Principles of external fixation AO Trauma Basic Principles
Principles of external fixation AO Trauma Basic Principles Course
Learning objectives • Describe the types of external fixators • Describe the indications for external fixation • Explain the “spectrum of stability” that can be achieved • Describe how to determine the stability of the frame by the method of construction • Describe how a modular frame is constructed and used to reduce and stabilize a fracture • Explain how to place anatomically safe and stable pins in the tibia
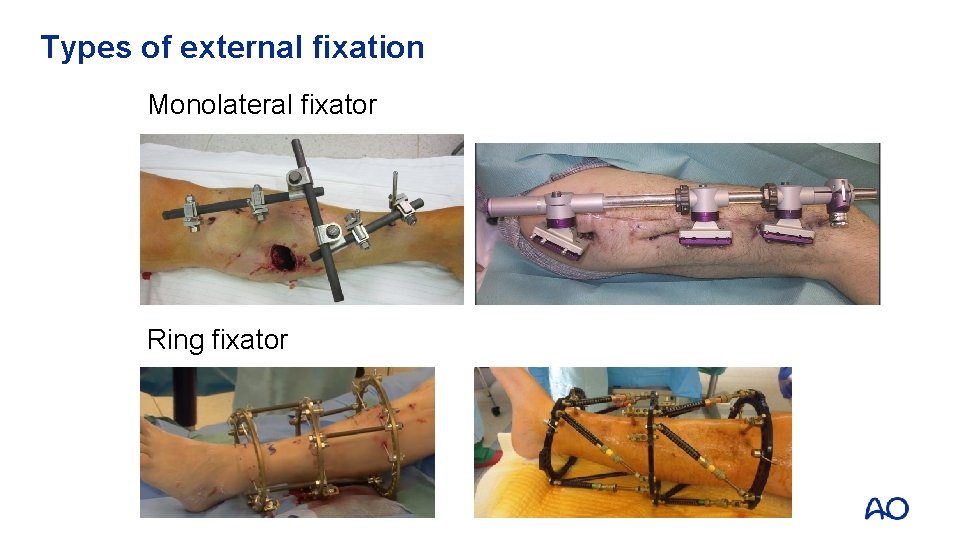
Types of external fixation Monolateral fixator Ring fixator
Advantages of external fixation • Minimally invasive—protects the local biology • Damage control—can be quick to apply • “Easy” • Anywhere, any time, by anyone • Wide range of indications • Very successful outcome for management of fractures and soft-tissue handling • Good results if done properly
Disadvantages of external fixation • Risk of pin infection • No or minimal experience with method • Equipment unavailable • Uncomfortable for the patient • Managing the patient in an external fixator can be challenging
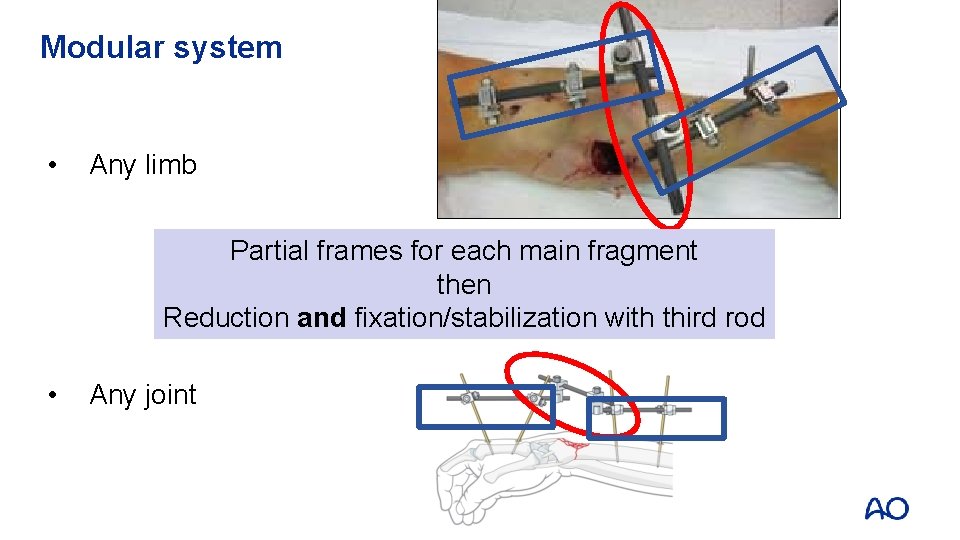
Modular system • Any limb Partial frames for each main fragment then Reduction and fixation/stabilization with third rod • Any joint
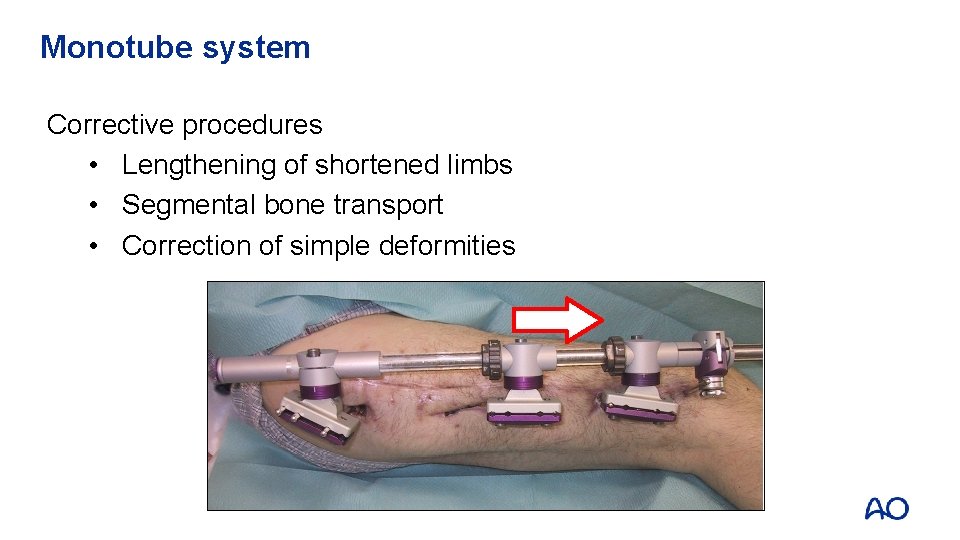
Monotube system Corrective procedures • Lengthening of shortened limbs • Segmental bone transport • Correction of simple deformities
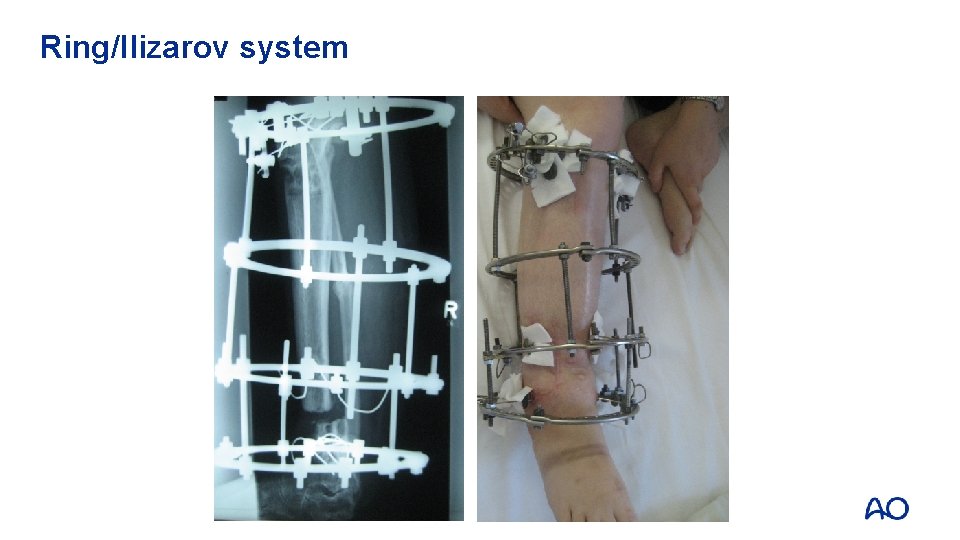
