PRIMARY CARE Prevention of staff contact events in
- Slides: 6
PRIMARY CARE Prevention of staff contact events in clinical and nonclinical settings – general advice This document is developed as a collaboration between PHE NHSE/I CCG IPC Leads With thanks and acknowledgement to the Leeds Teaching Hospitals NHS Trust Date: 20. 10. 20 Version: 7. 0
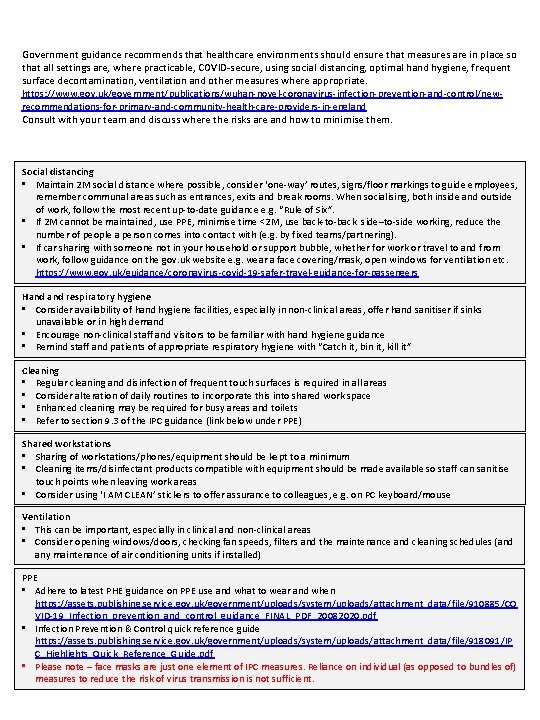
Government guidance recommends that healthcare environments should ensure that measures are in place so that all settings are, where practicable, COVID-secure, using social distancing, optimal hand hygiene, frequent surface decontamination, ventilation and other measures where appropriate. https: //www. gov. uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/newrecommendations-for-primary-and-community-health-care-providers-in-england Consult with your team and discuss where the risks are and how to minimise them. Social distancing • Maintain 2 M social distance where possible, consider ‘one-way’ routes, signs/floor markings to guide employees, remember communal areas such as entrances, exits and break rooms. When socialising, both inside and outside of work, follow the most recent up-to-date guidance e. g. “Rule of Six”. • If 2 M cannot be maintained, use PPE, minimise time <2 M, use back-to-back side–to-side working, reduce the number of people a person comes into contact with (e. g. by fixed teams/partnering). • If car sharing with someone not in your household or support bubble, whether for work or travel to and from work, follow guidance on the gov. uk website e. g. wear a face covering/mask, open windows for ventilation etc. https: //www. gov. uk/guidance/coronavirus-covid-19 -safer-travel-guidance-for-passengers Hand respiratory hygiene • Consider availability of hand hygiene facilities, especially in non-clinical areas, offer hand sanitiser if sinks unavailable or in high demand • Encourage non-clinical staff and visitors to be familiar with hand hygiene guidance • Remind staff and patients of appropriate respiratory hygiene with “Catch it, bin it, kill it” Cleaning • Regular cleaning and disinfection of frequent touch surfaces is required in all areas • Consider alteration of daily routines to incorporate this into shared work space • Enhanced cleaning may be required for busy areas and toilets • Refer to section 9. 3 of the IPC guidance (link below under PPE) Shared workstations • Sharing of workstations/phones/equipment should be kept to a minimum • Cleaning items/disinfectant products compatible with equipment should be made available so staff can sanitise touch points when leaving work areas • Consider using ‘I AM CLEAN’ stickers to offer assurance to colleagues, e. g. on PC keyboard/mouse Ventilation • This can be important, especially in clinical and non-clinical areas • Consider opening windows/doors, checking fan speeds, filters and the maintenance and cleaning schedules (and any maintenance of air conditioning units if installed) PPE • Adhere to latest PHE guidance on PPE use and what to wear and when https: //assets. publishing. service. gov. uk/government/uploads/system/uploads/attachment_data/file/910885/CO VID-19_Infection_prevention_and_control_guidance_FINAL_PDF_20082020. pdf • Infection Prevention & Control quick reference guide https: //assets. publishing. service. gov. uk/government/uploads/system/uploads/attachment_data/file/918091/IP C_Highlights_Quick_Reference_Guide. pdf • Please note – face masks are just one element of IPC measures. Reliance on individual (as opposed to bundles of) measures to reduce the risk of virus transmission is not sufficient.
