Primary bloodstream infection as an indication Regulatory perspective
Primary bloodstream infection as an indication: Regulatory perspective FDA/IDSA/ISAP Workshop April 15, 2004 David Ross, M. D. , Ph. D.
Outline • Regulatory history • Defining anti-infective (AI) indications • Primary bloodstream infection as an AI indication 2
Bloodstream infection (BSI): history • 10 drugs indicated for bacteremia or septicemia • All labeled prior to 1992 • Labeling based on variable or unspecified clinical manifestations in different studies • Includes bacteremia associated with focal infection and bacteremia of unknown origin • Patients pooled from trials of other indications 3
9/93 Anti-Infective Drugs AC meeting • Bacteremia did not affect outcome in a large NDA dataset • Bacteremia is due to infection at a primary site • Bacteremic SIRS patients form a heterogeneous population • Unclear if bacteremic SIRS patients were sicker than nonbacteremic patients 4
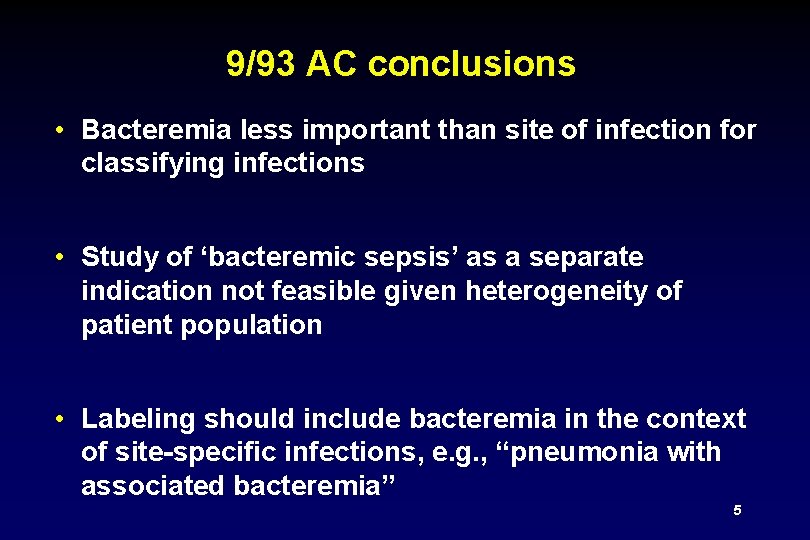
9/93 AC conclusions • Bacteremia less important than site of infection for classifying infections • Study of ‘bacteremic sepsis’ as a separate indication not feasible given heterogeneity of patient population • Labeling should include bacteremia in the context of site-specific infections, e. g. , “pneumonia with associated bacteremia” 5