Ring/Ilizarov system
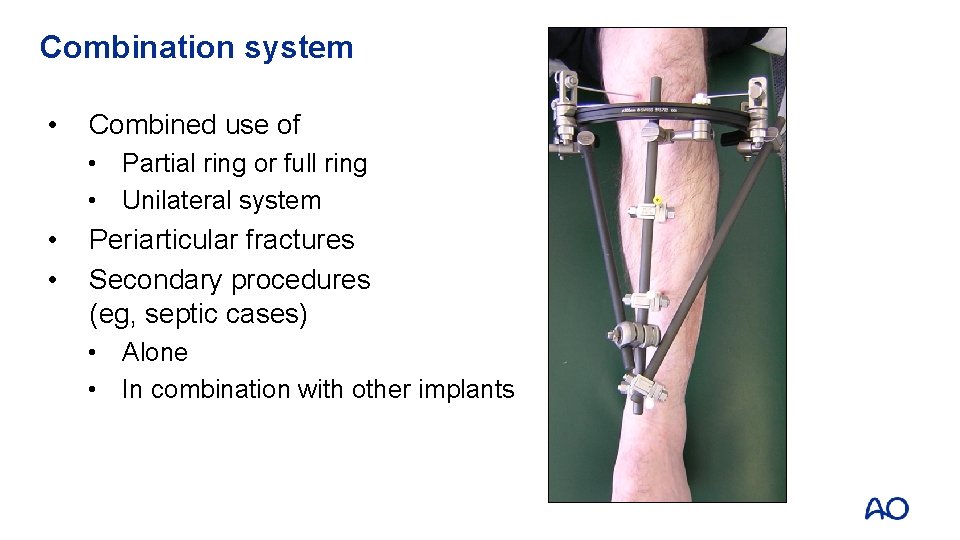
Combination system • Combined use of • Partial ring or full ring • Unilateral system • • Periarticular fractures Secondary procedures (eg, septic cases) • Alone • In combination with other implants
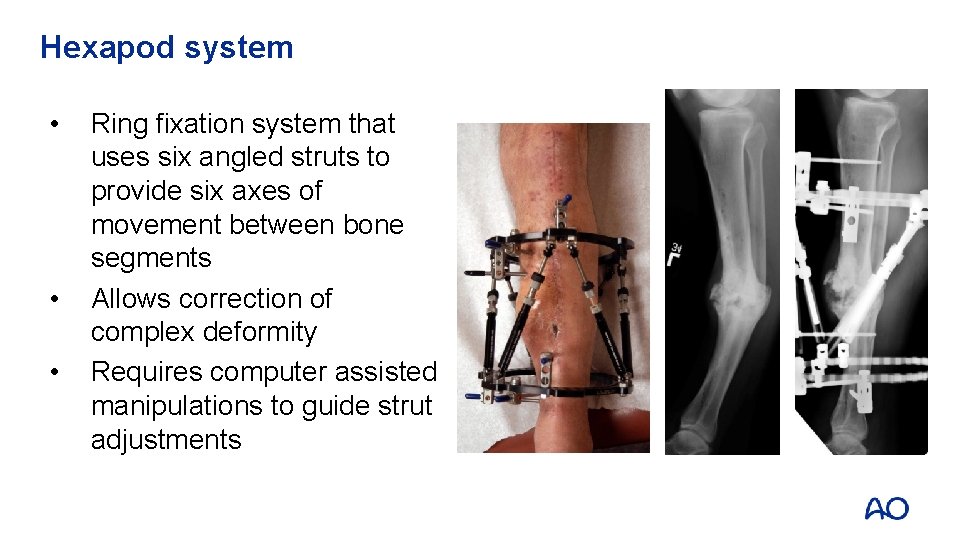
Hexapod system • • • Ring fixation system that uses six angled struts to provide six axes of movement between bone segments Allows correction of complex deformity Requires computer assisted manipulations to guide strut adjustments
Indications for external fixation • • • Fractures with soft-tissue damage Polytrauma—damage control surgery Skeletal infection Corrective surgery (deformity or nonunion) Definitive fracture care (pediatric and adult patients)

