Primary Angle Closure PAC F Fazel MD Reference










- Slides: 38
Primary Angle Closure (PAC) F. Fazel MD Reference: PPP American academy of ophthalmology 2010
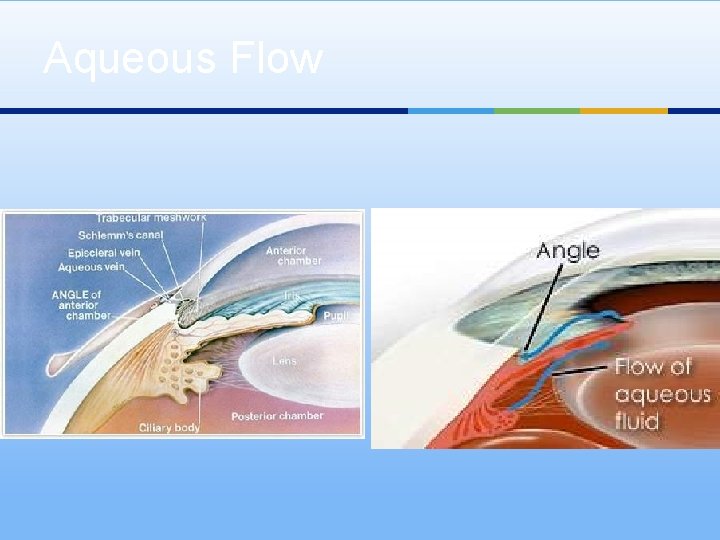
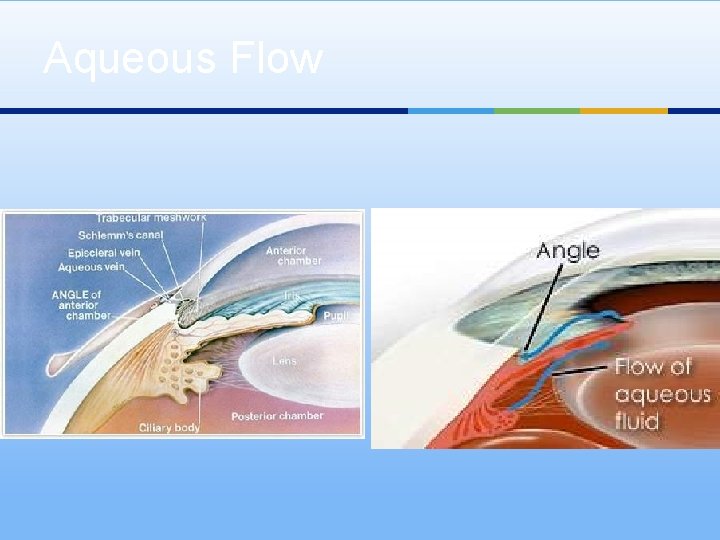
Aqueous Flow
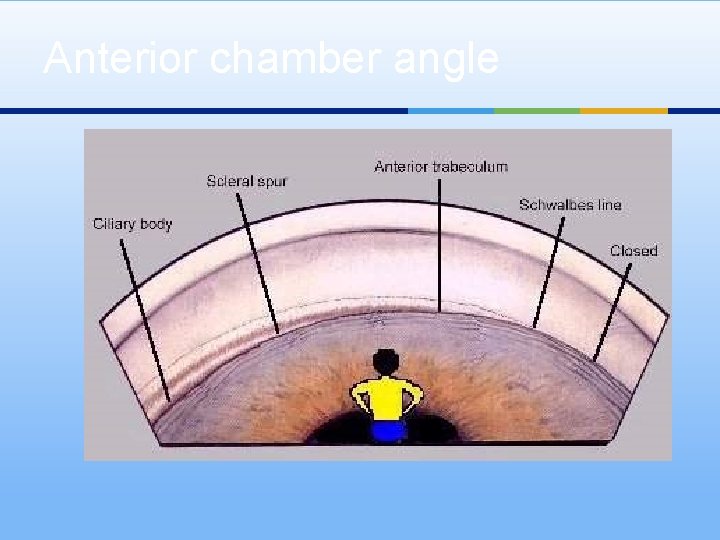
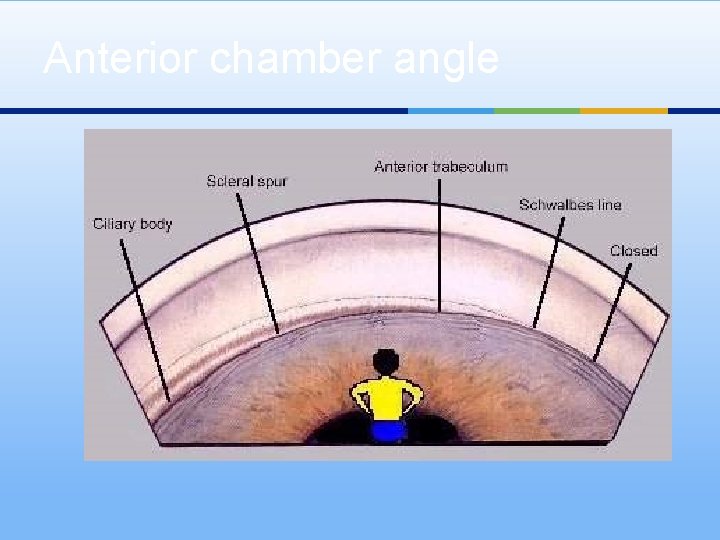
Anterior chamber angle
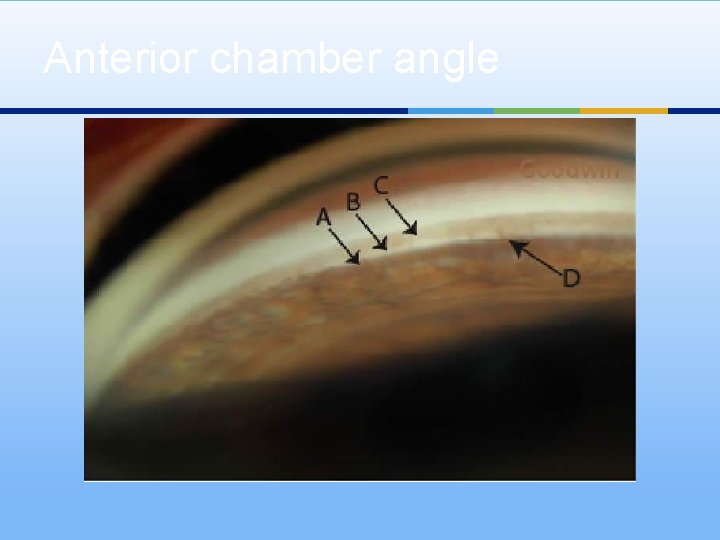
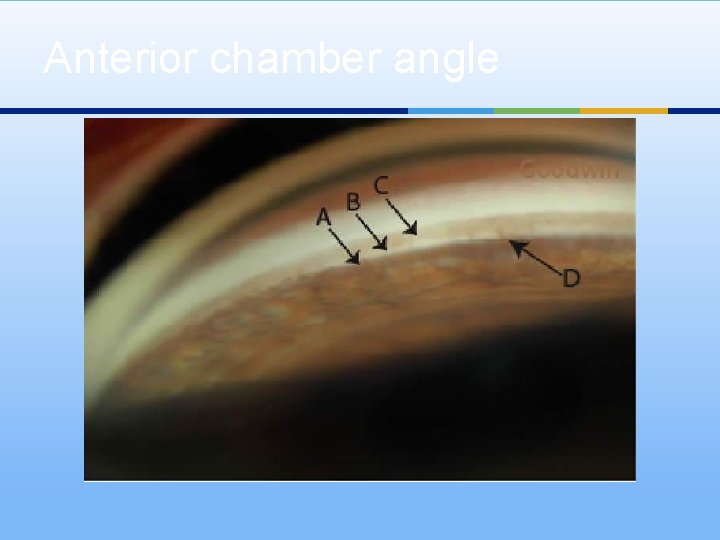
Anterior chamber angle
Angle Closure: Disease Definition Appositional or synechial closure of AC angle. ¥ Pupil block is key element. ¥ Pressure of PC is higher than AC causing ant -bowing of iris and crowd the angle. ¥ Pupil dilatation and thickening of lens increase pressure disparity of two chambers. ¥ Other mechanisms(position and thickness of CB, location of iris insertion, volume of iris, . . ). ¥ Lens size, position, shape play important role. ¥
