Principle of Computed tomography Introduction n In 1950Allan

![Central Slice Projection Theorem P( t) ky y t μ(x, y) F[P( t)] x Central Slice Projection Theorem P( t) ky y t μ(x, y) F[P( t)] x](https://slidetodoc.com/presentation_image_h/b8767626d578b1cc80a05af9e3c10543/image-38.jpg)
![y ky F-1[F(kx, ky)] v x u(x, y) u F(kx, ky) Inverse 2 D-FT y ky F-1[F(kx, ky)] v x u(x, y) u F(kx, ky) Inverse 2 D-FT](https://slidetodoc.com/presentation_image_h/b8767626d578b1cc80a05af9e3c10543/image-39.jpg)
- Slides: 69
Principle of Computed tomography 嘉義長庚放射科 廖書柏
Introduction n In 1950,Allan M. Cormack develop theoretical and mathematical methods used to reconstruct CT images. n In 1972 Godfrey N. Hounsfield and colleagues of EMI Central Research Laboratories built the first CAT scan machine, taking Cormack's theoretical calculation into a real application. n For their independent efforts, Cormack and Hounsfield shared the Nobel Prize in medicine and physiology in 1979.
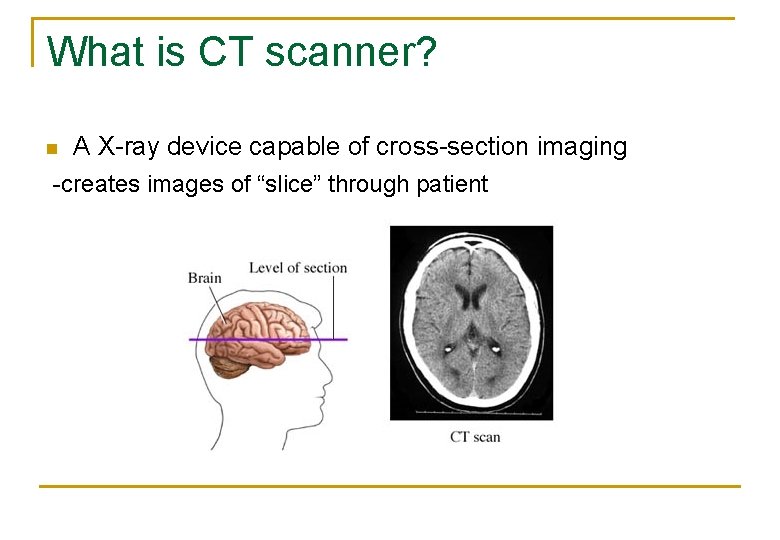
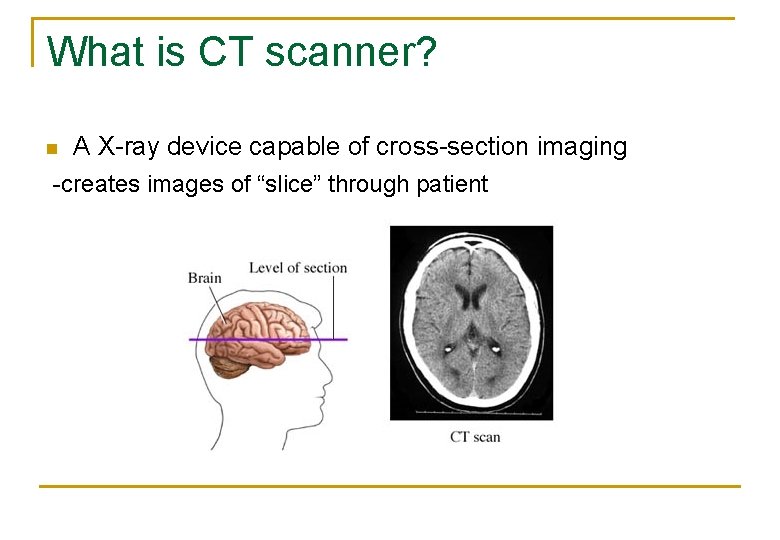
What is CT scanner? n A X-ray device capable of cross-section imaging -creates images of “slice” through patient
Advantages of CT scanning Ability of differentiate overlying structure n Excellent contrast -overlying structure don’t decrease contrast -digital images, so variable window settings n
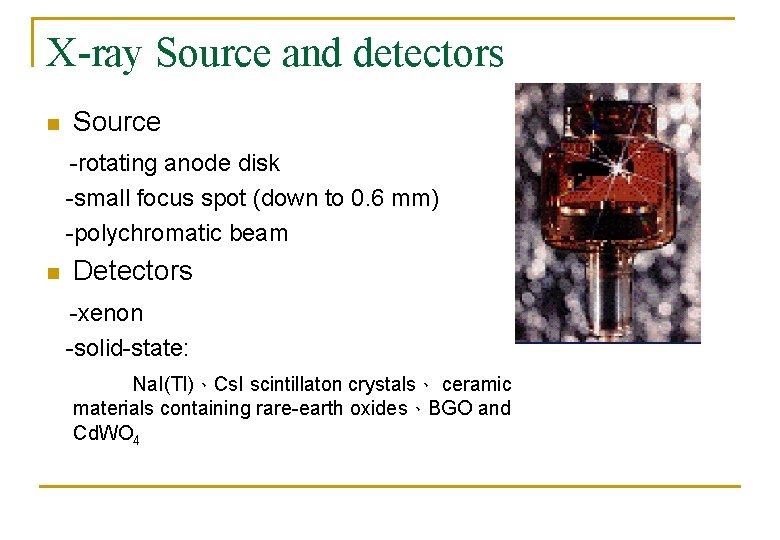
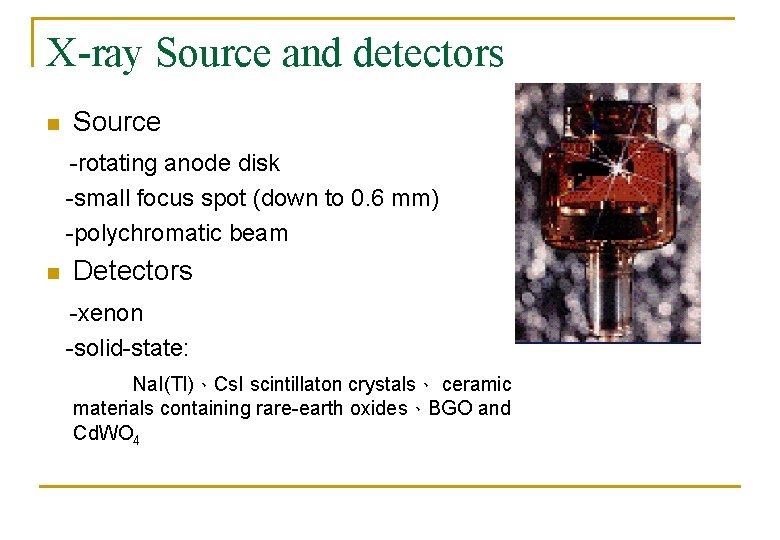
X-ray Source and detectors n Source -rotating anode disk -small focus spot (down to 0. 6 mm) -polychromatic beam n Detectors -xenon -solid-state: Na. I(Tl)、Cs. I scintillaton crystals、 ceramic materials containing rare-earth oxides、BGO and Cd. WO 4
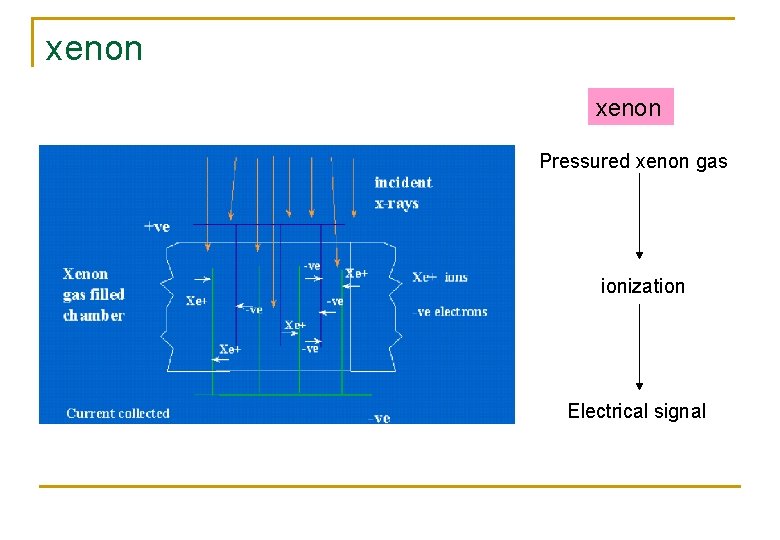
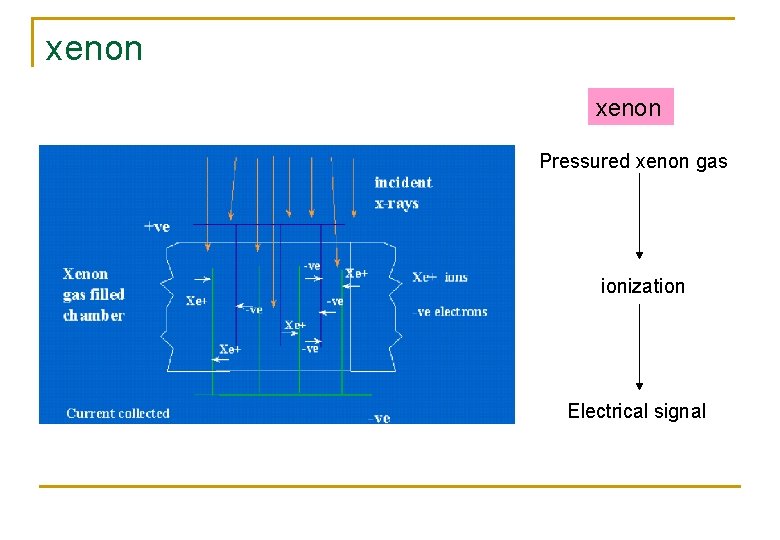
xenon Pressured xenon gas ionization Electrical signal
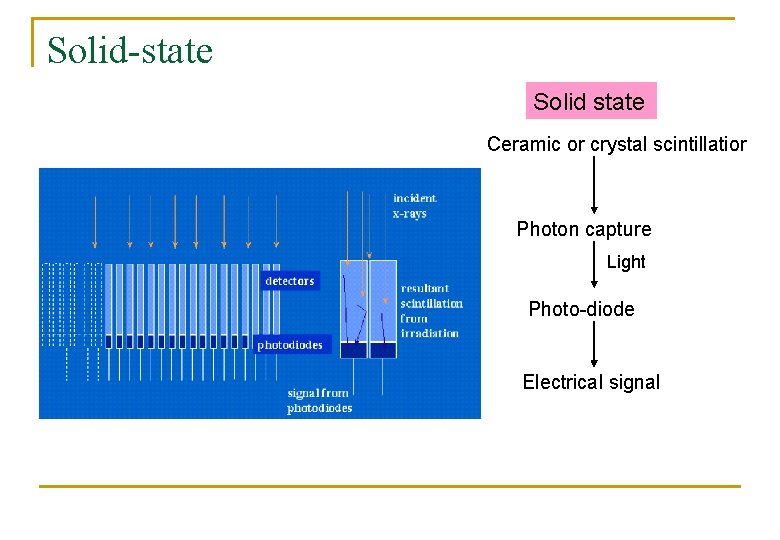
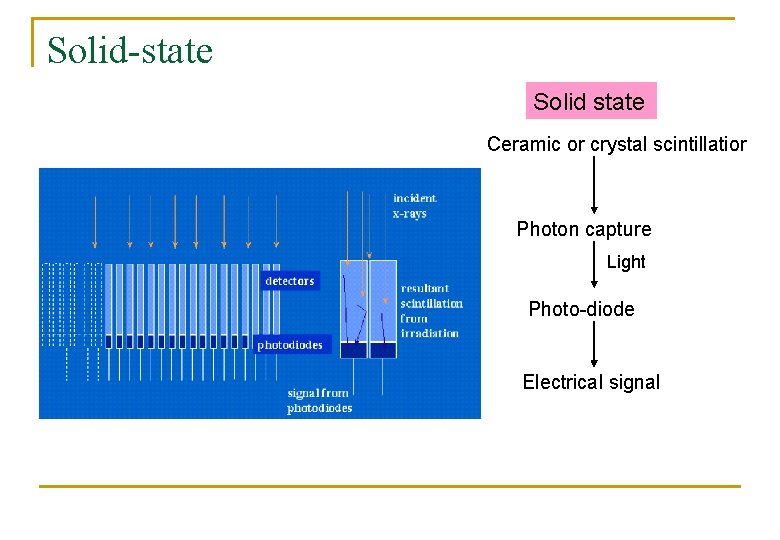
Solid-state Solid state Ceramic or crystal scintillatior Photon capture Light Photo-diode Electrical signal
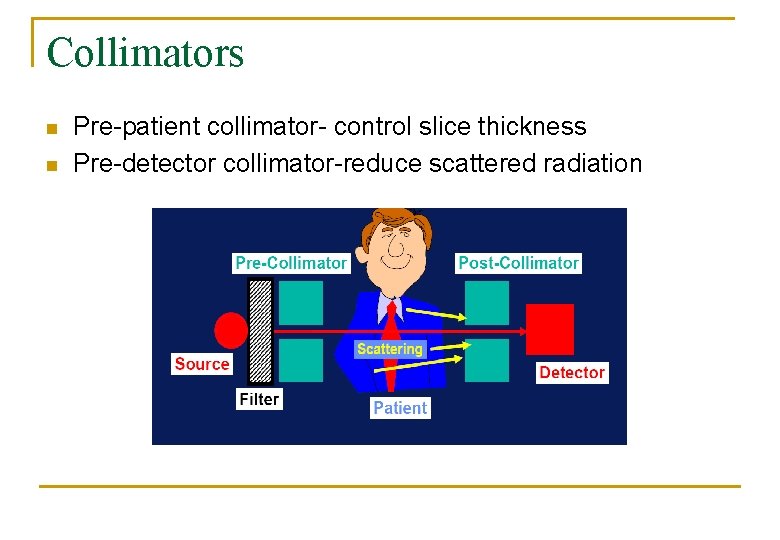
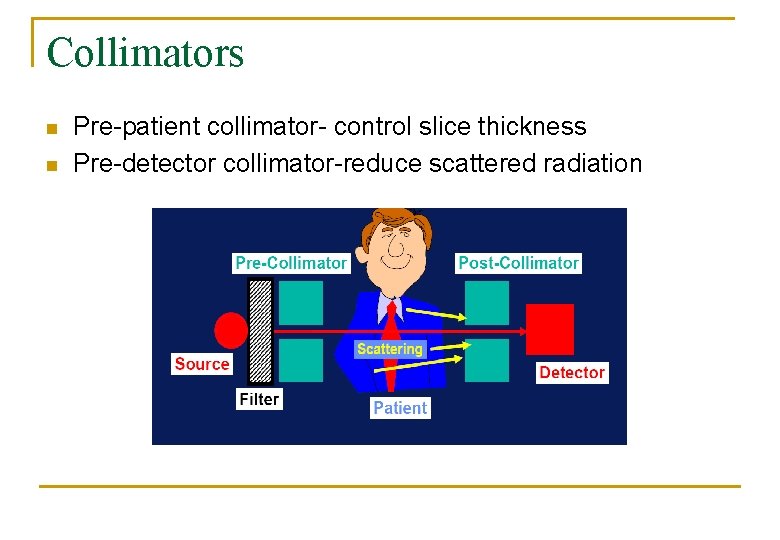
Collimators n n Pre-patient collimator- control slice thickness Pre-detector collimator-reduce scattered radiation
History of CT
n Variations in scanner design based on : l l l X-ray tube and detector movement Detector arrangement Rotating mechanism
