PRIME MY 13 Project Update Projects 2 7


- Slides: 44
PRIME MY 13 Project Update Project(s): 2. 7 Comprehensive Advanced Illness Planning & Care Metric(s): 2. 7. 1, 2. 7. 3 -2. 7. 6 PRIME Steering Committee Last Update: 12/15/2017 1

2
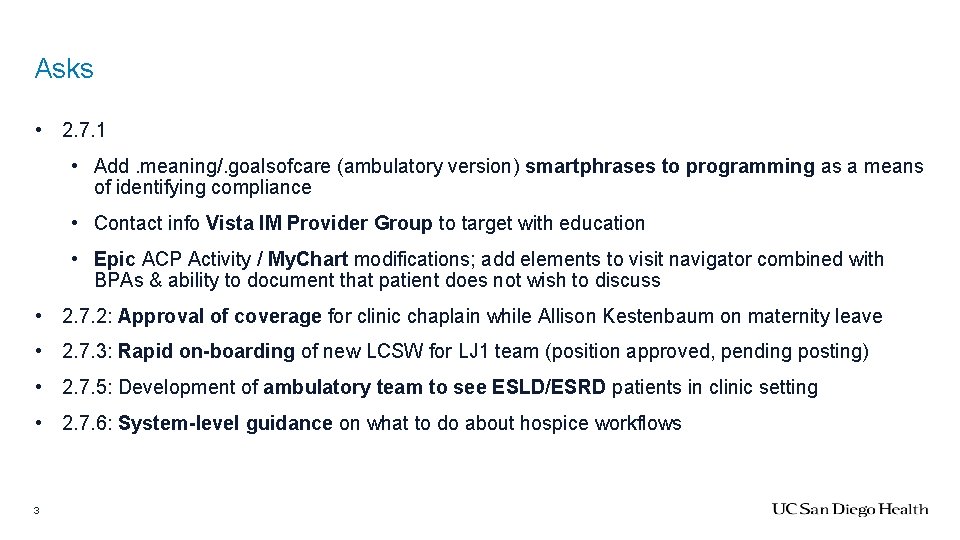
Asks • 2. 7. 1 • Add. meaning/. goalsofcare (ambulatory version) smartphrases to programming as a means of identifying compliance • Contact info Vista IM Provider Group to target with education • Epic ACP Activity / My. Chart modifications; add elements to visit navigator combined with BPAs & ability to document that patient does not wish to discuss • 2. 7. 2: Approval of coverage for clinic chaplain while Allison Kestenbaum on maternity leave • 2. 7. 3: Rapid on-boarding of new LCSW for LJ 1 team (position approved, pending posting) • 2. 7. 5: Development of ambulatory team to see ESLD/ESRD patients in clinic setting • 2. 7. 6: System-level guidance on what to do about hospice workflows 3
Challenges • Multiple sub-denominator populations of PRIME patients • Patients >65 yo (non-onc, outpt) • Seen by inpt palliative team (some onc, inpt) • Seen by outpt palliative team (all onc, outpt) • ESLD or ESRD (non-onc, mostly outpt) • Die with hospice services (mostly onc, outpt) • Goal of required projects = strengthen system-wide generalist palliative skills; metrics = very process-focused, shifting definitions, highly complex & time-consuming to capture 4
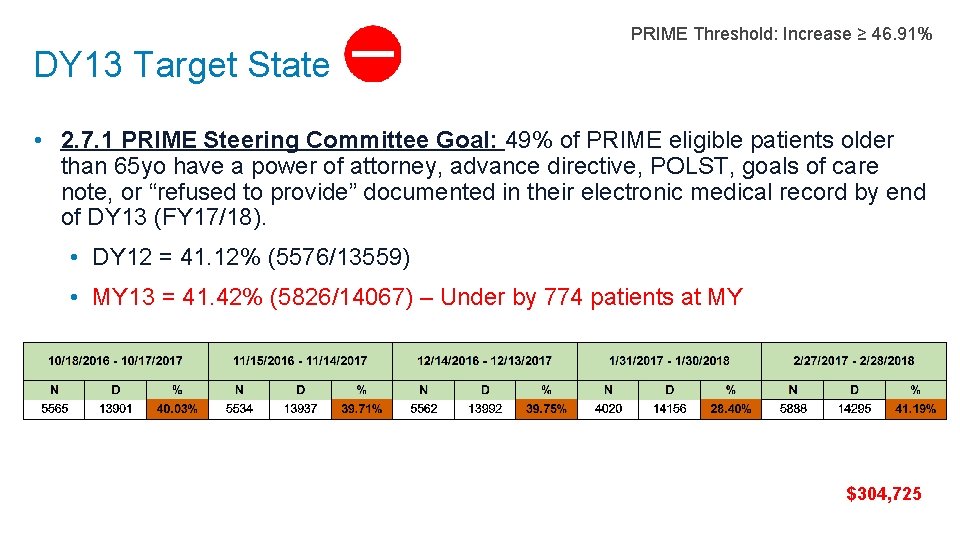
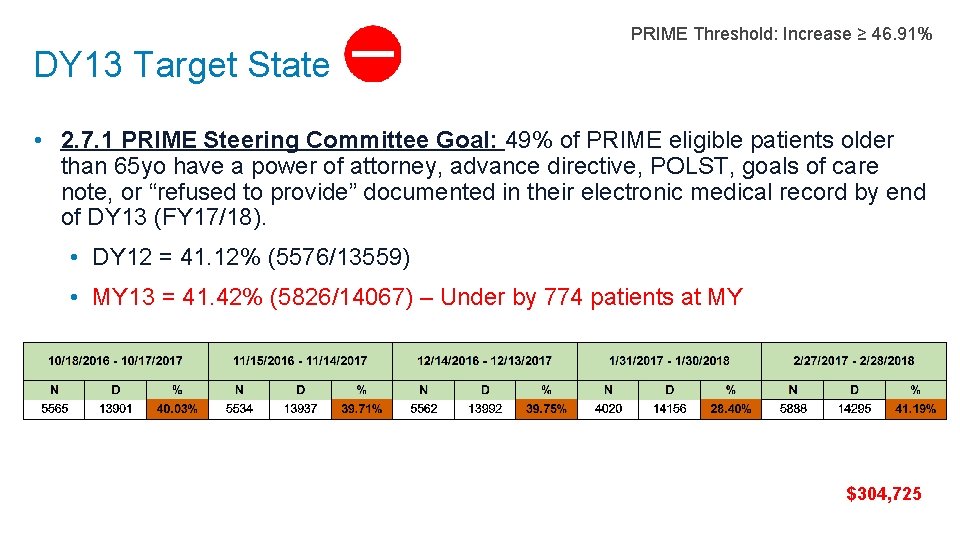
DY 13 Target State PRIME Threshold: Increase ≥ 46. 91% • 2. 7. 1 PRIME Steering Committee Goal: 49% of PRIME eligible patients older than 65 yo have a power of attorney, advance directive, POLST, goals of care note, or “refused to provide” documented in their electronic medical record by end of DY 13 (FY 17/18). • DY 12 = 41. 12% (5576/13559) • MY 13 = 41. 42% (5826/14067) – Under by 774 patients at MY $304, 725
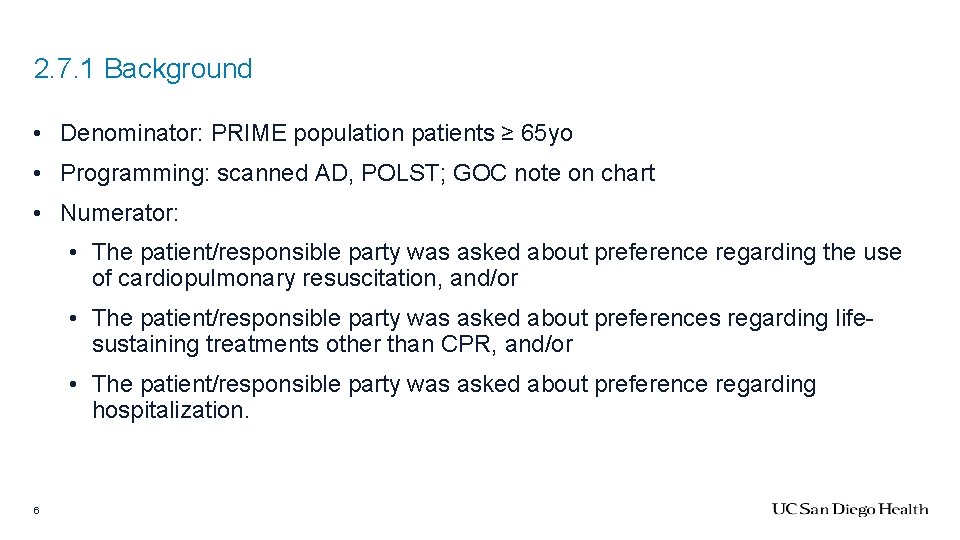
2. 7. 1 Background • Denominator: PRIME population patients ≥ 65 yo • Programming: scanned AD, POLST; GOC note on chart • Numerator: • The patient/responsible party was asked about preference regarding the use of cardiopulmonary resuscitation, and/or • The patient/responsible party was asked about preferences regarding lifesustaining treatments other than CPR, and/or • The patient/responsible party was asked about preference regarding hospitalization. 6
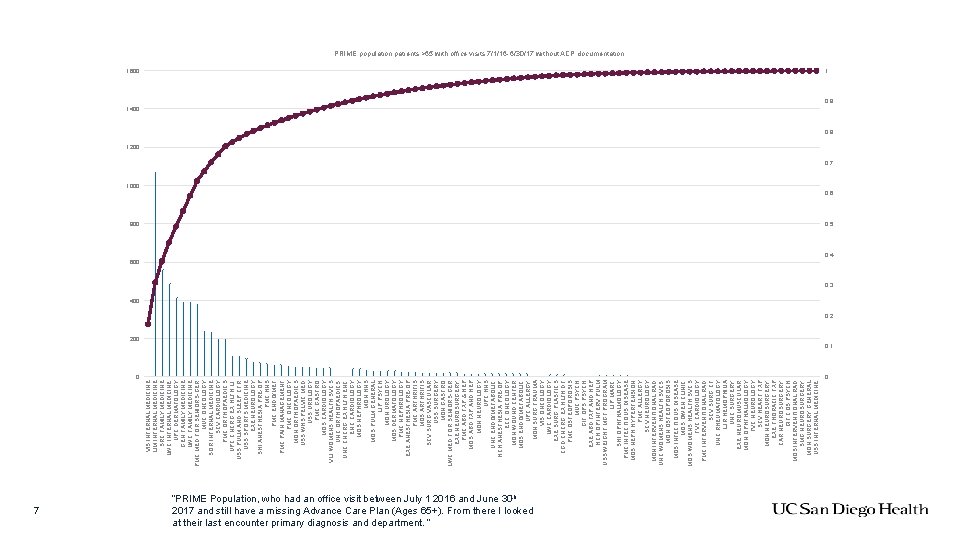
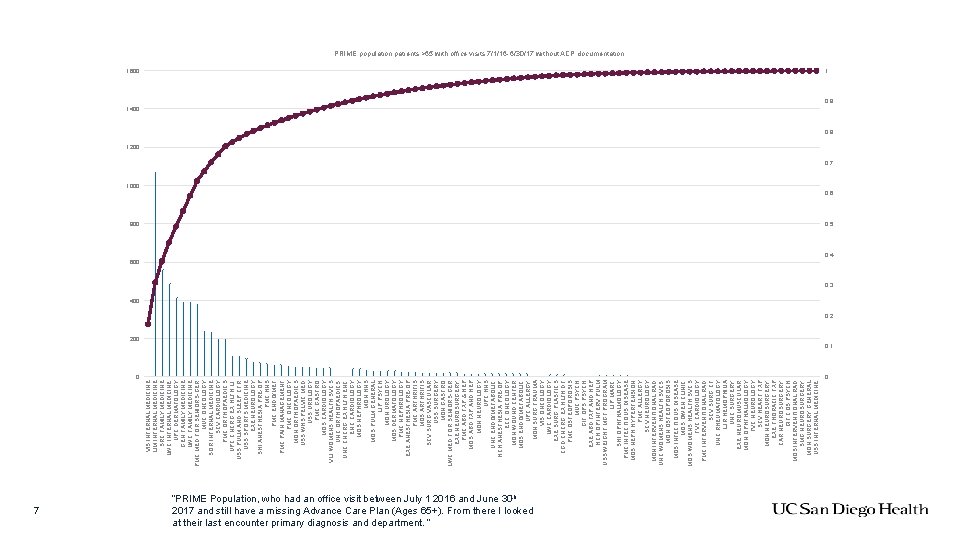
0 7 VIS INTERNAL MEDICINE LIM INTERNAL MEDICINE SRC FAMILY MEDICINE LWC INTERNAL MEDICINE UPC DERMATOLOGY GEN FAMILY MEDICINE LWC FAMILY MEDICINE PMC MED FOR SENIORS-GER MUC ONCOLOGY SOR INTERNAL MEDICINE SCV CARDIOLOGY PMC ORTHOPAEDICS UPC CNCRG EX HLTH LJ USS PULM AND SLEEP CTR USS SPORTS MEDICINE EXE NEUROLOGY SHI ANESTHESIA PRE-OP PMC HNS PMC ENDO/MET PMC PAIN MANAGEMENT PMC ONCOLOGY MON ORTHOPAEDICS USS WHS PELVIC MED USS UROLOGY PMC GASTRO MOS CARDIOLOGY VLJ WOMENS HEALTH SVCS UNC ORTHOPAEDICS UNC CNCRG EX HLTH ENC CARDIOLOGY MOS NEPHROLOGY MON HNS MOS PULM GENERAL LJP PSYCH MON UROLOGY MOS DERMATOLOGY PMC NEPHROLOGY EXE ANESTHESIA PRE-OP PMC ARTHRITIS MOS ARTHRITIS SCV SURG VASCULAR USS SURGERY MON GASTRO LWC MED FOR SENIORS-GER EXE NEUROSURGERY PMC ABD TXP & HEP MOS ABD