Prevention of Surgical Site Infections Considerations in Measuring


- Slides: 47
Prevention of Surgical Site Infections: Considerations in Measuring Effectiveness Michele L. Pearson, MD Division of Healthcare Quality Promotion National Center for Infectious Diseases
Objectives • Provide overview of epidemiology of surgical site infections (SSI) • Discuss SSI prevention strategies • Highlight current surveillance systems for SSI • Provide overview of HICPAC/CDC process for developing recommendations for prevention healthcare-associated infections
Public Health Importance of Surgical Site Infections • In U. S. , >40 million inpatient surgical procedures each year; 2 -5% complicated by surgical site infection • SSIs second most common nosocomial infection (24% of all nosocomial infections) • Prolong hospital stay by 7. 4 days • Cost $400 -$2, 600 per infection (TOTAL: $130 -$845 million/year)
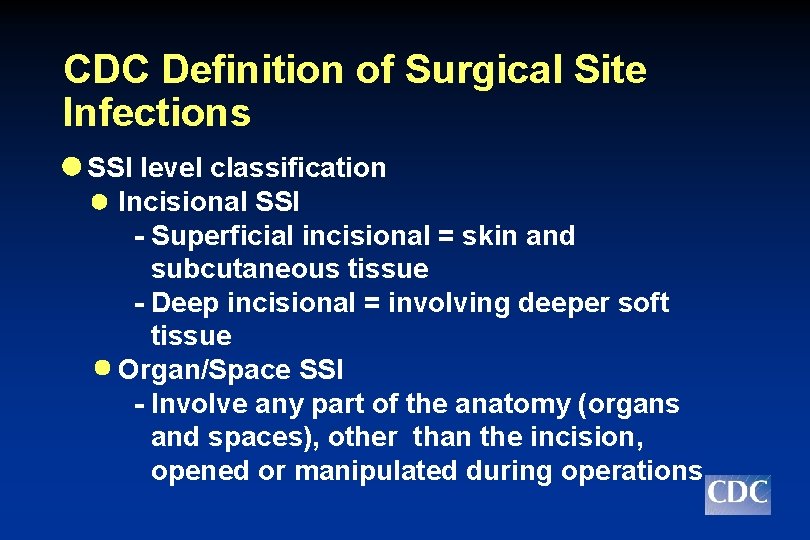
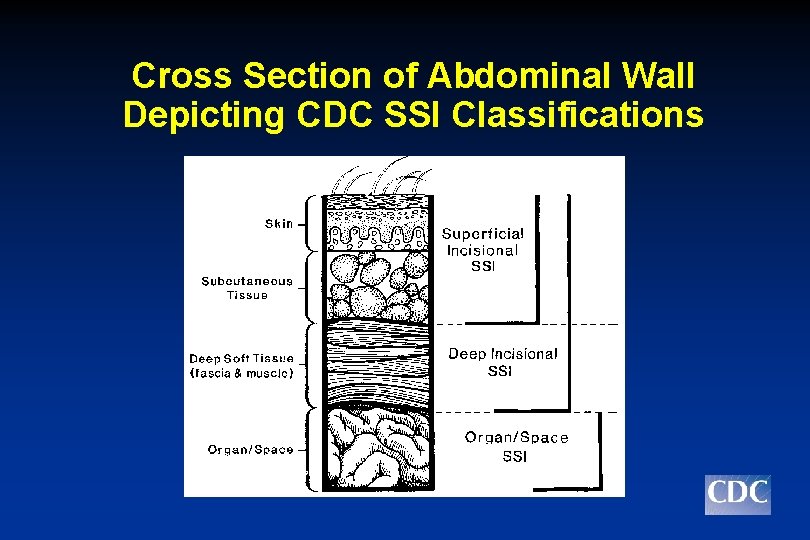
CDC Definition of Surgical Site Infections SSI level classification Incisional SSI - Superficial incisional = skin and subcutaneous tissue - Deep incisional = involving deeper soft tissue Organ/Space SSI - Involve any part of the anatomy (organs and spaces), other than the incision, opened or manipulated during operations
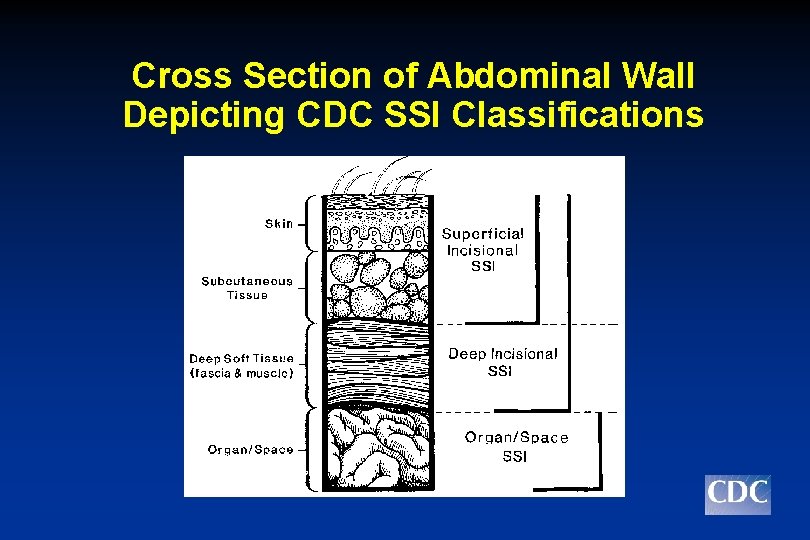
Cross Section of Abdominal Wall Depicting CDC SSI Classifications
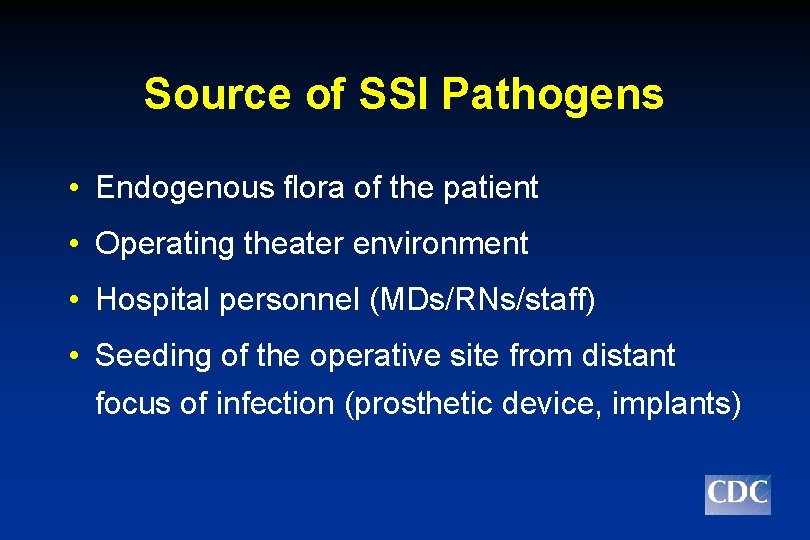
Source of SSI Pathogens • Endogenous flora of the patient • Operating theater environment • Hospital personnel (MDs/RNs/staff) • Seeding of the operative site from distant focus of infection (prosthetic device, implants)
