PRINCIPLES OF FLUID THERAPY PREPARED BY DR PANCHAJANI
PRINCIPLES OF FLUID THERAPY PREPARED BY DR. PANCHAJANI. R

FLUID THERAPY • Can be life saving in certain conditions • Loss of body water whether acute or chronic can cause a range of problems from mild headache to convulsions, coma & in some cases death. • Though fluid therapy can be a life saver , its never always safe, & can be very harmful. •

FLUID THERAPY Points noted before are, . • Pt. really need fluids( indications) • Which fluid is most suitable( depends on fluid balance, acid base, electrolyte balance) • How much fluid is needed • At what rate • Which route is to be used(IV, IM, subcutaneous etc. ) • Likely complications and contraindications.

Fluid therapy – Indications • For rapid restoration of fluid & electrolytes in dehydration( vomiting, diarrhoea, shock, Hge, sepsis, burns) • Total parenteral nutrition • Anaphylaxis, cardiac arrest, hypoxia. • Post GIT surgeries • For maintenance, replacement of loss or as a special fluid.

Fluid therapy- Amount Calculated roughly by, • History of the nature & quantity of fluid loss • Appearance & examination of the patient • Exam-; thirst, dryness of mucousa, loss of skin turgor, orthostatic hypotension, tacchycardia, decreased urine output, reduced JVP. • If large quantity of fluid is necessary monitoring of CVP, Pulmonary wedge pressure, urine output to determine the rate & volume of infusion.
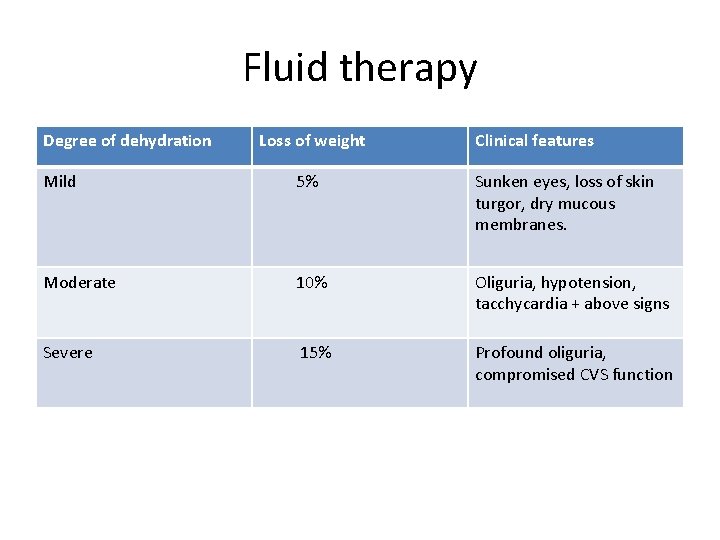
Fluid therapy Degree of dehydration Loss of weight Clinical features Mild 5% Sunken eyes, loss of skin turgor, dry mucous membranes. Moderate 10% Oliguria, hypotension, tacchycardia + above signs Severe 15% Profound oliguria, compromised CVS function

Fluid therapy- amount • Replacement commenced by giving isotonic saline solution IV & maintained by dextrose saline solution. • In extreme dehydration is maintained by Dextran or Plasma infusion followed by isotonic saline solution or dextrose saline solution. • In infants with dehydration the amount of fluid required will be approximately same as that of wt. loss , ie, difference between the estimated & actual wt. ( 1 gm- 1 ml)
Fluid therapy- Route of administration • In health- by enteral route. • For rapid correction of hypovolaemia or electrolyte abnormalities- IV route • Parenteral fluid therapy- administration of fluid by any route other than the alimentary canal.

IV Fluid therapy- Rate of flow • Rate of infusion is controlled by adjusting the number of drops/ minute. • 16 drops = 1 ml • At a rate of 30 drops/ minute 1 litre will be given in 8 hrs. • 45 drops/ m will take 6 hrs • 60 drops/m will take 4 hrs. • Microdrip set 1 ml= 60 drops

IV Fluid therapy – rate of flow • In severely dehydrated pts. rate of flow of 1 st hour can be accelerated to over 100 d/m after that it cut to 50 or 60 drops. • Maintenance dose is 30 drops/m(3 liters in 24 hrs) Calculations • 1. To multiply the number of litres of required fluid to be given in 24 hrs by 11 or 10. this provides the number of drops/ m. • 2. volume of fluid in ml to be infused in 1 hr divided by 4 = number of drops/ minute • Special care is needed in extreemes of age and in pts. with overloaded circulation. • IV Potassium is administered slowly and with extra care. • Rate to be used should be written down in the treatment card.

