Preventing Pediatric Intravenous Extravasation Injuries Neil Johnson MD



- Slides: 70

Preventing Pediatric Intravenous Extravasation Injuries • • • Neil Johnson, MD Barb Tofani, RN, MSN Sylvia Rineair, RN, MSHA, VA-BC Mary Haygood, RN, BSN (Retired) Julie Stalf, RN, MSN, VA-BC Darcy Doellman, MSN, RN, CRNI, VA-BC March, 2014
Objectives • High Level Overview: – Cincinnati’s 4 Year Intra Venous Extravasation Harm Reduction Initiative • Our 4 Components – – Reliable Hourly Bedside PIV Checks Evidence Based 3 Tier Medication Tissue Toxicity List “No Grade” 2 Component Assessment / Documentation Tool Real Cross-Cultural Leadership • Discussion - Questions
Basic Principles • • It takes a Team Culture change is really hard work “What would we do for our own children” ? No-one has all the answers
Basic Principles • • It takes a Team Culture change is really hard work “What would we do for our own children” ? No-one has all the answers What would we do for our own children ?
CCHMC Safety Culture
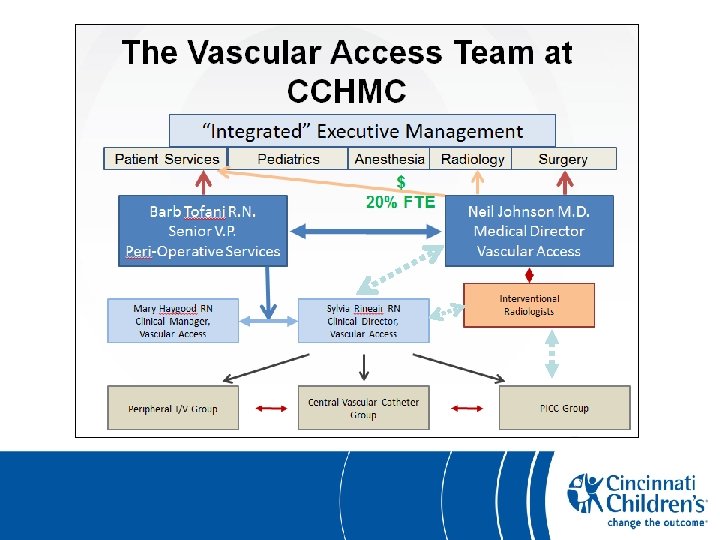
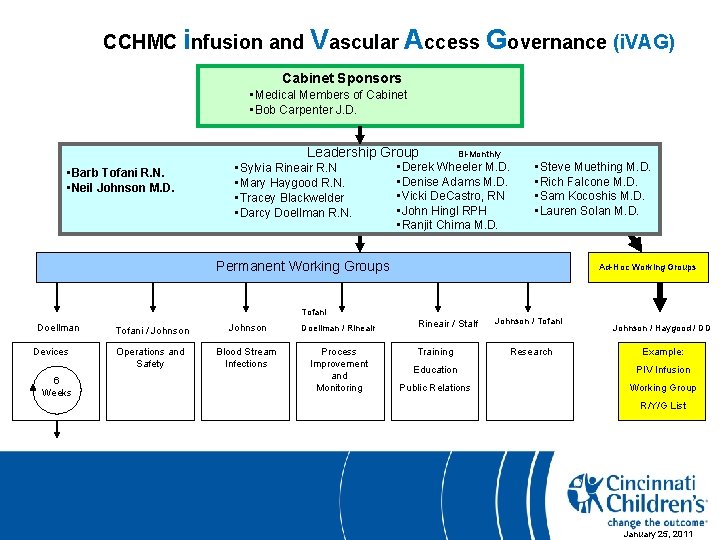
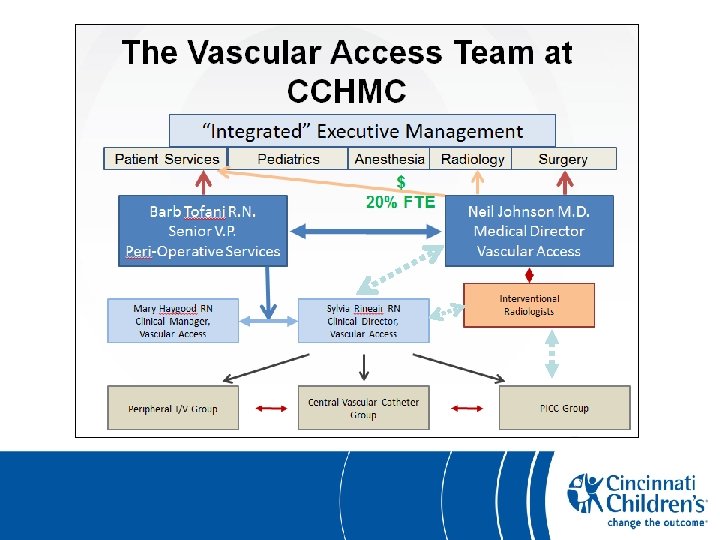
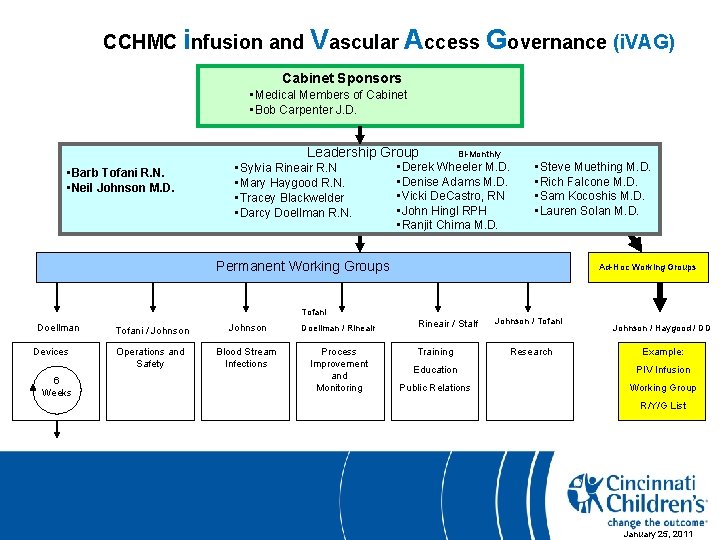
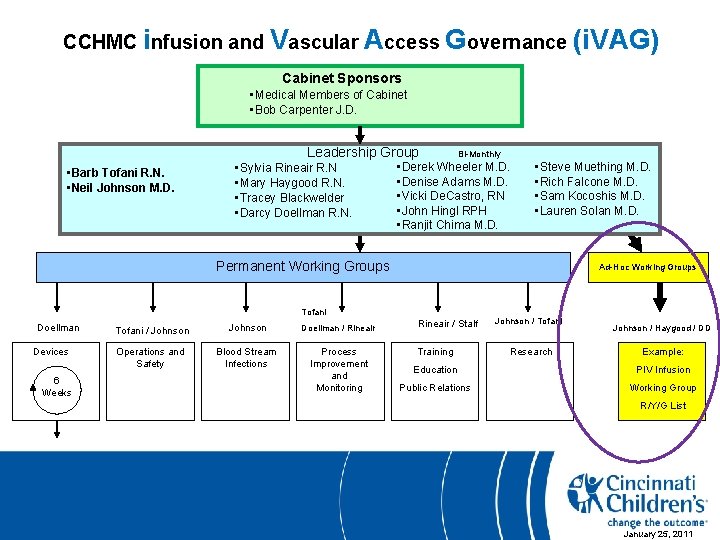
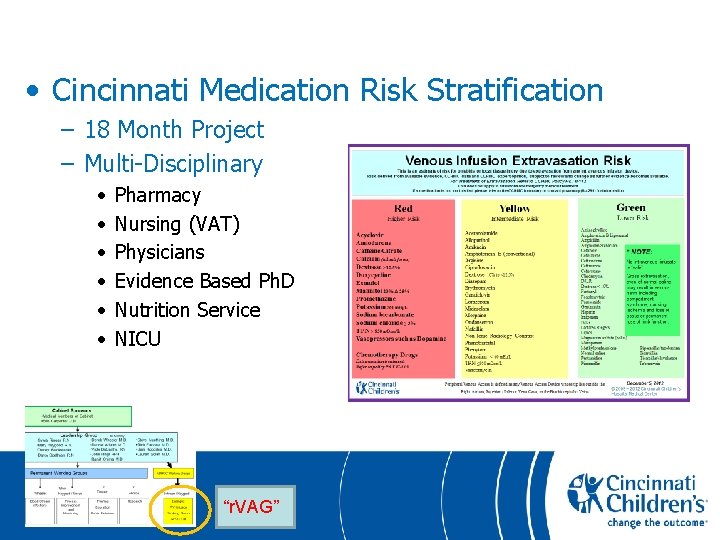