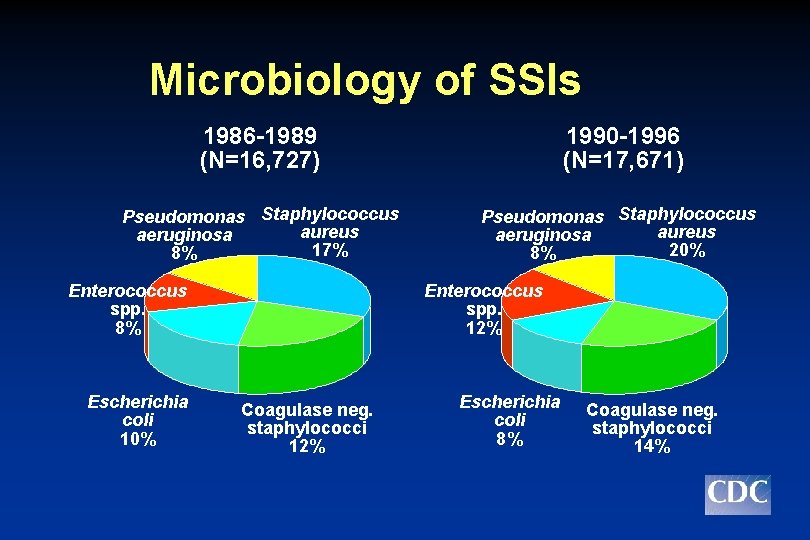
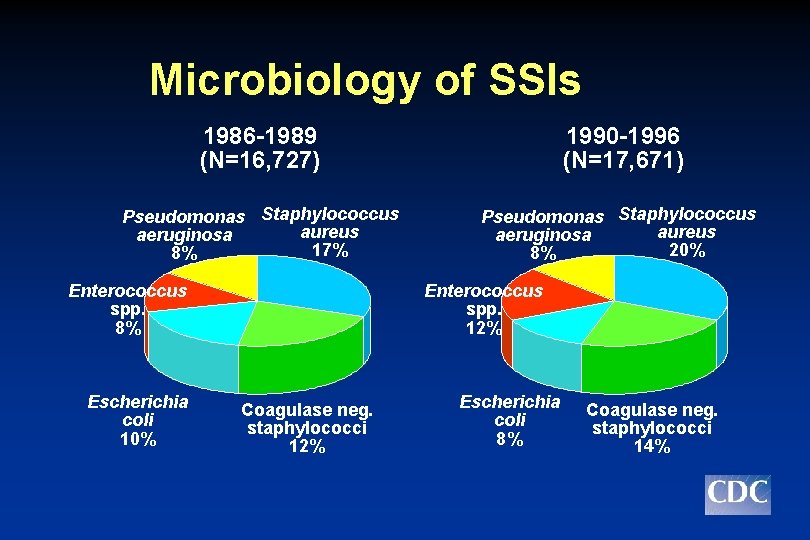
Microbiology of SSIs 1986 -1989 (N=16, 727) 1990 -1996 (N=17, 671) Pseudomonas Staphylococcus aureus aeruginosa 17% 8% Pseudomonas Staphylococcus aureus aeruginosa 20% 8% Enterococcus spp. 8% Escherichia coli 10% Enterococcus spp. 12% Coagulase neg. staphylococci 12% Escherichia coli 8% Coagulase neg. staphylococci 14%
Microbiology of SSIs • Unusual pathogens • Rhizopus oryzea - elastoplast adhesive bandage • Clostridium perfringens - elastic bandages • Rhodococcus bronchialis - colonized health care personnel • Legionella dumoffii and pneumophila - tap water • Pseudomonas multivorans - disinfectant solution
Pathogenesis of SSI • Relationship equation Dose of bacterial contamination x Virulence Resistance of host
SSI Risk Factors • • • Age Obesity Diabetes Malnutrition Prolonged preoperative stay • Infection at remote site • Systemic steroid use • Nicotine use • • • Hair removal/Shaving Duration of surgery Surgical technique Presence of drains Inappropriate use of antimicrobial prophylaxis
Perioperative Preventive Measures
Role of Antimicrobial Prophylaxis (AP) in Preventing SSI • Refers to very brief course of an antimicrobial agent initiated just before the operation begins • Should be viewed as an adjunctive preventive measure • Appropriately administered AP associated with a 5 -fold decrease in SSI rates
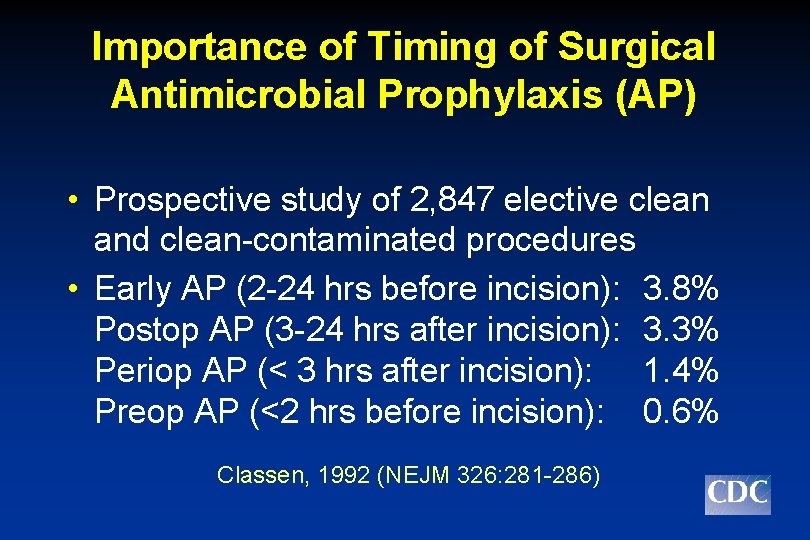
Importance of Timing of Surgical Antimicrobial Prophylaxis (AP) • Prospective study of 2, 847 elective clean and clean-contaminated procedures • Early AP (2 -24 hrs before incision): 3. 8% Postop AP (3 -24 hrs after incision): 3. 3% Periop AP (< 3 hrs after incision): 1. 4% Preop AP (<2 hrs before incision): 0. 6% Classen, 1992 (NEJM 326: 281 -286)
