Primary Care ECG Seminar Dr Sandeep Gandhi 8

































- Slides: 109
Primary Care ECG Seminar Dr Sandeep Gandhi 8 th May 2006
Learning Objectives • Importance of ECG to the primary care health practitioner • Understanding the normal ECG • Learning a structured approach to ECG interpretation • Interpreting the ECG in the clinical context

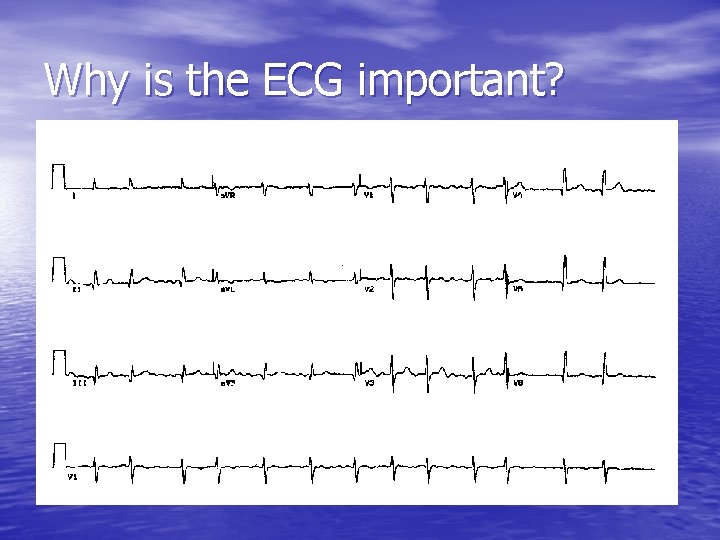
Why is the ECG important for GPs? • As a diagnostic aid in – – – – Chest pain SOB Syncope Presyncope Palpitations Electrolyte disorders hypothermia • As a screening tool – FH of SCD – Looking for end organ damage in HT and diabetes
Why is the ECG important?

QOF 2 Clinical Indicators Clinical indicator CHD Total points 89 Heart failure 20 AF 30 Total 139
Why bother when we have computer assisted interpretation? • Interpretative software is of variable accuracy • Diagnosis of arrhythmias is the Achilles heel of software packages. • Can over diagnose inferior and septal MI. • Can over diagnose LVH in young black people with normal hearts.
Continued • However one study showed how computer aided diagnosis actually improved the diagnostic accuracy when combined with physician evaluation • The best approach is computer and physician evaluation combined
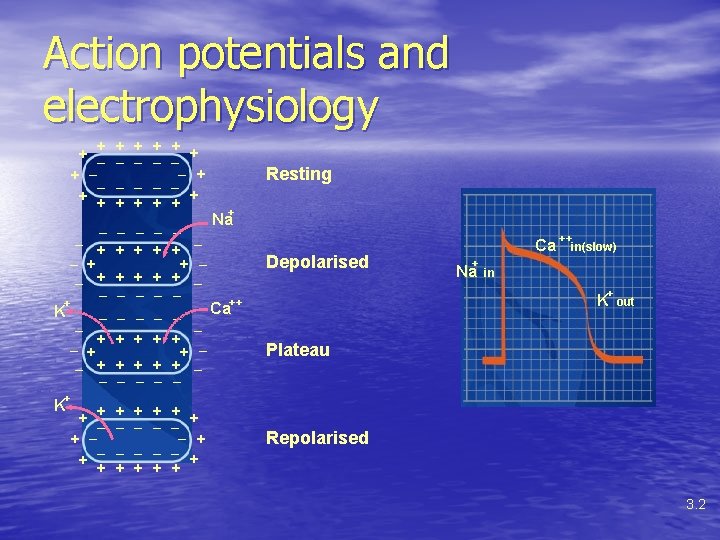
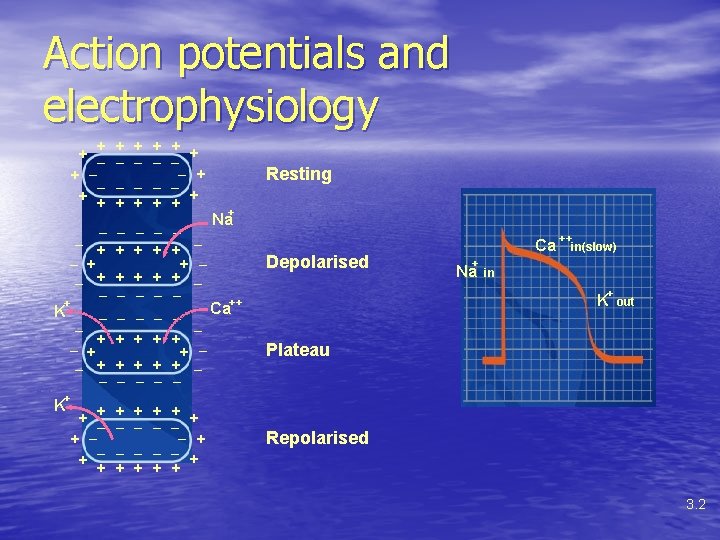
Action potentials and electrophysiology + + _ _ _ _ _ + + + + + __ + + + Na _ _ _ _ + + + _ _ + + + _ _ _ + + + _ _ + + + + + _ _ _ + K _ _ _ + + + + _ _ _ _ _ + + + + K Resting Depolarised Ca + Na ++ in(slow) in + K ++ Ca out Plateau Repolarised 3. 2
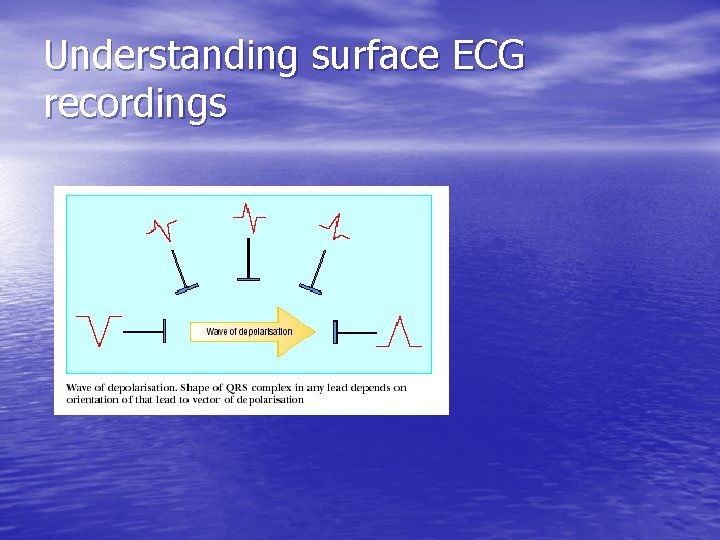
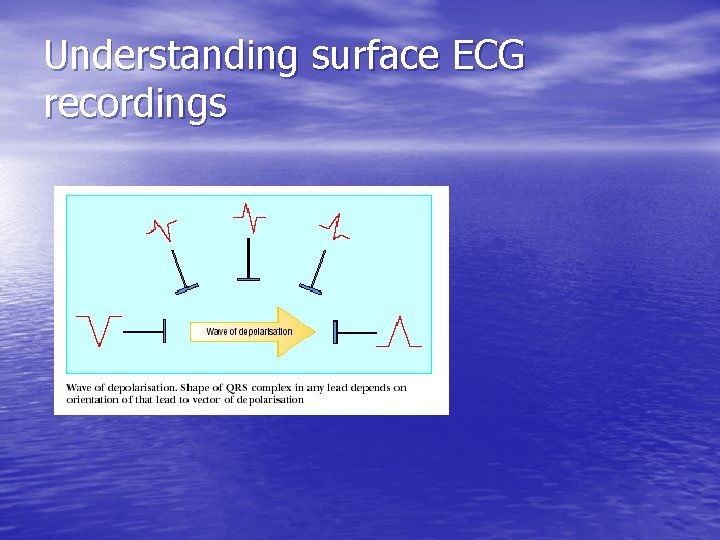
Understanding surface ECG recordings
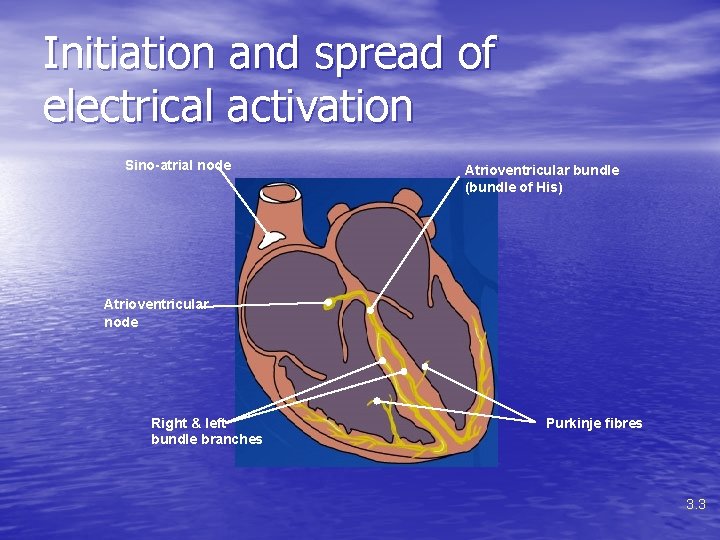
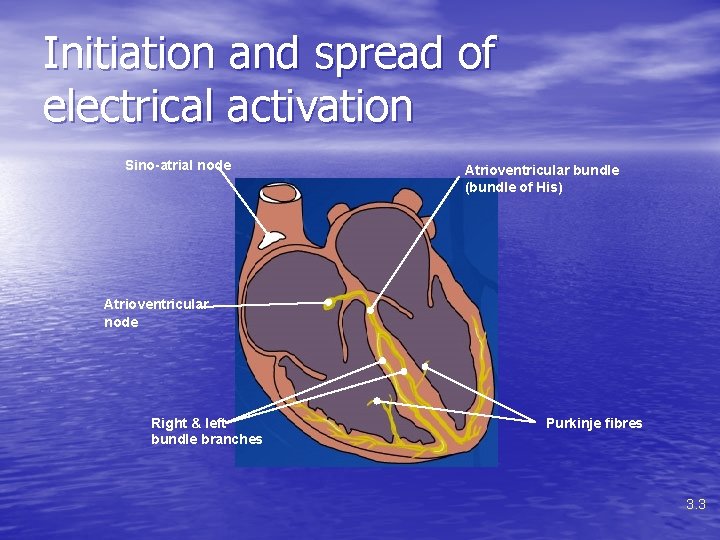
Initiation and spread of electrical activation Sino-atrial node Atrioventricular bundle (bundle of His) Atrioventricular node Right & left bundle branches Purkinje fibres 3. 3
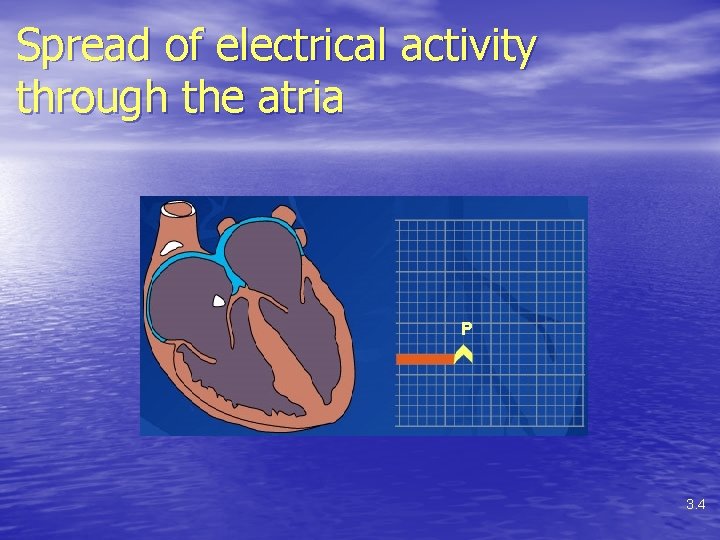
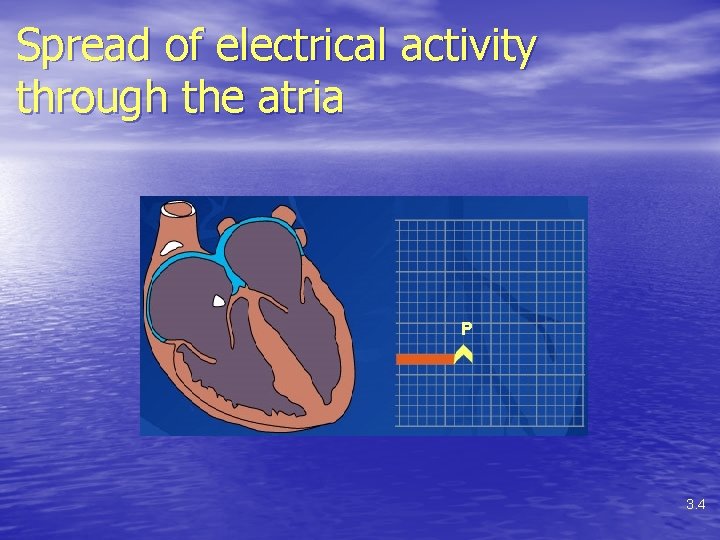
Spread of electrical activity through the atria P 3. 4

Atrioventricular node and the bundle of His 3. 5

Spread of electrical activity throughout the ventricle R T Q S Depolarisation of Ventricles Repolarisation 3. 6
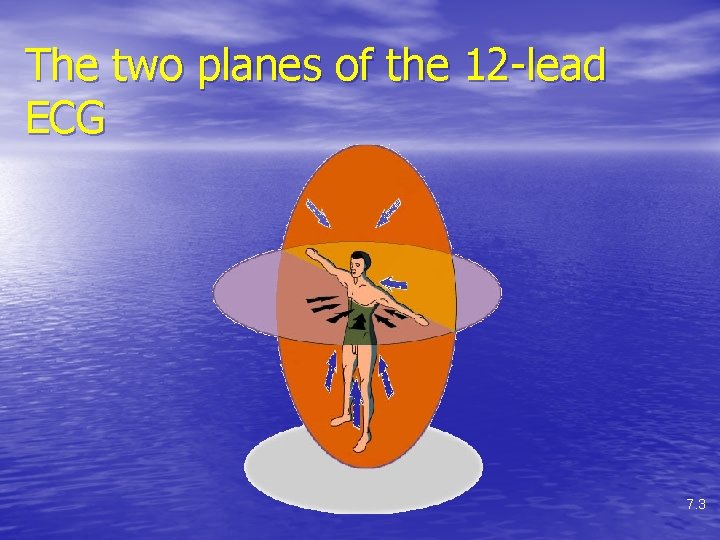
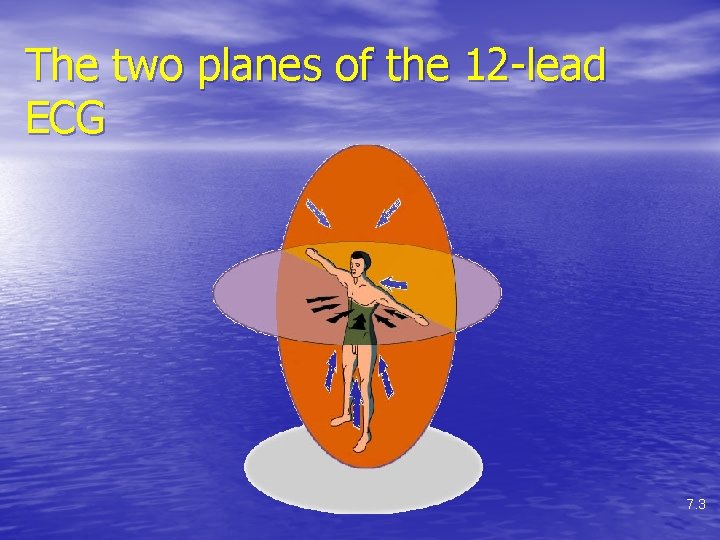
The two planes of the 12 -lead ECG 7. 3
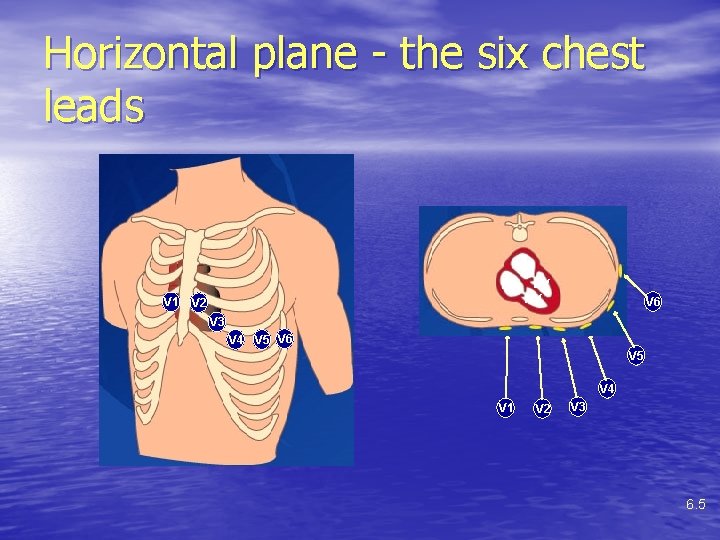
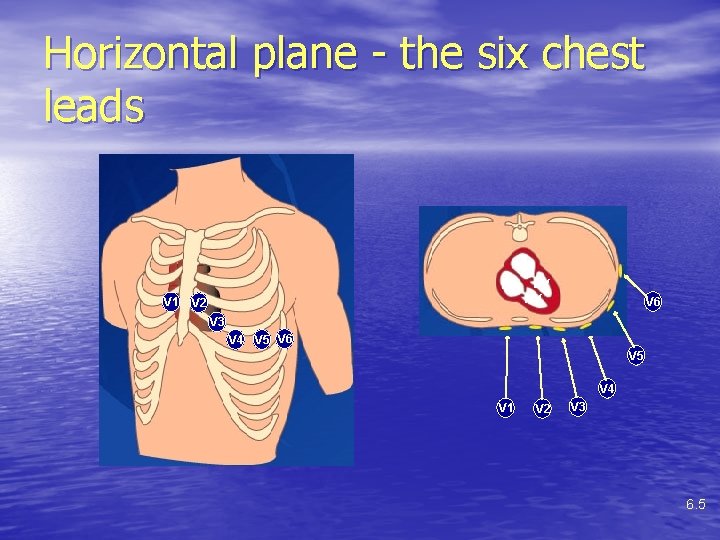
Horizontal plane - the six chest leads LA RA V 1 V 2 LV RV V 6 V 3 V 4 V 5 V 6 V 5 V 4 V 1 V 2 V 3 6. 5