IV Fluid therapy- Site of administration • The vein on the forearm or back of hand is choosen (vein around the wrist) • A visible or palpable vein may not be found in the arm another site used. • External jugular vein, internal jugular vein, subclavian vein or cephalic vein can be selected. • Because of the risk of pulmonary embolism or thromboplebitis vein of the leg ( long saphenous vein) should not be selected.

IV Fluid therapy- site • Suitable vein may be made prominent by the application of light torniquiet • It can be entered by a hollow needle. • vein of the forearm is immobilized with a few strips of adhesive plaster. • Limb is immobilized by placing it on a light splint
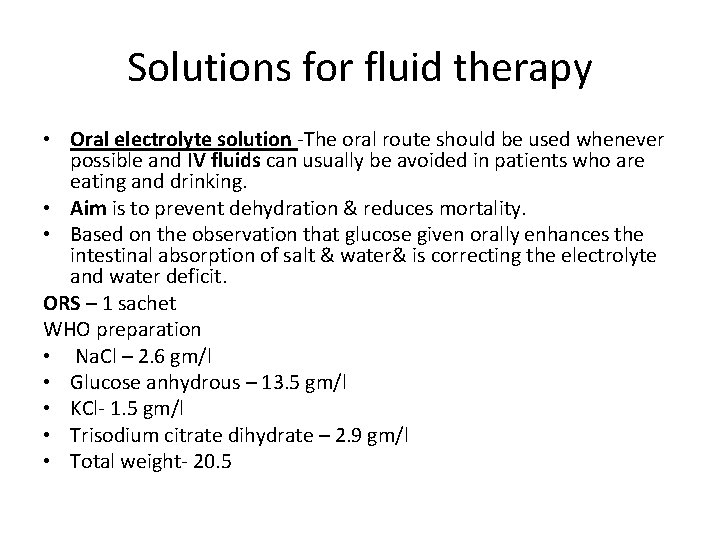
Solutions for fluid therapy • Oral electrolyte solution -The oral route should be used whenever possible and IV fluids can usually be avoided in patients who are eating and drinking. • Aim is to prevent dehydration & reduces mortality. • Based on the observation that glucose given orally enhances the intestinal absorption of salt & water& is correcting the electrolyte and water deficit. ORS – 1 sachet WHO preparation • Na. Cl – 2. 6 gm/l • Glucose anhydrous – 13. 5 gm/l • KCl- 1. 5 gm/l • Trisodium citrate dihydrate – 2. 9 gm/l • Total weight- 20. 5

Fluid – ORS • 1 sachet dissolved in 1 litre of water give 90 mmol/L of Na, 20 mmol/L of K, 80 mmol/L of Cl, 9. 9 mmol/ L of citrate & 11. 1 mmol/L of dextrose. • This solution is isotonic & a rich source of Na, K, Cl and dextrose. • At first ORS is sodium bicarbonate based. • inclusion of tri sodium citrate in place of sodium bicarbonate made the product more stable, results in less stool output in high output diarrhoea. • Direct effect of trisodium citrate increases the intestinal absorption of sodium & water.
IV Infusion – Procedure Intravenous therapy (IV) is a therapy that delivers liquid substances directly into a vein. The intravenous route of administration can be used for injections or infusions. Intravenous infusions are commonly referred to as drips. Requisites; • IV fluid • IV infusion set • Scalp vein (butterfly needle or IV canula) • Needle – size – number increases size decreases. Smallest – 28 ( introduce even the veins of scalp) , normal -23 size • Plaster , glouse, IV stand, antiseptic solution, torniquet

IV infusion – Procedure Select a vein – • Use distal veins of arms • Use non dominant limb • Avoid areas of flexion • Avoid highly visible veins & phlebitis veins.
IV infusion - Procedure Select the site-vein become prominent by, • Vein to be dilated by place the extremity in a dependant position • Select the site by applying a torniquet 15 -20 cm above the venepuncture site. • Massage to the site(from away from the site) • Clench & unclench the fist • Tap lightly over the vein or warmth application, or entire limb in warm water. • Vein finding device is available by using laser. Vein can be seen clearly by violet colour. • Last procedure is venesection.
IV infusion – Procedure Venepuncture • Clean the site with artery forceps by a cotton swab soaked in antiseptic solution & clean from centre to periphery. After cleaning should not be wiped out. Introduce needle Venepuncture is done at an angle of 30 degree in such a way that the cut edge upwards, as soon as enters the vein blood appears, advance a little more and reduce the angle at 15 degree or parallel to the skin , advance it to about. 5 - 2 cm. Remove the needle and canula left.
IV infusion – Procedure • Torniquet remove and remove the side cap and insert IV set & cap is introduced in to the upper lid by opening the cap. • Regulator (roller clamp)move downward , close the tube • Upper part of the tube a dilated part to collect the solution (dip chamber- fill half) • If air is present in the tube it is removed by slowly allowing to throw out some solution by pressing out the bubble by dragging down the tube( air embolism occurs)

