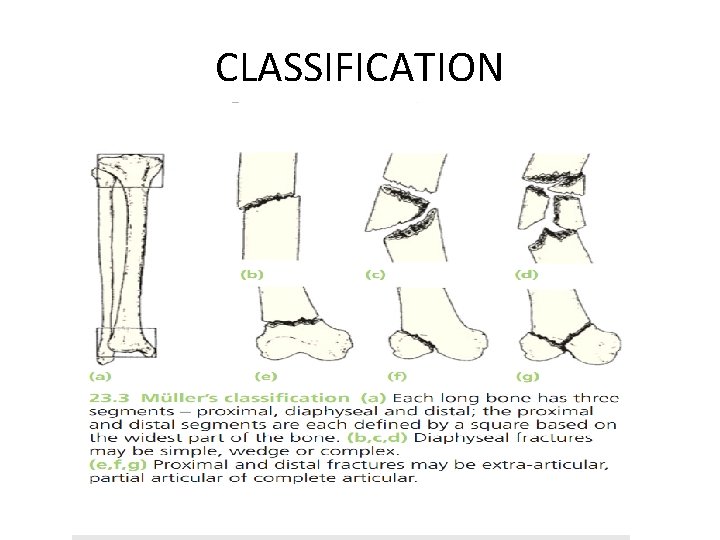
CLASSIFICATION • Universally, anatomically based system facilitates communication • An alphanumeric classification developed by Muller et al is widely acceptable
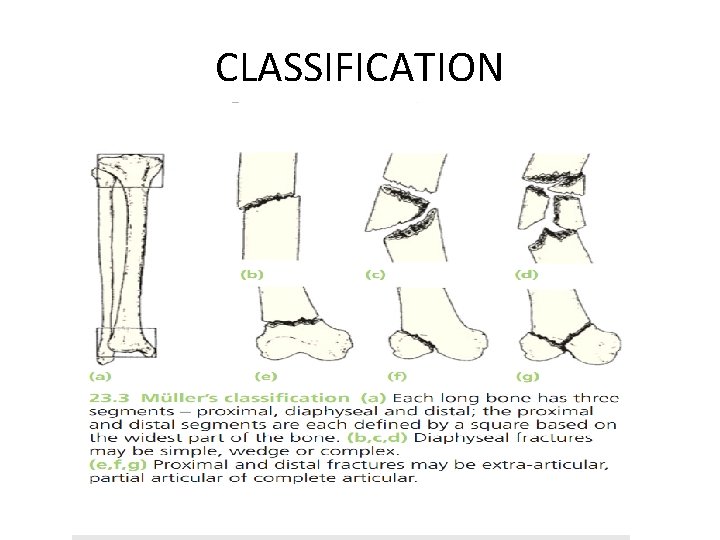
CLASSIFICATION
Classification- others • Fracture Line – Transverse – Oblique – Spiral • Linear Nature – Linear – Communited – Segmental
• Fracture Configuration – Avulsion – Transverse – Oblique/Spiral – Impacted/Compression – Communited – Greenstick – Displaced
AETIOLOGY • • Fractures could be due to - Traumatic events (direct/indirect force) - Repetitive stress - Diseased bone
PATHOPHYSIOLOGY • Following fracture , bone healing commences and this occurs either as indirect or direct
BONE HEALING • Indirect (Spontaneous) Healing – Tissue Destruction & Haematoma formation – Inflammation & Cellular proliferation – Callus formation-chondrogenic and Osteogenic cells – Consolidation – Remodelling • Direct (Primary) Healing – Contact healing
PATHOPHYSIOLOGY CONT’D • Granulation tissue is formed by 7 days to 2 weeks. • By the 3 rd week, callus begins to form. This is through cell differentiation to produce Osteoblasts and Chondroblasts in the granulation tissue. • This stage lasts between 4 – 16 weeks • Factors that affect healing include age, comorbidities, medications, nutrition etc.
