Principles of Ethics Code of this lecture Objectives
Principles of Ethics
Code of this lecture

Objectives � Define Principles of Ethics � Identify Principles of Ethics. � Enumerate Unethical Behaviors within Organization.
Principles of Ethics A popular approach to ethics in health care, involves using a set of ethical principles that is drawn from the common or widely shared conception of morality.
Definition of principles Ethical Principles are guidelines that can apply to situations to decide whether they are morals or immoral in nursing.
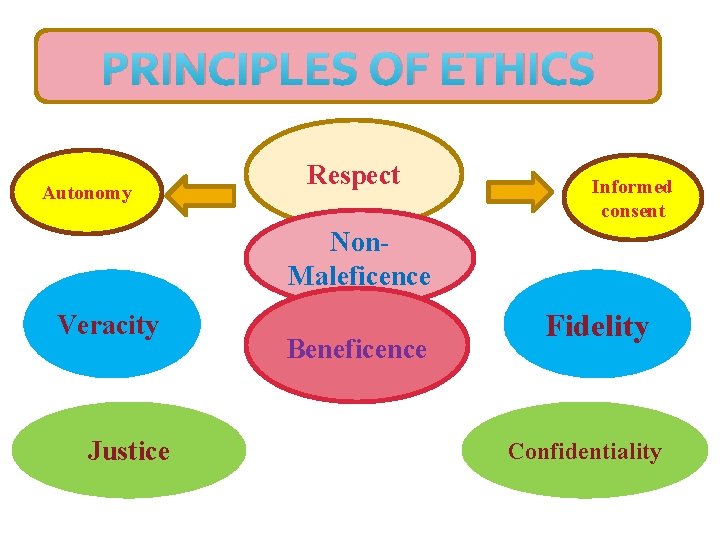
PRINCIPLES OF ETHICS Autonomy Respect Informed consent Non. Maleficence Veracity Justice Beneficence Fidelity Confidentiality


A. Autonomy: q. It is a principle that dictates that health care professionals respect a person’s right to make decisions concerning the treatment plan. q. Autonomy is the right to independence, selfdetermination and self reliance.
q Respect a person’s right to make their own decisions according to their own reasons and purposes. q Teach people to be able to make their own choices. q Support people in their individual choices. q Do not force people to do things. q Respect for autonomy requires that a person honor another’s right to govern him/or herself.
B. Informed Consent: � Is the permission obtained from a patient to undergo the treatment after the patient has been fully informed about the test or procedure (a two step process).
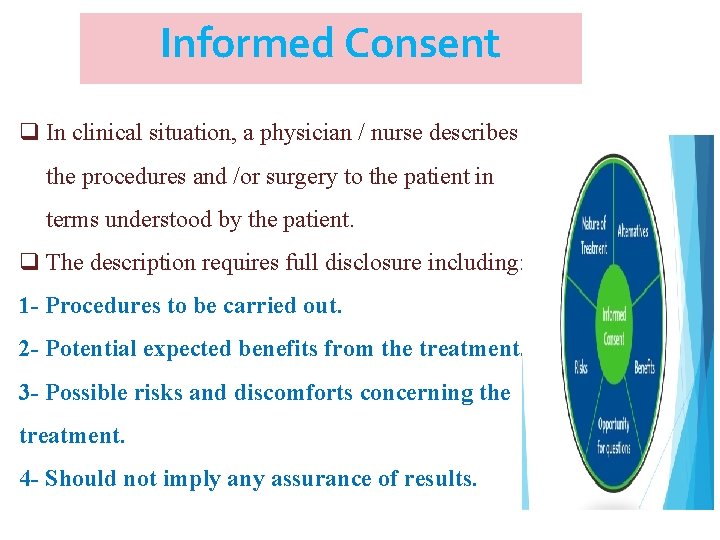
Informed Consent q In clinical situation, a physician / nurse describes the procedures and /or surgery to the patient in terms understood by the patient. q The description requires full disclosure including: 1 - Procedures to be carried out. 2 - Potential expected benefits from the treatment. 3 - Possible risks and discomforts concerning the treatment. 4 - Should not imply any assurance of results.
Informed Consent � The consent may or may not be in writing, but a written consent provides better legal protection for health care providers. � Patients must give the consent voluntarily without compulsion or persuasion. � They must be mentally competent (having mental and psychological capacity to make decisions).
Informed Consent Vulnerable people who cannot give consent : Children Elderly Patients who are unconscious. Patients have serious or enduring mental health problems. Individuals with learning disabilities may lack competence, either temporarily or permanently.
Informed Consent Informed consent is limited when there is a high probability that a person may harm himself or herself or others. � Example: the patient has the right to refuse treatment EXCEPT transmittable diseases. in cases contagious/