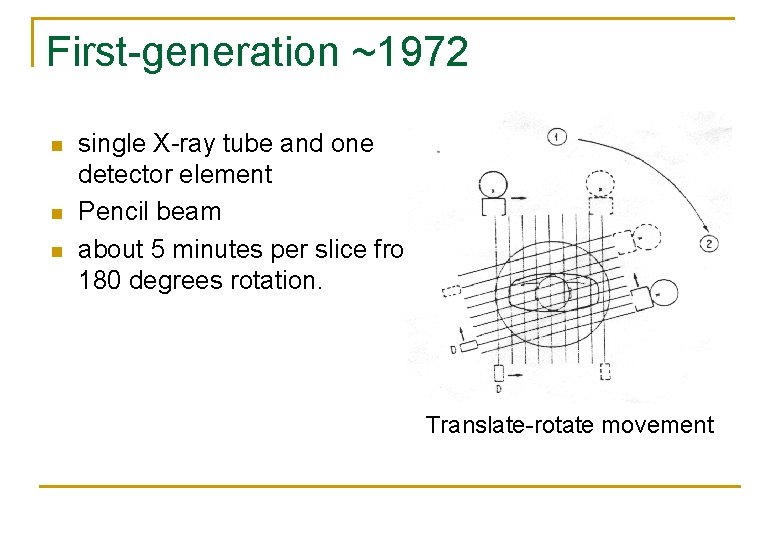
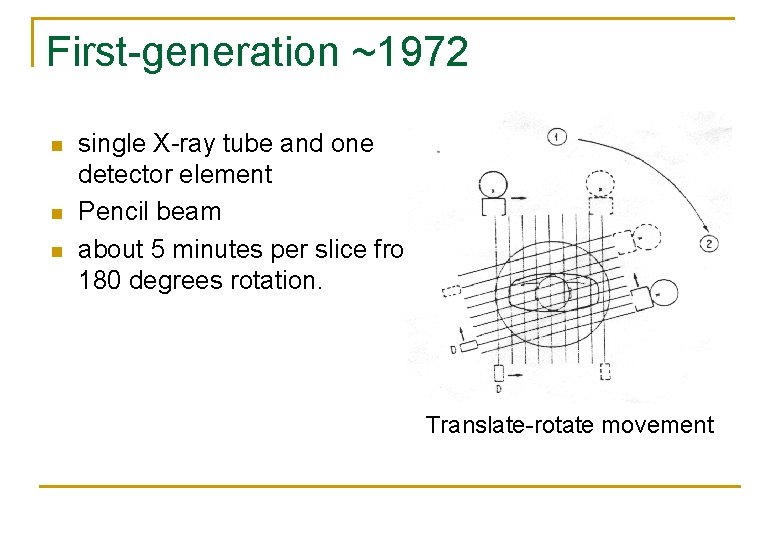
First-generation ~1972 n n n single X-ray tube and one detector element Pencil beam about 5 minutes per slice from 180 degrees rotation. Translate-rotate movement
EMI CT 1000
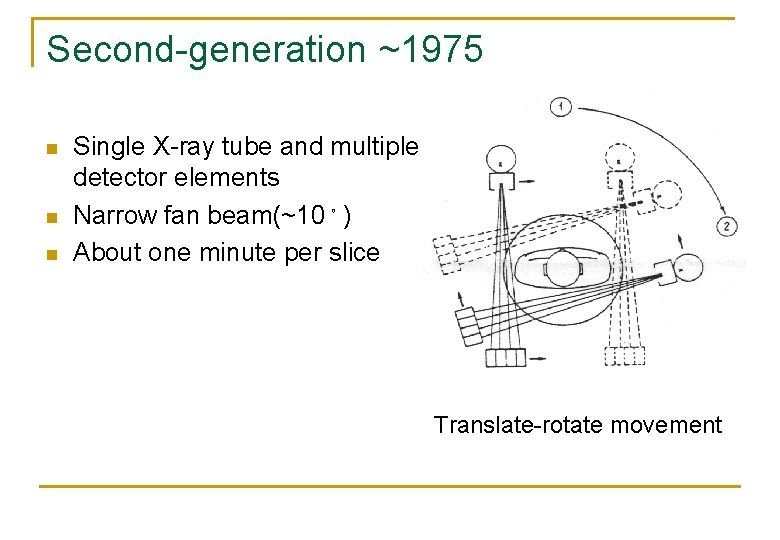
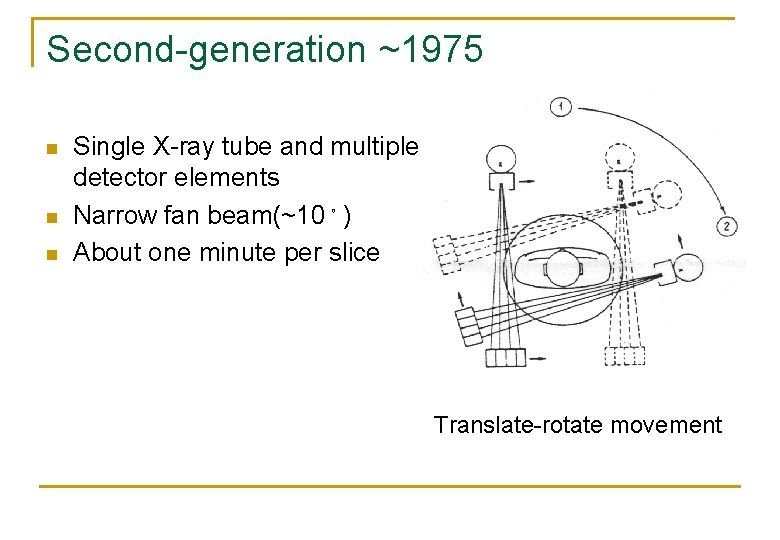
Second-generation ~1975 n n n Single X-ray tube and multiple detector elements Narrow fan beam(~10。) About one minute per slice Translate-rotate movement
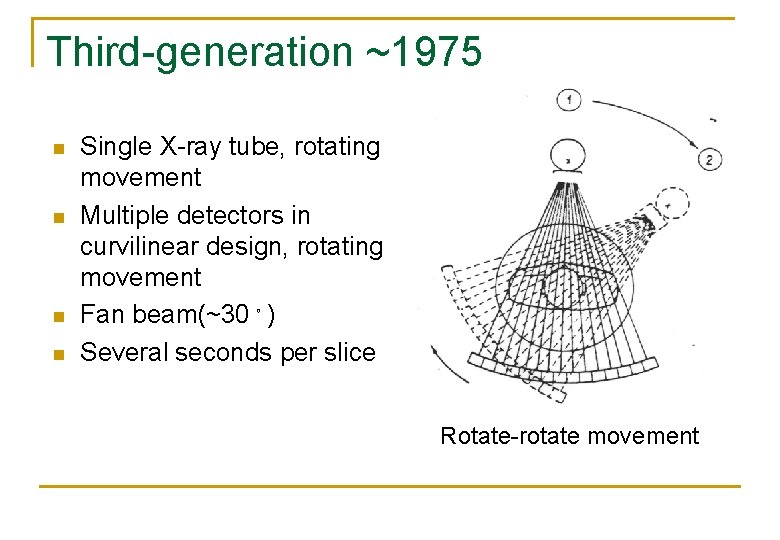
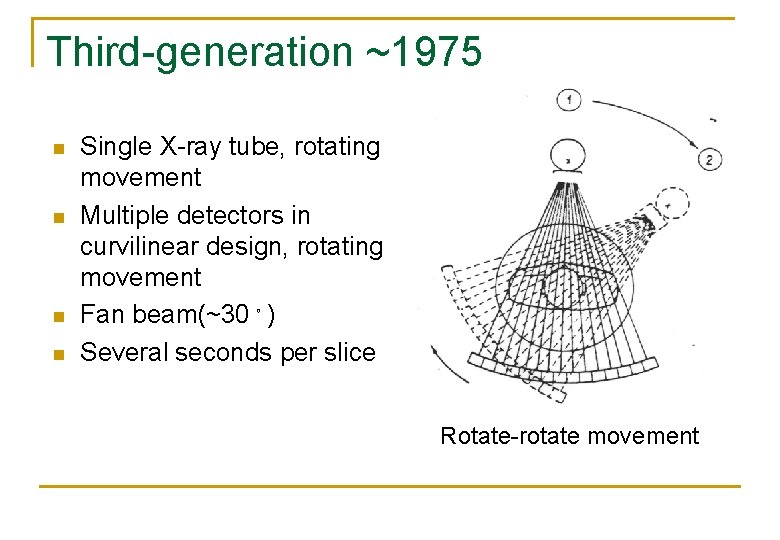
Third-generation ~1975 n n Single X-ray tube, rotating movement Multiple detectors in curvilinear design, rotating movement Fan beam(~30。) Several seconds per slice Rotate-rotate movement
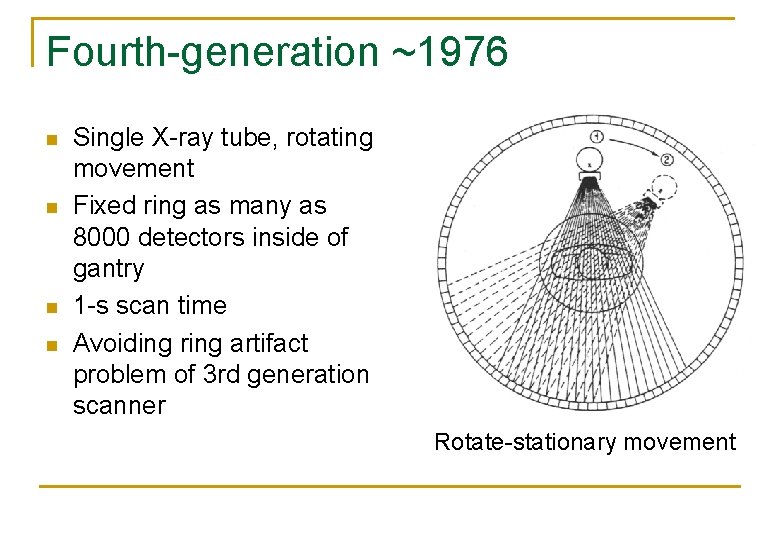
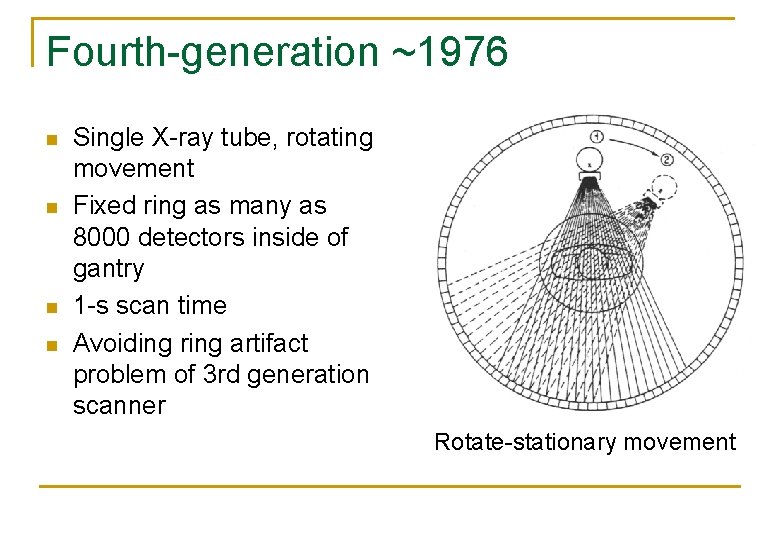
Fourth-generation ~1976 n n Single X-ray tube, rotating movement Fixed ring as many as 8000 detectors inside of gantry 1 -s scan time Avoiding ring artifact problem of 3 rd generation scanner Rotate-stationary movement
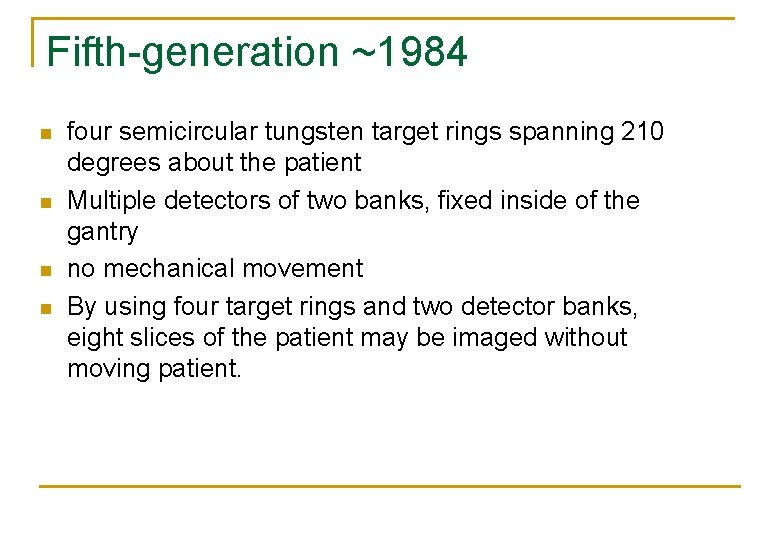
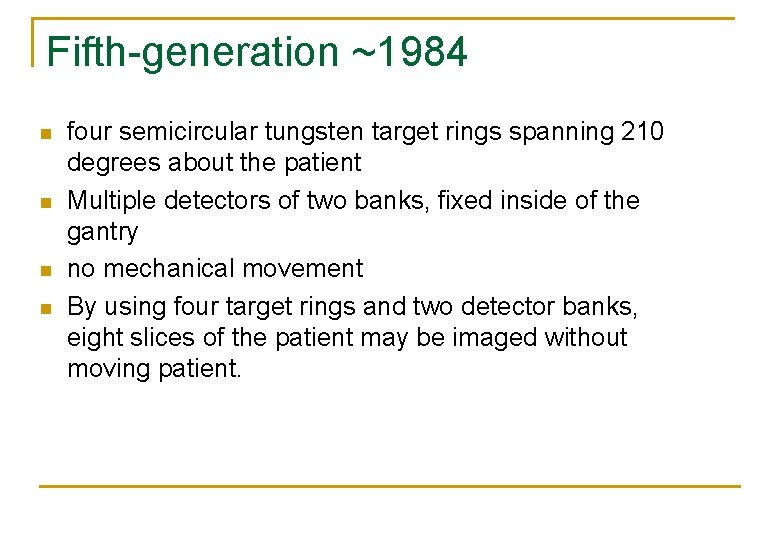
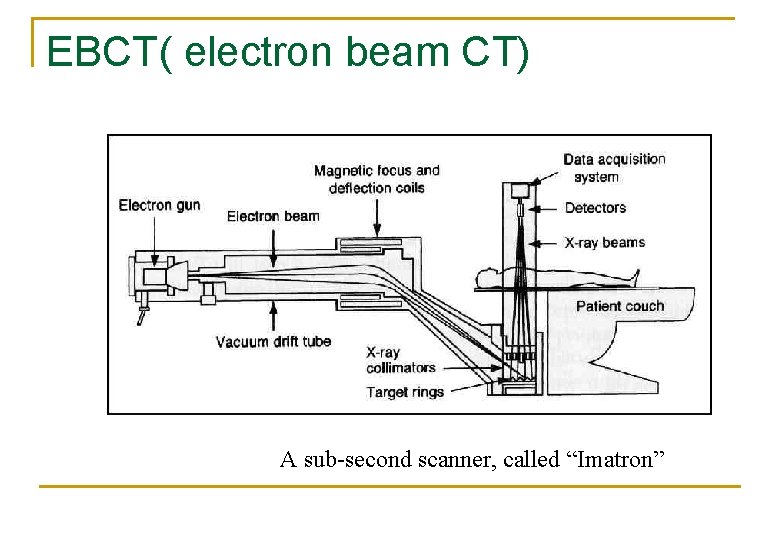
Fifth-generation ~1984 n n four semicircular tungsten target rings spanning 210 degrees about the patient Multiple detectors of two banks, fixed inside of the gantry no mechanical movement By using four target rings and two detector banks, eight slices of the patient may be imaged without moving patient.
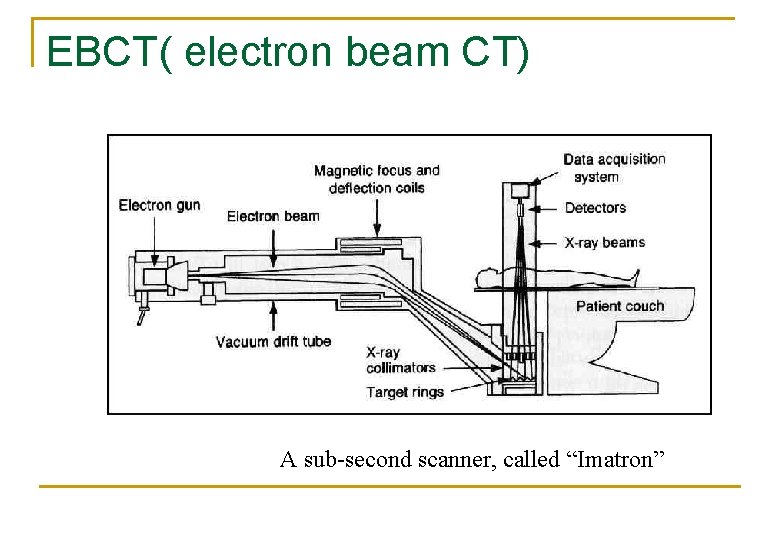
EBCT( electron beam CT) A sub-second scanner, called “Imatron”
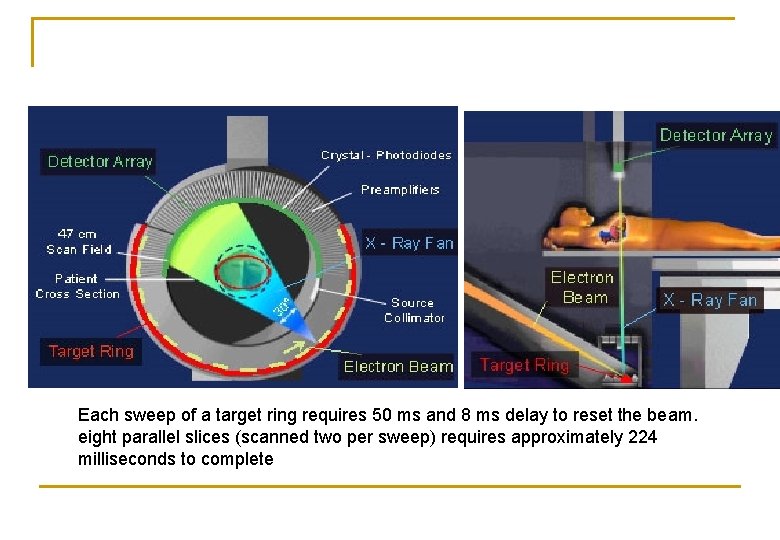
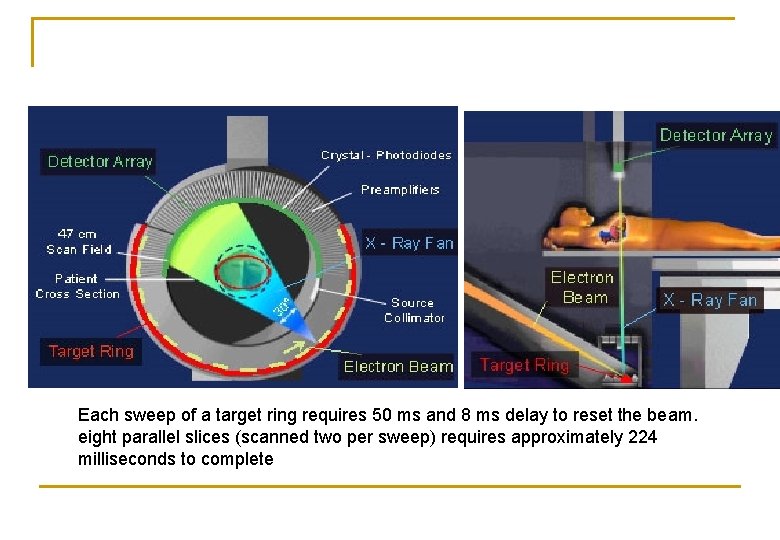
Each sweep of a target ring requires 50 ms and 8 ms delay to reset the beam. eight parallel slices (scanned two per sweep) requires approximately 224 milliseconds to complete
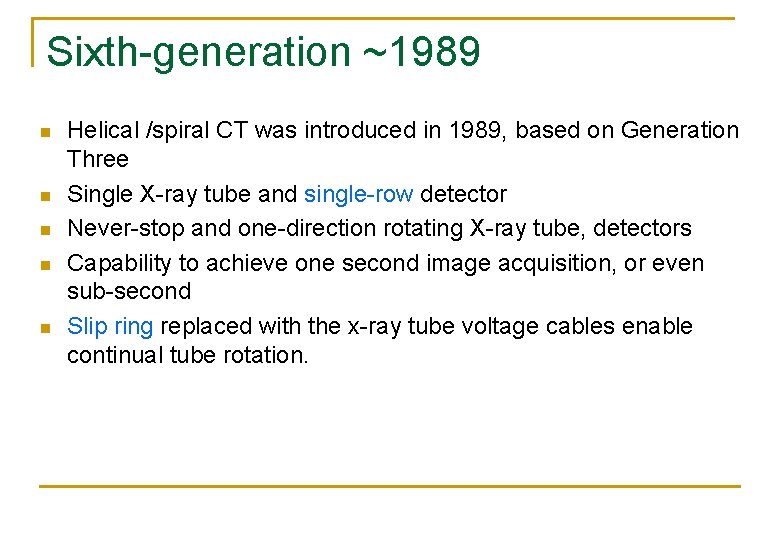
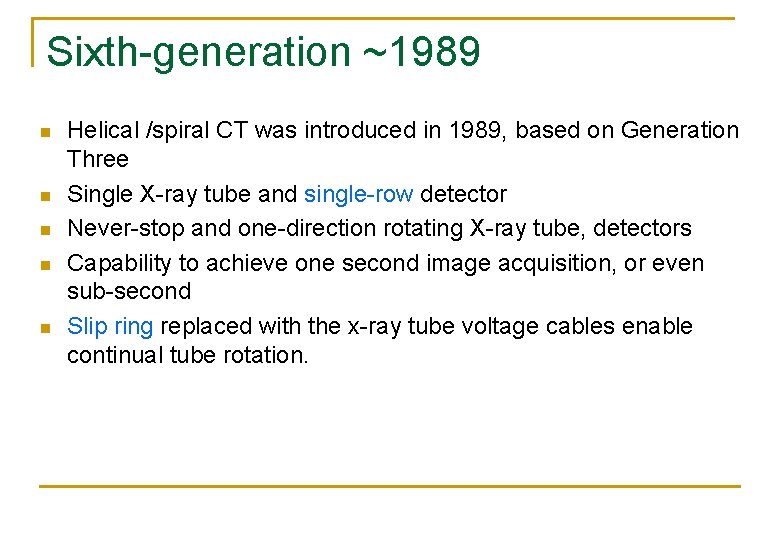
Sixth-generation ~1989 n n n Helical /spiral CT was introduced in 1989, based on Generation Three Single X-ray tube and single-row detector Never-stop and one-direction rotating X-ray tube, detectors Capability to achieve one second image acquisition, or even sub-second Slip ring replaced with the x-ray tube voltage cables enable continual tube rotation.