CCHMC infusion and Vascular Access Governance (i. VAG) Cabinet Sponsors • Medical Members of Cabinet • Bob Carpenter J. D. Leadership Group • Barb Tofani R. N. • Neil Johnson M. D. • Sylvia Rineair R. N • Mary Haygood R. N. • Tracey Blackwelder • Darcy Doellman R. N. Bi-Monthly • Derek Wheeler M. D. • Denise Adams M. D. • Vicki De. Castro, RN • John Hingl RPH • Ranjit Chima M. D. • Steve Muething M. D. • Rich Falcone M. D. • Sam Kocoshis M. D. • Lauren Solan M. D. Permanent Working Groups Ad-Hoc Working Groups Tofani Doellman Devices 6 Weeks Tofani / Johnson Doellman / Rineair Operations and Safety Blood Stream Infections Process Improvement and Monitoring Rineair / Stalf Training Johnson / Tofani Research Johnson / Haygood / DD Example: Education PIV Infusion Public Relations Working Group R/Y/G List January 25, 2011
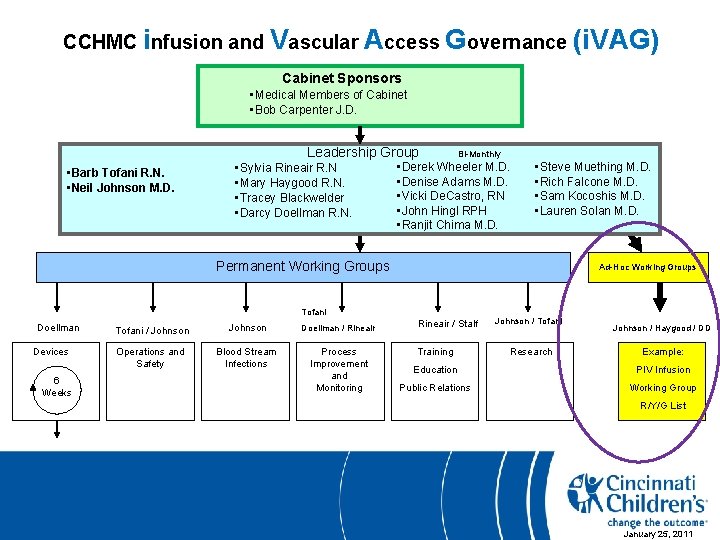
CCHMC infusion and Vascular Access Governance (i. VAG) Cabinet Sponsors • Medical Members of Cabinet • Bob Carpenter J. D. Leadership Group • Barb Tofani R. N. • Neil Johnson M. D. • Sylvia Rineair R. N • Mary Haygood R. N. • Tracey Blackwelder • Darcy Doellman R. N. Bi-Monthly • Derek Wheeler M. D. • Denise Adams M. D. • Vicki De. Castro, RN • John Hingl RPH • Ranjit Chima M. D. • Steve Muething