Definition cont. . ¥ Contact of iris periphery with TM lead to functional damage of TM and PAS formation. ¥ PAC may occur as Acute form or Chronic. ¥ Secondary form of angle closure (ICE syndrome, inflammation, or neovascularization)
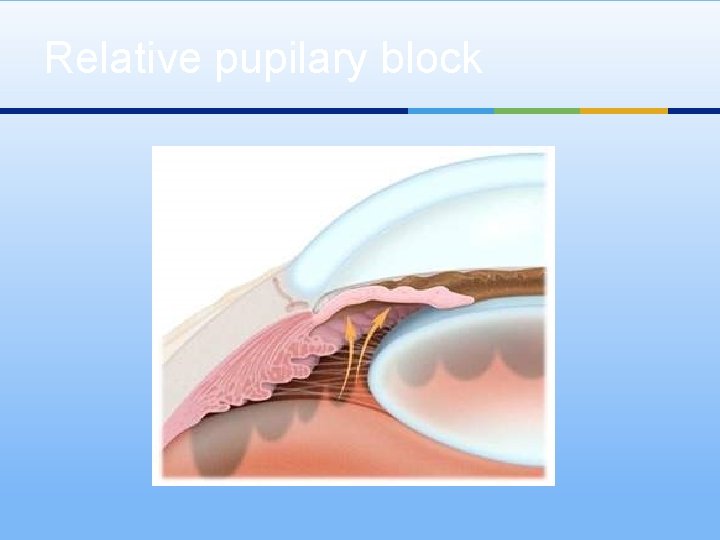
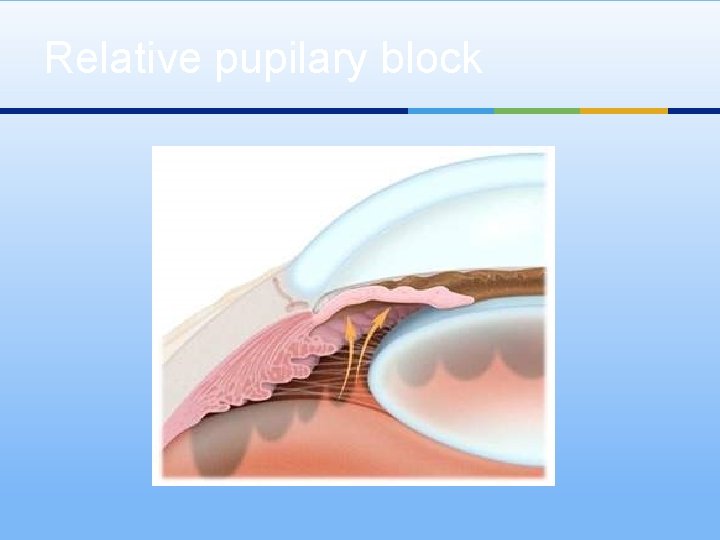
Relative pupilary block
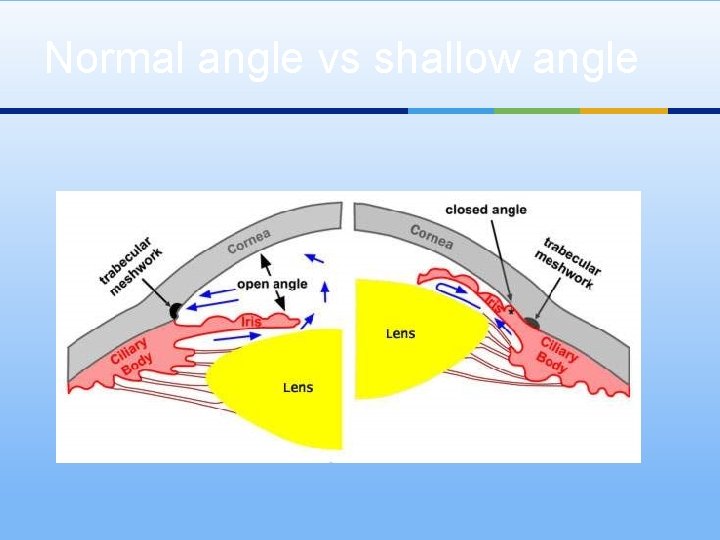
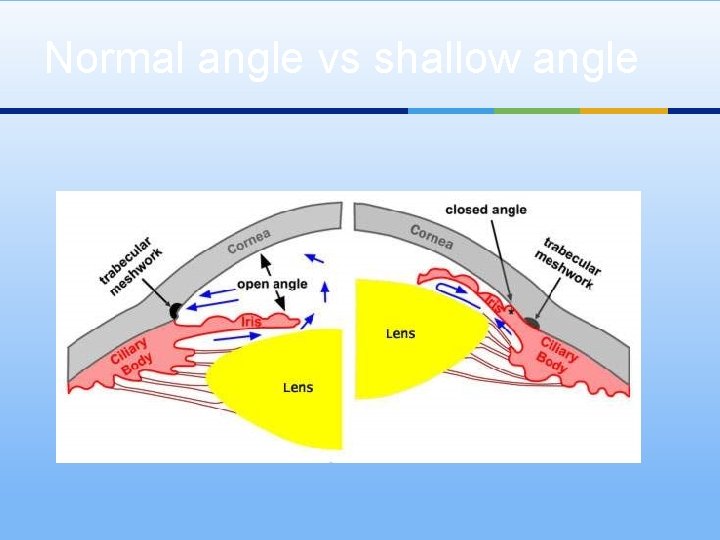
Normal angle vs shallow angle
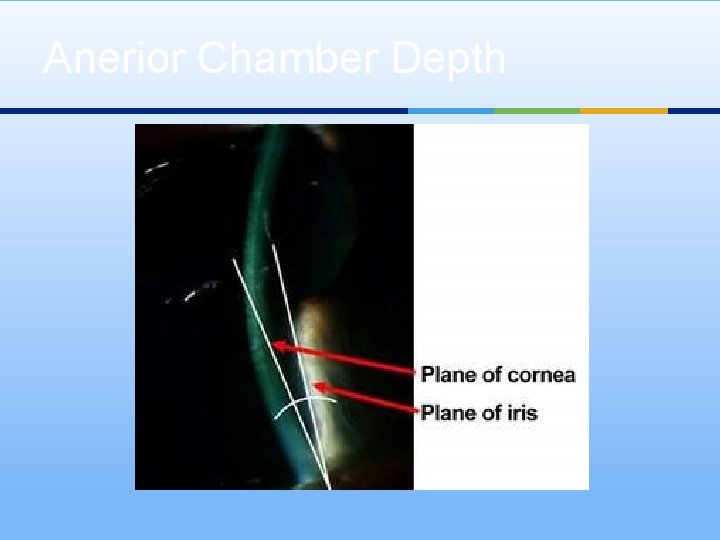
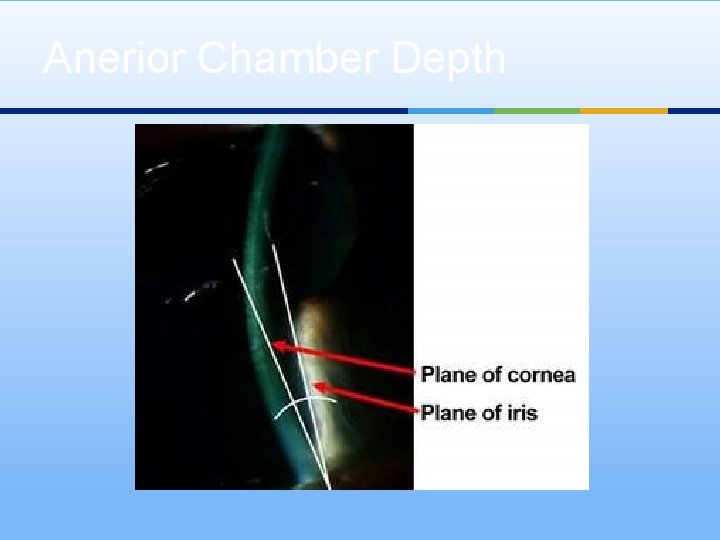
Anerior Chamber Depth
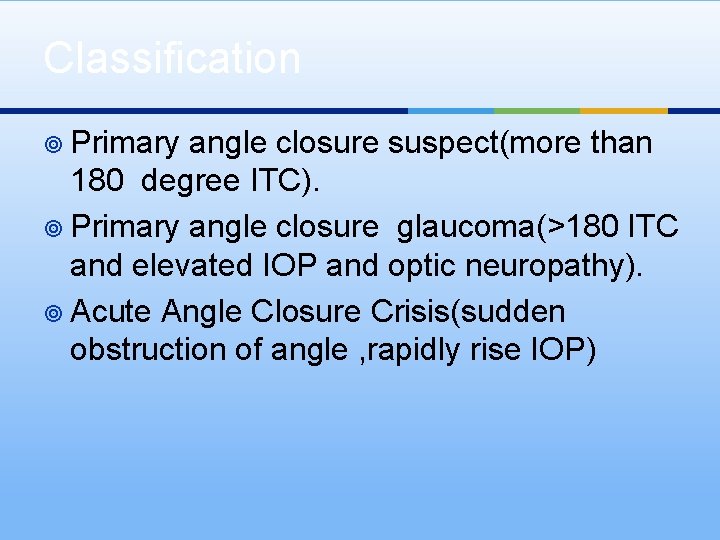
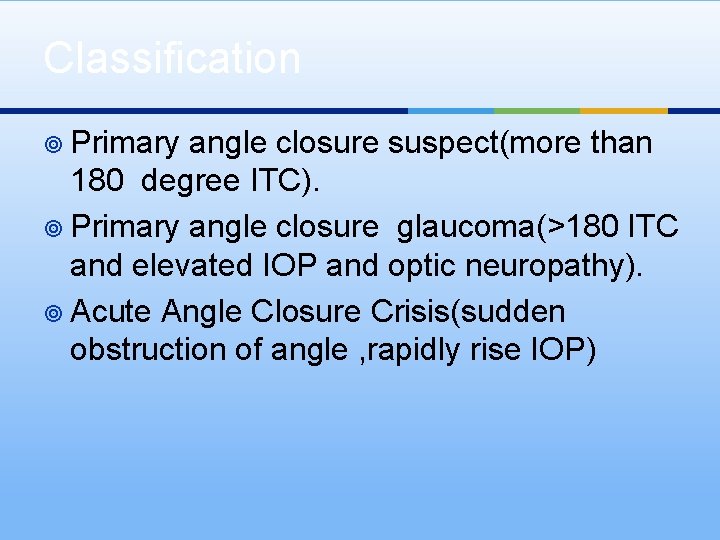