Perkins fracture healing time table • For normal fracture healing – A spiral fracture in the upper limb unites in 3 weeks – Double it for consolidation – Double it again for the lower limbs – Double it again for transverse fracture • For children, its faster, fracture heals in 36 weeks
PRINCIPLES • • 4 Rs Resuscitation Reduction Hold reduction(immobilization) Rehabilitation
RESUSCITATION • An emergency approach • Follow the ATLS for the multiply injured patients, primary survey with simultanous resuscitation – – – Airway maintenance with restriction of cervical spine motion Breathing and ventilation Circulation with hemorrhage control Disability Exposure/environmental control
RESUSCITATION INITIAL TREATMENT CONTD • Adequate analgesia. • Antibiotics, Gram + cover, Aminoglycosides and anaerobic cover for open #. No need for antibiotics in close #
RESUSCITATION • Tetanus prophylaxis • Judicious use of antithrombotic agents when indicated
History -History of injury -Inability to use the injured limb -Patients age and mechanism of injury - Pain, bruising and swelling - Deformity in displaced fractures. - Associated injuries – numbness, loss of movement, haematuria, abnormal pains, difficulty with breathing, transient loss of consciousness etc.
- Hx of previous injuries - General medical Hx- Medical conditions that contraindicate surgery or anaesthesia e. g recent myocardial infarction
EXAMINATION-General • Examining for – Conscious, – pallor, – cyanosis – Dehydration
Local Signs • Examine the most obviously injured part • Look for; • swelling, bruises, deformity, intact skin? - Colour of skin • vascular and nerve damage, ligamentous and tendon ruptures. • associated injuries in distal parts. • Feel – Gently palpate the injured part
investigations • X-ray - Mandatory – Rule of two - Two views – AP & Lat. - Two joints - Two limbs - Two injuries - Two occasions Other Investigations – CT- not routine but useful in periarticular and pelvic#, MRI-spine, Radiosotope scanning
REDUCTION • It aims to achieve adequate apposition and normal alignment of bone fragments • The greater the contact surface area the more likely healing occurs • It should be done without undue delay as swelling of soft parts occurs in the first 12 hours making reduction difficult