Indications for external fixation Fractures with soft-tissue damage Closed fractures with soft-tissue compromise Open fractures with soft-tissue wound
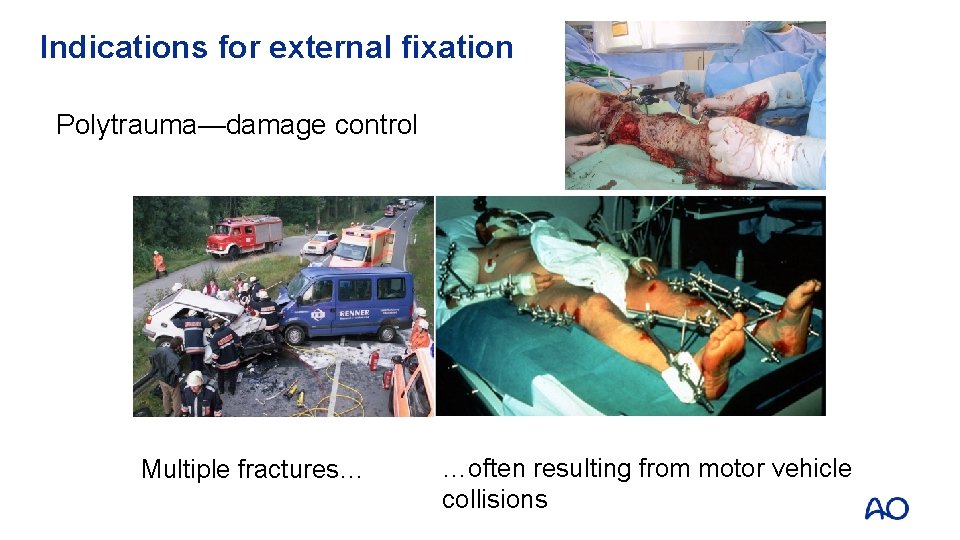
Indications for external fixation Polytrauma—damage control Multiple fractures… …often resulting from motor vehicle collisions

Indications for external fixation Infection
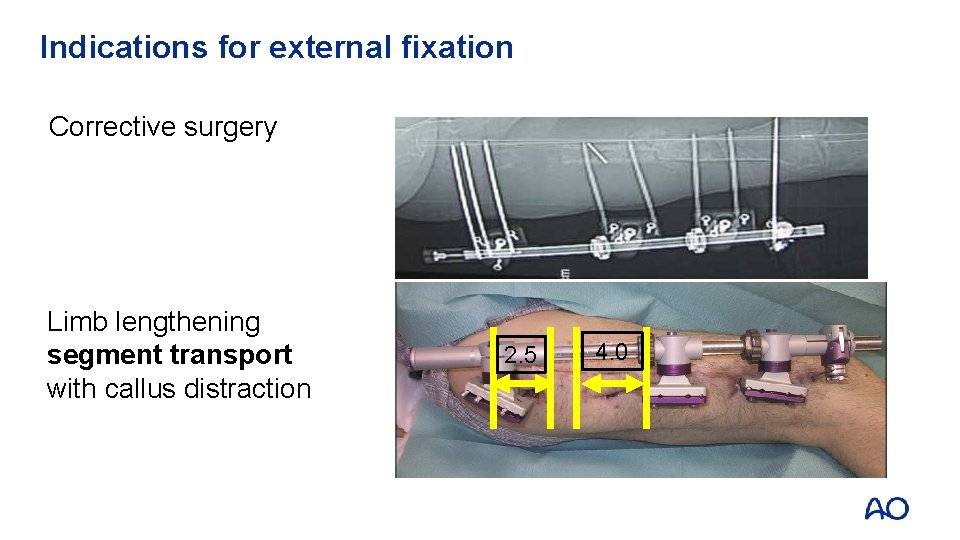
Indications for external fixation Corrective surgery Limb lengthening segment transport with callus distraction 2. 5 4. 0

Indications for external fixation Definitive fracture care • In children: avoid second operation for removal • Soft-tissue complication: cannot use cast • Avoid epiphyseal plate
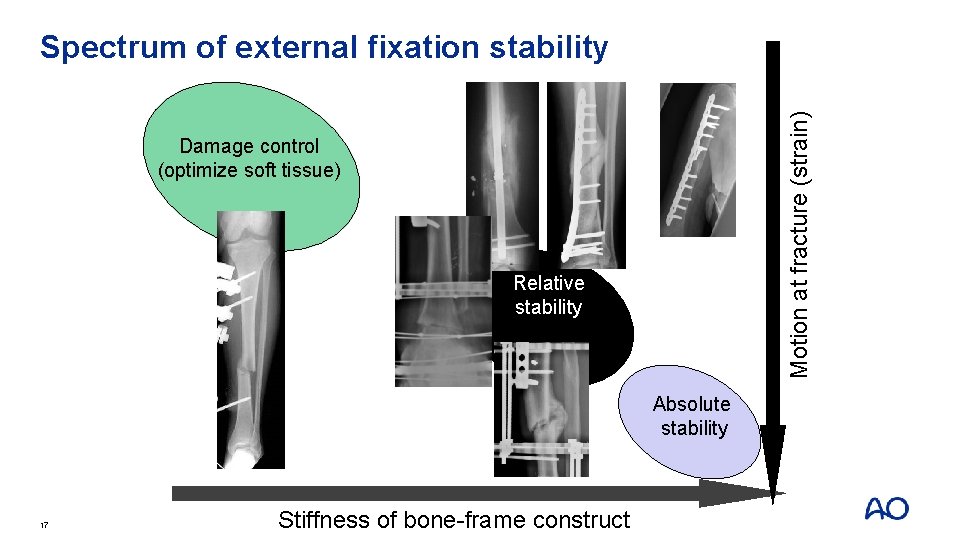