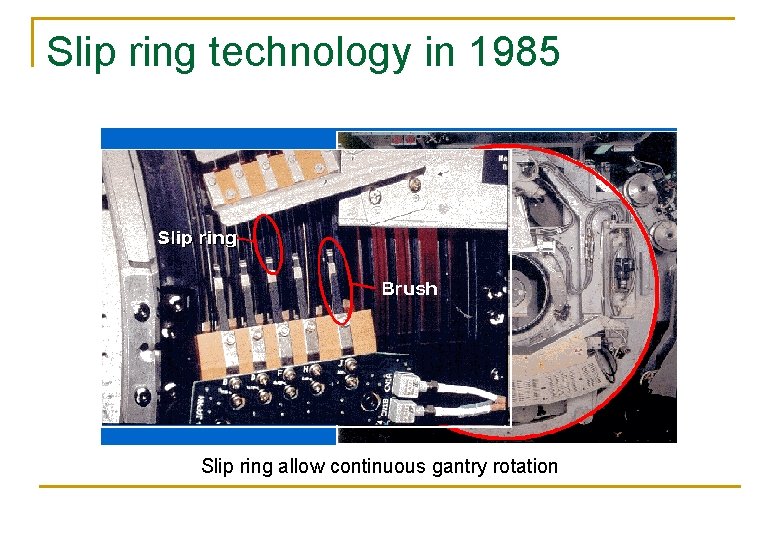
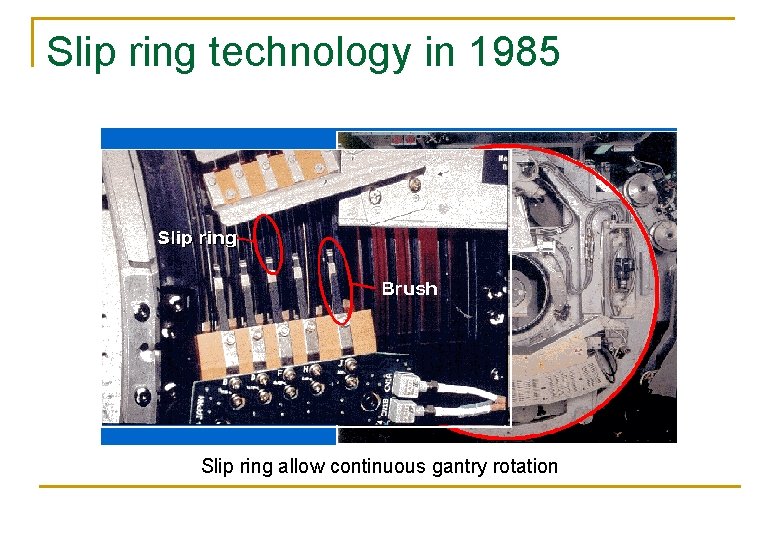
Slip ring technology in 1985 Slip ring allow continuous gantry rotation
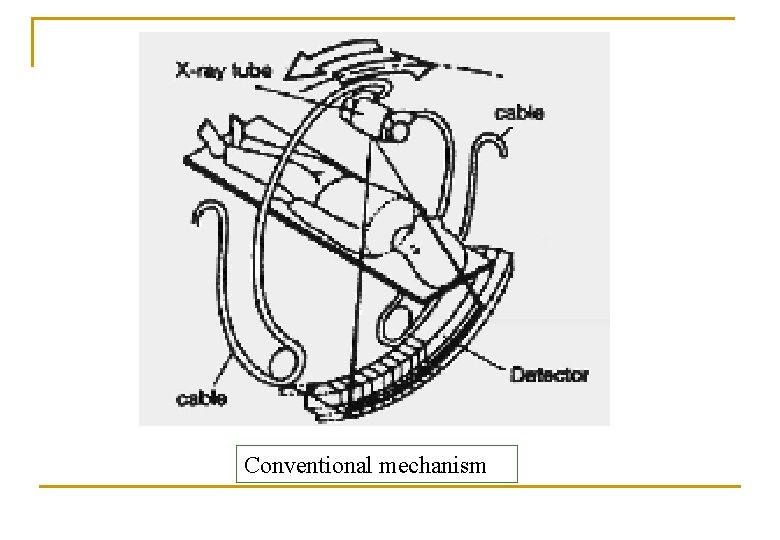
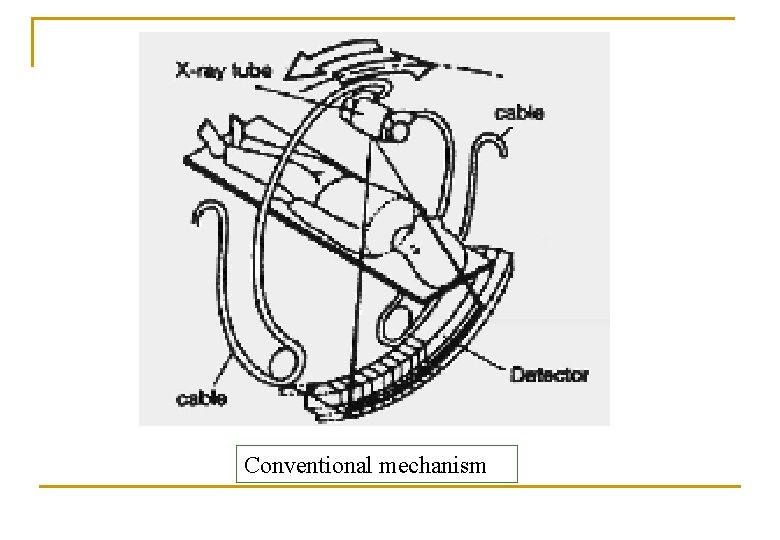
Conventional mechanism
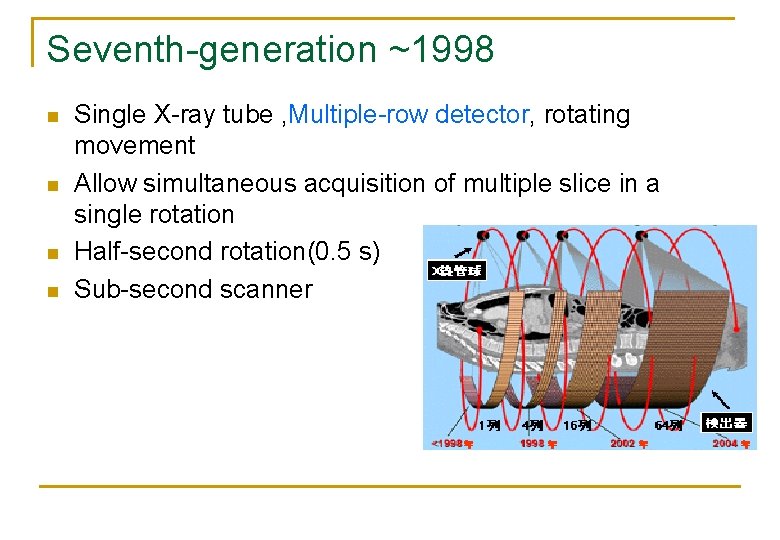
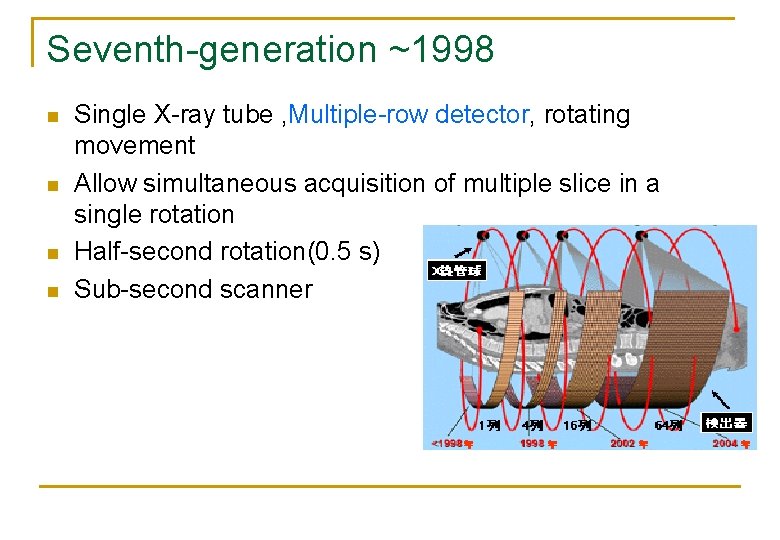
Seventh-generation ~1998 n n Single X-ray tube , Multiple-row detector, rotating movement Allow simultaneous acquisition of multiple slice in a single rotation Half-second rotation(0. 5 s) Sub-second scanner
The Basic CT Term n n n Image matrix Linear attenuation coefficient CT numbers
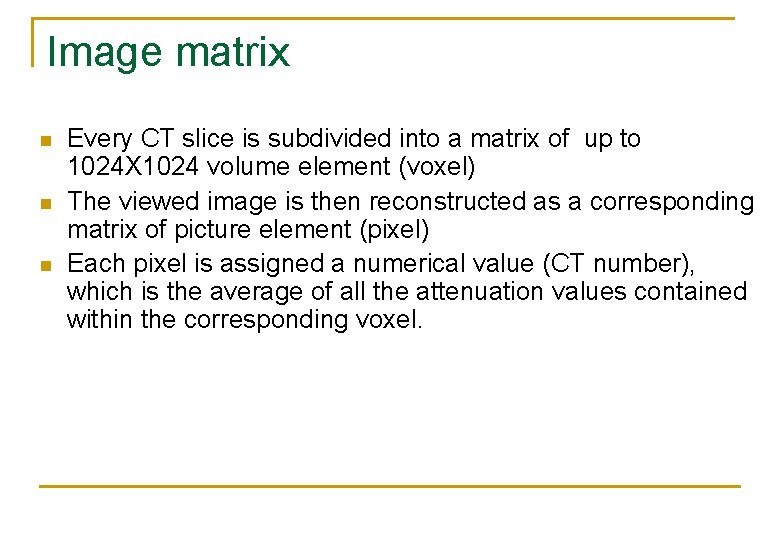
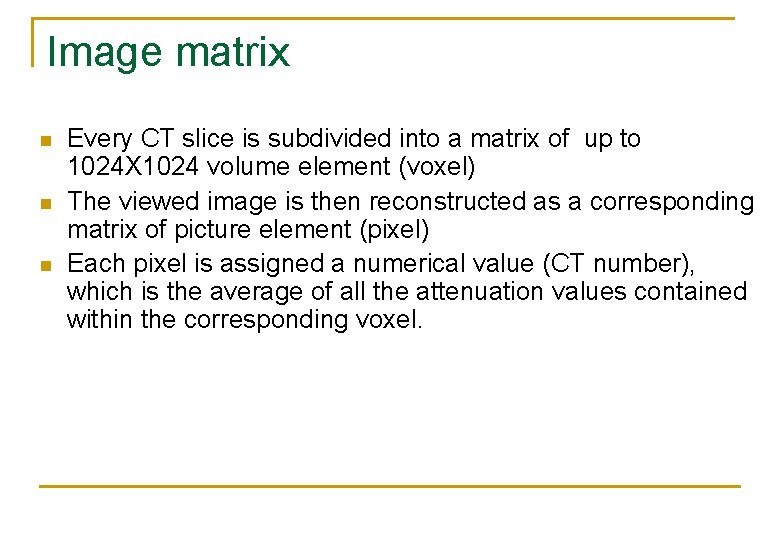
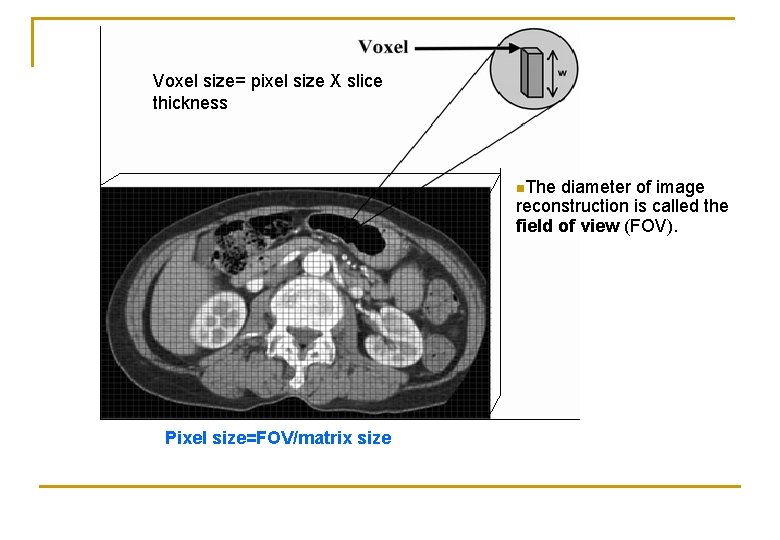
Image matrix n n n Every CT slice is subdivided into a matrix of up to 1024 X 1024 volume element (voxel) The viewed image is then reconstructed as a corresponding matrix of picture element (pixel) Each pixel is assigned a numerical value (CT number), which is the average of all the attenuation values contained within the corresponding voxel.