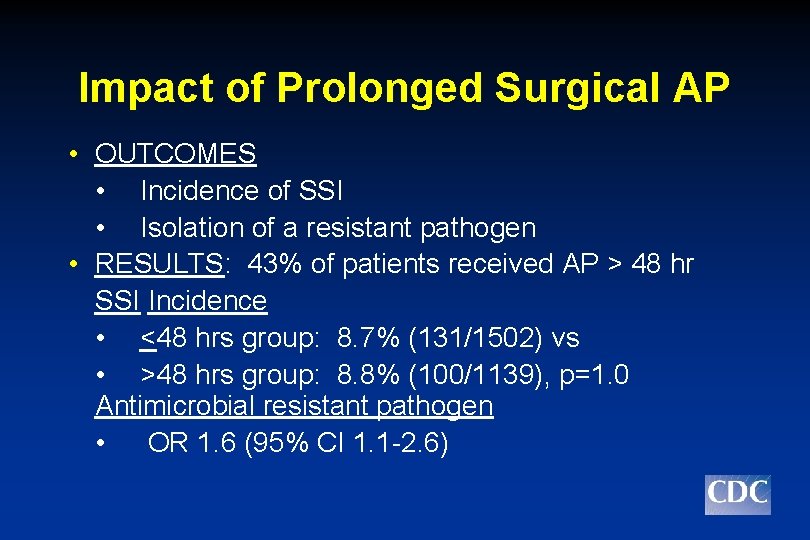
Impact of Prolonged Surgical Prophylaxis • DESIGN: Prospective • POPULATION: CABG patients (N=2641) Group 1: pts who received < 48 hours of AP Group 2: pts who received > 48 hrs of AP
Impact of Prolonged Surgical AP • OUTCOMES • Incidence of SSI • Isolation of a resistant pathogen • RESULTS: 43% of patients received AP > 48 hr SSI Incidence • <48 hrs group: 8. 7% (131/1502) vs • >48 hrs group: 8. 8% (100/1139), p=1. 0 Antimicrobial resistant pathogen • OR 1. 6 (95% CI 1. 1 -2. 6)
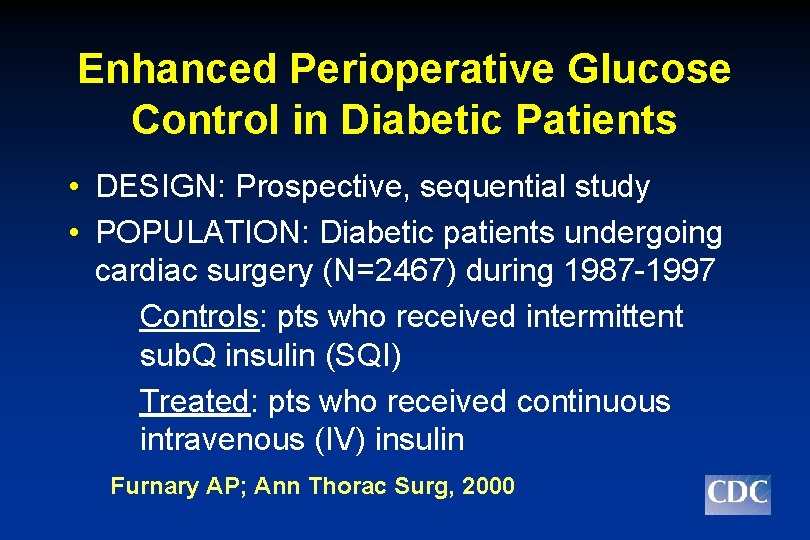
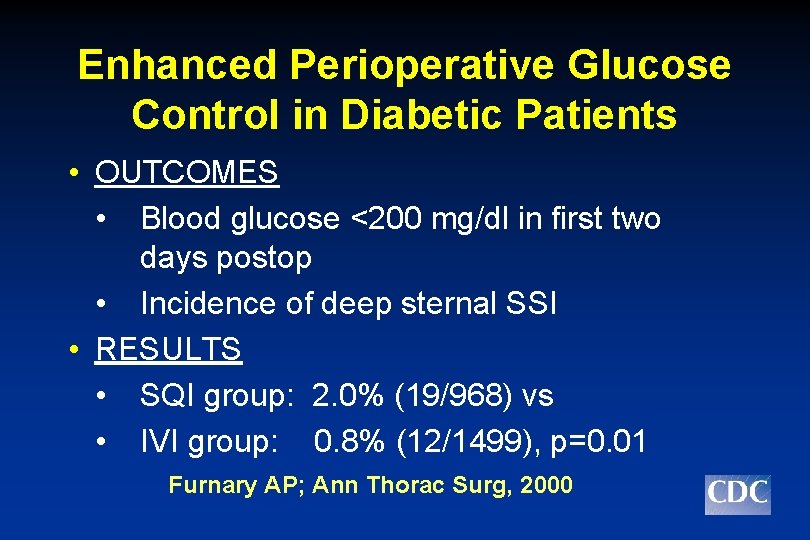
Enhanced Perioperative Glucose Control in Diabetic Patients • DESIGN: Prospective, sequential study • POPULATION: Diabetic patients undergoing cardiac surgery (N=2467) during 1987 -1997 Controls: pts who received intermittent sub. Q insulin (SQI) Treated: pts who received continuous intravenous (IV) insulin Furnary AP; Ann Thorac Surg, 2000
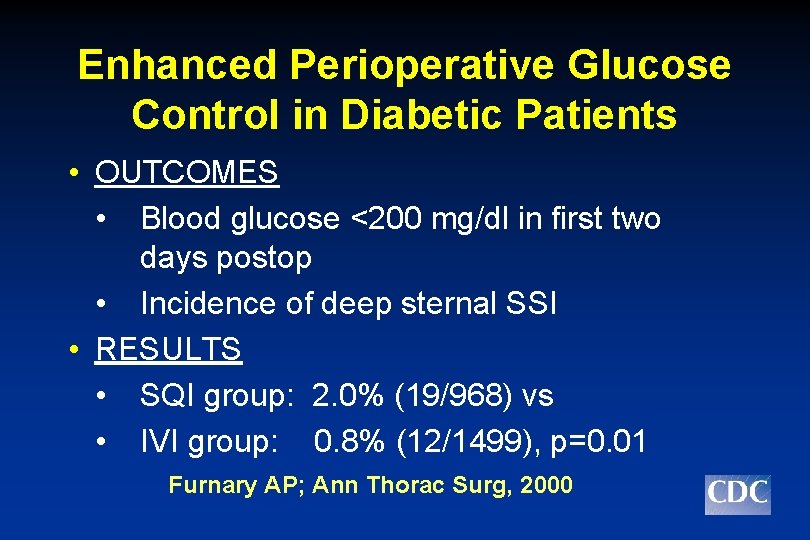
Enhanced Perioperative Glucose Control in Diabetic Patients • OUTCOMES • Blood glucose <200 mg/dl in first two days postop • Incidence of deep sternal SSI • RESULTS • SQI group: 2. 0% (19/968) vs • IVI group: 0. 8% (12/1499), p=0. 01 Furnary AP; Ann Thorac Surg, 2000
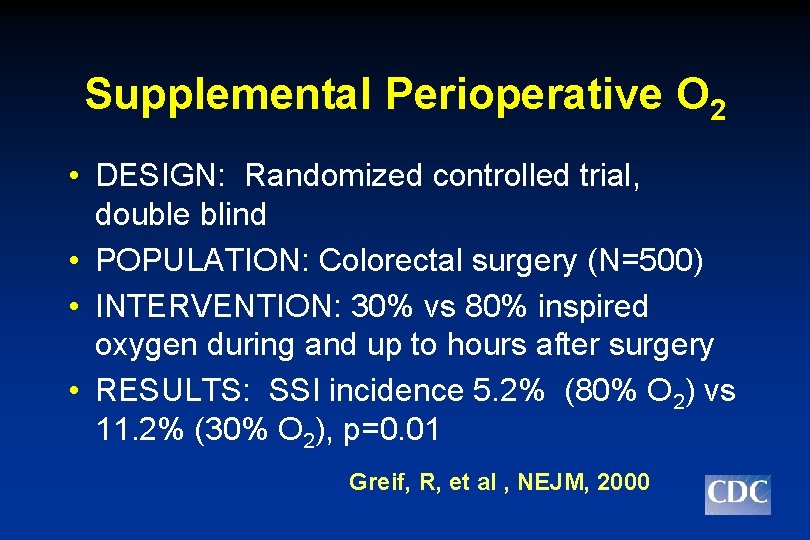
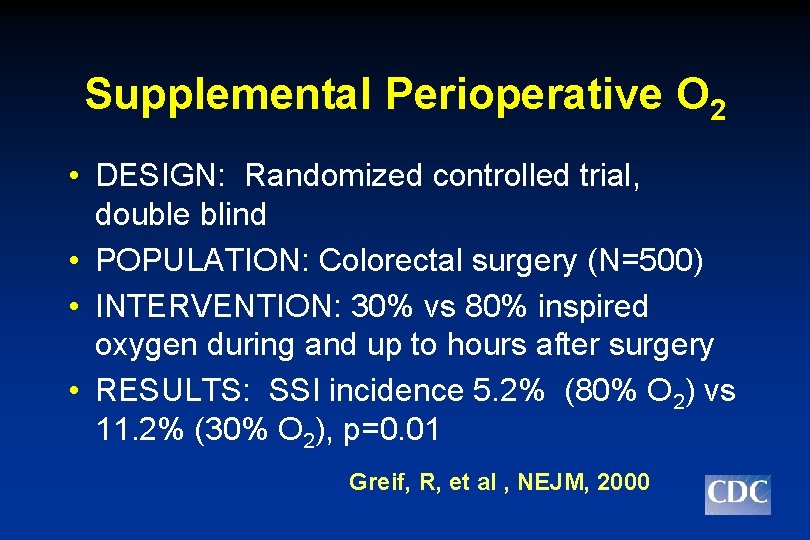
Supplemental Perioperative O 2 • DESIGN: Randomized controlled trial, double blind • POPULATION: Colorectal surgery (N=500) • INTERVENTION: 30% vs 80% inspired oxygen during and up to hours after surgery • RESULTS: SSI incidence 5. 2% (80% O 2) vs 11. 2% (30% O 2), p=0. 01 Greif, R, et al , NEJM, 2000