M. D. • Rich Falcone M. D. • Sam Kocoshis M. D. • Lauren Solan M. D. Permanent Working Groups Ad-Hoc Working Groups Tofani Doellman Devices 6 Weeks Tofani / Johnson Doellman / Rineair Operations and Safety Blood Stream Infections Process Improvement and Monitoring Rineair / Stalf Training Johnson / Tofani Research Johnson / Haygood / DD Example: Education PIV Infusion Public Relations Working Group R/Y/G List January 25, 2011

Definition • HARM – Institute for Healthcare Improvement (IHI) • “Unintended physical injury resulting from …. medical care…” – Canadian Disclosure Guidelines (JAMA 2012 Vol 307 #20) • “an outcome that negatively affects a patient’s health / quality of life…”
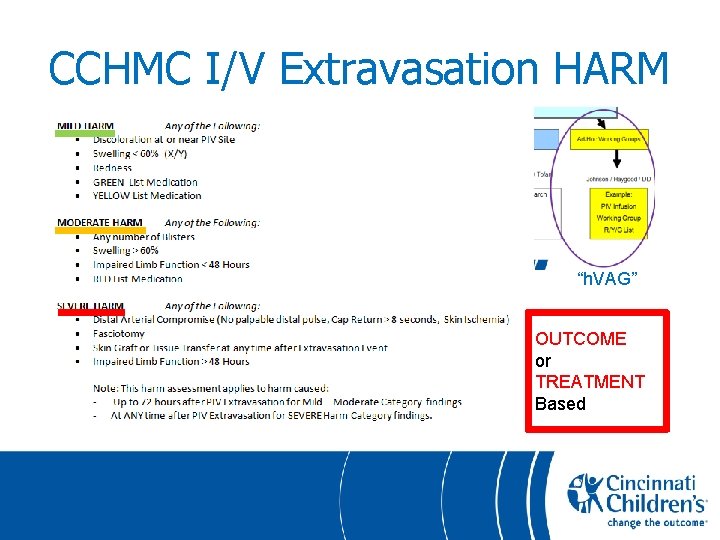
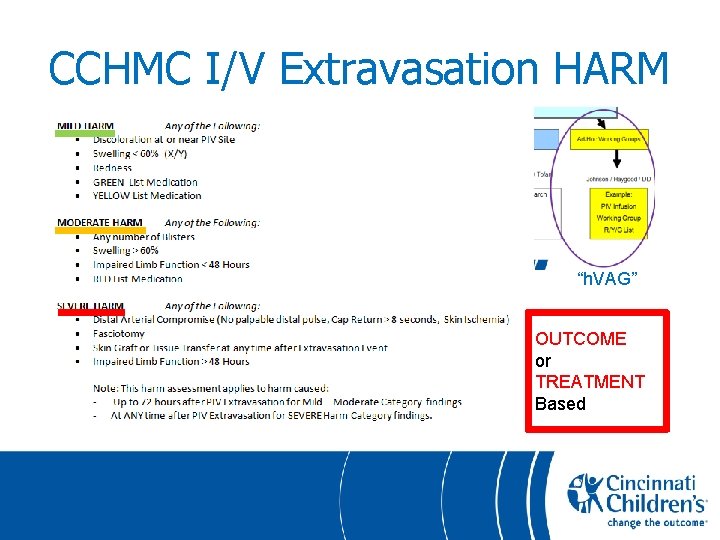
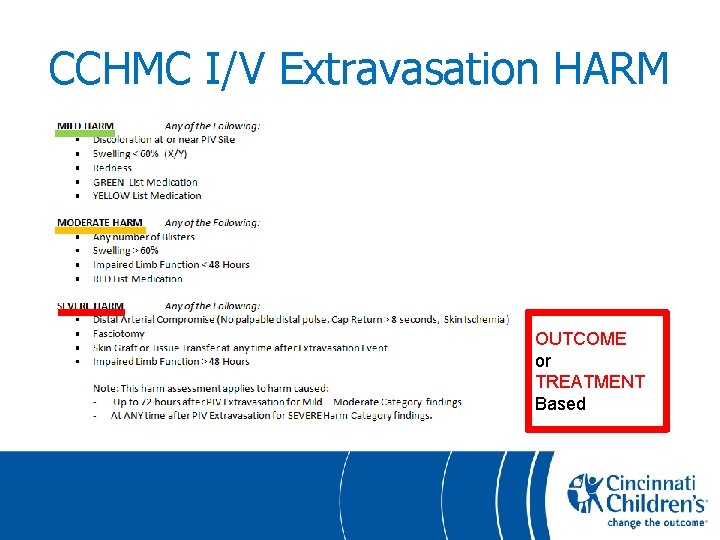
CCHMC I/V Extravasation HARM “h. VAG” OUTCOME or TREATMENT Based
Definition • SAFETY Institute of Medicine (2000): “…. no commonly accepted definition of the safety net exists…. . ” Institute of Medicine, 2000 America’s Health Care Safety Net: Intact but Endangered. National Academy Press p 3 -4
Definition (CCHMC Vascular Access Team ) • SAFETY: • The Processes, Policies, People and Systems which seek to: • MINIMIZE Necessary Risk • AVOID Unnecessary Risk
