Preventing Suicides in Hackney Update for GPs Dr
- Slides: 35
Preventing Suicides in Hackney Update for GPs Dr Nicole Klynman, Consultant in Public Health and Dr Morminah Nisa, GP trainee in Public Health
Introduction • Globally suicide leads to over 800, 000 deaths per year • It is the second largest cause of deaths in young people ages 15 -29 years • Economic cost of £ 1. 67 million per death by suicide • Within UK, suicide has significant gender and social inequalities • Suicides are not inevitable, and so each death may be prevented • ‘Five Year Forward View for Mental Health’ set out an aim to reduce suicides in England by 10% by 2020
Latest Suicide Statistics for Great Britain • There were 5, 668 deaths by suicide and undetermined injury • The rate of suicide for Great Britain is 10. 1 per 100, 000 and in London is 7. 8 per 100, 000 people • From 2007 the rate of suicide increased each year until a peak of 11. 1 per 100, 000 in 2013 • After 2013 this is the third consecutive year that suicide rate has decreased • Approximately 75% suicides were in men • The commonest age group for suicide was 40 -44 years for men and 50 -54 years for women • The commonest method of suicide is by hanging Source: ONS suicide data- September 2017
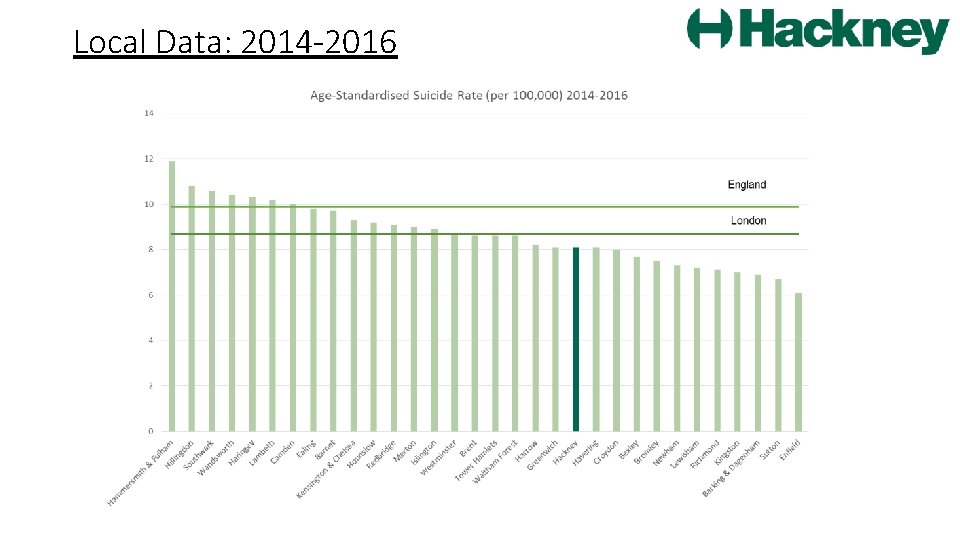
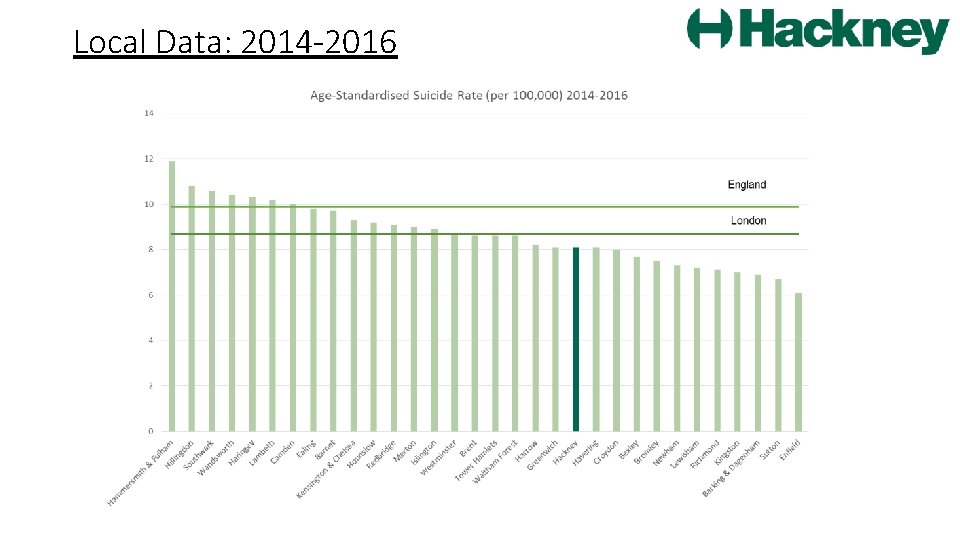
Local Data: 2014 -2016
• The age-standardised rate of suicide over a three year average (20142016) in Hackney is 8. 1 • The rate in London is 8. 7 and in England is 9. 9 • The rate of suicide for Hackney has decreased from 9. 2 in 2013 -2015 • The rate of suicide in London in 2013 -2015 was 8. 6, and England was 10. 1 Source: PHE Fingertips Tool, ONS data 2017