Classification ¥ Primary angle closure suspect(more than 180 degree ITC). ¥ Primary angle closure glaucoma(>180 ITC and elevated IOP and optic neuropathy). ¥ Acute Angle Closure Crisis(sudden obstruction of angle , rapidly rise IOP)

Risk Factors Demographic Factors ¥ ¥ Family history Older age Female sex Asian or Inuit descent Ocular Factors ¥ ¥ ¥ Hyperopia Shallow peripheral and central AC depth Steep corneal curvature Thick crystalline lens Short axial length

Natural History ¥ PAC is bilateral. ¥ 90% of acute attack are unilateral. ¥ In ACCC optic neuropathy rapidly developed ¥ Fellow phakic eye are at risk ¥ Significant visual morbidity after ACCC
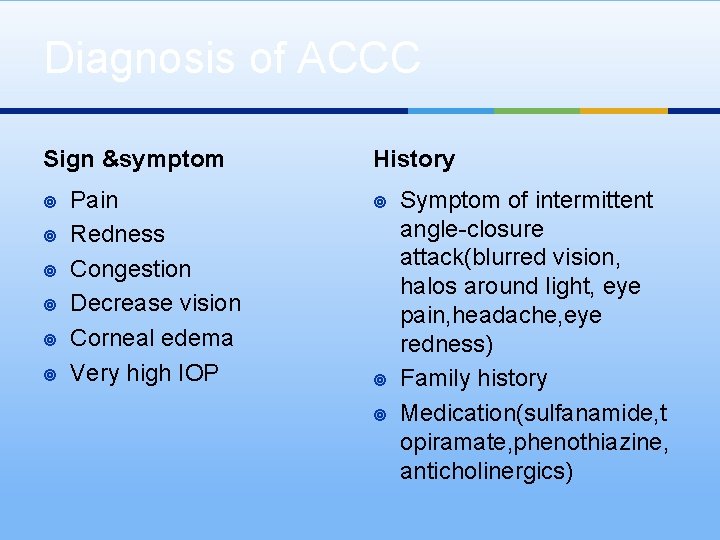
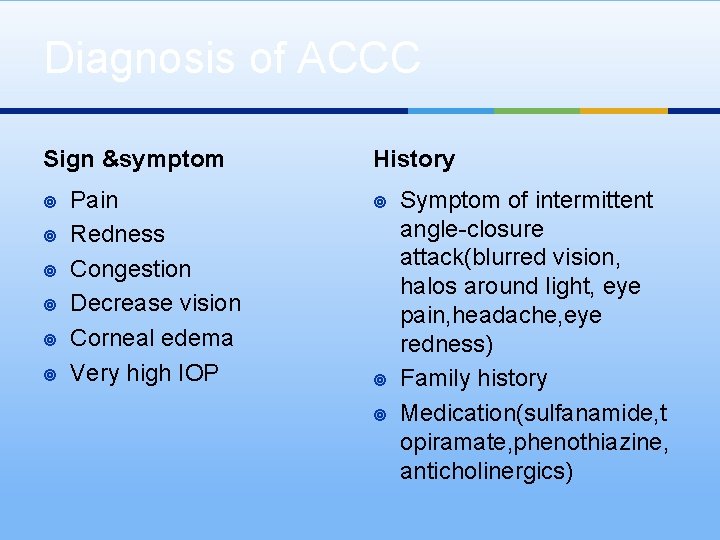
Diagnosis of ACCC Sign &symptom ¥ ¥ ¥ Pain Redness Congestion Decrease vision Corneal edema Very high IOP History ¥ ¥ ¥ Symptom of intermittent angle-closure attack(blurred