TXP AND HEP MON NEUROLOGY UPC HNS UNC ENDO/METABOLIC HCH ANESTHESIA PRE-OP ECC ONCOLOGY MON WOUND CENTER MOS ENDO/METABOLIC UPC ALLERGY MON SURG TRAUMA VIS ONCOLOGY LWC CARDIOLOGY EXE SURG PLASTICS CGD CNCRG EX HLTH DT PMC OSTEOPOROSIS MUC PSYCH GIF OPS PSYCH EXE ABD TXP AND HEP HCH OP INTERV PULM USS WEIGHT MGT PROGRAM LJP MARC SHI OPHTHALMOLOGY PMC INFECTIOUS DISEASE MOS NEPH HYPERTENSION PMC ALLERGY SCV NEUROLOGY MON INTERVENTIONAL RAD UNC WOMENS HEALTH SVCS MON OSTEOPOROSIS MOS INFECTIOUS DISEASE MOS OWEN CLINIC MOS WOMENS HEALTH SVCS TVC CARDIOLOGY PMC INTERVENTIONAL RAD SCV SURG CT UNC RHEUMATOLOGY LJR HEMOPHILIA UNC SURGERY EXE NEUROMUSCULAR MON OPHTHALMOLOGY TVC NEUROLOGY SCV HEART TXP MON NEUROSURGERY EXE THORACIC TXP CAR NEUROSURGERY GIF COS PSYCH MOS INTERVENTIONAL RAD SMG NEUROSURGERY MON SURGERY GENERAL USS INTERNAL MEDICINE PRIME population patients >65 with office visits 7/1/16 -6/30/17 without ACP documentation 1600 1 1400 0. 9 0. 8 1200 0. 7 1000 0. 6 800 0. 5 600 0. 4 0. 3 400 0. 2 200 0. 1 “PRIME Population, who had an office visit between July 1 2016 and June 30 th 2017 and still have a missing Advance Care Plan (Ages 65+). From there I looked at their last encounter primary diagnosis and department. “ 0
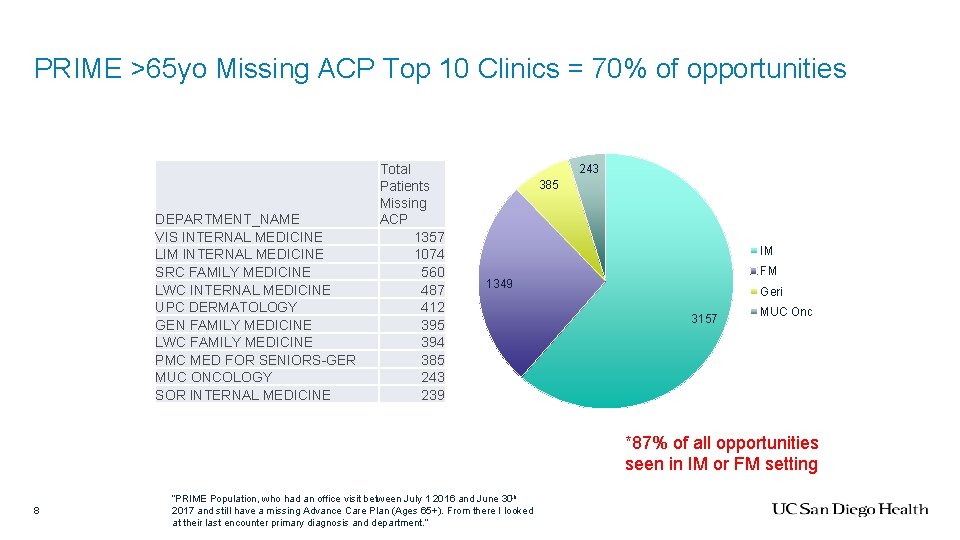
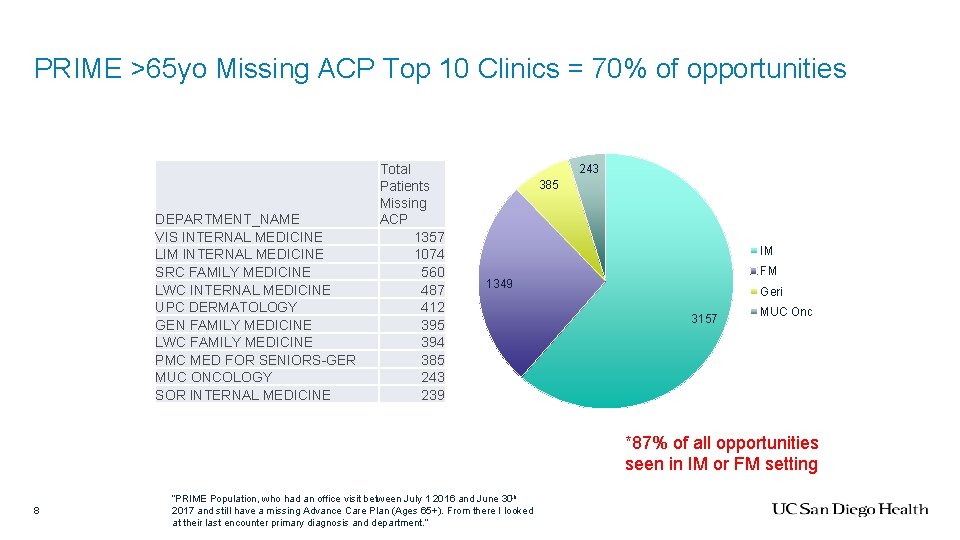
PRIME >65 yo Missing ACP Top 10 Clinics = 70% of opportunities DEPARTMENT_NAME VIS INTERNAL MEDICINE LIM INTERNAL MEDICINE SRC FAMILY MEDICINE LWC INTERNAL MEDICINE UPC DERMATOLOGY GEN FAMILY MEDICINE LWC FAMILY MEDICINE PMC MED FOR SENIORS-GER MUC ONCOLOGY SOR INTERNAL MEDICINE Total Patients Missing ACP 1357 1074 560 487 412 395 394 385 243 239 243 385 IM FM 1349 Geri 3157 MUC Onc *87% of all opportunities seen in IM or FM setting 8 “PRIME Population, who had an office visit between July 1 2016 and June 30 th 2017 and still have a missing Advance Care Plan (Ages 65+). From there I looked at their last encounter primary diagnosis and department. ”
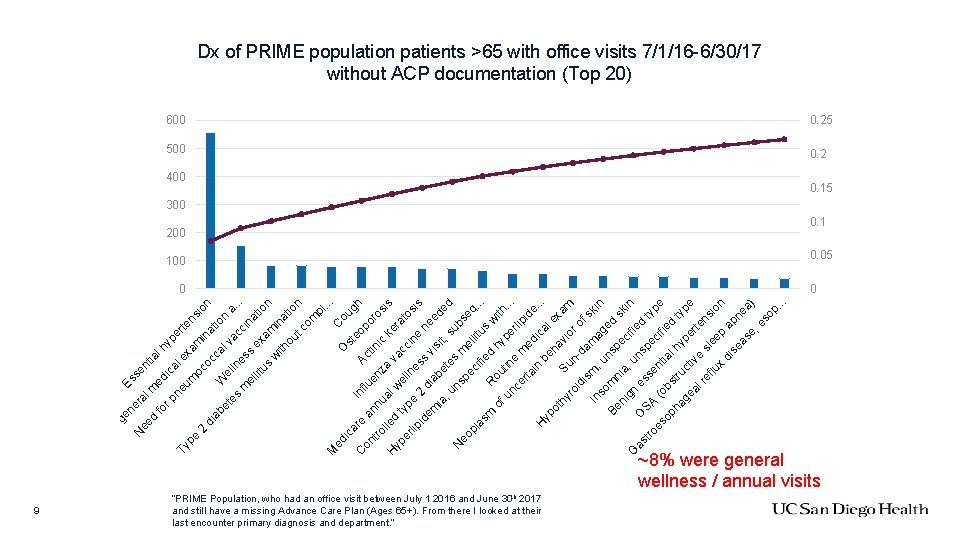
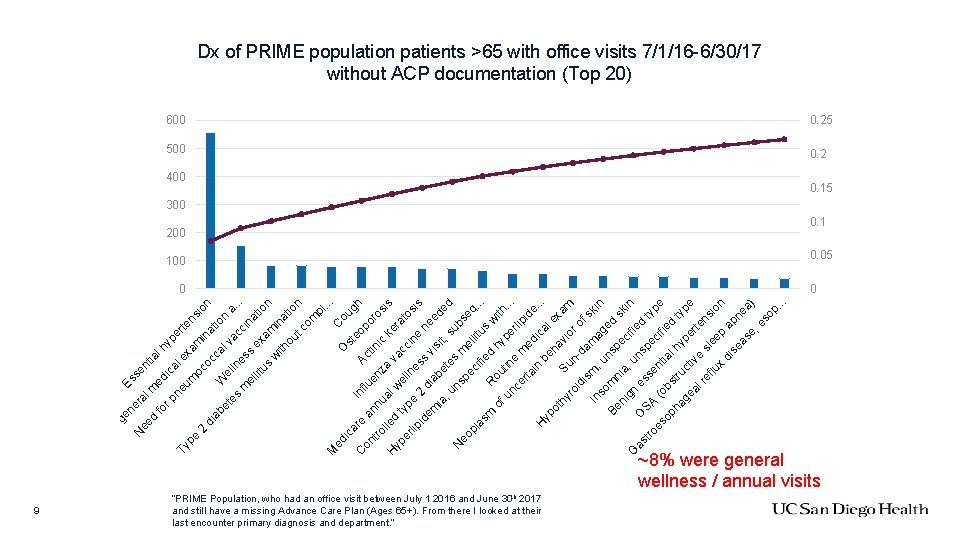
9 fo ed tia rp lh y ic ne al e per Ty um xa ten pe si m o on 2 co in di a c t ab ca i et We l v on a es lln ac. . . es ci m na s el ex lit t us am ion w ith ina tio ou n tc om pl. . . M C ed O ic st oug ar I nf C Ac eop h lu on e a or tin en tro nn os i c u z lle is a al k H er va d w yp a ty el er ln ccin tos lip pe e is e s 2 id ne em dia s v ed is b ia it, ed , u ete su s ns N b s eo pe me llit eq. pl c i. . as fie us m d R w ou h of i tin ype th. . un. e rl ce rta me ipid e. di in H. . be cal yp ex ha ot am hy vi Su or ro n -d id of is s m am In ag kin , u so e ns m Be pe d s ni ni k ci gn a, u fie in G n as O d sp SA ess tro ec typ e es n e ( ifi ed op obs tial ha tr hy t pe ype ge uct iv rte al re e s ns le flu io e n x p di se apn as ea e, ) es op. . . d se n Es lm ra ne ge N ee e tin ou R Dx of PRIME population patients >65 with office visits 7/1/16 -6/30/17 without ACP documentation (Top 20) 600 0. 25 500 0. 2 400 “PRIME Population, who had an office visit between July 1 2016 and June 30 th 2017 and still have a missing Advance Care Plan (Ages 65+). From there I looked at their last encounter primary diagnosis and department. ” 0. 15 300 200 0. 1 100 0. 05 0 0 ~8% were general wellness / annual visits