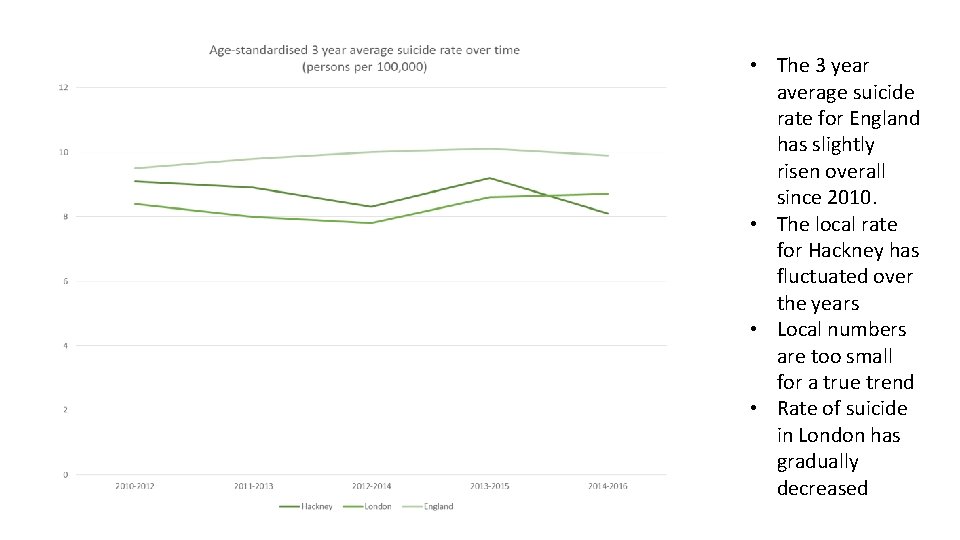
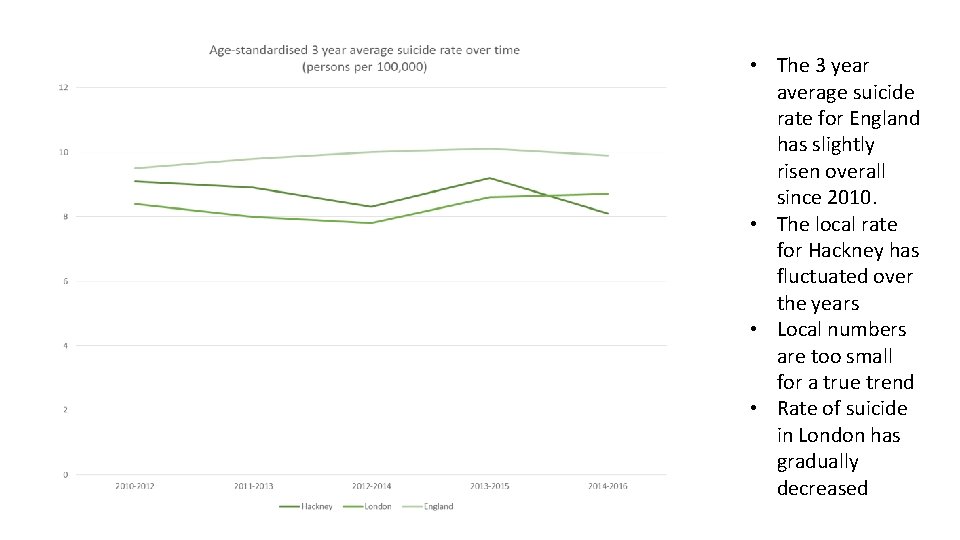
• The 3 year average suicide rate for England has slightly risen overall since 2010. • The local rate for Hackney has fluctuated over the years • Local numbers are too small for a true trend • Rate of suicide in London has gradually decreased
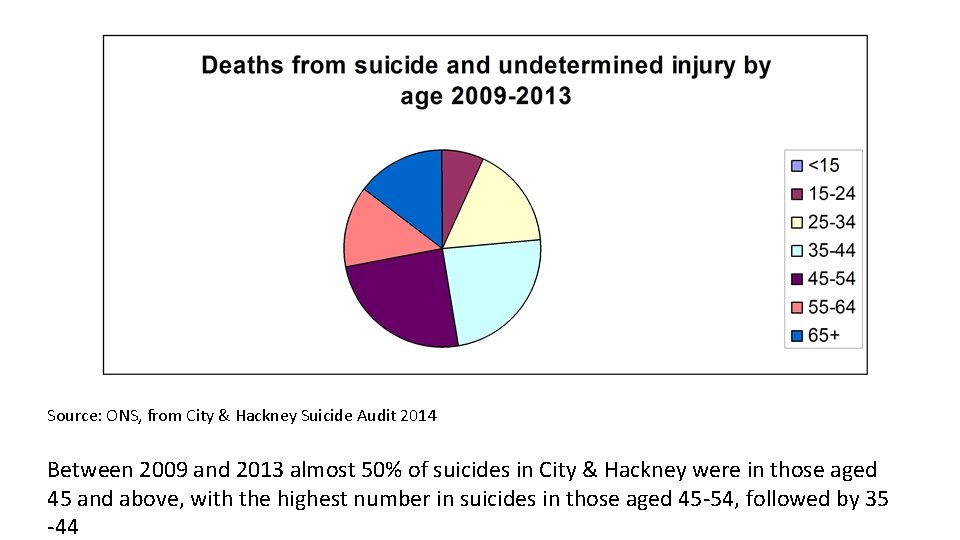
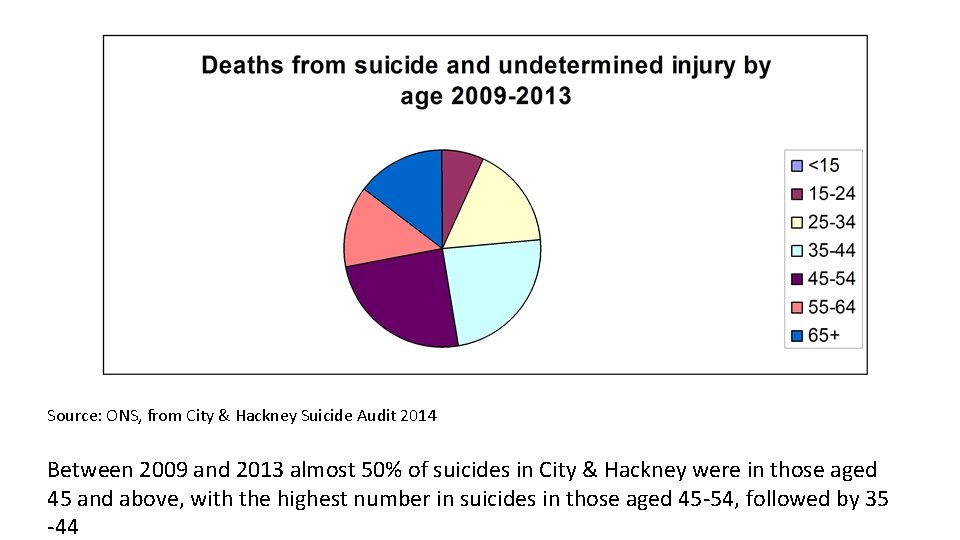
Source: ONS, from City & Hackney Suicide Audit 2014 Between 2009 and 2013 almost 50% of suicides in City & Hackney were in those aged 45 and above, with the highest number in suicides in those aged 45 -54, followed by 35 -44
• Between 2009 and 2013 77% of suicides in City of London and Hackney were in men; in keeping with national figures • Current data shows that for 2014 -2016, 64% of suicides were in males with a rise in female suicided from 23% to 36% but numbers are too small for true interpretation • The commonest method of suicide is by hanging, in keeping with the rest of England • 55% of cases who died by suicide in 2009 -2013 were born in the UK
Preventing Suicides in Hackney- Action Plan • In 2013, suicide prevention became a local authority-led initiative involving close collaboration with CCGs, the police, NHS England, coroners and the voluntary sector as part of a ‘suicide prevention group’ • An Action Plan has been built around key areas for action as described in the National Suicide Prevention Strategy (2012); tailored to address the need in Hackney guided by the City and Hackney Suicide Audit in 2014 • New audit is currently in progress to guide a refreshed Action Plan