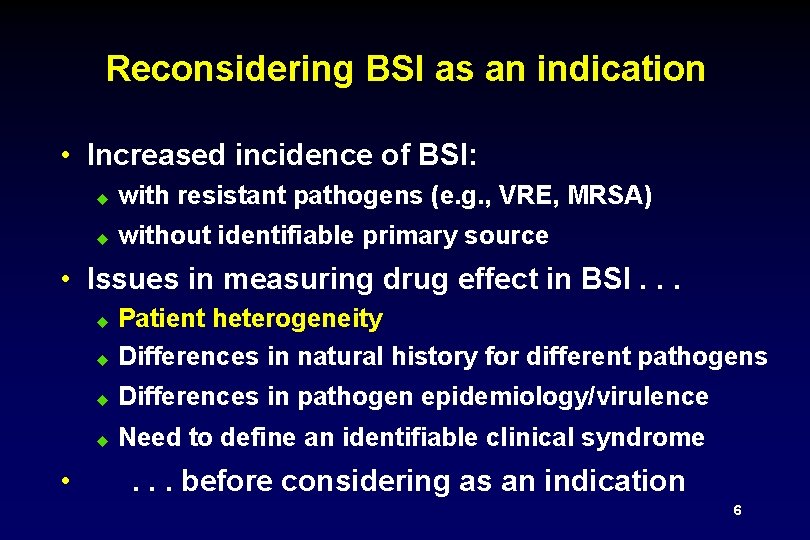
Reconsidering BSI as an indication • Increased incidence of BSI: u with resistant pathogens (e. g. , VRE, MRSA) u without identifiable primary source • Issues in measuring drug effect in BSI. . . u Patient heterogeneity Differences in natural history for different pathogens u Differences in pathogen epidemiology/virulence u Need to define an identifiable clinical syndrome u • . . . before considering as an indication 6
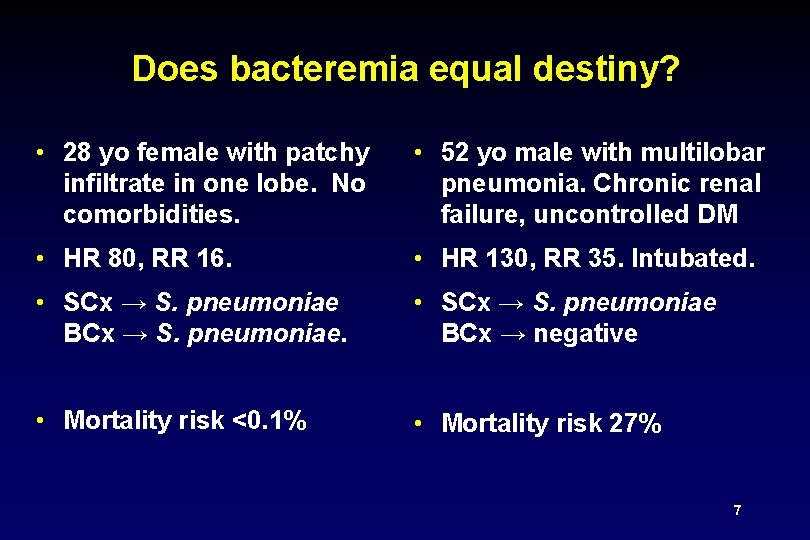
Does bacteremia equal destiny? • 28 yo female with patchy infiltrate in one lobe. No comorbidities. • 52 yo male with multilobar pneumonia. Chronic renal failure, uncontrolled DM • HR 80, RR 16. • HR 130, RR 35. Intubated. • SCx → S. pneumoniae BCx → S. pneumoniae. • SCx → S. pneumoniae BCx → negative • Mortality risk <0. 1% • Mortality risk 27% 7
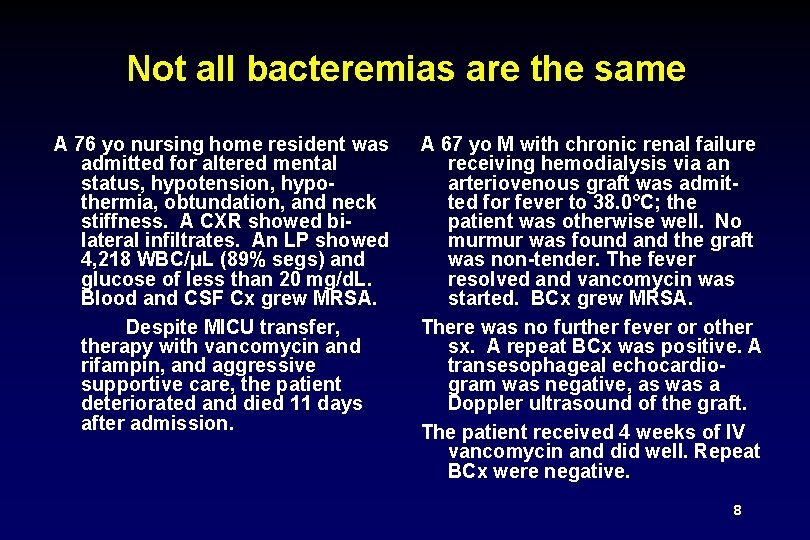
Not all bacteremias are the same A 76 yo nursing home resident was admitted for altered mental status, hypotension, hypothermia, obtundation, and neck stiffness. A CXR showed bilateral infiltrates. An LP showed 4, 218 WBC/μL (89% segs) and