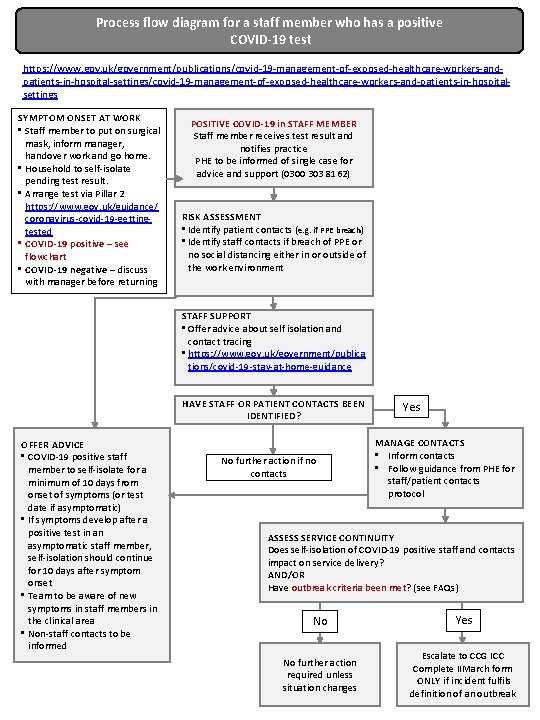
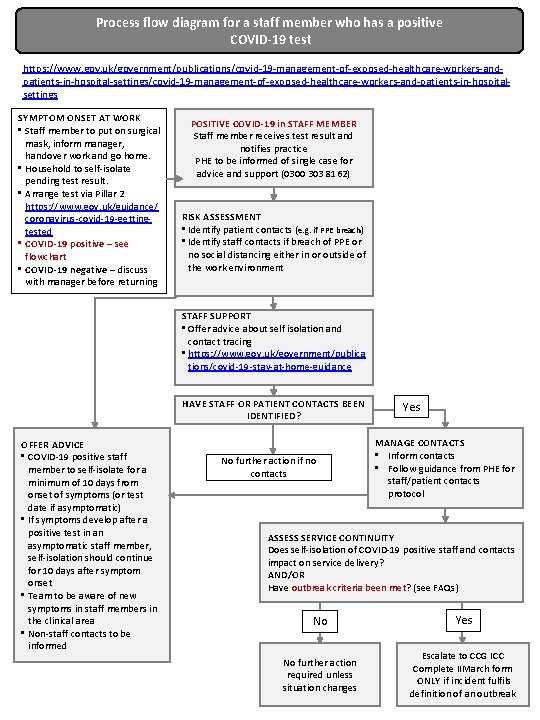
Process flow diagram for a staff member who has a positive COVID-19 test https: //www. gov. uk/government/publications/covid-19 -management-of-exposed-healthcare-workers-andpatients-in-hospital-settings/covid-19 -management-of-exposed-healthcare-workers-and-patients-in-hospitalsettings SYMPTOM ONSET AT WORK • Staff member to put on surgical mask, inform manager, handover work and go home. • Household to self-isolate pending test result. • Arrange test via Pillar 2 https: //www. gov. uk/guidance/ coronavirus-covid-19 -gettingtested • COVID-19 positive – see flowchart • COVID-19 negative – discuss with manager before returning POSITIVE COVID-19 in STAFF MEMBER Staff member receives test result and notifies practice PHE to be informed of single case for advice and support (0300 303 8162) RISK ASSESSMENT • Identify patient contacts (e. g. if PPE breach) • Identify staff contacts if breach of PPE or no social distancing either in or outside of the work environment STAFF SUPPORT • Offer advice about self isolation and contact tracing • https: //www. gov. uk/government/publica tions/covid-19 -stay-at-home-guidance HAVE STAFF OR PATIENT CONTACTS BEEN IDENTIFIED? OFFER ADVICE • COVID-19 positive staff member to self-isolate for a minimum of 10 days from onset of symptoms (or test date if asymptomatic) • If symptoms develop after a positive test in an asymptomatic staff member, self-isolation should continue for 10 days after symptom onset • Team to be aware of new symptoms in staff members in the clinical area • Non-staff contacts to be informed No further action if no contacts Yes MANAGE CONTACTS • Inform contacts • Follow guidance from PHE for staff/patient contacts protocol ASSESS SERVICE CONTINUITY Does self-isolation of COVID-19 positive staff and contacts impact on service delivery? AND/OR Have outbreak criteria been met? (see FAQs) No Yes No further action required unless situation changes Escalate to CCG ICC Complete IIMarch form ONLY if incident fulfils definition of an outbreak