Definition • SAFETY: – (CCHMC Vascular Access Team ) The Processes, Policies, People and Systems which seek to: • MINIMIZE Necessary Risk • AVOID Unnecessary Risk “NOTHING in Life or Medical Practice is Risk Free” The ONLY way to achieve Zero Risk is to close the Hospital
“PIV” Peripheral Intravenous • PIV – A “simple” device for administration of medical fluids directly into a peripheral vein – A simple procedure not worthy of the attention of an MD • Common Medical Procedure – 70 – 80% of Hospital Inpatients
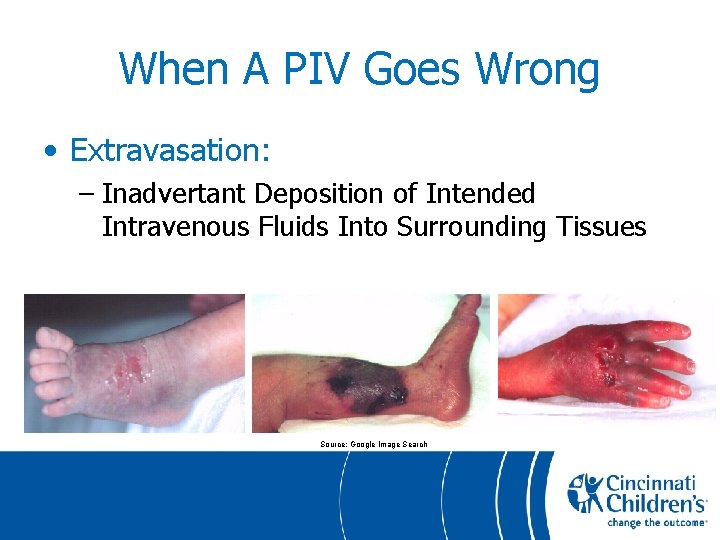
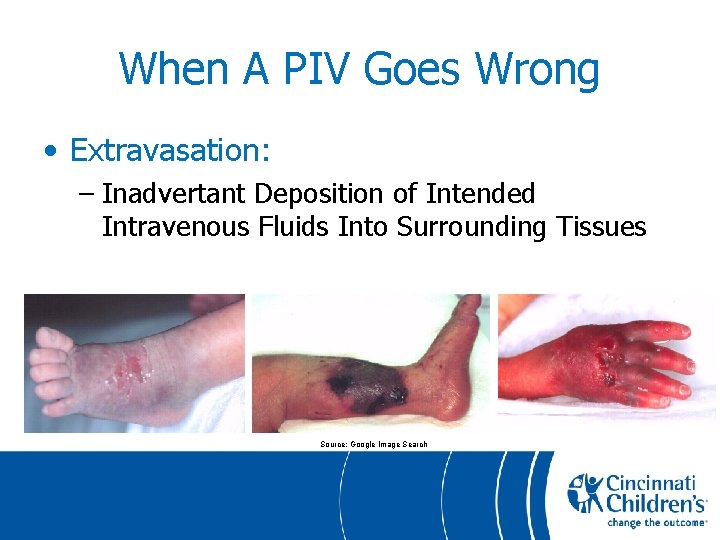
When A PIV Goes Wrong • Extravasation: – Inadvertant Deposition of Intended Intravenous Fluids Into Surrounding Tissues Source: Google Image Search
Terminology: Extravasation (Vs Infiltration) • Cincinnati Only Uses “EXTRAVASATION” • EXTRA = “Out Of or Outside” • VASCULAR = “Vessel” • EXTRAVASATION = “Out of the Vessel” “Infiltration” Better used to describe purposeful subcutaneous injection of fluids Example: “The skin was infiltrated with local anesthetic solution before incision”
PIV Extravasation • Basic Mechanisms of Injury 1. VOLUME • “Simple” PIV Fluids Leak into Subcutaneous Tissues • Pressure Compresses Local Veins and later, Arteries • Reduces then Blocks Blood Supply To The Limb
