Primary Immunodeficiency Syndromes Welcome to the module on
- Slides: 43
Primary Immunodeficiency Syndromes
Welcome to the module on Primary Immunodeficiency Syndromes Please take this brief pre-module quiz https: //goo. gl/forms/z. X 57 Lnn. RKx. MDXhj. B 2 2
Case 1 v 63 year old man presents with failure to thrive, dysphagia, diarrhea, cough, and SOB v. He was in his USOH until 6 weeks prior, when he developed watery diarrhea 4 -7 x/day v. Cough and SOB in the last few days v Saw his PCP, negative C dif, tried Cipro/azithro, immodium, and probiotics, without improvement v Now he is presenting to the ED febrile, ill-appearing, and profoundly SOB
Past Medical History v. Thymoma: v Initially diagnosed in late 1980’s, when he developed Myasthenia Gravis (ptosis). He initially had local disease treated w/ resection v 1990’s: local recurrence with lung invasion (stage 3 disease), received surgery, chemotherapy, radiation v 2000’s: residual disease burden remains, but fairly inactive and he was followed by Hematology-Oncology until 12/2013 (his Dr retired)
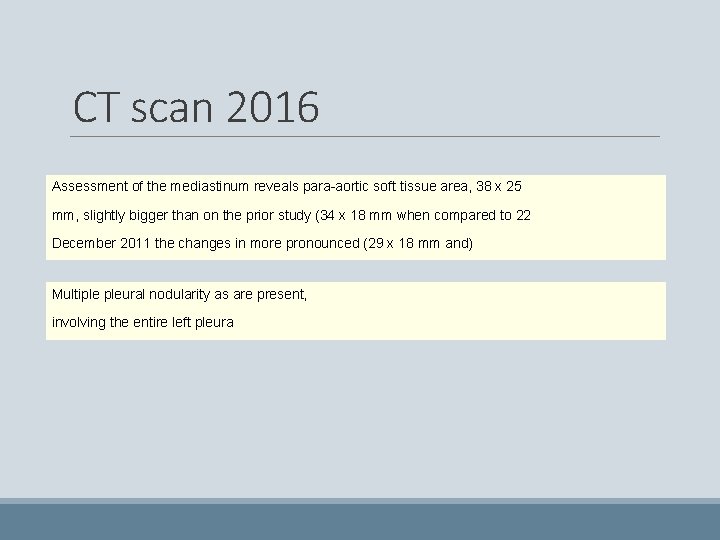
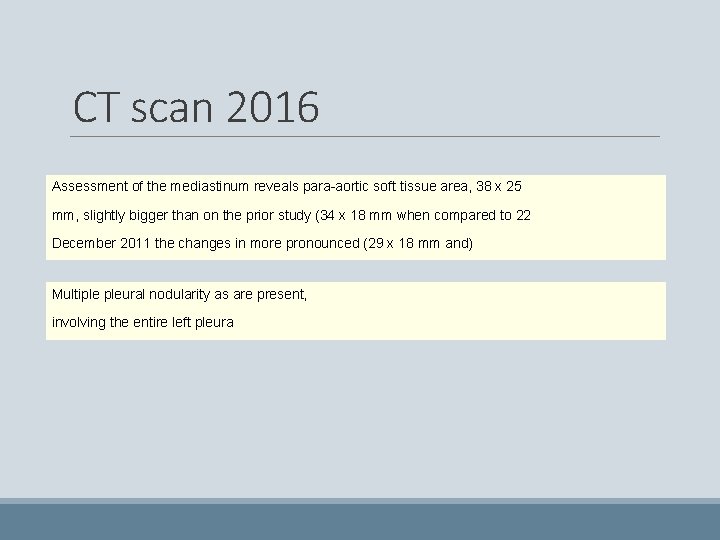
CT scan 2016 Assessment of the mediastinum reveals para-aortic soft tissue area, 38 x 25 mm, slightly bigger than on the prior study (34 x 18 mm when compared to 22 December 2011 the changes in more pronounced (29 x 18 mm and) Multiple pleural nodularity as are present, involving the entire left pleura
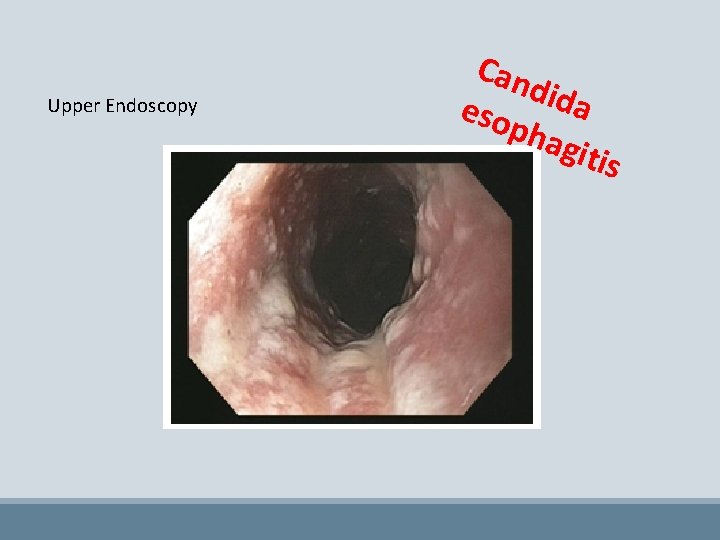
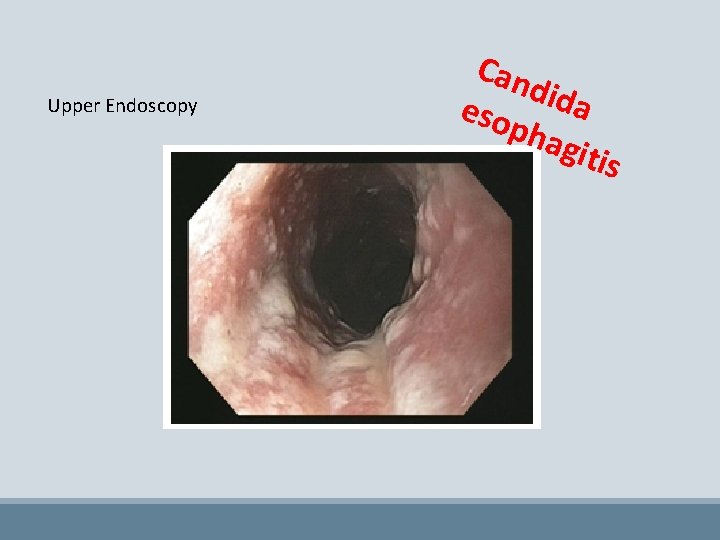
Upper Endoscopy Can dida eso pha gitis
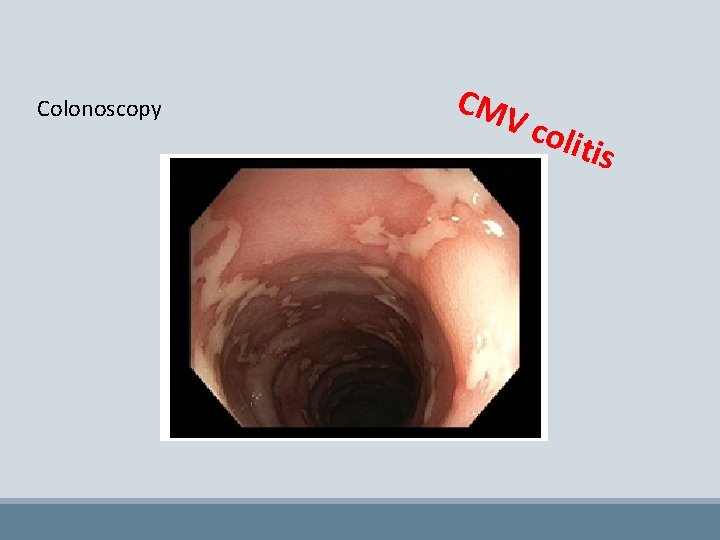
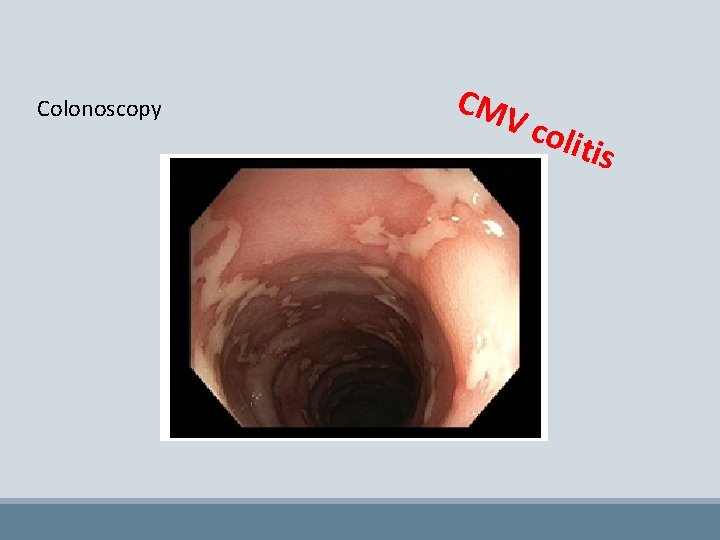
Colonoscopy CM V co litis
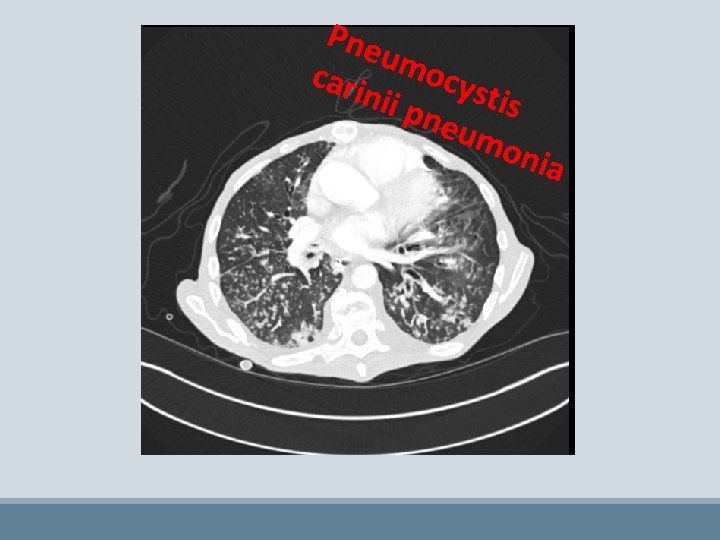
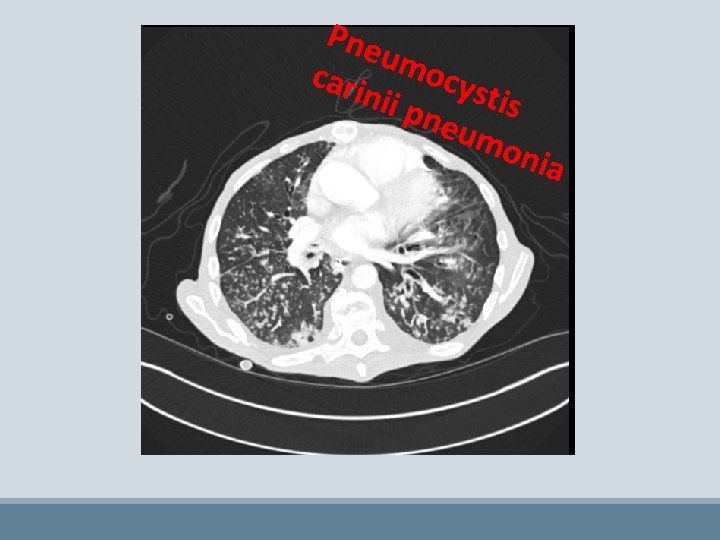
Pne umo cari c nii p ystis neu mon ia
v Also found to have giardia via stool DFA, and Salmonella bacteremia v HIV (3 rd gen assay and viral load) negative v WBC 4. 2, with normal differential (no neutropenia or lymphopenia)
Infectious Disease consult o “Please help us sort out treatment plan” o “…and figure out if he is immunosuppressed, and if so why” o “…and what prophylaxis he should be on” o “…Thanks!”