Extending the horizontal plane with V 7, V 8, and V 9 V 7 V 8 V 9 6. 6
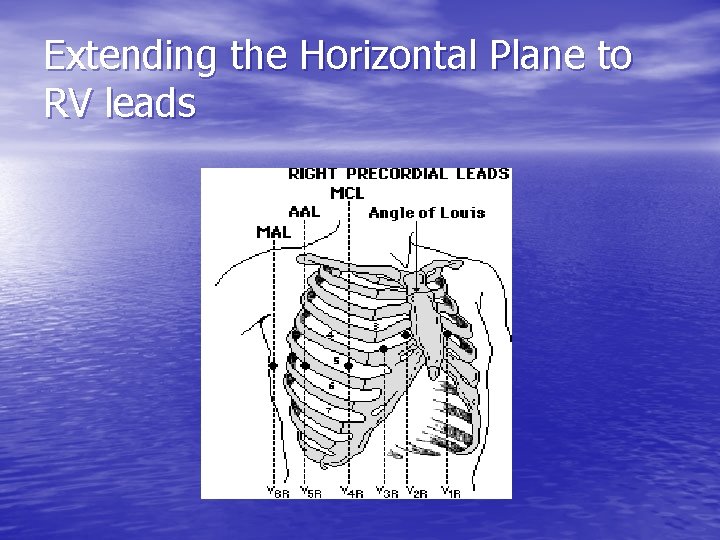
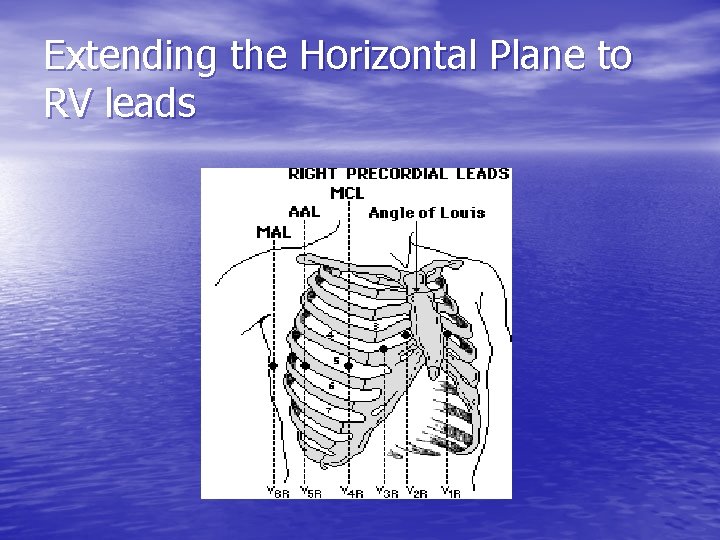
Extending the Horizontal Plane to RV leads
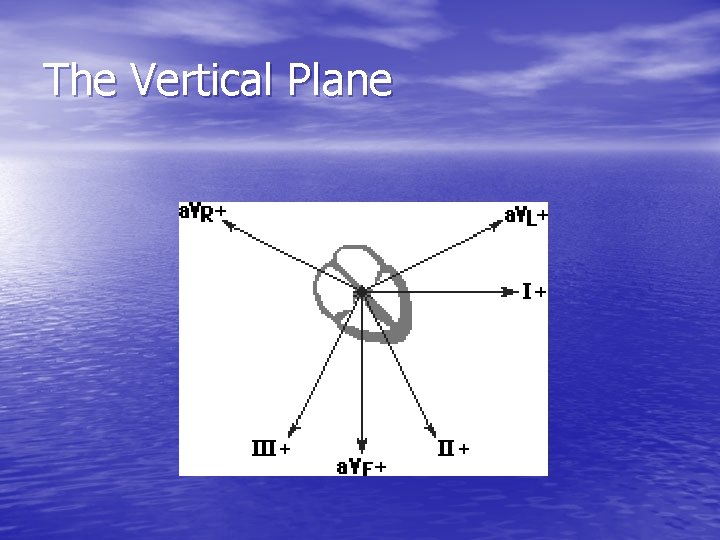
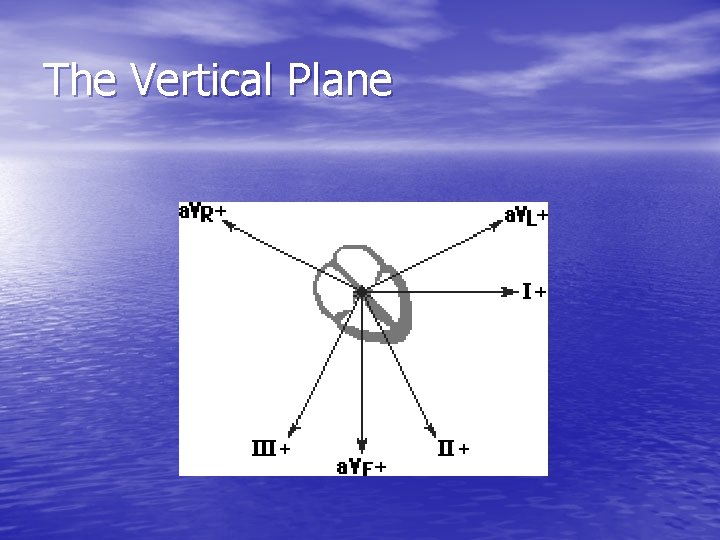
The Vertical Plane
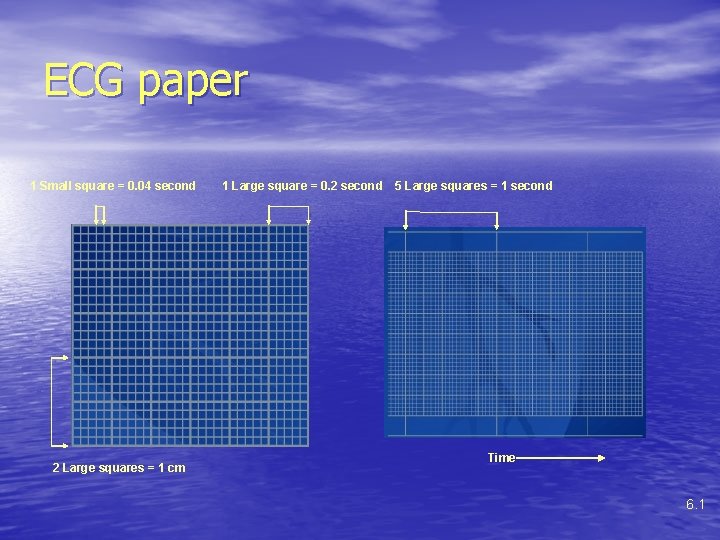
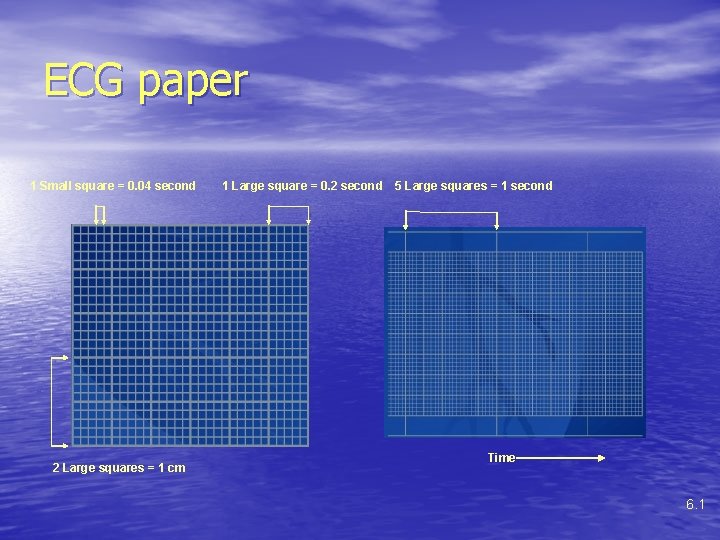
ECG paper 1 Small square = 0. 04 second 2 Large squares = 1 cm 1 Large square = 0. 2 second 5 Large squares = 1 second Time 6. 1
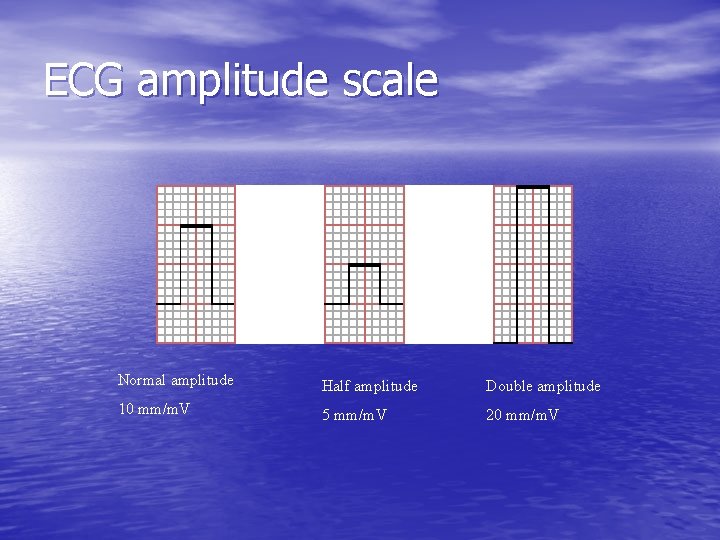
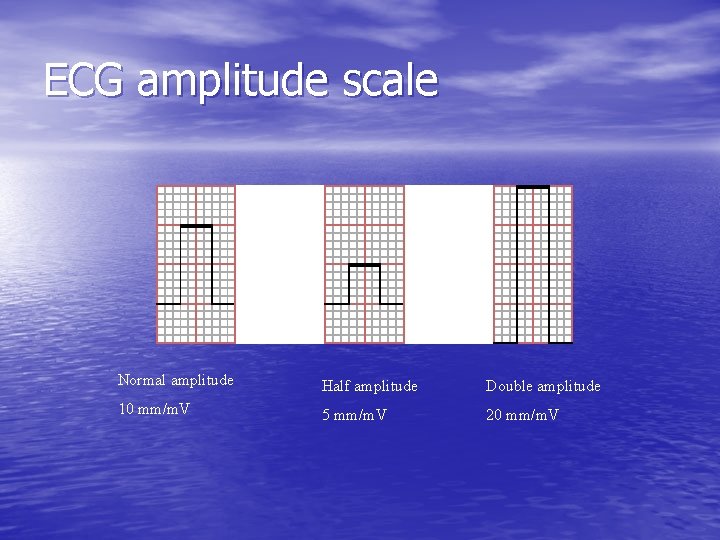
ECG amplitude scale Normal amplitude Half amplitude Double amplitude 10 mm/m. V 5 mm/m. V 20 mm/m. V
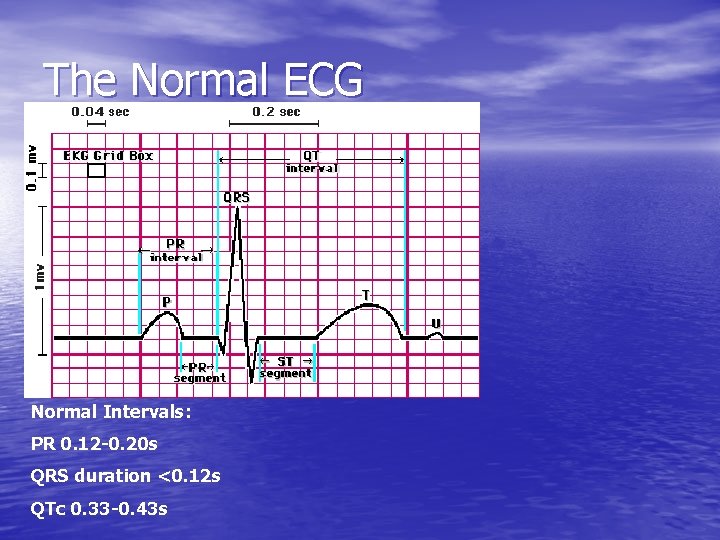
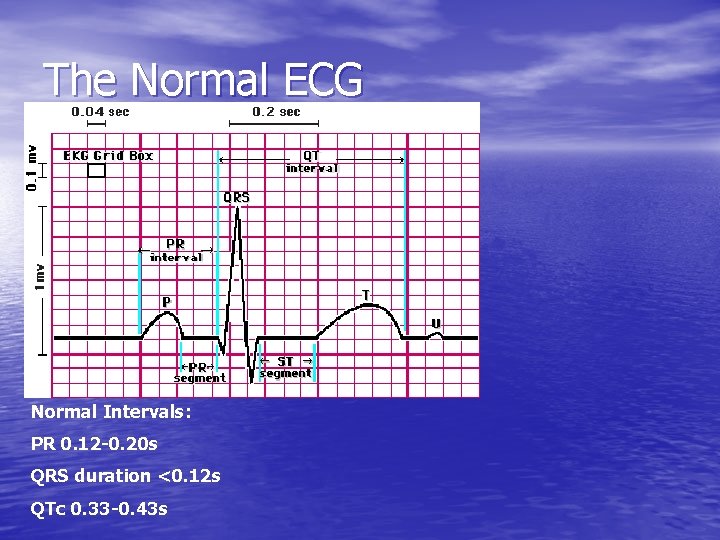
The Normal ECG Normal Intervals: PR 0. 12 -0. 20 s QRS duration <0. 12 s QTc 0. 33 -0. 43 s
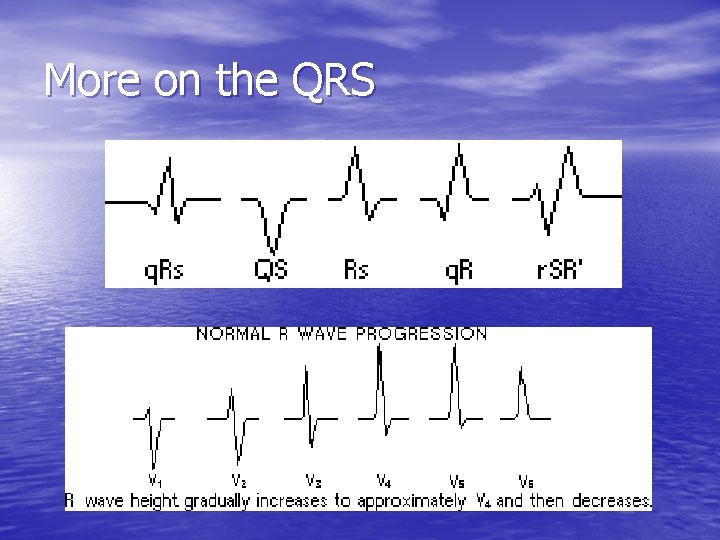
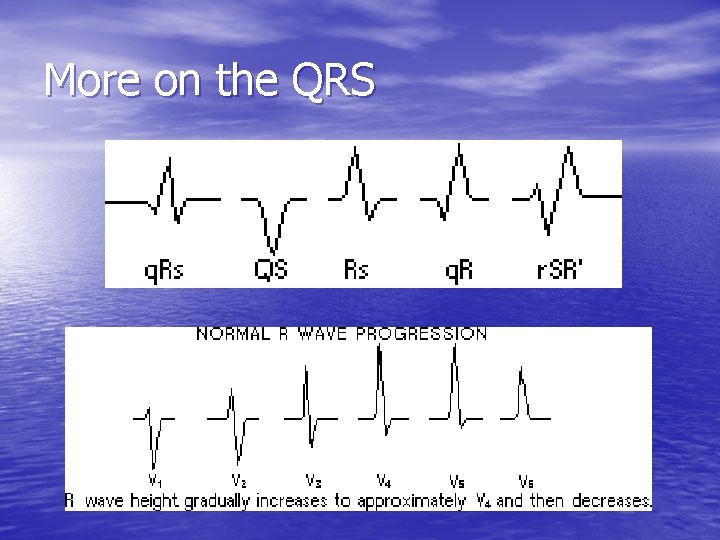
More on the QRS
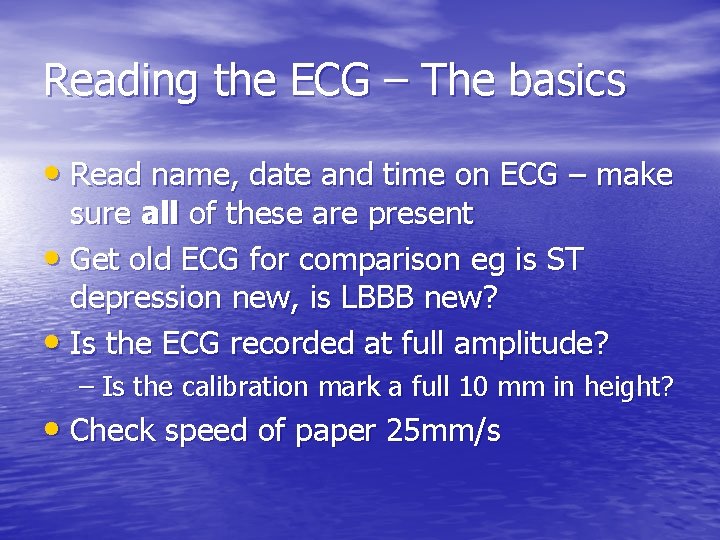
Reading the ECG – The basics • Read name, date and time on ECG – make sure all of these are present • Get old ECG for comparison eg is ST depression new, is LBBB new? • Is the ECG recorded at full amplitude? – Is the calibration mark a full 10 mm in height? • Check speed of paper 25 mm/s
Reading the ECG - The 3 Rs • Rate – 300/no. of squares between successive R-R intervals – <60 bradycardia, >100 tachycardia • Rhythm – sinus or not • Regular or not
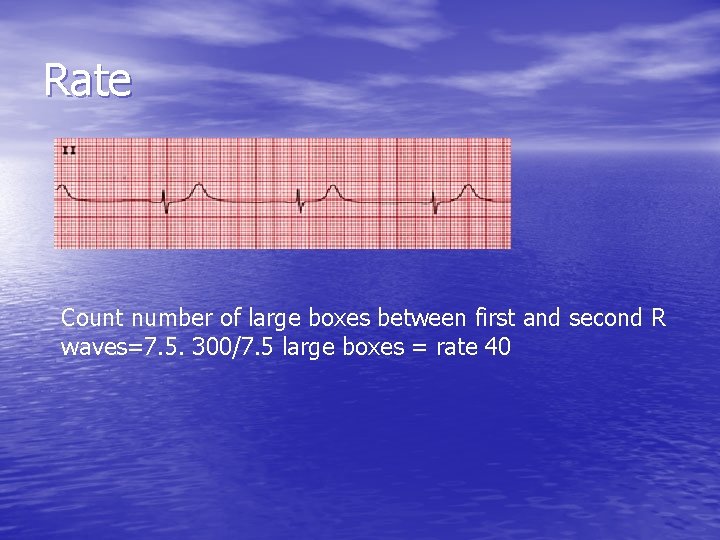
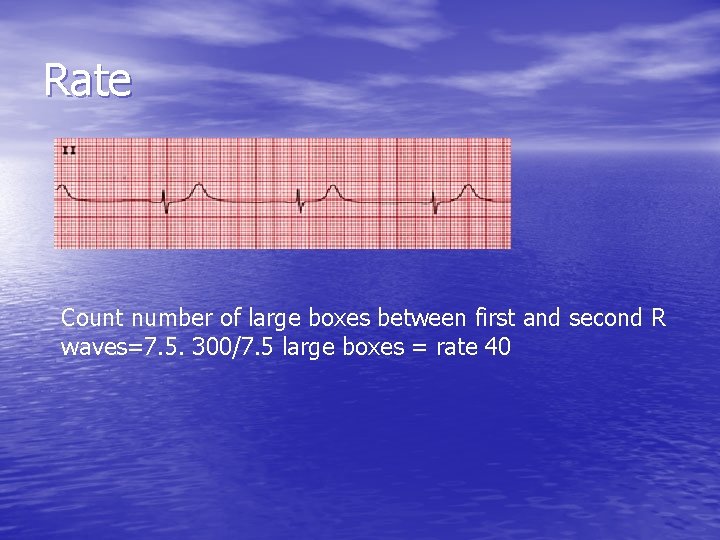
Rate Count number of large boxes between first and second R waves=7. 5. 300/7. 5 large boxes = rate 40
Rhythm • To diagnose sinus (normal) rhythm – One P wave must be present before every QRS – The PR interval must be normal and constant – The P wave morphology remains constant • If sinus rhythm is not present then the actual rhythm must be determined
Systematic Approach to Reading ECG • Cardiac axis • P wave • PR interval • QRS complex • ST segment • T wave • QTc

The electrical axis Normal Limits of QRS Axis in Adults: -30° to +90°.