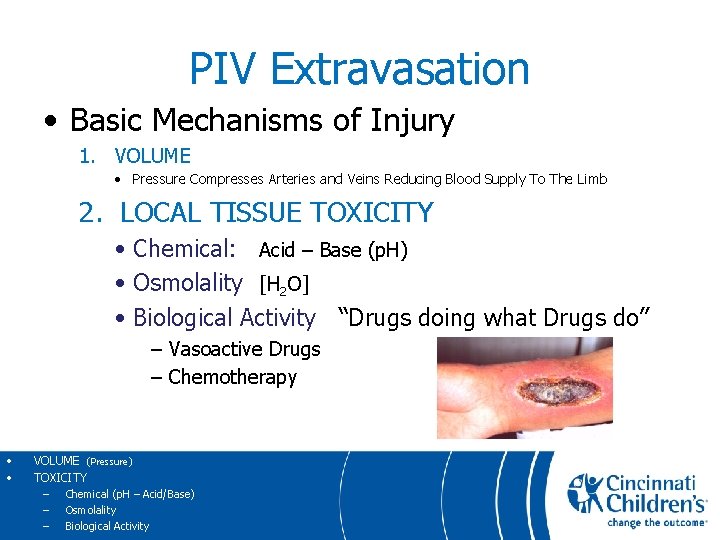
PIV Extravasation • Basic Mechanisms of Injury 1. VOLUME • Pressure Compresses Arteries and Veins Reducing Blood Supply To The Limb 2. LOCAL TISSUE TOXICITY • Chemical: Acid – Base (p. H) • Osmolality [H 2 O] • Biological Activity “Drugs doing what Drugs do” – Vasoactive Drugs – Chemotherapy • • VOLUME (Pressure) TOXICITY – Chemical (p. H – Acid/Base) – Osmolality – Biological Activity
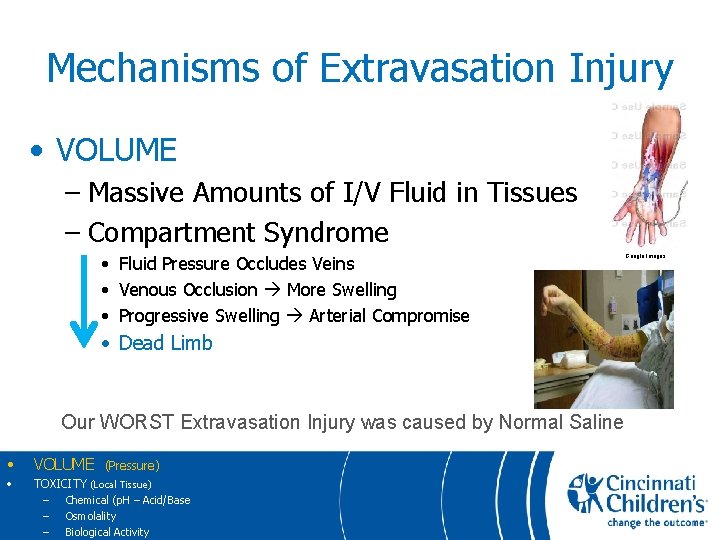
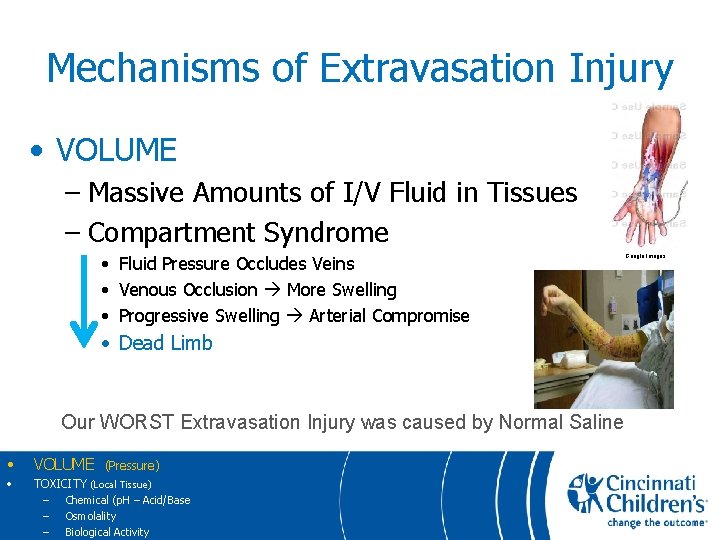
Mechanisms of Extravasation Injury • VOLUME – Massive Amounts of I/V Fluid in Tissues – Compartment Syndrome • Fluid Pressure Occludes Veins • Venous Occlusion More Swelling • Progressive Swelling Arterial Compromise • Dead Limb Our WORST Extravasation Injury was caused by Normal Saline • VOLUME • TOXICITY (Local Tissue) – Chemical (p. H – Acid/Base – Osmolality – Biological Activity (Pressure) Google Images
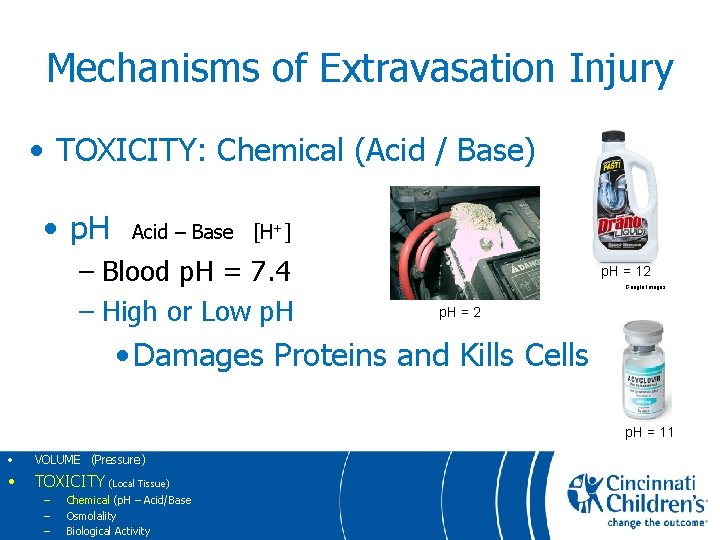
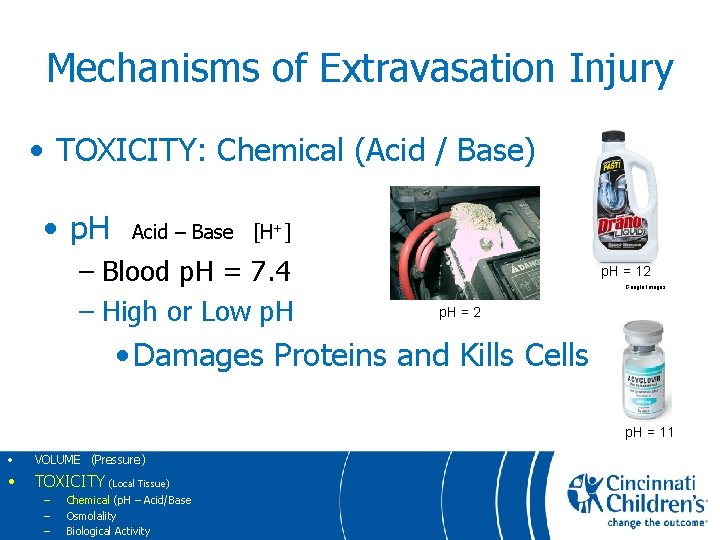
Mechanisms of Extravasation Injury • TOXICITY: Chemical (Acid / Base) • p. H Acid – Base [H+] – Blood p. H = 7. 4 – High or Low p. H = 12 Google Images p. H = 2 • Damages Proteins and Kills Cells p. H = 11 • VOLUME (Pressure) • TOXICITY (Local Tissue) – – – Chemical (p. H – Acid/Base Osmolality Biological Activity