Voxel size= pixel size X slice thickness n. The diameter of image reconstruction is called the field of view (FOV). Pixel size=FOV/matrix size
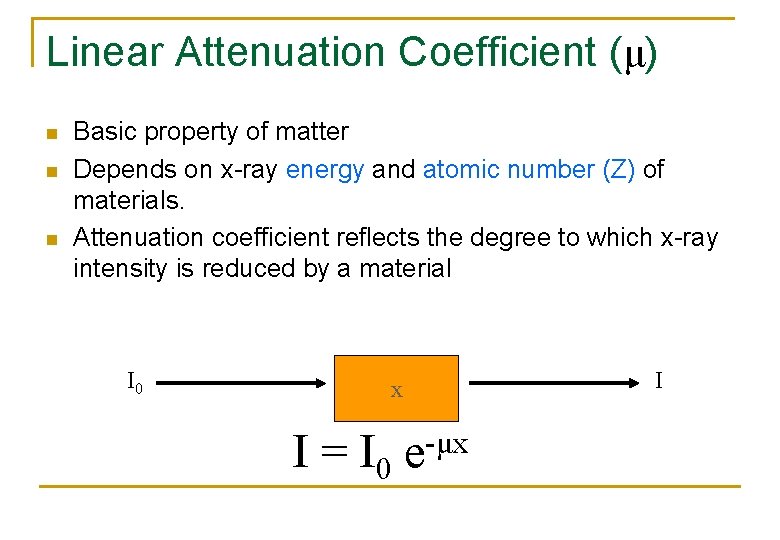
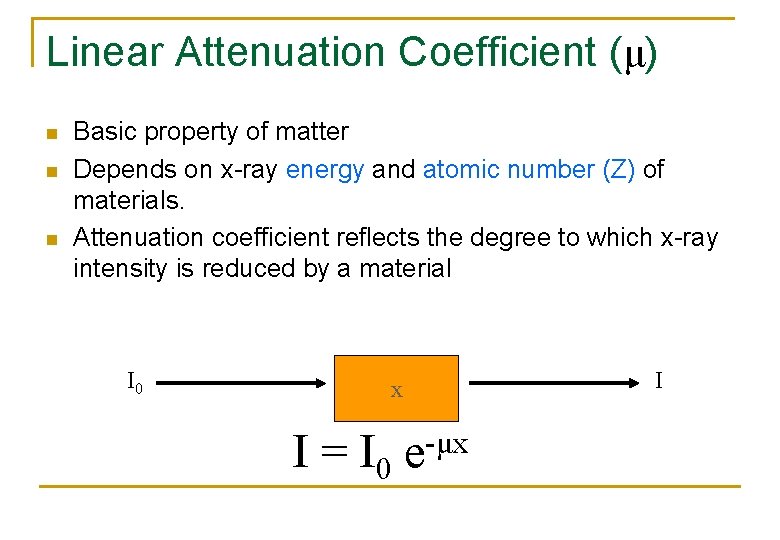
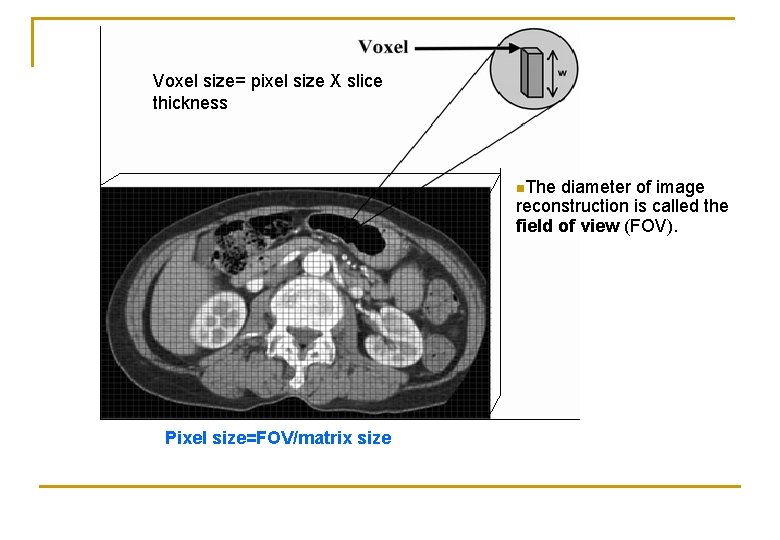
Linear Attenuation Coefficient (μ) n n n Basic property of matter Depends on x-ray energy and atomic number (Z) of materials. Attenuation coefficient reflects the degree to which x-ray intensity is reduced by a material I 0 x I = I 0 e-μx I
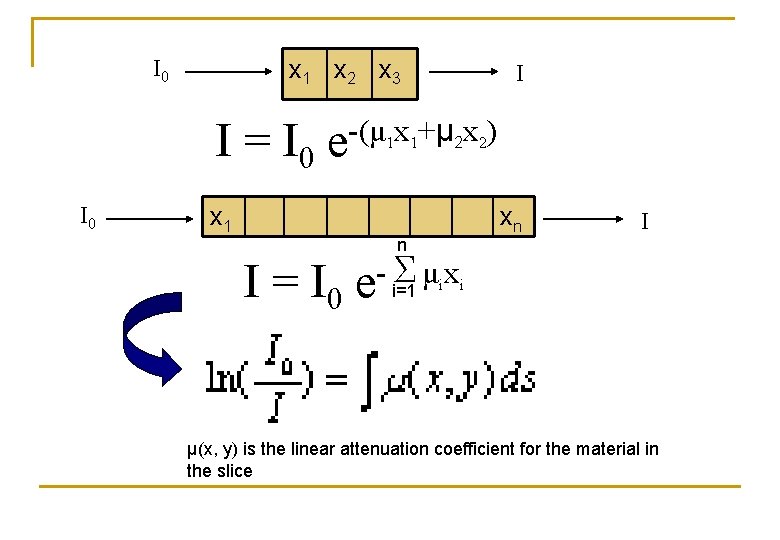
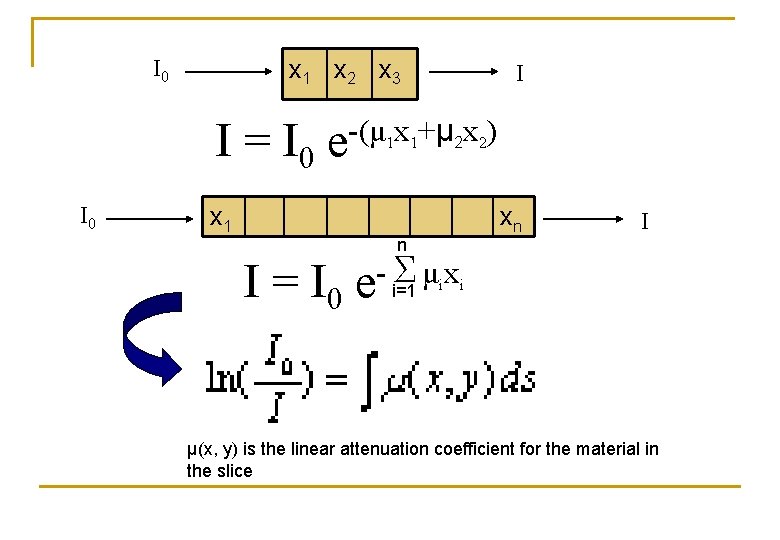
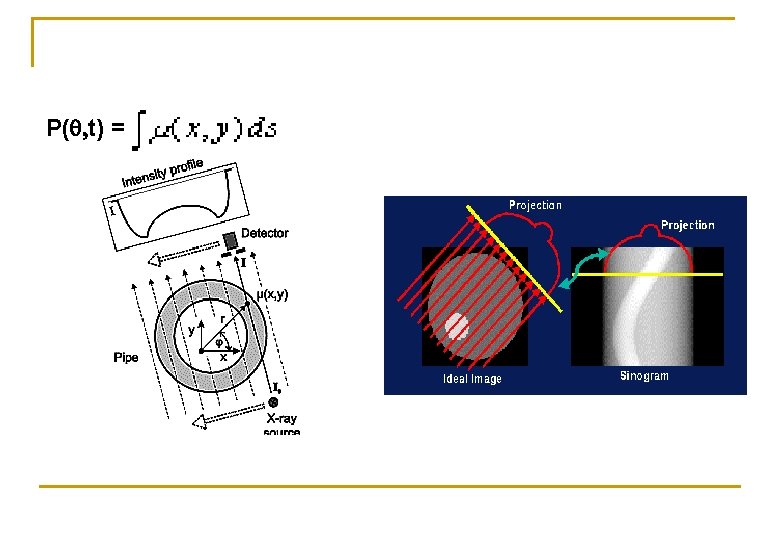
x 1 x 2 x 3 I 0 I I = I 0 e-(μ x +μ x ) 1 1 I 0 x 1 n 2 2 xn I Σ μ x i I = I 0 e i=1 i μ(x, y) is the linear attenuation coefficient for the material in the slice
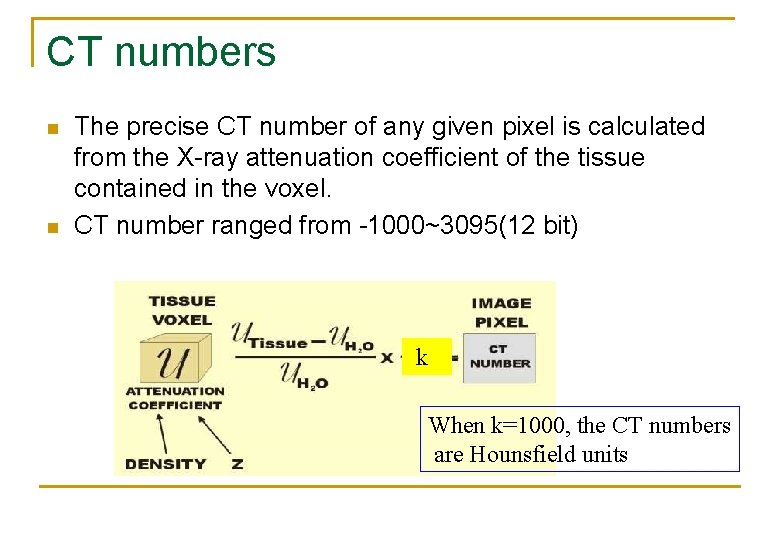
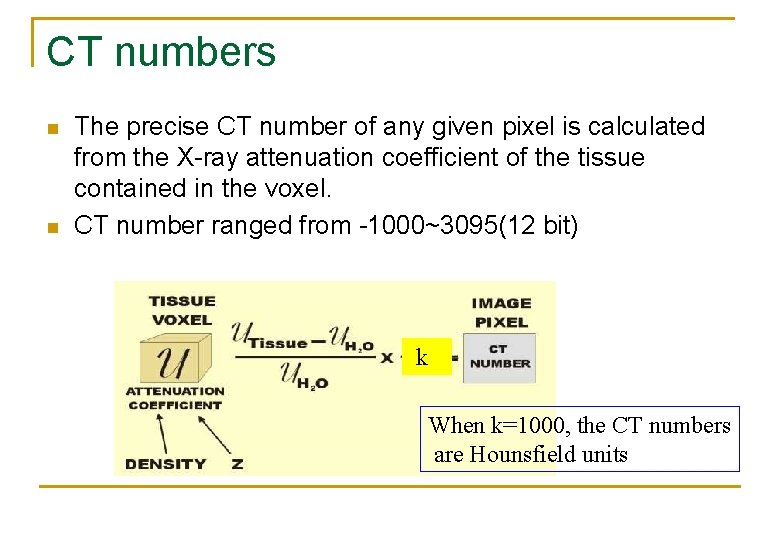
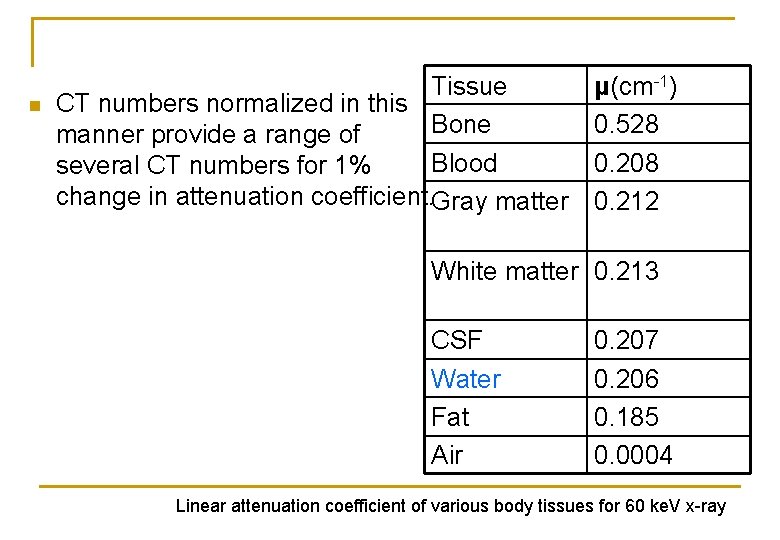
CT numbers n n The precise CT number of any given pixel is calculated from the X-ray attenuation coefficient of the tissue contained in the voxel. CT number ranged from -1000~3095(12 bit) k When k=1000, the CT numbers are Hounsfield units
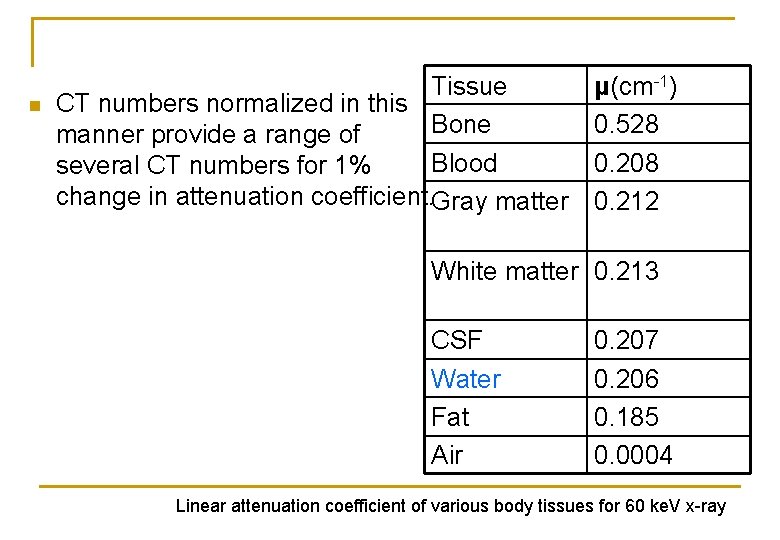
n Tissue CT numbers normalized in this Bone manner provide a range of Blood several CT numbers for 1% change in attenuation coefficient. Gray matter μ(cm-1) 0. 528 0. 208 0. 212 White matter 0. 213 CSF Water Fat Air 0. 207 0. 206 0. 185 0. 0004 Linear attenuation coefficient of various body tissues for 60 ke. V x-ray
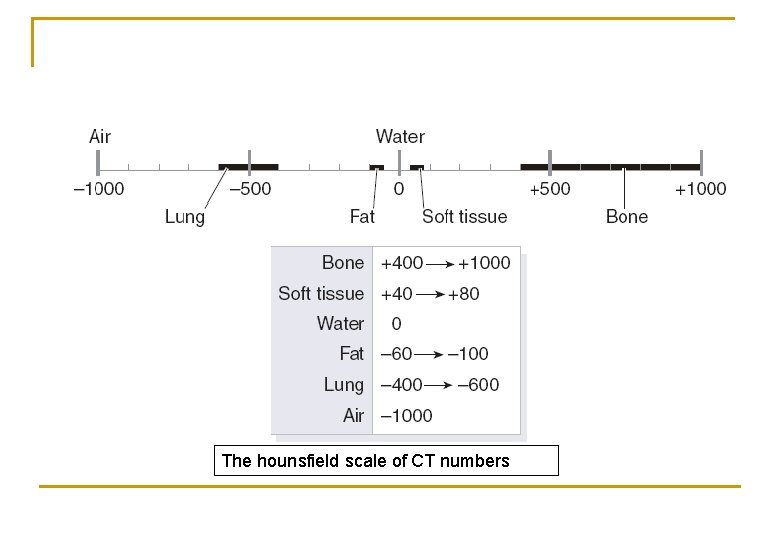
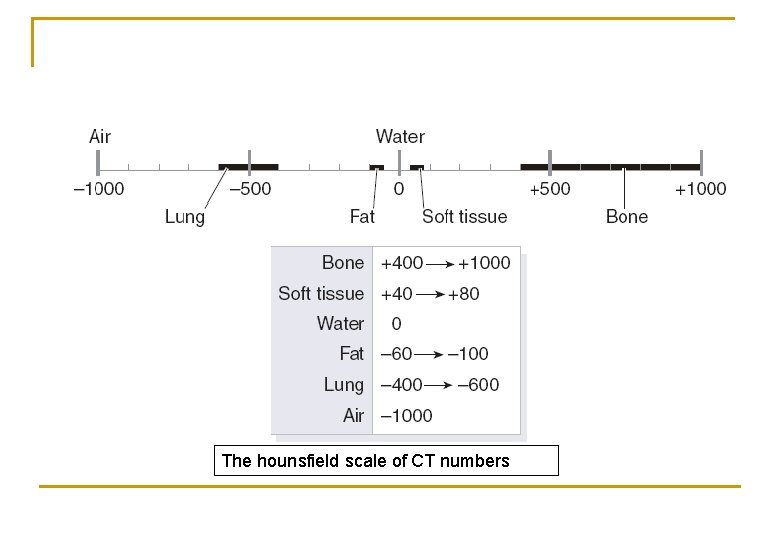
The hounsfield scale of CT numbers

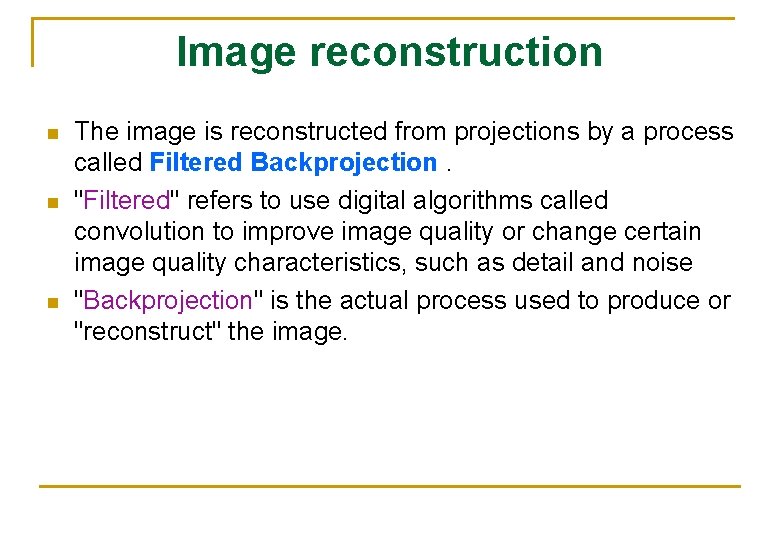
Image reconstruction
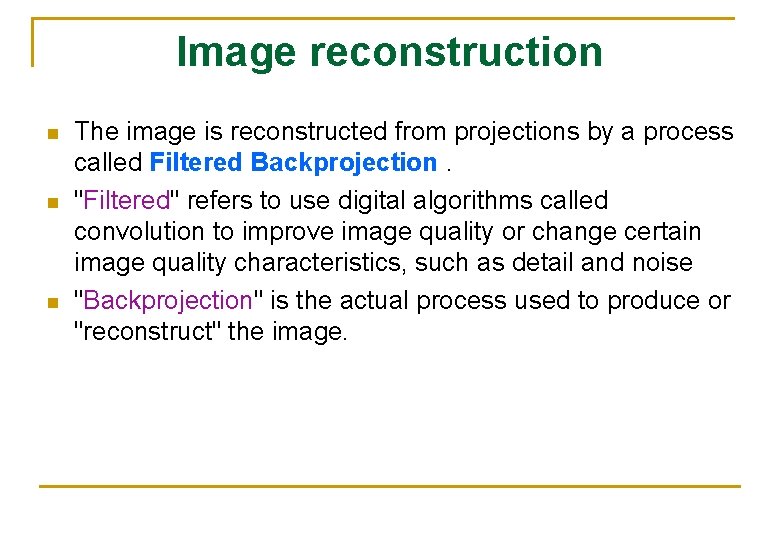
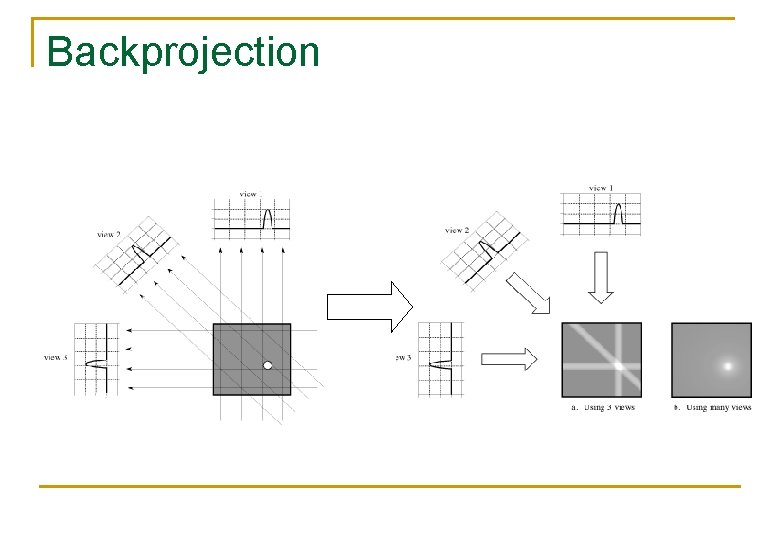
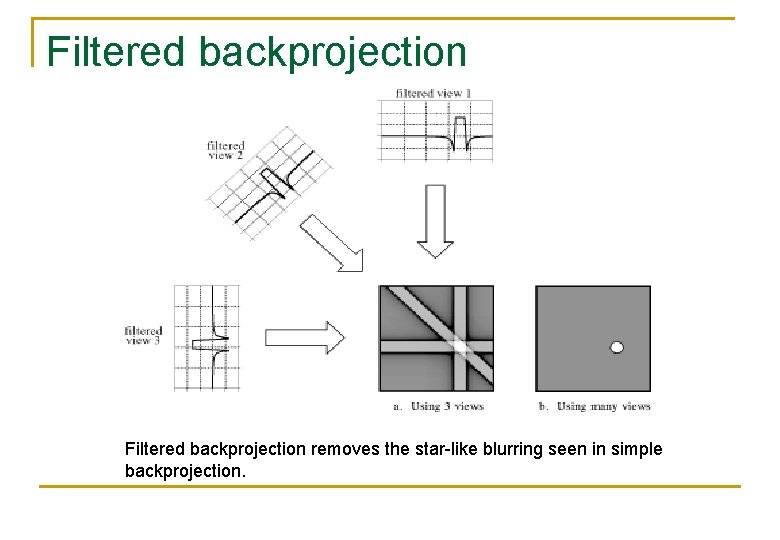
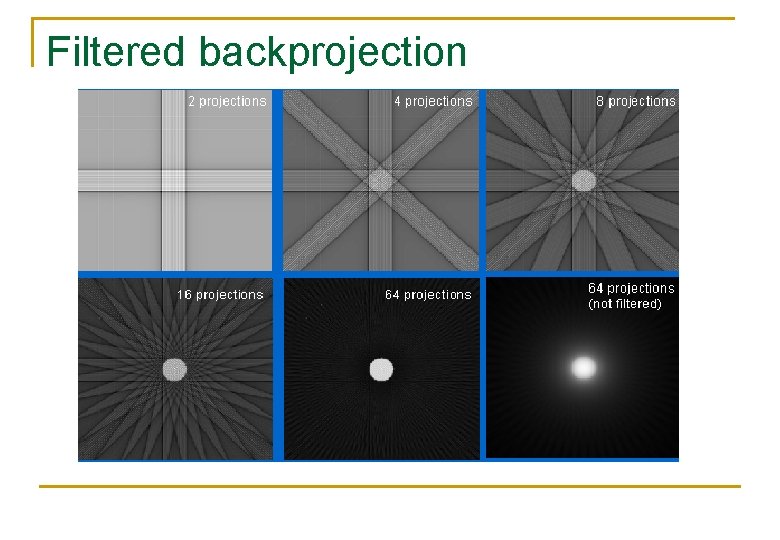
Image reconstruction n The image is reconstructed from projections by a process called Filtered Backprojection. "Filtered" refers to use digital algorithms called convolution to improve image quality or change certain image quality characteristics, such as detail and noise "Backprojection" is the actual process used to produce or "reconstruct" the image.