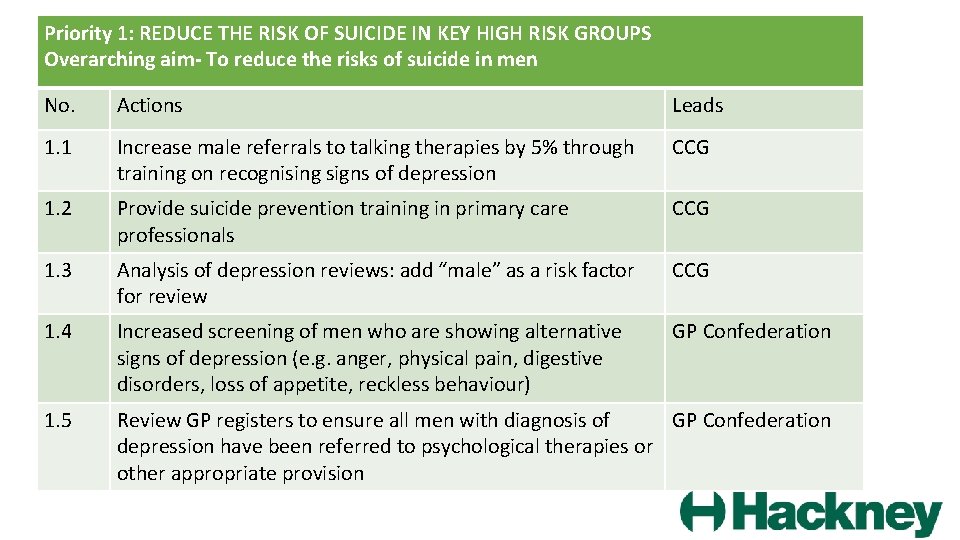
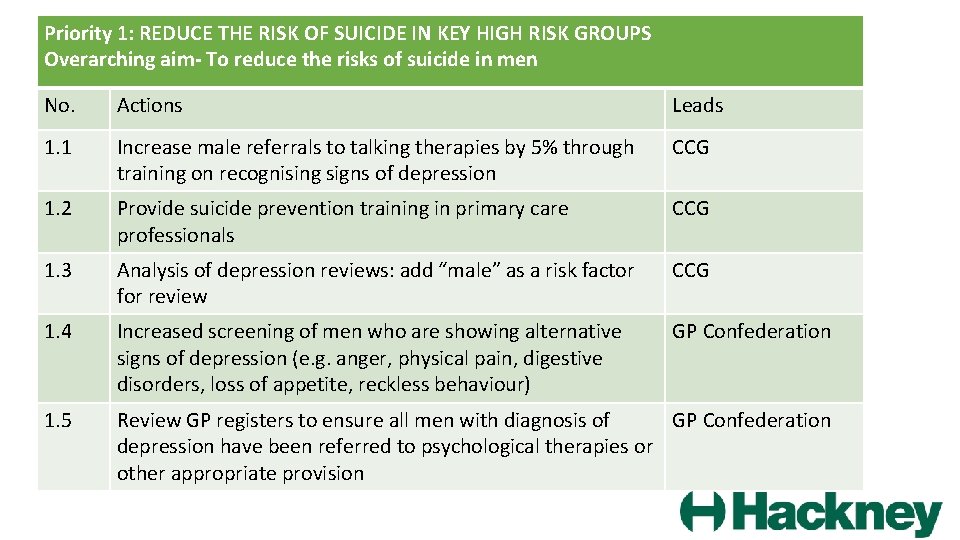
Priority 1: REDUCE THE RISK OF SUICIDE IN KEY HIGH RISK GROUPS Overarching aim- To reduce the risks of suicide in men No. Actions Leads 1. 1 Increase male referrals to talking therapies by 5% through training on recognising signs of depression CCG 1. 2 Provide suicide prevention training in primary care professionals CCG 1. 3 Analysis of depression reviews: add “male” as a risk factor for review CCG 1. 4 Increased screening of men who are showing alternative signs of depression (e. g. anger, physical pain, digestive disorders, loss of appetite, reckless behaviour) GP Confederation 1. 5 Review GP registers to ensure all men with diagnosis of GP Confederation depression have been referred to psychological therapies or other appropriate provision
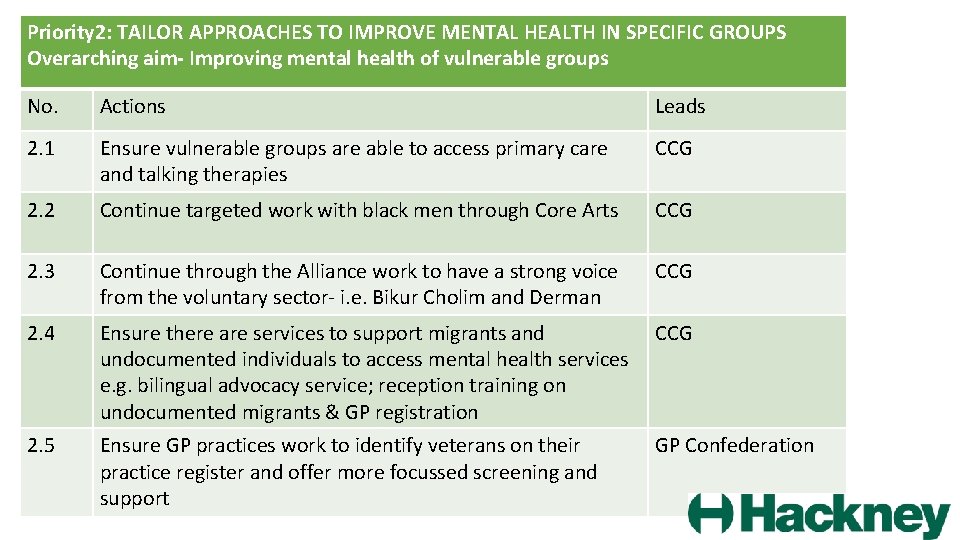
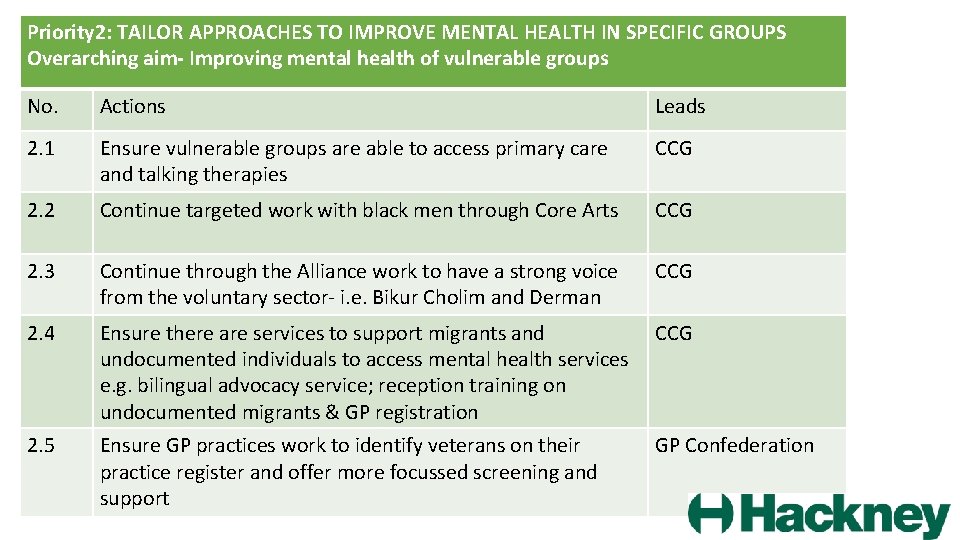
Priority 2: TAILOR APPROACHES TO IMPROVE MENTAL HEALTH IN SPECIFIC GROUPS Overarching aim- Improving mental health of vulnerable groups No. Actions Leads 2. 1 Ensure vulnerable groups are able to access primary care and talking therapies CCG 2. 2 Continue targeted work with black men through Core Arts CCG 2. 3 Continue through the Alliance work to have a strong voice from the voluntary sector- i. e. Bikur Cholim and Derman CCG 2. 