IV fluids- Procedure • IV stand – 3 feet above the pt. Note the, • Sediments • Turbidity • Change of colour • Straighten tube • Dip chamber • Roller clamp • Solution must be sterile , free from bacteria & other toxins. Removal- swab soak in antiseptic solution, withdraw needle along the vein • After withdrawing examine the canula ( all out) because of the possibility of breakage.
IV FLUIDS – Types The Fluid used in clinical practice are classified in to colloids, crystalloids & blood products. Types ; • Colloids – Are of large molecules which shift fluid from interstitial compartments to intravascular compartments and are used as plasma expanders. • Too costly • Difficult to store • Never used as first solution • Albumin, steroids Eg. Haemoccel, hetastarch, penta starch, dextran 40/70

IV FLUIDS - types Crystalloids – pass through a semipermeable membranes which is not in colloids. Contain electrolytes, Move across capillary membranes. eg. NS, DNS, 5% Dextrose, Ringer lactate( RL), Isolyte G, Isolyte M.
IV fluids- CRYSTALLOIDS • Isotonic – same tonicity as another solution compared. ( Plasma/ ECF) • Hypotonic- Low • Hypertonic - high Half life - the period in which the radioactivity or number of radioactive substance decreases by half. Osmolality – assessed by the amount of solute dissolved in a solvent Normal plasma osmolality is 285 mosmol/kg Normal plasma osmotic pressure – 25 mmof Hg.
IV fluids – Crystalloids Tonicity -A solutions’ salt balance compared to plasma. . Around 300 m. Osm/L § Isotonic • - Nearly the same as serum. - for ECF deficit NS: 0. 9% Sodium Chloride, RL Generally, initial fluid replacement should not exceed three liters before blood is infused Balanced salt solutions 3 ml of isotonic crystalloid are needed to replace 1 ml of blood
IV FLUIDS- CRYSTALLOIDS § Hypotonic - for cellular dehydration. Less osmolarity than serum – Dilutes serum • 0. 45% Na. Cl, D 5 NS. 45 (5% Dextrose in ½ normal saline) • Water is pulled from vascular compartment into interstitial fluid compartment, then into adjacent cells • Helpful when cells are dehydrated – Dialysis pt on diuretics – Hyperglycemia - DKA • Can be dangerous – sudden fluid shift can cause cardiovascular collapse
IV fluids – Crystalloids Hypertonic - maintain circulatory volume, • Higher osmolarity • Pulls F&E from intracellular and interstitial compartments into intravascular compartment. • Can help stabilize BP, • increase urine output, • reduce edema • Rarely used in prehospital setting. • Dangerous if cell dehydration exists • D-5%-W in Lactated Ringers, 10% NS • Example: Albumin

IV FLUIDS- CRYSTALLOIDS • Isotonic no movement initially • Hypertonic attracts water • Hypotonic gives up water
IV FLUIDS Special Purpose fluids – • sodium bicarbonate fluids 7. 5 % & 8. 5% - Used in metabolic acidosis, forced diuresis, hyperkalaemia • Manitol 10/20% - osmotic diuretic agent • Hypertonic saline 1. 6%, 3%, 5%, 7. 5% - hyponatreamia. • Albumin 4. 5% - plasma expander • Albumin 20% - hypoalbuminaemia
IV fluids Normal concentrations - • In Plasma – Na- 140 meq/L, Cl- 100 m. Eq/ L, K- 5 m. Eq/L, HCo 3 - 24 m. Eq/L. • In ECF- Na- 142 m. Eq/L, Cl- 103 m. Eq/L, K- 4 m. Eq/L , HCo 3 – 27 m. Eq/L, Ca- 5 m. Eq/L • Daily requirement – Na- 100 m. Eq, K- 60 m. Eq, Ca- 5 m. Eq, Mg- 1 m. Eq