2. 7. 1 Background: Education Effort by Gary Buckholz & Chris Onderdonk • Education plan developed and rolled out • Multiple iterations and rapid cycle improvement • Focused on means for documenting brief ACP as well as generalist palliative skills • Targeted to high-yield PRIME ambulatory sites 10
2. 7. 1 Background: MCC Education by Gary Buckholz & Chris Onderdonk • 8/25 - Planning with leadership • 10/10 - APP planning with Vicki Bradford • 10/23 - MOSL, not well-attended • 12/18 - APPs, well-attended • 1/9 - RN CMs, well-attended • 1/11 - Gyn Onc team, well-attended • 2/5 - Process & measurement strategy w Dr. Califano • 2/27 - Social workers, well-attended • 3/9 - Neurooncology, well-attended 11
2. 7. 1 Background: Education by Gary Buckholz & Chris Onderdonk • 6/30 - Planning with Larry Friedman for Primary Care • 7/5 - Planning with Marilyn Obee for Managed Care • 9/20 - Family Medicine Faculty meeting, well-attended • 9/28 - Geriatrics Division meeting, well-attended • 10/4 - Cardiology Faculty meeting, well-attended • 11/1 - IM Division meeting, well-attended • 11/8 - Transplant Leadership, poorly attended—education offered & encouraged • 12/19 - Transplant, attempt to follow up with John Dickerson, offered education • 2/7 - Family Medicine Faculty follow-up, well-attended • 3/22 - Geriatrics Division meeting, follow-up scheduled
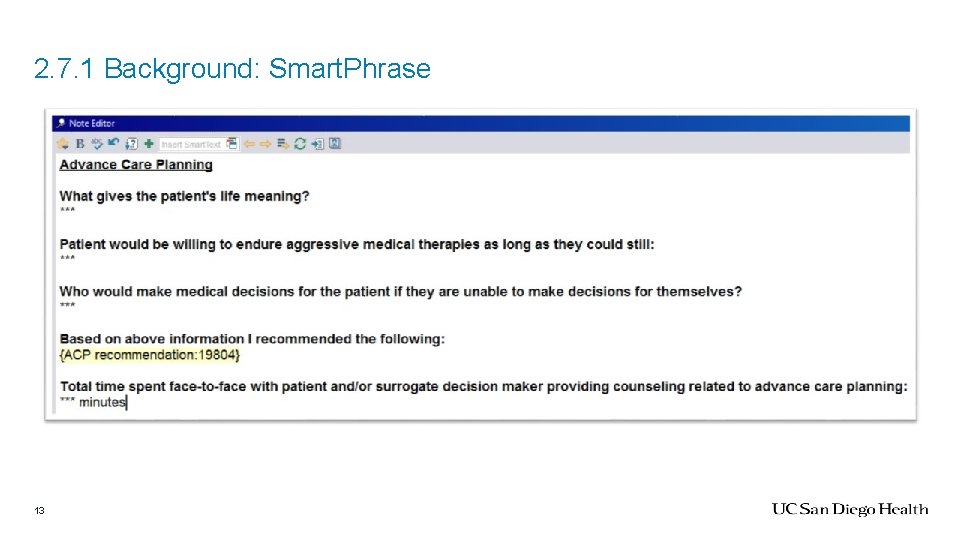
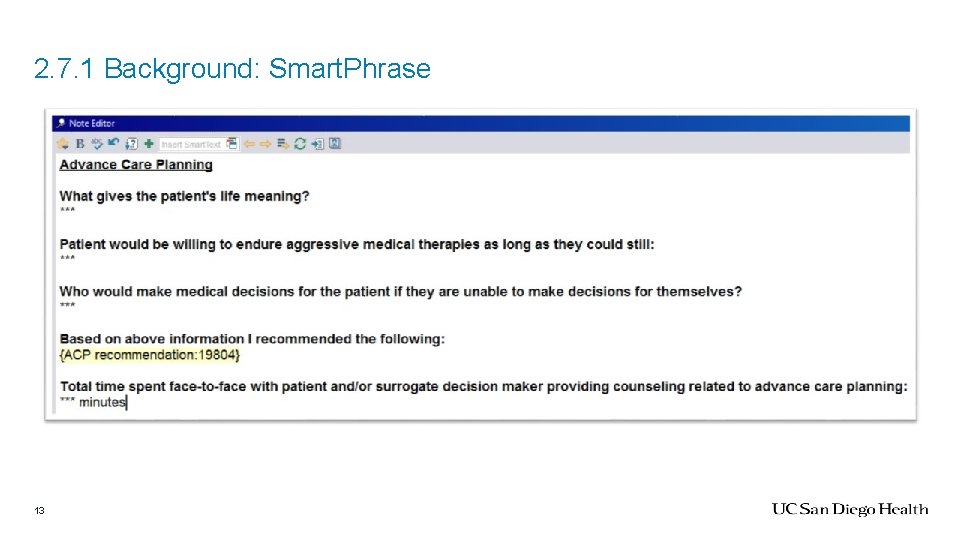
2. 7. 1 Background: Smart. Phrase 13
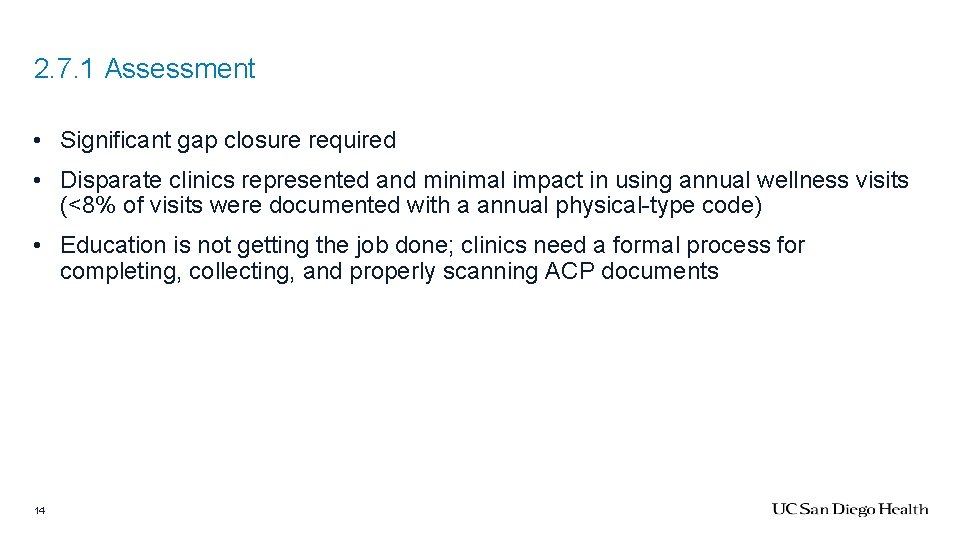
2. 7. 1 Assessment • Significant gap closure required • Disparate clinics represented and minimal impact in using annual wellness visits (<8% of visits were documented with a annual physical-type code) • Education is not getting the job done; clinics need a formal process for completing, collecting, and properly scanning ACP documents 14
2. 7. 1 Recommendation • Add. meaning/. goalsofcare (ambulatory version) smartphrases to code as a means of identifying compliance • Population health measures in process • Formal workflows for completing, collecting, scanning ACP documents • Targeting wellness visits (not going to be sufficient for gap closure) • My. Chart push for those patients with opportunity • Gary/Chris to target Vista medical group for education (need contact) • Epic ACP Activity / My. Chart modifications; add elements to visit navigator combined with BPAs & ability to document that patient does not wish to discuss • Complete MCC pilot of new ACP metric and process (APP-led so impact attenuated) 15
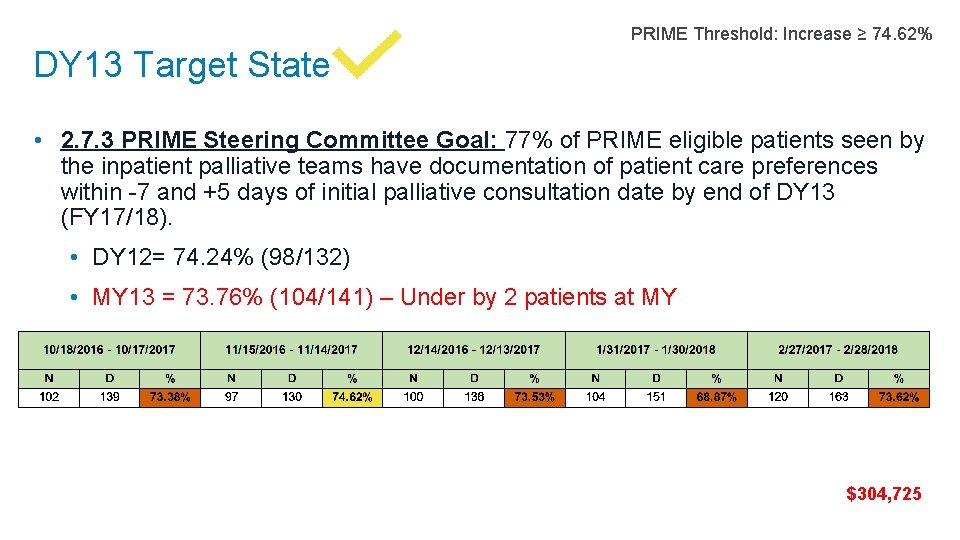
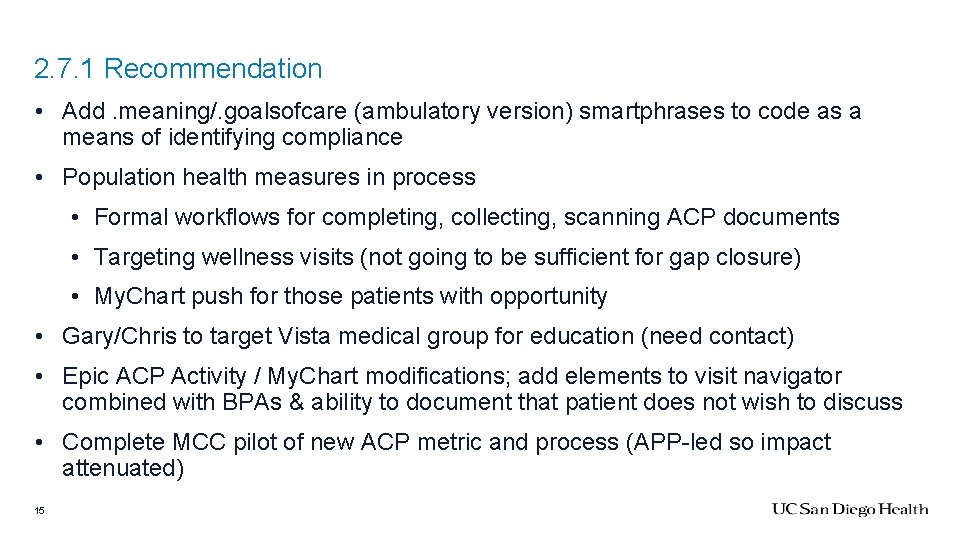
DY 13 Target State PRIME Threshold: Increase ≥ 74. 62% • 2. 7. 3 PRIME Steering Committee Goal: 77% of PRIME eligible patients seen by the inpatient palliative teams have documentation of patient care preferences within -7 and +5 days of initial palliative consultation date by end of DY 13 (FY 17/18). • DY 12= 74. 24% (98/132) • MY 13 = 73. 76% (104/141) – Under by 2 patients at MY $304, 725
2. 7. 3 Background 17 55% improvement in compliance from LJ 1 team KPE begins reporting monthly rates & makes formal presentation to La Jolla teams; joint development of Smart. Phrase
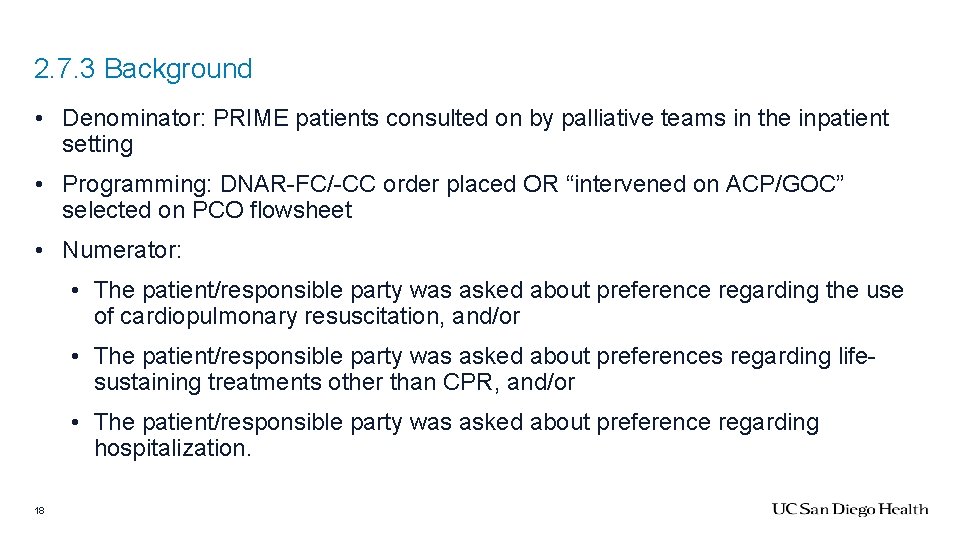
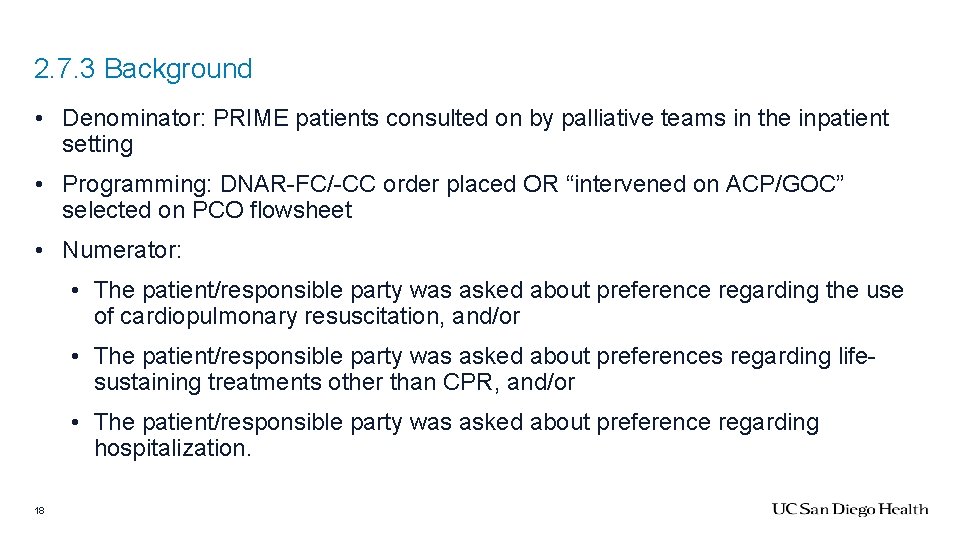