4 Ensure there are services to support migrants and undocumented individuals to access mental health services e. g. bilingual advocacy service; reception training on undocumented migrants & GP registration CCG 2. 5 Ensure GP practices work to identify veterans on their practice register and offer more focussed screening and support GP Confederation
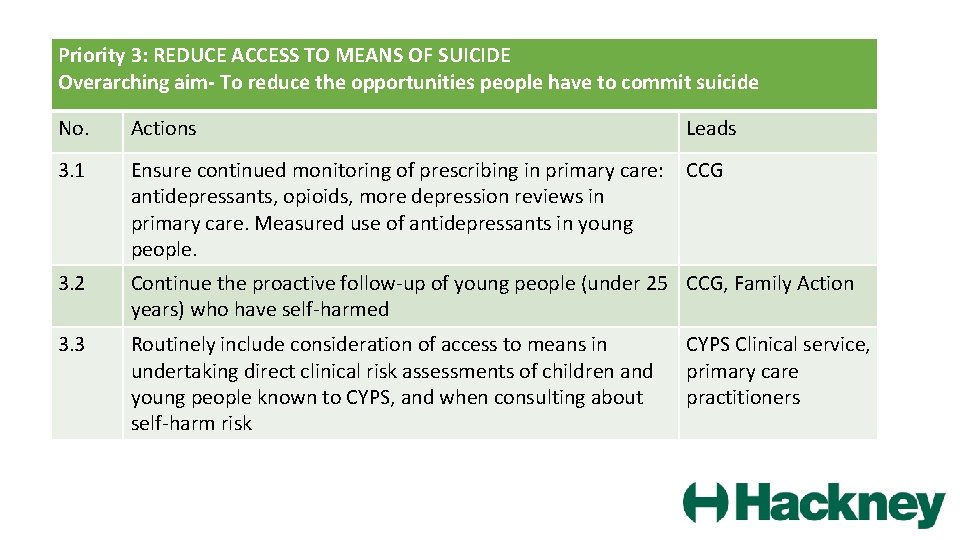
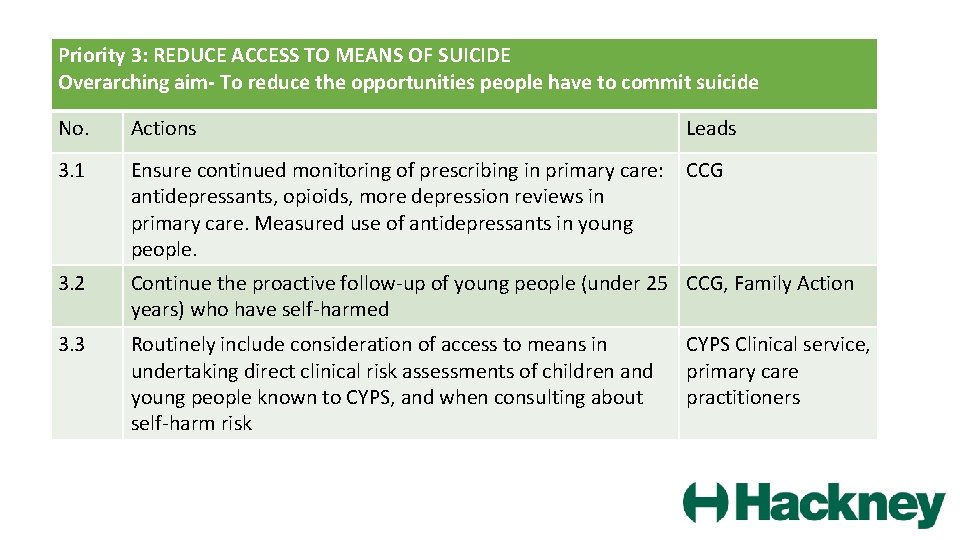
Priority 3: REDUCE ACCESS TO MEANS OF SUICIDE Overarching aim- To reduce the opportunities people have to commit suicide No. Actions Leads 3. 1 Ensure continued monitoring of prescribing in primary care: CCG antidepressants, opioids, more depression reviews in primary care. Measured use of antidepressants in young people. 3. 2 Continue the proactive follow-up of young people (under 25 CCG, Family Action years) who have self-harmed 3. 3 Routinely include consideration of access to means in undertaking direct clinical risk assessments of children and young people known to CYPS, and when consulting about self-harm risk CYPS Clinical service, primary care practitioners
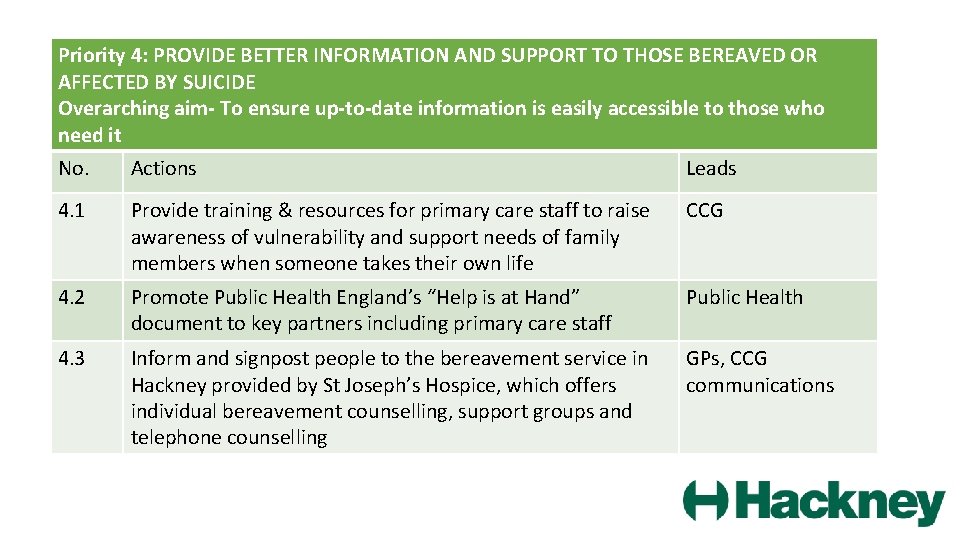
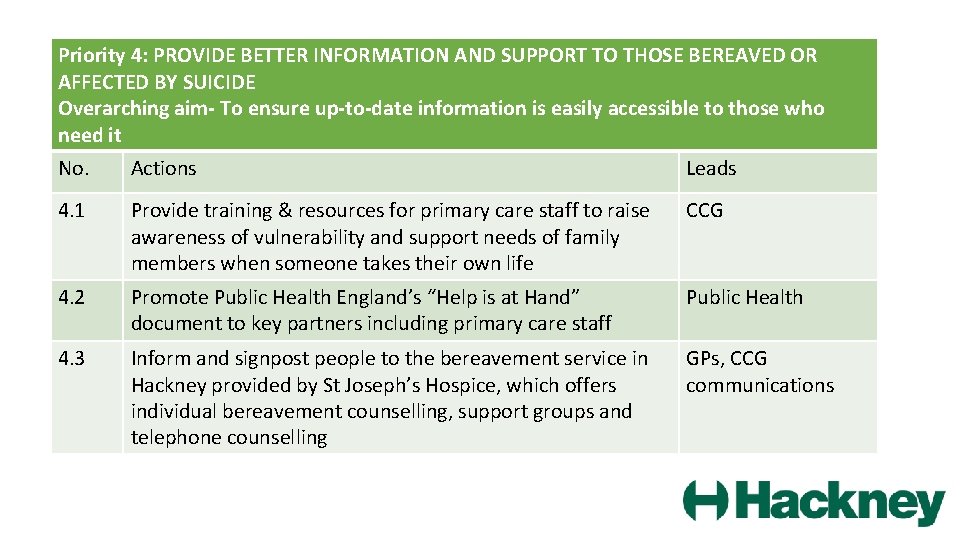
Priority 4: PROVIDE BETTER INFORMATION AND SUPPORT TO THOSE BEREAVED OR AFFECTED BY SUICIDE Overarching aim- To ensure up-to-date information is easily accessible to those who need it No. Actions Leads 4. 1 Provide training & resources for primary care staff to raise awareness of vulnerability and support needs of family members when someone takes their own life CCG 4. 2 Promote Public Health England’s “Help is at Hand” document to key partners including primary care staff Public Health 4. 3 Inform and signpost people to the bereavement service in Hackney provided by St Joseph’s Hospice, which offers individual bereavement counselling, support groups and telephone counselling GPs, CCG communications