IV FLUIDS - CRYSTALLOIDS Normal saline or Na. Cl (0. 9%) • Contains Na & Cl in the same concentration almost similar to plasma. • Provides 150 mmol of Na & 150 mmol of Cl/ L • Isotonic/Iso osmolar with plasma & ECF • Good replacement solution for ECF volume deficit in presence of hyponatraemia. • Solution for replacing G. I. T fluid loss. • Should not be used in first 24 hrs after operation due to normal Na conservation(ADH, aldosterone) • Because of increased chloride content higher than that of plasma infusion of too much of NS produce hyperchloraemic acidosis.
IV fluids- crystalloids Dextrose 5% &10% in H 2 O – D 5, D 10 5%- 50 gm of dextrose/ L(5 gm/100 ml) 10%- 100 gm/L(10 gm/100 ml)
IV Fluids – Crystalloids Dextrose 5%; • Slightly hypotonic to plasma • Supplies calories with out any electrolytes • After infusion dextrose is metabolised & water is left in the ECF. • Too much infusion causes dilution &hypotonicity of ECF • Indicated when pt. not require any electrolyte but restore blood volume. • Used in immediate post-operative period (Na excretion diminished) • Prolonged administration will result in hyponatremia & may cause thrombosis of veins. • Should not be used in the treatment of shock( hypotonic soln- poor volume expanders)
IV Fluids – Crystalloids Dextrose with normal saline – DNS – 5% dextrose with 0. 9% saline – solutions having greater osmotic pressure. Indications- vomiting, diarrhoea, diabetic ketoacidosis, renal salt wasting diseases, paralytic illeus, salt lossing bowel disease, ascitis.

IV Fluids – Crystalloids Ringer lactate solution – • Contains Na, K, Cl in the same concentration in plasma & also contain Ca& lactate. • Contains Na- 130 mmol/L, K- 4 mmol/L, Ca – 3 mmol/L, HCo 3 - 28 m. Eq/L, Cl - 109 mmol/L. Lactate ions-28 mmol/ L. • Almost similar electrolyte concentration as ECF & PH remains normal even if infused in large quantities. • Slightly hypotonic to plasma. Indications- hypovolaemic shock, GITfluid loss, excessive drainage of intestinal secretions. • No glucose so used in diabetic pts. • Should not be given in pts. with liver disease & in presence of lactic acidosis ( lactate ion is converted in to bicarbonate in liver & correcting metabolic acidosis& a part of lactate is converted in to glucose in liver. These reactions are supressed in pts with liver disease & lactate accumulate in blood)
IV Fluids – Crystalloids Ringer acetate solution • Na- 130 mmol/L, K- 4 mmol/L, Ca- 3 mmol/L, Cl- 109 mmol, acetate- 28 mmol/L • Osmolality- 270 mmol/L • Indications- GIT & ECFdeficit in pts with liver disease & lactic acidosis. • Acetate ion is oxidized to HCo 3 in muscles with minimal O 2 & correct metabolic acidosis.
IV Fluids – Crystalloids Darrow’s solution – • Only solution contain more K than in plasma& ECF. • K-36 m. Eq/L, Na- 124 meq/L, Cl- 104 m. Eq/L, Lactate- 56 meq/L • Indications- Hypokalaemia, GIT fluid loss with K loss. • Supplies K at a safe rate • Rate of infusion should be slower than other solution to avoid hyperkalaemic state which is more dangerous • Should not be given more than 60 drops.
IV Fluids – Crystalloids • Hypertonic saline solution – (1. 6%, 3%, 5%, 7. 5%) • Provides 274 mmol/L of Na, 274 mmol/L of Cl. • Osmolality- 574 mmol/L. Indications- hyponatremia, in pts with anuria or oliguria who can’t given much water volume. • Supply required Na ions with less water. • Resuscitation of pts. with trauma & haemorrhage. • Shown that even with 50 % blood loss a small volume of 7. 2 -7. 5 % Na. Cl ( 4 ml/Kg of body wt. ) restores cardiac output & BP with in 1 minute. • Hypertonic solution is given through a peripheral vein very fast over 2 -5 minutes. This results in a marked rise in plasma Na level & plasma osmolality causing a shift of body water in to the vascular tree.
IV Fluids – Crystalloids Hypertonic saline solution resuscitation benefits • Immediate rise in systolic pressure & cardiac output. • Increase in nutritional blood flow through micro circulation reducing post ischaemic reperfusion injury. • Decreased incidence of multi organ failure. • Improved survival.
IV Fluids – Crystalloids Maintainance fluid replacement solution( M-soln)- Na- 40 mmol/L, K- 35 mmol/L, Cl- 40 mmol/L , HPo 4 - 15 meq/L, Acetate- 20 meq/L. • Correction of hypokalaemia & metabolic acidosis. ECF replacements- E Solution- Na- 140 mmol/L, k- 10 mmol/L, Ca- 5 meq/L, Mg- 3 meq/L, Cl- 103 meq/L, Acetate- 47 meq/L, Citrate- 8 meq/L. • Correction of ECF deficit, metabolic acidosis.