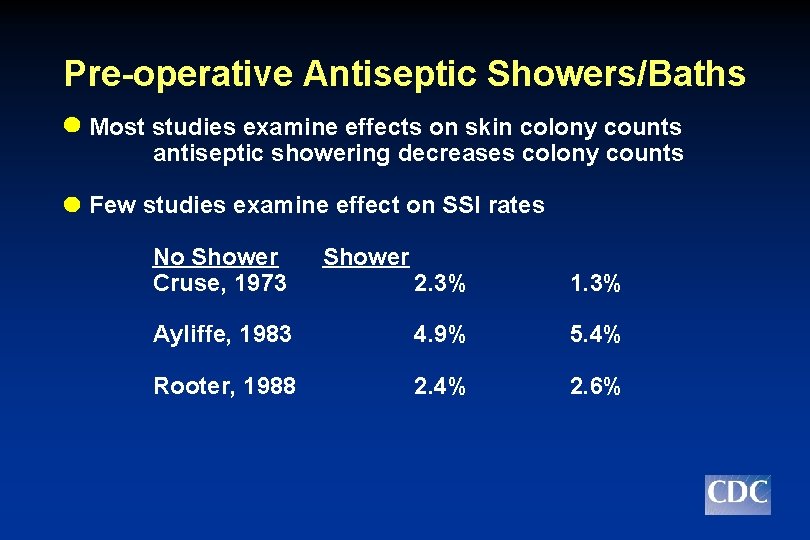
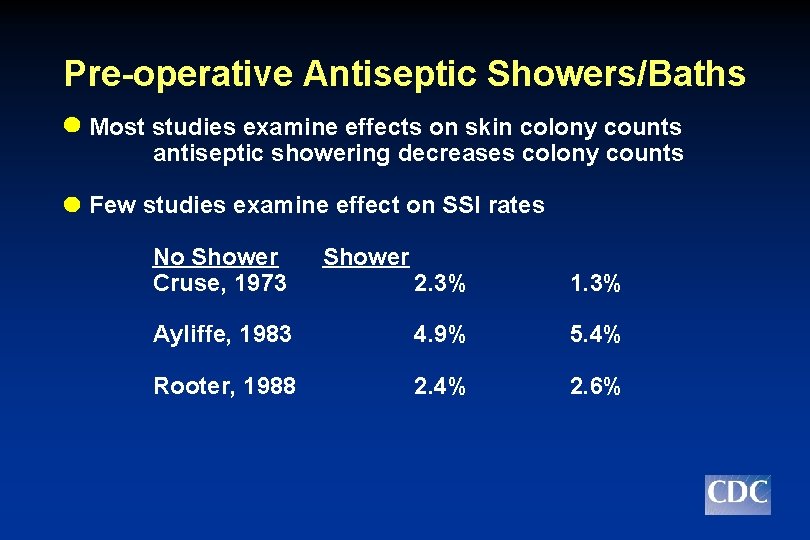
Pre-operative Antiseptic Showers/Baths Most studies examine effects on skin colony counts antiseptic showering decreases colony counts Few studies examine effect on SSI rates No Shower Cruse, 1973 Shower 2. 3% 1. 3% Ayliffe, 1983 4. 9% 5. 4% Rooter, 1988 2. 4% 2. 6%
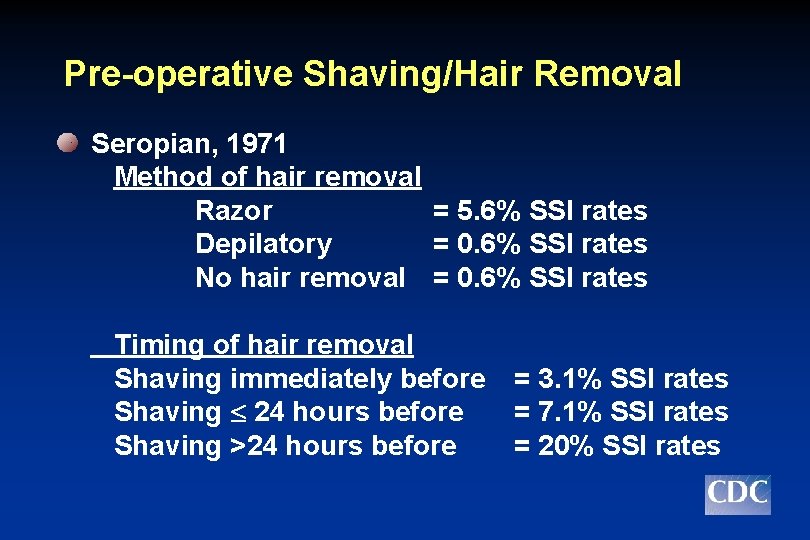
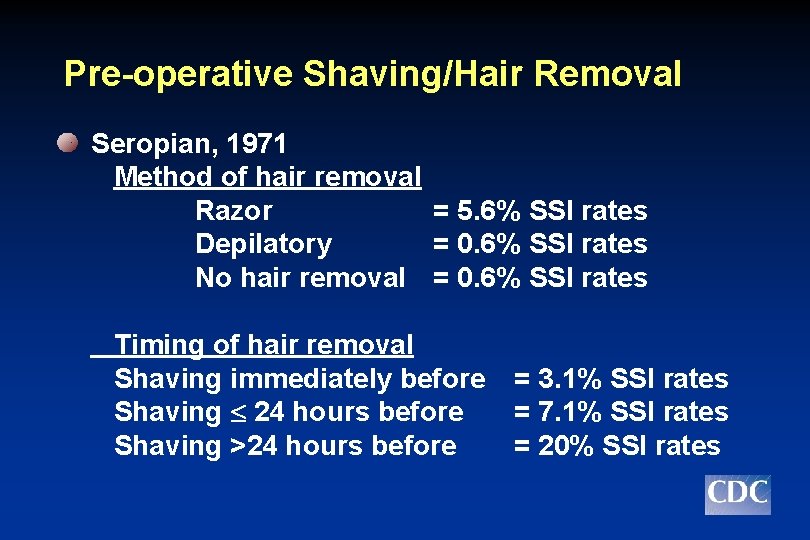
Pre-operative Shaving/Hair Removal Seropian, 1971 Method of hair removal Razor = 5. 6% SSI rates Depilatory = 0. 6% SSI rates No hair removal = 0. 6% SSI rates Timing of hair removal Shaving immediately before Shaving 24 hours before Shaving >24 hours before = 3. 1% SSI rates = 7. 1% SSI rates = 20% SSI rates
Pre-operative Shaving/Hair Removal Multiple studies show - Clipping immediately before operation associated with lower SSI risk than shaving or clipping the night before operation CENTERS FOR DISEASE CONTROL AND PREVENTION
Surgical Attire • Scrub suits • Cap/hoods • Shoe covers • Masks • Gloves • Gowns
Surgical Technique • • • Removing devitalized tissue Maintaining effective hemostasis Gently handling tissues Eradicating dead space Avoiding inadvertent entries into a viscus Using drains and suture material appropriately
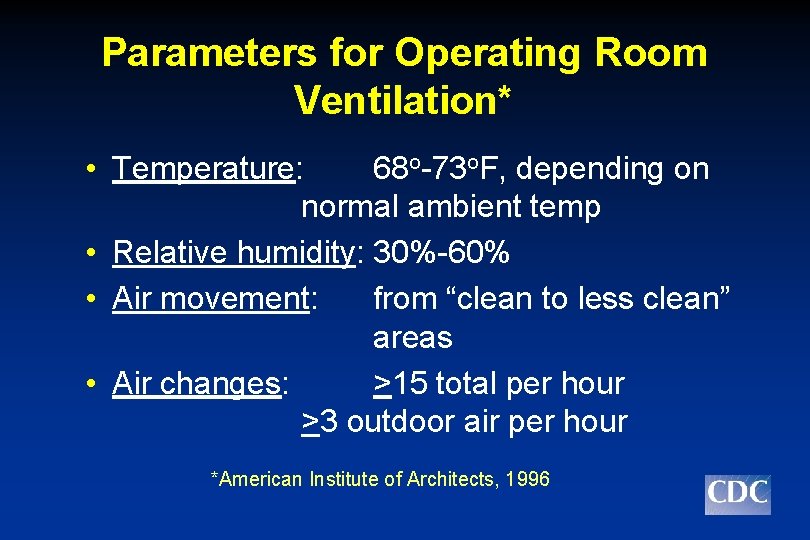
Parameters for Operating Room Ventilation* • Temperature: 68 o-73 o. F, depending on normal ambient temp • Relative humidity: 30%-60% • Air movement: from “clean to less clean” areas • Air changes: >15 total per hour >3 outdoor air per hour *American Institute of Architects, 1996
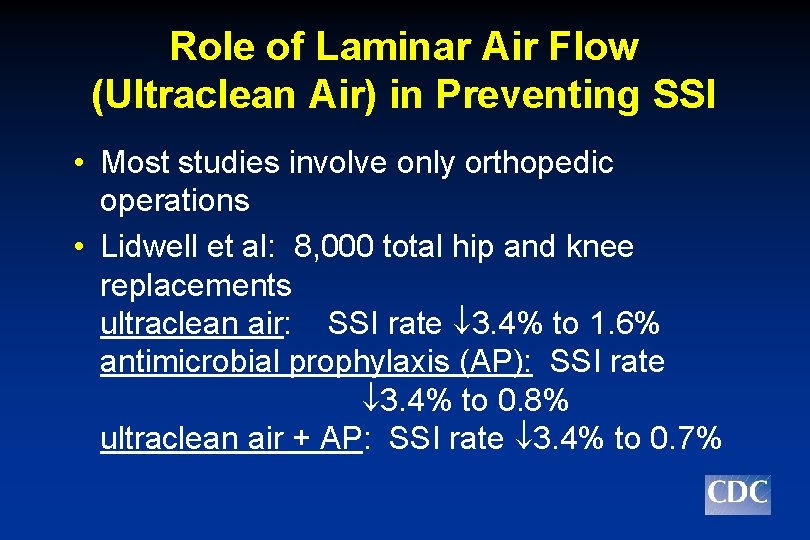