Determining the Axis • 2 simple methods – 1. Look at leads I and II: QRS vector should be positive in both. If positive in I and negative in II then LAD; if negative in I RAD – 2. Look for isopotential vector in limb leads: ie QRS with equal positive and negative deflections. The axis is 90 deg to this.
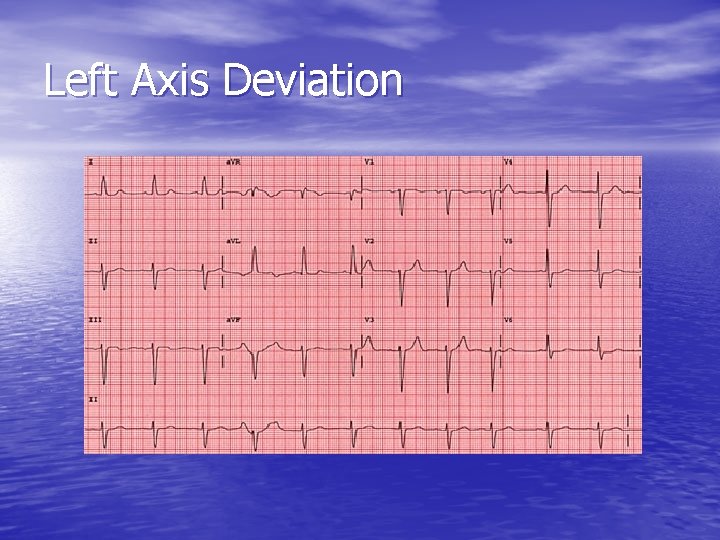
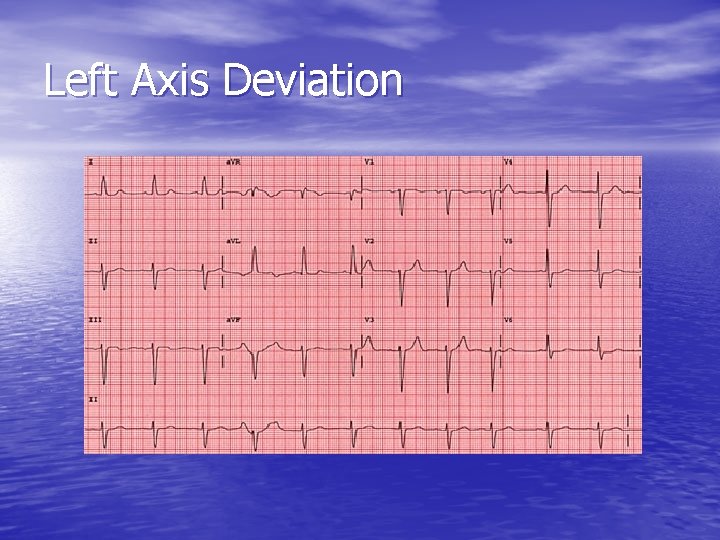
Left Axis Deviation
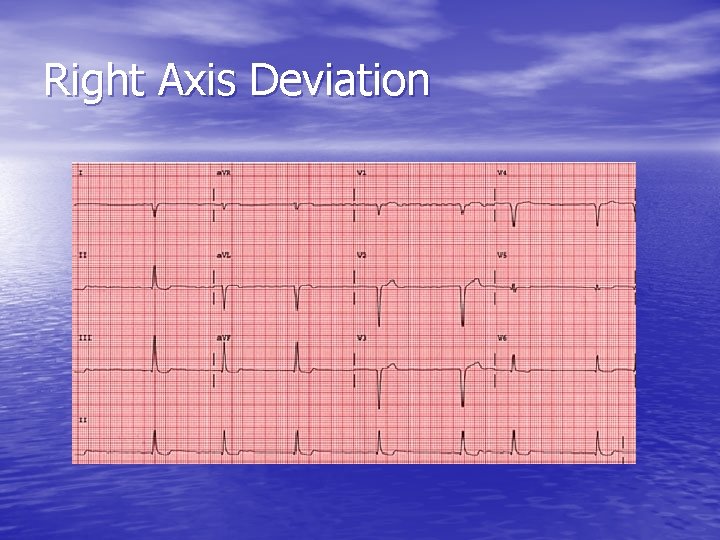
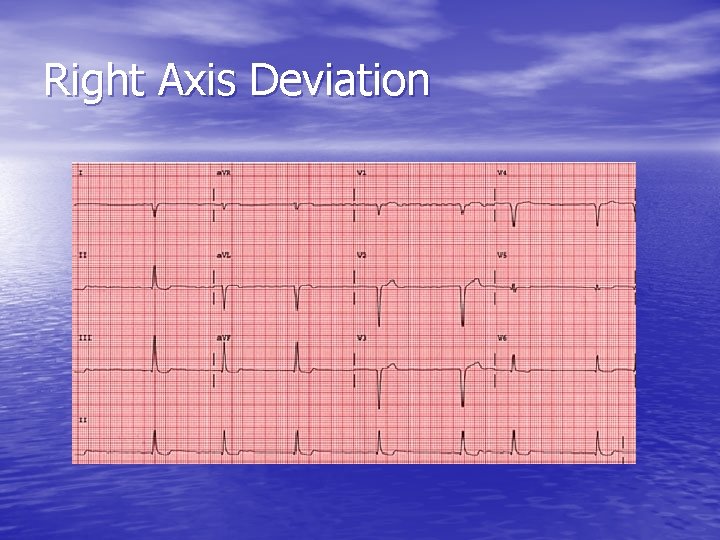
Right Axis Deviation

Causes of Axis Deviation • Right Axis Deviation – – – – Infancy RVH Cor pulmonale Acute RV strain Secundum ASD Fallot, severe PS Left posterior hemiblock • Left Axis Deviation – – – LVH LBBB Left anterior hemiblock Cardiomyopathies Primum ASD Inferior MI
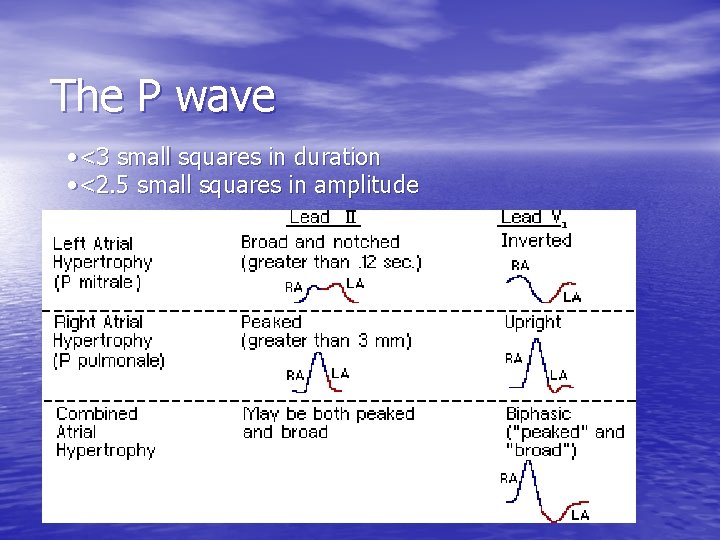
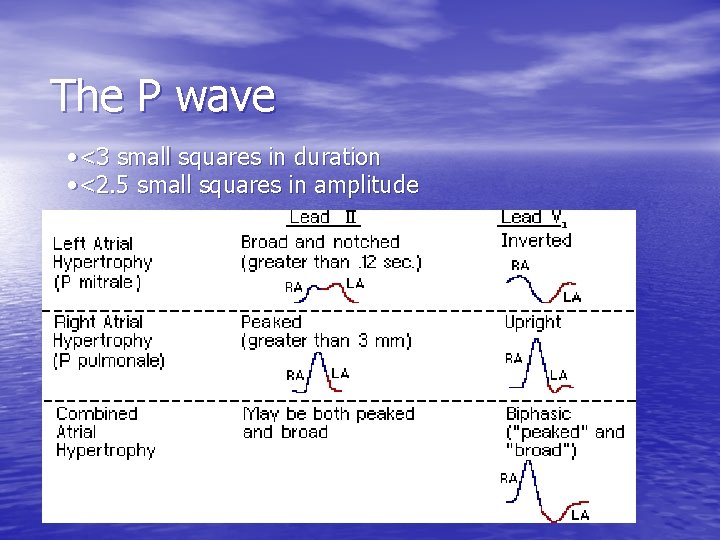
The P wave • <3 small squares in duration • <2. 5 small squares in amplitude
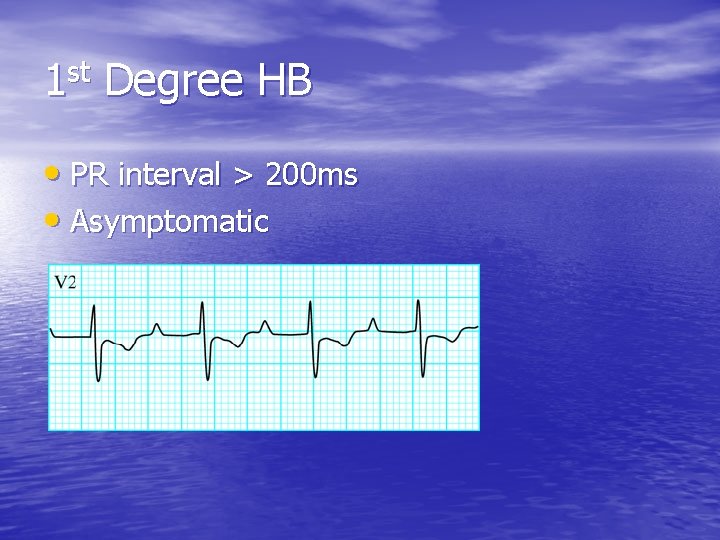
PR interval • Normal is between 3 and 5 little squares • PR > 200 ms = 1 st degree HB • PR < 120 ms may suggest accessory pathway (eg WPW) • PR interval should be constant, if it varies this suggests some form of AV conduction block
AV block • 1 st degree • 2 nd degree – Mobitz type 1 – Mobitz type II • 3 rd degree HB
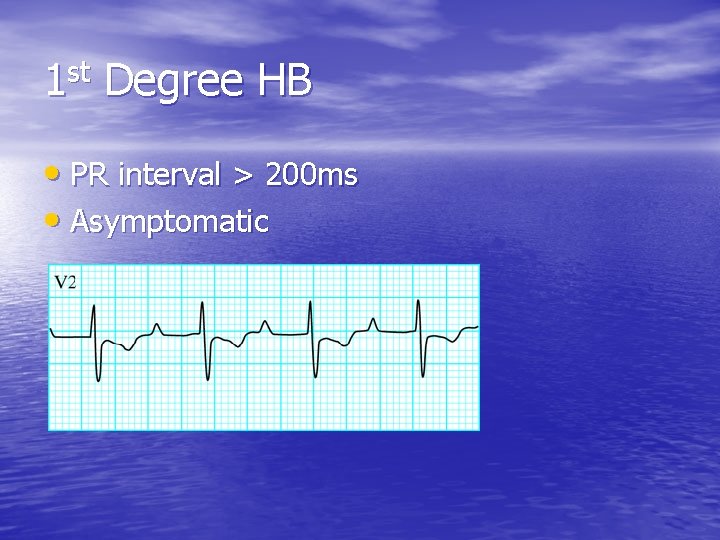
1 st Degree HB • PR interval > 200 ms • Asymptomatic
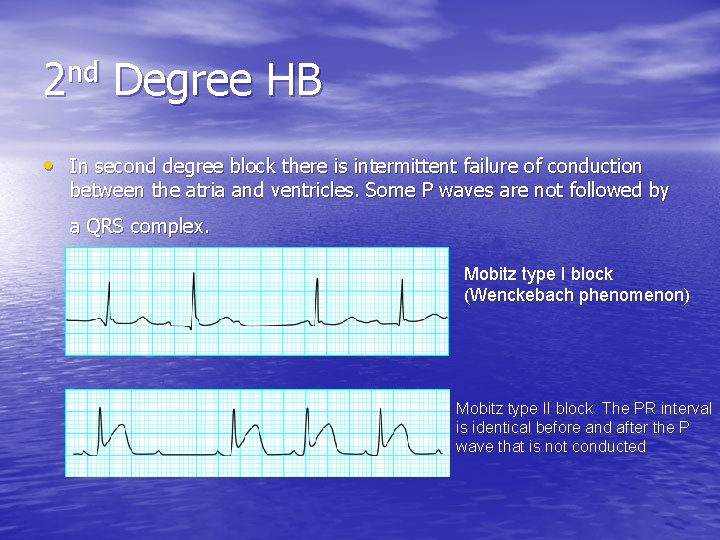
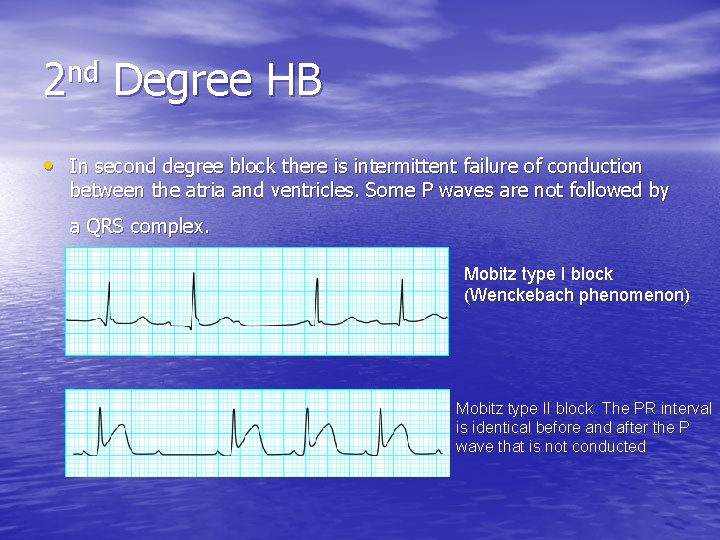
2 nd Degree HB • In second degree block there is intermittent failure of conduction between the atria and ventricles. Some P waves are not followed by a QRS complex. Mobitz type I block (Wenckebach phenomenon) Mobitz type II block The PR interval is identical before and after the P wave that is not conducted