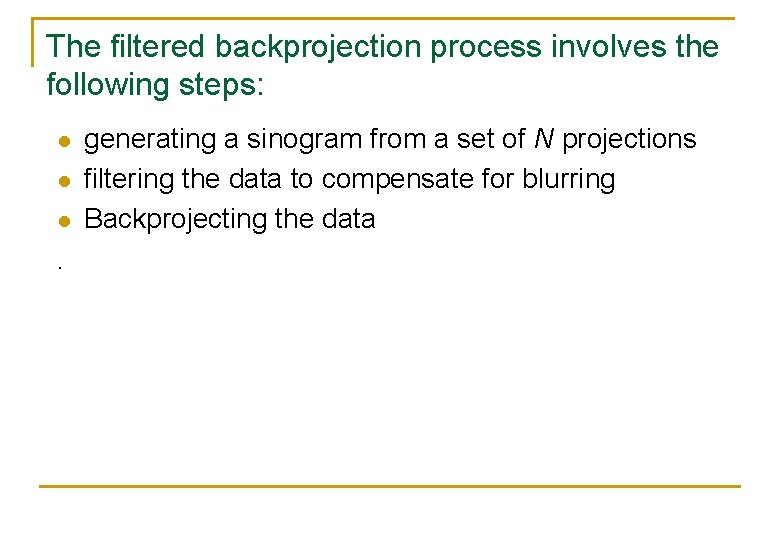
The filtered backprojection process involves the following steps: l l l . generating a sinogram from a set of N projections filtering the data to compensate for blurring Backprojecting the data
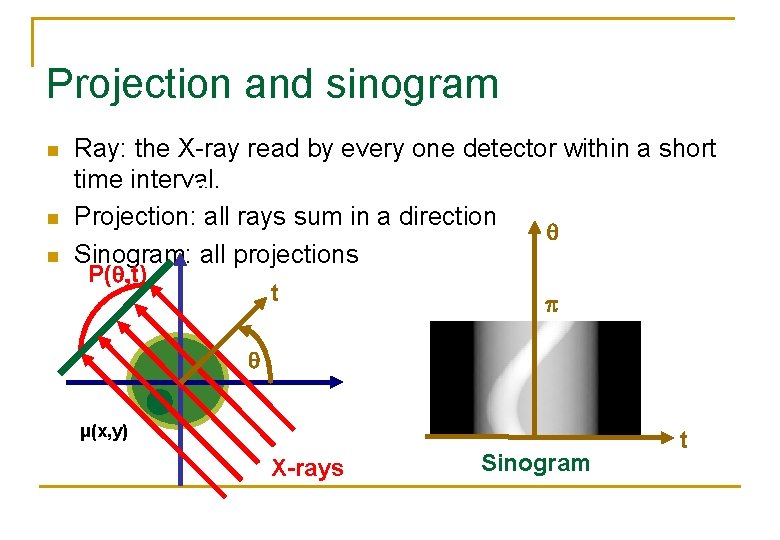
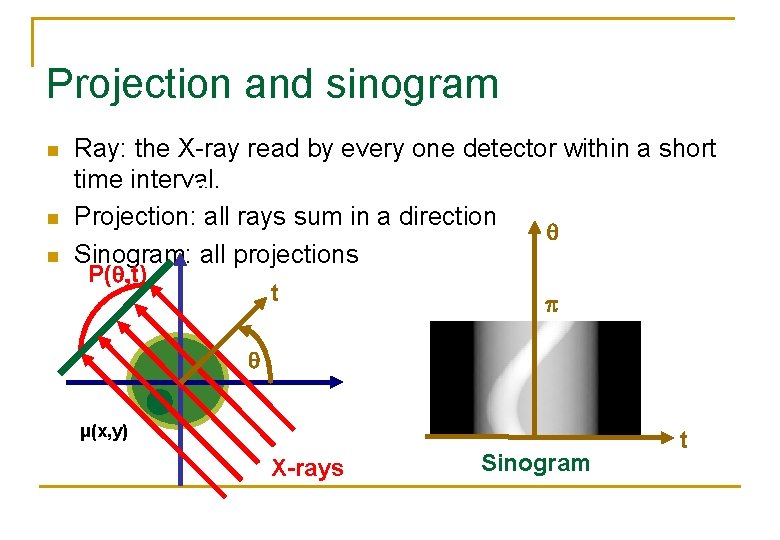
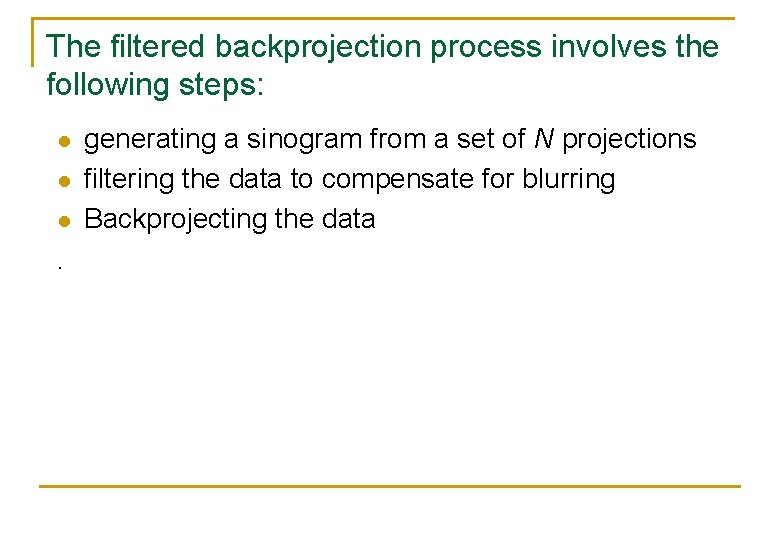
Projection and sinogram n n n Ray: the X-ray read by every one detector within a short time interval. y Projection: all rays sum in a direction Sinogram: all projections P( t) t p x μ(x, y) X-rays Sinogram t
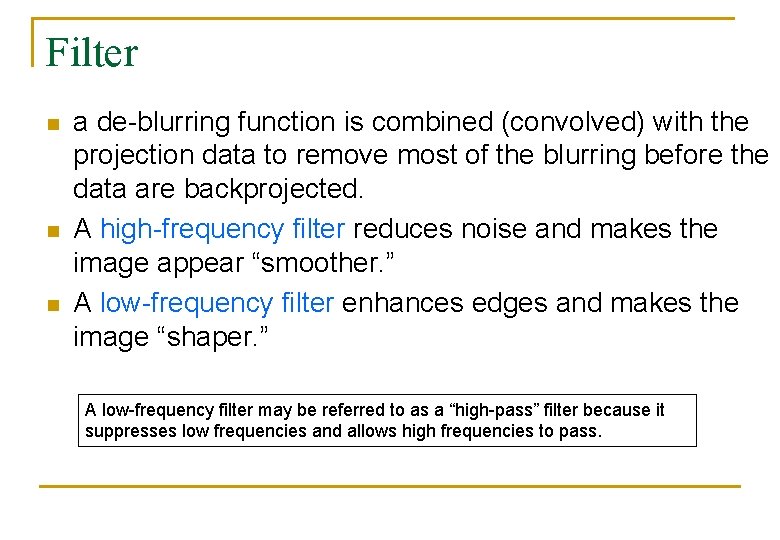
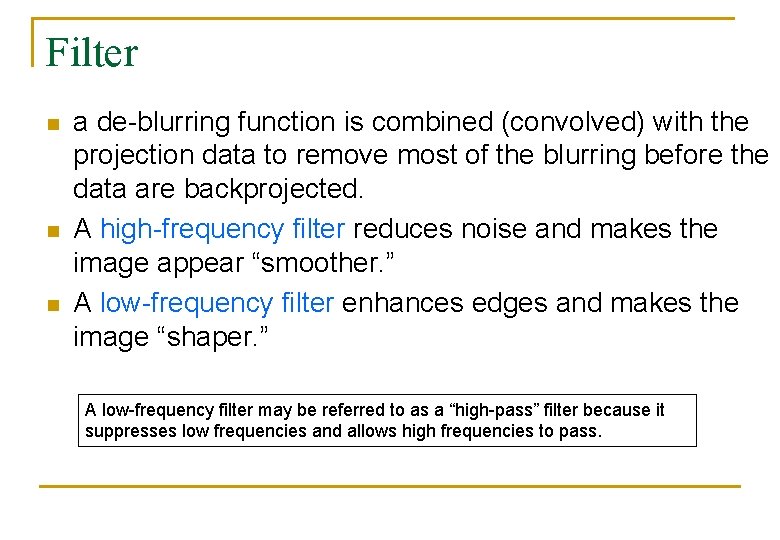
Filter n n n a de-blurring function is combined (convolved) with the projection data to remove most of the blurring before the data are backprojected. A high-frequency filter reduces noise and makes the image appear “smoother. ” A low-frequency filter enhances edges and makes the image “shaper. ” A low-frequency filter may be referred to as a “high-pass” filter because it suppresses low frequencies and allows high frequencies to pass.
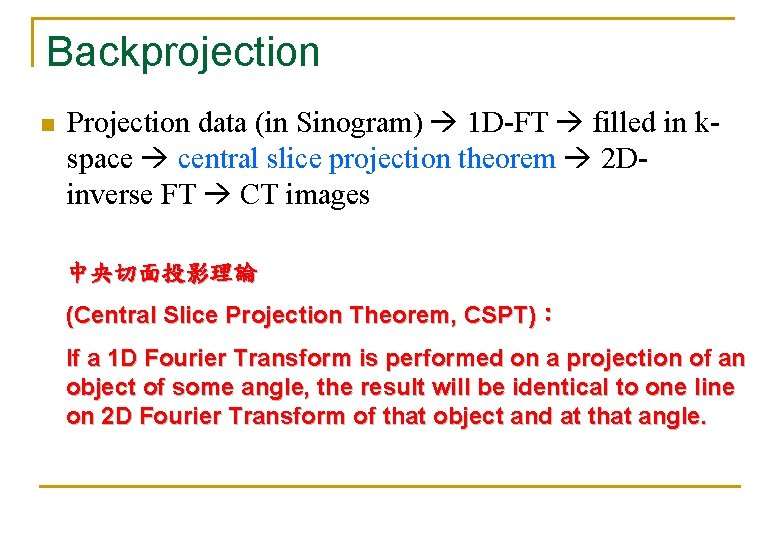
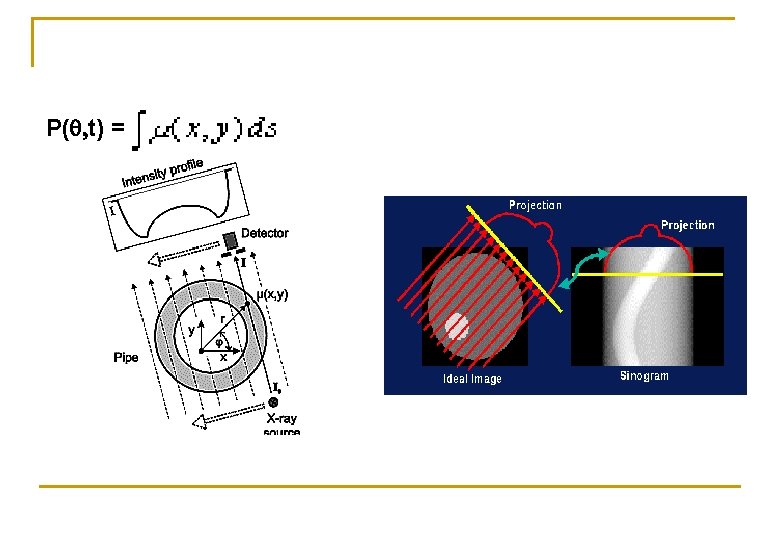
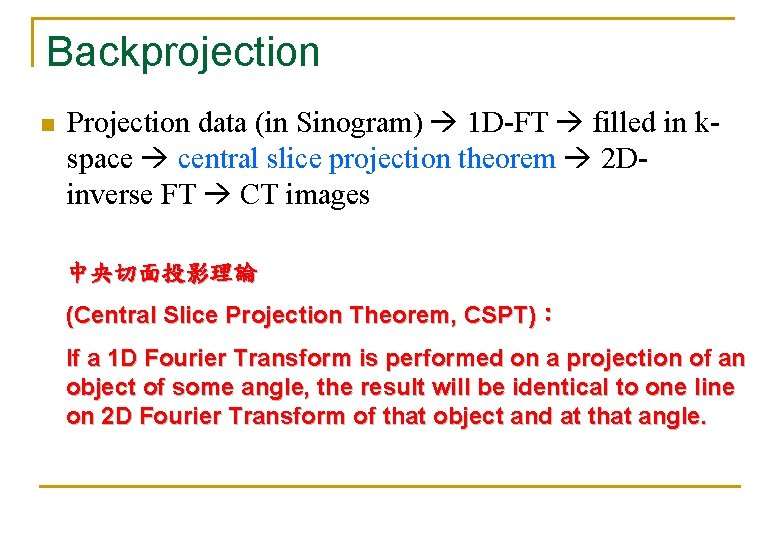
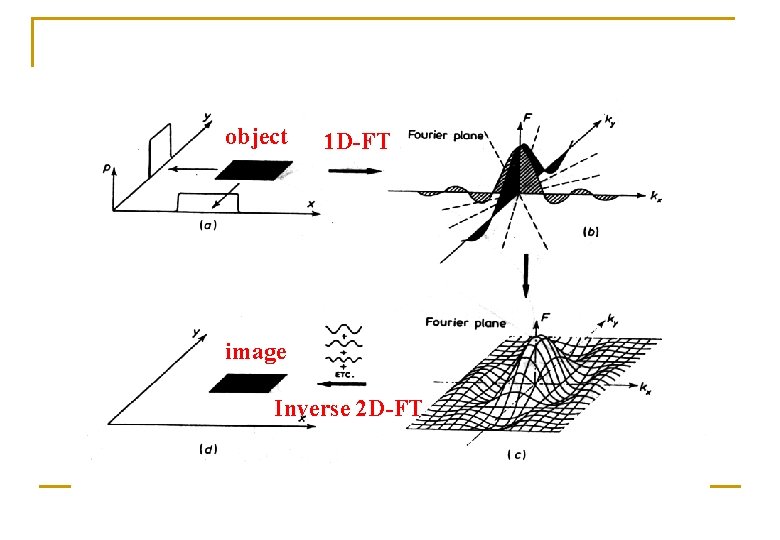
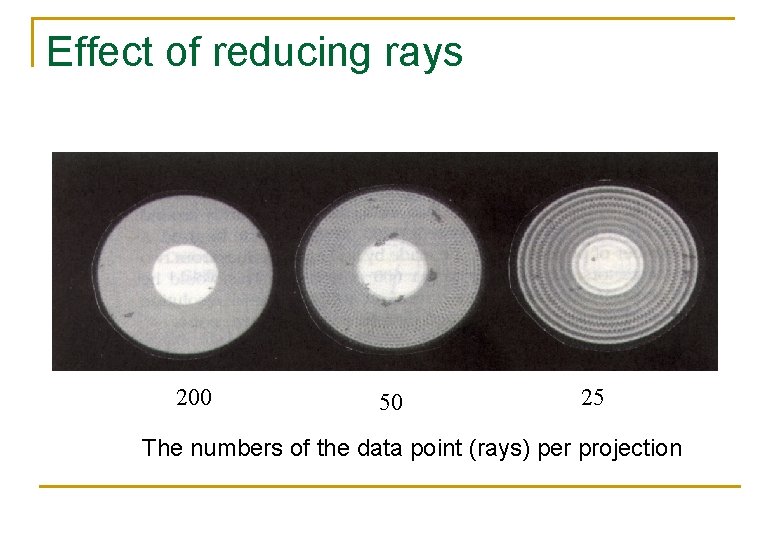
Backprojection n Projection data (in Sinogram) 1 D-FT filled in kspace central slice projection theorem 2 Dinverse FT CT images 中央切面投影理論 (Central Slice Projection Theorem, CSPT): If a 1 D Fourier Transform is performed on a projection of an object of some angle, the result will be identical to one line on 2 D Fourier Transform of that object and at that angle.