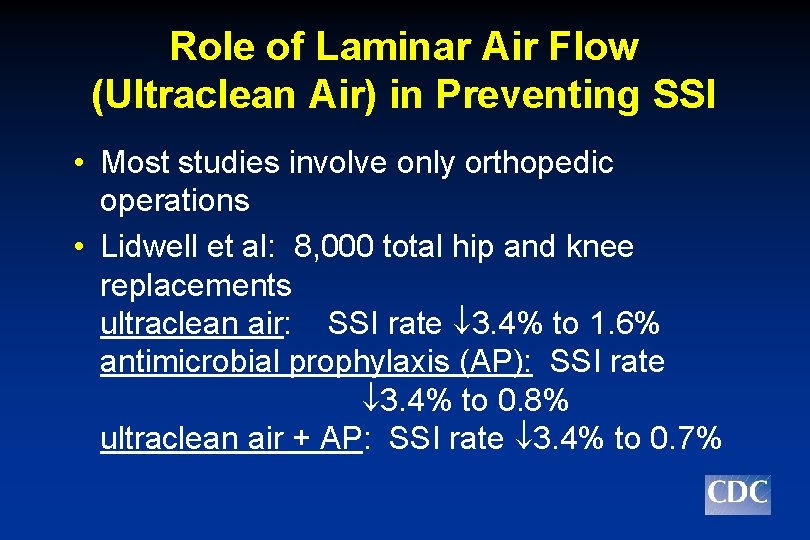
Role of Laminar Air Flow (Ultraclean Air) in Preventing SSI • Most studies involve only orthopedic operations • Lidwell et al: 8, 000 total hip and knee replacements ultraclean air: SSI rate 3. 4% to 1. 6% antimicrobial prophylaxis (AP): SSI rate 3. 4% to 0. 8% ultraclean air + AP: SSI rate 3. 4% to 0. 7%
Status of SSI Surveillance
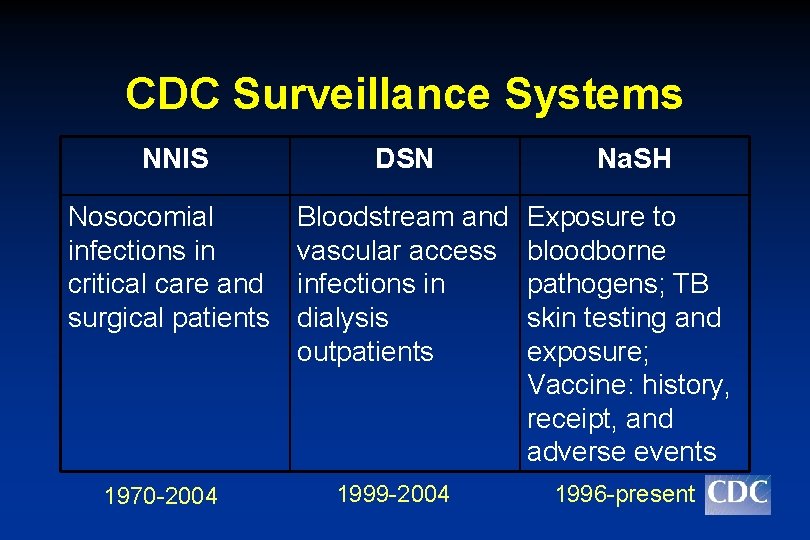
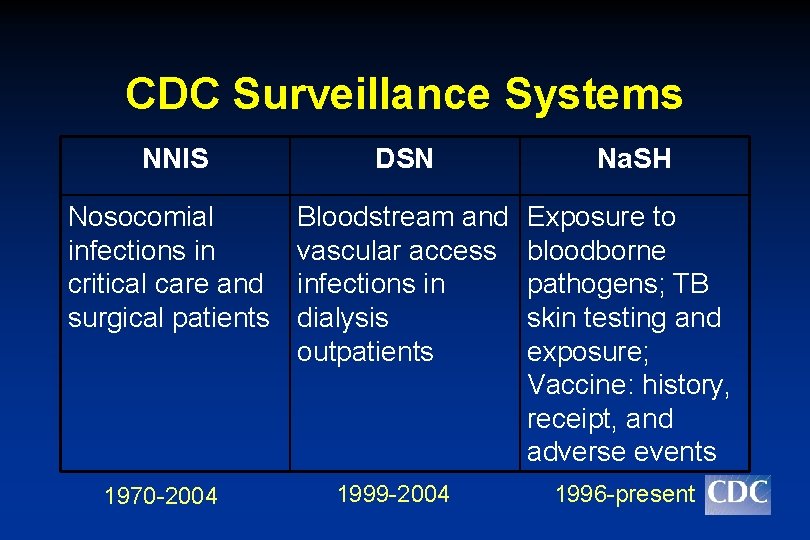
CDC Surveillance Systems NNIS DSN Na. SH Nosocomial infections in critical care and surgical patients Bloodstream and vascular access infections in dialysis outpatients Exposure to bloodborne pathogens; TB skin testing and exposure; Vaccine: history, receipt, and adverse events 1970 -2004 1999 -2004 1996 -present
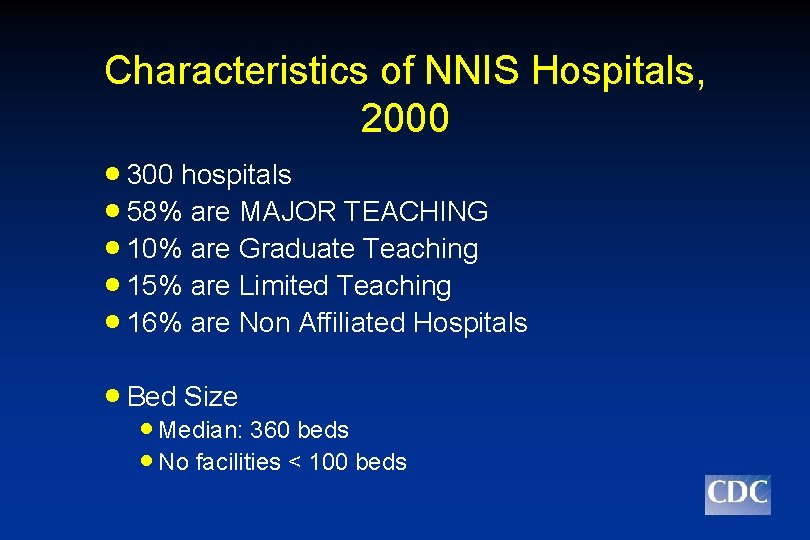
Characteristics of NNIS Hospitals, 2000 · 300 hospitals · 58% are MAJOR TEACHING · 10% are Graduate Teaching · 15% are Limited Teaching · 16% are Non Affiliated Hospitals · Bed Size · Median: 360 beds · No facilities < 100 beds
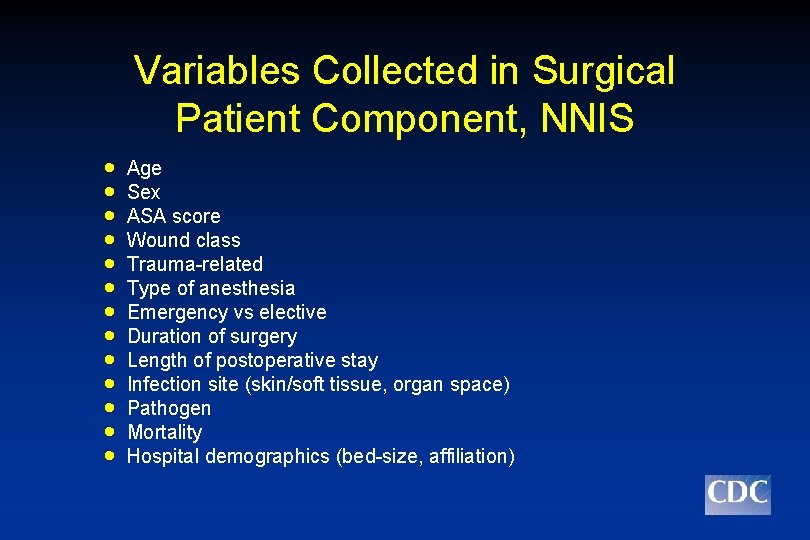
Variables Collected in Surgical Patient Component, NNIS · · · · Age Sex ASA score Wound class Trauma-related Type of anesthesia Emergency vs elective Duration of surgery Length of postoperative stay Infection site (skin/soft tissue, organ space) Pathogen Mortality Hospital demographics (bed-size, affiliation)
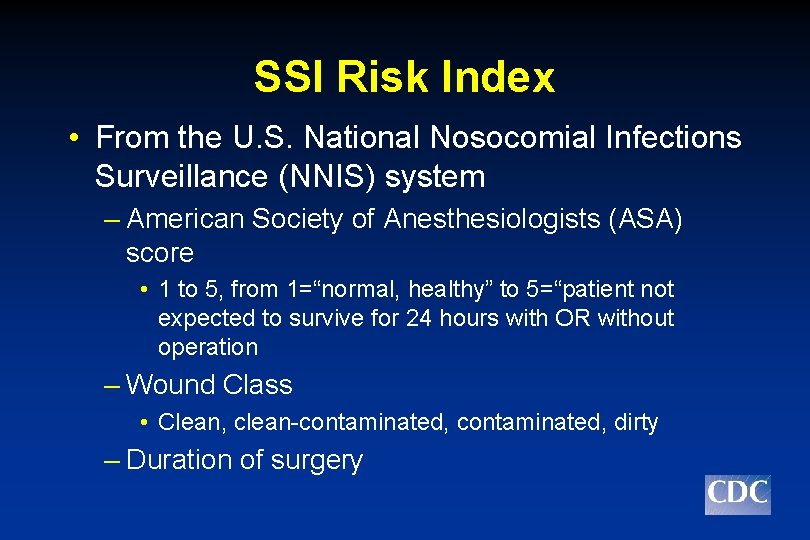
SSI Risk Index • From the U. S. National Nosocomial Infections Surveillance (NNIS) system – American Society of Anesthesiologists (ASA) score • 1 to 5, from 1=“normal, healthy” to 5=“patient not expected to survive for 24 hours with OR without operation – Wound Class • Clean, clean-contaminated, dirty – Duration of surgery