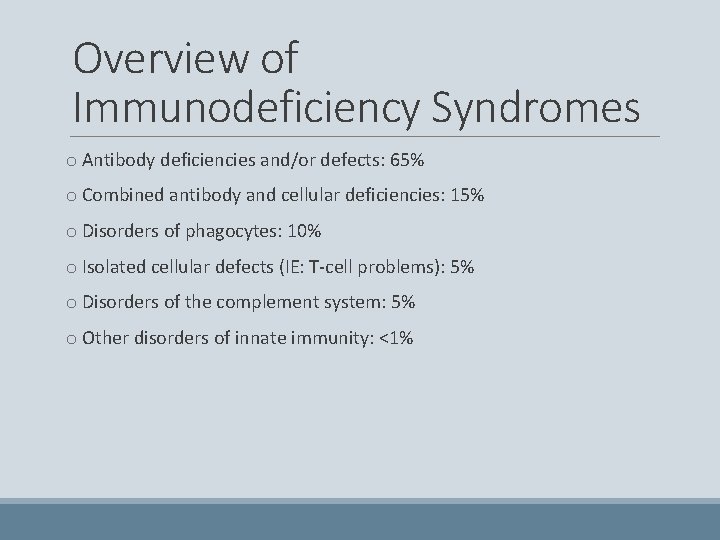
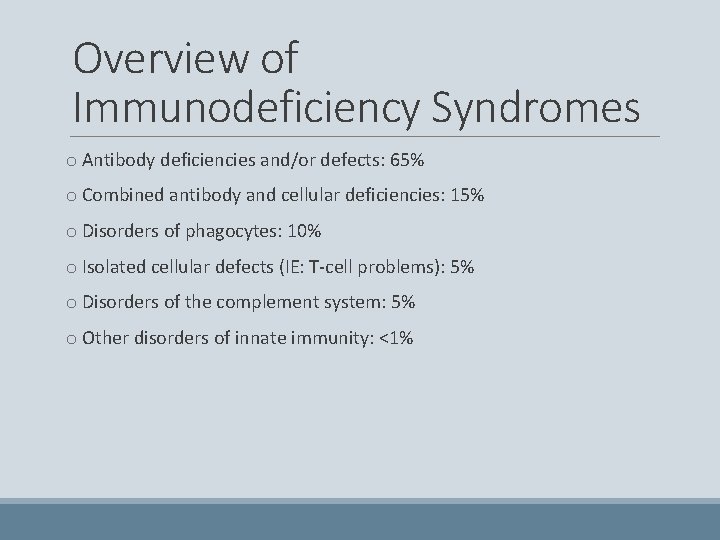
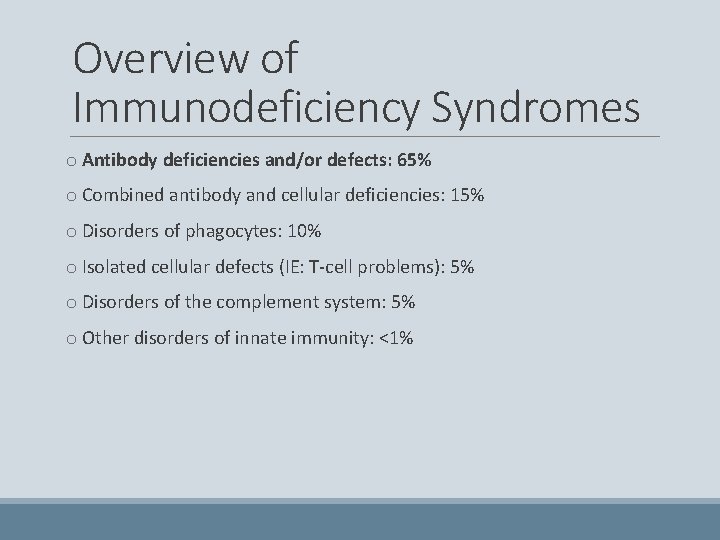
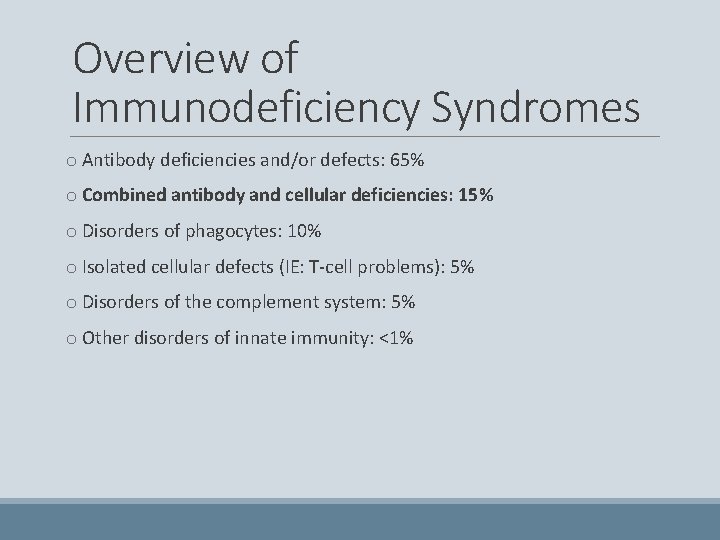
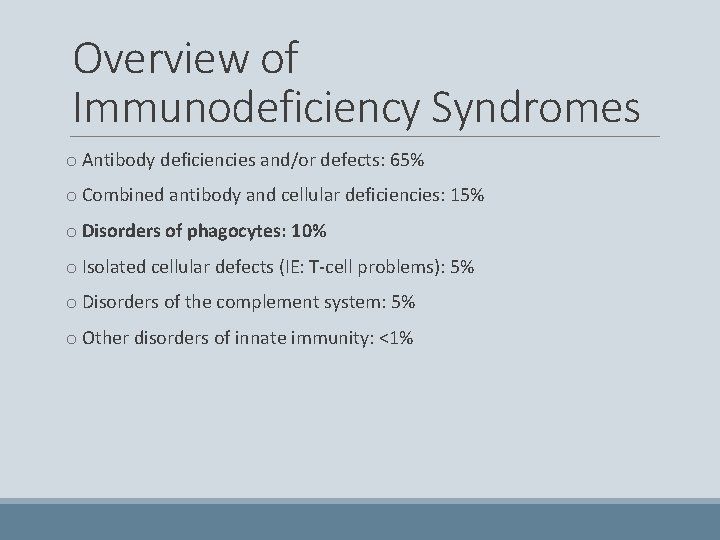
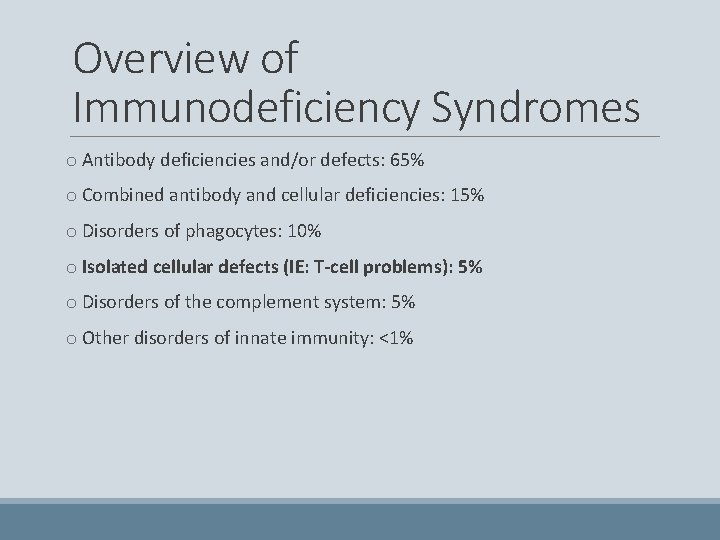
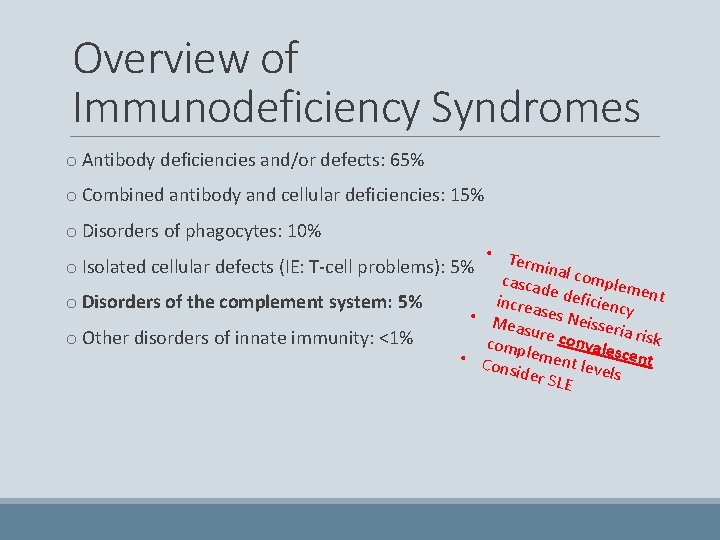
Overview of Immunodeficiency Syndromes o Antibody deficiencies and/or defects: 65% o Combined antibody and cellular deficiencies: 15% o Disorders of phagocytes: 10% o Isolated cellular defects (IE: T-cell problems): 5% o Disorders of the complement system: 5% o Other disorders of innate immunity: <1%
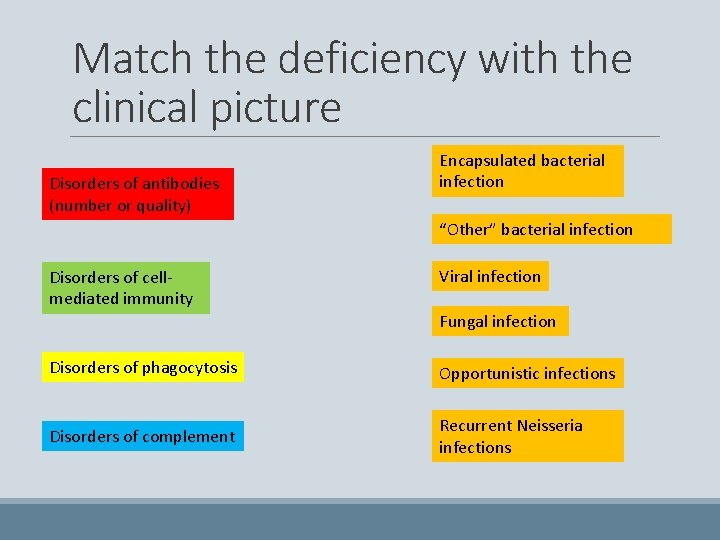
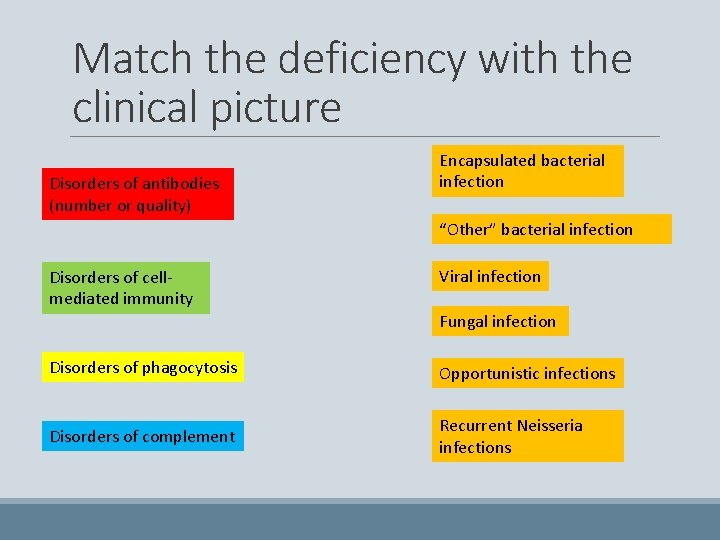
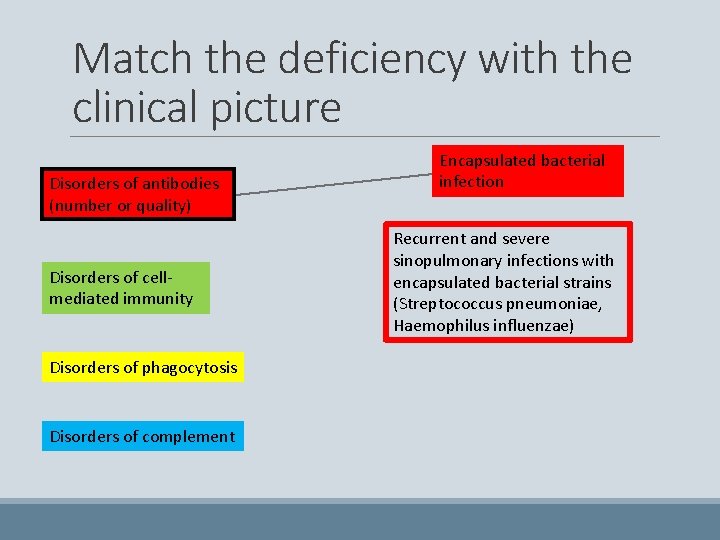
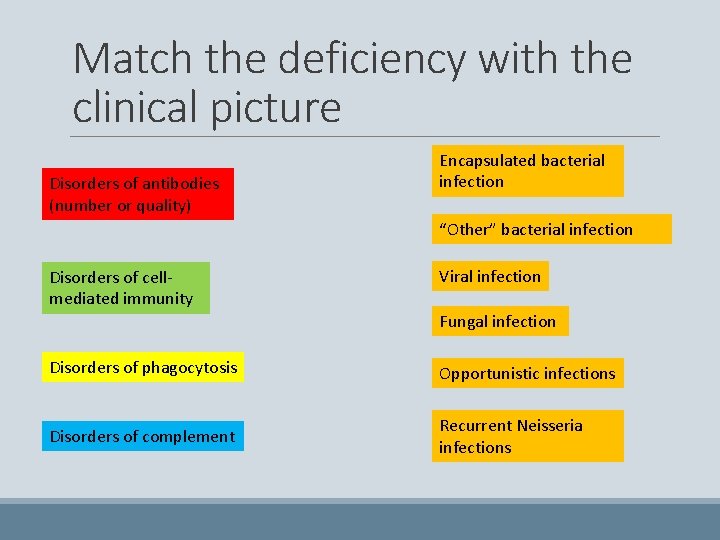
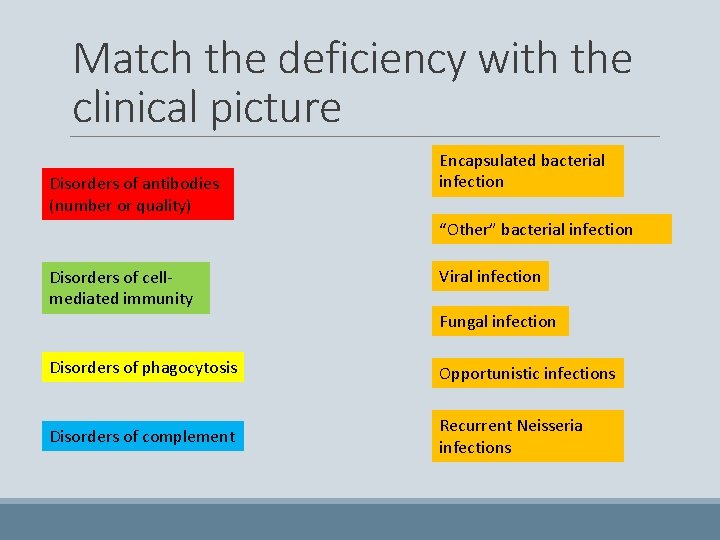
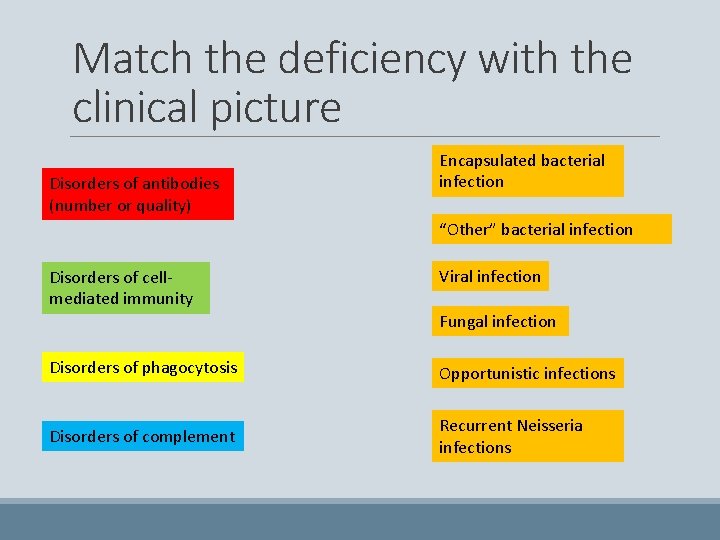
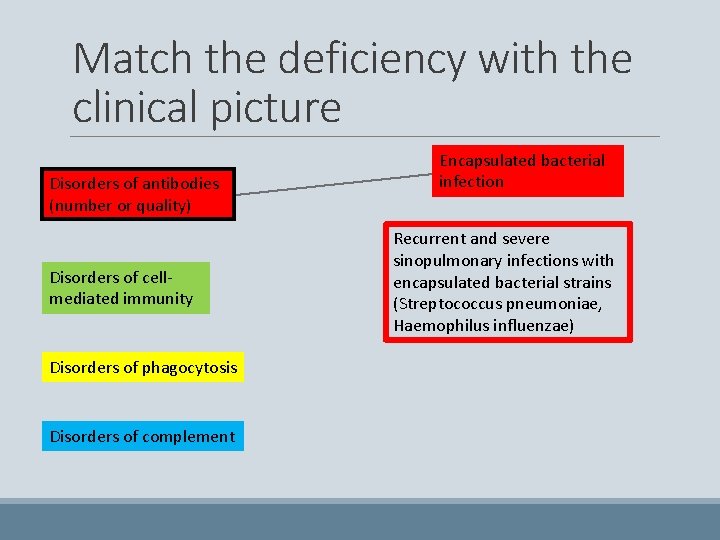
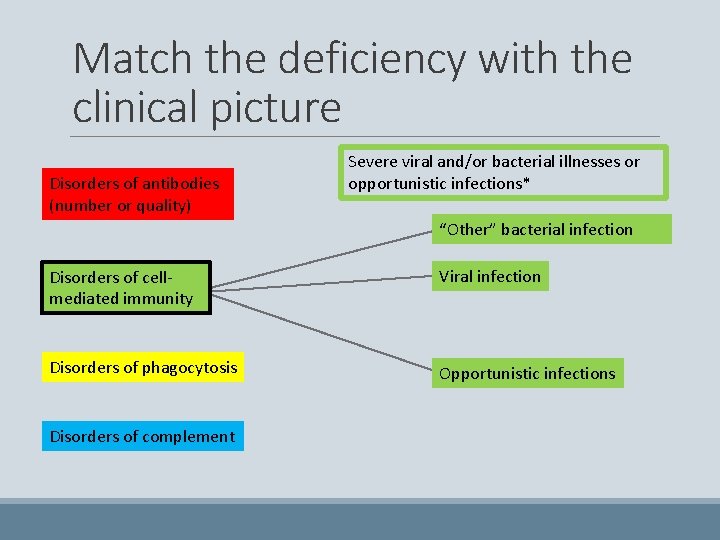
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Encapsulated bacterial infection “Other” bacterial infection Disorders of cellmediated immunity Viral infection Fungal infection Disorders of phagocytosis Opportunistic infections Disorders of complement Recurrent Neisseria infections
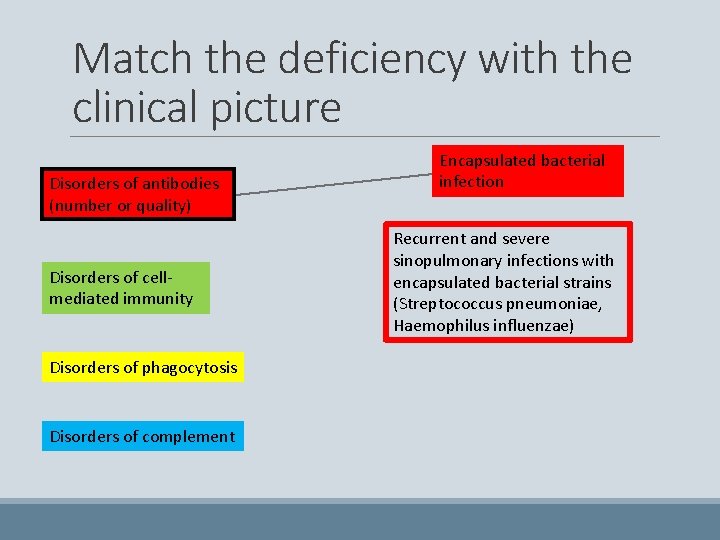
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Disorders of cellmediated immunity Disorders of phagocytosis Disorders of complement Encapsulated bacterial infection Recurrent and severe sinopulmonary infections with encapsulated bacterial strains (Streptococcus pneumoniae, Haemophilus influenzae)
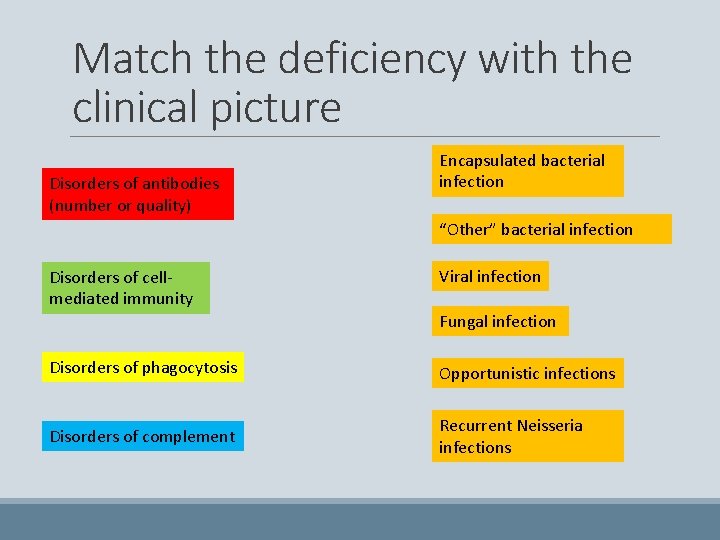
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Encapsulated bacterial infection “Other” bacterial infection Disorders of cellmediated immunity Viral infection Fungal infection Disorders of phagocytosis Opportunistic infections Disorders of complement Recurrent Neisseria infections
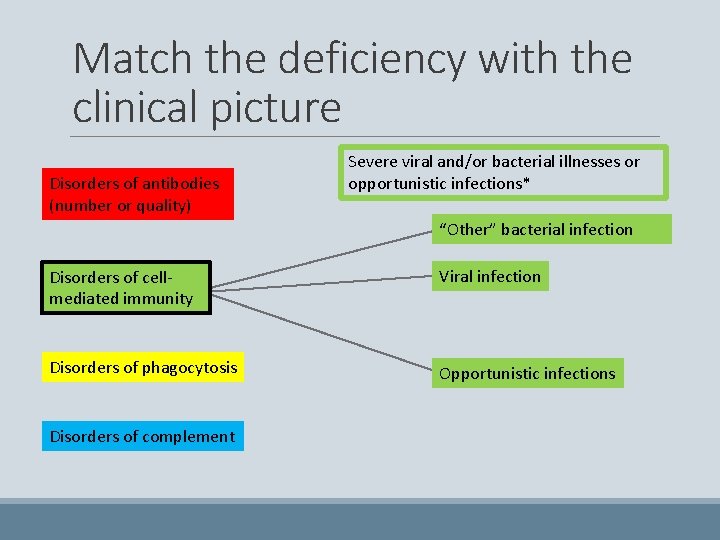