Complete Heart Block • Third degree heart block. A pacemaker in the bundle of His produces a narrow QRS complex (top), whereas more distal pacemakers tend to produce broader complexes (bottom). Arrows show P waves
QRS Complex • Height – LVH/RVH • Width – should be <3 little squares. BBB>120 ms: either RBBB or LBBB (can be indeterminate sometimes)
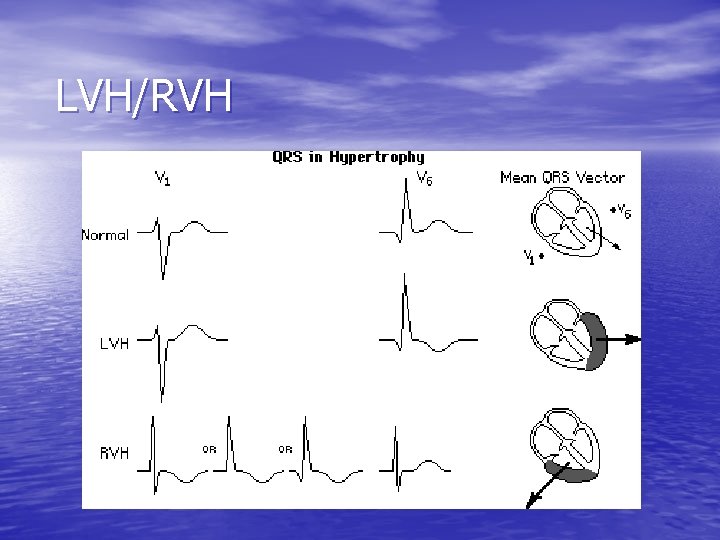
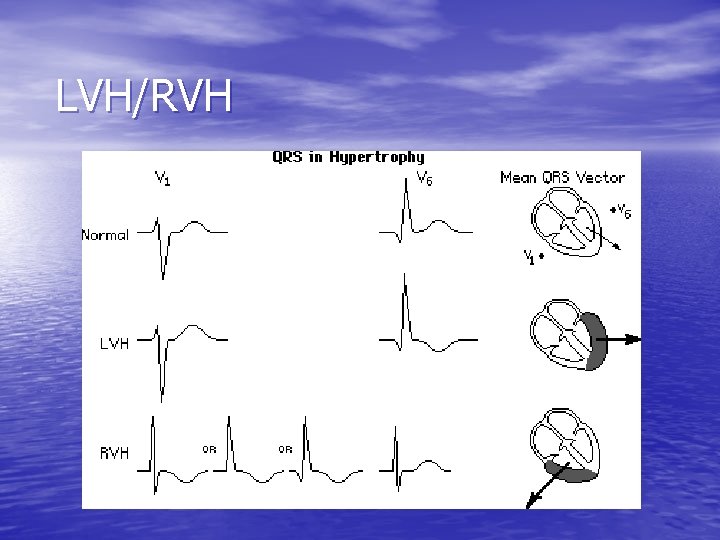
LVH/RVH
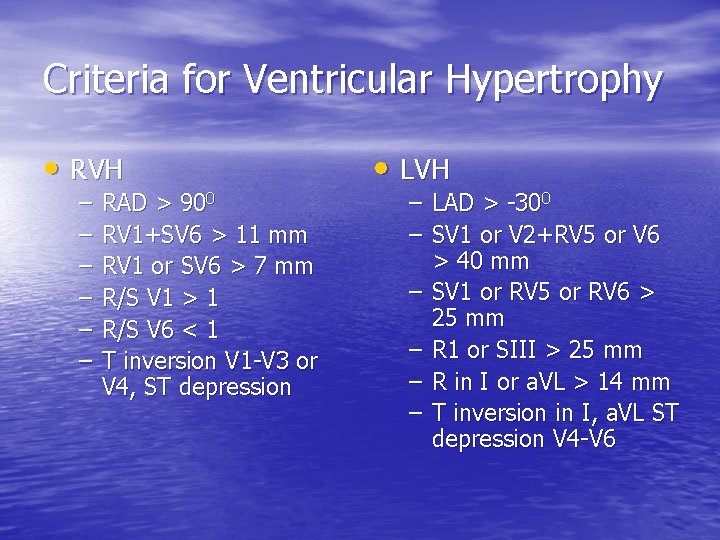
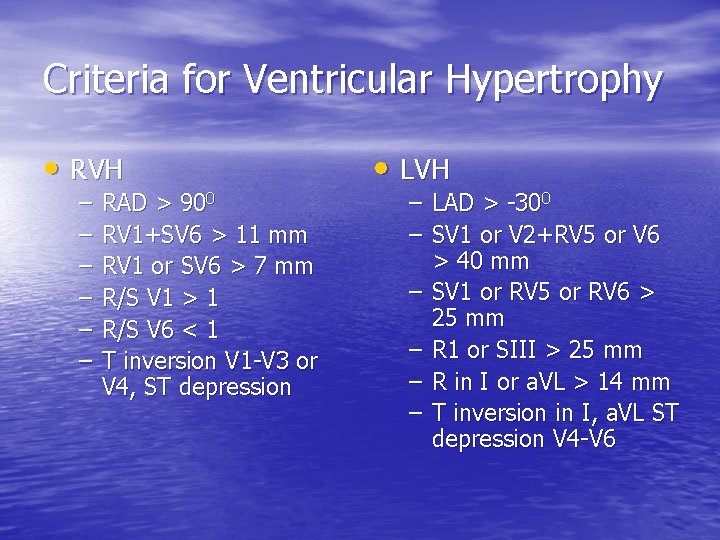
Criteria for Ventricular Hypertrophy • RVH – – – RAD > 900 RV 1+SV 6 > 11 mm RV 1 or SV 6 > 7 mm R/S V 1 > 1 R/S V 6 < 1 T inversion V 1 -V 3 or V 4, ST depression • LVH – LAD > -300 – SV 1 or V 2+RV 5 or V 6 > 40 mm – SV 1 or RV 5 or RV 6 > 25 mm – R 1 or SIII > 25 mm – R in I or a. VL > 14 mm – T inversion in I, a. VL ST depression V 4 -V 6
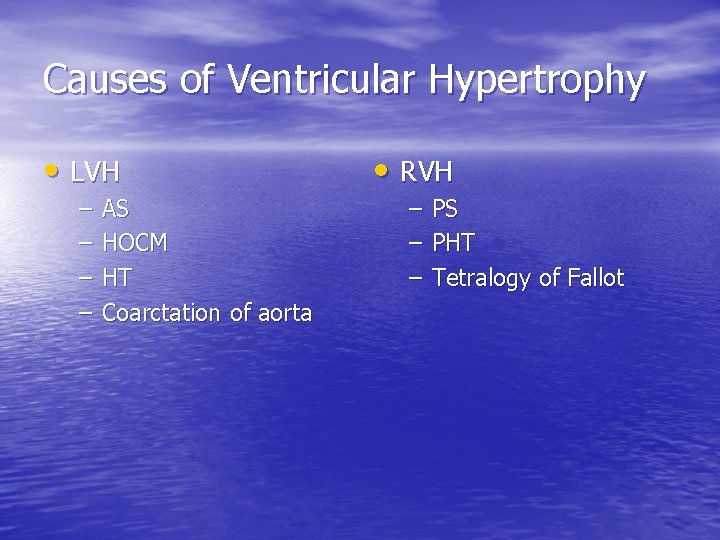
Causes of Ventricular Hypertrophy • LVH • RVH – – – – AS HOCM HT Coarctation of aorta PS PHT Tetralogy of Fallot
Dominant R in V 1 • Other causes of tall R in V 1 – RBBB – WPW (type A) – Posterior MI – Muscular dystrophy – Any cause of RVH
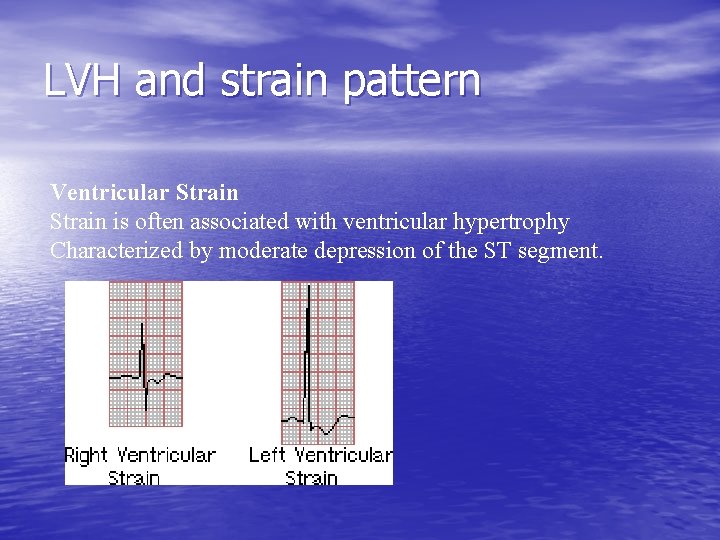
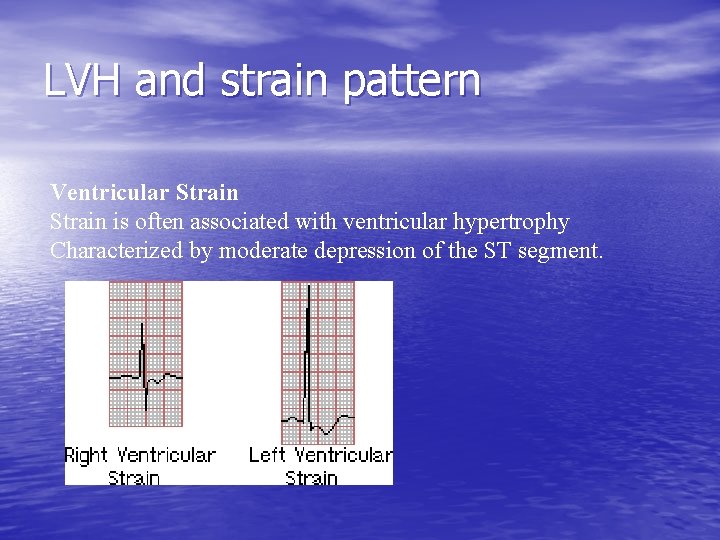
LVH and strain pattern Ventricular Strain is often associated with ventricular hypertrophy Characterized by moderate depression of the ST segment.
Small voltage QRS • Defined as < 5 mm peak-to-peak in all limb leads or <10 mm in precordial leads. • Chronic causes — pulmonary disease, hypothyroidism, obesity, cardiomyopathy. • Acute causes — pleural and/or pericardial effusions
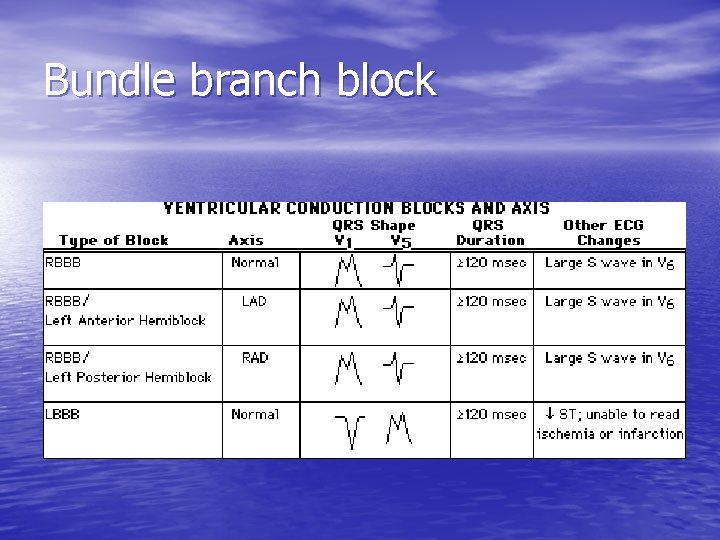
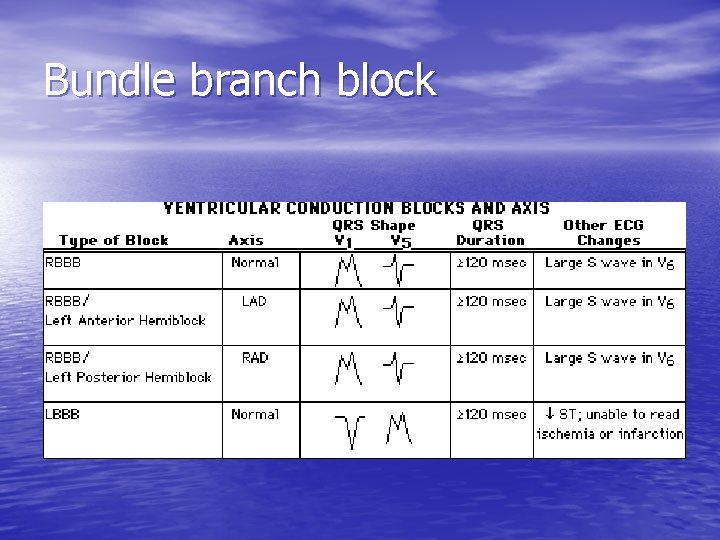
Bundle branch block

RBBB
Causes of RBBB • Can be normal • ASD (and other congenital heart disease) • PE • Cor pulmonale
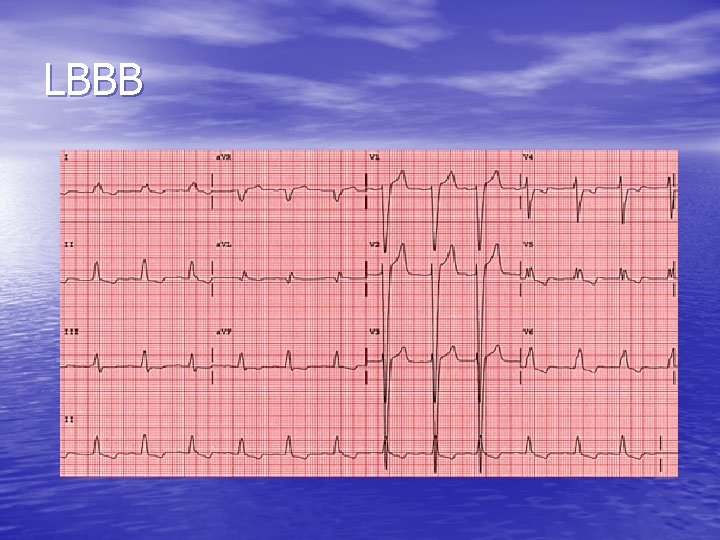
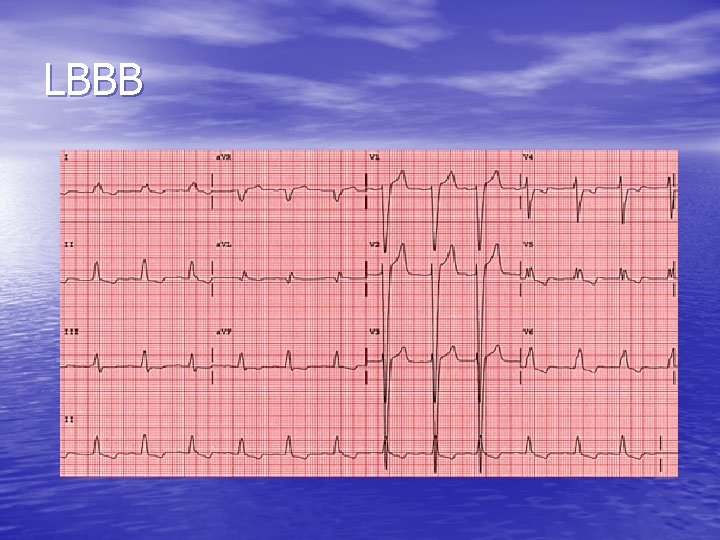
LBBB
Causes of LBBB • IHD • HT • Cardiomyopathy • Idiopathic fibrosis

The Q wave • A Q wave is a negative deflection preceding the R wave • Normal (ie less than 1/4 of R wave height) • • • allowed in I, a. VL, V 5 -6. Represents septal depolarisation (L to R). Normal Q < 0. 04 s wide Pathological Q is >1/4 R wave height and signifies old MI ‘Pathological’ Qs allowed in V 1, III and a. VR
ST segment • ST segment should be an isoelectric line • Pathological ST segment manifest as – ST segment depression – or ST segment elevation
Characteristic changes in AMI • • • ST segment elevation over area of damage ST depression in leads opposite infarction Pathological Q waves Reduced R waves Inverted T waves 7. 13

Sequence of changes in evolving AMI R R T R ST ST P P P QS T Q 1 minute after onset Q 1 hour or so after onset A few hours after onset R ST P P T Q A day or so after onset ST T P T Q Later changes Q A few months after AMI 7. 18

Anterior infarction I II III Left coronary artery a. VR a. VL a. VF V 1 V 2 V 3 V 4 V 5 V 6 7. 19
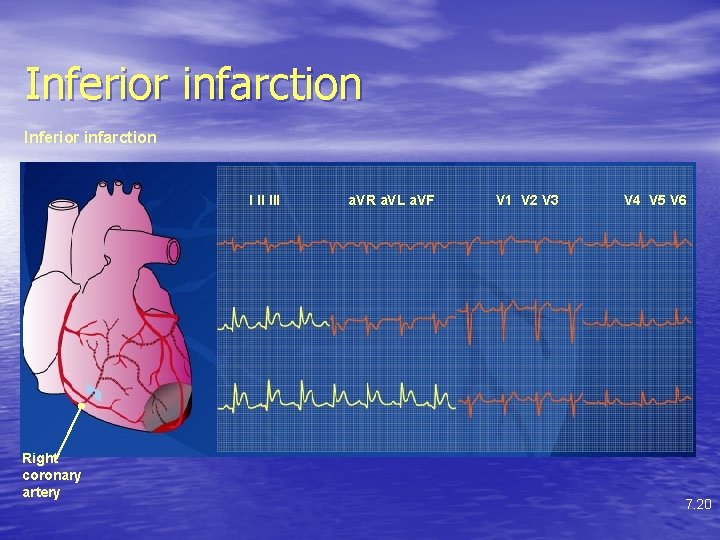
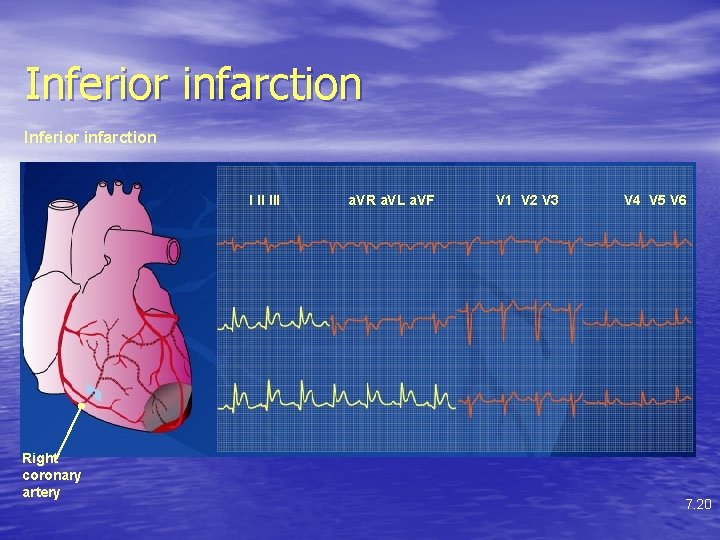
Inferior infarction I II III Right coronary artery a. VR a. VL a. VF V 1 V 2 V 3 V 4 V 5 V 6 7. 20
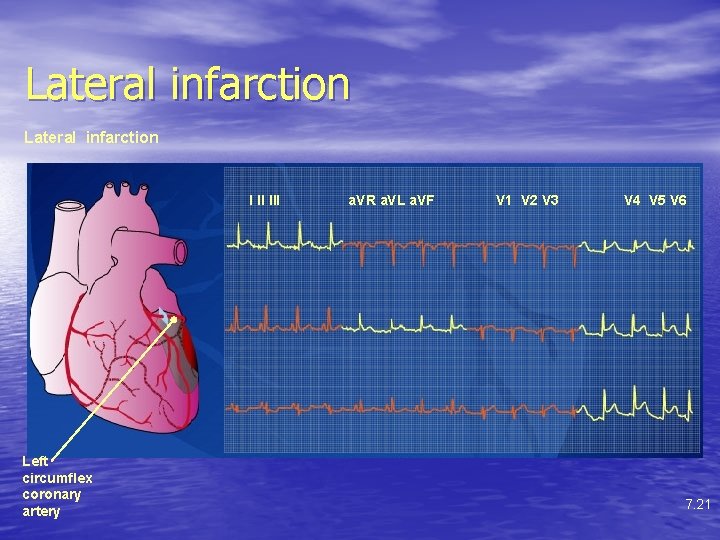
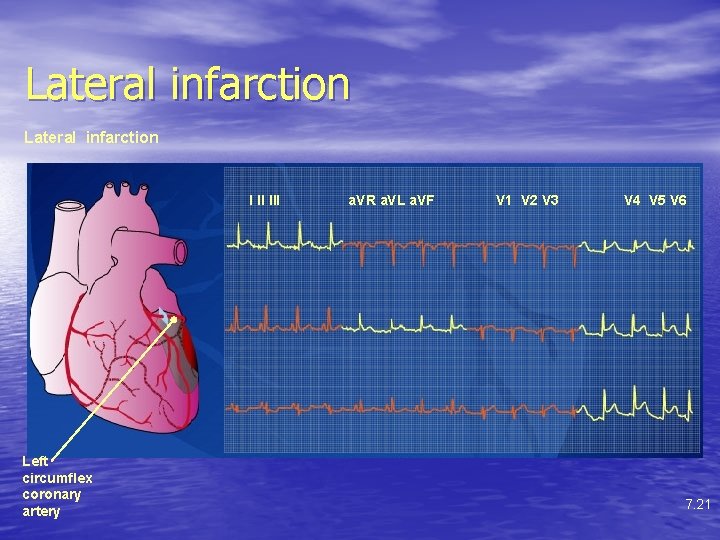
Lateral infarction I II III Left circumflex coronary artery a. VR a. VL a. VF V 1 V 2 V 3 V 4 V 5 V 6 7. 21
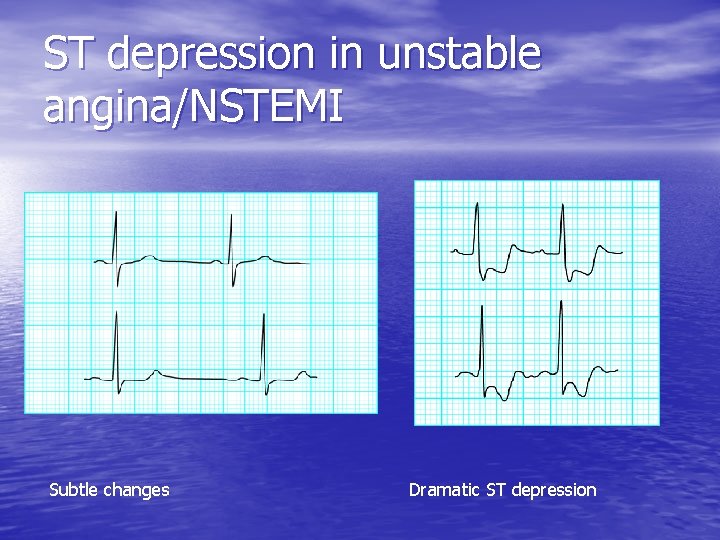
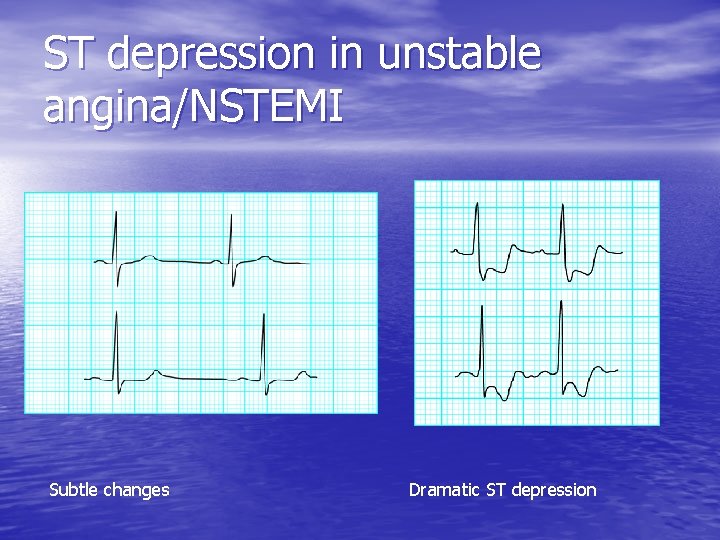
ST depression in unstable angina/NSTEMI Subtle changes Dramatic ST depression
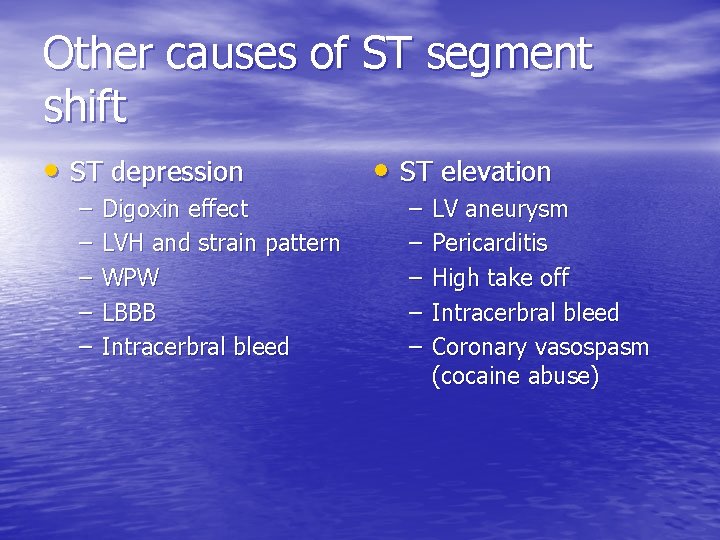
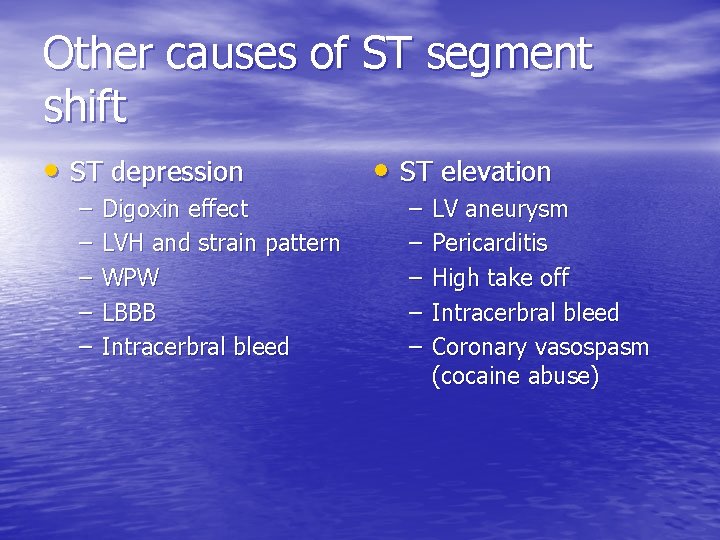
Other causes of ST segment shift • ST depression – – – Digoxin effect LVH and strain pattern WPW LBBB Intracerbral bleed • ST elevation – – – LV aneurysm Pericarditis High take off Intracerbral bleed Coronary vasospasm (cocaine abuse)