REDUCTION • Its not necessary when • There is little or no displacement • When displacement does not matter initially • When its unlikely to succeed • There are two methods – Closed – Opened
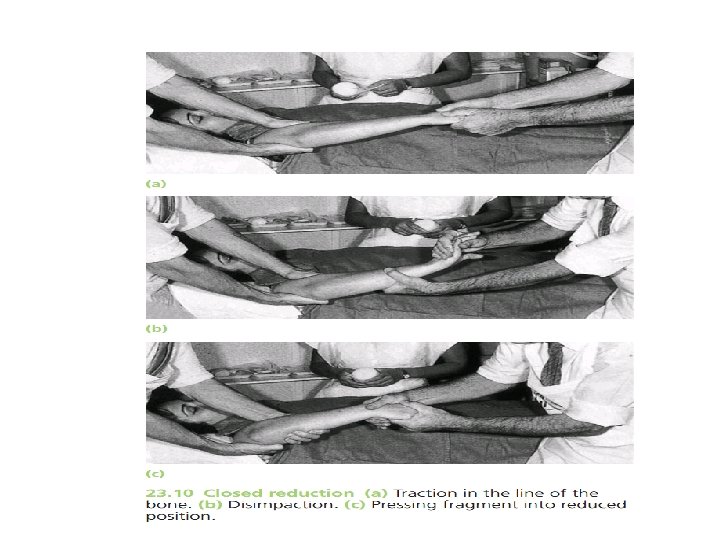
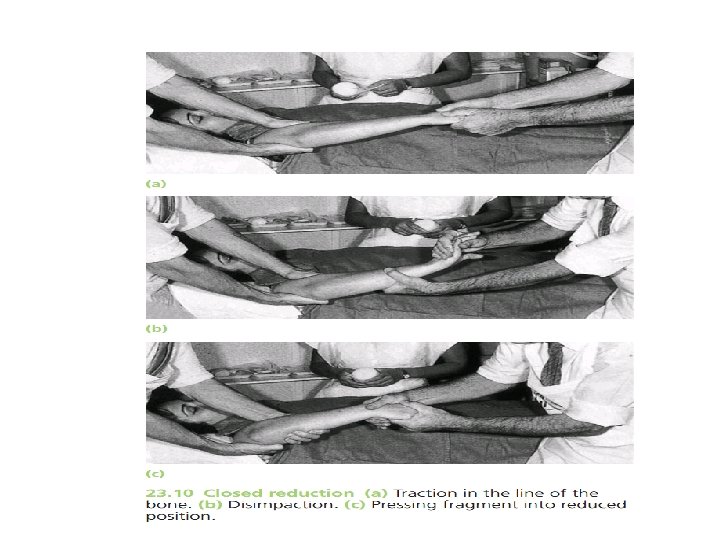
REDUCTION • Closed reduction • Under appropriate anesthesia and muscle relaxation • Reduced in a three-fold manoeuver – The distal part is pulled in the line of the bone – As the fragment disengage, they are reposited – Alignment is adjusted in each plane
REDUCTION • Open reduction • Its indicated when • Closed reduction fails, either because of difficulty in controlling the fragments or soft tissue interposing between them • There is a large articular fragment that needs accurate positioning • For traction(avulsion) fractures in which the fragments are held apart
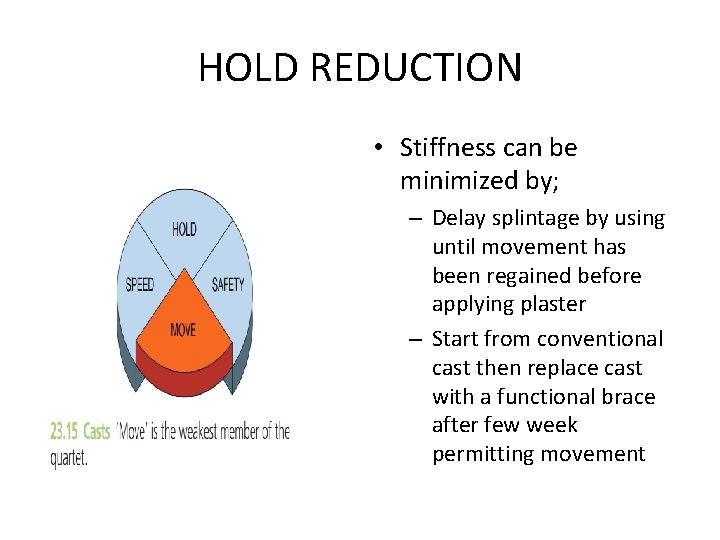
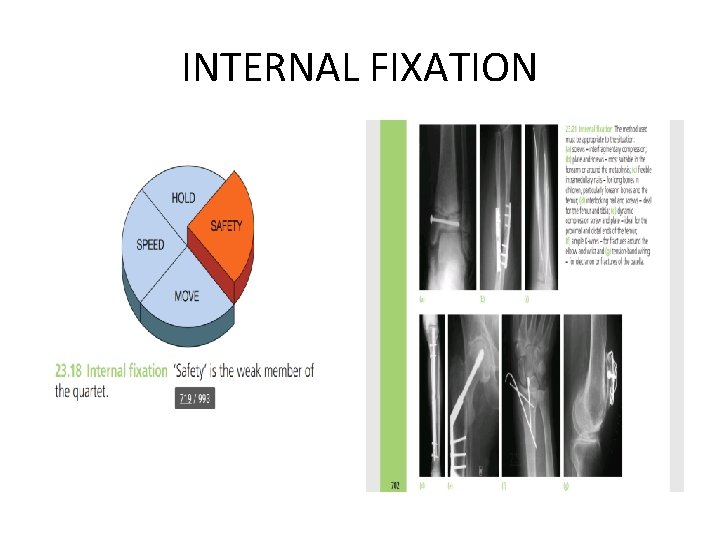
HOLD REDUCTION • Methods to Hold Reduction; • • • Continous traction Cast splintage Functonal bracing Internal fixation External fixation • These work based on the concept of the ‘fracture quartet’ principles consisting ; • Hold and move • Speed and safety