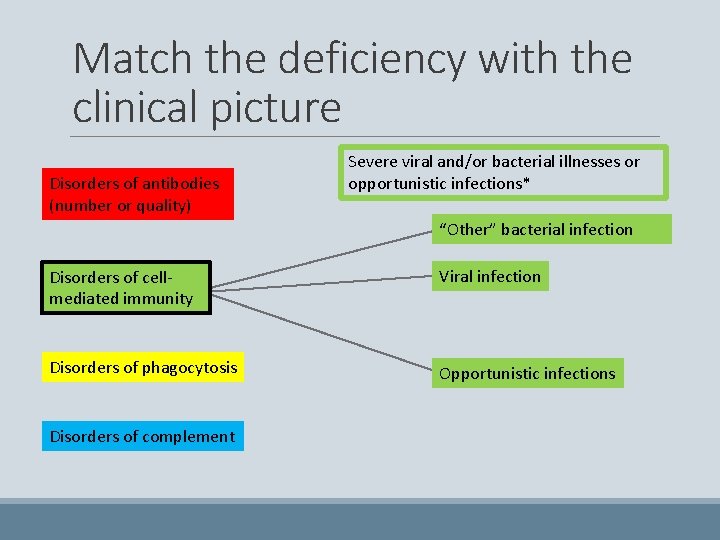
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Severe viral and/or bacterial illnesses or opportunistic infections* “Other” bacterial infection Disorders of cellmediated immunity Viral infection Disorders of phagocytosis Opportunistic infections Disorders of complement
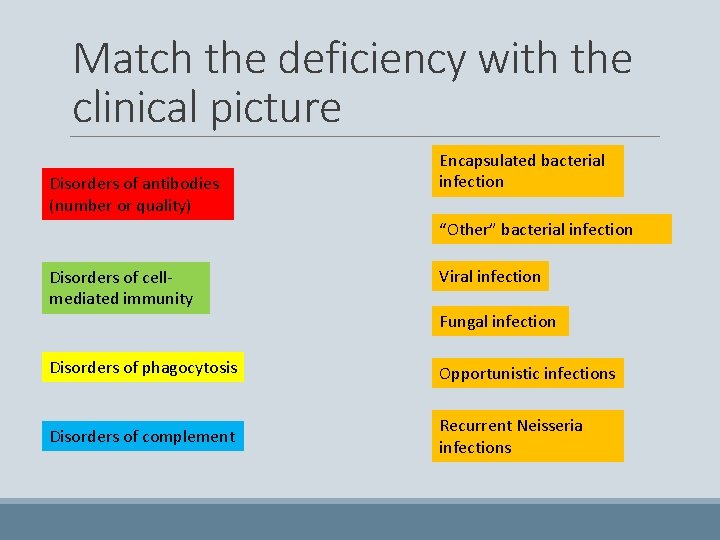
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Encapsulated bacterial infection “Other” bacterial infection Disorders of cellmediated immunity Viral infection Fungal infection Disorders of phagocytosis Opportunistic infections Disorders of complement Recurrent Neisseria infections
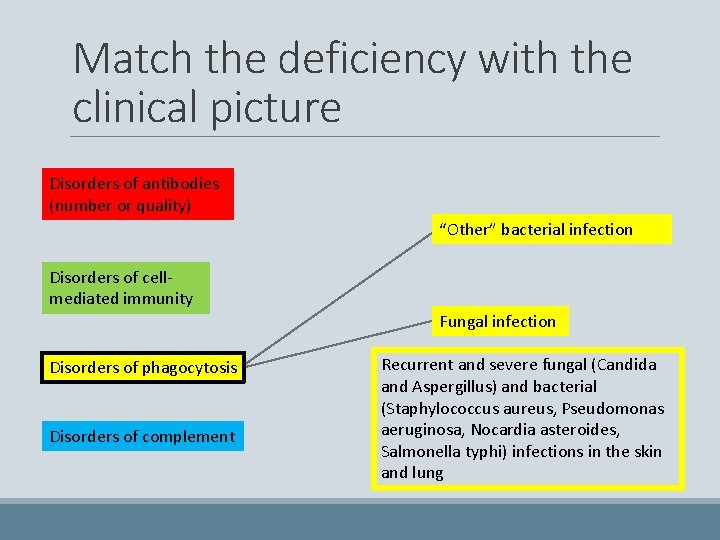
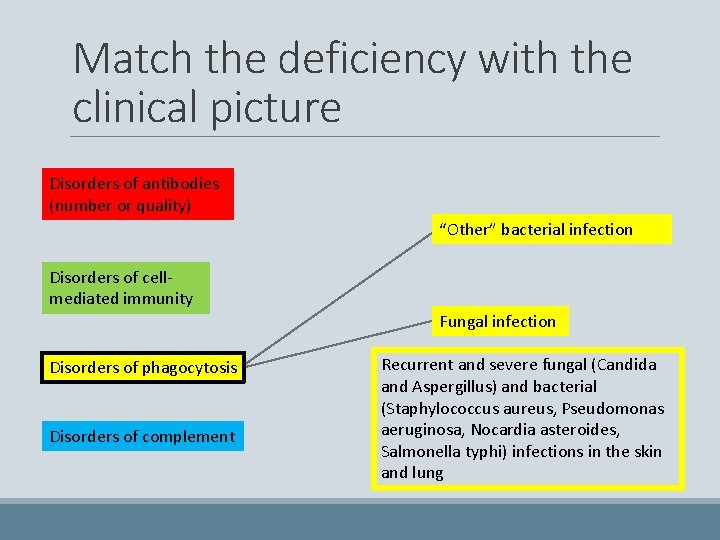
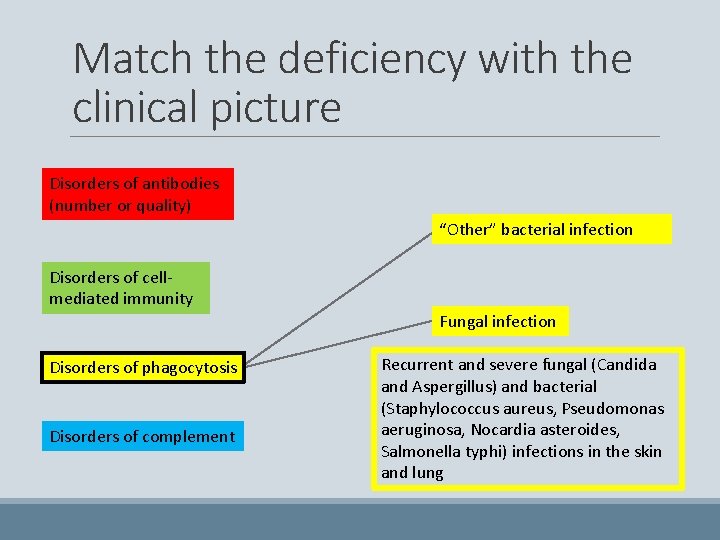
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) “Other” bacterial infection Disorders of cellmediated immunity Fungal infection Disorders of phagocytosis Disorders of complement Recurrent and severe fungal (Candida and Aspergillus) and bacterial (Staphylococcus aureus, Pseudomonas aeruginosa, Nocardia asteroides, Salmonella typhi) infections in the skin and lung
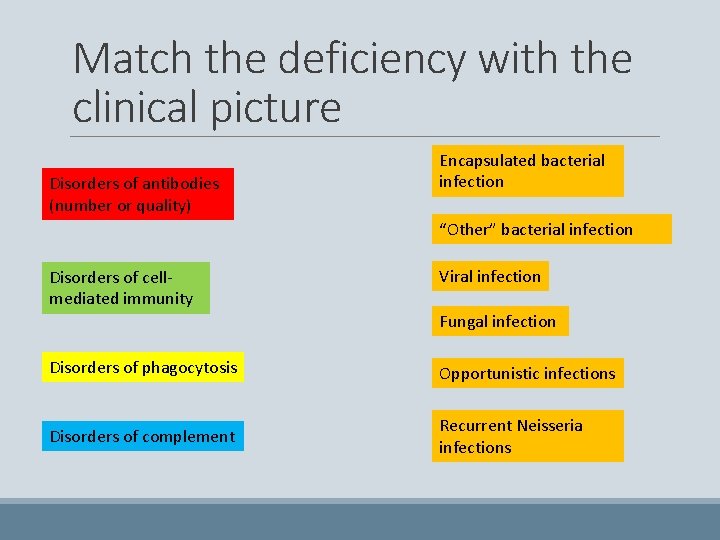
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Encapsulated bacterial infection “Other” bacterial infection Disorders of cellmediated immunity Viral infection Fungal infection Disorders of phagocytosis Opportunistic infections Disorders of complement Recurrent Neisseria infections
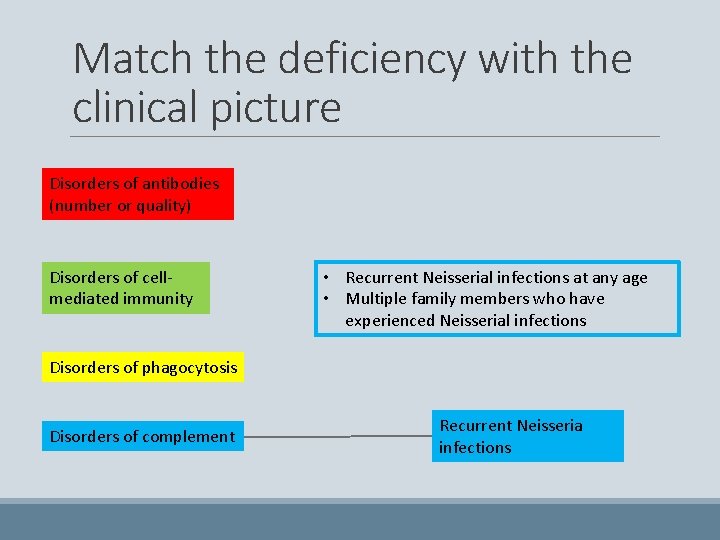
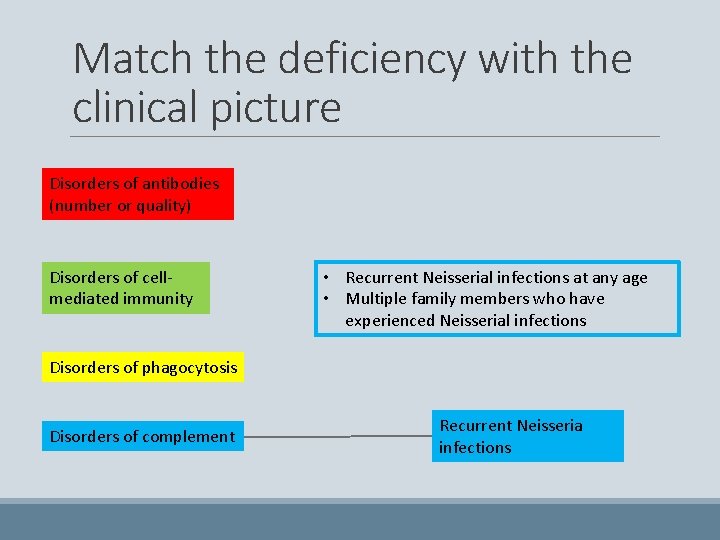
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Disorders of cellmediated immunity • Recurrent Neisserial infections at any age • Multiple family members who have experienced Neisserial infections Disorders of phagocytosis Disorders of complement Recurrent Neisseria infections
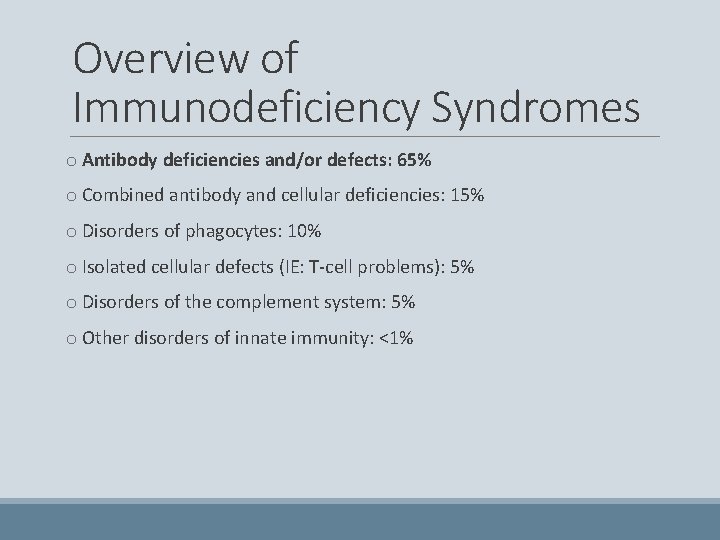