Non-ischaemic ST segment changes: in patient taking digoxin (top) and in patient with left ventricular hypertrophy (bottom) Channer, K. et al. BMJ 2002; 324: 1023 -1026 Copyright © 2002 BMJ Publishing Group Ltd.
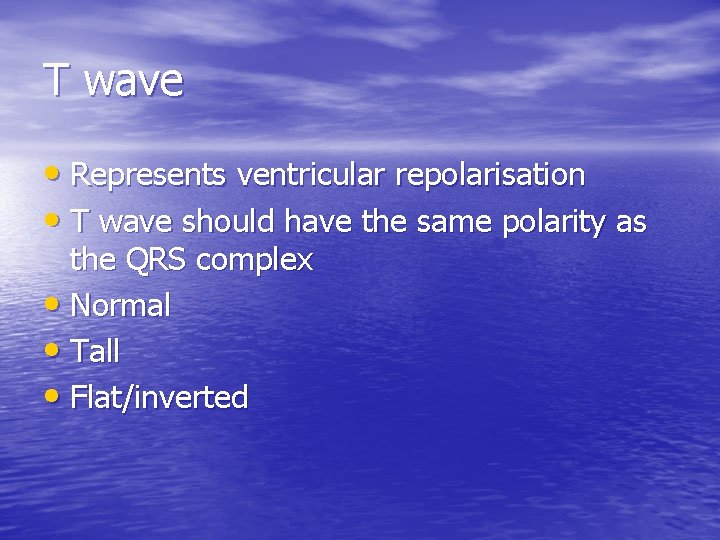
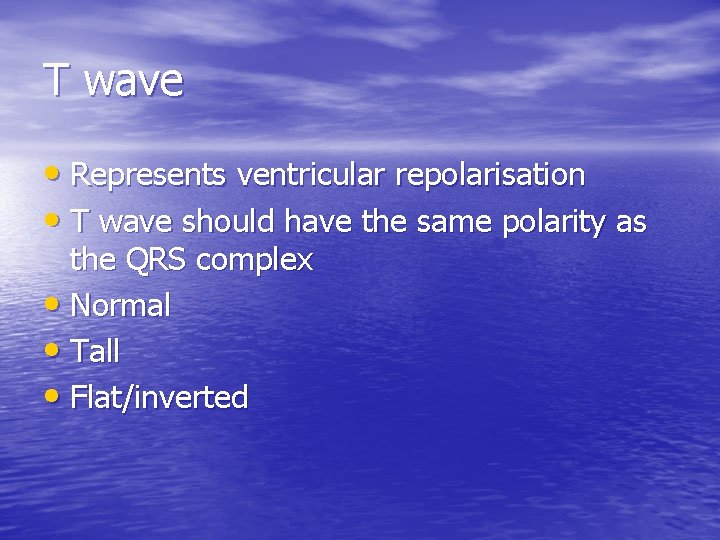
T wave • Represents ventricular repolarisation • T wave should have the same polarity as the QRS complex • Normal • Tall • Flat/inverted

Examples of T wave abnormalities Copyright © 2002 BMJ Publishing Group Ltd. Channer, K. et al. BMJ 2002; 324: 1023 -1026
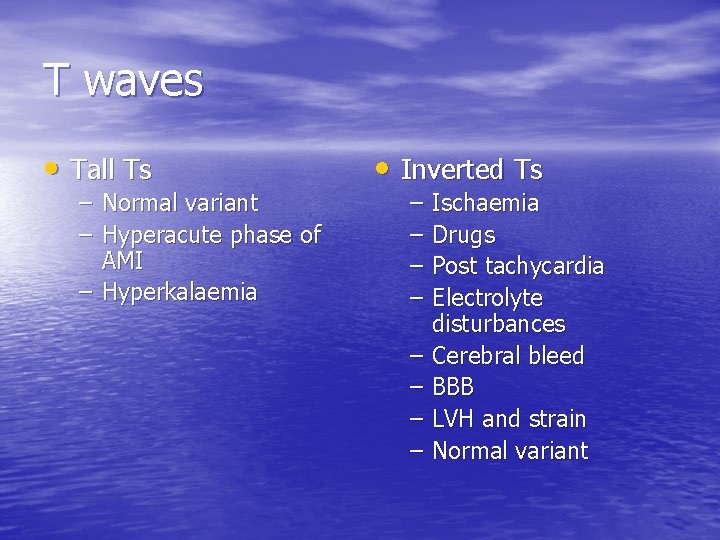
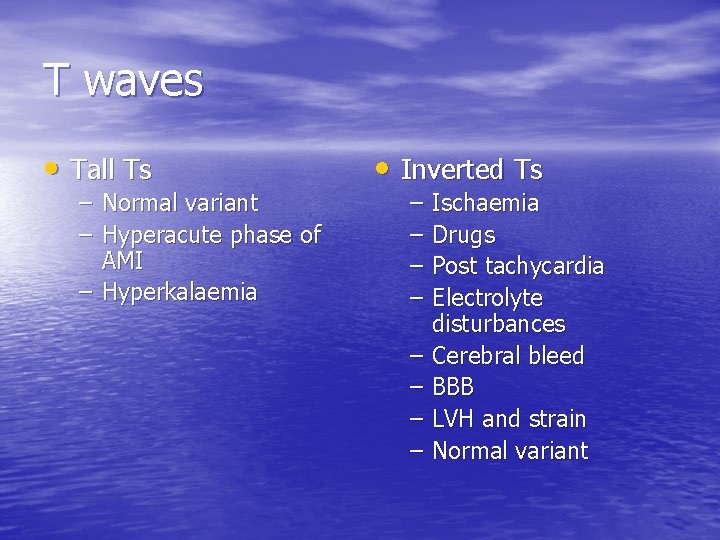
T waves • Tall Ts – Normal variant – Hyperacute phase of AMI – Hyperkalaemia • Inverted Ts – – – – Ischaemia Drugs Post tachycardia Electrolyte disturbances Cerebral bleed BBB LVH and strain Normal variant

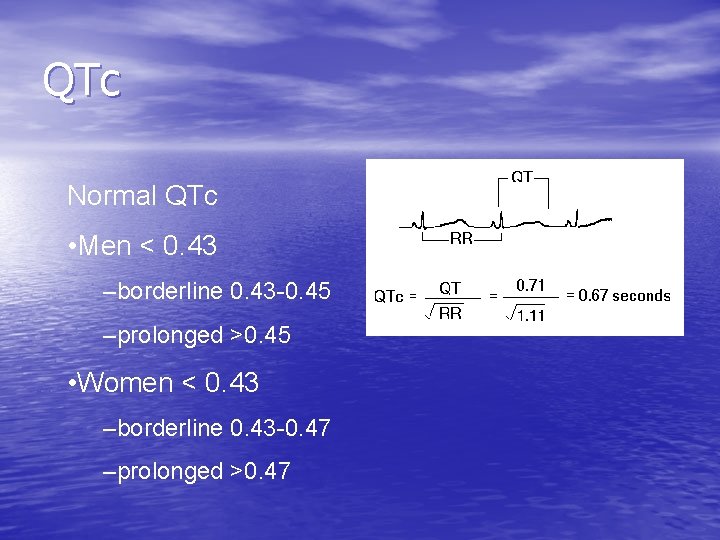
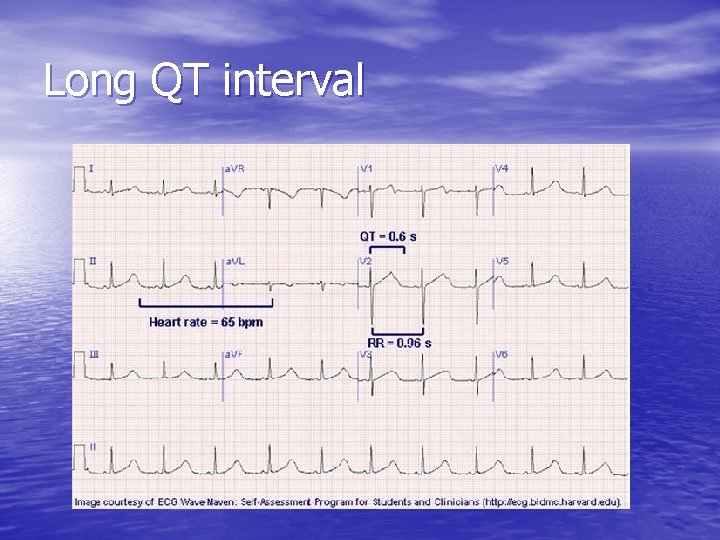
QTc interval • The QT interval represents the total duration of • • • ventricular depolarisation and repolarisation. It represents the period of ventricular refractoriness QT interval increases normally with slower heart rates. QTc is the interval corrected for heart rate, calculated by the Bazell Formula It should be less than ½ of preceding R-R interval as a rule of thumb
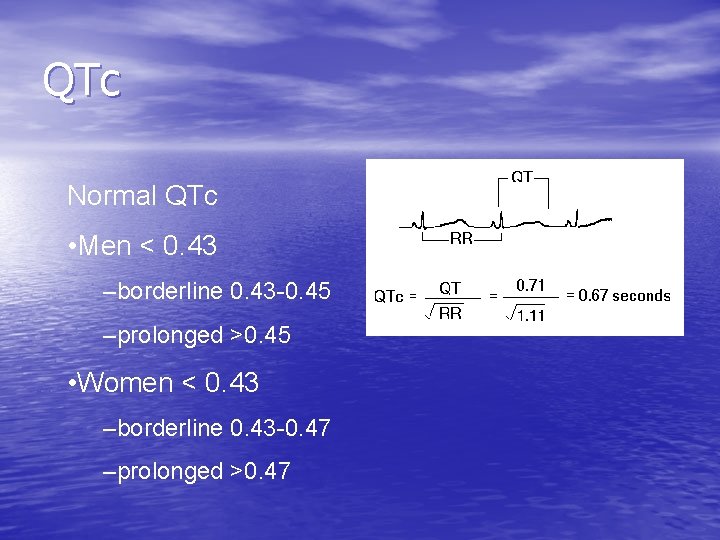
QTc Normal QTc • Men < 0. 43 –borderline 0. 43 -0. 45 –prolonged >0. 45 • Women < 0. 43 –borderline 0. 43 -0. 47 –prolonged >0. 47
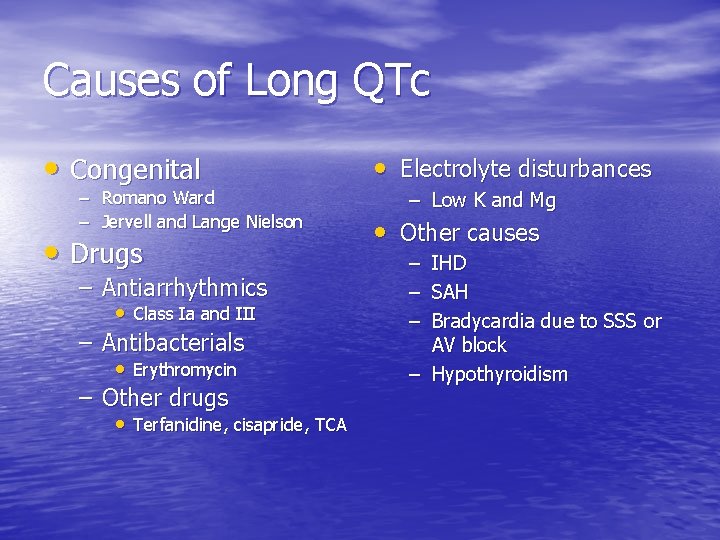
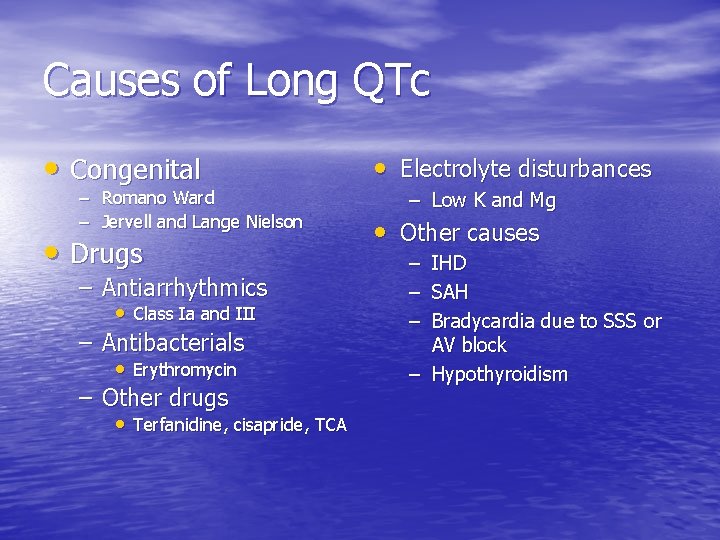
Causes of Long QTc • Congenital – Romano Ward – Jervell and Lange Nielson • Drugs – Antiarrhythmics • Class Ia and III – Antibacterials • Erythromycin – Other drugs • Terfanidine, cisapride, TCA • Electrolyte disturbances – Low K and Mg • Other causes – – – IHD SAH Bradycardia due to SSS or AV block – Hypothyroidism
Sick sinus syndrome • Disease of the sino-atrial node, usually due to • • • age related fibrosis Risk of cardioembolic phenomena Can cause syncope/presyncope ECG shows – – – Sinus bradycardia Sinoatrial block Sinus arrest Infranodal escape rhythms PAF/flutter
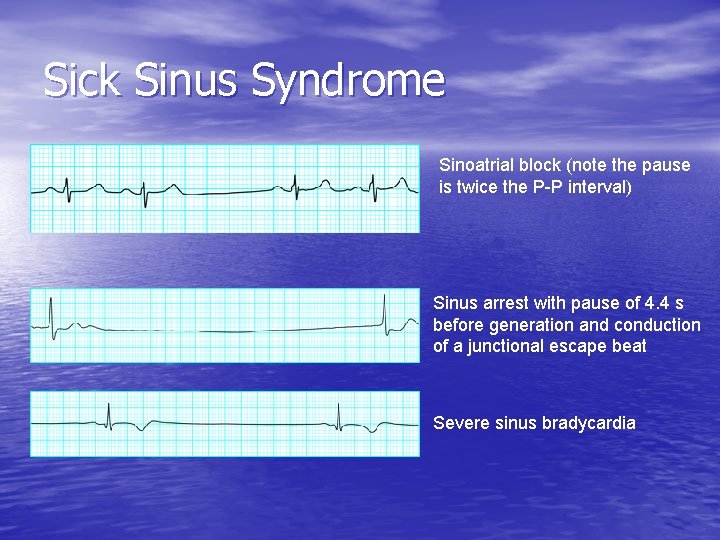
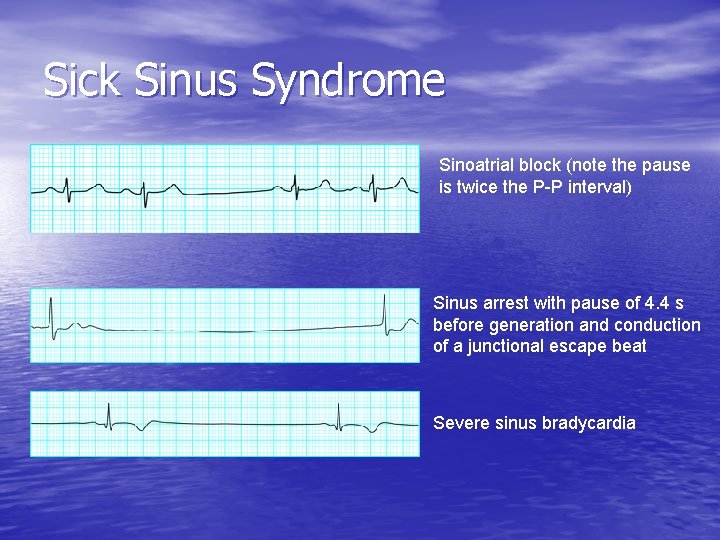
Sick Sinus Syndrome Sinoatrial block (note the pause is twice the P-P interval) Sinus arrest with pause of 4. 4 s before generation and conduction of a junctional escape beat Severe sinus bradycardia
What you should know… • All patterns of myocardial infarction – Including true posterior infarction – Distinguish this from acute pericarditis • Recognise ST depression/ T wave inversion and • • know their causes AF, VT/VF All forms of AV block The BBBs Digoxin effect