HOLD REDUCTION • Cast splintage • Splints - POP-made of Calcium sulphate hemihydrate, wood or metal, light – weight casting materials e. g. scotch cast or fibre glass
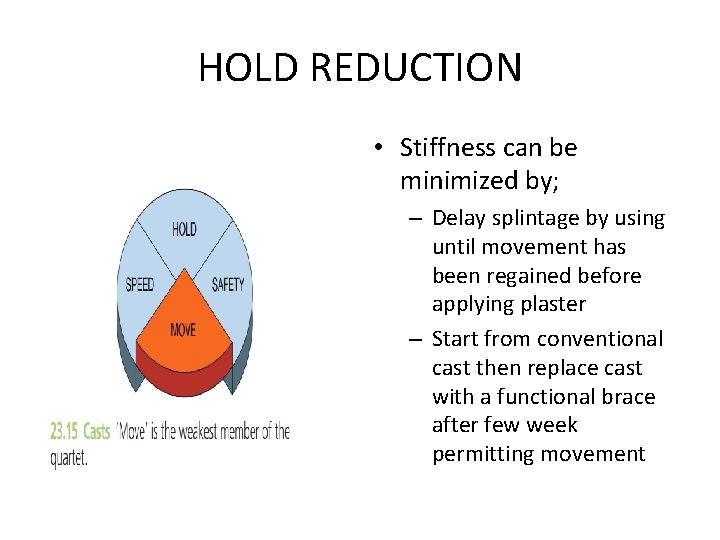
HOLD REDUCTION • Stiffness can be minimized by; – Delay splintage by using until movement has been regained before applying plaster – Start from conventional cast then replace cast with a functional brace after few week permitting movement

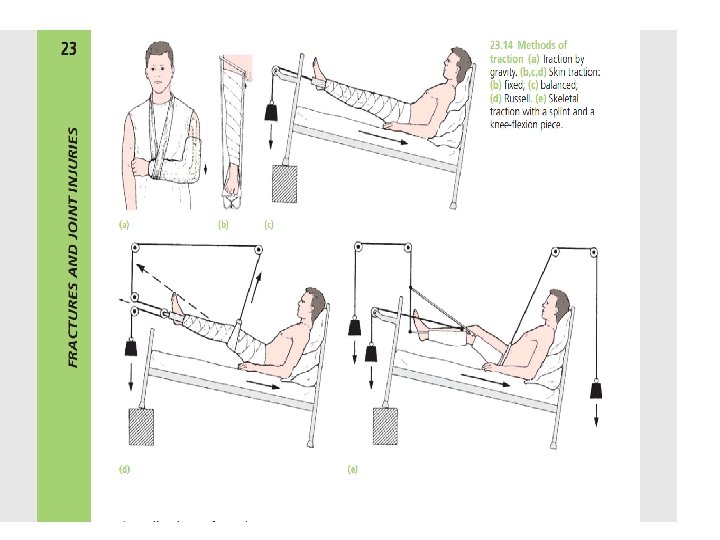
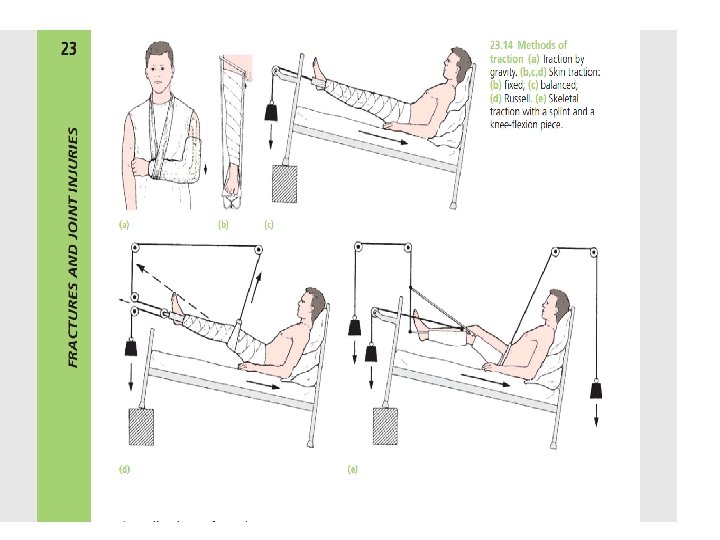
HOLD REDUCTION • 2) Traction • It can be achieved through; – Continuous traction • Traction by gravity • Skin traction • Skeletal traction – Fixed traction – Balanced traction – Combined traction
HOLD REDUCTION – Newton’s 2 nd law of motion states that “for every action, there is an equal and opposite reaction”. – Traction can not hold a fracture still, it can pull a long bone straight and hold it out to length but to maintain accurate reduction is difficult. – Thus speed is the weakest member of the quartet
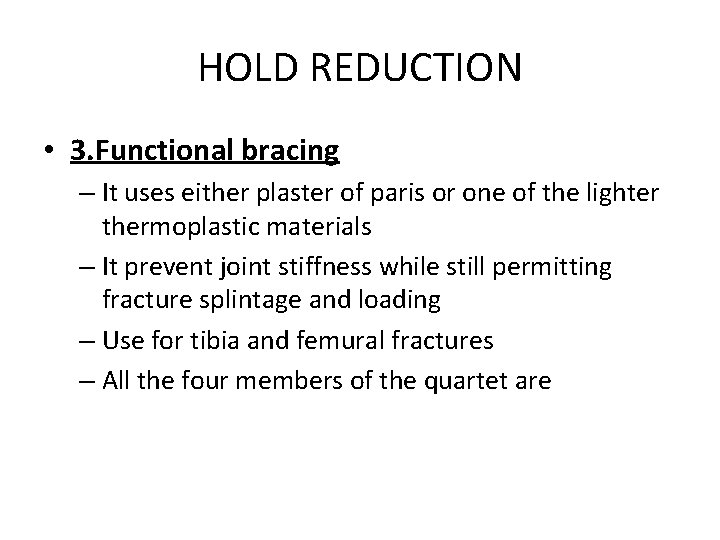