Overview of Immunodeficiency Syndromes o Antibody deficiencies and/or defects: 65% o Combined antibody and cellular deficiencies: 15% o Disorders of phagocytes: 10% o Isolated cellular defects (IE: T-cell problems): 5% o Disorders of the complement system: 5% o Other disorders of innate immunity: <1%
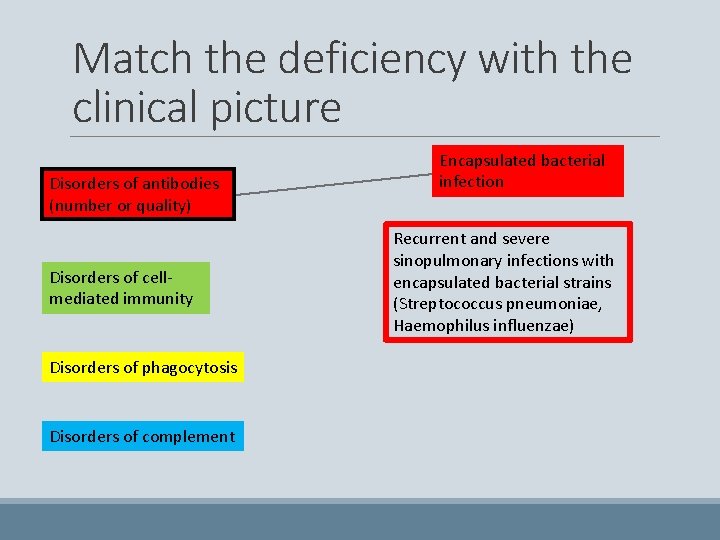
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Disorders of cellmediated immunity Disorders of phagocytosis Disorders of complement Encapsulated bacterial infection Recurrent and severe sinopulmonary infections with encapsulated bacterial strains (Streptococcus pneumoniae, Haemophilus influenzae)
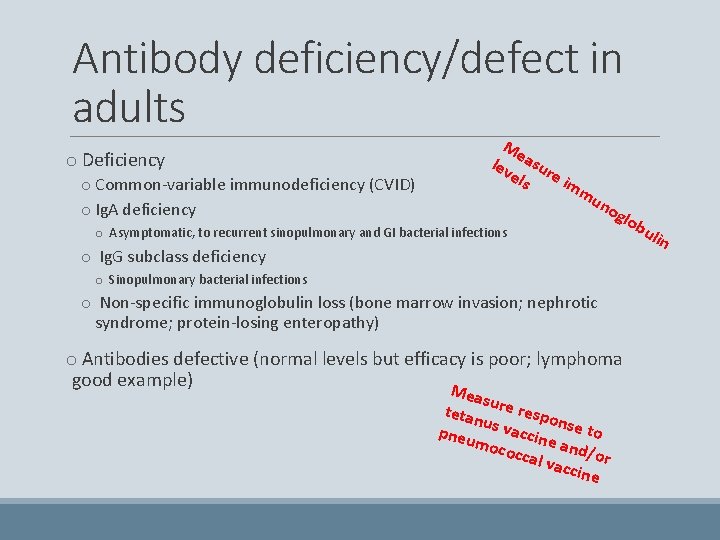
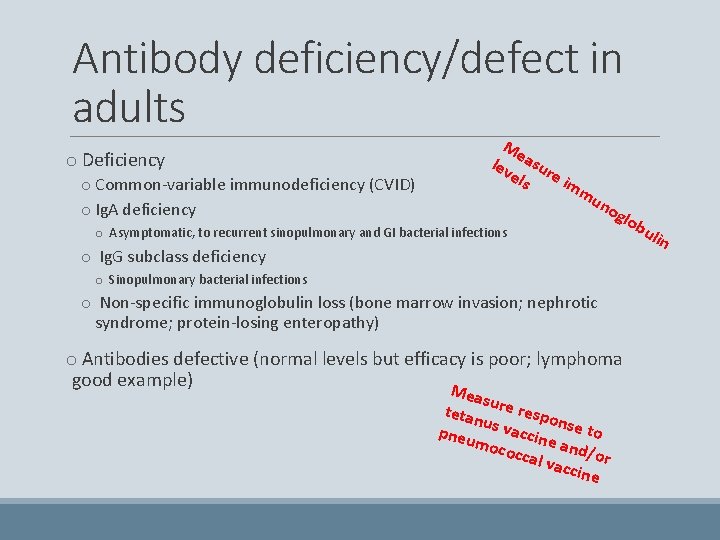
Antibody deficiency/defect in adults o Deficiency o Common-variable immunodeficiency (CVID) o Ig. A deficiency Me lev asur els e im mu o Asymptomatic, to recurrent sinopulmonary and GI bacterial infections no glo o Ig. G subclass deficiency o Sinopulmonary bacterial infections o Non-specific immunoglobulin loss (bone marrow invasion; nephrotic syndrome; protein-losing enteropathy) o Antibodies defective (normal levels but efficacy is poor; lymphoma good example) M easu tetan re respo n u pneu s vaccin se to ea moco ccal nd/or vacc ine bu lin
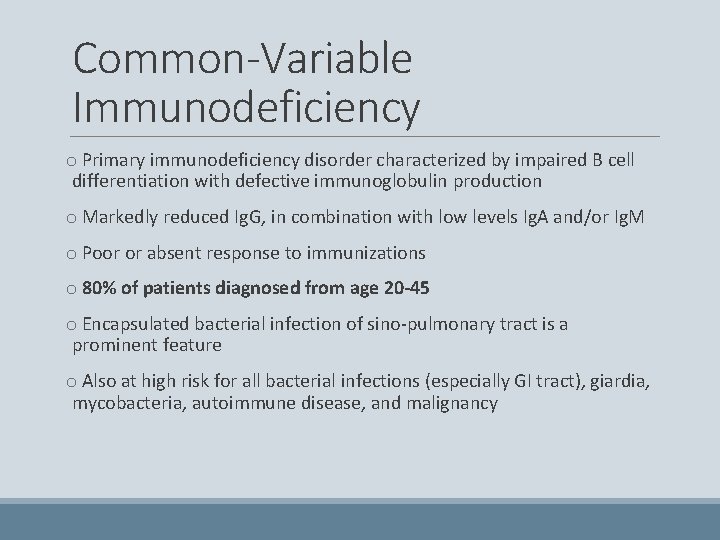
Common-Variable Immunodeficiency o Primary immunodeficiency disorder characterized by impaired B cell differentiation with defective immunoglobulin production o Markedly reduced Ig. G, in combination with low levels Ig. A and/or Ig. M o Poor or absent response to immunizations o 80% of patients diagnosed from age 20 -45 o Encapsulated bacterial infection of sino-pulmonary tract is a prominent feature o Also at high risk for all bacterial infections (especially GI tract), giardia, mycobacteria, autoimmune disease, and malignancy