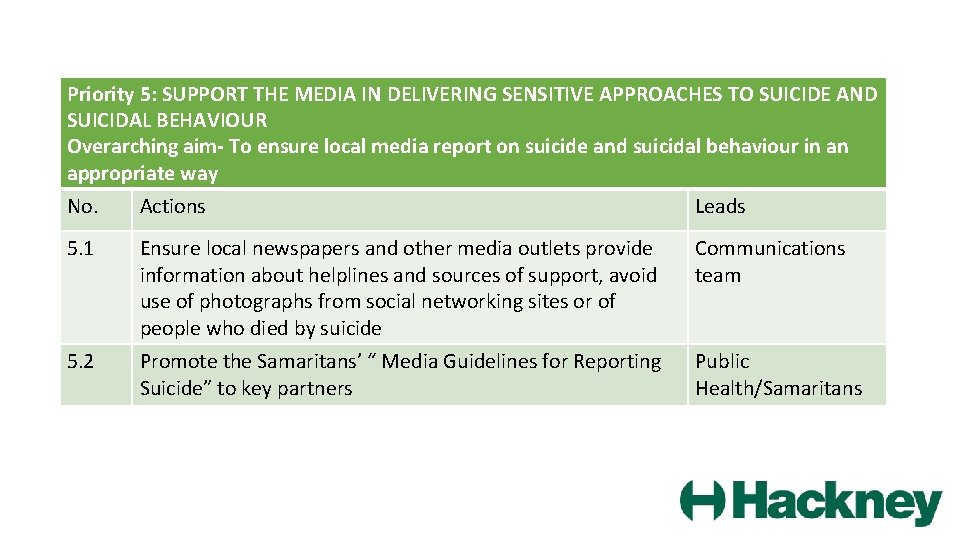
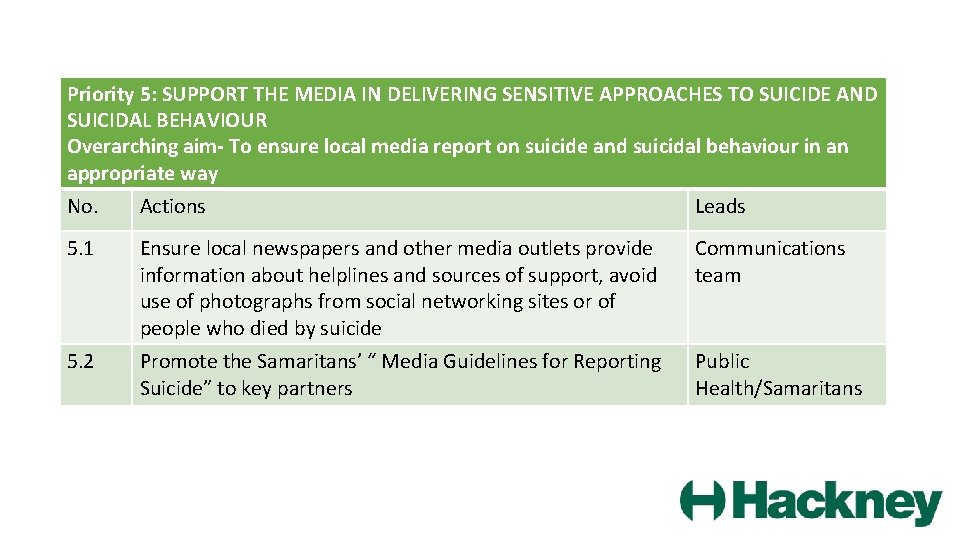
Priority 5: SUPPORT THE MEDIA IN DELIVERING SENSITIVE APPROACHES TO SUICIDE AND SUICIDAL BEHAVIOUR Overarching aim- To ensure local media report on suicide and suicidal behaviour in an appropriate way No. Actions Leads 5. 1 Ensure local newspapers and other media outlets provide information about helplines and sources of support, avoid use of photographs from social networking sites or of people who died by suicide Communications team 5. 2 Promote the Samaritans’ “ Media Guidelines for Reporting Suicide” to key partners Public Health/Samaritans
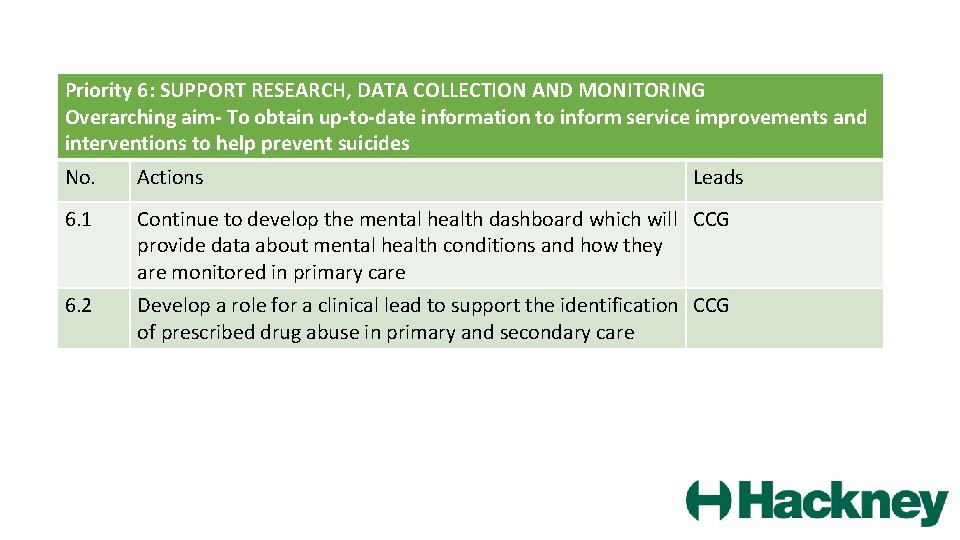
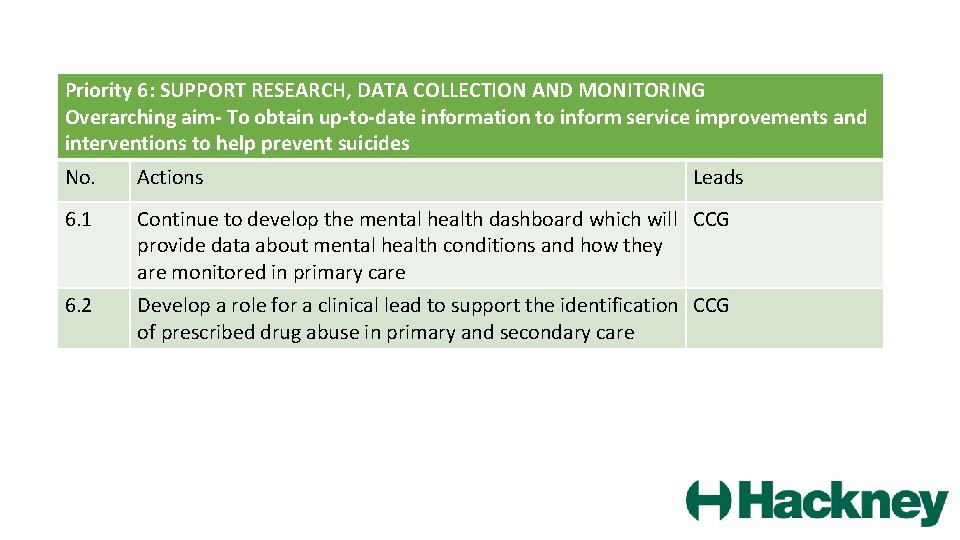
Priority 6: SUPPORT RESEARCH, DATA COLLECTION AND MONITORING Overarching aim- To obtain up-to-date information to inform service improvements and interventions to help prevent suicides No. Actions Leads 6. 1 Continue to develop the mental health dashboard which will CCG provide data about mental health conditions and how they are monitored in primary care 6. 2 Develop a role for a clinical lead to support the identification CCG of prescribed drug abuse in primary and secondary care
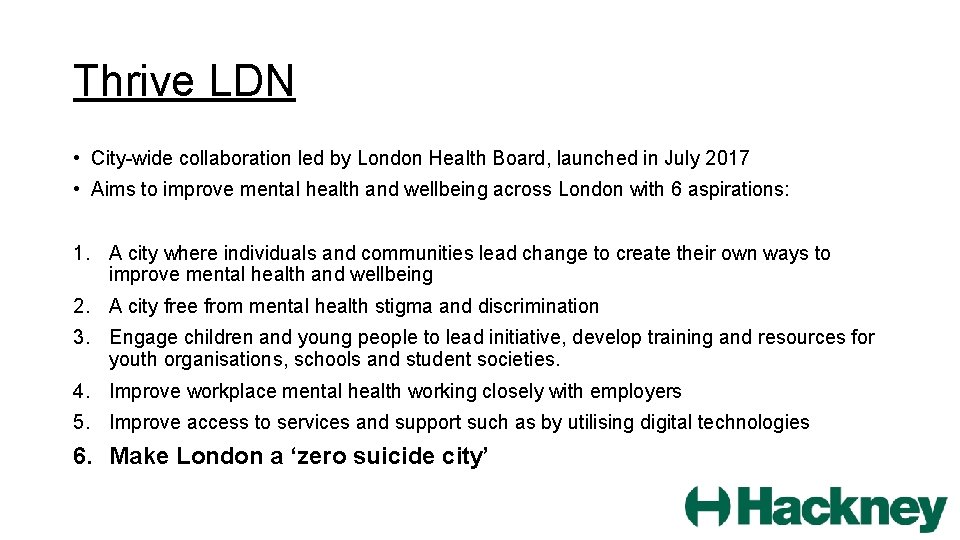
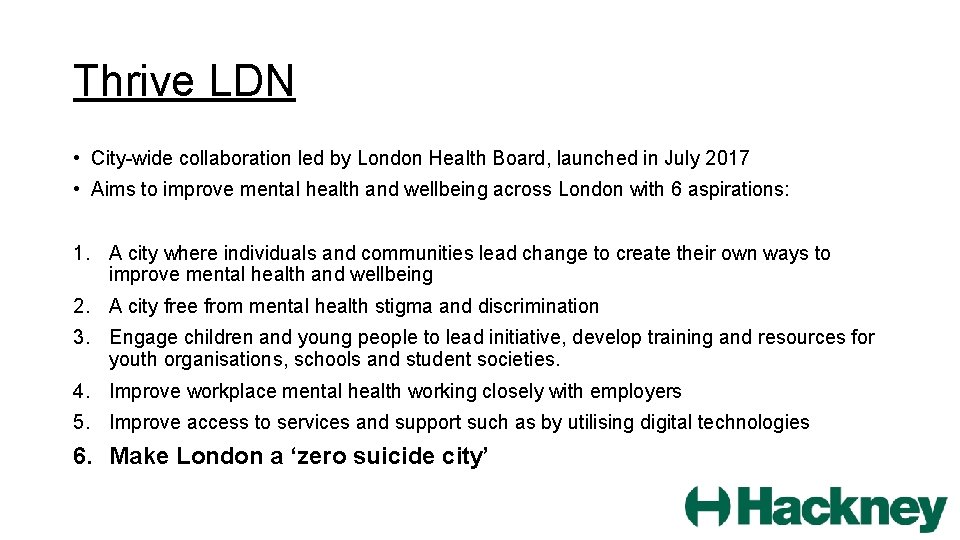