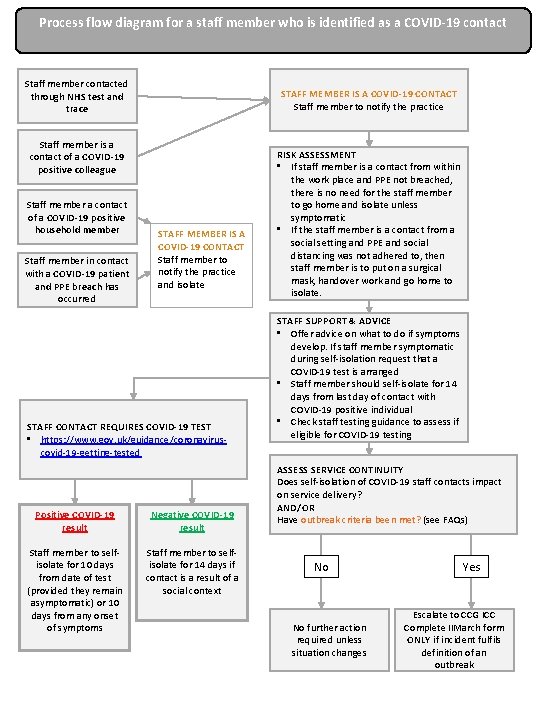
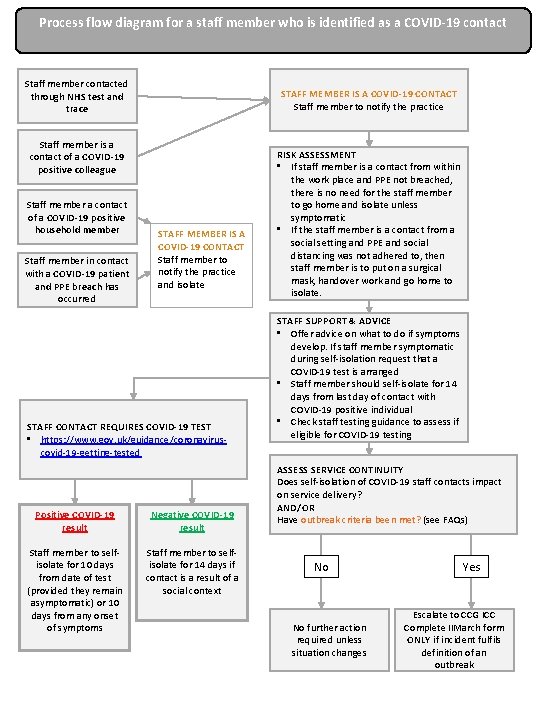
Process flow diagram for a staff member who is identified as a COVID-19 contact Staff member contacted through NHS test and trace STAFF MEMBER IS A COVID-19 CONTACT Staff member to notify the practice Staff member is a contact of a COVID-19 positive colleague Staff member a contact of a COVID-19 positive household member Staff member in contact with a COVID-19 patient and PPE breach has occurred STAFF MEMBER IS A COVID-19 CONTACT Staff member to notify the practice and isolate STAFF CONTACT REQUIRES COVID-19 TEST • https: //www. gov. uk/guidance/coronaviruscovid-19 -getting-tested Positive COVID-19 result Negative COVID-19 result Staff member to selfisolate for 10 days from date of test (provided they remain asymptomatic) or 10 days from any onset of symptoms Staff member to selfisolate for 14 days if contact is a result of a social context RISK ASSESSMENT • If staff member is a contact from within the work place and PPE not breached, there is no need for the staff member to go home and isolate unless symptomatic • If the staff member is a contact from a social setting and PPE and social distancing was not adhered to, then staff member is to put on a surgical mask, handover work and go home to isolate. STAFF SUPPORT & ADVICE • Offer advice on what to do if symptoms develop. If staff member symptomatic during self-isolation request that a COVID-19 test is arranged • Staff member should self-isolate for 14 days from last day of contact with COVID-19 positive individual • Check staff testing guidance to assess if eligible for COVID-19 testing ASSESS SERVICE CONTINUITY Does self-isolation of COVID-19 staff contacts impact on service delivery? AND/OR Have outbreak criteria been met? (see FAQs) No No further action required unless situation changes Yes Escalate to CCG ICC Complete IIMarch form ONLY if incident fulfils definition of an outbreak