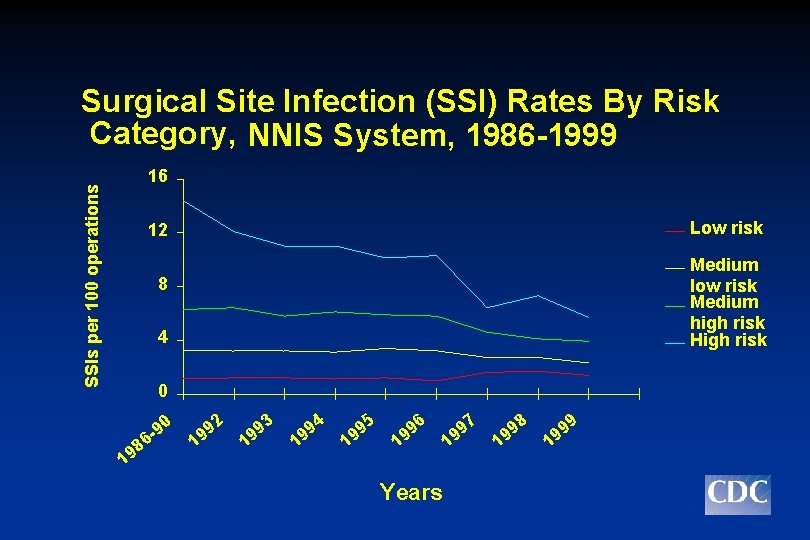
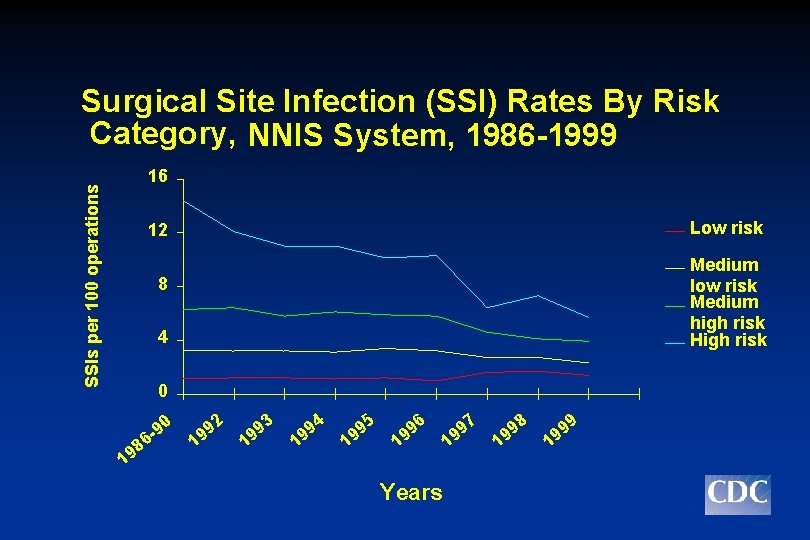
Surgical Site Infection (SSI) Rates By Risk Category, NNIS System, 1986 -1999 SSIs per 100 operations 16 Low risk 12 Medium low risk Medium high risk High risk 8 4 0 19 8 90 6 2 9 9 1 93 9 1 94 9 1 95 9 1 96 9 1 Years 97 9 1 8 9 9 1 9 9 9 1
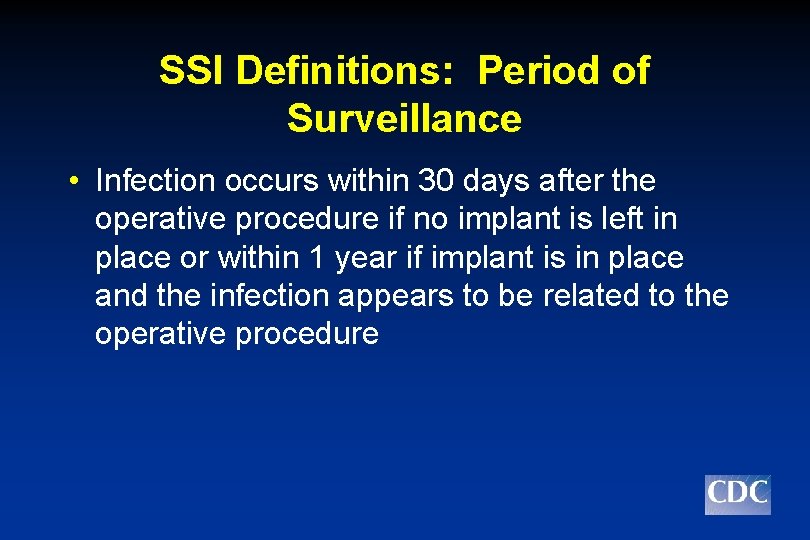
SSI Definitions: Period of Surveillance • Infection occurs within 30 days after the operative procedure if no implant is left in place or within 1 year if implant is in place and the infection appears to be related to the operative procedure
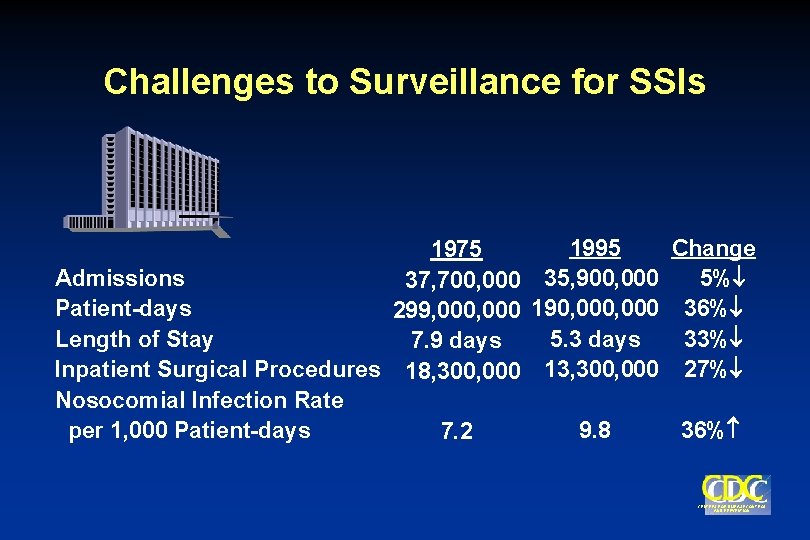
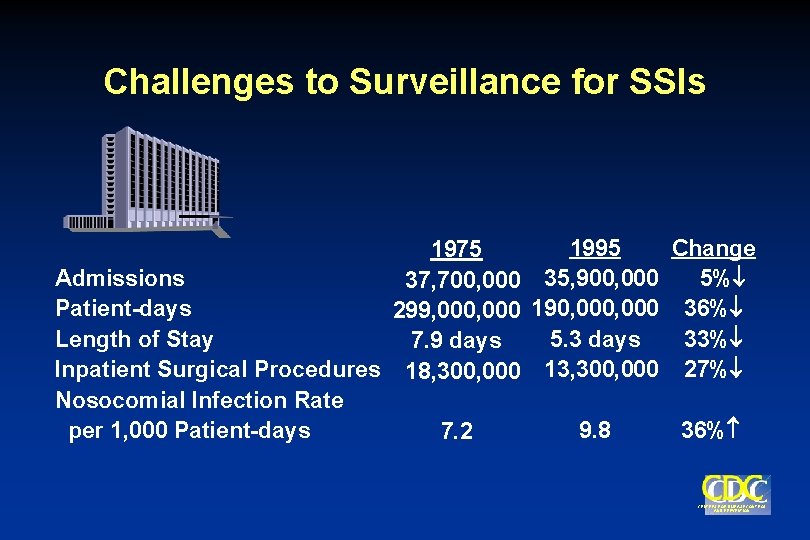
Challenges to Surveillance for SSIs 1995 Change 1975 Admissions 5% 37, 700, 000 35, 900, 000 Patient-days 299, 000 190, 000 36% Length of Stay 5. 3 days 33% 7. 9 days Inpatient Surgical Procedures 18, 300, 000 13, 300, 000 27% Nosocomial Infection Rate per 1, 000 Patient-days 9. 8 36% 7. 2 CENTERS FOR DISEASE CONTROL AND PREVENTION
What Is NHSN? Integration of CDC’s three patient and healthcare personnel surveillance systems NNIS Na. SH DSN
NHSN Premises • Maintain the goals of predecessor systems • Minimize data collection and manual data entry burden – Streamline existing surveillance protocols – Increase capacity for capturing electronic data (e. g. , Laboratory information systems, operating room, pharmacy, clinical, administrative databases) • Extensible web-based application
Priority Areas for NHSN Development • Inclusion of process measures linked to outcomes – Surgical prophylaxis – Central line insertion practices • Completion of HCP Safety Component – Na. SH NHSN • Influenza pilot: vaccine coverage and use of antiviral medications