Thrive LDN • City-wide collaboration led by London Health Board, launched in July 2017 • Aims to improve mental health and wellbeing across London with 6 aspirations: 1. A city where individuals and communities lead change to create their own ways to improve mental health and wellbeing 2. A city free from mental health stigma and discrimination 3. Engage children and young people to lead initiative, develop training and resources for youth organisations, schools and student societies. 4. Improve workplace mental health working closely with employers 5. Improve access to services and support such as by utilising digital technologies 6. Make London a ‘zero suicide city’
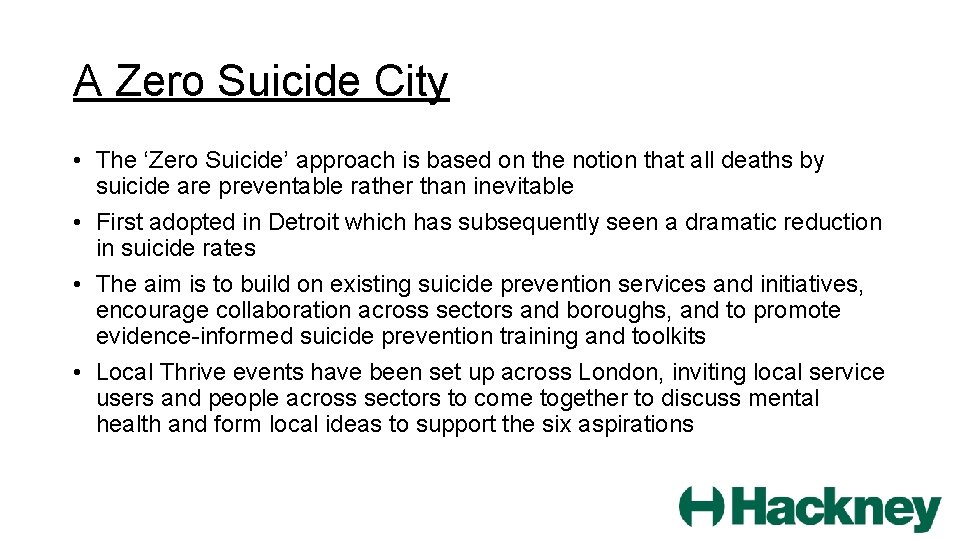
A Zero Suicide City • The ‘Zero Suicide’ approach is based on the notion that all deaths by suicide are preventable rather than inevitable • First adopted in Detroit which has subsequently seen a dramatic reduction in suicide rates • The aim is to build on existing suicide prevention services and initiatives, encourage collaboration across sectors and boroughs, and to promote evidence-informed suicide prevention training and toolkits • Local Thrive events have been set up across London, inviting local service users and people across sectors to come together to discuss mental health and form local ideas to support the six aspirations
Further Recommendations for Hackney - Based on National policies, guidance and evidence • Self-harm is the biggest risk factor for suicide and so should be addressed as a separate key area of focus in suicide prevention action plans • School-based interventions such as youth mental health awareness programmes