2. 7. 3 Background • Denominator: PRIME patients consulted on by palliative teams in the inpatient setting • Programming: DNAR-FC/-CC order placed OR “intervened on ACP/GOC” selected on PCO flowsheet • Numerator: • The patient/responsible party was asked about preference regarding the use of cardiopulmonary resuscitation, and/or • The patient/responsible party was asked about preferences regarding lifesustaining treatments other than CPR, and/or • The patient/responsible party was asked about preference regarding hospitalization. 18
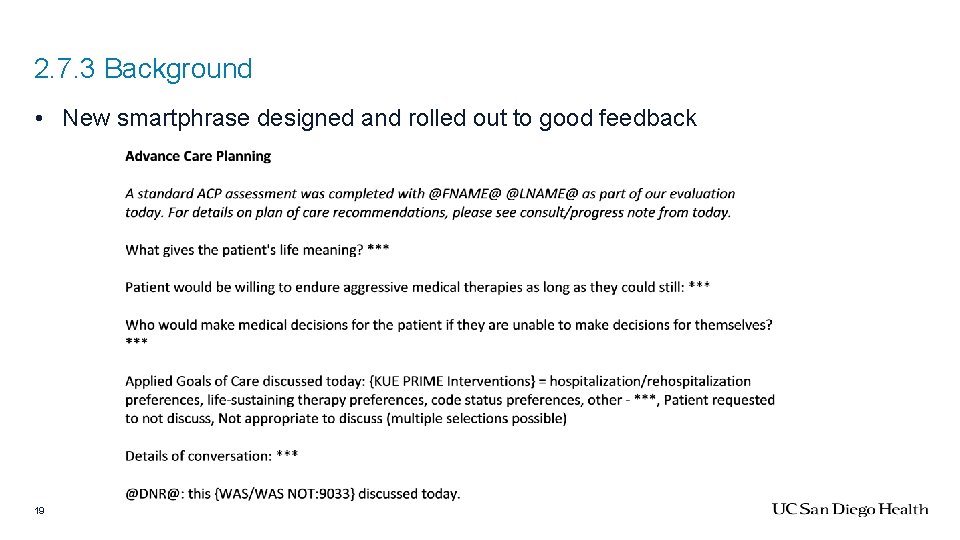
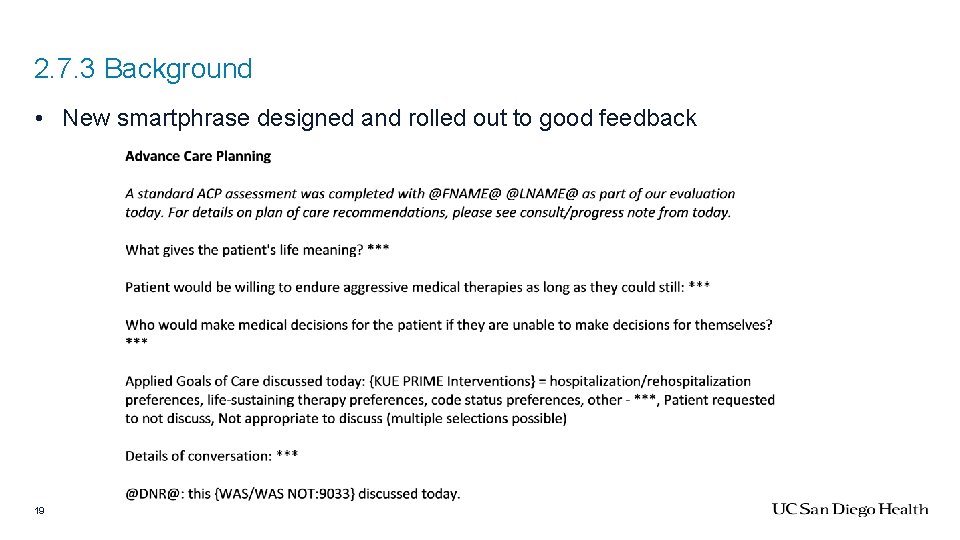
2. 7. 3 Background • New smartphrase designed and rolled out to good feedback 19
2. 7. 3 Assessment • Gap closure is achievable • Only 53% of our consults are formal ACP/GOC discussions How much can/do we push on symptom consults w/o alienating consulting teams? 20
2. 7. 3 Recommendation • Starting this week: Kyle to send Thursday email to teams indicating likely PRIME population patients who need a note using the new smartphrase • Continue to provide monthly report cards to inpatient teams using rolling data • Rapid on-boarding of new LCSW for LJ 1 team (position approved, pending posting) 21
DY 13 Target State PRIME Threshold: Report baseline • 2. 7. 4 PRIME Steering Committee Goal: 70% of PRIME eligible patients seen by the ambulatory palliative care team ≥ 2 visits have documentation of patient care preferences by end of DY 13 (FY 17/18). • DY 12 = 69. 70% (23/33) • MY 13 = 72. 73% (23/33) *Manual chart review
2. 7. 4 Background • Denominator: PRIME population seen by Palliative Clinic Team w/in • Chart review: searching the chart with the following phrase: “DNAR OR Full Code OR Goals of… OR Life Support OR Comfort Measures OR CPR OR Resuscitation OR CMO OR DNI OR Intubat* OR aggressive OR palliative OR POLST OR advance directive OR DPOA OR power of attorney OR surrogate” and then manually searching through the returned notes/scanned documents/orders • Numerator: palliative team member acknowledging DPOA, code status, lifesustaining treatment preferences, hospitalization preference 23
2. 7. 4 Assessment • Clinic team has made steady progress without directive action • Addition of Allison Kestenbaum, palliative chaplain has been beneficial (complicated by challenges with access to GOC note type) 24
2. 7. 4 Recommendation • No change or formal directives • Continued monthly progress report to team based on rolling year data (as available) • Re-assess with next month’s rolling data to determine if targeted intervention necessary to maintain compliance • As Allison is leaving for maternity leave x 4 mos, we are requesting temporary funding for chaplain to maintain gains / be compliant with PRIME 2. 7. 2 metric 25
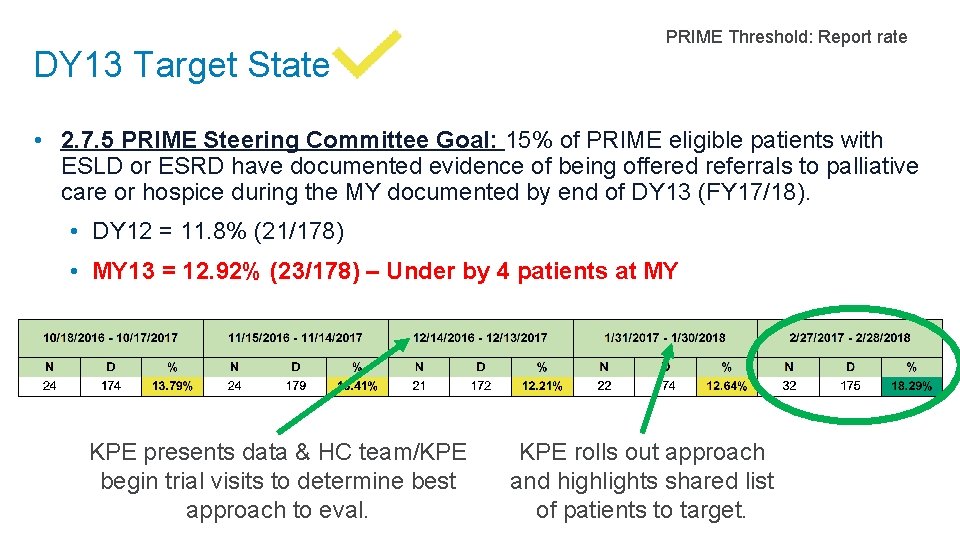
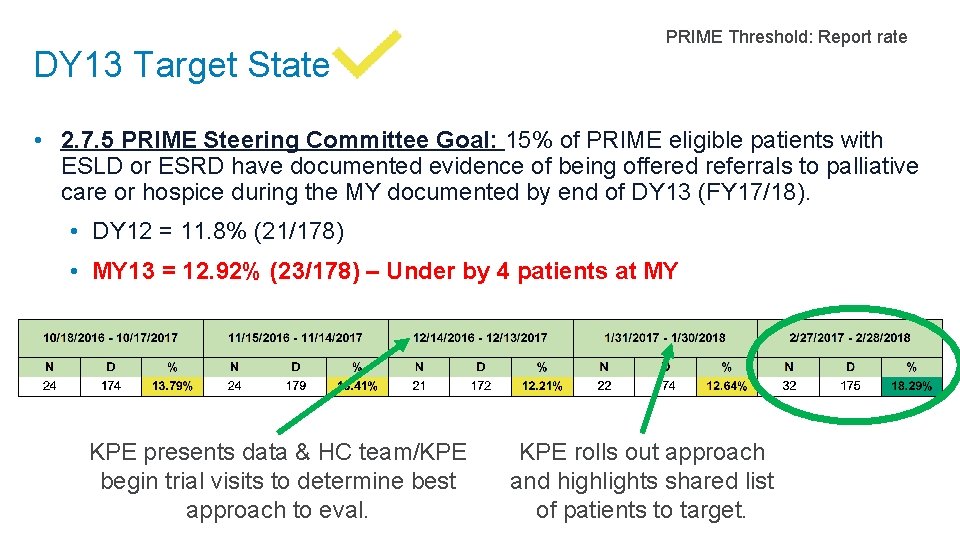
DY 13 Target State PRIME Threshold: Report rate • 2. 7. 5 PRIME Steering Committee Goal: 15% of PRIME eligible patients with ESLD or ESRD have documented evidence of being offered referrals to palliative care or hospice during the MY documented by end of DY 13 (FY 17/18). • DY 12 = 11. 8% (21/178) • MY 13 = 12. 92% (23/178) – Under by 4 patients at MY KPE presents data & HC team/KPE begin trial visits to determine best approach to eval. KPE rolls out approach and highlights shared list of patients to target.