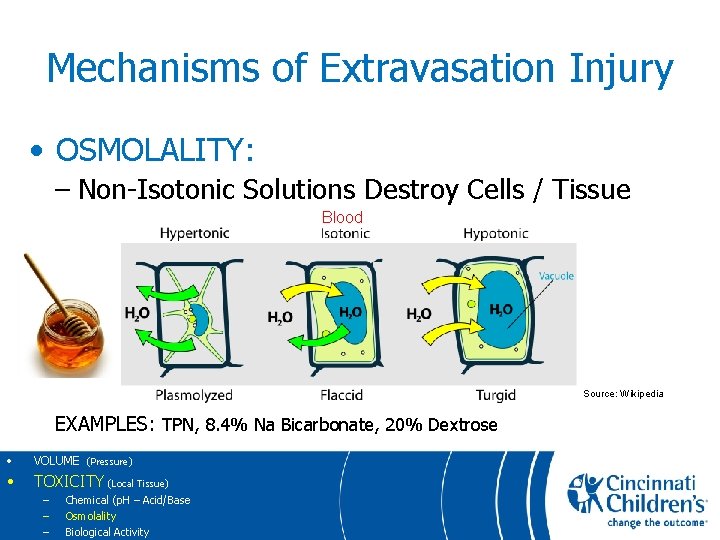
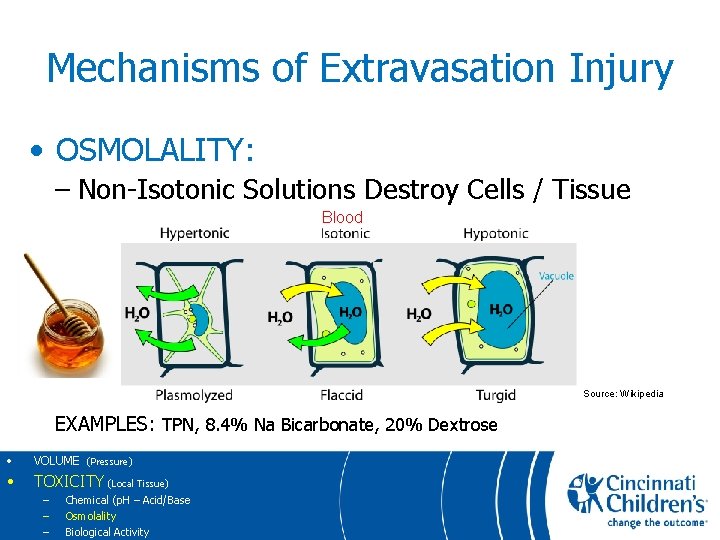
Mechanisms of Extravasation Injury • OSMOLALITY: – Non-Isotonic Solutions Destroy Cells / Tissue Blood Source: Wikipedia EXAMPLES: TPN, 8. 4% Na Bicarbonate, 20% Dextrose • VOLUME (Pressure) • TOXICITY (Local Tissue) – – – Chemical (p. H – Acid/Base Osmolality Biological Activity
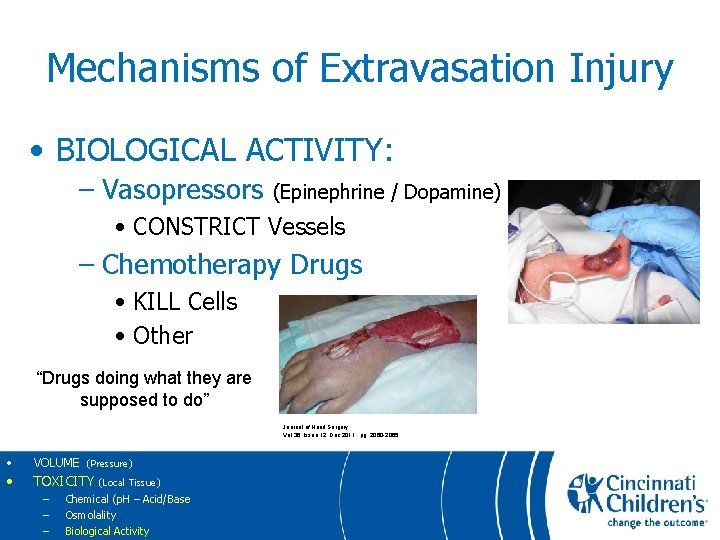
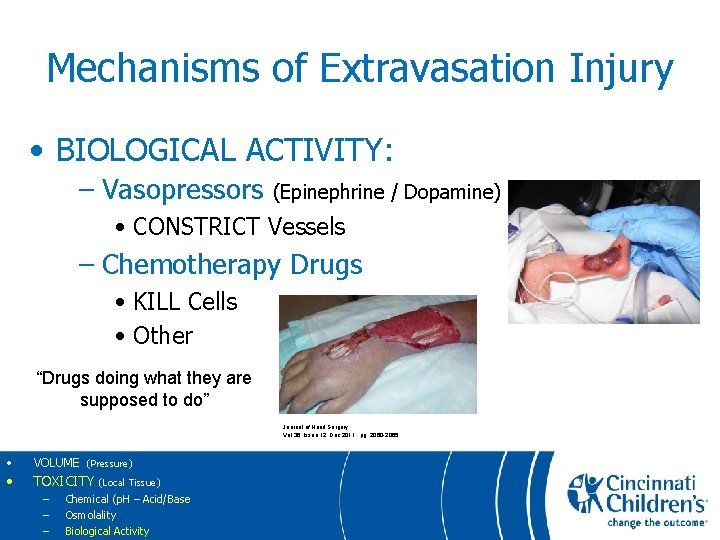
Mechanisms of Extravasation Injury • BIOLOGICAL ACTIVITY: – Vasopressors (Epinephrine / Dopamine) • CONSTRICT Vessels – Chemotherapy Drugs • KILL Cells • Other “Drugs doing what they are supposed to do” Journal of Hand Surgery Vol 36, Issue 12, Dec 2011. pg: 2060 -2065 • VOLUME (Pressure) • TOXICITY (Local Tissue) – – – Chemical (p. H – Acid/Base Osmolality Biological Activity
Preventing PIV Extravasation Injuries • Two Simple Ideas – AVOID Unnecessary Risk • Give Tissue Toxic Drugs Centrally – MINIMIZE Necessary Risk • Catch Extravasations Early • Use Oral Medications When Indicated