Motion at fracture (strain) Spectrum of external fixation stability Damage control (optimize soft tissue) Relative stability Absolute stability 17 Stiffness of bone-frame construct
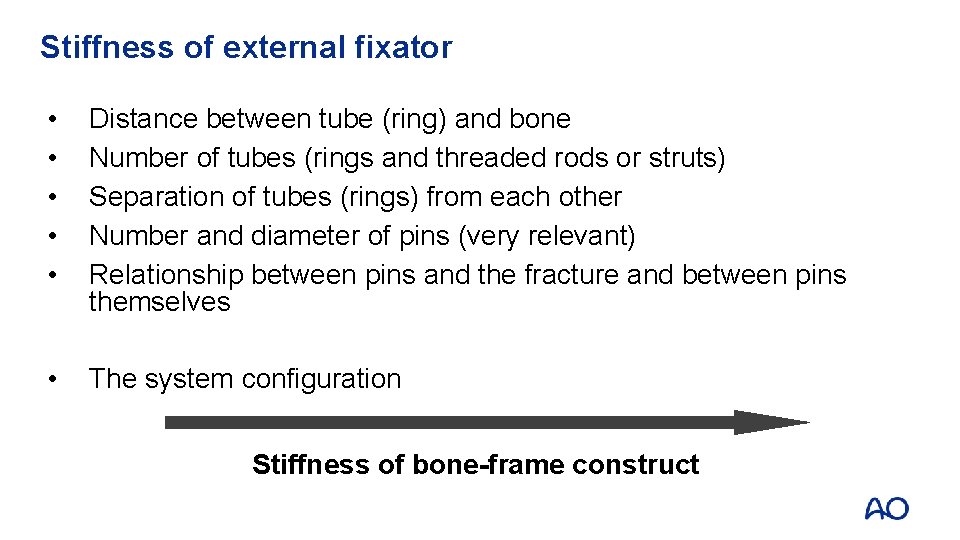
Stiffness of external fixator • • • Distance between tube (ring) and bone Number of tubes (rings and threaded rods or struts) Separation of tubes (rings) from each other Number and diameter of pins (very relevant) Relationship between pins and the fracture and between pins themselves • The system configuration Stiffness of bone-frame construct
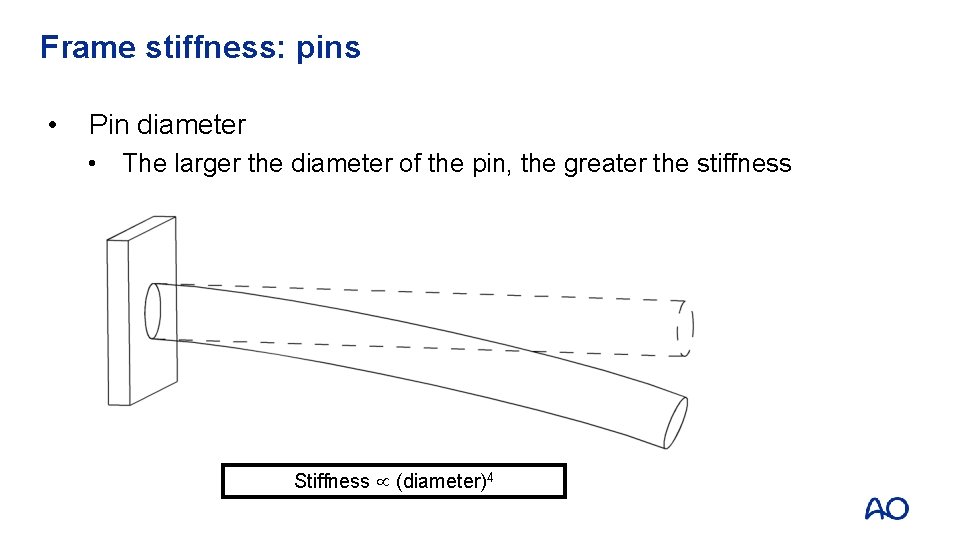
Frame stiffness: pins • Pin diameter • The larger the diameter of the pin, the greater the stiffness Stiffness µ (diameter)4