Overview of Immunodeficiency Syndromes o Antibody deficiencies and/or defects: 65% o Combined antibody and cellular deficiencies: 15% o Disorders of phagocytes: 10% o Isolated cellular defects (IE: T-cell problems): 5% o Disorders of the complement system: 5% o Other disorders of innate immunity: <1%
Overview of Immunodeficiency Syndromes o Antibody deficiencies and/or defects: 65% o Combined antibody and cellular deficiencies: 15% o Disorders of phagocytes: 10% o Isolated cellular defects (IE: T-cell problems): 5% o Disorders of the complement system: 5% o Other disorders of innate immunity: <1%
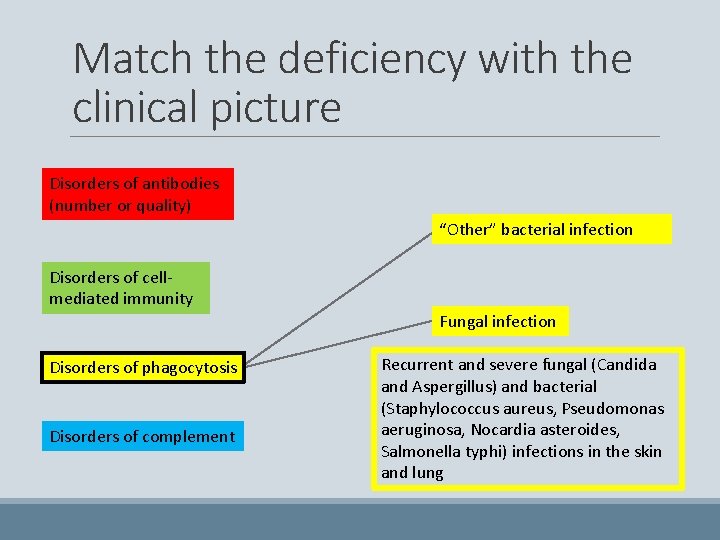
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) “Other” bacterial infection Disorders of cellmediated immunity Fungal infection Disorders of phagocytosis Disorders of complement Recurrent and severe fungal (Candida and Aspergillus) and bacterial (Staphylococcus aureus, Pseudomonas aeruginosa, Nocardia asteroides, Salmonella typhi) infections in the skin and lung
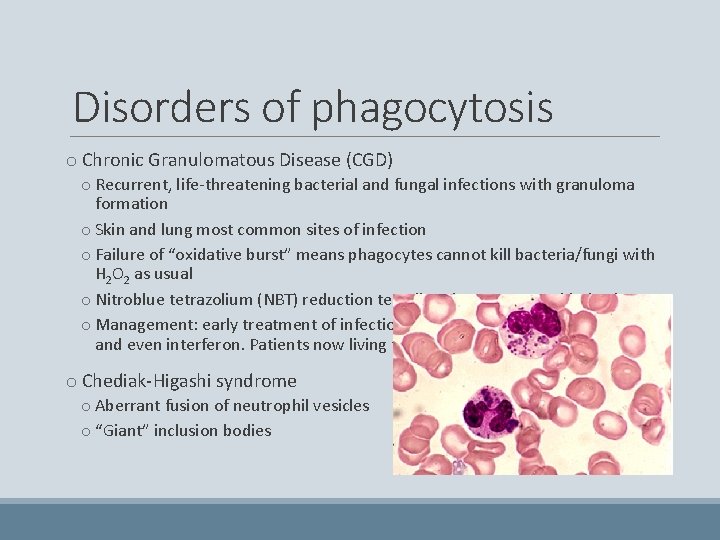
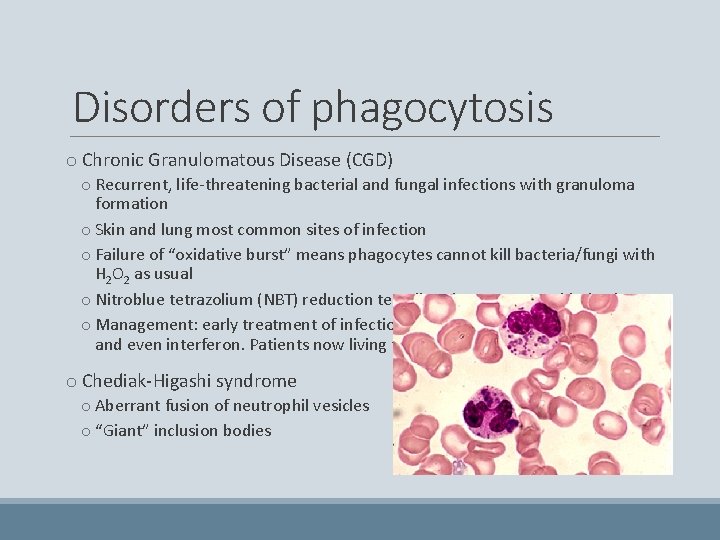
Disorders of phagocytosis o Chronic Granulomatous Disease (CGD) o Recurrent, life-threatening bacterial and fungal infections with granuloma formation o Skin and lung most common sites of infection o Failure of “oxidative burst” means phagocytes cannot kill bacteria/fungi with H 2 O 2 as usual o Nitroblue tetrazolium (NBT) reduction test directly measures oxidative burst o Management: early treatment of infections; prophylaxis with Bactrim, azole, and even interferon. Patients now living to middle-age. o Chediak-Higashi syndrome o Aberrant fusion of neutrophil vesicles o “Giant” inclusion bodies
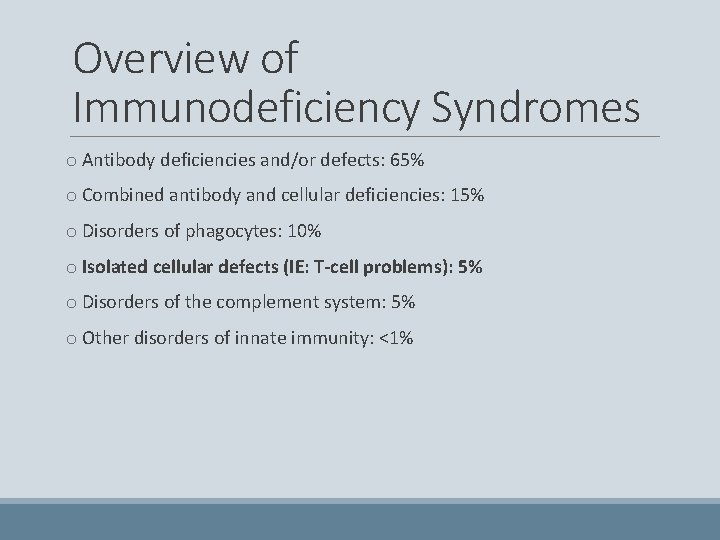
Overview of Immunodeficiency Syndromes o Antibody deficiencies and/or defects: 65% o Combined antibody and cellular deficiencies: 15% o Disorders of phagocytes: 10% o Isolated cellular defects (IE: T-cell problems): 5% o Disorders of the complement system: 5% o Other disorders of innate immunity: <1%