Some clinical vignettes

Patients presenting with chest pain

A 48 year old male smoker with positive FH, HT and 2 week history of exertional chest pain • Cholesterol 7. 2 • BP 170/98 • Commence aspirin 75 mg od, statin, GTN spray, beta blocker • Smoking cessation advice • Family screening Rate: 70 Hypertrophy: None Rhythm: Sinus Infarct: None Intervals: Normal Axis: Normal • Advise about MI warning symptoms and what to do • Refer to RACPC
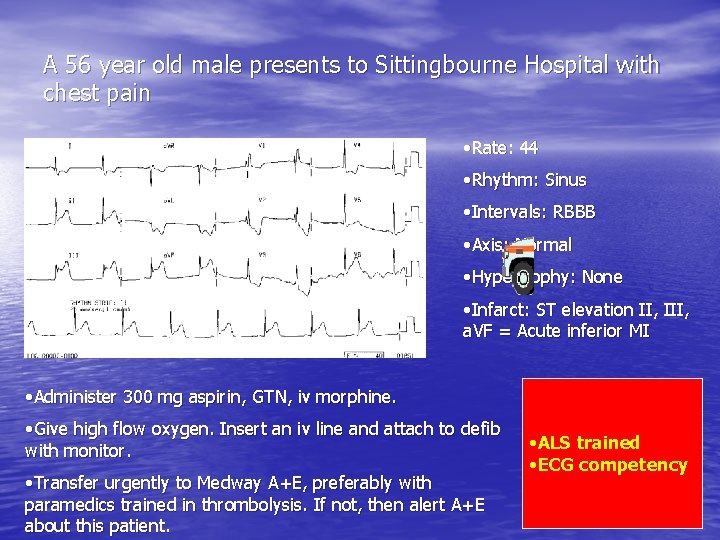
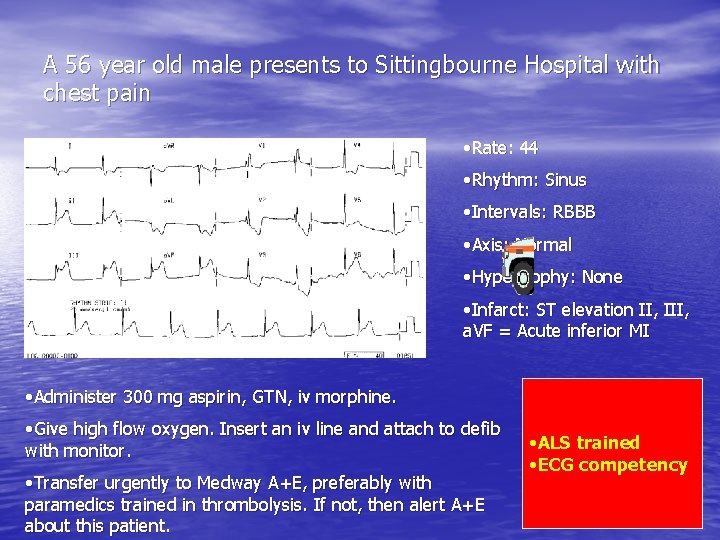
A 56 year old male presents to Sittingbourne Hospital with chest pain • Rate: 44 • Rhythm: Sinus • Intervals: RBBB • Axis: Normal • Hypertrophy: None • Infarct: ST elevation II, III, a. VF = Acute inferior MI • Administer 300 mg aspirin, GTN, iv morphine. • Give high flow oxygen. Insert an iv line and attach to defib with monitor. • Transfer urgently to Medway A+E, preferably with paramedics trained in thrombolysis. If not, then alert A+E about this patient. • ALS trained • ECG competency
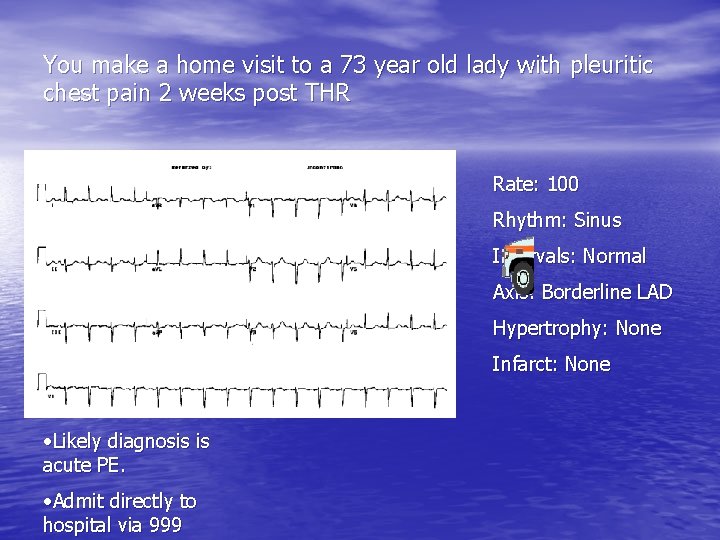
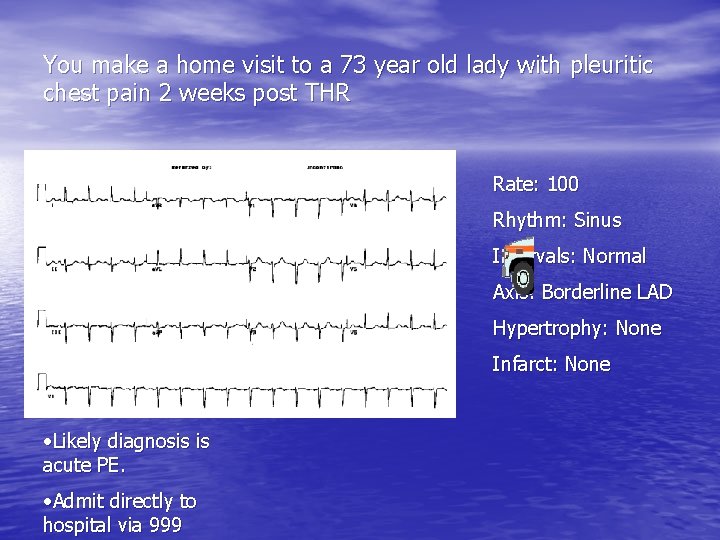
You make a home visit to a 73 year old lady with pleuritic chest pain 2 weeks post THR Rate: 100 Rhythm: Sinus Intervals: Normal Axis: Borderline LAD Hypertrophy: None Infarct: None • Likely diagnosis is acute PE. • Admit directly to hospital via 999
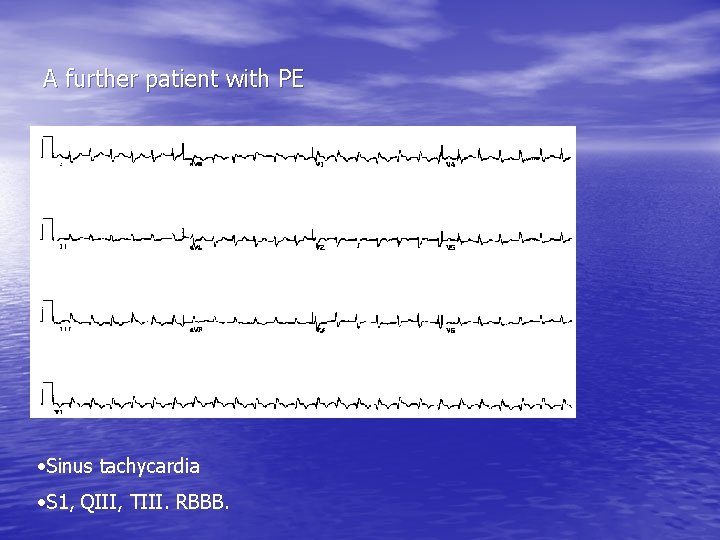
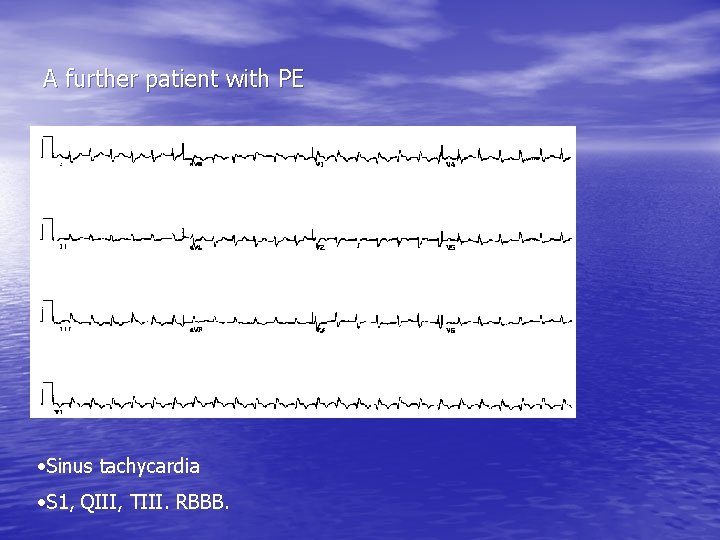
A further patient with PE • Sinus tachycardia • S 1, QIII, TIII. RBBB.
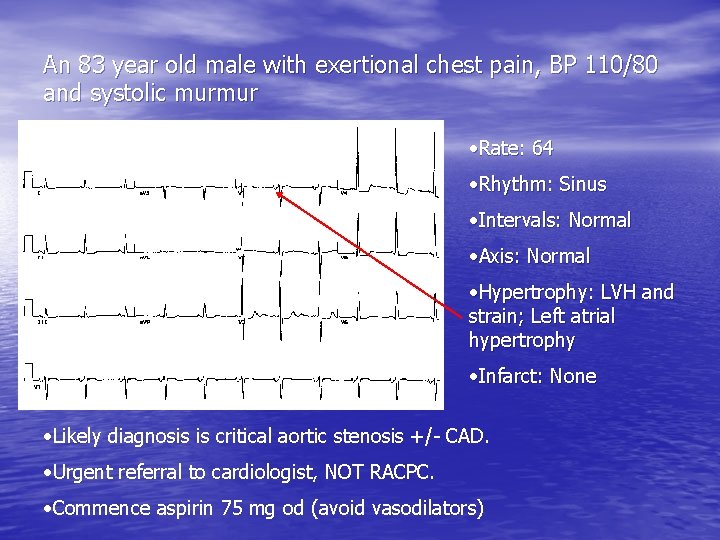
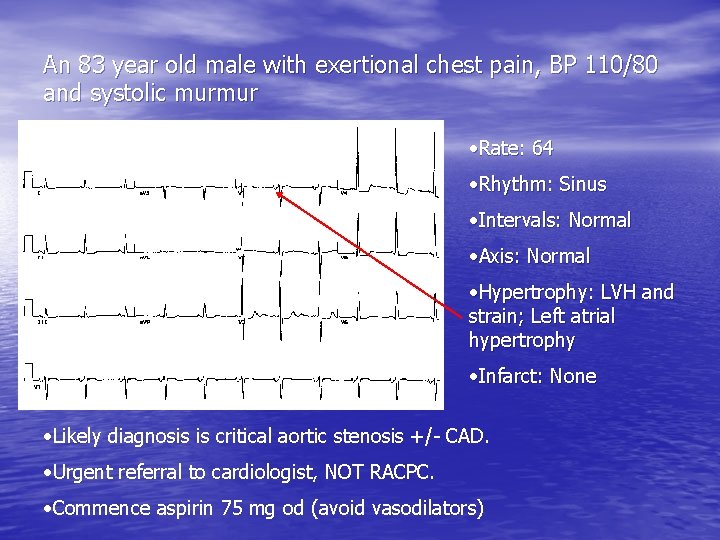
An 83 year old male with exertional chest pain, BP 110/80 and systolic murmur • Rate: 64 • Rhythm: Sinus • Intervals: Normal • Axis: Normal • Hypertrophy: LVH and strain; Left atrial hypertrophy • Infarct: None • Likely diagnosis is critical aortic stenosis +/- CAD. • Urgent referral to cardiologist, NOT RACPC. • Commence aspirin 75 mg od (avoid vasodilators)

A 64 year old female with typical exertional chest pain. Recently started on voltarol for back pain. • This is the ECG during ETT. It shows ST depression I, III, a. VF, V 5 -6. • Hb came back as 4 g/d. L. Her angina was due to severe anaemia. Repeat ETT once her Hb was corrected was normal.

Lessons… • These last 2 cases demonstrate that angina is a • • • syndrome and not a diagnosis It is caused by a mismatch in O 2 demand supply. In patients presenting with angina always check pulse for arrhythmia, look for pallor and listen for murmur of aortic stenosis Always check FBC and U+Es (as well as glucose and cholesterol).

SOB cases
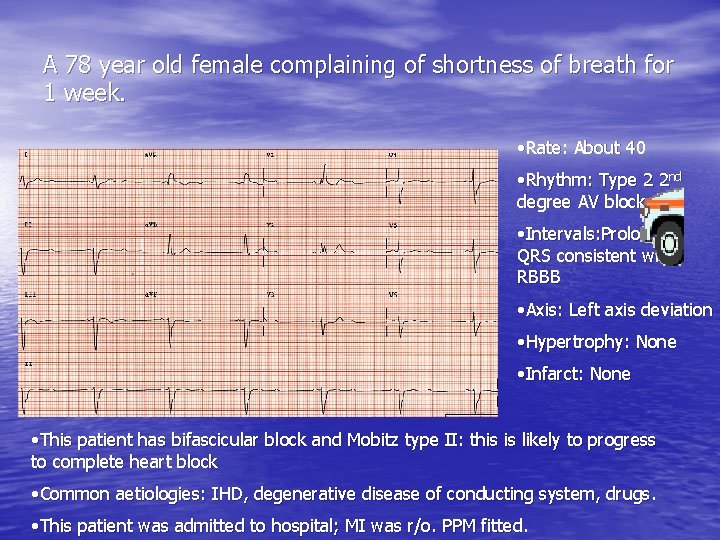
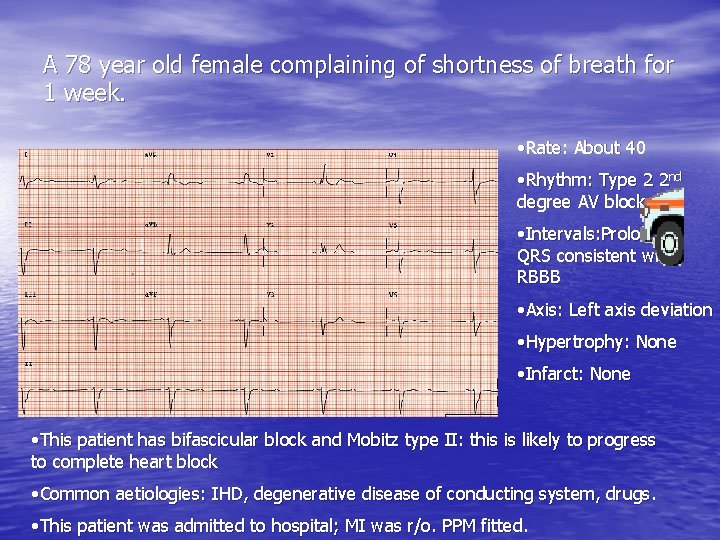
A 78 year old female complaining of shortness of breath for 1 week. • Rate: About 40 • Rhythm: Type 2 2 nd degree AV block • Intervals: Prolonged QRS consistent with RBBB • Axis: Left axis deviation • Hypertrophy: None • Infarct: None • This patient has bifascicular block and Mobitz type II: this is likely to progress to complete heart block • Common aetiologies: IHD, degenerative disease of conducting system, drugs. • This patient was admitted to hospital; MI was r/o. PPM fitted.
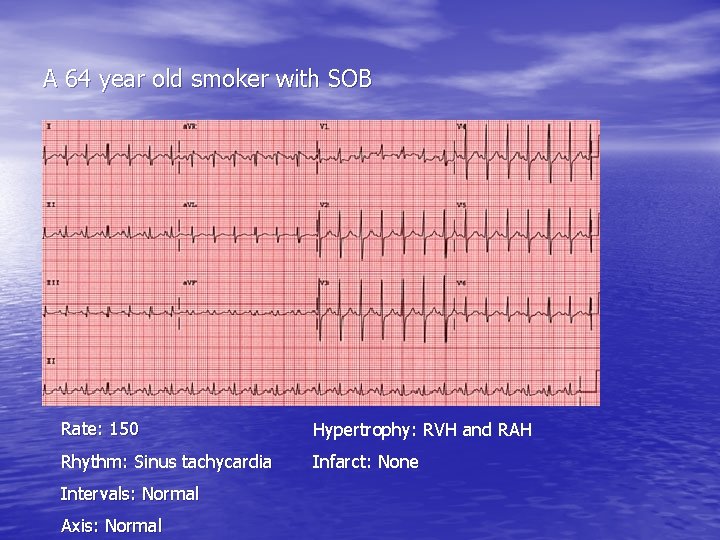
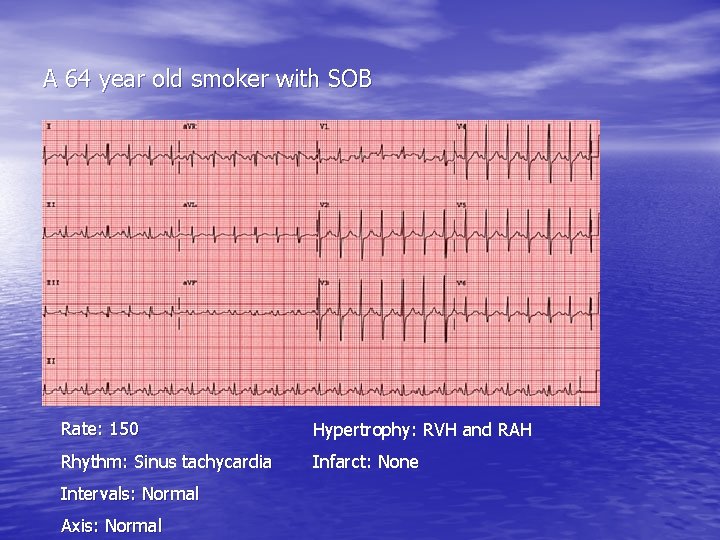
A 64 year old smoker with SOB Rate: 150 Hypertrophy: RVH and RAH Rhythm: Sinus tachycardia Infarct: None Intervals: Normal Axis: Normal
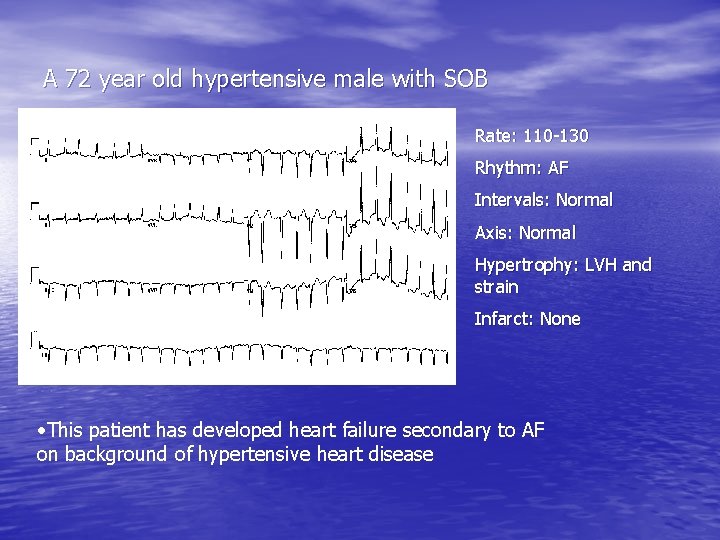
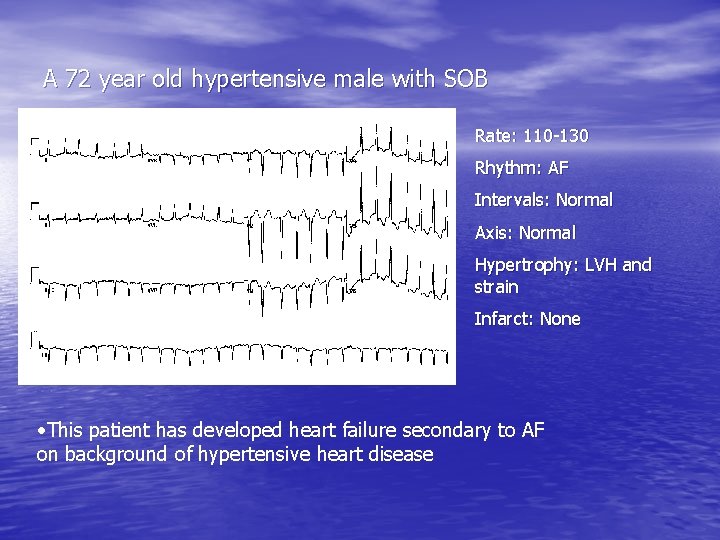
A 72 year old hypertensive male with SOB Rate: 110 -130 Rhythm: AF Intervals: Normal Axis: Normal Hypertrophy: LVH and strain Infarct: None • This patient has developed heart failure secondary to AF on background of hypertensive heart disease
Previous case continued • Commence digoxin and warfarin if no contraindication • Arrange U+E, FBC and TFT • Diuretics if fluid overloaded • Refer urgently to cardiologist or heart failure clinic.