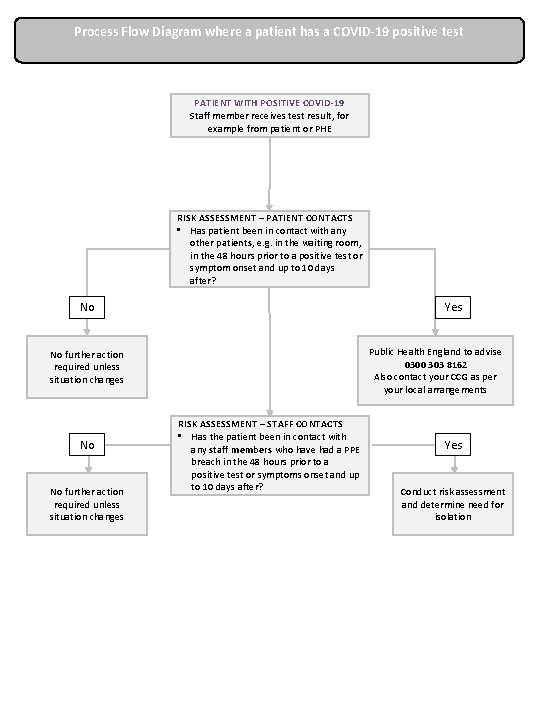
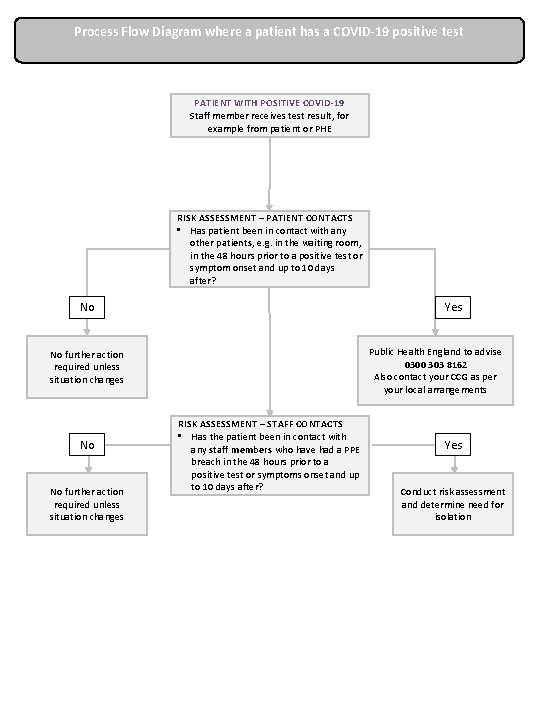
Process Flow Diagram where a patient has a COVID-19 positive test PATIENT WITH POSITIVE COVID-19 Staff member receives test result, for example from patient or PHE RISK ASSESSMENT – PATIENT CONTACTS • Has patient been in contact with any other patients, e. g. in the waiting room, in the 48 hours prior to a positive test or symptom onset and up to 10 days after? No Yes Public Health England to advise 0300 303 8162 Also contact your CCG as per your local arrangements No further action required unless situation changes No No further action required unless situation changes RISK ASSESSMENT – STAFF CONTACTS • Has the patient been in contact with any staff members who have had a PPE breach in the 48 hours prior to a positive test or symptoms onset and up to 10 days after? Yes Conduct risk assessment and determine need for isolation
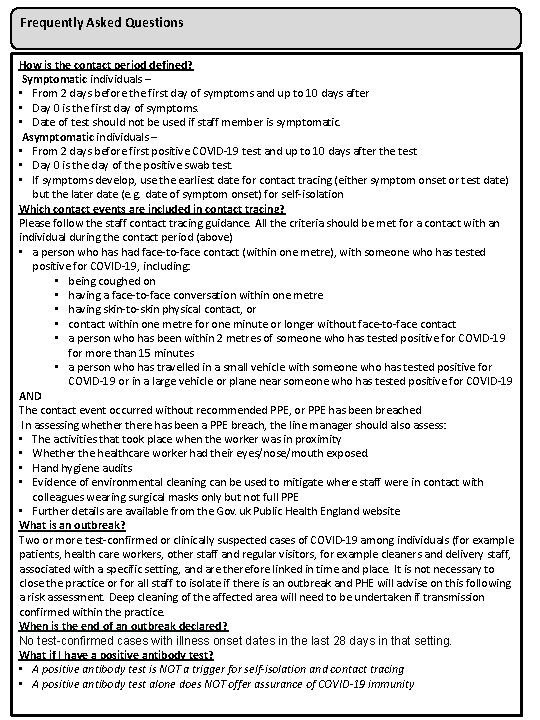
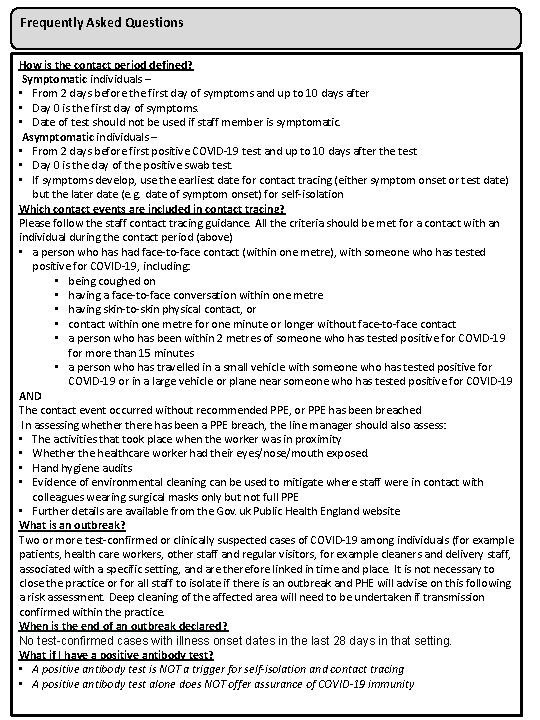
Frequently Asked Questions How is the contact period defined? Symptomatic individuals – • From 2 days before the first day of symptoms and up to 10 days after • Day 0 is the first day of symptoms. • Date of test should not be used if staff member is symptomatic. Asymptomatic individuals – • From 2 days before first positive COVID-19 test and up to 10 days after the test • Day 0 is the day of the positive swab test. • If symptoms develop, use the earliest date for contact tracing (either symptom onset or test date) but the later date (e. g. date of symptom onset) for self-isolation Which contact events are included in contact tracing? Please follow the staff contact tracing guidance. All the criteria should be met for a contact with an individual during the contact period (above) • a person who has had face-to-face contact (within one metre), with someone who has