IV Fluids – Crystalloids Gastric acid replacement solution- (G soln) • Solution containing ammonium chloride • Used to correct metabolic alkalosis. • Not recomented for most cases of metabolic alkalosis with damaged liver. Pediatric fluid replacement solution ( P soln)

IV Fluids – Colloids Human plasma - • Most common colloid soln. • used for restoration of shock patients& for maintainence of I. V. fluid therapy. • easily available in many blood banks • Composition & osmolality similar to ECF • Advantage- risk of transmitting hepatitis &AIDS is minimized if proper screening of blood donors is done.

IV Fluids – Colloids Human Albumin – • Plasma substitute derived from plasma. • Provides 2. 3 mmol/L of K ions & 140 mmol/L of Na. • Rarely an anaphylactic reaction occurs. • Purified human albumin solution 20% is available, it is costly.
IV Fluids – Colloids Synthetic plasma expanders - Gelatin & dextran based solutions Gelatin soln • 3. 5% Soln of degraded gelatin polypeptide called polygeline. • Contains electrolytes in a same concentration very similar to plasma • Its average shelf life is 4 hrs. • Commonest plasma expander used in clinical practice. • cheap & easily available • Doesn’t cause any bleeding problem or organ dysfunction even in large quantities. • Its volume expansion capacity is 50% of the volume of polygeline soln & its effects starts immediately. • Side effects- urticaria, rigor, bronchospasm, hypotension
IV Fluids – Colloids Dextrans – Branched sucrose polysaccharides. Dextran 40 – • Molecular wt. 40000 • Contains 10% soln of dextran 40 with 5% dextrose. • Hypotonic to plasma. • Half life is about 2 -4 hrs • 90% get excreted in urine in 12 hrs. • It decreases blood viscosity & helps in improving circulation through microvasculature. • Useful in improving blood flow in an acutely ischaemic limb where arterial surgery or embolectomy is not possible. • For this purpose about 1 litre of dextran 40 with 500 ml of dextran 70 is slowly infused over 24 hrs for 2 -3 days. •
IV Fluids – Colloids Dextran 70 • Molecular weight- 70, 000 • Isotonic with plasma • Half life is 24 hrs • side effects of dextrans- anaphylaxis, renal failure, bleeding tendency due to platelet dysfunction. •
Assessment for maintaining correct fluid balance • Fluid intake & output chart • Clinical signs • Blood indices – serum elecrolyte estimation , Hb, haematocrit, plasma proteins, serum urea, Na, K, Cl. • Weight- daily weighing • Blood volume estimation • Monitoring of pulse, BP, CVP, • In critically ill patients fluid should be prescribed for 4 -6 hrs & then pt. is re-assessed.

IV fluids Contraindications • Failing heart • Pulmonary congestion Complications • Fluid overload • Pulmonary oedema • Cardiac failure • Infection • Air embolism • Bacteraemia • Thromboplebitis • Haematoma • Cellulitis in local area • Pyrogenic infections
Post operative fluid therapy Physiological effects – raise the ADH& Aldosterone activity • Renal retention of sodium & water • Increased loss of urinary K • Cellular K comes out in to ECF. First 24 hrs • Dextrose 5%- 1. 5 -2 L & NS (0. 9%) -500 ml in 24 hrs. After 24 hrs • Replace the fluid loss in last 24 hrs plus insensible loss of about 1 L. • K need not be added for the first 3 -4 days unless serum K level is low • Recommented regimen- RL- 1 L , DNS- 1 L • On day 3 onwards- 600 mmol of K/ day in the form of KCl in bottles of Dextrose or DNS
REFERENCE • • • Bailey and Love’s short practice of Surgery Manipal manual of Surgery SRB’s Manual of surgery Text book of Surgery- ASI Clinical Surgery, Das
Thank you, Dr. Panchajani. R Associate professor, Dept. of Surgery, SKHMC
- Slides: 50