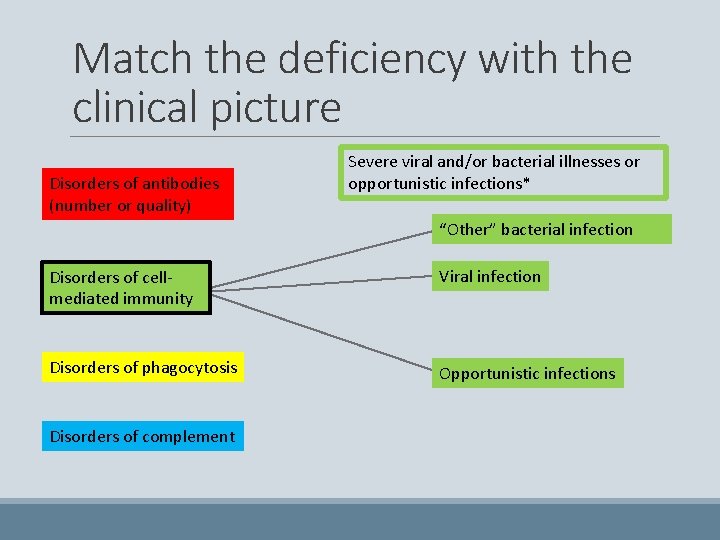
Match the deficiency with the clinical picture Disorders of antibodies (number or quality) Severe viral and/or bacterial illnesses or opportunistic infections* “Other” bacterial infection Disorders of cellmediated immunity Viral infection Disorders of phagocytosis Opportunistic infections Disorders of complement
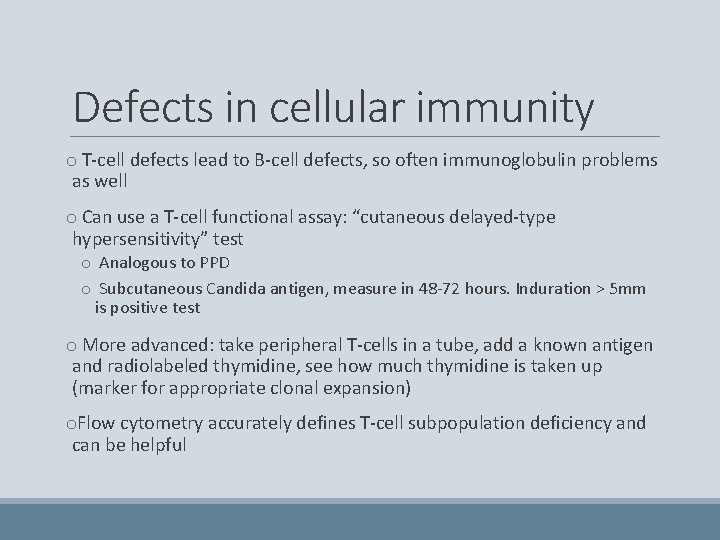
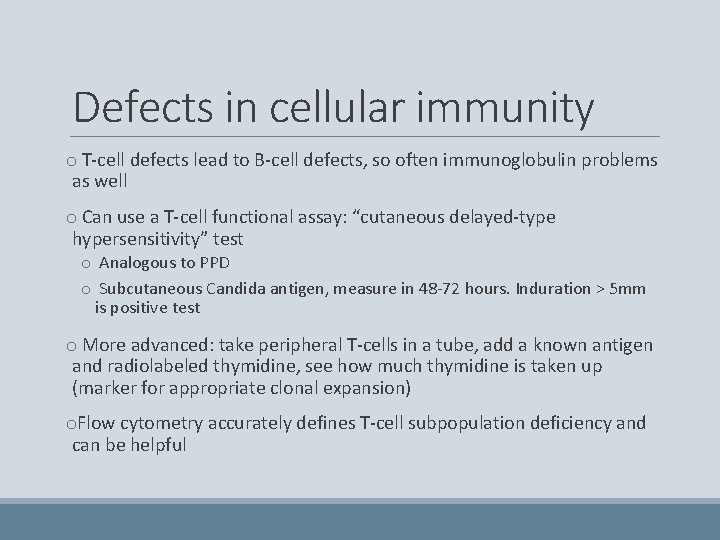
Defects in cellular immunity o T-cell defects lead to B-cell defects, so often immunoglobulin problems as well o Can use a T-cell functional assay: “cutaneous delayed-type hypersensitivity” test o Analogous to PPD o Subcutaneous Candida antigen, measure in 48 -72 hours. Induration > 5 mm is positive test o More advanced: take peripheral T-cells in a tube, add a known antigen and radiolabeled thymidine, see how much thymidine is taken up (marker for appropriate clonal expansion) o. Flow cytometry accurately defines T-cell subpopulation deficiency and can be helpful
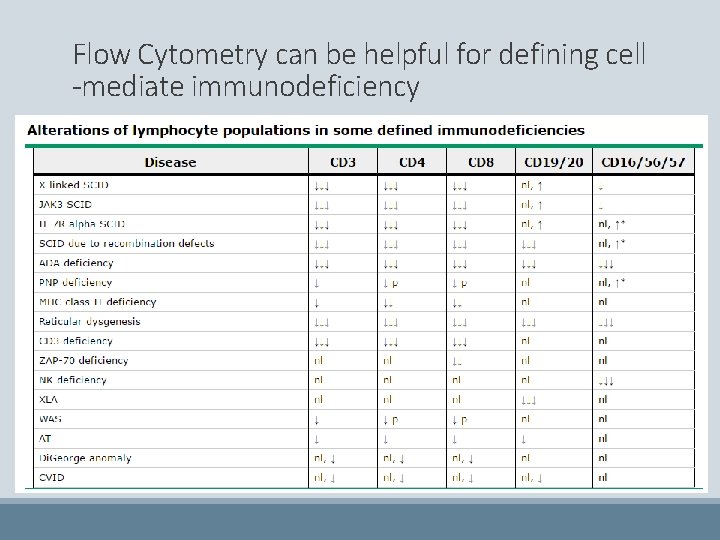
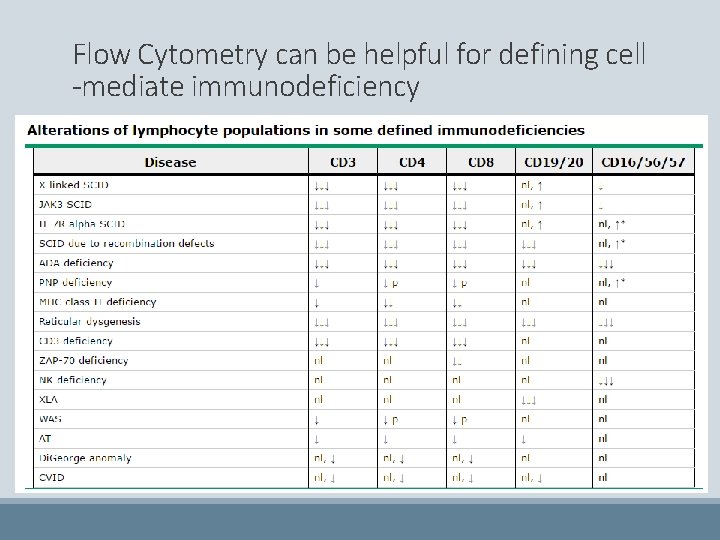
Flow Cytometry can be helpful for defining cell -mediate immunodeficiency
Overview of Immunodeficiency Syndromes o Antibody deficiencies and/or defects: 65% o Combined antibody and cellular deficiencies: 15% o Disorders of phagocytes: 10% • Te rmina o Isolated cellular defects (IE: T-cell problems): 5% casca l complem de de ficien ent i n o Disorders of the complement system: 5% creas cy es Ne • Me i sseria asure risk c o Other disorders of innate immunity: <1% onval comp • Co lement le escent nside r SLE vels
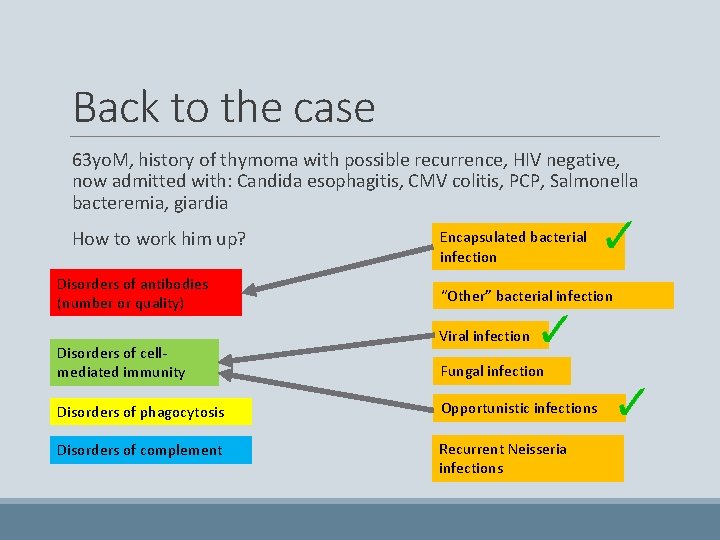
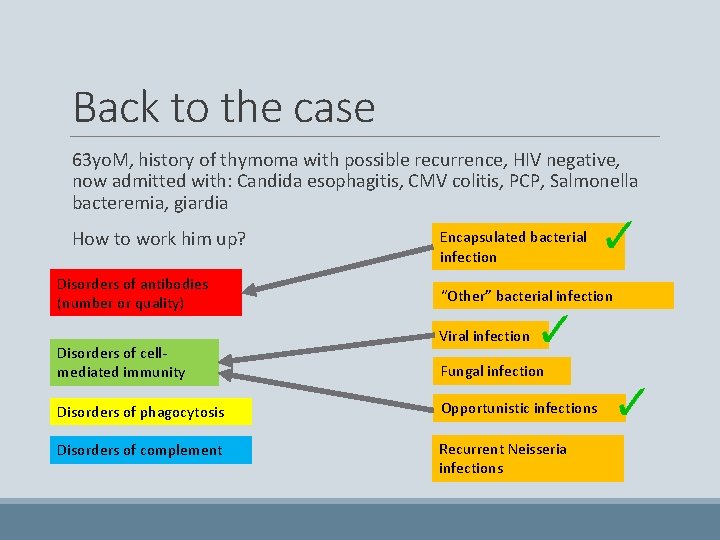