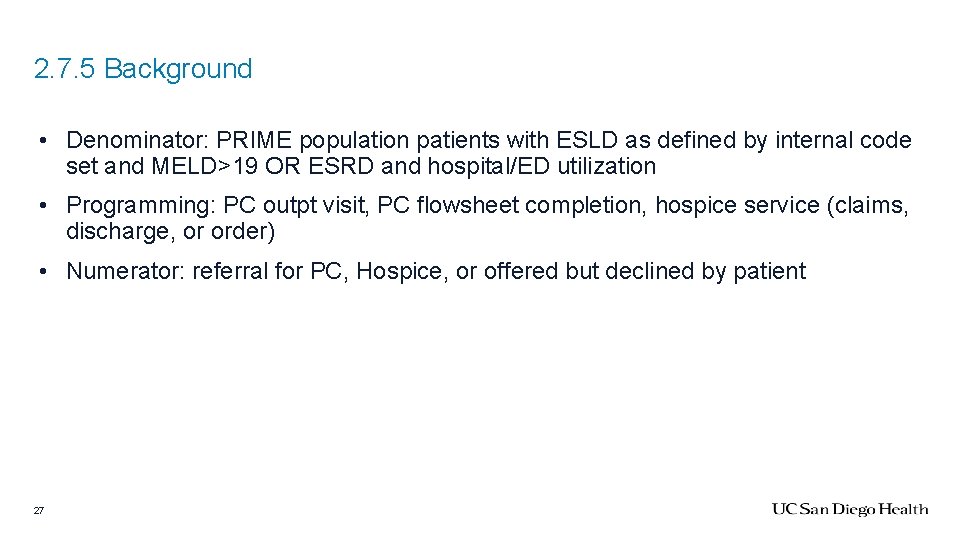
2. 7. 5 Background • Denominator: PRIME population patients with ESLD as defined by internal code set and MELD>19 OR ESRD and hospital/ED utilization • Programming: PC outpt visit, PC flowsheet completion, hospice service (claims, discharge, or order) • Numerator: referral for PC, Hospice, or offered but declined by patient 27
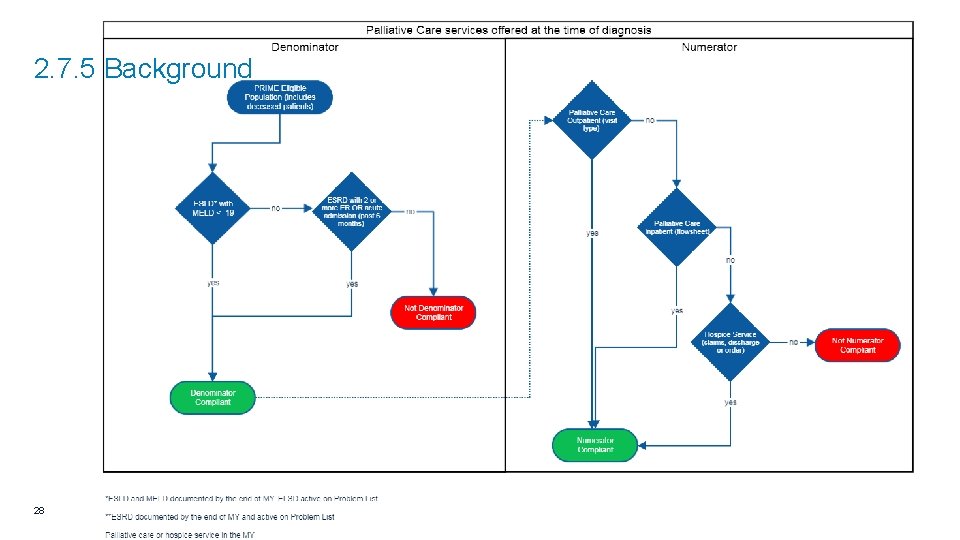
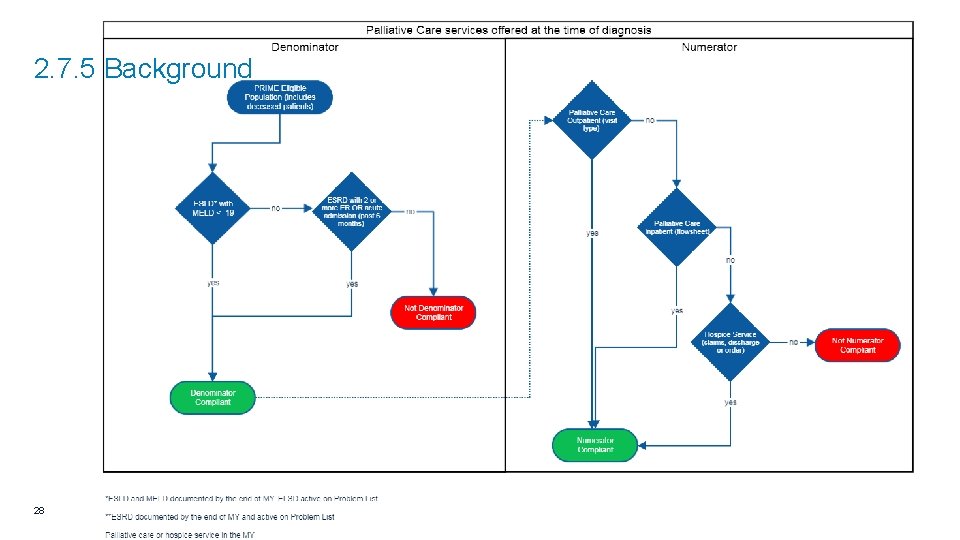
2. 7. 5 Background 28
2. 7. 5 Assessment • I have been proactively identifying admitted patients in this population • from rolling data • targeting for palliative assessments & ACP • currently 157 living patients on the shared list (Bill & I as well as NPs on all three consult teams have access) 29
2. 7. 5 Recommendation • We will scale back inpatient team efforts for now and focus on 2. 7. 3 • Development of ambulatory team to see these patients in clinic setting 30
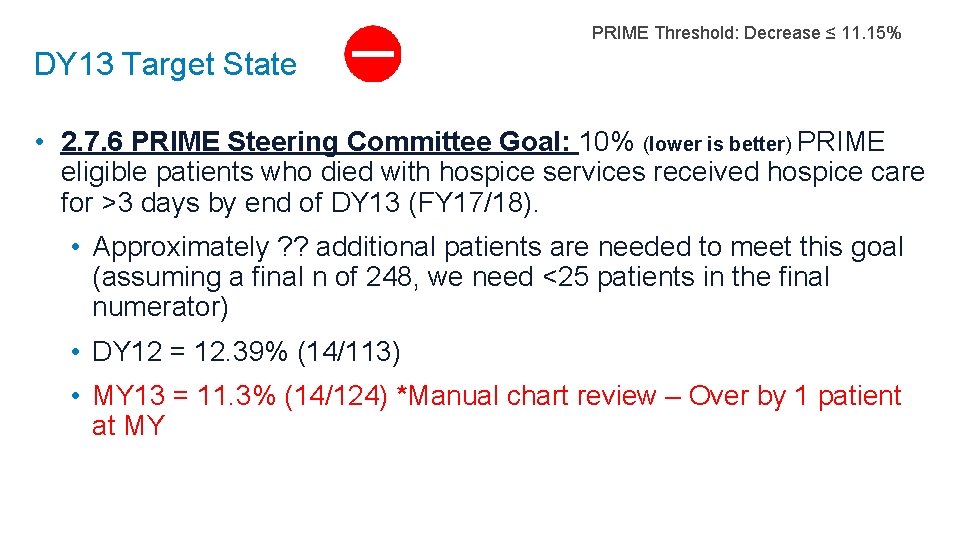
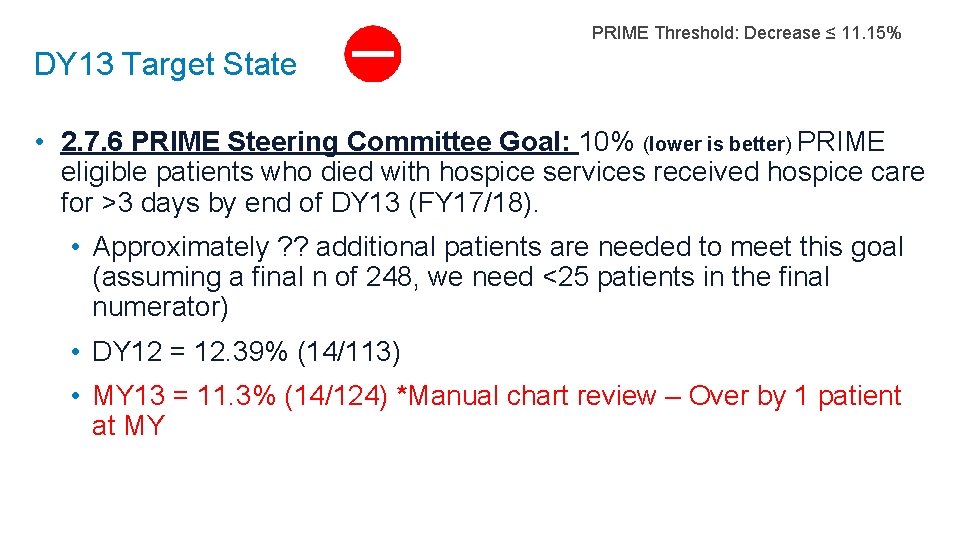
PRIME Threshold: Decrease ≤ 11. 15% DY 13 Target State • 2. 7. 6 PRIME Steering Committee Goal: 10% (lower is better) PRIME eligible patients who died with hospice services received hospice care for >3 days by end of DY 13 (FY 17/18). • Approximately ? ? additional patients are needed to meet this goal (assuming a final n of 248, we need <25 patients in the final numerator) • DY 12 = 12. 39% (14/113) • MY 13 = 11. 3% (14/124) *Manual chart review – Over by 1 patient at MY
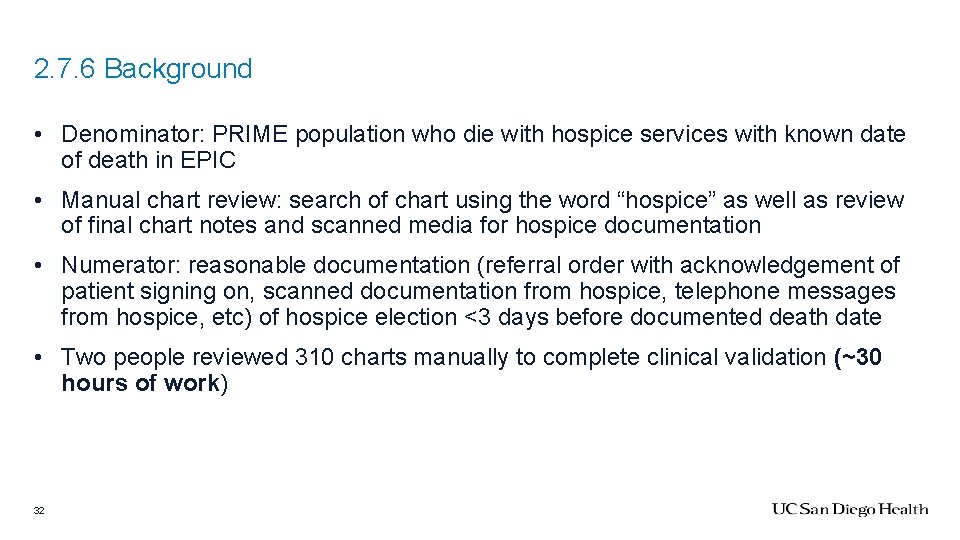
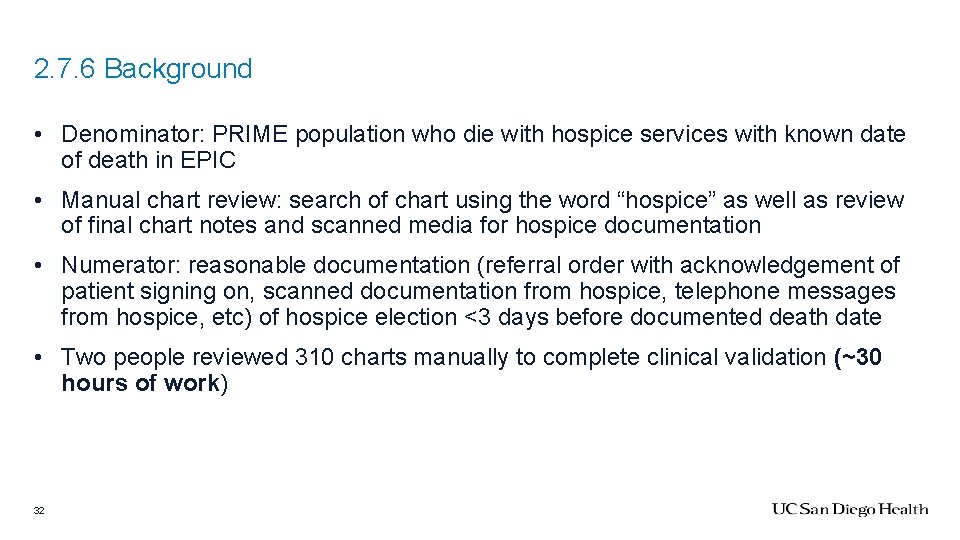
2. 7. 6 Background • Denominator: PRIME population who die with hospice services with known date of death in EPIC • Manual chart review: search of chart using the word “hospice” as well as review of final chart notes and scanned media for hospice documentation • Numerator: reasonable documentation (referral order with acknowledgement of patient signing on, scanned documentation from hospice, telephone messages from hospice, etc) of hospice election <3 days before documented death date • Two people reviewed 310 charts manually to complete clinical validation (~30 hours of work) 32
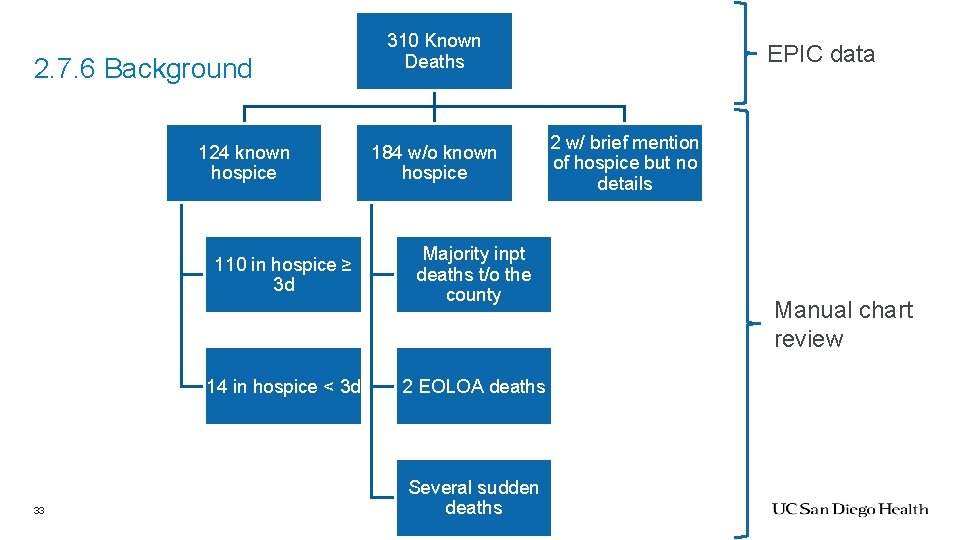
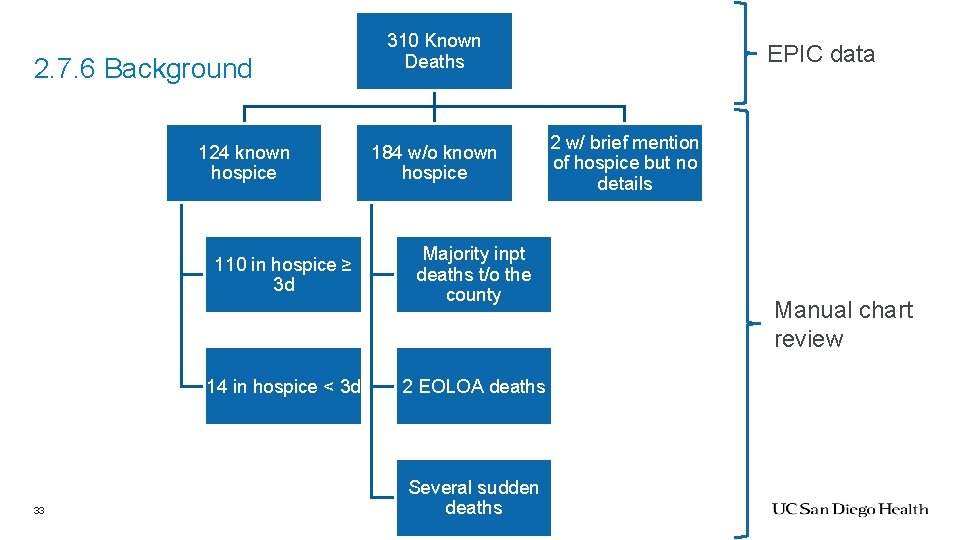
2. 7. 6 Background 124 known hospice 110 in hospice ≥ 3 d 14 in hospice < 3 d 33 310 Known Deaths 184 w/o known hospice Majority inpt deaths t/o the county 2 EOLOA deaths Several sudden deaths EPIC data 2 w/ brief mention of hospice but no details Manual chart review
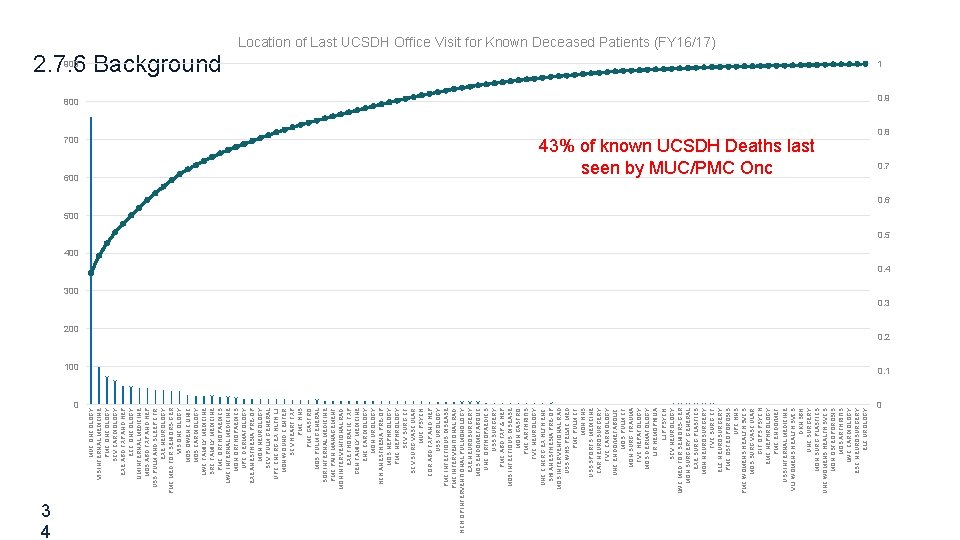
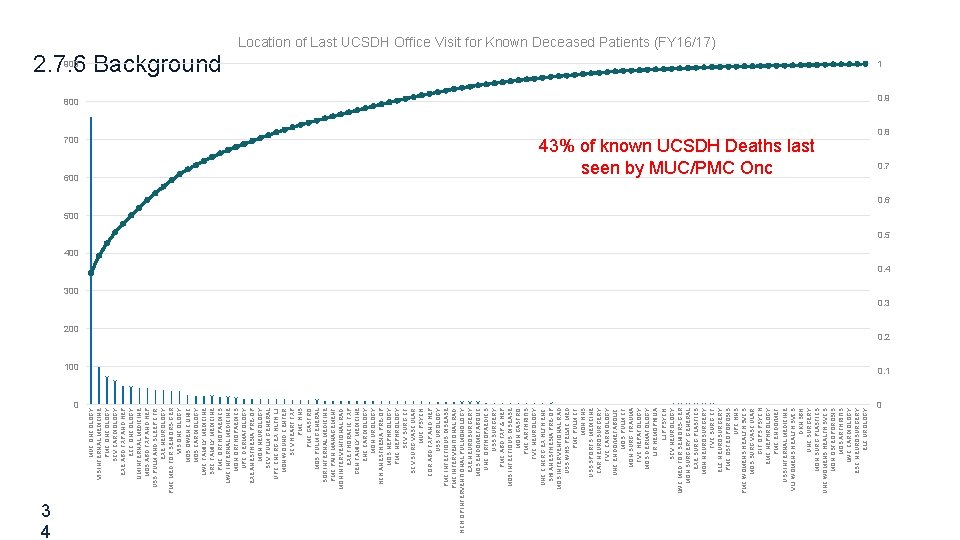