vision, halos around light, eye pain, headache, eye redness) Family history Medication(sulfanamide, t opiramate, phenothiazine, anticholinergics)
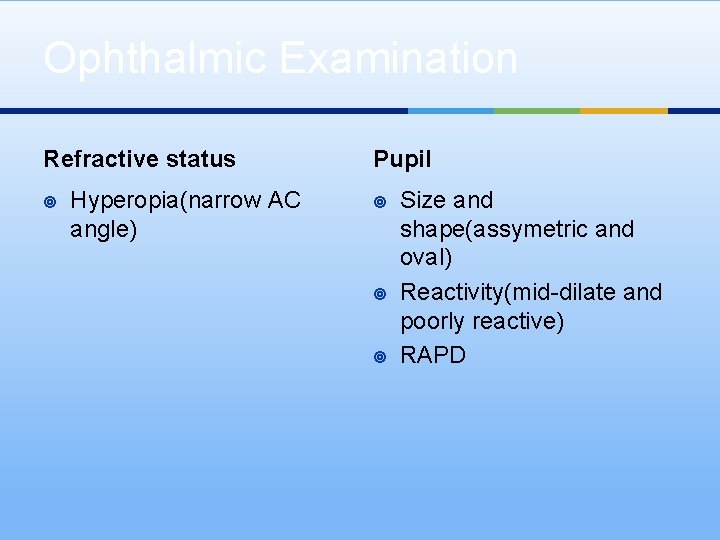
Ophthalmic Examination Refractive status ¥ Hyperopia(narrow AC angle) Pupil ¥ ¥ ¥ Size and shape(assymetric and oval) Reactivity(mid-dilate and poorly reactive) RAPD

Slit-lamp biomicroscopy ¥ Conjunctival hyperemia ¥ Narrow AC depth ¥ AC inflammation ¥ Corneal swelling ¥ Iris abnormality(focal or diffuse atrophy, irrigular pupil, PS, . . ) ¥ Lens change(glaucomflecken, cataract) ¥ Corneal endothelial cell loss
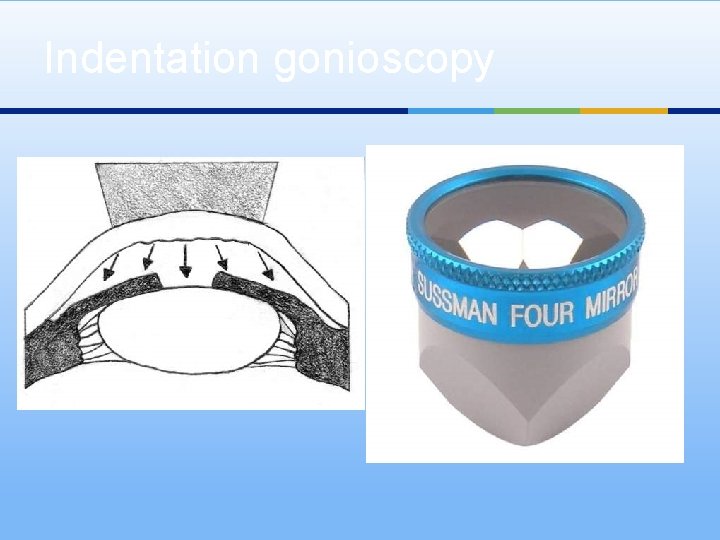
Examination Determination of IOP ¥ ¥ Goldman applanation Ccc measurement postponed Gonioscopy ¥ ¥ Of both eyes is mandatory To determine appositional closure, PAS and extend of them Topical glyserin in corneal edema. Compression (indentation) gonioscopy is more helpful