Non – Maleficence v Maleficence is the opposite of beneficence. v Non-maleficence: means the duty to do no harm. v This is the basic of most codes of nursing ethics. v Harm can mean deliberate harm, risk of harm, and unintentional harm. v In nursing, intentional harm is always unacceptable. v A client may be at risk of harm during a nursing intervention that is intended to be helpful.
Non – Maleficence �Do not to inflict harm on people. �Do not cause pain or suffering. �Do not weaken. �Do not cause offence. �Do not deprive people. �Do not kill.
BENEFICENCE Beneficence means doing good to benefit others. Our actions must aim to ‘benefit’ people – health, welfare, comfort, well-being, improve quality of life. ‘Benefit’ should be defined by the person themselves. It’s not what we think that is important.
BENEFICENCE ü The ethical principle of beneficence represents a continuum from not harming to doing good, 1) Not inflicting harm. 2) Preventing harm. 3) Removing harm. 4) Promoting and doing good. 5) Create a safe and supportive environment.
JUSTICE � Refers to the need to treat all people equally and fairly. � Not favouring some individuals/groups over others. � Acting in a non– biased way. � Respect for people’s rights. � Respect for the law.
JUSTICE q Distributive Justice means sharing the limited resources in society in a fair and just manner (e. g. health services, professional time). q Problems of distributive justice arise under conditions of insufficiency, competition, and unequal access to health care. q Patients should get…. . An equal share ? Just enough to meet their needs ? What they deserve regardless the ability to pay?
VERACITY ü The obligation to tell the truth and not to lie or deceive others. ü Dealing honestly with patients.
VERACITY � Hippocratic Promise does not require that physicians deal honestly with patients, he claims that it releases patient distress, focusing on the consequences but not inherent moral element.
VERACITY There are three levels of Veracity: Fully disclosing information. Withholding information. Giving false information. q In health care, family members will often request health care providers not to tell their loved ones the truth about their diagnosis or prognosis.
VERACITY When the patient has a terminal diagnosis such as cancer etc…. . , health care providers, may have difficulty sharing such information with patient that will result in unhappiness, anxiety, depression or fear.
FIDELITY q Is the individual’s obligation to keep the commitments/ promises he/she has made. q It means that a person should faithfully fulfill his/her duties and responsibilities. q Nurses have responsibilities to clients, managers, government, society, profession, and themselves (Loyalty). the
FIDELITY Commitments / promises may be implicit or explicit. q Implicit: promises that are implied, not verbally communicated. Ex: when patients comes into the hospital, they expect to be cared for. q Explicit: promises that are verbally communicated. Ex: if a nurse tell the patient that she ’ll be back with pain medication, she’d better come back.
CONFIDENTIALITY Means that information entrusted to professionals in the line of duty should not be revealed to others.
CONFIDENTIALITY v All health professions include in their professional code a requirement to preserve the confidentiality of health information, which is considered an integral component of the nurse-patient relationship.
CONFIDENTIALITY v In the course of caring for a patient, nurses get to know many things about that person. v The patient must feel that he or she and the nurse are in a relationship of trust and confidence for such information to be shared.
CONFIDENTIALITY � private information must be kept confidential except when protecting one person’s privacy harms self or another (direct threat to self or another person).
Unethical behaviors within organization • • Lying to supervisors. Recording more expenses. Stealing. Accepting gifts against company’s policy. Favoritism. Taking credit for others work. Terminating employees without any reason. Using company property for personal use.
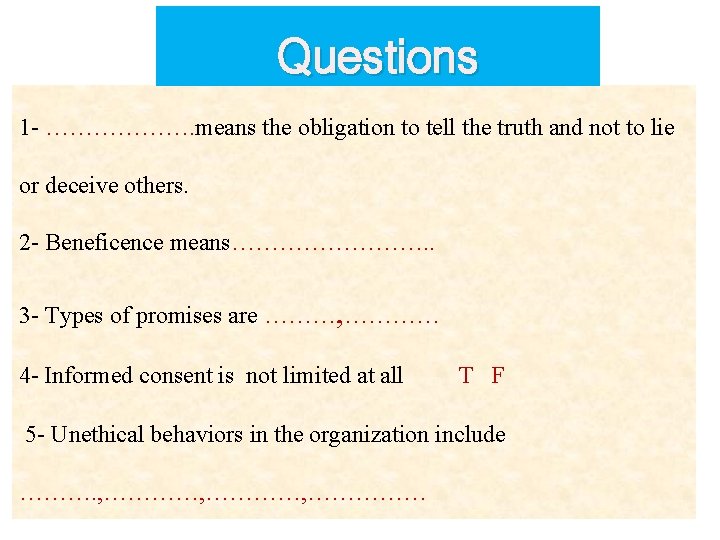
Questions 1 - ………………. means the obligation to tell the truth and not to lie or deceive others. 2 - Beneficence means…………. . 3 - Types of promises are ………, ………… 4 - Informed consent is not limited at all T F 5 - Unethical behaviors in the organization include ………. , …………, ……………

- Slides: 33