A 63 year old woman with SOB, reduced exercise capacity and PND Rate: 100 -120 Rhythm: AF Intervals: LBBB Axis: N/A Hypertrophy: N/A Infarct: N/A • This patient also has CCF. The LBBB suggests structural heart disease which in this case was secondary to previous MI. • Arrange bloods (including BNP) and refer to heart failure clinic. You could commence ACEI once BNP taken as CCF seems likely

Some palpitation cases
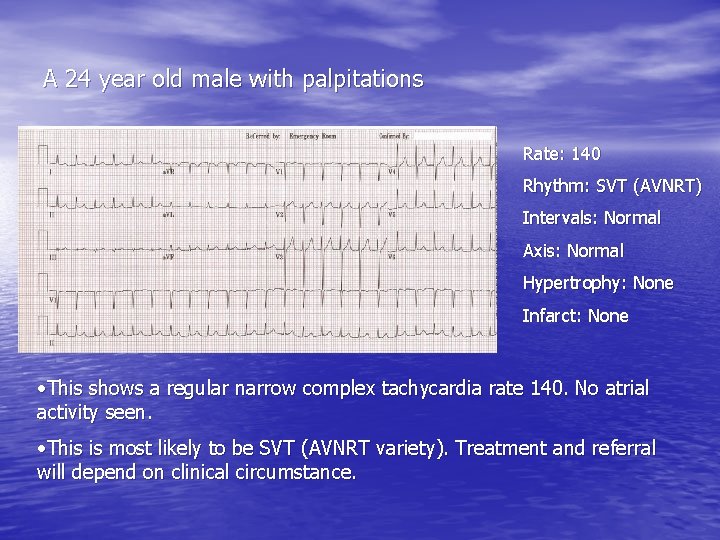
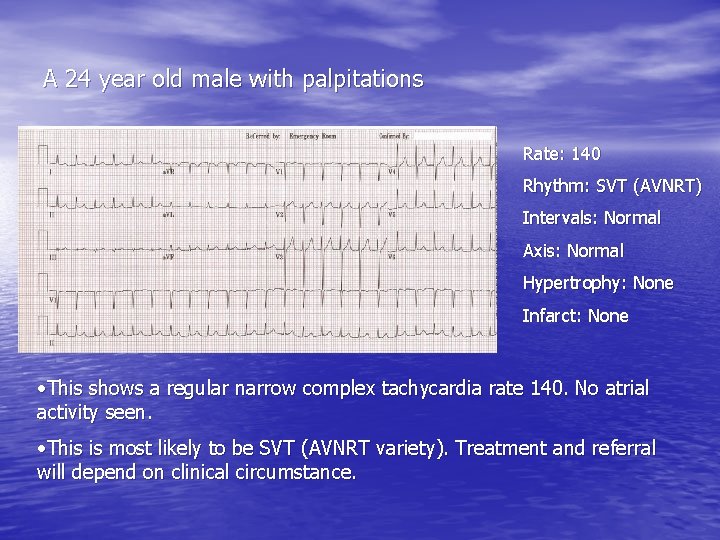
A 24 year old male with palpitations Rate: 140 Rhythm: SVT (AVNRT) Intervals: Normal Axis: Normal Hypertrophy: None Infarct: None • This shows a regular narrow complex tachycardia rate 140. No atrial activity seen. • This is most likely to be SVT (AVNRT variety). Treatment and referral will depend on clinical circumstance.
Previous case continued • First of all try and eliminate potential triggers eg • • alcohol, caffeine, stress, sleep deprivation, chocolate) If symptoms persist treatment may be warranted Verapamil, beta blockers 2 nd line agents : sotalol, flecainide Consider radio frequency ablation for failure of medical treatment (or drug SE).

A 48 year old female with palpitations • Rate: 75 • Rhythm: Sinus with atrial premature beat (PAC) • Intervals: Normal • Axis: Normal • Hypertrophy: None • Infarct: None • Take a full history of the palpitations and carry out CVS examination • If normal then simply reassure the patient
More on tachycardias • 3 important questions: – Broad or narrow complex (ie more or less than 3 little squares) – Regular or irregular – Is the patient compromised or not? • Chest pain • Low GCS • Low BP • SOB/HF

Some syncopal cases
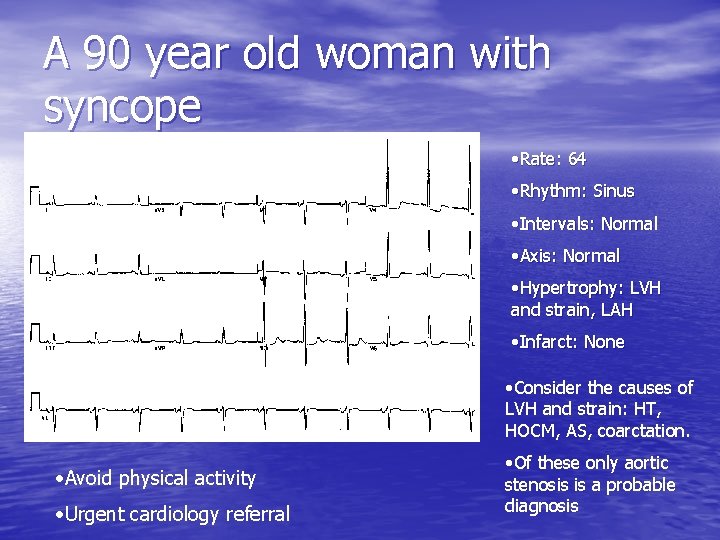
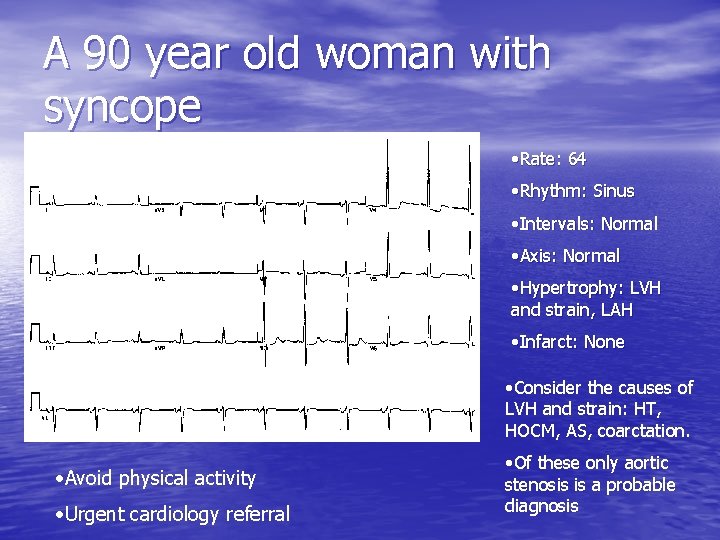
A 90 year old woman with syncope • Rate: 64 • Rhythm: Sinus • Intervals: Normal • Axis: Normal • Hypertrophy: LVH and strain, LAH • Infarct: None • Consider the causes of LVH and strain: HT, HOCM, AS, coarctation. • Avoid physical activity • Urgent cardiology referral • Of these only aortic stenosis is a probable diagnosis
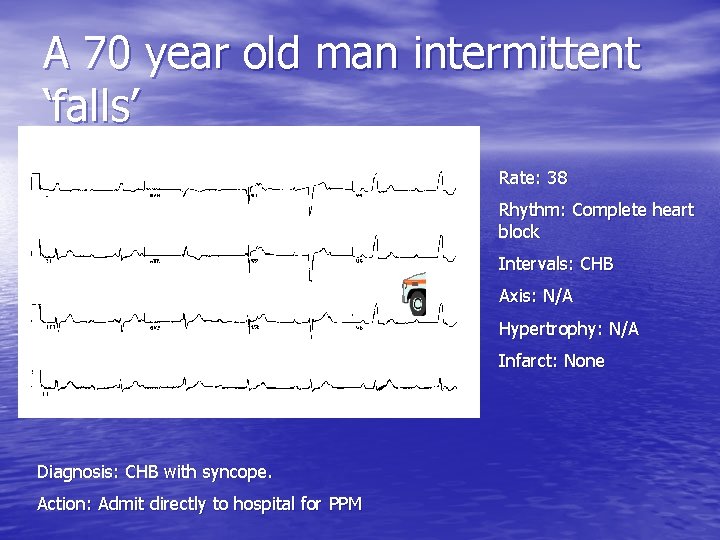
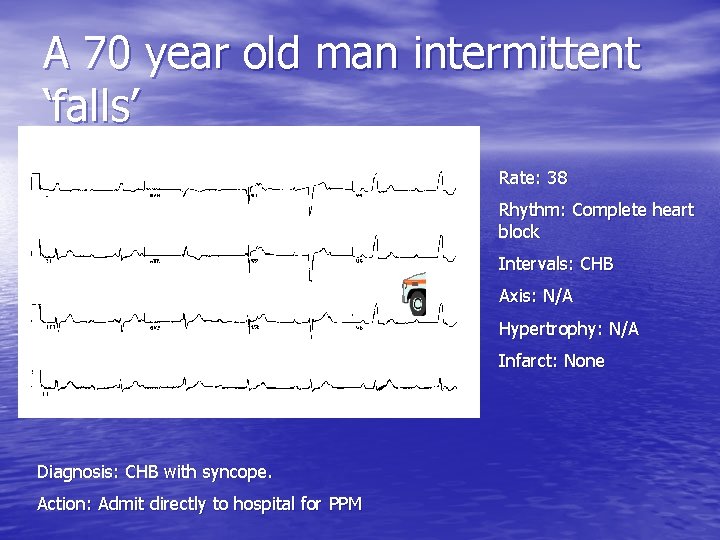
A 70 year old man intermittent ‘falls’ Rate: 38 Rhythm: Complete heart block Intervals: CHB Axis: N/A Hypertrophy: N/A Infarct: None Diagnosis: CHB with syncope. Action: Admit directly to hospital for PPM
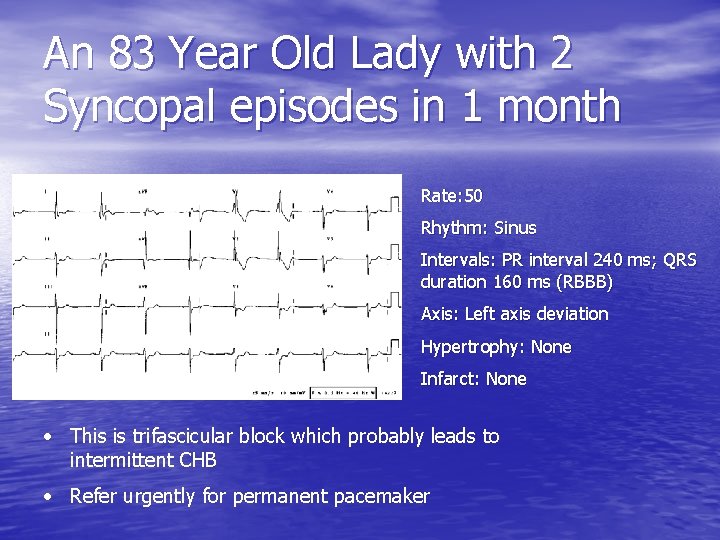
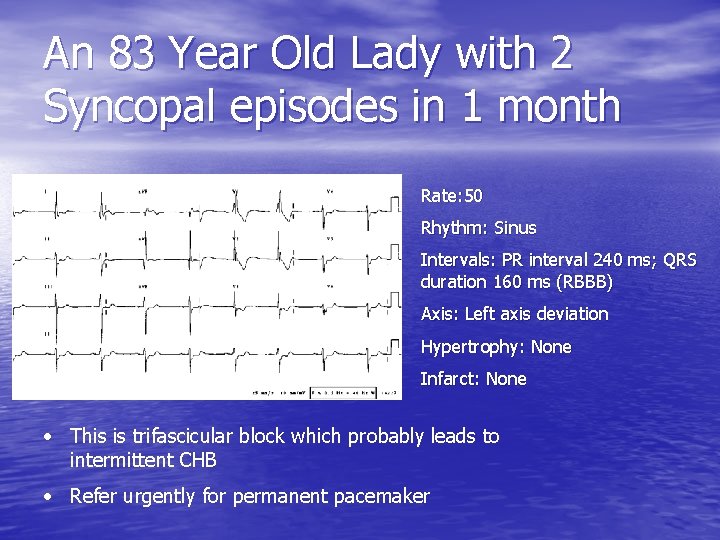
An 83 Year Old Lady with 2 Syncopal episodes in 1 month Rate: 50 Rhythm: Sinus Intervals: PR interval 240 ms; QRS duration 160 ms (RBBB) Axis: Left axis deviation Hypertrophy: None Infarct: None • This is trifascicular block which probably leads to intermittent CHB • Refer urgently for permanent pacemaker

A 56 year old man with CCF and frequent episodes of presyncope • You organise an event recorder: • • Rate: 140 Rhythm: VT High risk for sudden death Arrange urgent admission to CCU
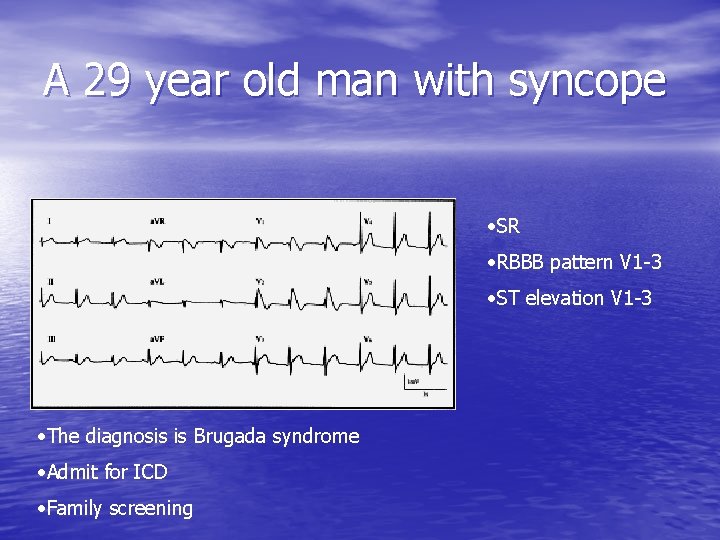
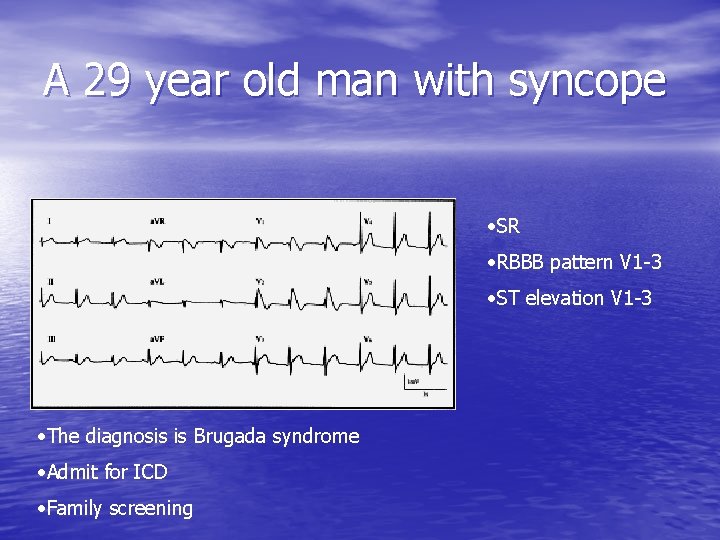
A 29 year old man with syncope • SR • RBBB pattern V 1 -3 • ST elevation V 1 -3 • The diagnosis is Brugada syndrome • Admit for ICD • Family screening
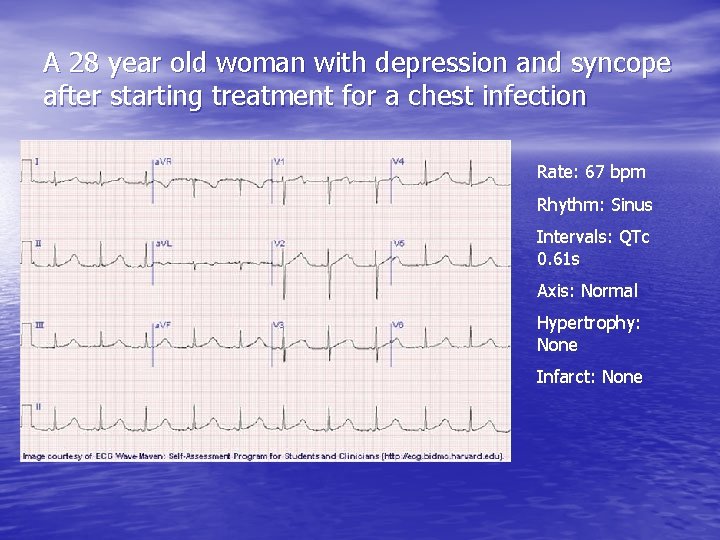
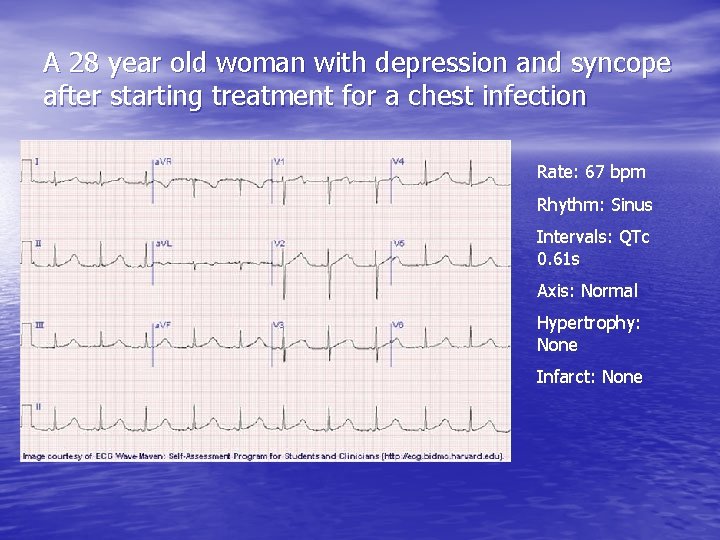
A 28 year old woman with depression and syncope after starting treatment for a chest infection Rate: 67 bpm Rhythm: Sinus Intervals: QTc 0. 61 s Axis: Normal Hypertrophy: None Infarct: None
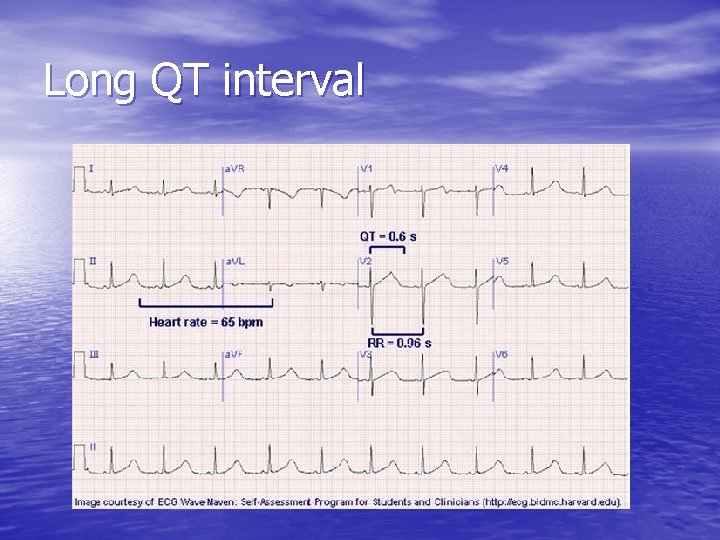
Long QT interval