have been shown to be effective in reducing suicide risk • Self-harm awareness training for all in contact with children, including GP staff • Consider LGBT group as an at-risk group of suicide and have low threshold for depression treatment, ensuring suicide risk is assessed • Multi-agency care plans for those who misuse drugs and alcohol, with inclusion of a crisis plan and assessment of suicide risk
Recommendations for Hackney (II) • Consider continuous collection of suicide data and regular compilation of self-harm data • Consider the use of real-time surveillance whereby the coroner’s office or police alert and inform public health of a suspected suicide and bereavement services are provided at the time
Unexpected Deaths Review DMT AUGUST 2017 DR SALLY DALY & ANDREW HOROBIN
Scope of Review Unexplained deaths over a 12 month period Patients known to ELFT June 2016 – June 2017 Focus on deaths by suicide
21 unexpected deaths SIR reports on 15 , Datix / 48 hr reports on 6 11 confirmed suicide 1 “ narrative verdict” – fall from height in context of acute psychotic episode
3 deaths as a consequence of established drug/alcohol dependency- likely accidental 5 natural causes (as a result of physical illness) 1 cause of death unknown – likely physical cause on review of notes
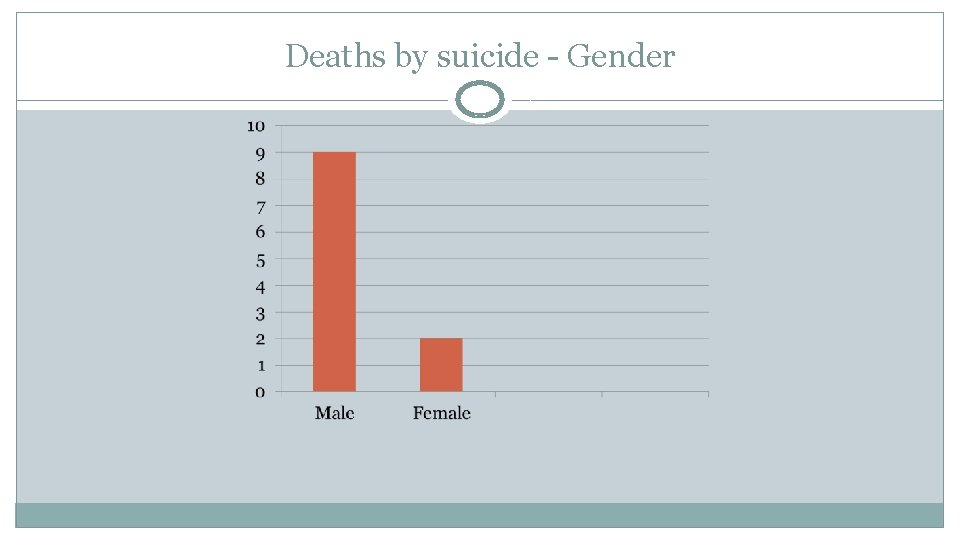
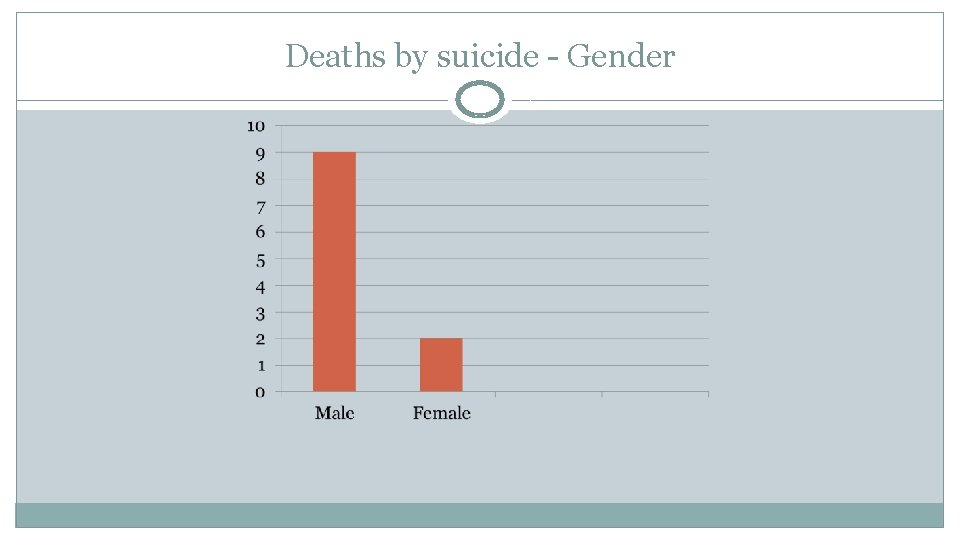
Deaths by suicide - Gender
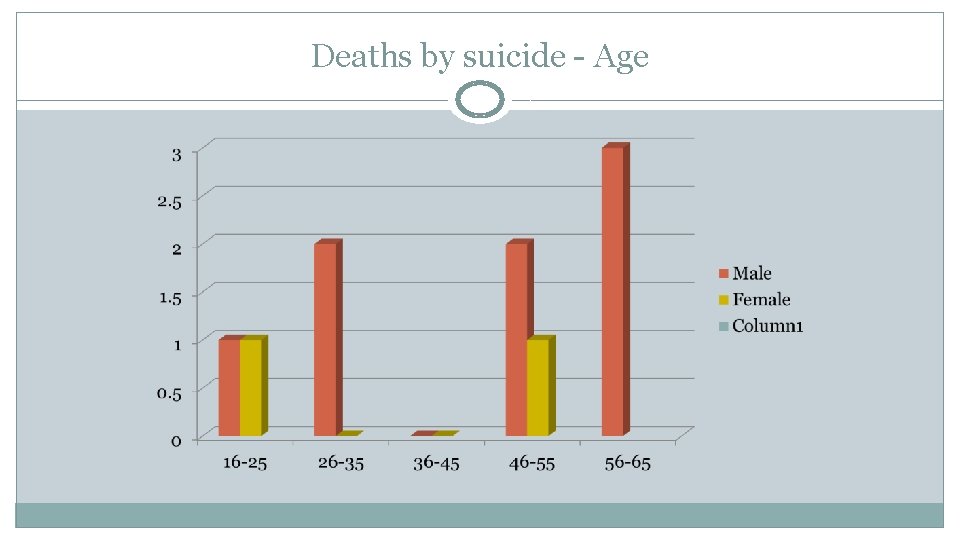
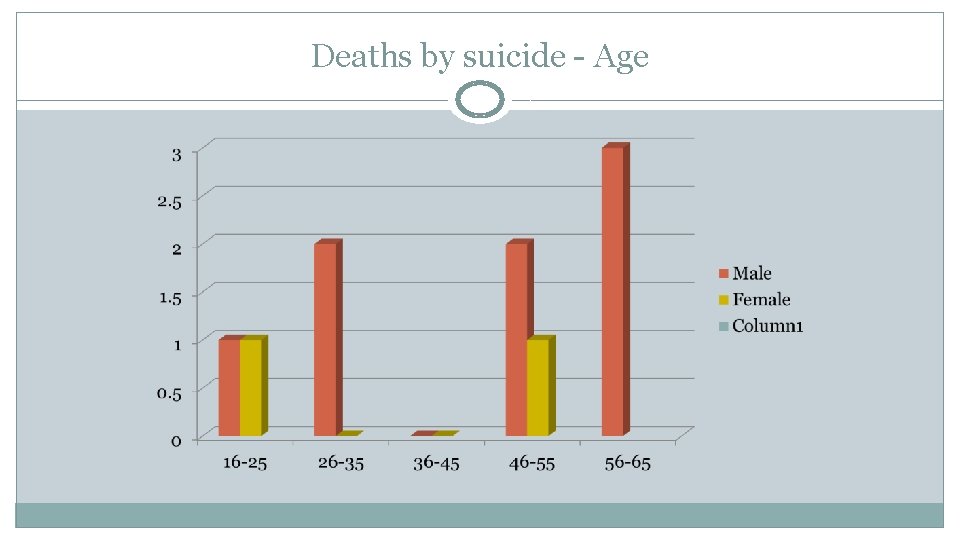
Deaths by suicide - Age
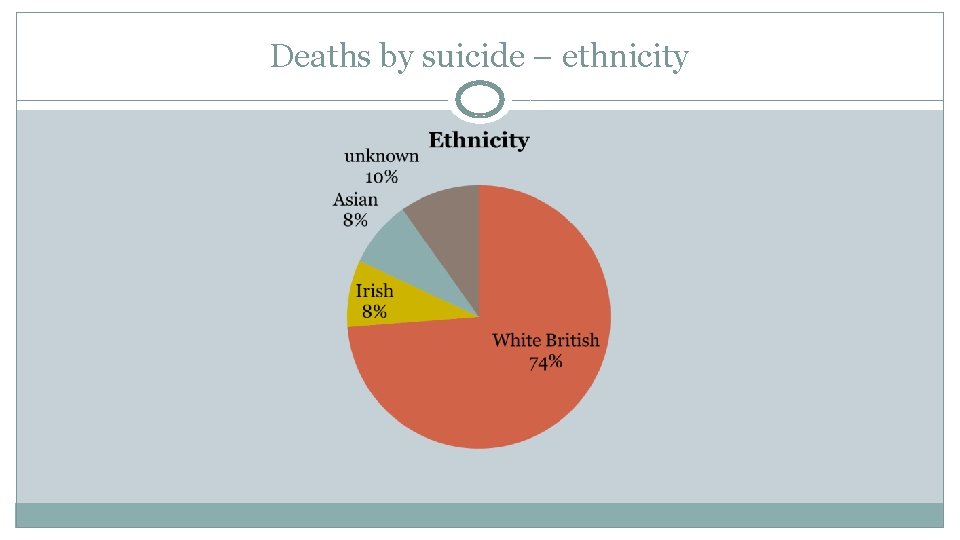
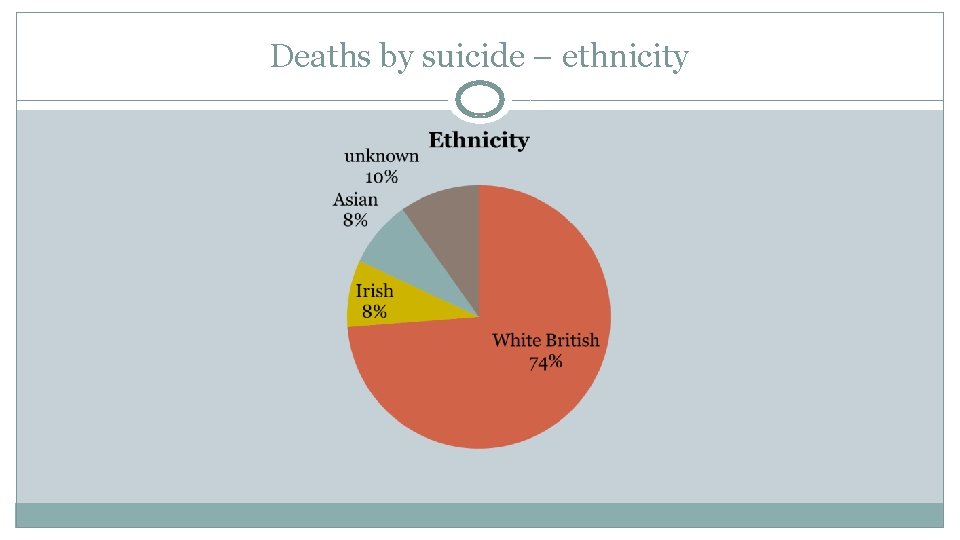