![Central Slice Projection Theorem P t ky y t μx y FP t x Central Slice Projection Theorem P( t) ky y t μ(x, y) F[P( t)] x](https://slidetodoc.com/presentation_image_h/b8767626d578b1cc80a05af9e3c10543/image-38.jpg)
Central Slice Projection Theorem P( t) ky y t μ(x, y) F[P( t)] x F(kx, ky) CSPT can relate the Fourier transform of the projection to one line in the 2 D K space formed by the 2 D Fourier transform of μ(x, y) kx
![y ky F1Fkx ky v x ux y u Fkx ky Inverse 2 DFT y ky F-1[F(kx, ky)] v x u(x, y) u F(kx, ky) Inverse 2 D-FT](https://slidetodoc.com/presentation_image_h/b8767626d578b1cc80a05af9e3c10543/image-39.jpg)
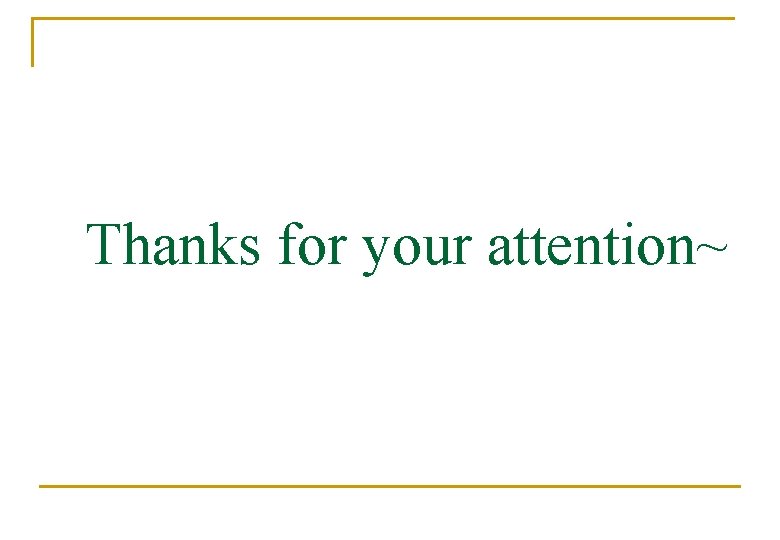
y ky F-1[F(kx, ky)] v x u(x, y) u F(kx, ky) Inverse 2 D-FT kx
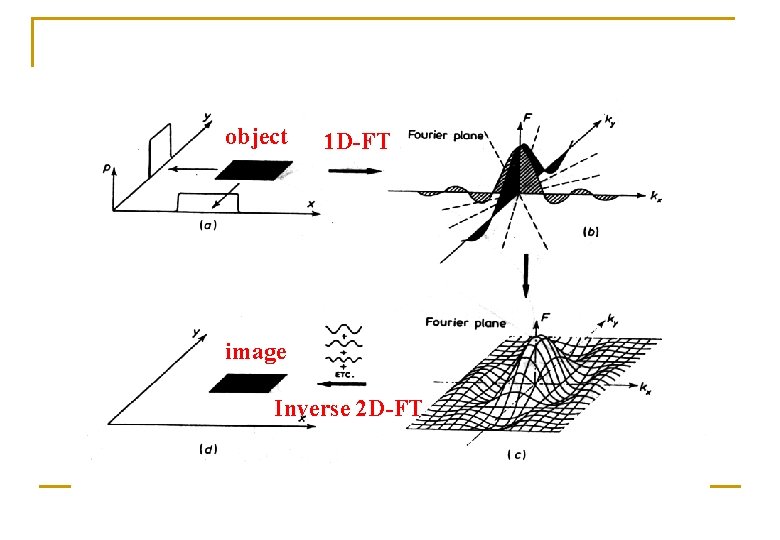
object 1 D-FT image Inverse 2 D-FT
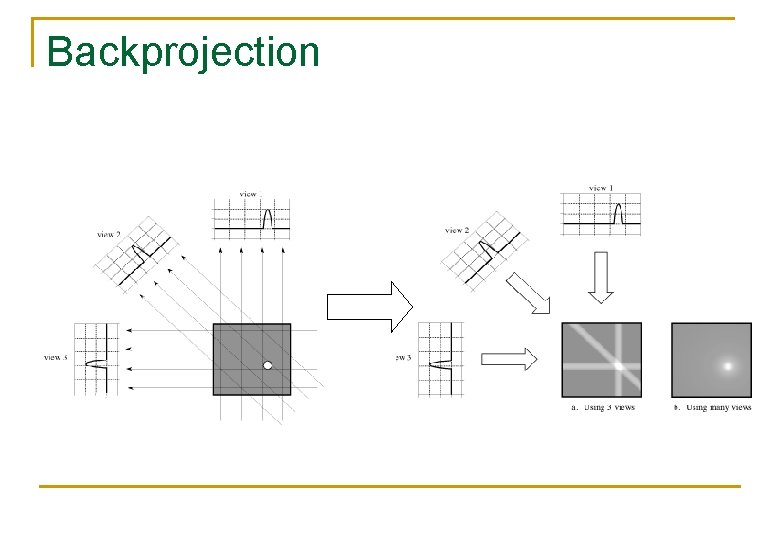
Backprojection
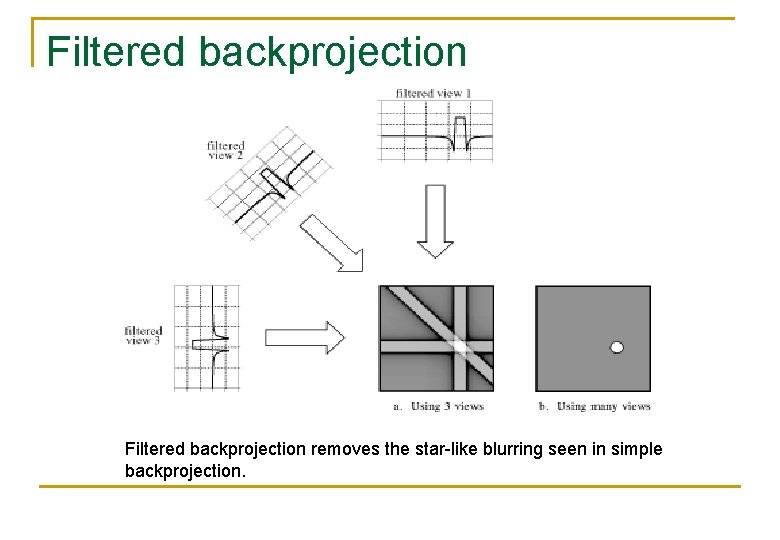
Filtered backprojection removes the star-like blurring seen in simple backprojection.
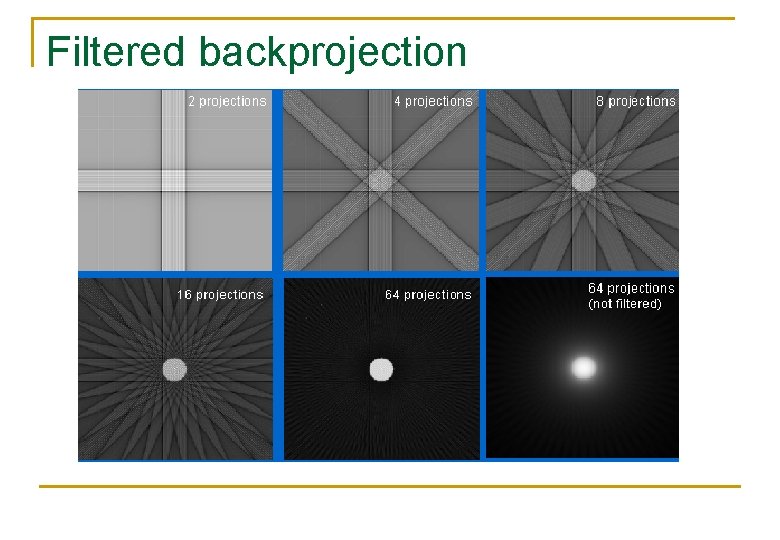
Filtered backprojection
Image display
Image manipulation n Image manipulation belongs to the domain of digital image processing.
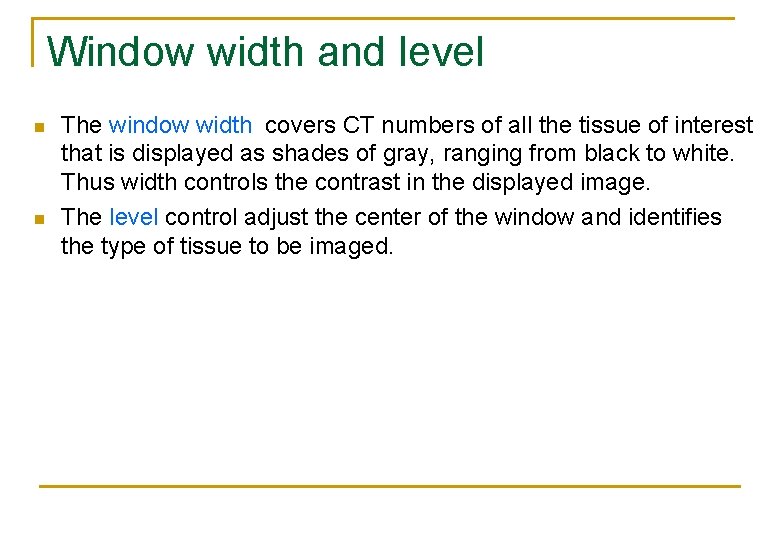
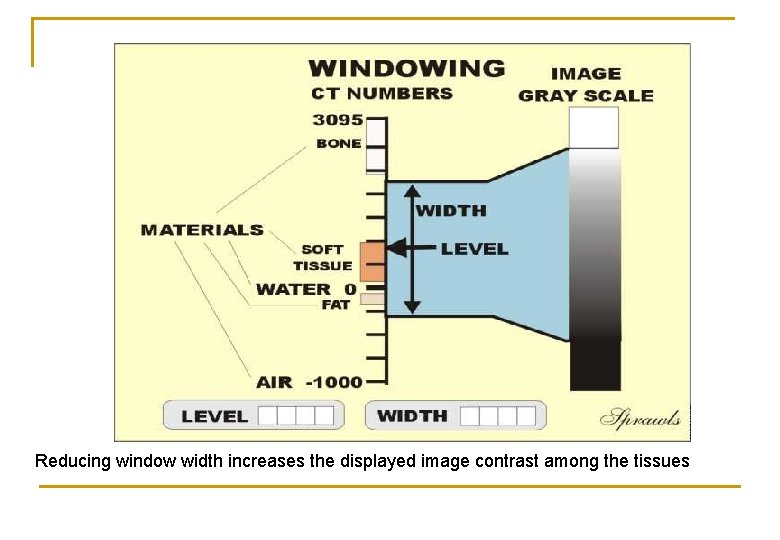
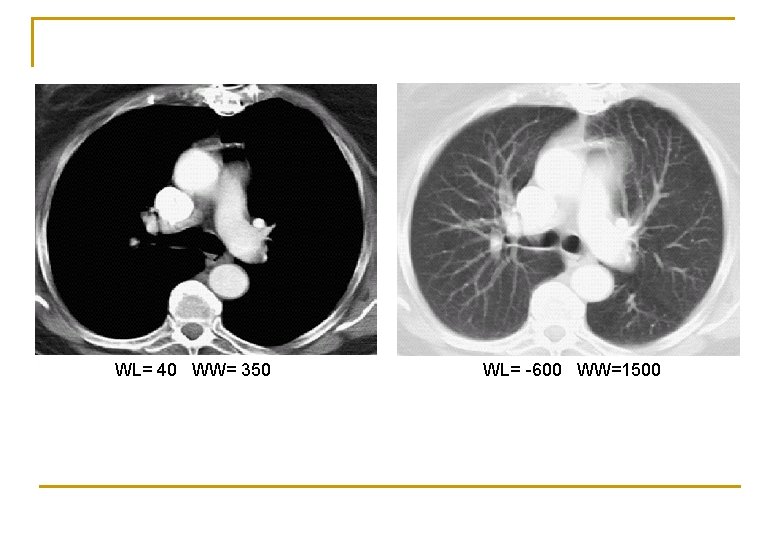
Window width and level n n The window width covers CT numbers of all the tissue of interest that is displayed as shades of gray, ranging from black to white. Thus width controls the contrast in the displayed image. The level control adjust the center of the window and identifies the type of tissue to be imaged.
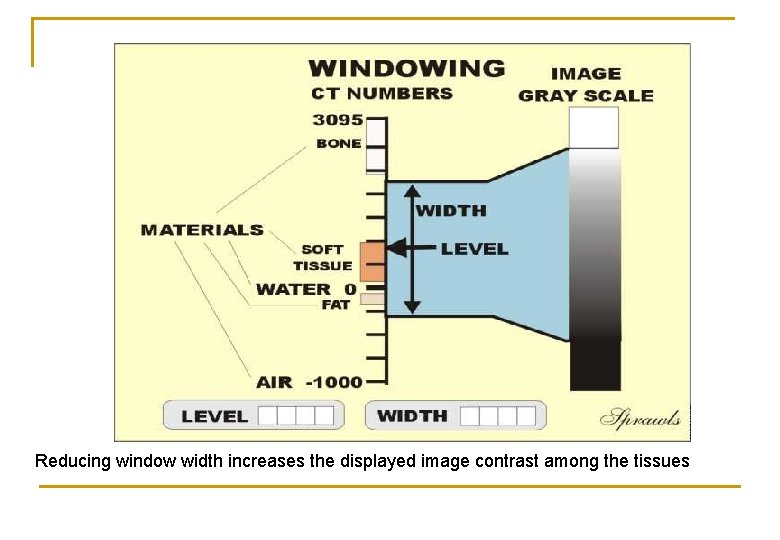
Reducing window width increases the displayed image contrast among the tissues
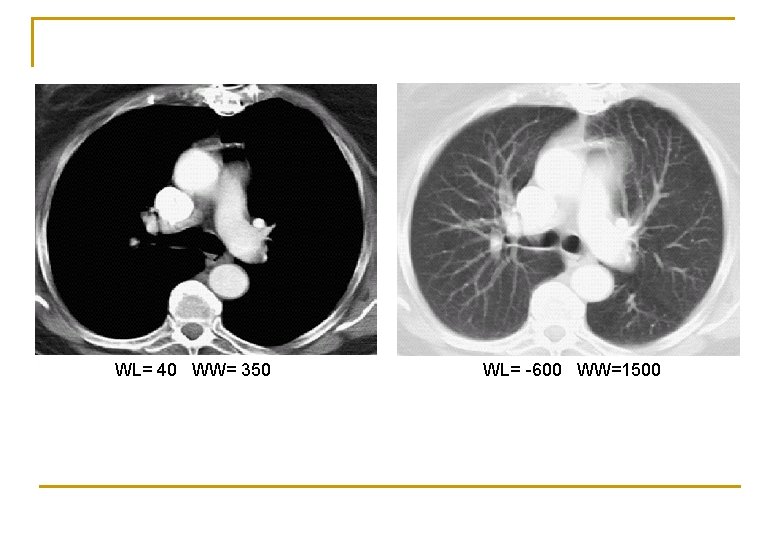
WL= 40 WW= 350 WL= -600 WW=1500
Spiral CT technology
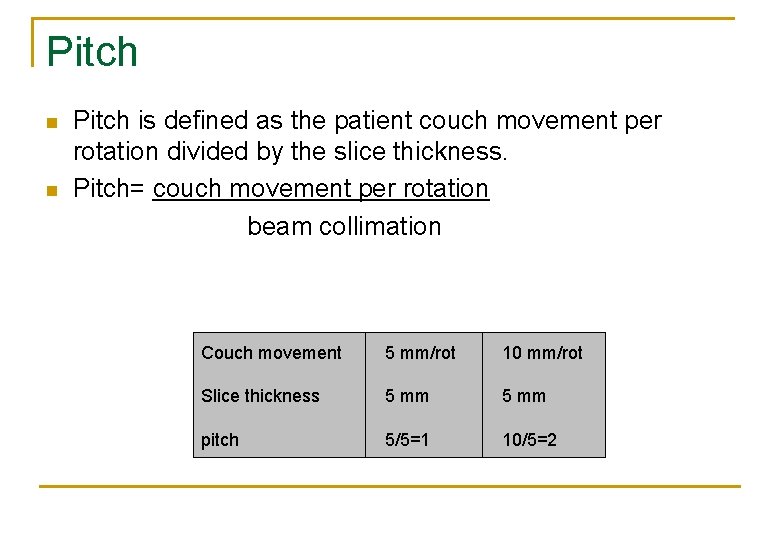
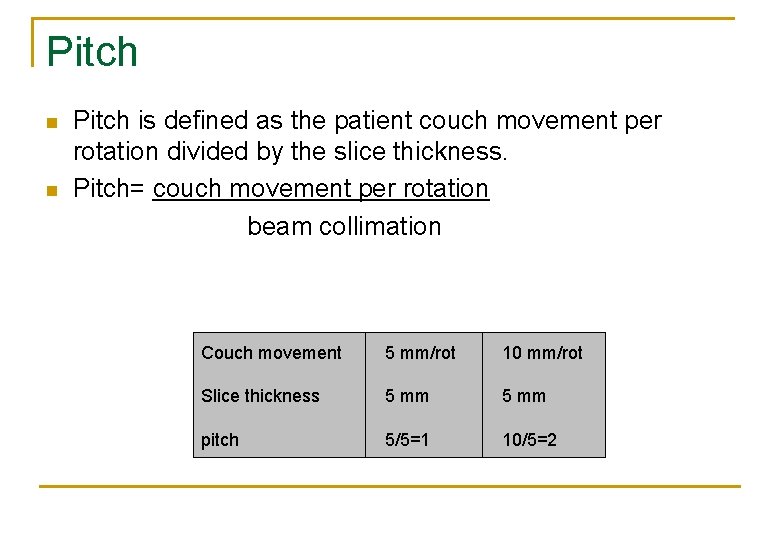
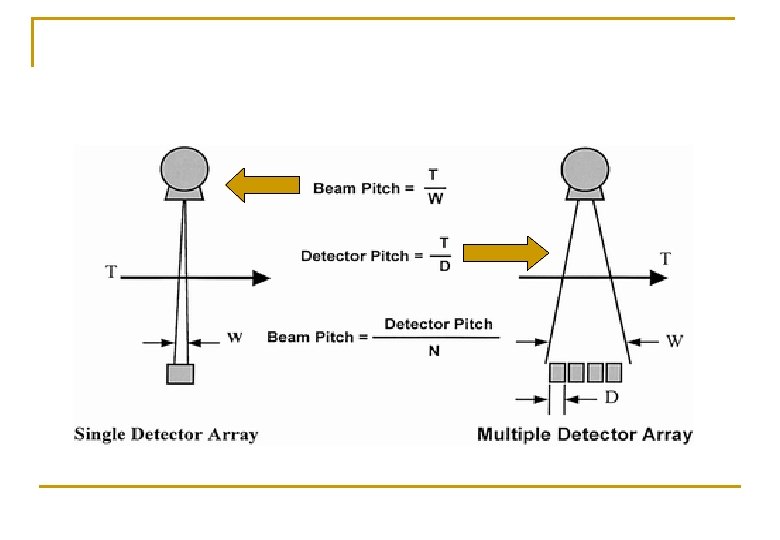
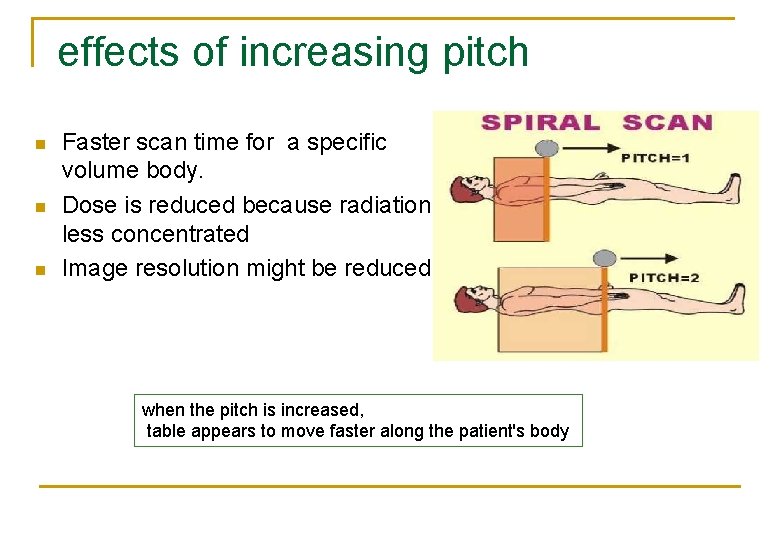