Preventing PIV Extravasation Injuries • Two Simple Ideas – AVOID Unnecessary Risk • Give Tissue Toxic Drugs Centrally – MINIMIZE Necessary Risk • Catch Extravasations Early • Use Oral Medications When Indicated “It’s not that simple”
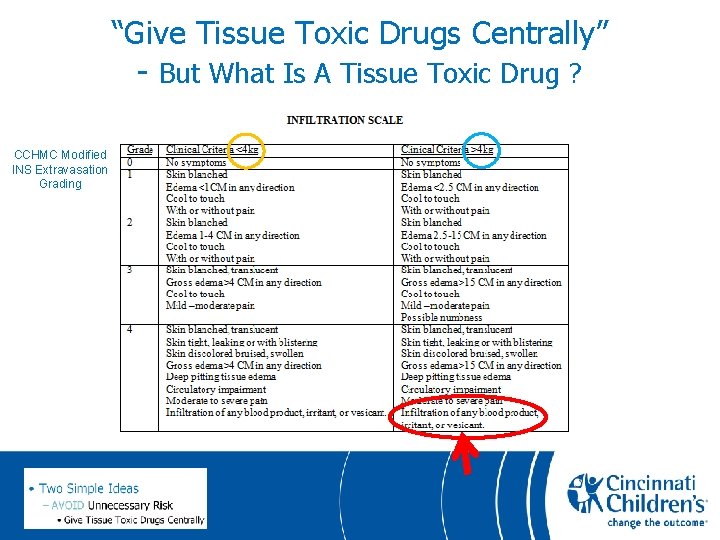
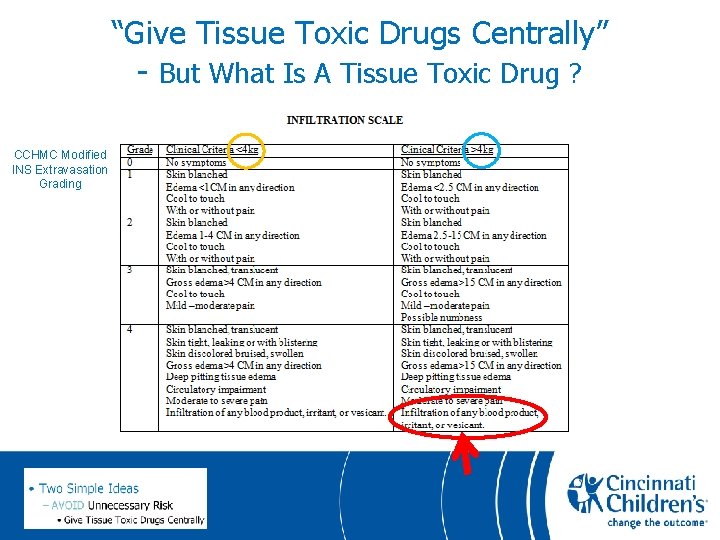
“Give Tissue Toxic Drugs Centrally” - But What Is A Tissue Toxic Drug ? CCHMC Modified INS Extravasation Grading
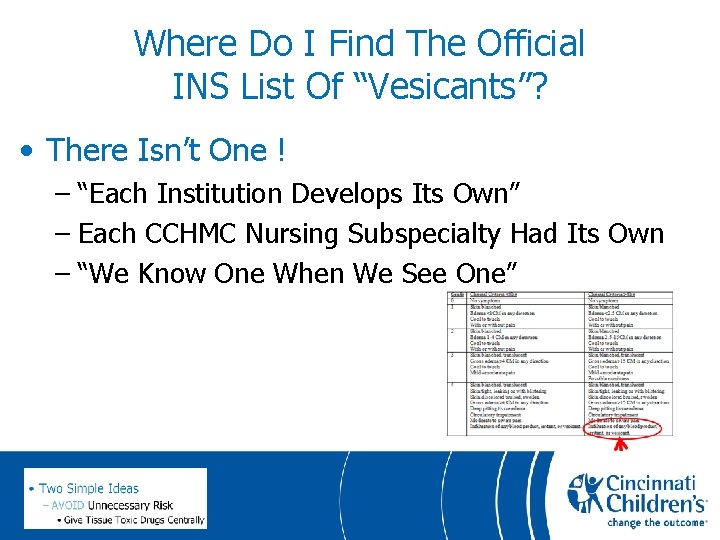
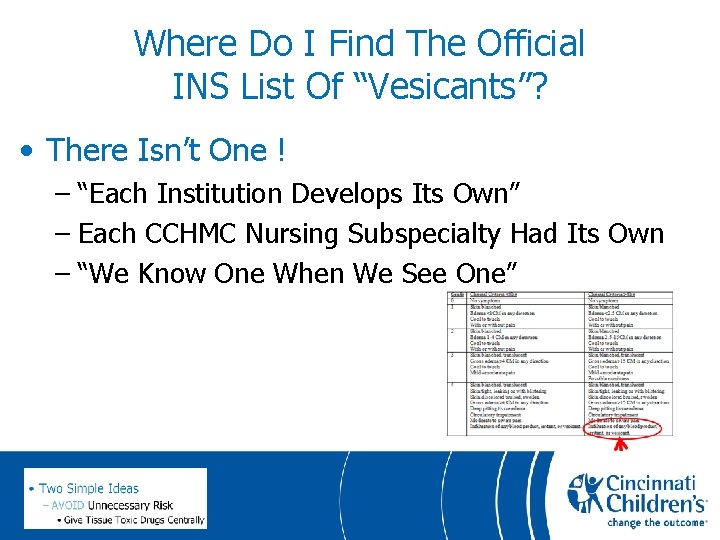
Where Do I Find The Official INS List Of “Vesicants”? • There Isn’t One ! – “Each Institution Develops Its Own” – Each CCHMC Nursing Subspecialty Had Its Own – “We Know One When We See One”
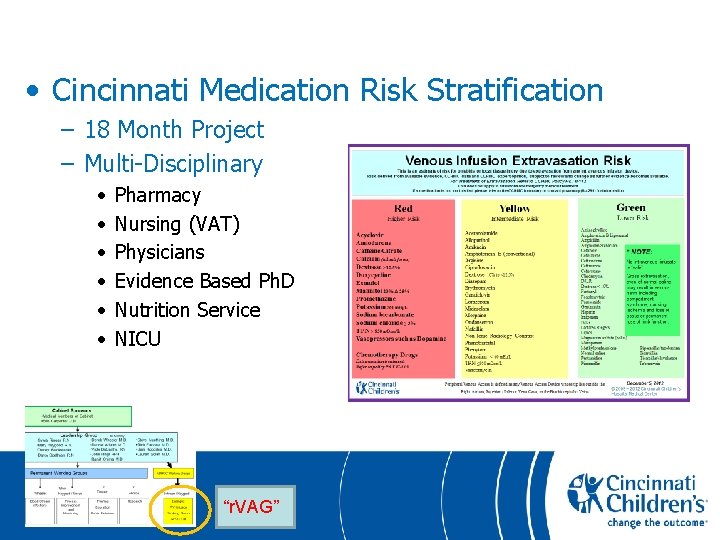
• Cincinnati Medication Risk Stratification – 18 Month Project – Multi-Disciplinary • • • Pharmacy Nursing (VAT) Physicians Evidence Based Ph. D Nutrition Service NICU “r. VAG”
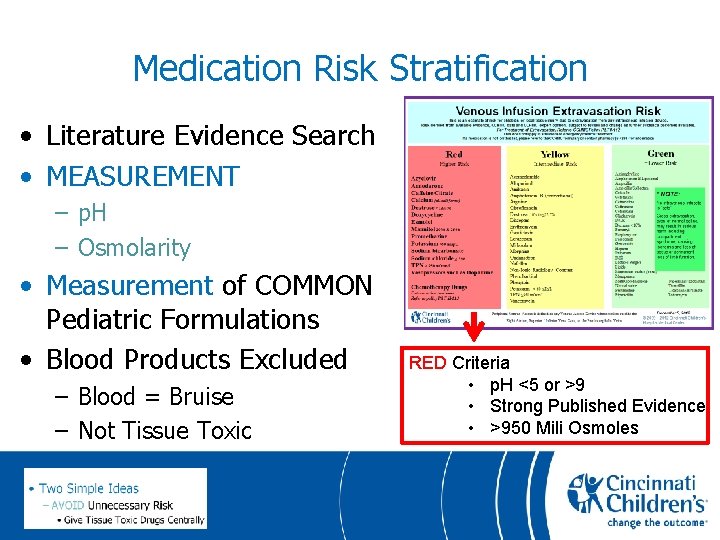
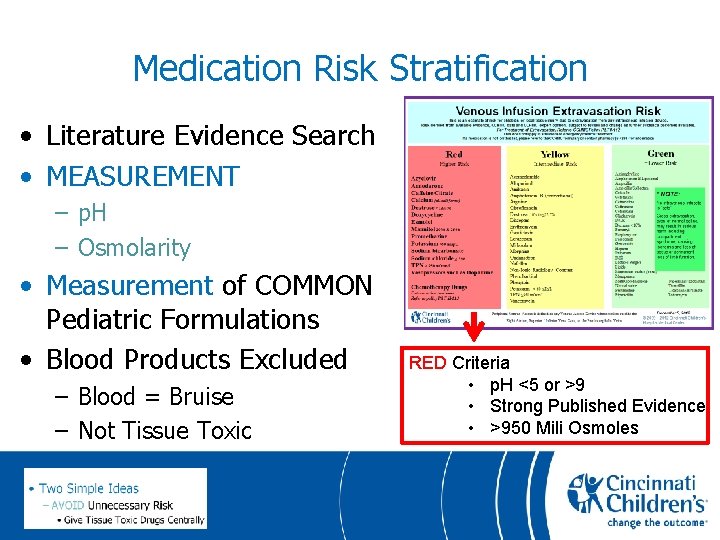
Medication Risk Stratification • Literature Evidence Search • MEASUREMENT – p. H – Osmolarity • Measurement of COMMON Pediatric Formulations • Blood Products Excluded – Blood = Bruise – Not Tissue Toxic RED Criteria • p. H <5 or >9 • Strong Published Evidence • >950 Mili Osmoles
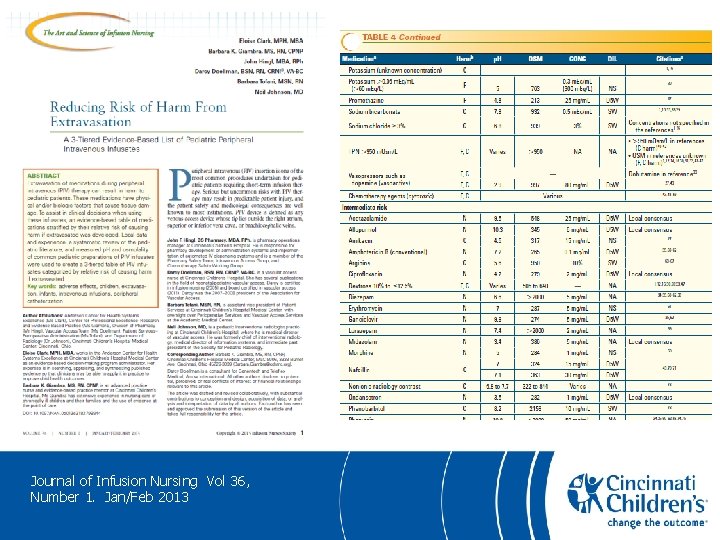
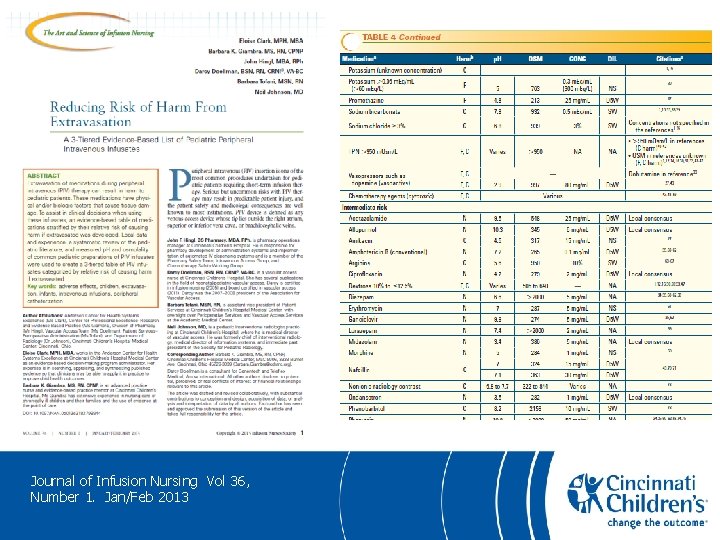