700 600 0 3 4 MUC ONCOLOGY VIS INTERNAL MEDICINE PMC ONCOLOGY SCV CARDIOLOGY EXE ABD TXP AND HEP ECC ONCOLOGY LIM INTERNAL MEDICINE MOS ABD TXP AND HEP USS PULM AND SLEEP CTR EXE NEUROLOGY PMC MED FOR SENIORS-GER VIS ONCOLOGY MOS OWEN CLINIC MOS CARDIOLOGY LWC FAMILY MEDICINE SRC FAMILY MEDICINE PMC ORTHOPAEDICS LWC INTERNAL MEDICINE MON ORTHOPAEDICS UPC DERMATOLOGY EXE ANESTHESIA PRE-OP MON NEUROLOGY SCV PULM GENERAL UPC CNCRG EX HLTH LJ MON WOUND CENTER SCV HEART TXP PMC HNS PMC GASTRO MOS PULM GENERAL SOR INTERNAL MEDICINE PMC PAIN MANAGEMENT MON INTERVENTIONAL RAD EXE THORACIC TXP GEN FAMILY MEDICINE ENC CARDIOLOGY MON UROLOGY HCH ANESTHESIA PRE-OP MOS NEPHROLOGY PMC NEPHROLOGY SCV SURG CT SCV SURG VASCULAR MUC PSYCH COR ABD TXP AND HEP USS UROLOGY PMC INFECTIOUS DISEASE PMC INTERVENTIONAL RAD HCH OP INTERVENTIONAL PULMONOLOGY EXE NEUROSURGERY MOS ENDO/METABOLIC UNC ORTHOPAEDICS USS SURGERY PMC ABD TXP & HEP MOS INFECTIOUS DISEASE MON GASTRO PMC ARTHRITIS TVC NEUROLOGY UNC CNCRG EX HLTH ENC SHI ANESTHESIA PRE-OP MOS INTERVENTIONAL RAD USS WHS PELVIC MED PMC PULM CF MON HNS USS SPORTS MEDICINE CAR NEUROSURGERY TVC CARDIOLOGY UNC ENDO/METABOLIC MOS PULM CF MON SURG TRAUMA TVC HEPATOLOGY MOS DERMATOLOGY LJR HEMOPHILIA LJP PSYCH SCV NEUROLOGY LWC MED FOR SENIORS-GER MON SURGERY GENERAL EXE SURG PLASTICS MON NEUROSURGERY TVC SURG CT ELC NEUROSURGERY PMC OSTEOPOROSIS UPC HNS PMC WOMENS HEALTH SVCS MOS SURG VASCULAR GIF OPS PSYCH EMC NEPHROLOGY PMC ENDO/MET USS INTERNAL MEDICINE VLJ WOMENS HEALTH SVCS DKN SBH UNC SURGERY MON SURG PLASTICS UNC WOMENS HEALTH SVCS MON OSTEOPOROSIS MOS ARTHRITIS LWC CARDIOLOGY ESC NEUROSURGERY ELC UROLOGY Location of Last UCSDH Office Visit for Known Deceased Patients (FY 16/17) 2. 7. 6 Background 900 1 800 0. 9 43% of known UCSDH Deaths last seen by MUC/PMC Onc 200 100 0. 8 0. 7 0. 6 500 0. 5 400 0. 4 300 0. 3 0. 2 0. 1 0
2. 7. 6 Assessment • Complicated gap closure required • Every clinic has a different process • Inpatient referrals don’t go through Epic • GIP initiative works against us (~2 fallouts at MY were in-house GIP) • We’re only looking at people we know have died, which is a skewed population • Most hospices provide no or inconsistent details back to us • The only evidence-based way to improve: individual report cards on provider hospice referral rate and average time to death. • This research (& this metric) are only in solid tumor oncology • CHF, ESLD, COPD, ILD, MDS, heme malignancy folks work against us earlier hospice may not be clinically indicated 35
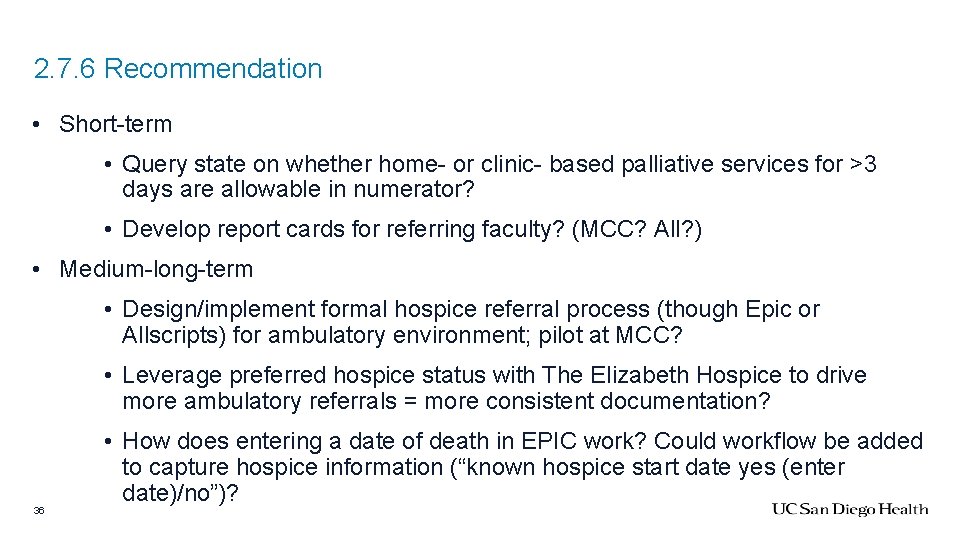
2. 7. 6 Recommendation • Short-term • Query state on whether home- or clinic- based palliative services for >3 days are allowable in numerator? • Develop report cards for referring faculty? (MCC? All? ) • Medium-long-term • Design/implement formal hospice referral process (though Epic or Allscripts) for ambulatory environment; pilot at MCC? • Leverage preferred hospice status with The Elizabeth Hospice to drive more ambulatory referrals = more consistent documentation? 36 • How does entering a date of death in EPIC work? Could workflow be added to capture hospice information (“known hospice start date yes (enter date)/no”)?