How do we develop policy?
Healthcare Infection Control Practices Advisory Committee (HICPAC)
Healthcare Infection Control Practices Advisory Committee MISSION • Advise the US Secretary of Health and the Director of CDC regarding the practice of infection control and strategies for surveillance, prevention and control of antimicrobial resistance, and related adverse events in healthcare settings
CDC/HICPAC GUIDELINE SCOPE • TARGET AUDIENCE: • clinicians • infection control professionals • public health officials • regulators • TARGET SETTINGS: • Inpatient • Outpatient • Home care • Long term care
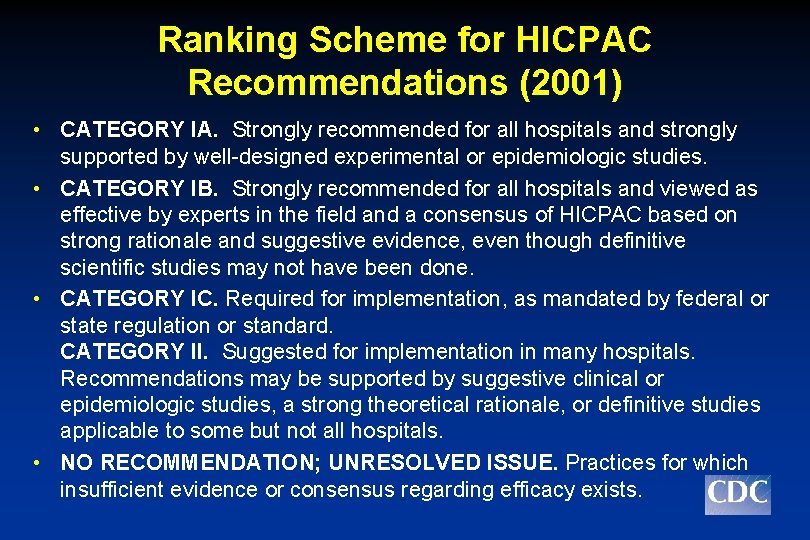
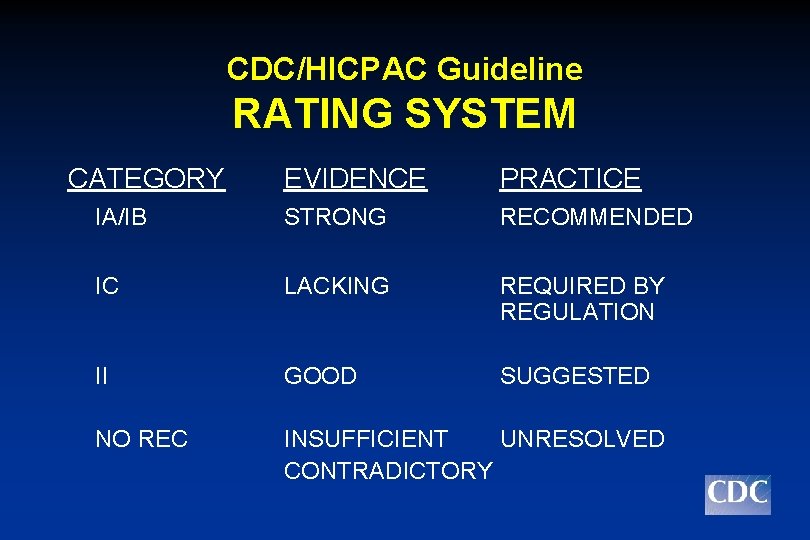
Ranking Scheme for HICPAC Recommendations (2001) • CATEGORY IA. Strongly recommended for all hospitals and strongly supported by well-designed experimental or epidemiologic studies. • CATEGORY IB. Strongly recommended for all hospitals and viewed as effective by experts in the field and a consensus of HICPAC based on strong rationale and suggestive evidence, even though definitive scientific studies may not have been done. • CATEGORY IC. Required for implementation, as mandated by federal or state regulation or standard. CATEGORY II. Suggested for implementation in many hospitals. Recommendations may be supported by suggestive clinical or epidemiologic studies, a strong theoretical rationale, or definitive studies applicable to some but not all hospitals. • NO RECOMMENDATION; UNRESOLVED ISSUE. Practices for which insufficient evidence or consensus regarding efficacy exists.