Frame stiffness: pins • Stiffness ratio: pin diameters • 4 mm vs 5 mm 1: 2. 44 • 4 mm vs 6 mm 1: 5. 06 • 5 mm vs 6 mm 1: 2. 07 • 6 mm pin is more than twice as stiff as a 5 mm pin
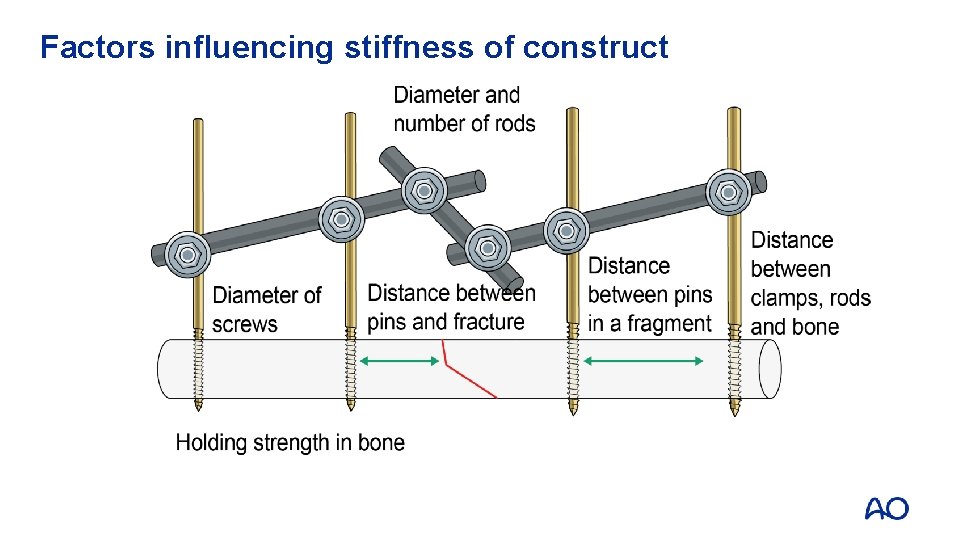
Factors influencing stiffness of construct
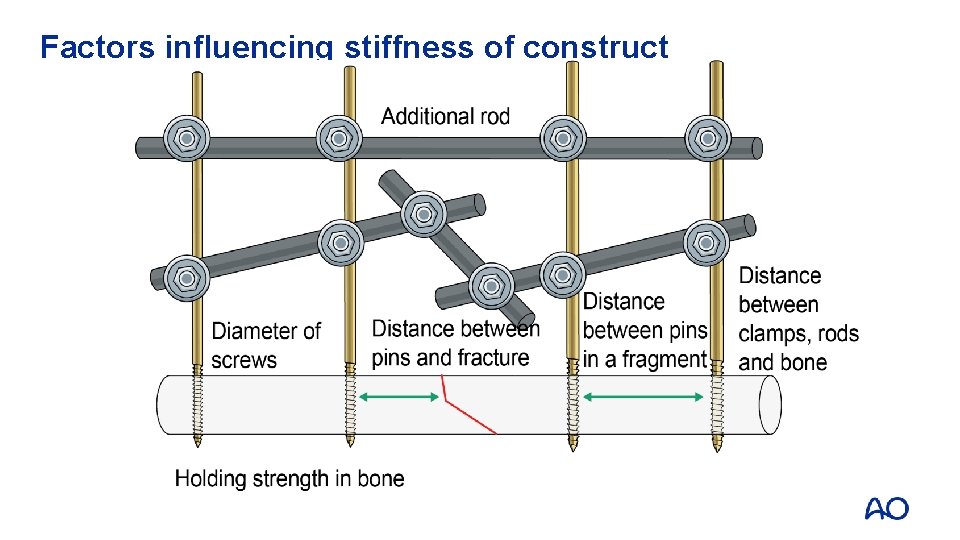
Factors influencing stiffness of construct
Modular external fixation recommended The modular external fixation technique is recommended by the AO for reduction and stabilization
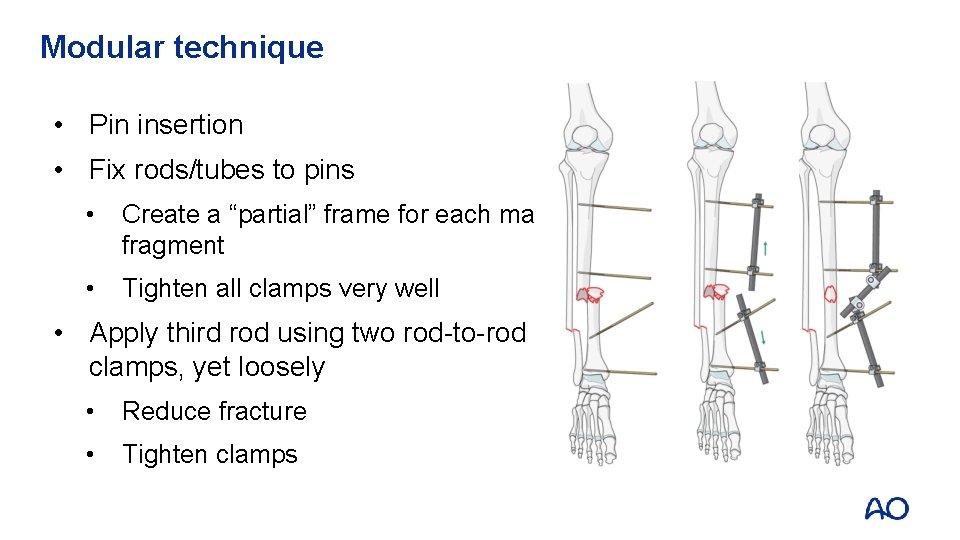
Modular technique • Pin insertion • Fix rods/tubes to pins • Create a “partial” frame for each main fragment • Tighten all clamps very well • Apply third rod using two rod-to-rod clamps, yet loosely • Reduce fracture • Tighten clamps
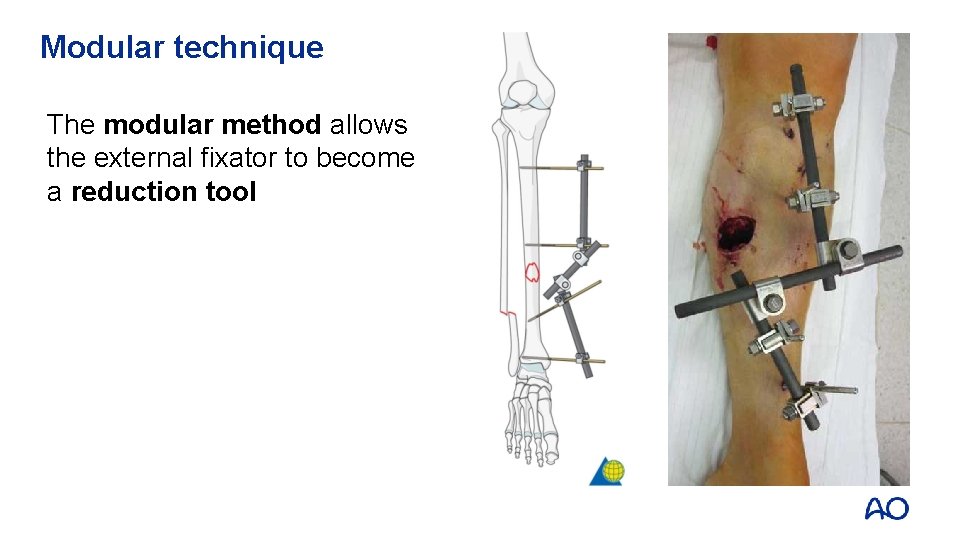