Other Exams ¥ Immaging (UBM, OCT…) ¥ Provocative test ¥ Fundus exam

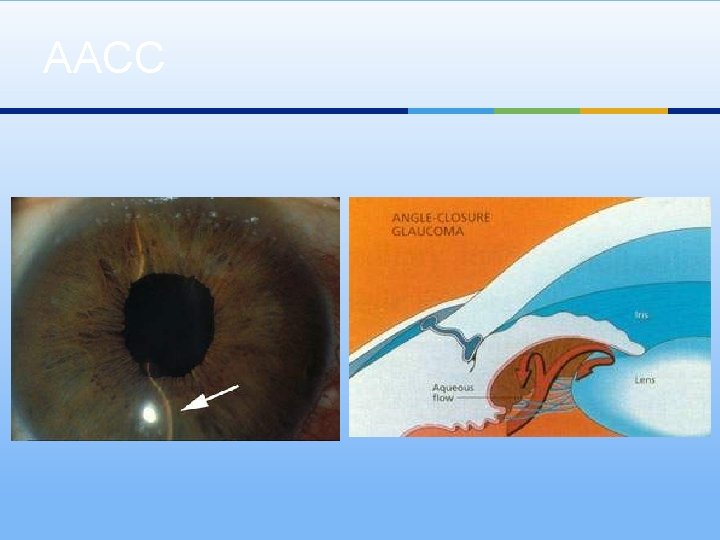
AACC

Bilateral AACC
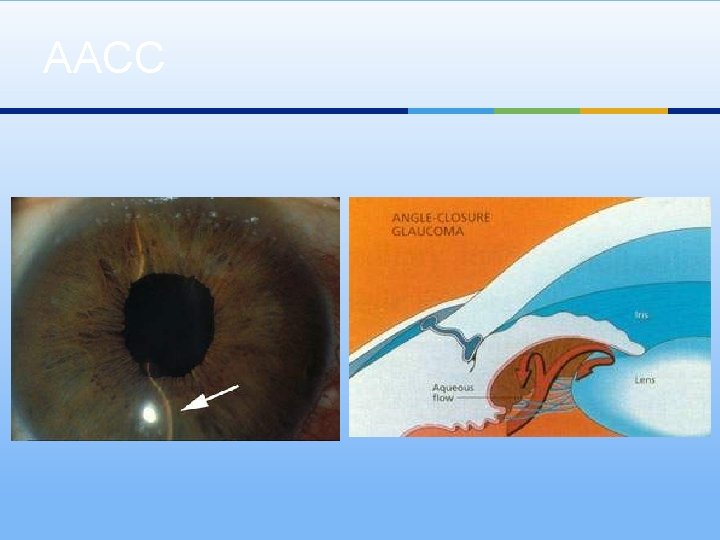
AACC
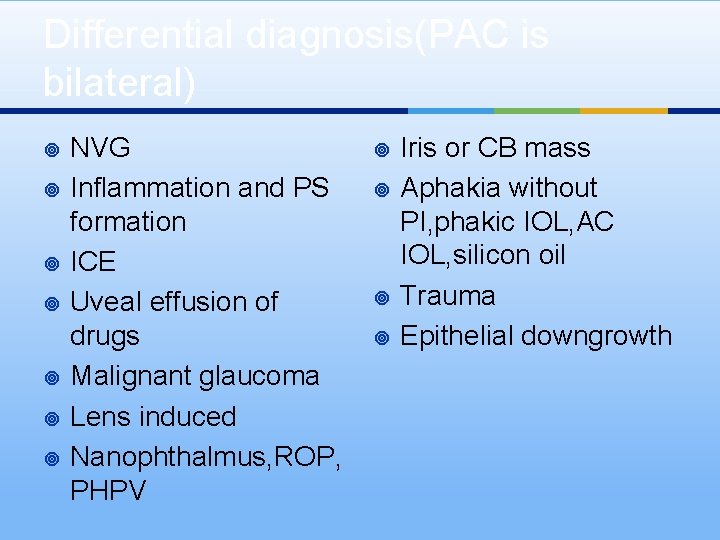
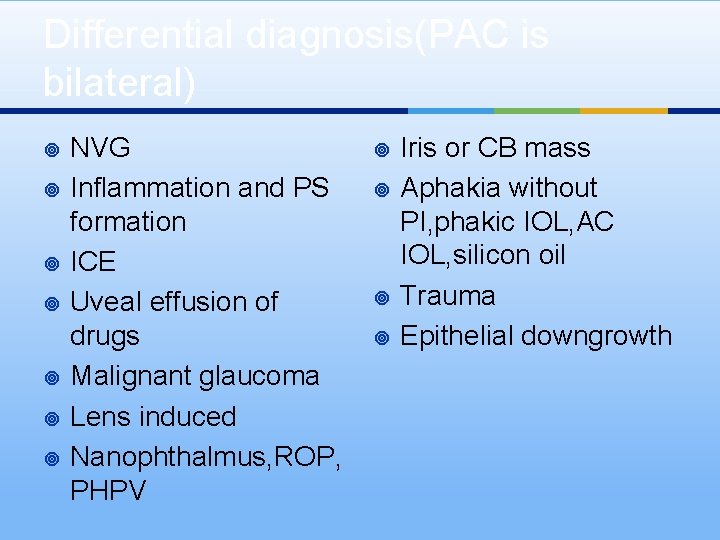
Differential diagnosis(PAC is bilateral) ¥ ¥ ¥ ¥ NVG Inflammation and PS formation ICE Uveal effusion of drugs Malignant glaucoma Lens induced Nanophthalmus, ROP, PHPV ¥ ¥ Iris or CB mass Aphakia without PI, phakic IOL, AC IOL, silicon oil Trauma Epithelial downgrowth

Management : Goals ¥ Reverse or prevent angle-closure process ¥ Control IOP ¥ Prevent damage to optic nerve
Management : Step 1 Lowering IOP to relieve acute symptom and potentially harmful high IOP. Reduced inflammation ¥ ¥ ¥ Medical therapy Peripheral laser iridoplasty paracentesis