tested positive for COVID-19, including: • being coughed on • having a face-to-face conversation within one metre • having skin-to-skin physical contact, or • contact within one metre for one minute or longer without face-to-face contact • a person who has been within 2 metres of someone who has tested positive for COVID-19 for more than 15 minutes • a person who has travelled in a small vehicle with someone who has tested positive for COVID-19 or in a large vehicle or plane near someone who has tested positive for COVID-19 AND The contact event occurred without recommended PPE, or PPE has been breached In assessing whethere has been a PPE breach, the line manager should also assess: • The activities that took place when the worker was in proximity • Whether the healthcare worker had their eyes/nose/mouth exposed. • Hand hygiene audits • Evidence of environmental cleaning can be used to mitigate where staff were in contact with colleagues wearing surgical masks only but not full PPE • Further details are available from the Gov. uk Public Health England website What is an outbreak? Two or more test-confirmed or clinically suspected cases of COVID-19 among individuals (for example patients, health care workers, other staff and regular visitors, for example cleaners and delivery staff, associated with a specific setting, and are therefore linked in time and place. It is not necessary to close the practice or for all staff to isolate if there is an outbreak and PHE will advise on this following a risk assessment. Deep cleaning of the affected area will need to be undertaken if transmission confirmed within the practice. When is the end of an outbreak declared? No test-confirmed cases with illness onset dates in the last 28 days in that setting. What if I have a positive antibody test? • A positive antibody test is NOT a trigger for self-isolation and contact tracing • A positive antibody test alone does NOT offer assurance of COVID-19 immunity