Modular technique The modular method allows the external fixator to become a reduction tool
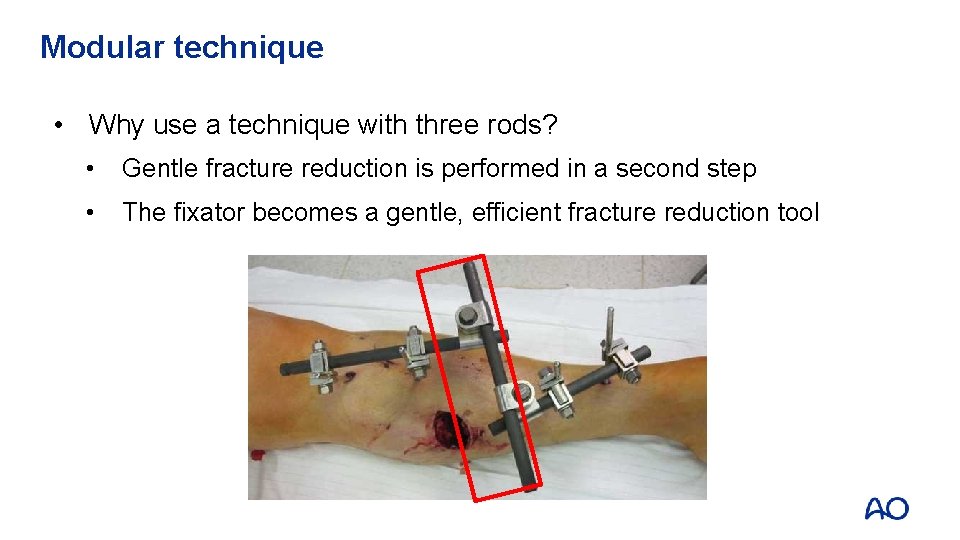
Modular technique • Why use a technique with three rods? • Gentle fracture reduction is performed in a second step • The fixator becomes a gentle, efficient fracture reduction tool
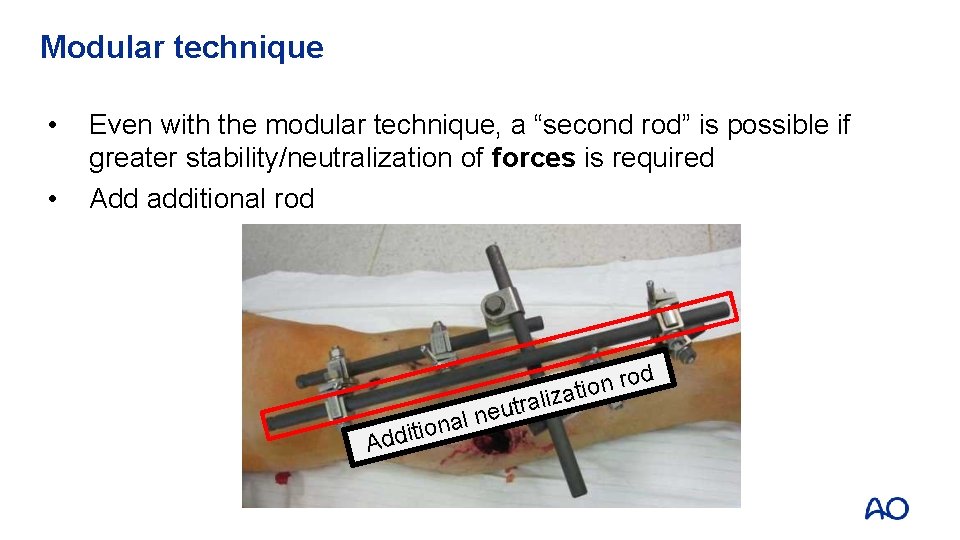
Modular technique • • Even with the modular technique, a “second rod” is possible if greater stability/neutralization of forces is required Add additional rod d o r n atio a n o i t i Add liz a r t u l ne
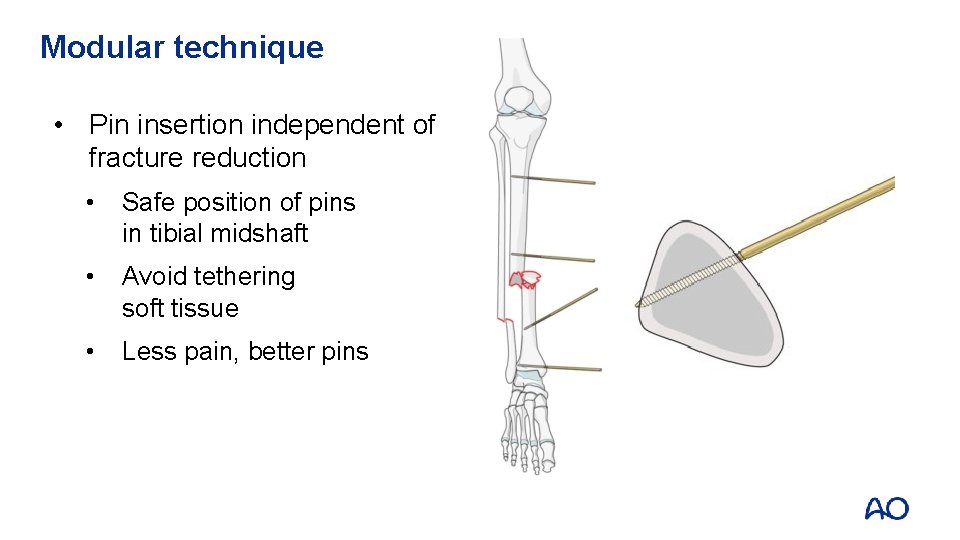
Modular technique • Pin insertion independent of fracture reduction • Safe position of pins in tibial midshaft • Avoid tethering soft tissue • Less pain, better pins
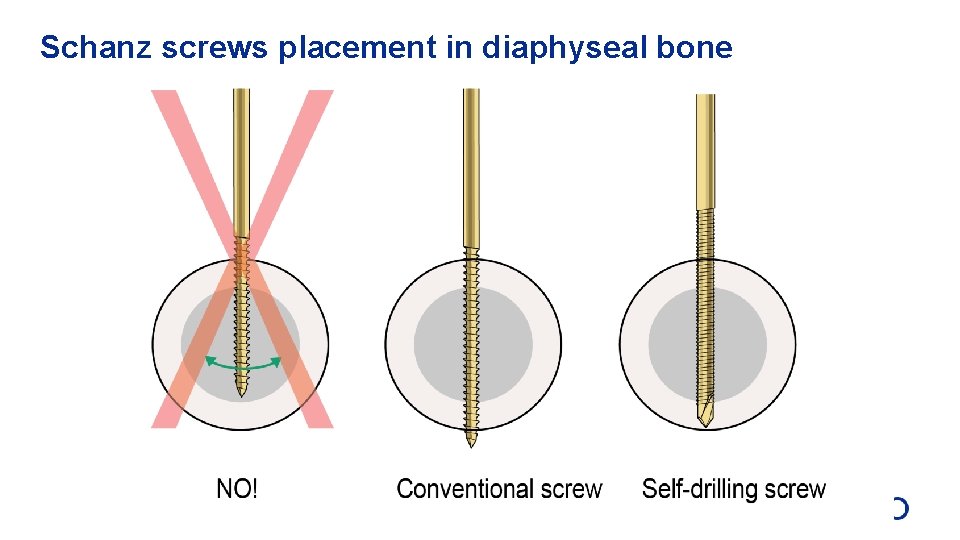