Medical Therapy ¥ ¥ ¥ Topical Beta-blocker Topical Alpha Agonist Topical and systemic CAI Topical miotics Systemic hyperosmotic Topical steroid ¥ ¥ ¥ Timolol or Betaxolol Brimonidin or alphagun Acetazolamide: IV-PO Pilocarpin Glycerin or Manitol Prednisolone or dexa
Failed medical therapy or laser iridotomy ¥ Laser peripheral iridoplasty ¥ Paracenthesis ¥ Incisional iridectomy
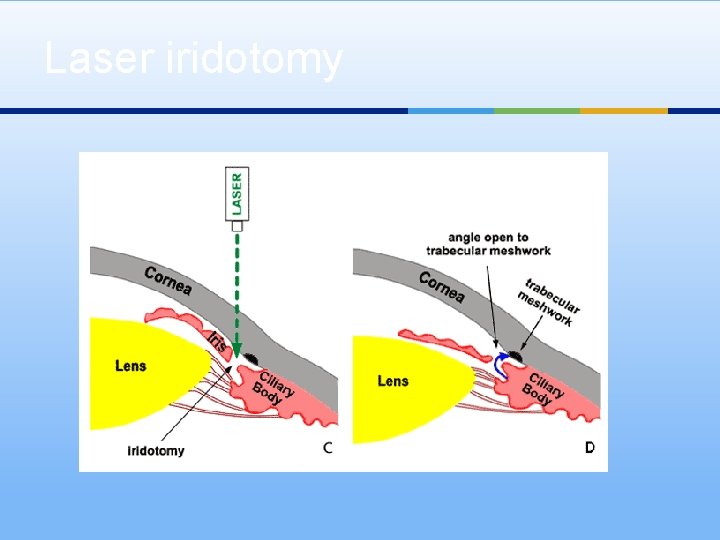
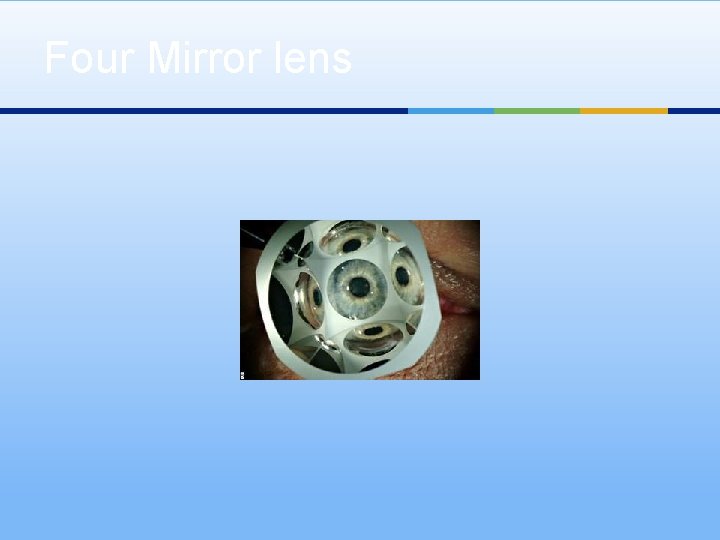
Relieves pupilary block: Step 2 (AS SOON AS POSSIBLE) ¥ Laser iridotomy ¥ Corneal indentation(four-mirror, cottontipped applicator, or tip of muscle hook)
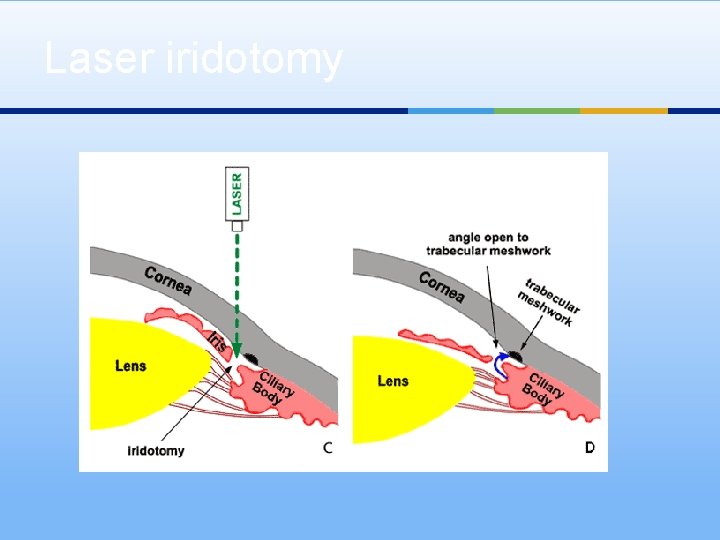
Laser iridotomy
Fellow-eye management: Step 3 ¥ Immediate laser iridotomy.