Pitch is defined as the patient couch movement per rotation divided by the slice thickness. n Pitch= couch movement per rotation beam collimation n Couch movement 5 mm/rot 10 mm/rot Slice thickness 5 mm pitch 5/5=1 10/5=2
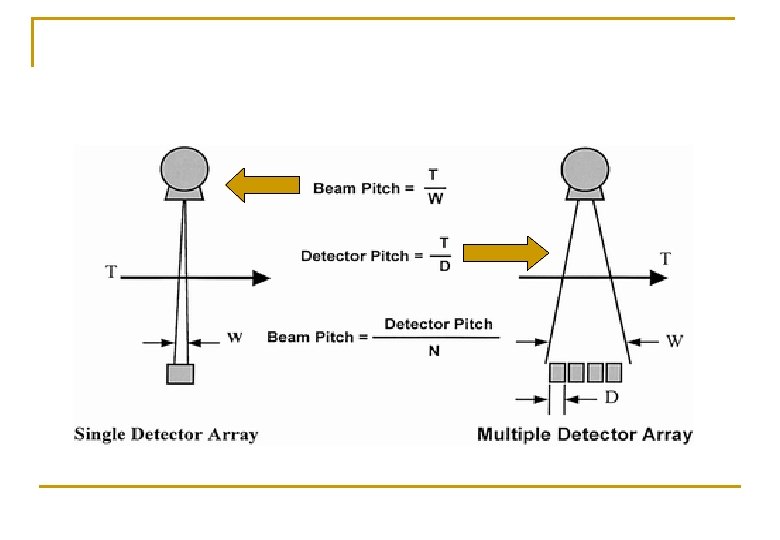
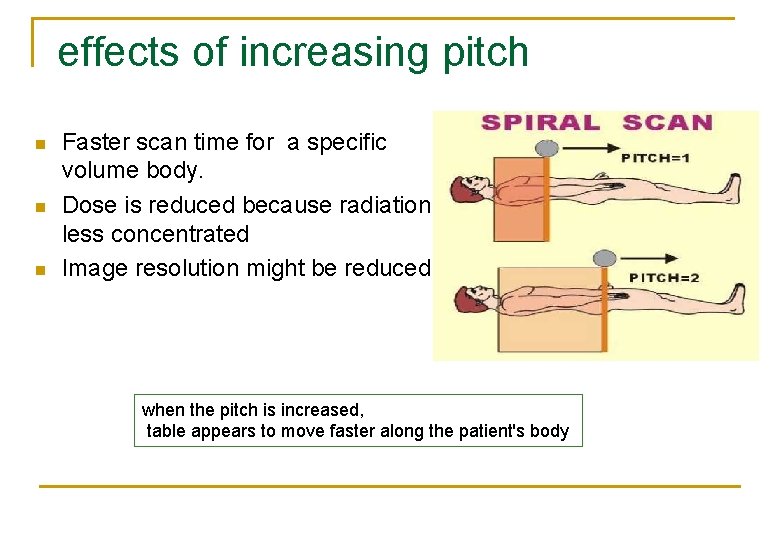
effects of increasing pitch n n n Faster scan time for a specific volume body. Dose is reduced because radiation is less concentrated Image resolution might be reduced when the pitch is increased, table appears to move faster along the patient's body
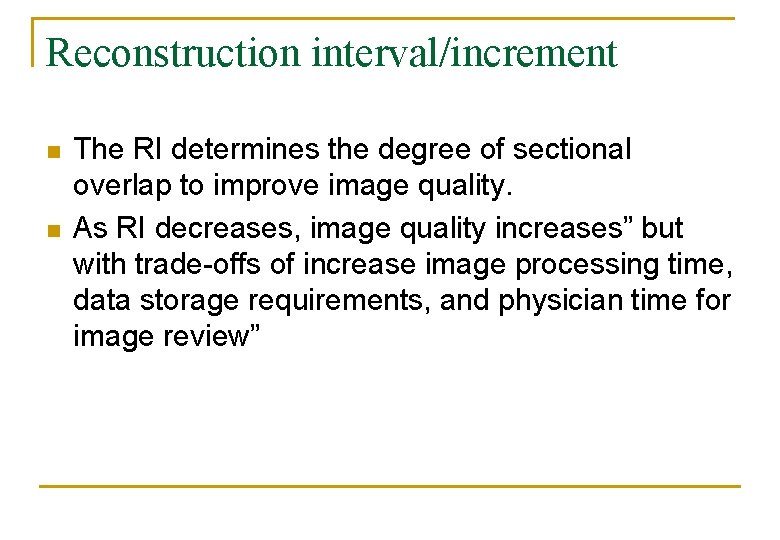
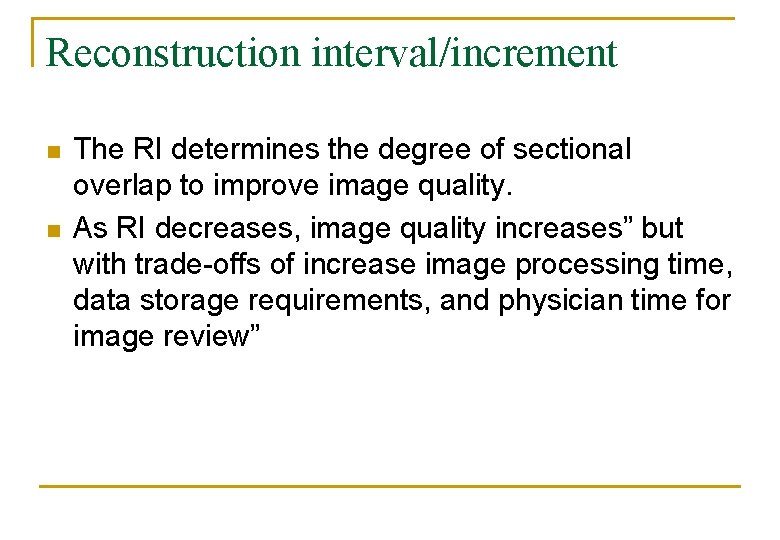
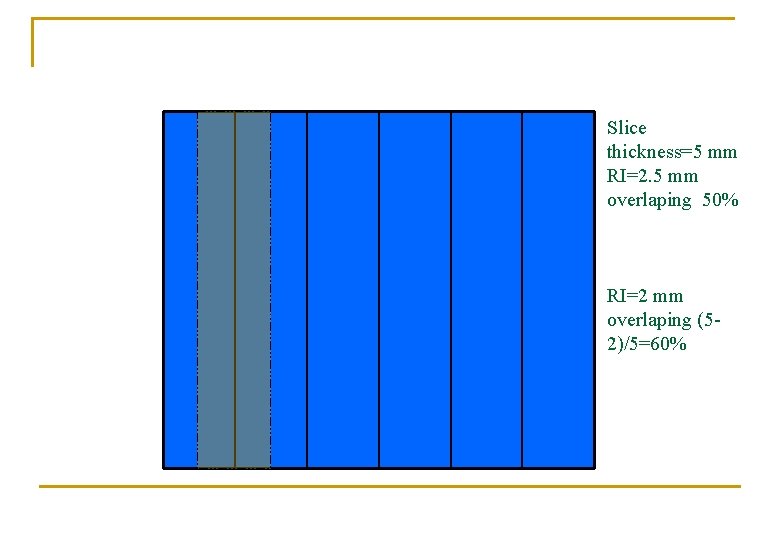
Reconstruction interval/increment n n The RI determines the degree of sectional overlap to improve image quality. As RI decreases, image quality increases” but with trade-offs of increase image processing time, data storage requirements, and physician time for image review”
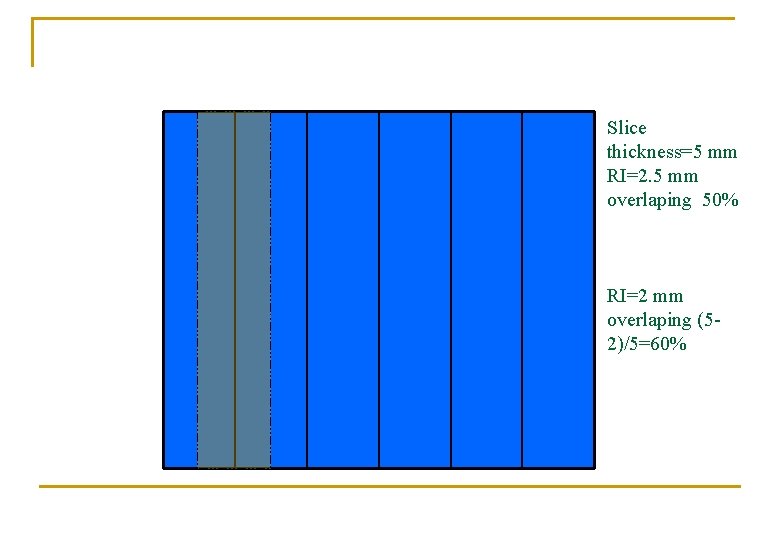
Slice thickness=5 mm RI=2. 5 mm overlaping 50% RI=2 mm overlaping (52)/5=60%
Image quality
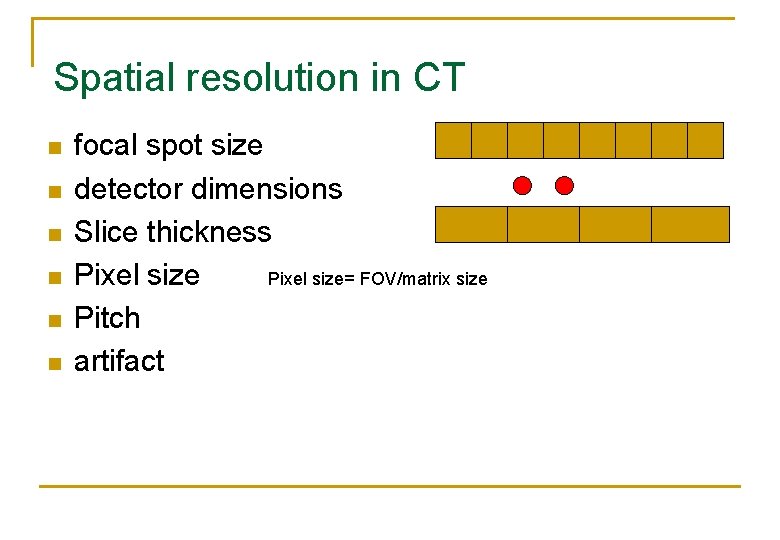
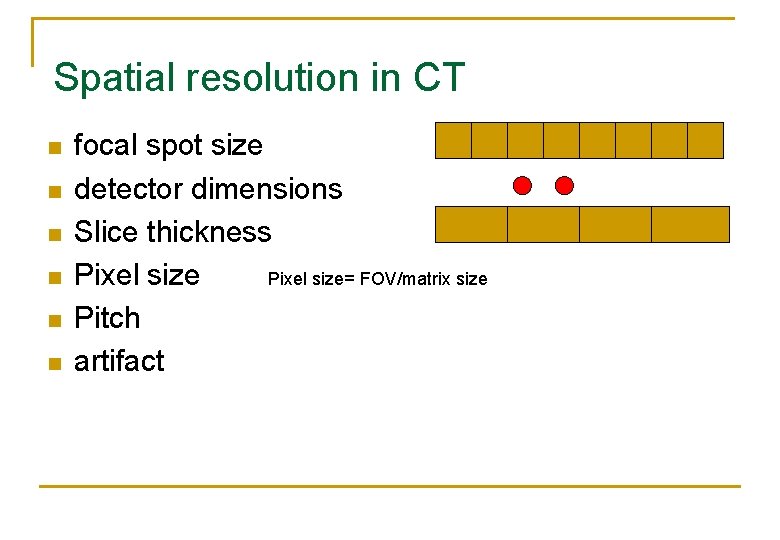
Spatial resolution in CT n n n focal spot size detector dimensions Slice thickness Pixel size= FOV/matrix size Pitch artifact
Image Artifact in CT
Image Artifact n n Artifacts are any discrepancy between the CT numbers represented in the image and the expected CT numbers Common artifacts Beam hardening l Partial volume effect l bad detector(3 th scanner) l Metal l Patient motion l
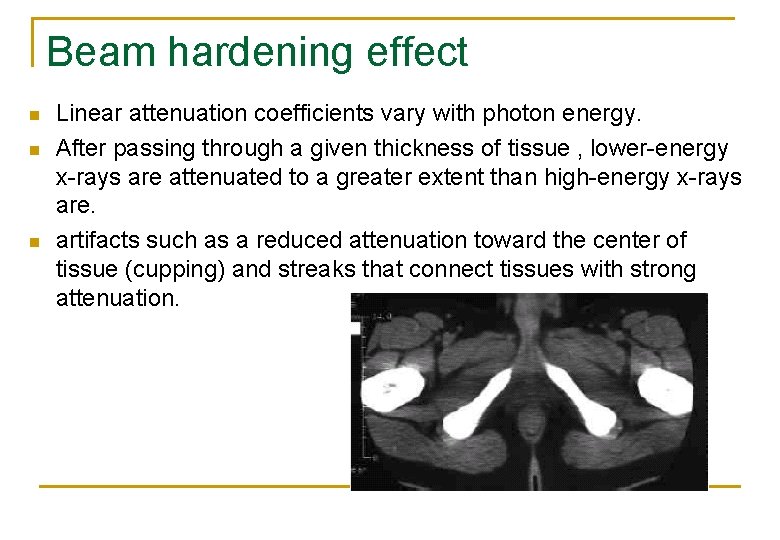
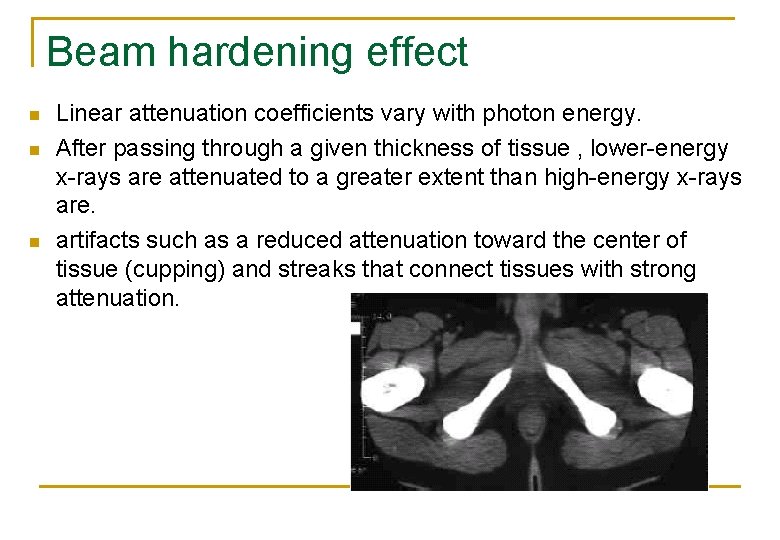
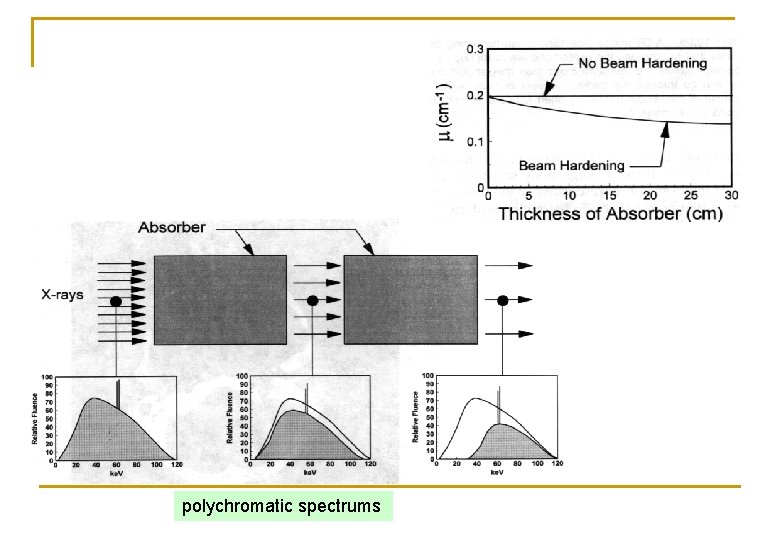
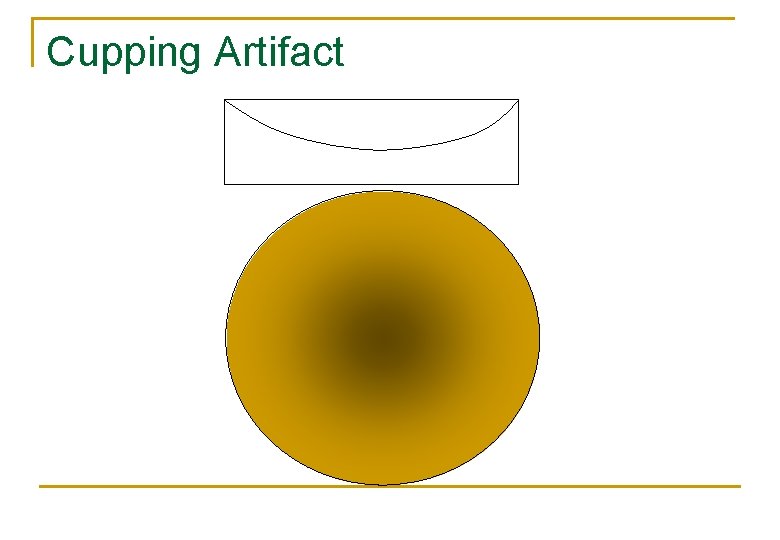
Beam hardening effect n n n Linear attenuation coefficients vary with photon energy. After passing through a given thickness of tissue , lower-energy x-rays are attenuated to a greater extent than high-energy x-rays are. artifacts such as a reduced attenuation toward the center of tissue (cupping) and streaks that connect tissues with strong attenuation.