Back to the case 63 yo. M, history of thymoma with possible recurrence, HIV negative, now admitted with: Candida esophagitis, CMV colitis, PCP, Salmonella bacteremia, giardia How to work him up? Disorders of antibodies (number or quality) Disorders of cellmediated immunity Encapsulated bacterial infection “Other” bacterial infection Viral infection Fungal infection Disorders of phagocytosis Opportunistic infections Disorders of complement Recurrent Neisseria infections
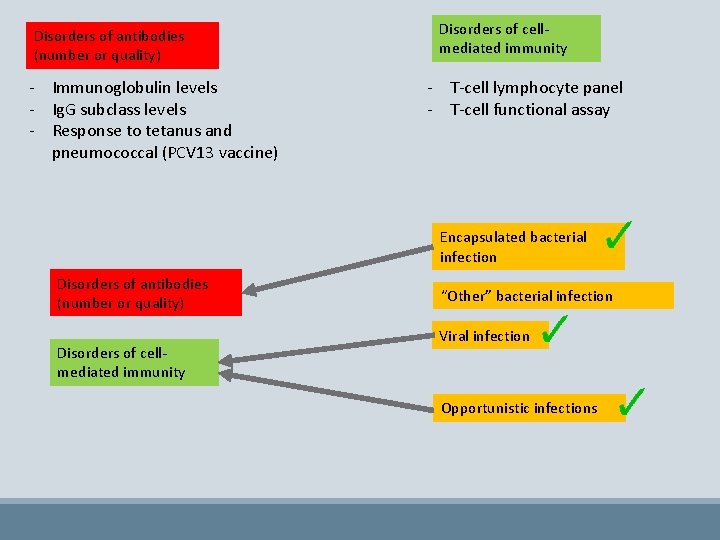
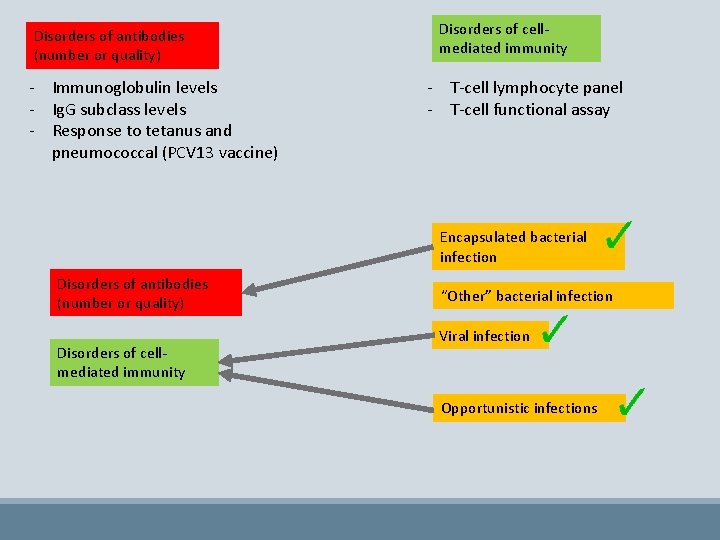
Disorders of antibodies (number or quality) - Immunoglobulin levels - Ig. G subclass levels - Response to tetanus and pneumococcal (PCV 13 vaccine) Disorders of cellmediated immunity - T-cell lymphocyte panel - T-cell functional assay Encapsulated bacterial infection Disorders of antibodies (number or quality) Disorders of cellmediated immunity “Other” bacterial infection Viral infection Opportunistic infections
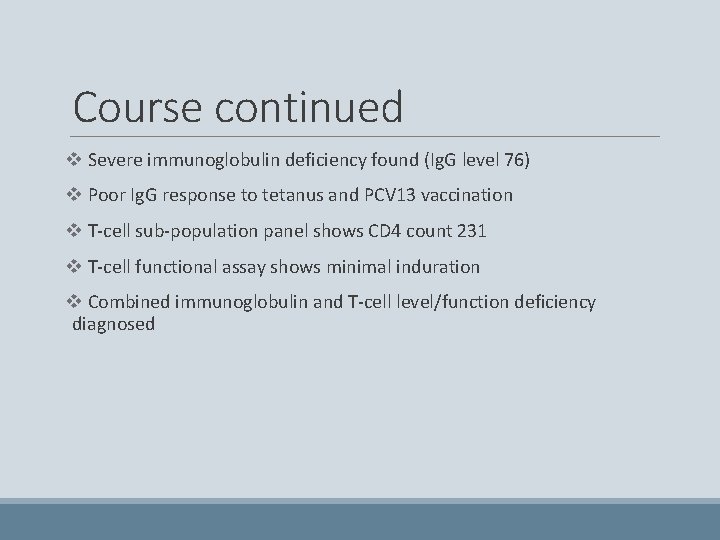
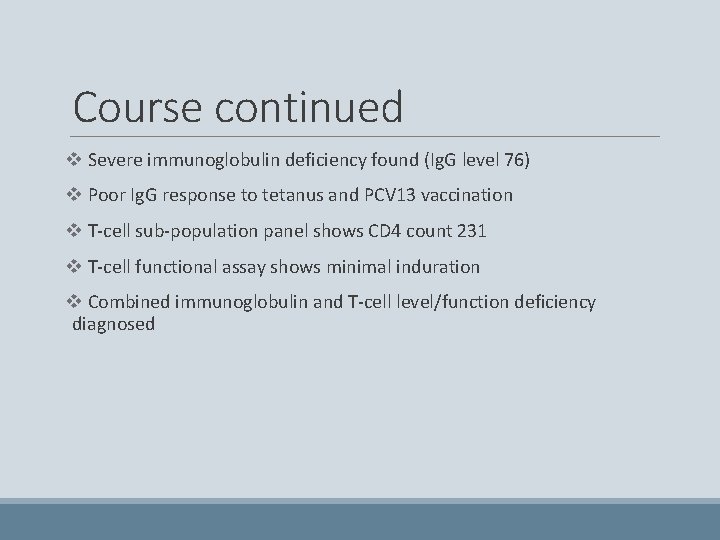
Course continued v Severe immunoglobulin deficiency found (Ig. G level 76) v Poor Ig. G response to tetanus and PCV 13 vaccination v T-cell sub-population panel shows CD 4 count 231 v T-cell functional assay shows minimal induration v Combined immunoglobulin and T-cell level/function deficiency diagnosed
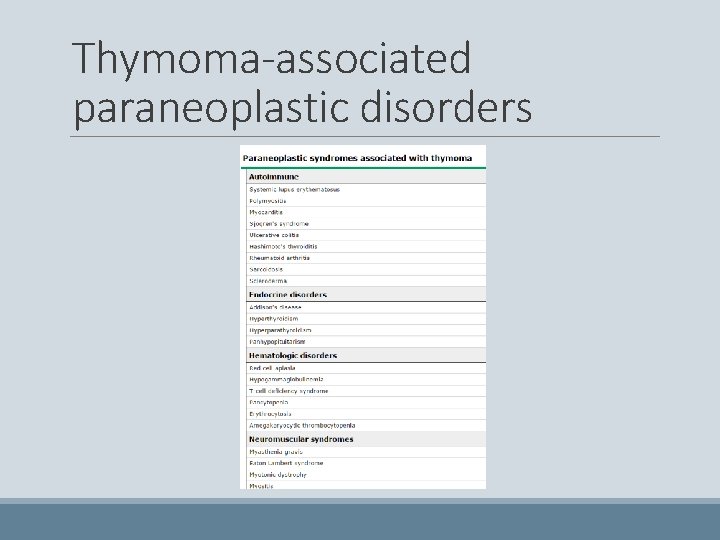
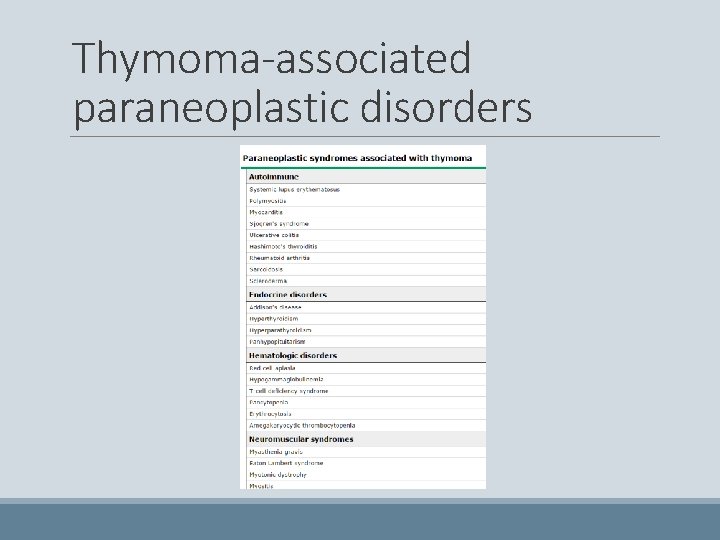
Thymoma-associated paraneoplastic disorders
v Good’s syndrome (thymoma with immunodeficiency) is a rare cause of combined B and T cell immunodeficiency in adults. v The clinical characteristics of Good’s syndrome are increased susceptibility to bacterial infections with encapsulated organisms and opportunistic viral and fungal infections
Patient outcome v. He is started on ganciclovir, fluconazole, ceftriaxone, Bactrim, and metronidazole v Discharged home after 35 day admission on valgancyclovir, fluconazole, and Bactrim prophylaxis v His recurrent thymoma is treated v Several more infections, though overall doing well