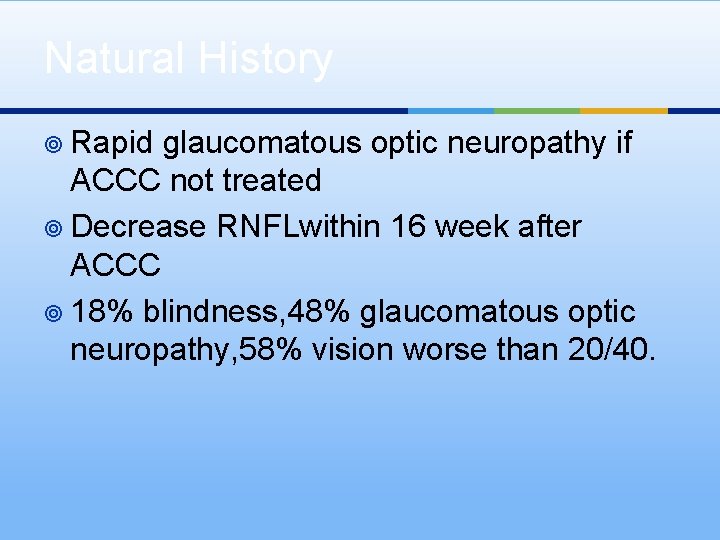
Natural History ¥ Rapid glaucomatous optic neuropathy if ACCC not treated ¥ Decrease RNFLwithin 16 week after ACCC ¥ 18% blindness, 48% glaucomatous optic neuropathy, 58% vision worse than 20/40.
Follow-up Evaluation: Step 4 ¥ After PI patient may have open angle or open sector with PAS. ¥ Evaluate patency of PI ¥ IOP measurment ¥ Gonioscopy ¥ Fundus exam

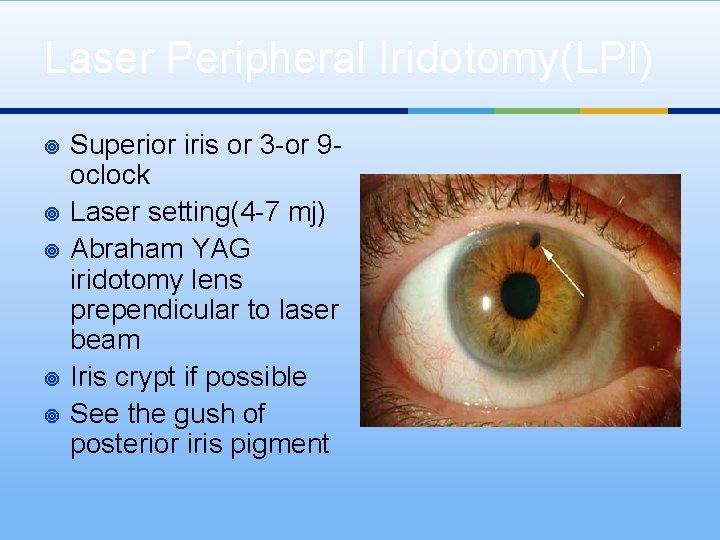
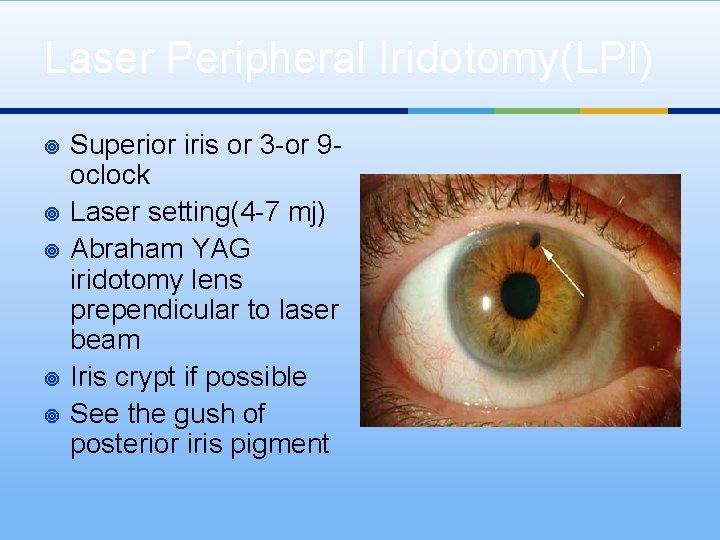