glucose of less than 20 mg/d. L. Blood and CSF Cx grew MRSA. Despite MICU transfer, therapy with vancomycin and rifampin, and aggressive supportive care, the patient deteriorated and died 11 days after admission. A 67 yo M with chronic renal failure receiving hemodialysis via an arteriovenous graft was admitted for fever to 38. 0°C; the patient was otherwise well. No murmur was found and the graft was non-tender. The fever resolved and vancomycin was started. BCx grew MRSA. There was no further fever or other sx. A repeat BCx was positive. A transesophageal echocardiogram was negative, as was a Doppler ultrasound of the graft. The patient received 4 weeks of IV vancomycin and did well. Repeat BCx were negative. 8
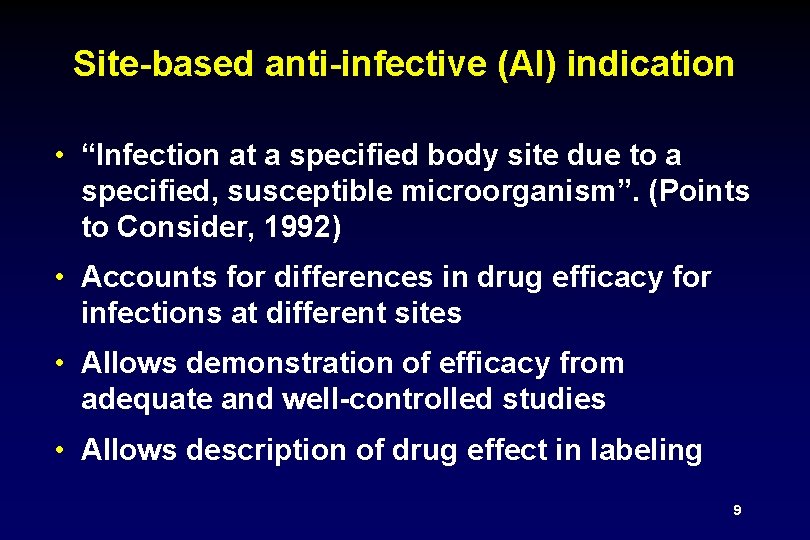
Site-based anti-infective (AI) indication • “Infection at a specified body site due to a specified, susceptible microorganism”. (Points to Consider, 1992) • Accounts for differences in drug efficacy for infections at different sites • Allows demonstration of efficacy from adequate and well-controlled studies • Allows description of drug effect in labeling 9
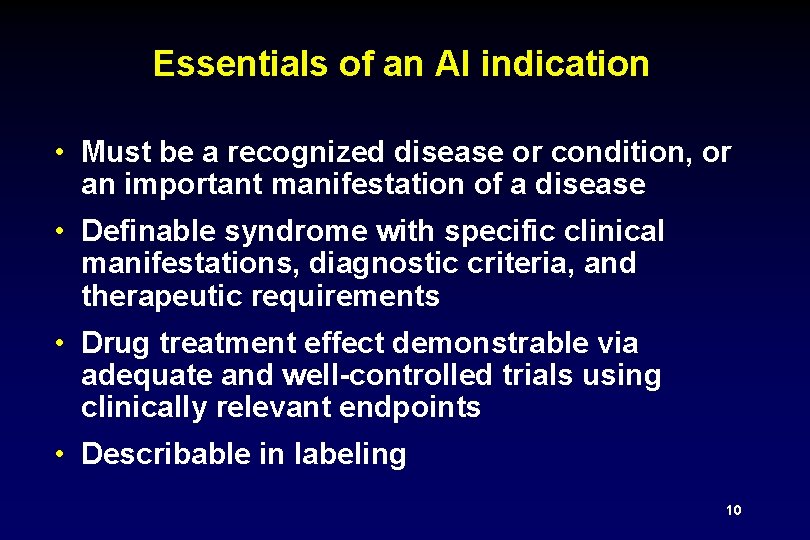