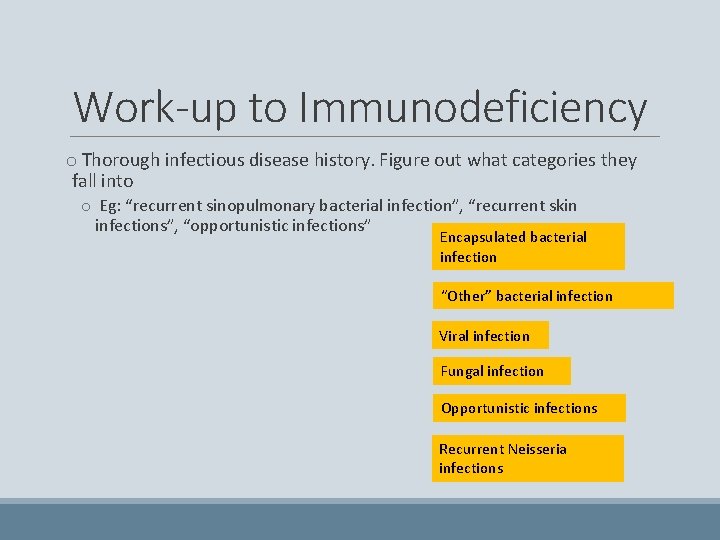
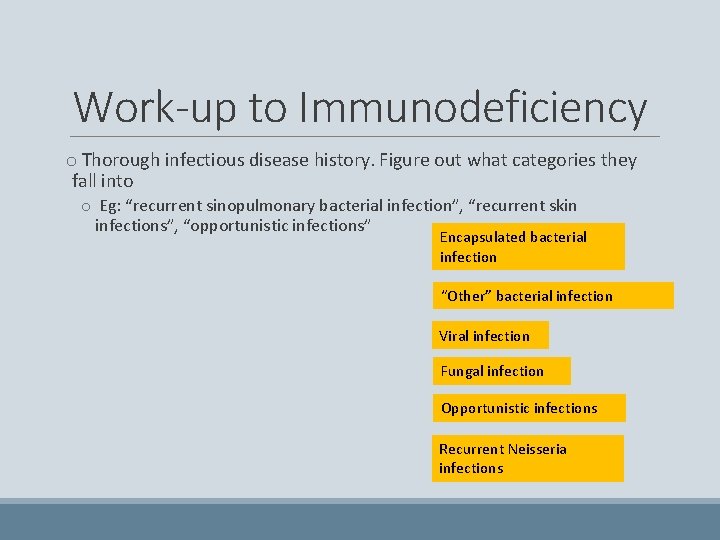
Work-up to Immunodeficiency o Thorough infectious disease history. Figure out what categories they fall into o Eg: “recurrent sinopulmonary bacterial infection”, “recurrent skin infections”, “opportunistic infections” Encapsulated bacterial infection “Other” bacterial infection Viral infection Fungal infection Opportunistic infections Recurrent Neisseria infections
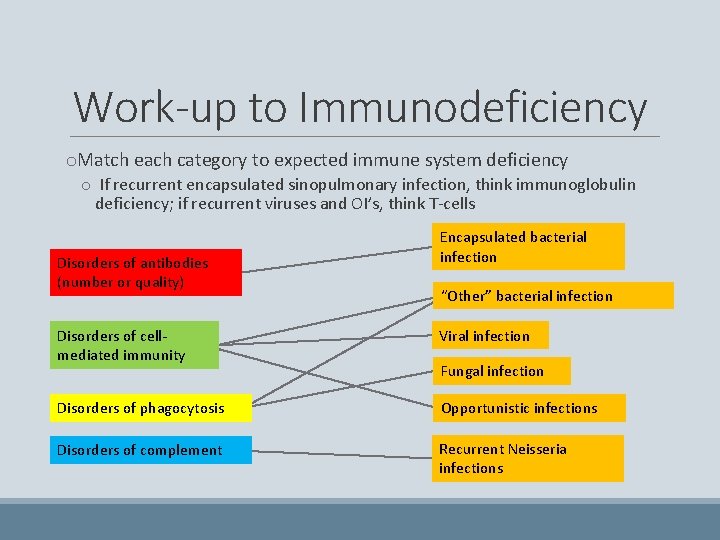
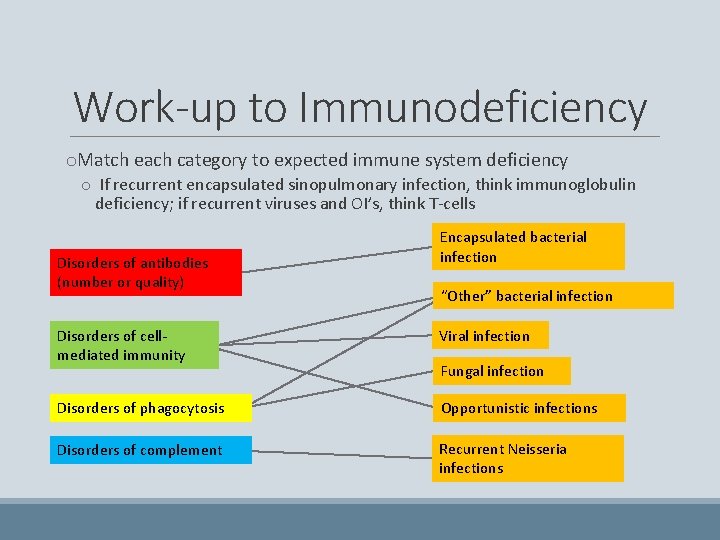
Work-up to Immunodeficiency o. Match each category to expected immune system deficiency o If recurrent encapsulated sinopulmonary infection, think immunoglobulin deficiency; if recurrent viruses and OI’s, think T-cells Disorders of antibodies (number or quality) Encapsulated bacterial infection “Other” bacterial infection Disorders of cellmediated immunity Viral infection Disorders of phagocytosis Opportunistic infections Disorders of complement Recurrent Neisseria infections Fungal infection
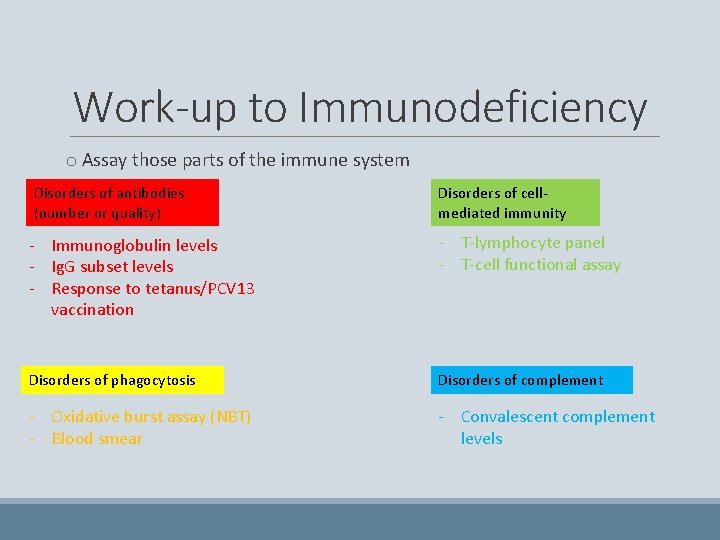
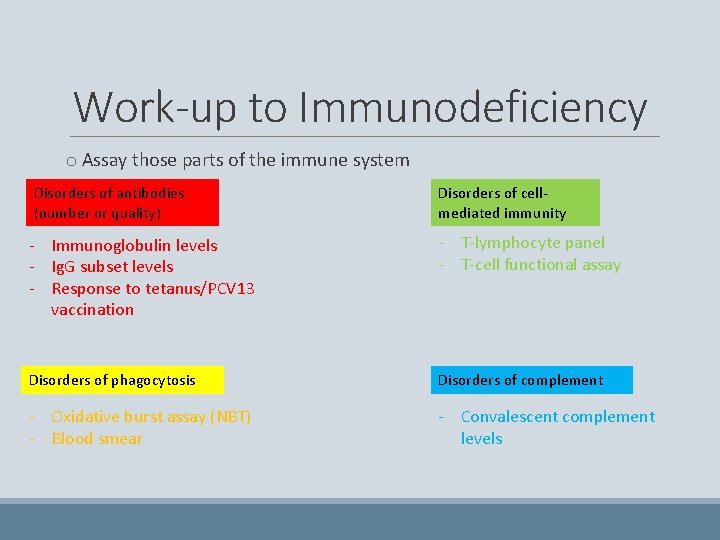
Work-up to Immunodeficiency o Assay those parts of the immune system Disorders of antibodies (number or quality) Disorders of cellmediated immunity - Immunoglobulin levels - Ig. G subset levels - Response to tetanus/PCV 13 vaccination - T-lymphocyte panel - T-cell functional assay Disorders of phagocytosis Disorders of complement - Oxidative burst assay (NBT) - Blood smear - Convalescent complement levels
Work-up to Immunodeficiency o Once you’ve defined what components of the immune system are down, considering the patients age and clinical context, hit the books (or Up. To. Date) to see what specific syndrome is a match
Congratulations on finishing the Primary Immunodeficiency Module! Please take this brief pre-module quiz https: //goo. gl/forms/8 h. Tt. Y 4 u 5 cgy. Qk 6 kw 1