ECG for screening purposes

A 42 year old man requiring medical clearance for an exercise program. He is a smoker, hypertensive and has a cholesterol of 6. 8 Rate: 70 Rhythm: Sinus Interval: Borderline PR prolongation (1 st degree AVB) Axis: Normal Hypertrophy: LVH and strain Infarct: Q waves V 1 -3 • This ECG shows an old septal MI (silent) and LVH and strain pattern • He cannot be cleared for his exercise program • He needs referral to cardiology for ETT and further assessment • In meantime commence aspirin, statin, ACEI, advice re MI signs.
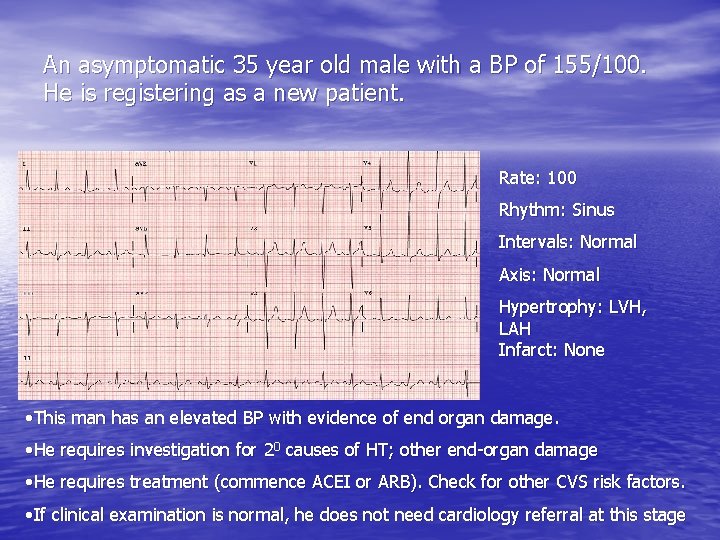
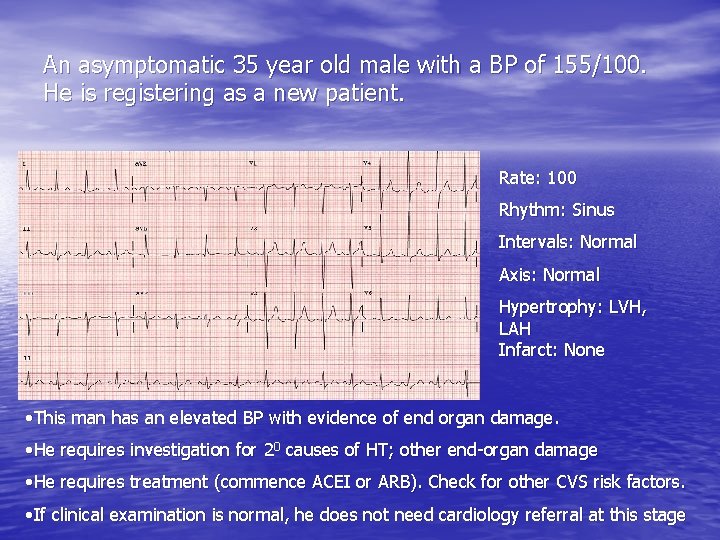
An asymptomatic 35 year old male with a BP of 155/100. He is registering as a new patient. Rate: 100 Rhythm: Sinus Intervals: Normal Axis: Normal Hypertrophy: LVH, LAH Infarct: None • This man has an elevated BP with evidence of end organ damage. • He requires investigation for 20 causes of HT; other end-organ damage • He requires treatment (commence ACEI or ARB). Check for other CVS risk factors. • If clinical examination is normal, he does not need cardiology referral at this stage

A 38 year old man whose brother died suddenly playing squash • Rate: 90 • Rhythm: Sinus • Intervals: Normal • Axis: Normal • Hypertrophy: LVH and strain • Infarct: None • Diagnosis: HOCM • Avoid physical exertion, commence beta-blocker • Urgent cardiology referral • Family screening (ECG and echo)
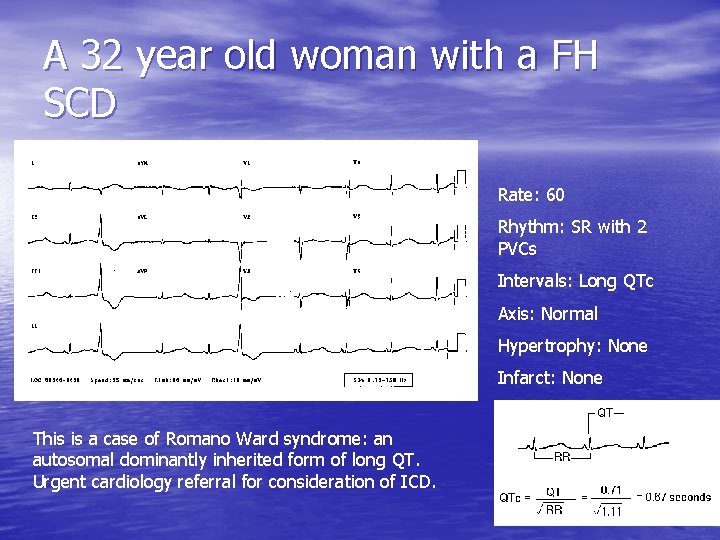
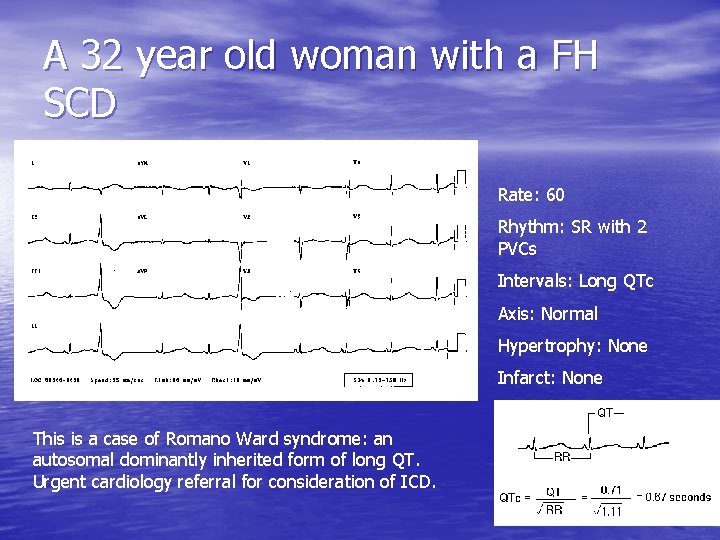
A 32 year old woman with a FH SCD Rate: 60 Rhythm: SR with 2 PVCs Intervals: Long QTc Axis: Normal Hypertrophy: None Infarct: None This is a case of Romano Ward syndrome: an autosomal dominantly inherited form of long QT. Urgent cardiology referral for consideration of ICD.
Now try some cases yourselves… • Remember – Rate – Rhythm – Intervals (PR, QRS, QTc) – Axis – Hypertrophy (ventricles and atria) – Infarct/ischaemia
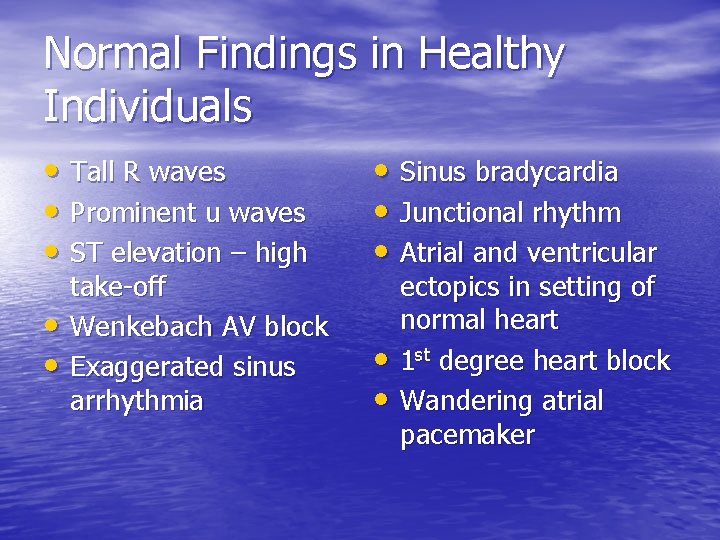
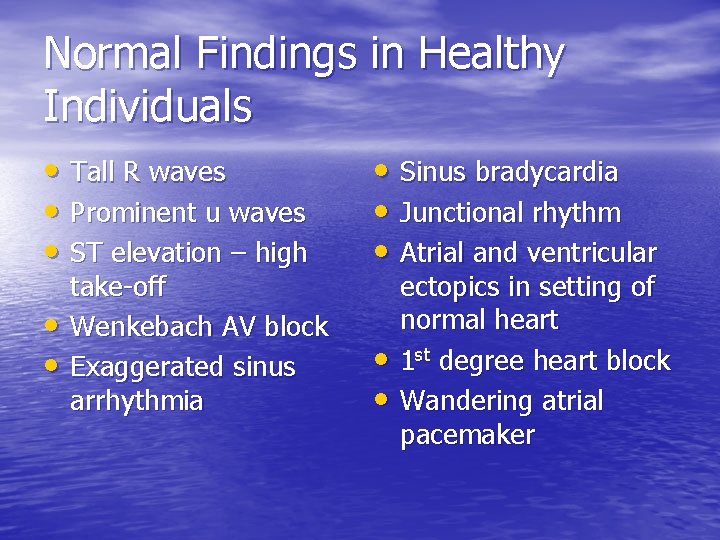
Normal Findings in Healthy Individuals • Tall R waves • Prominent u waves • ST elevation – high • • take-off Wenkebach AV block Exaggerated sinus arrhythmia • Sinus bradycardia • Junctional rhythm • Atrial and ventricular • • ectopics in setting of normal heart 1 st degree heart block Wandering atrial pacemaker

Summing up • ECG is a very valuable tool in primary care • The ECG, like any other test, must always be interpreted with the clinical scenario • Computer aided diagnosis and trained physician/nurse evaluation are complementary • Adopt a systematic approach to ECG evaluation

Summing up • Look at 5 areas in turn: – Rate – Rhythm (intervals) – Axis – Hypertrophy – Infarction/ischaemia

The Normal ECG Normal Intervals: PR 0. 12 -0. 20 s QRS duration <0. 12 s QTc 0. 33 -0. 43 s Normal P wave parameters: P wave width < 0. 12 s P wave height <2. 5 mm
 Sick sinus syndrome ecg criteria
Sick sinus syndrome ecg criteria Primary secondary tertiary health care definition
Primary secondary tertiary health care definition Sandeep singh jolly berlin
Sandeep singh jolly berlin Sandeep bhattaram
Sandeep bhattaram Sandeep somaiya
Sandeep somaiya Sandeep chinchali
Sandeep chinchali Sandeep walia md
Sandeep walia md Sandeep sahany
Sandeep sahany Sandeep agarwal aditya birla
Sandeep agarwal aditya birla Dean deakin
Dean deakin Sandeep tamrakar
Sandeep tamrakar Sandeep mallipattu
Sandeep mallipattu Gampa sandeep
Gampa sandeep Dr sandeep sekhon
Dr sandeep sekhon Sandeep modhvadia
Sandeep modhvadia Sandeep modhvadia
Sandeep modhvadia Sandeep baruah
Sandeep baruah Sandeep rajan md
Sandeep rajan md Personal care products seminar
Personal care products seminar Ee457
Ee457 Gandhi lord irwin
Gandhi lord irwin Gandhi rhetorical analysis
Gandhi rhetorical analysis Nelson mandela and gandhi venn diagram
Nelson mandela and gandhi venn diagram Mahatma gandhi life history
Mahatma gandhi life history Cuando nacio gandhi
Cuando nacio gandhi Savannah bukant
Savannah bukant Varsha gandhi
Varsha gandhi Mathatma ghandi
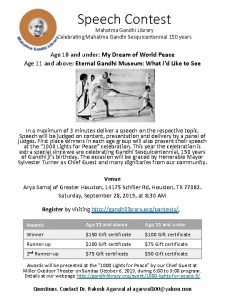
Mathatma ghandi Gandhi smriti library
Gandhi smriti library Gandhi king and mandela what made non-violence work dbq
Gandhi king and mandela what made non-violence work dbq Dr. anshul gandhi
Dr. anshul gandhi Trusteeship model of csr
Trusteeship model of csr Mirabel gandhi
Mirabel gandhi Gandhi niketan ashram history
Gandhi niketan ashram history Rajiv gandhi groundwater raipur
Rajiv gandhi groundwater raipur Gandhism
Gandhism Fact file on mahatma gandhi
Fact file on mahatma gandhi Gandhi dbq
Gandhi dbq Gandh
Gandh Sirswal caste category
Sirswal caste category Twenty points program
Twenty points program Objectives of kgbv
Objectives of kgbv Characteristics of competency
Characteristics of competency Dr shilpa gandhi
Dr shilpa gandhi Gandhi lesson plan
Gandhi lesson plan Gandhi 3 movie
Gandhi 3 movie Dr. vidyachandra gandhi
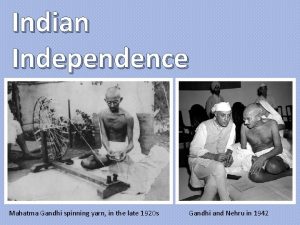
Dr. vidyachandra gandhi Gandhi spinning yarn
Gandhi spinning yarn Why did gandhi encourage indians to weave their own cloth?
Why did gandhi encourage indians to weave their own cloth? Quora
Quora Gandhi
Gandhi Mahatma gandhi transformational leader
Mahatma gandhi transformational leader Gandhi
Gandhi Gandhi disobbedienza civile frasi
Gandhi disobbedienza civile frasi Vidhyachandra gandhi
Vidhyachandra gandhi Brian dominick
Brian dominick Mahatma gandhi university library
Mahatma gandhi university library Poesia mahatma gandhi
Poesia mahatma gandhi Mahatma gandhi young photo
Mahatma gandhi young photo Sabar dan bijak ala gandhi
Sabar dan bijak ala gandhi Vyomika gandhi
Vyomika gandhi Mahatma gandhi bibliografia
Mahatma gandhi bibliografia Mahatma gandhi short note
Mahatma gandhi short note Lions are mostly nocturnal predators phrase or clause
Lions are mostly nocturnal predators phrase or clause Gandhi (film)
Gandhi (film) Nikhil gandhi pipavav
Nikhil gandhi pipavav Gandhi presentation
Gandhi presentation Vidhyachandra gandhi
Vidhyachandra gandhi The primary pigment colors are ____.
The primary pigment colors are ____. Trafford primary care trust
Trafford primary care trust Uccs lane center
Uccs lane center Australian primary health care research institute
Australian primary health care research institute Starfield primary care
Starfield primary care Team nursing
Team nursing Dc primary care association
Dc primary care association Konsep primary health care
Konsep primary health care Principles of primary health care
Principles of primary health care Principles of phc
Principles of phc Defination of phc
Defination of phc Concepts of primary health care
Concepts of primary health care United healthcare community plan primary care providers
United healthcare community plan primary care providers Mount auburn primary care
Mount auburn primary care Modello primary care
Modello primary care Icd 10 buka jahitan
Icd 10 buka jahitan Types of family in community medicine
Types of family in community medicine Extended primary care team
Extended primary care team Structural adjustment programs
Structural adjustment programs Multicultural primary care
Multicultural primary care Wellone primary care
Wellone primary care Kent station clinic primary care
Kent station clinic primary care Primary care information project
Primary care information project Dr sanjiv ahluwalia
Dr sanjiv ahluwalia Basic requirements for sound phc
Basic requirements for sound phc Primary care network map
Primary care network map Sutton & merton primary care trust
Sutton & merton primary care trust Goroll primary care medicine test bank
Goroll primary care medicine test bank Missouri primary care association
Missouri primary care association United states bureau of labor statistics
United states bureau of labor statistics Swedish primary care shoreline
Swedish primary care shoreline Feinberg match list
Feinberg match list Nutrition in primary health care
Nutrition in primary health care Direct primary care lincoln ne
Direct primary care lincoln ne Elements of primary health care
Elements of primary health care Comprehensive primary health care approach
Comprehensive primary health care approach Principles of community health
Principles of community health Severn school of primary care
Severn school of primary care Alexandra primary school student care
Alexandra primary school student care West lancashire primary care trust
West lancashire primary care trust Primary school camp packing list
Primary school camp packing list Team and modular nursing
Team and modular nursing