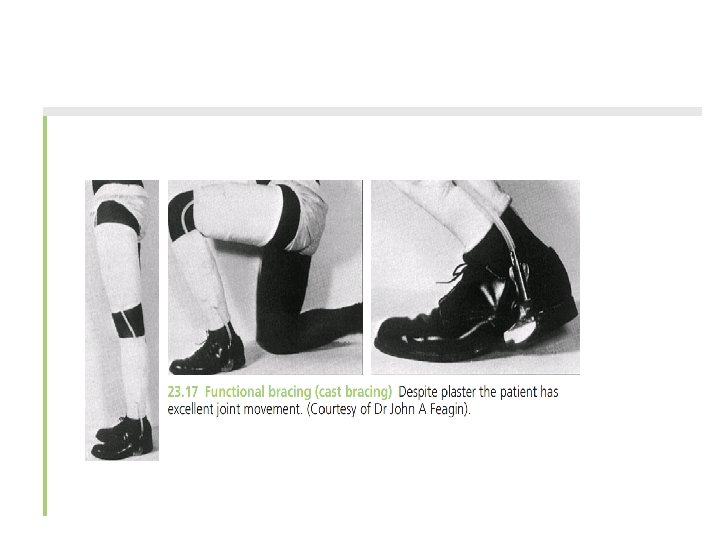
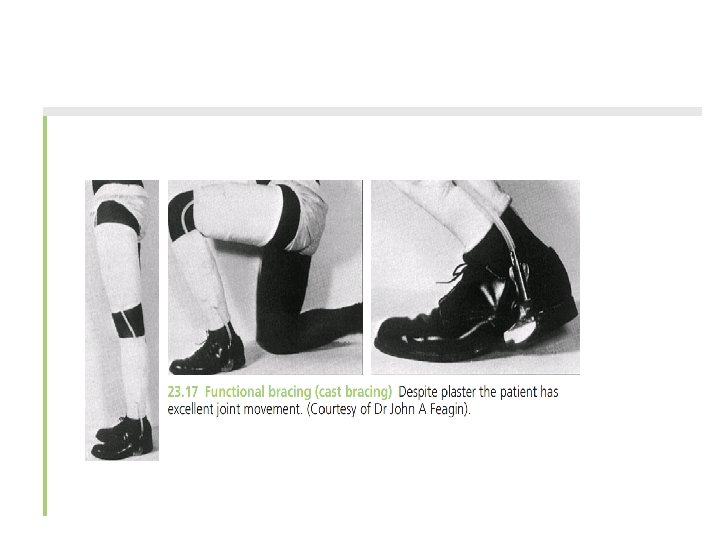
HOLD REDUCTION • 3. Functional bracing – It uses either plaster of paris or one of the lighter thermoplastic materials – It prevent joint stiffness while still permitting fracture splintage and loading – Use for tibia and femural fractures – All the four members of the quartet are
INTERNAL FIXATION - INDICATIONS FOR INTERNAL FIXATIONS Failure of closed reduction Failure of maintaining reduction – oblique/spiral fractures Pathological fractures Multiple fractures Fractures in elderly and paraplegic patients Delayed or nonunion – femoral neck fracture Associated arterial injury
INTERNAL FIXATION • The aim of open reduction is to bring the # ends together. • Once reduction is achieved, then it must be maintained • There are several ways of achieving this;
Type of internal fixation i. Interfragmentary screw ii. Wires.
INTERNAL FIXATION iii. Plates and screws – used in articular #. • There are five main plate designs ; a. Buttress b. Compression plates c. Protection plates. d. Tension band plate e. Bridge plates