Asks • 2. 7. 1 • Add. meaning/. goalsofcare (ambulatory version) smartphrases to programming as a means of identifying compliance • Contact info Vista IM Provider Group to target with education • Epic ACP Activity / My. Chart modifications; add elements to visit navigator combined with BPAs & ability to document that patient does not wish to discuss • 2. 7. 2: Approval of coverage for clinic chaplain while Allison Kestenbaum on maternity leave • 2. 7. 3: Rapid on-boarding of new LCSW for LJ 1 team (position approved, pending posting) • 2. 7. 5: Development of ambulatory team to see ESLD/ESRD patients in clinic setting • 2. 7. 6: System-level guidance on what to do about hospice workflows 37

Q&A 38
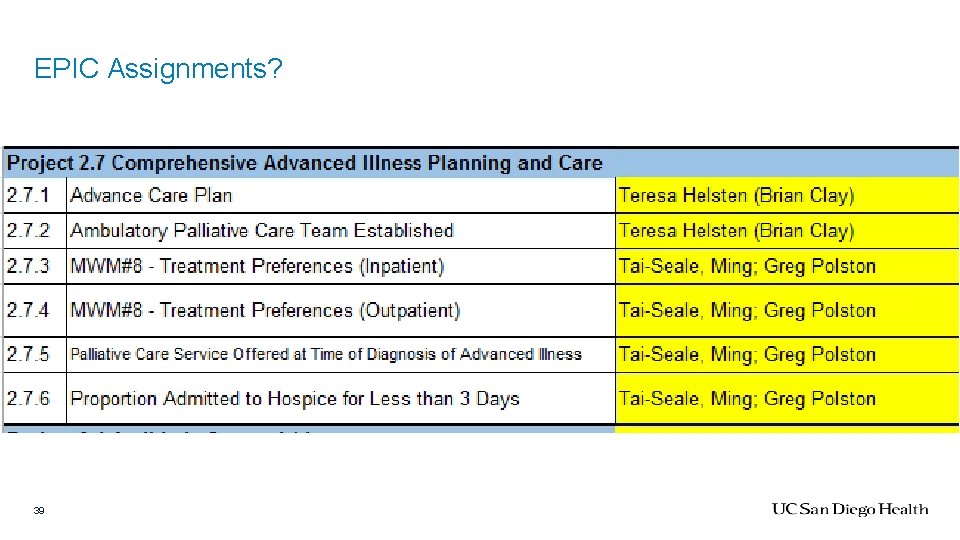
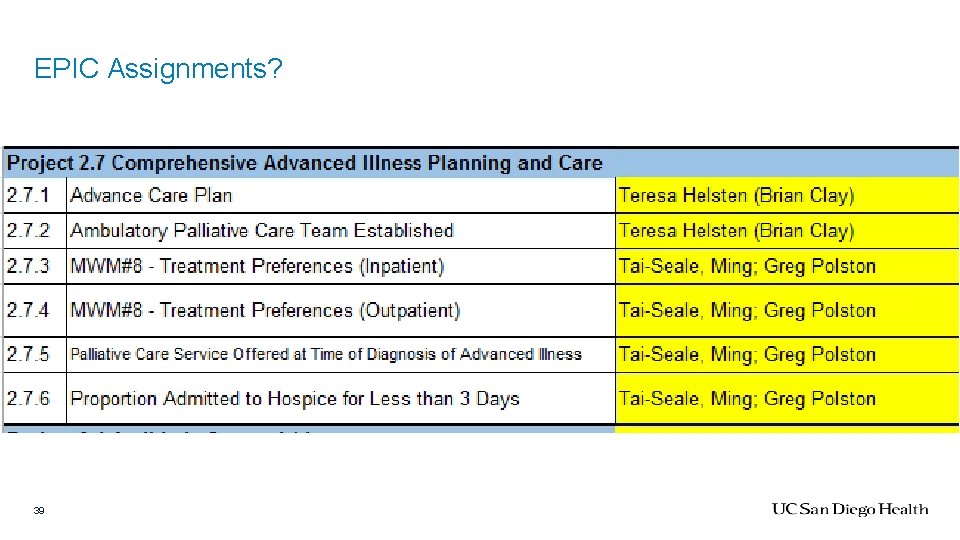
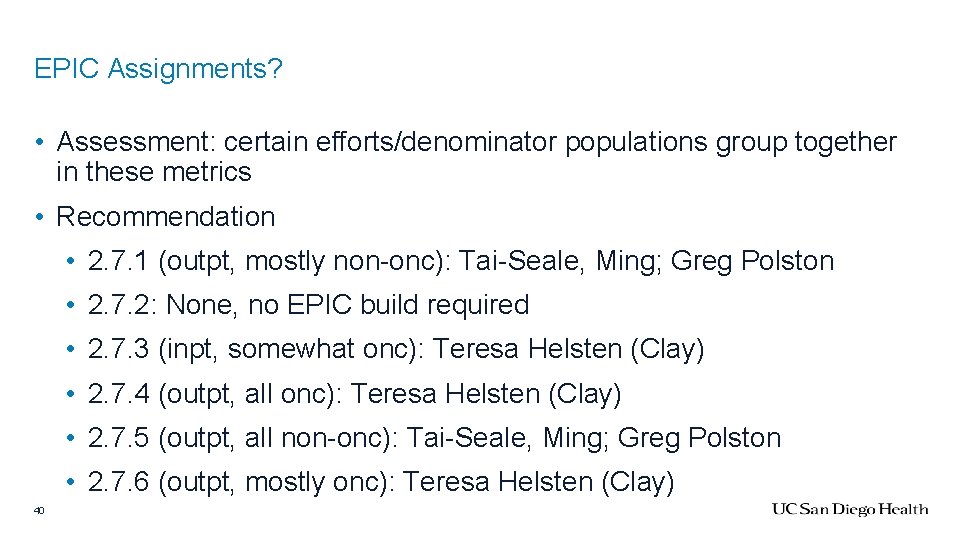
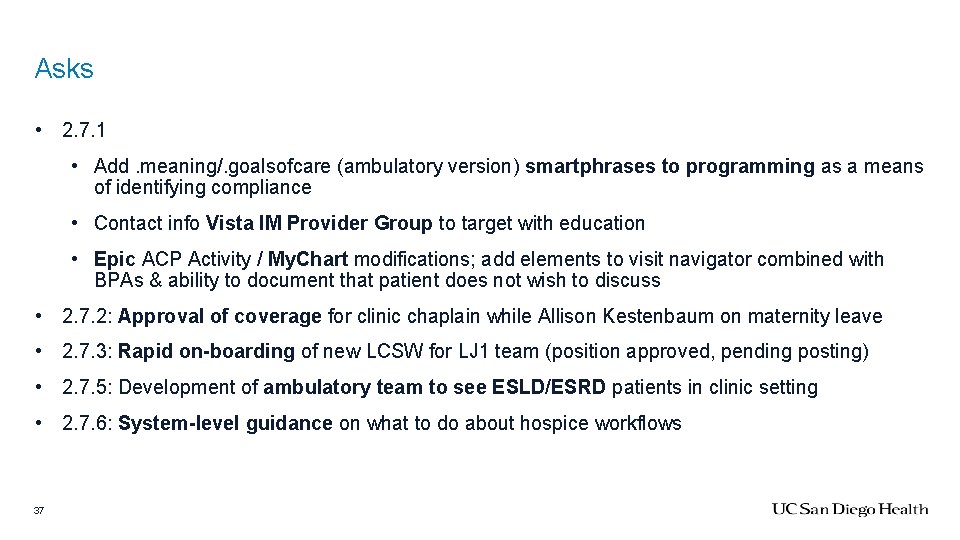
EPIC Assignments? 39
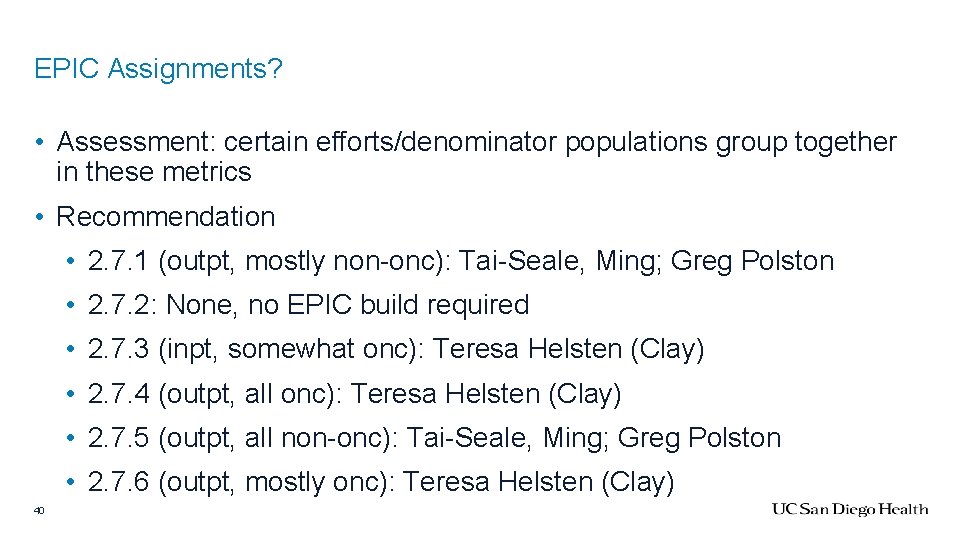
EPIC Assignments? • Assessment: certain efforts/denominator populations group together in these metrics • Recommendation • 2. 7. 1 (outpt, mostly non-onc): Tai-Seale, Ming; Greg Polston • 2. 7. 2: None, no EPIC build required • 2. 7. 3 (inpt, somewhat onc): Teresa Helsten (Clay) • 2. 7. 4 (outpt, all onc): Teresa Helsten (Clay) • 2. 7. 5 (outpt, all non-onc): Tai-Seale, Ming; Greg Polston • 2. 7. 6 (outpt, mostly onc): Teresa Helsten (Clay) 40
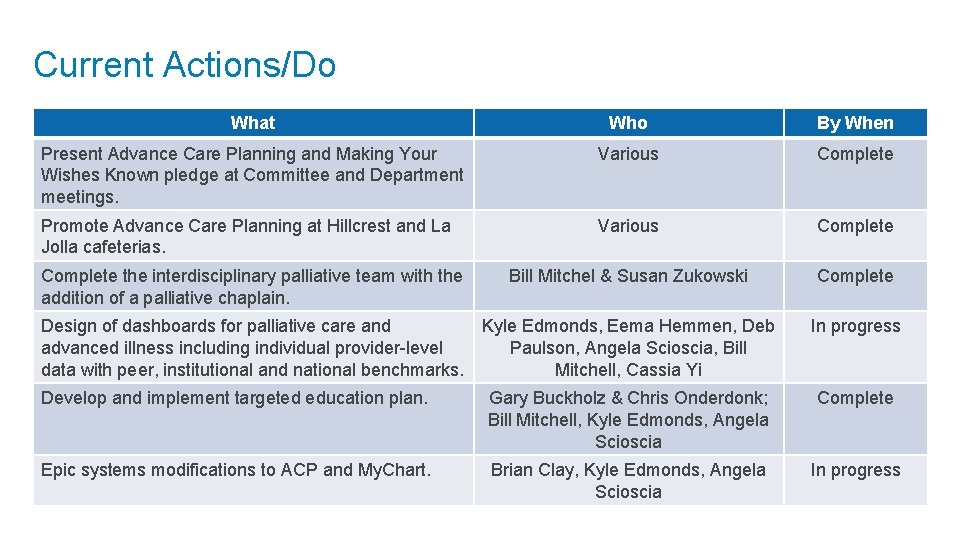
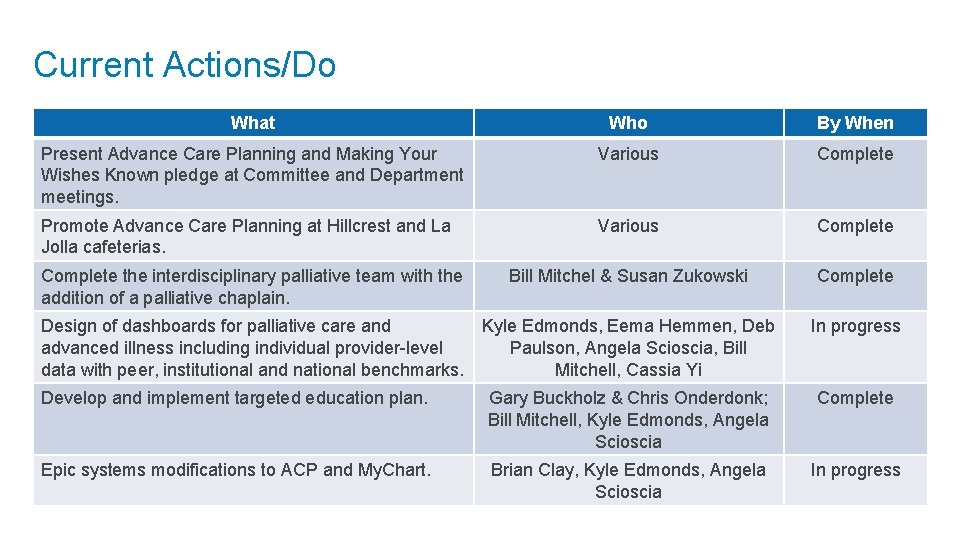
Current Actions/Do What Who By When Present Advance Care Planning and Making Your Wishes Known pledge at Committee and Department meetings. Various Complete Promote Advance Care Planning at Hillcrest and La Jolla cafeterias. Various Complete Bill Mitchel & Susan Zukowski Complete the interdisciplinary palliative team with the addition of a palliative chaplain. Design of dashboards for palliative care and Kyle Edmonds, Eema Hemmen, Deb advanced illness including individual provider-level Paulson, Angela Scioscia, Bill data with peer, institutional and national benchmarks. Mitchell, Cassia Yi In progress Develop and implement targeted education plan. Gary Buckholz & Chris Onderdonk; Bill Mitchell, Kyle Edmonds, Angela Scioscia Complete Epic systems modifications to ACP and My. Chart. Brian Clay, Kyle Edmonds, Angela Scioscia In progress
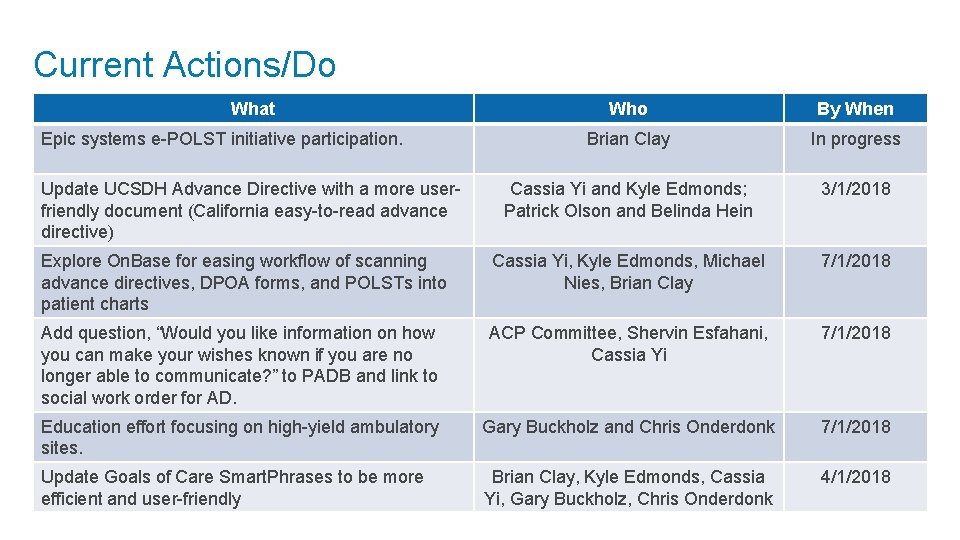
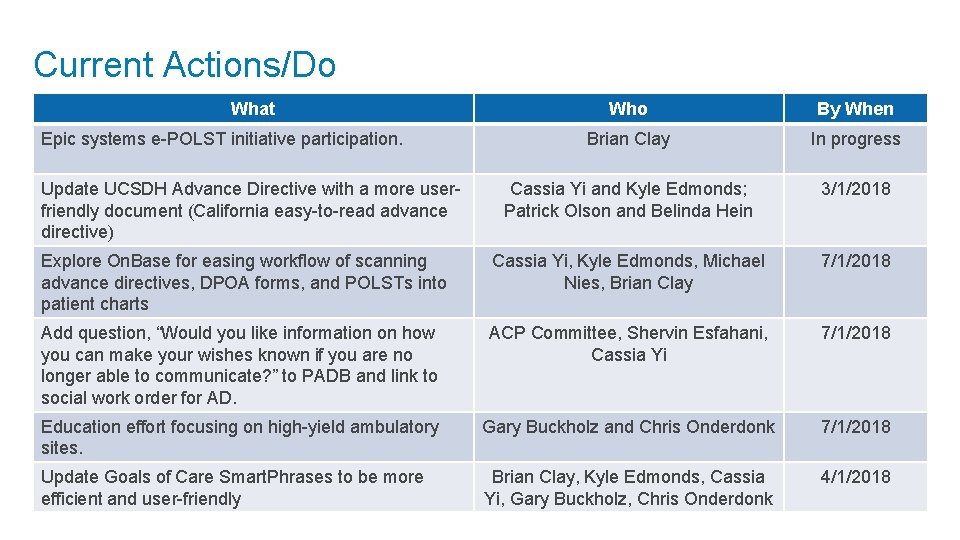