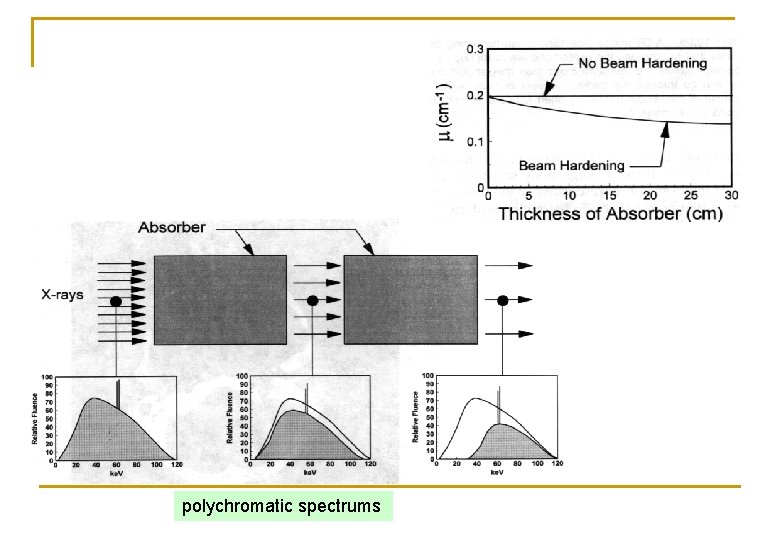
polychromatic spectrums
Cupping Artifact
Means for suppressing beam hardening effect n n n pre-filtering X-rays avoiding high X-ray absorbing regions if possible applying appropriate algorithms
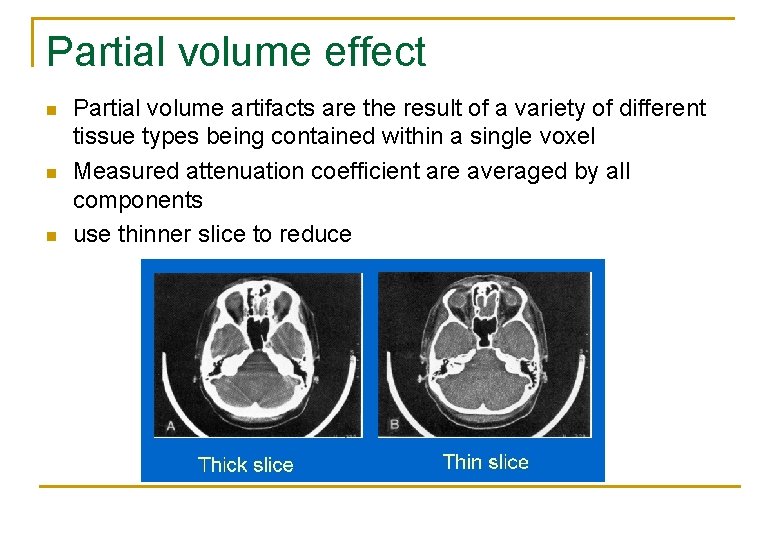
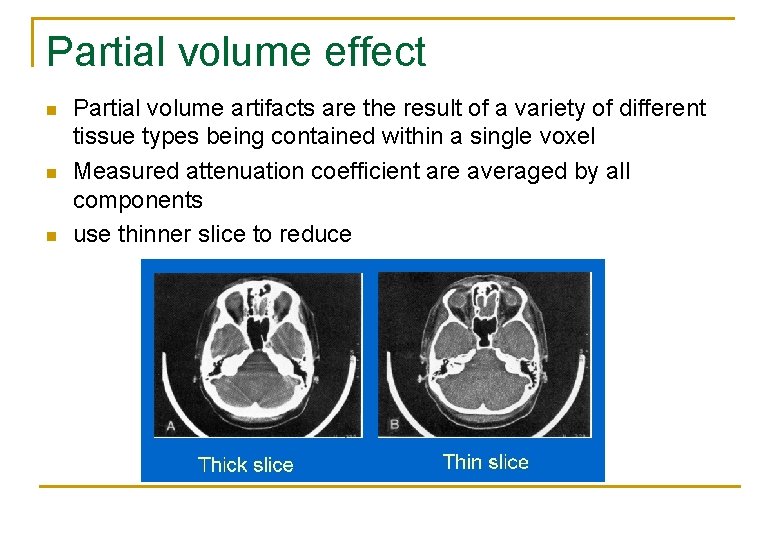
Partial volume effect n n n Partial volume artifacts are the result of a variety of different tissue types being contained within a single voxel Measured attenuation coefficient are averaged by all components use thinner slice to reduce
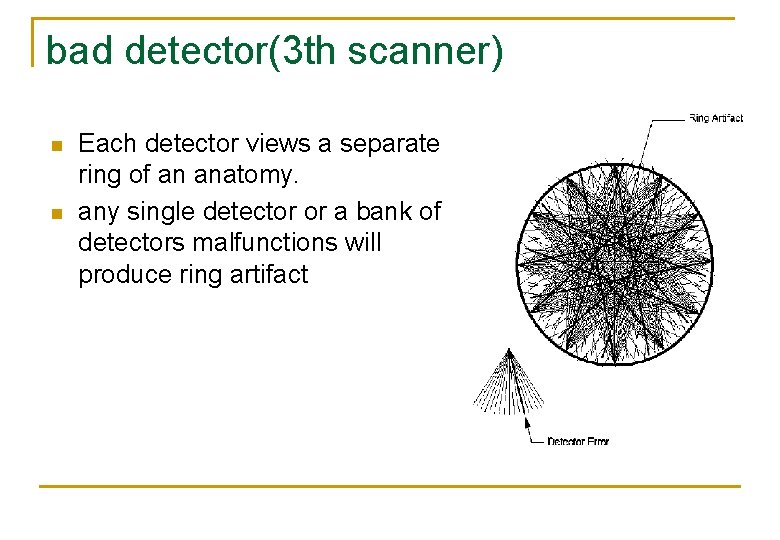
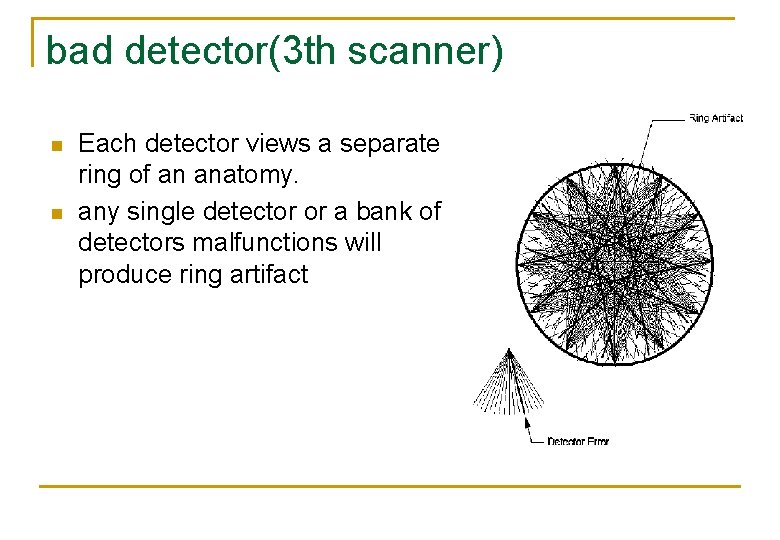
bad detector(3 th scanner) n n Each detector views a separate ring of an anatomy. any single detector or a bank of detectors malfunctions will produce ring artifact
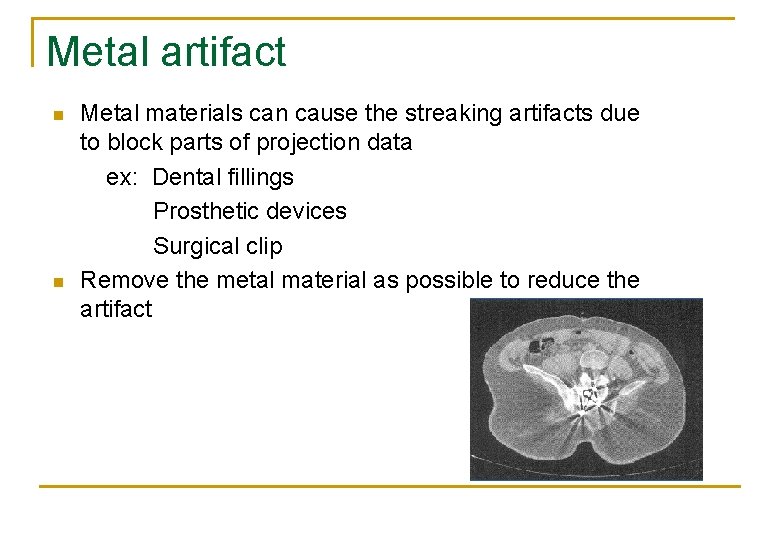
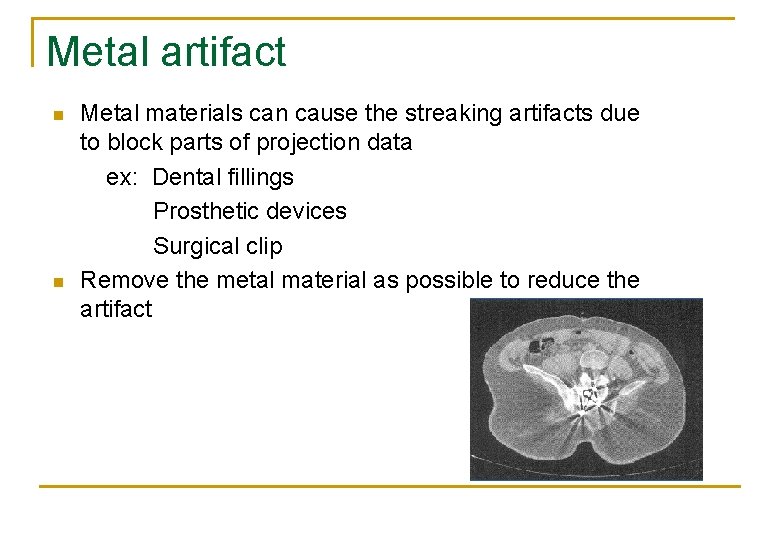
Metal artifact Metal materials can cause the streaking artifacts due to block parts of projection data ex: Dental fillings Prosthetic devices Surgical clip n Remove the metal material as possible to reduce the artifact n
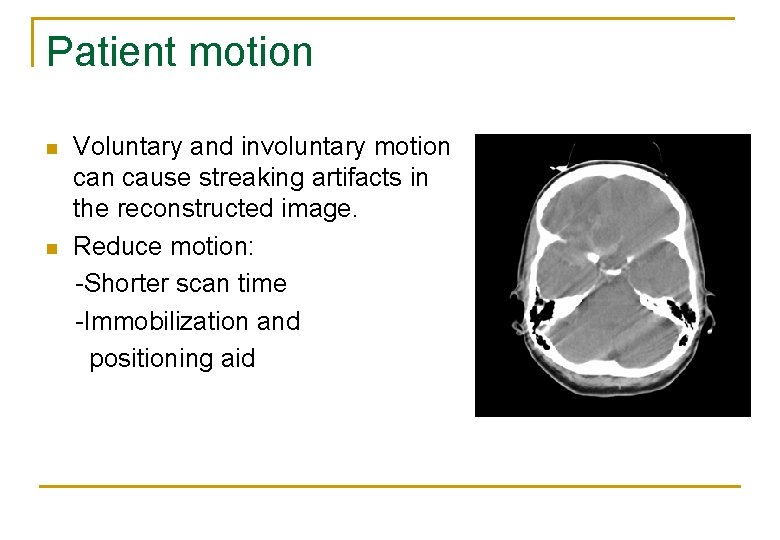
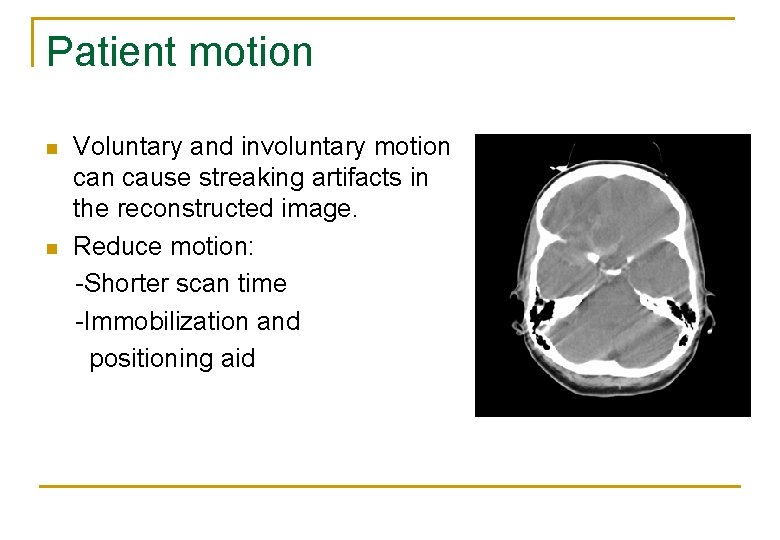
Patient motion Voluntary and involuntary motion cause streaking artifacts in the reconstructed image. n Reduce motion: -Shorter scan time -Immobilization and positioning aid n
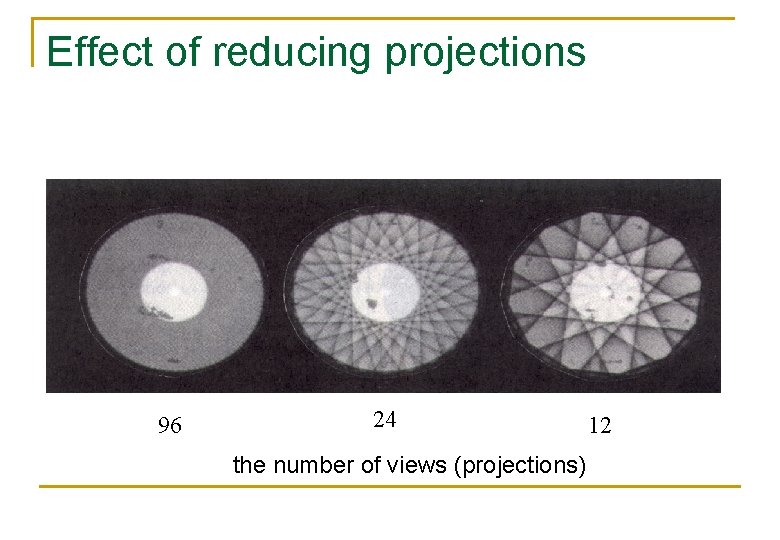
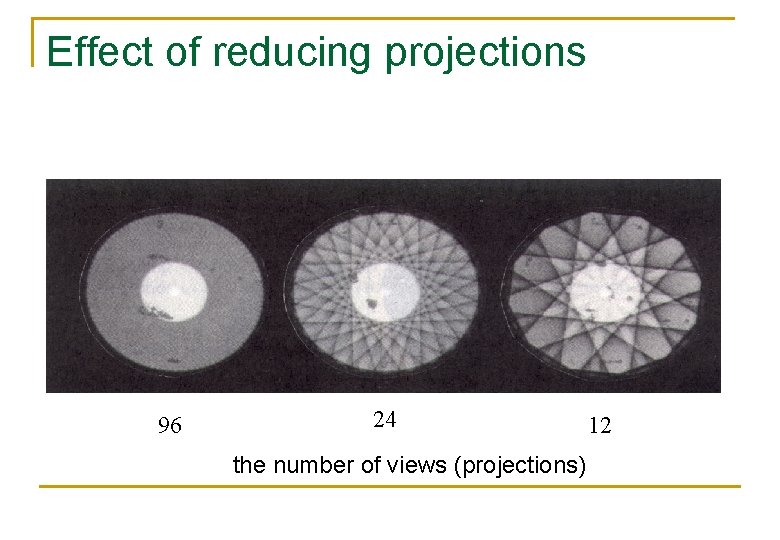
Effect of reducing projections 96 24 the number of views (projections) 12
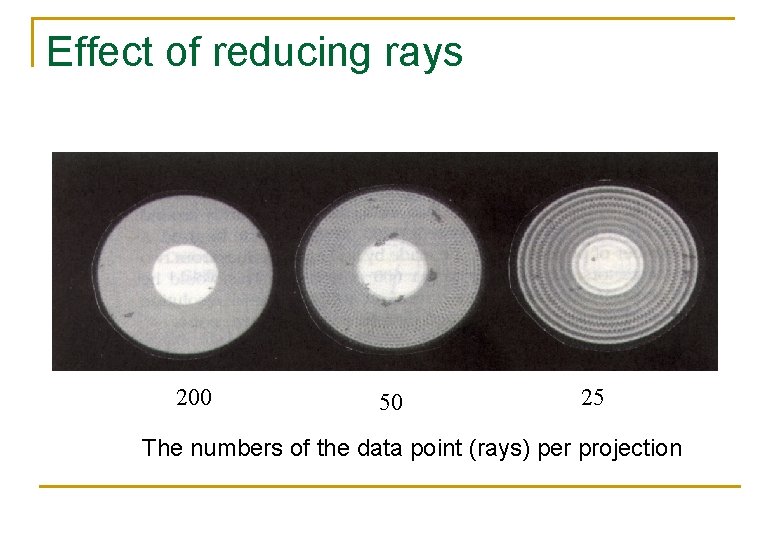
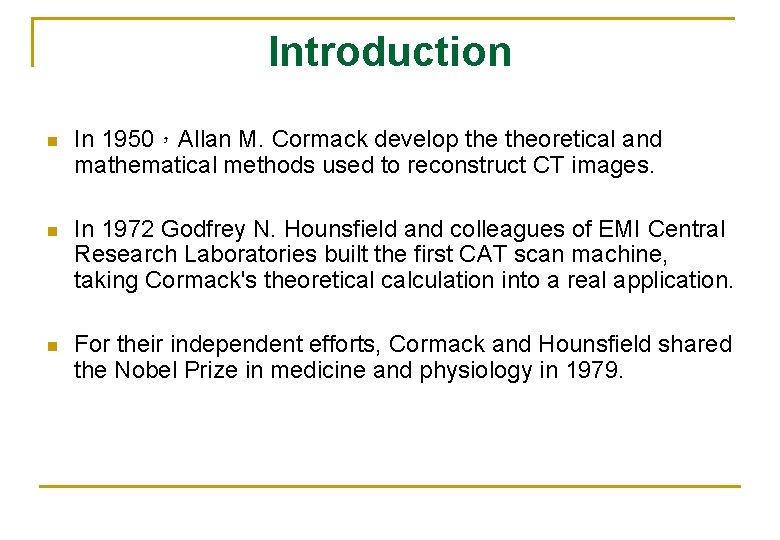
Effect of reducing rays 200 50 25 The numbers of the data point (rays) per projection
Thanks for your attention~