Essentials of an AI indication • Must be a recognized disease or condition, or an important manifestation of a disease • Definable syndrome with specific clinical manifestations, diagnostic criteria, and therapeutic requirements • Drug treatment effect demonstrable via adequate and well-controlled trials using clinically relevant endpoints • Describable in labeling 10
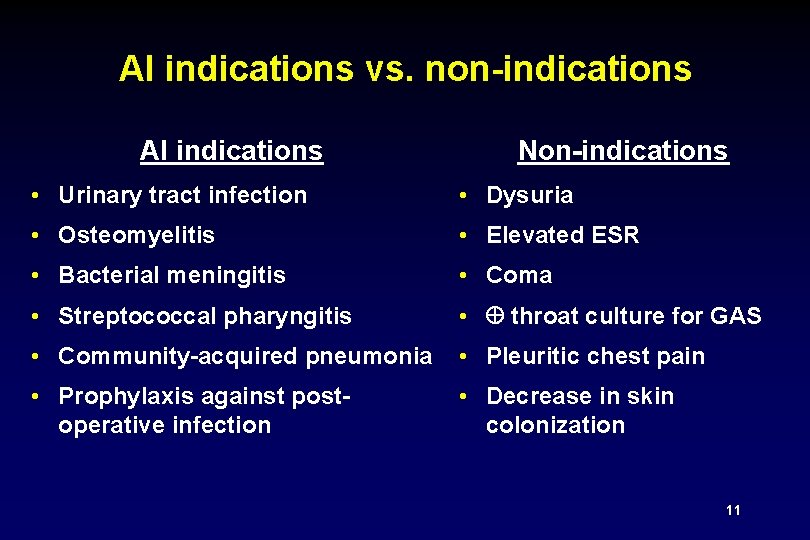
AI indications vs. non-indications AI indications Non-indications • Urinary tract infection • Dysuria • Osteomyelitis • Elevated ESR • Bacterial meningitis • Coma • Streptococcal pharyngitis • throat culture for GAS • Community-acquired pneumonia • Pleuritic chest pain • Prophylaxis against postoperative infection • Decrease in skin colonization 11
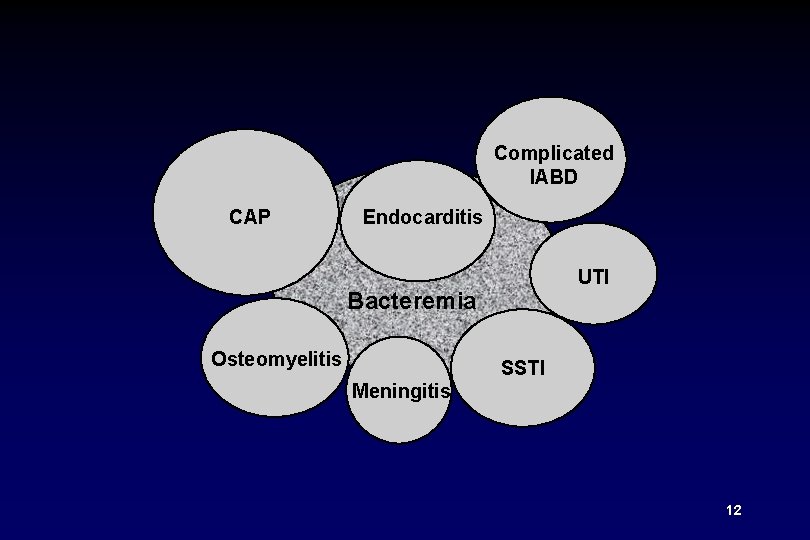
Complicated IABD CAP Endocarditis UTI Bacteremia Osteomyelitis SSTI Meningitis 12
BSI vs. bacteremia • Candidal BSI (candidemia) u Accepted AI indication u Frequently primary BSI (no identifed underlying infection) u Definable clinical syndrome • Escherichia coli bacteremia u Not accepted AI indication u Virtually never primary BSI u Variety of potential underlying infections (e. g. , GI, GU) u Variety of clinical manifestations 13
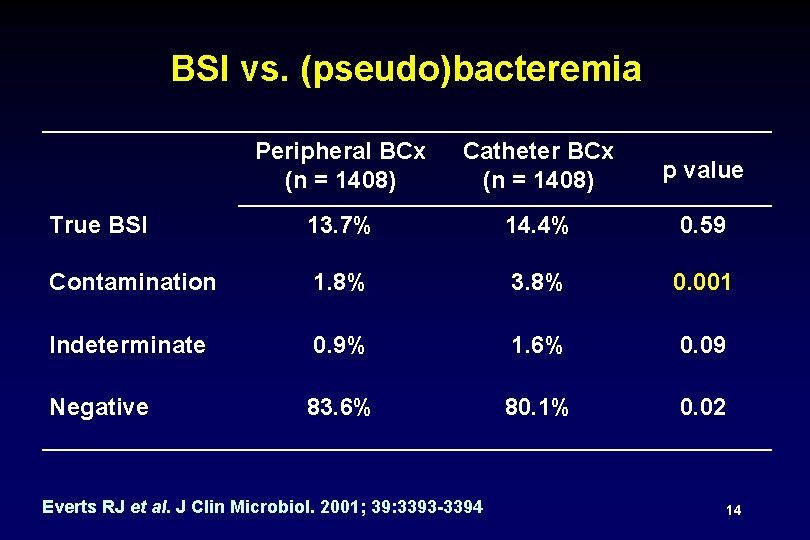