Deaths by suicide – ethnicity
Social Factors 54% lived alone 54% unemployed
Method Used 8 died by hanging 2 died by drowning (jumped into Thames) 1 – method unknown 54% had prior suicide attempt/self harm
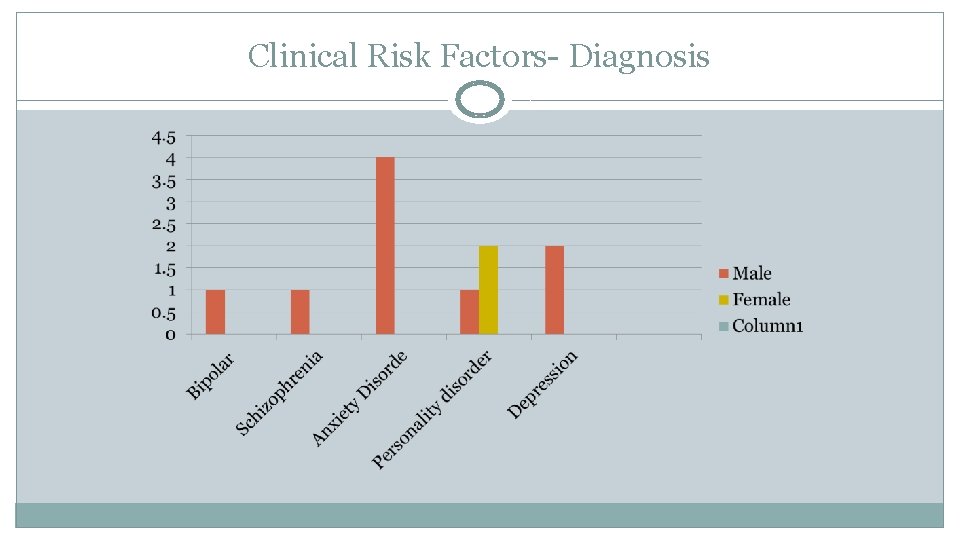
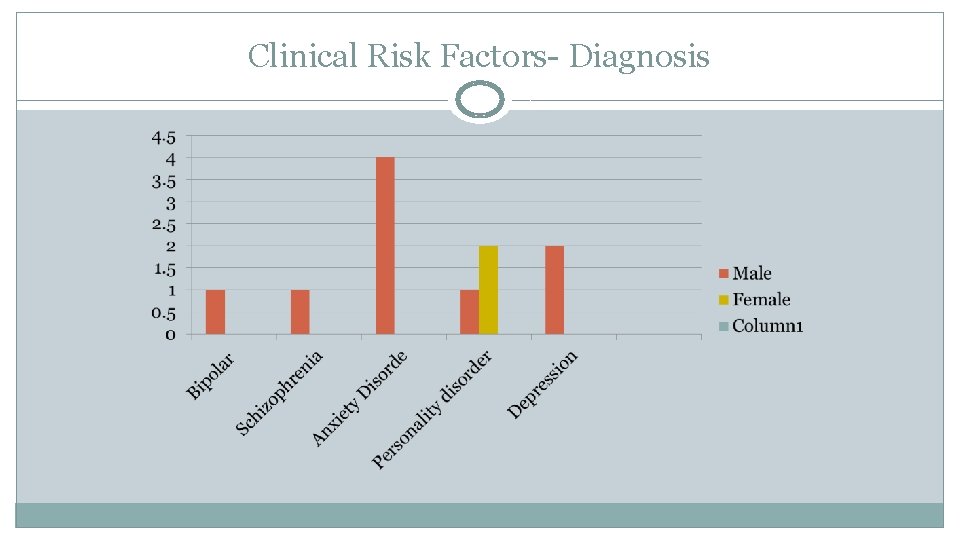
Clinical Risk Factors- Diagnosis
Comorbid Drug /Alcohol use 27% had a history of current drug/alcohol use
Mental Health Services 6 patients open to community team – 1 care coordinated 1 open to psychotherapy 2 open to HTT (one joint care with community team) 1 open to CHAMHRAS 1 inpatient – on leave
Recommendations Criteria for referrals to Psychology in the Recovery Teams to be reviewed Psychology to consider how best to convey outcomes of decisions to relevant staff Communication re management of patients placed on different ward to consultant base to be reviewed Review of admin process at CMHT and Rio access Consideration as to whether partner organisations should be given Rio access
Recommendations CPA review meetings to take place even if patient is not engaging and system to check actions have been completed Remind staff to accurately document telephone calls with service users and family Prompt follow up of outcome of welfare checks Ensure tasks allocated are completed Contact with external therapists to be considered and made when appropriate Ensure full and detailed clinical records Training on management of pts with Personality disorder for inpatient and community teams
Themes Communication – patient/carers/ professionals/external agencies Documentation Task allocation