Laser Peripheral Iridotomy(LPI) ¥ ¥ ¥ Superior iris or 3 -or 9 oclock Laser setting(4 -7 mj) Abraham YAG iridotomy lens prependicular to laser beam Iris crypt if possible See the gush of posterior iris pigment

Abraham YAG-Laser lens

Effect of laser iridotomy
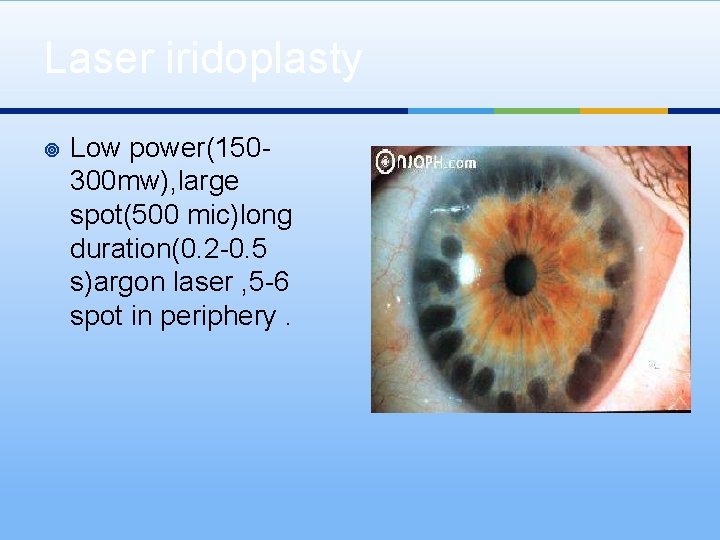
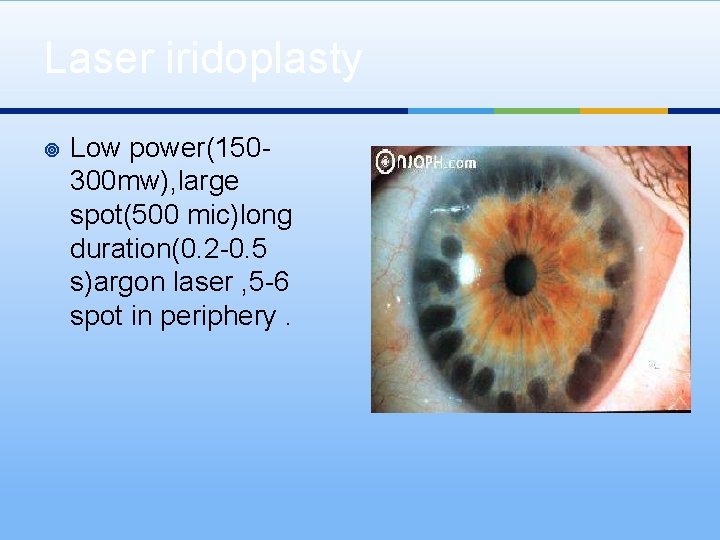
Laser iridoplasty ¥ Low power(150300 mw), large spot(500 mic)long duration(0. 2 -0. 5 s)argon laser , 5 -6 spot in periphery.

Type of Gonioscopy lenses
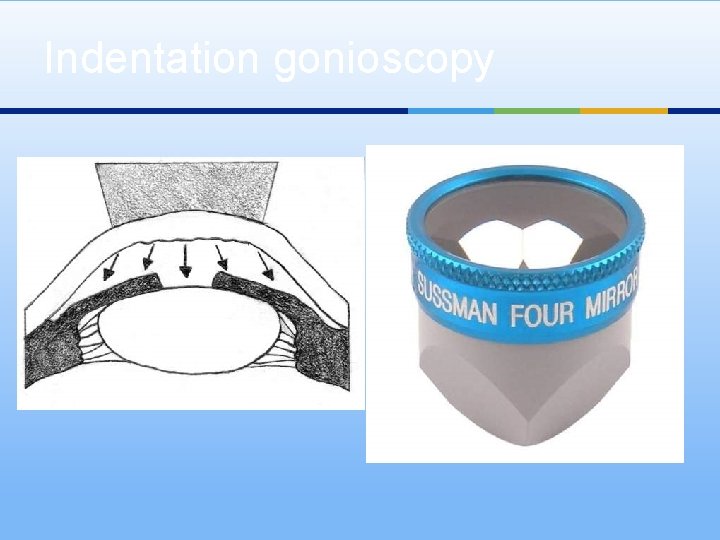
Indentation gonioscopy
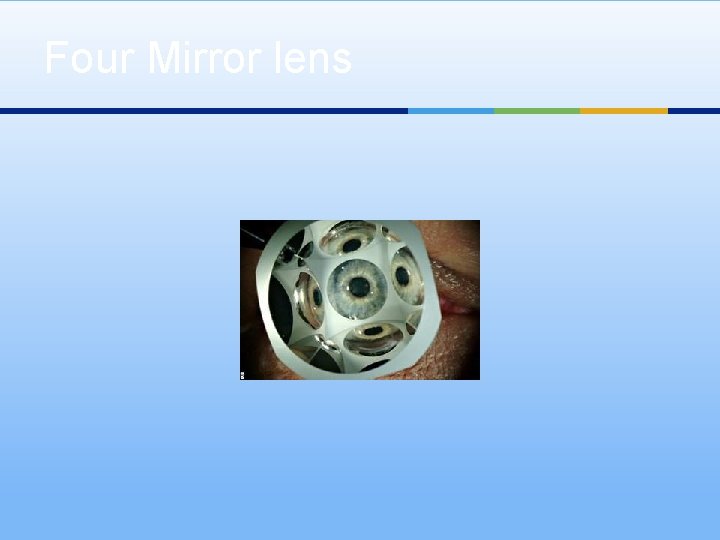
Four Mirror lens