INTERNAL FIXATION iv. Intramedullary nails –for long bones act as internal splints • May be rigid or flexible. • Reamed, Unreamed, locked or unlocked, dynamic or static.
INTERNAL FIXATION Complications – Infection, non-union, implant failure, refracture Adv. Early mobilization
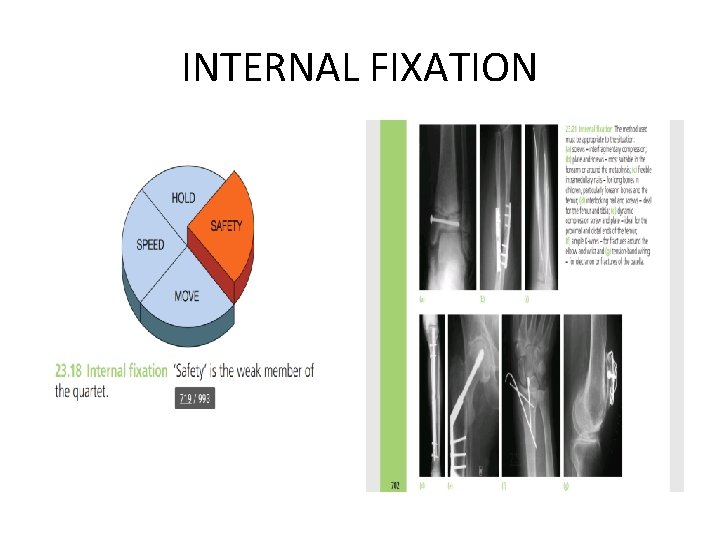
INTERNAL FIXATION
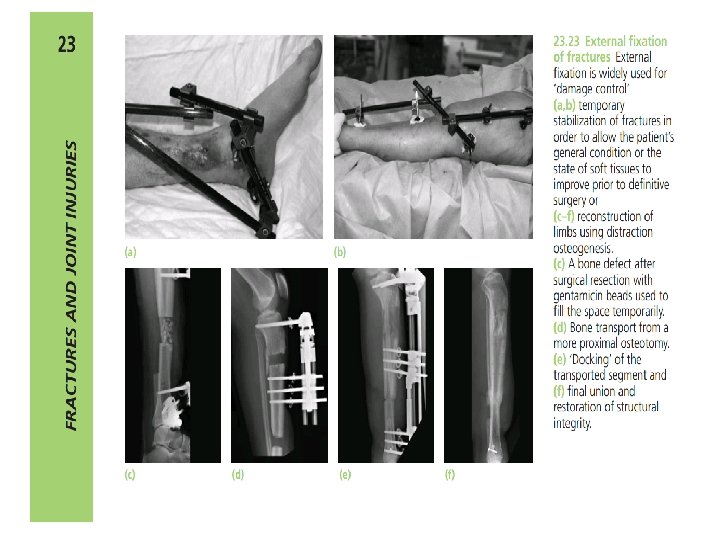
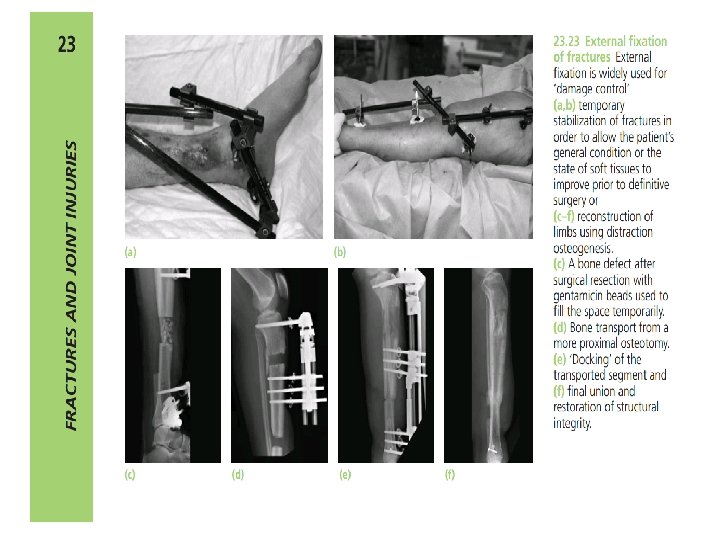
EXTERNAL FIXATION • Designed to provide # stabilization at a distance from the #. • Allows for tissue inspection while maintaining leg alignment.
Indications - Fractures associated with nerve or vessel damage - Fractures associated with severe tissue damage - Severe comminuted and unstable fractures - Fractures of pelvis - Infected fractures - Severe multiple injuries, head injury and burns - Comminuted and unstable fractures.
TREATMENT OF OPEN FRACTURES - An emergency - Initial management • • Appropriate Treatment at scene of accident. Wound covered before reaching hospital Rapid assessment in hospital Tetanus prophylaxis - Classify the injury – GA Classification.
• • Obtain inform consent Choice of anaesthesia C arm Portable radiography.