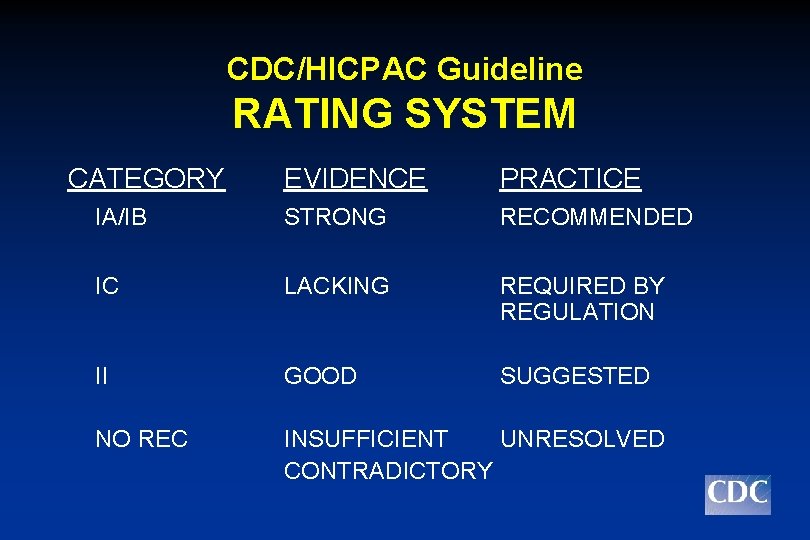
CDC/HICPAC Guideline RATING SYSTEM CATEGORY EVIDENCE PRACTICE IA/IB STRONG RECOMMENDED IC LACKING REQUIRED BY REGULATION II GOOD SUGGESTED NO REC INSUFFICIENT UNRESOLVED CONTRADICTORY
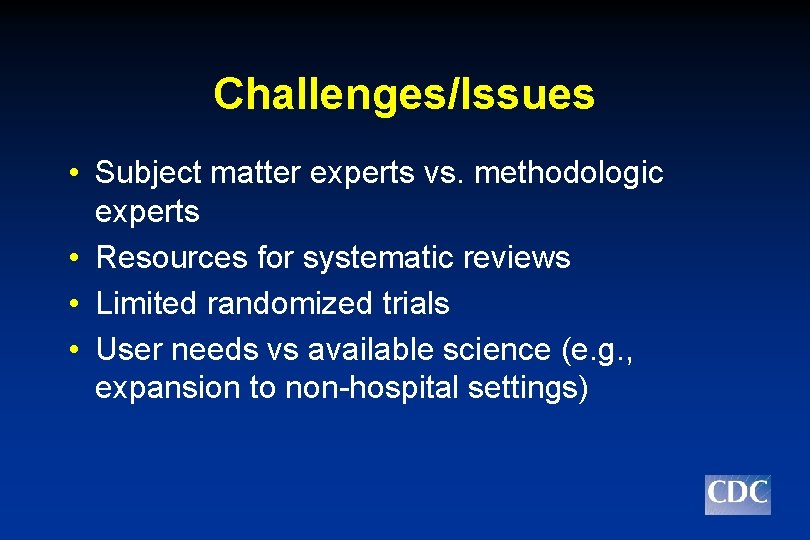
Challenges/Issues • Subject matter experts vs. methodologic experts • Resources for systematic reviews • Limited randomized trials • User needs vs available science (e. g. , expansion to non-hospital settings)
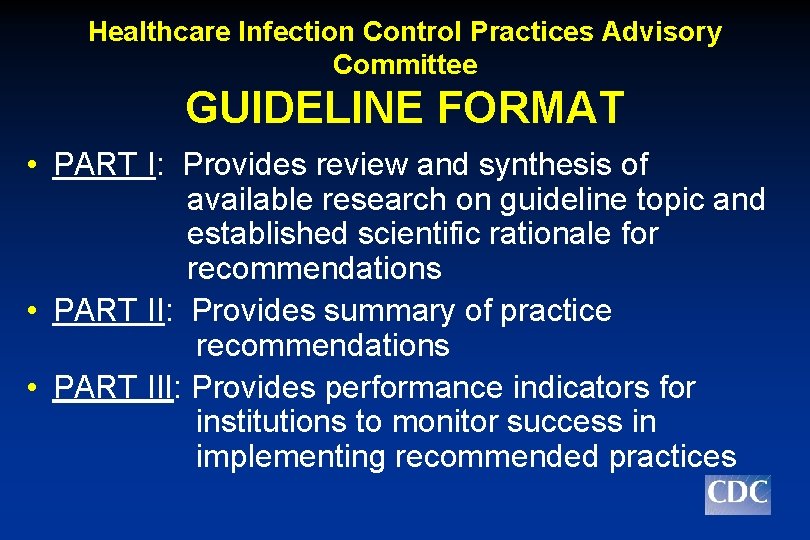
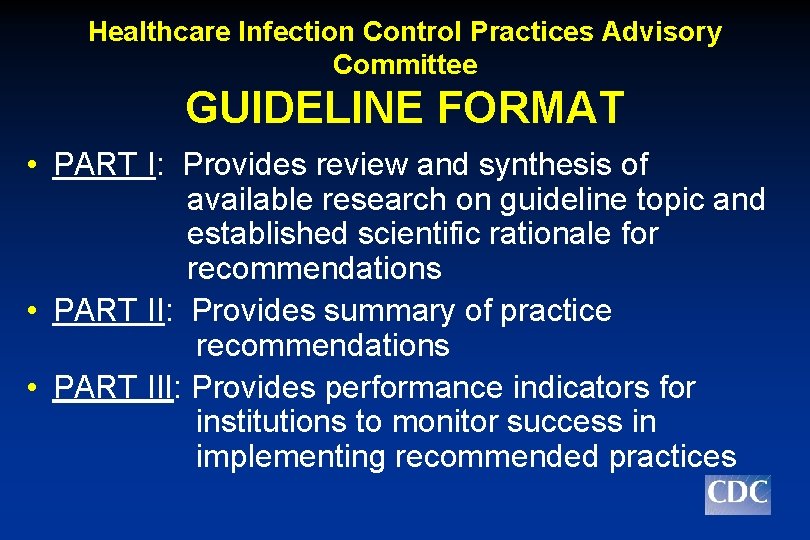
Healthcare Infection Control Practices Advisory Committee GUIDELINE FORMAT • PART I: Provides review and synthesis of available research on guideline topic and established scientific rationale for recommendations • PART II: Provides summary of practice recommendations • PART III: Provides performance indicators for institutions to monitor success in implementing recommended practices
Summary • Prevention of SSI require a multifaceted approach targeting pre-, intra-, and postoperative factors • Current surveillance systems do collect data on perioperative processes • Increasing shift of surgical procedures to outpatient settings and decrease in postoperative length of stay complicate surveillance efforts • Incidence is generally low; so studies would require large sample size • Some prevention practices (e. g. hand hygiene) would be difficult to study using traditional randomized controlled trial research design

PREVENTION IS PRIMARY! Protect patients…protect healthcare personnel… promote quality healthcare! Division of Healthcare Quality Promotion
To obtain HICPAC guidelines visit the Division of Healthcare Quality Promotion (DHQP) website http: //www. cdc. gov/ncidod/hip/default. htm