Current Actions/Do What Who By When Brian Clay In progress Cassia Yi and Kyle Edmonds; Patrick Olson and Belinda Hein 3/1/2018 Explore On. Base for easing workflow of scanning advance directives, DPOA forms, and POLSTs into patient charts Cassia Yi, Kyle Edmonds, Michael Nies, Brian Clay 7/1/2018 Add question, “Would you like information on how you can make your wishes known if you are no longer able to communicate? ” to PADB and link to social work order for AD. ACP Committee, Shervin Esfahani, Cassia Yi 7/1/2018 Education effort focusing on high-yield ambulatory sites. Gary Buckholz and Chris Onderdonk 7/1/2018 Update Goals of Care Smart. Phrases to be more efficient and user-friendly Brian Clay, Kyle Edmonds, Cassia Yi, Gary Buckholz, Chris Onderdonk 4/1/2018 Epic systems e-POLST initiative participation. Update UCSDH Advance Directive with a more userfriendly document (California easy-to-read advance directive)
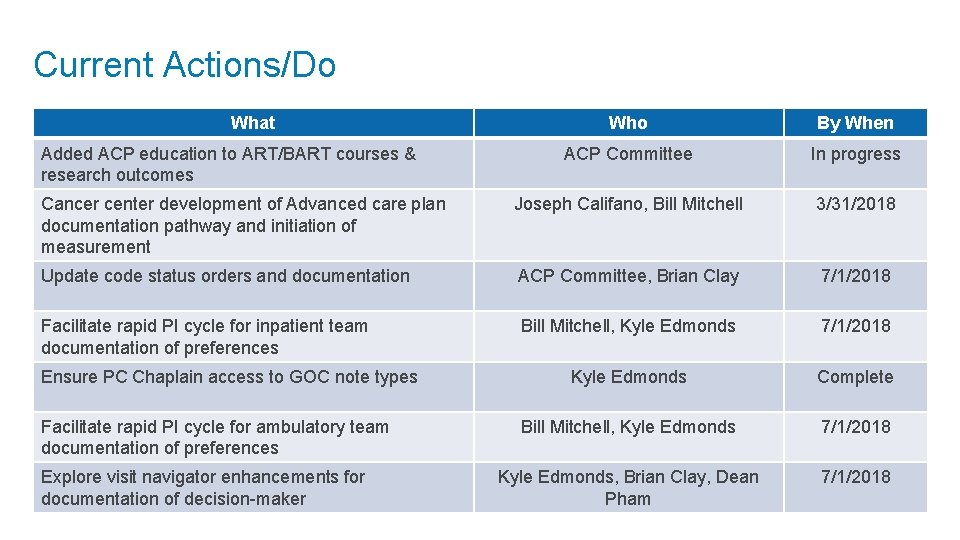
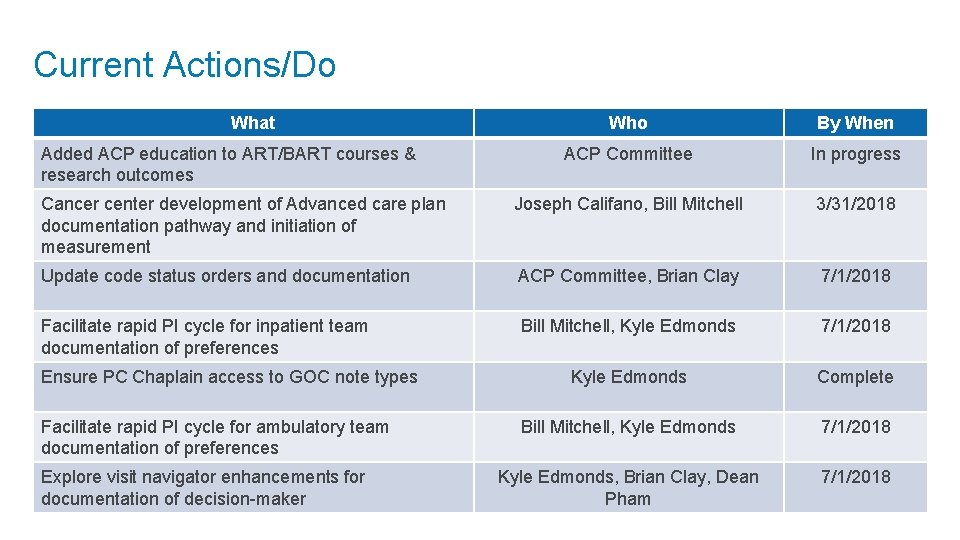
Current Actions/Do What Who By When ACP Committee In progress Cancer center development of Advanced care plan documentation pathway and initiation of measurement Joseph Califano, Bill Mitchell 3/31/2018 Update code status orders and documentation ACP Committee, Brian Clay 7/1/2018 Facilitate rapid PI cycle for inpatient team documentation of preferences Bill Mitchell, Kyle Edmonds 7/1/2018 Kyle Edmonds Complete Bill Mitchell, Kyle Edmonds 7/1/2018 Kyle Edmonds, Brian Clay, Dean Pham 7/1/2018 Added ACP education to ART/BART courses & research outcomes Ensure PC Chaplain access to GOC note types Facilitate rapid PI cycle for ambulatory team documentation of preferences Explore visit navigator enhancements for documentation of decision-maker
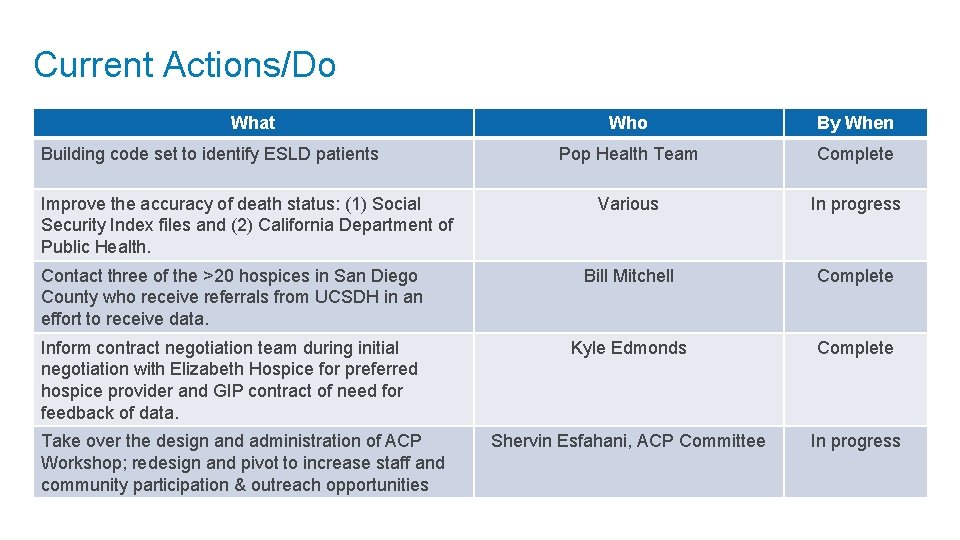
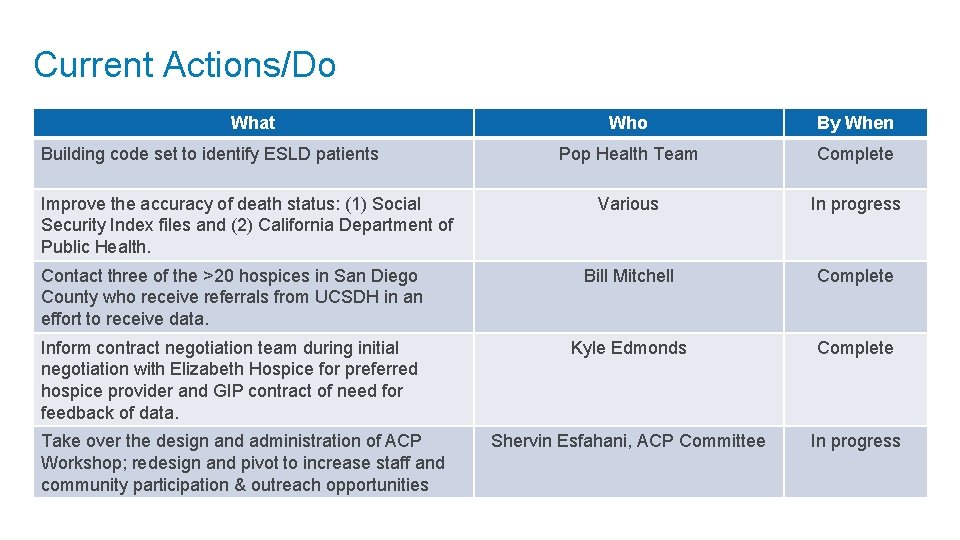
Current Actions/Do What Who By When Pop Health Team Complete Various In progress Contact three of the >20 hospices in San Diego County who receive referrals from UCSDH in an effort to receive data. Bill Mitchell Complete Inform contract negotiation team during initial negotiation with Elizabeth Hospice for preferred hospice provider and GIP contract of need for feedback of data. Kyle Edmonds Complete Shervin Esfahani, ACP Committee In progress Building code set to identify ESLD patients Improve the accuracy of death status: (1) Social Security Index files and (2) California Department of Public Health. Take over the design and administration of ACP Workshop; redesign and pivot to increase staff and community participation & outreach opportunities