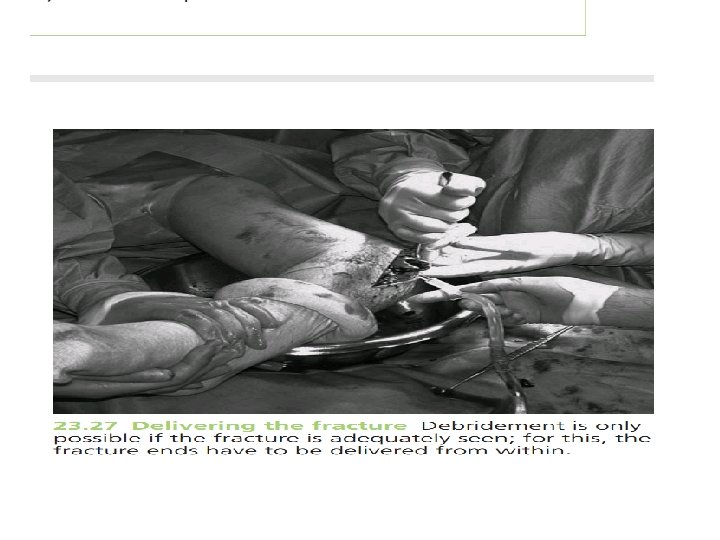
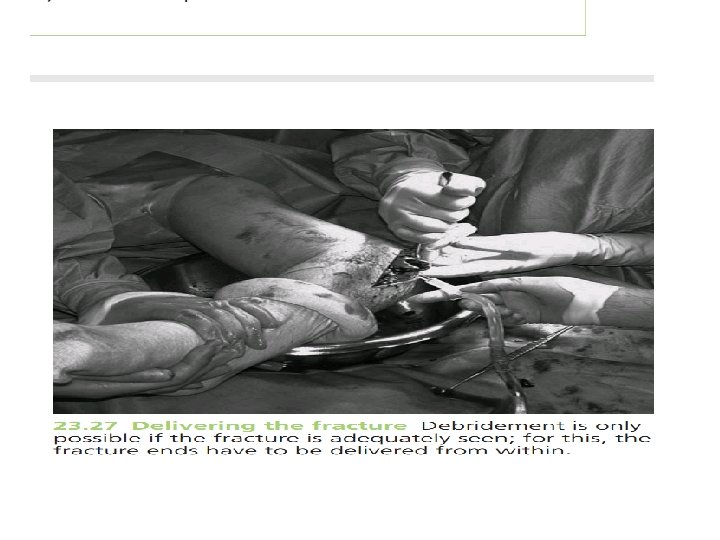
Principles of Treatment • Wound debridement • Antibiotic prophylaxis • Stabilization of the fracture • Early wound cover • Elevation of limb
REHABILITATION Aim to restore function to – Injured part Objectives - Prevention of oedema -Elevations, exercise -Preserve joint movement -Restore muscle power -Guide patient to normal activity • • OTHERS; Back to work Socially Occupational therapy
COMPLICATIONS COMPLICATION OF FRACTURES General Haemorrhage Shock Fat embolism Cardiorespiratory failure
Local – Early Local visceral injury Vascular injury Nerve injury Compartment Syndrome Haemathrosis Infection Gas gangrene Others: Fracture blisters, plaster sores and pressure sores
Late Complication Delayed union Malunion Non-union Avascular necrosis Muscle contracture Joint instability Osteoarthritis
FOLLOW UP • Careful use of knowledgeable, friendly rehabilitation specialists. • Early ROM • Monitor for and treat complications
Peculiarities to our environment • Influence of TBS • Logistics
THE FUTURE • Use of biologic agents – Autologous and cadaveric bone grafts to fill gaps. • Organic and synthetic agents like hydroxy apatite. • Peptide signalling molecules like bone morphogenic proteins, TGFB, PDGF, Gene family fibroblast growth factor.
CONCLUSION • Fracture management will remain an important and challenging aspect of the surgeons practice in our environment • Its important therefore to acquaint with the principles of its management to improve outcome and productivity
REFERENCES • Apley’s system of orthopaedics and fracture 9 th edition 2010 pg 687 -710 • Essential orthopaedics 3 rd edition 2004 pg 20 -41 • Internet-consult a doctor, college of medicine, university of ibadan • ATLS 10 th edition student course manual 2018 pg 713 • Previous powerpoint presentation
• THANK YOU FOR LISTENING