BSI vs. (pseudo)bacteremia Peripheral BCx (n = 1408) Catheter BCx (n = 1408) p value True BSI 13. 7% 14. 4% 0. 59 Contamination 1. 8% 3. 8% 0. 001 Indeterminate 0. 9% 1. 6% 0. 09 Negative 83. 6% 80. 1% 0. 02 Everts RJ et al. J Clin Microbiol. 2001; 39: 3393 -3394 14
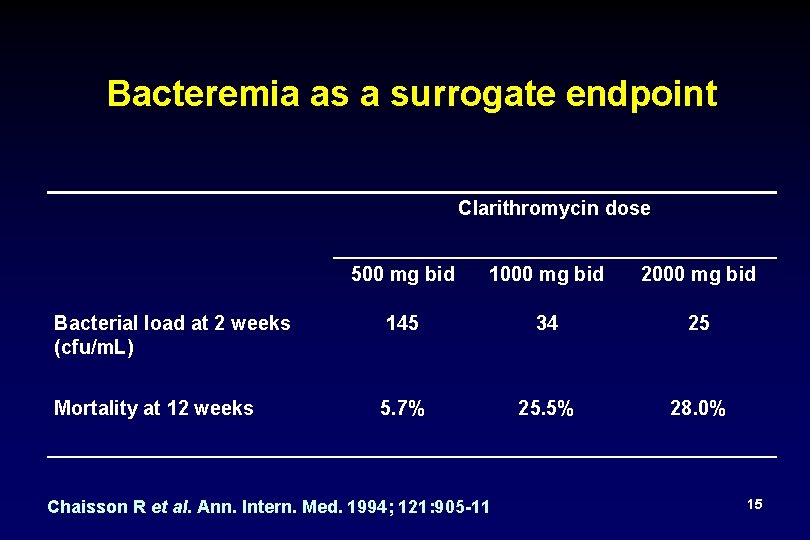
Bacteremia as a surrogate endpoint Clarithromycin dose Bacterial load at 2 weeks (cfu/m. L) Mortality at 12 weeks 500 mg bid 1000 mg bid 2000 mg bid 145 34 25 5. 7% 25. 5% 28. 0% Chaisson R et al. Ann. Intern. Med. 1994; 121: 905 -11 15
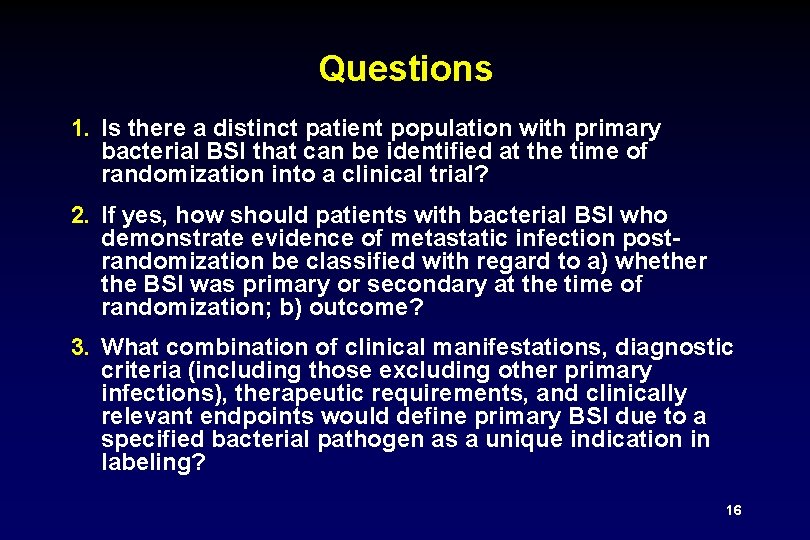
Questions 1. Is there a distinct patient population with primary bacterial BSI that can be identified at the time of randomization into a clinical trial? 2. If yes, how should patients with bacterial BSI who demonstrate evidence of metastatic infection postrandomization be classified with regard to a) whether the BSI was primary or secondary at the time of randomization; b) outcome? 3. What combination of clinical manifestations, diagnostic criteria (including those excluding other primary infections), therapeutic requirements, and clinically relevant endpoints would define primary BSI due to a specified bacterial pathogen as a unique indication in labeling? 16
- Slides: 16