Schanz screws placement in diaphyseal bone
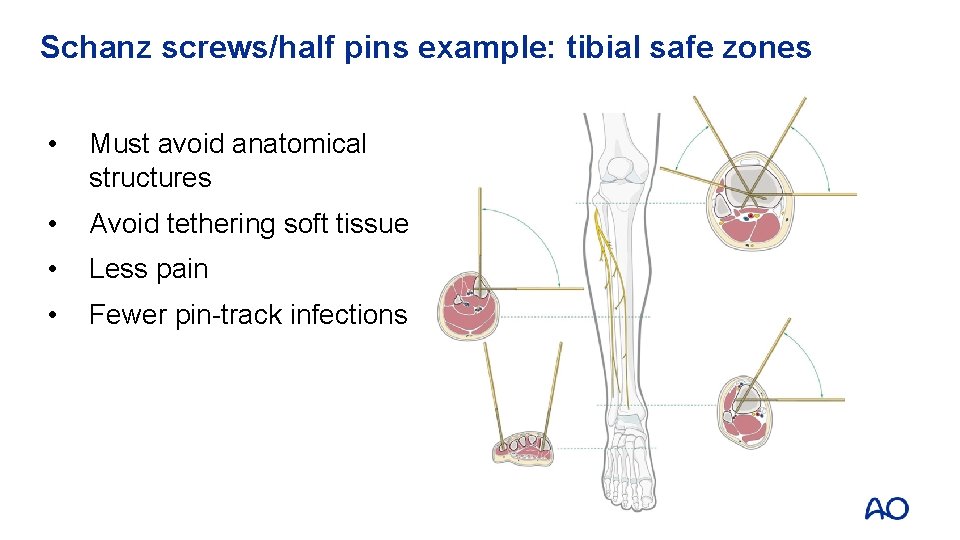
Schanz screws/half pins example: tibial safe zones • Must avoid anatomical structures • Avoid tethering soft tissue • Less pain • Fewer pin-track infections

Polytrauma—damage control external fixation
Postoperative care to prevent pin infection Controversial—no clear consensus Removal of crusts Saline or disinfectant solution Cleaning
Take-home messages • • • External fixators have broad indications Many types of fixators are available with specific functions The stability of a fixator is surgeon-controlled The modular technique is the standard for damage control applications Technique and location of pin placement is important to minimize infection and pain
- Slides: 33