Journal of Infusion Nursing Vol 36, Number 1. Jan/Feb 2013
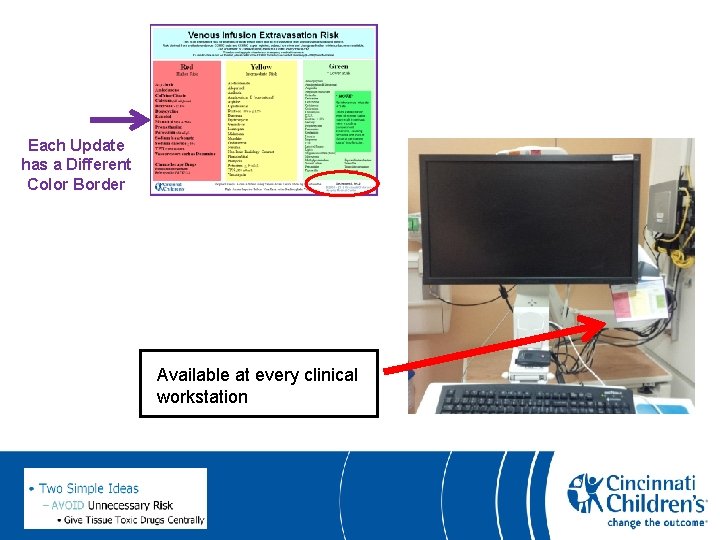
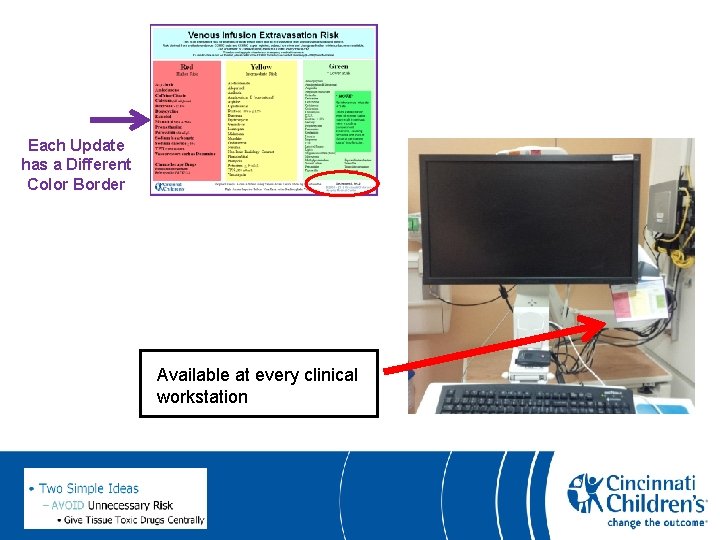
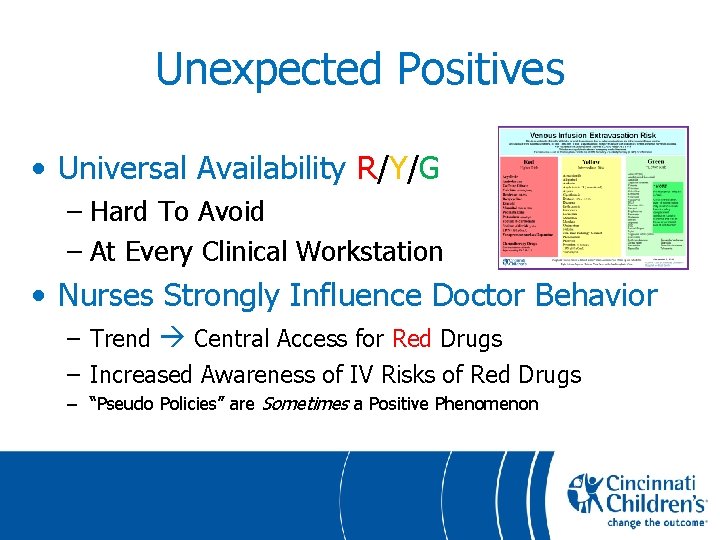
Each Update has a Different Color Border Available at every clinical workstation
Unexpected Positives • Universal Availability R/Y/G – Hard To Avoid – At Every Clinical Workstation • Nurses Strongly Influence Doctor Behavior – Trend Central Access for Red Drugs – Increased Awareness of IV Risks of Red Drugs – “Pseudo Policies” are Sometimes a Positive Phenomenon
Preventing PIV Extravasation Injuries • Two Simple Ideas – AVOID Unnecessary Risk • Give Tissue Toxic Drugs Centrally – MINIMIZE Necessary Risk • Catch Extravasations Early • Use Oral Medications When Indicated
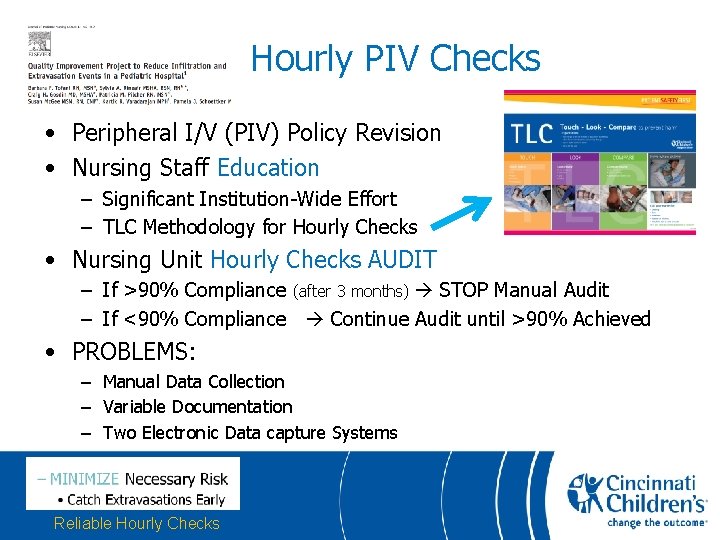
Journal Pediatric Nursing (2012) 27, 682 -689)
Hourly PIV Checks • Peripheral I/V (PIV) Policy Revision • Nursing Staff Education – Significant Institution-Wide Effort – TLC Methodology for Hourly Checks • Nursing Unit Hourly Checks AUDIT – If >90% Compliance (after 3 months) STOP Manual Audit – If <90% Compliance Continue Audit until >90% Achieved • PROBLEMS: – Manual Data Collection – Variable Documentation – Two Electronic Data capture Systems Reliable Hourly Checks
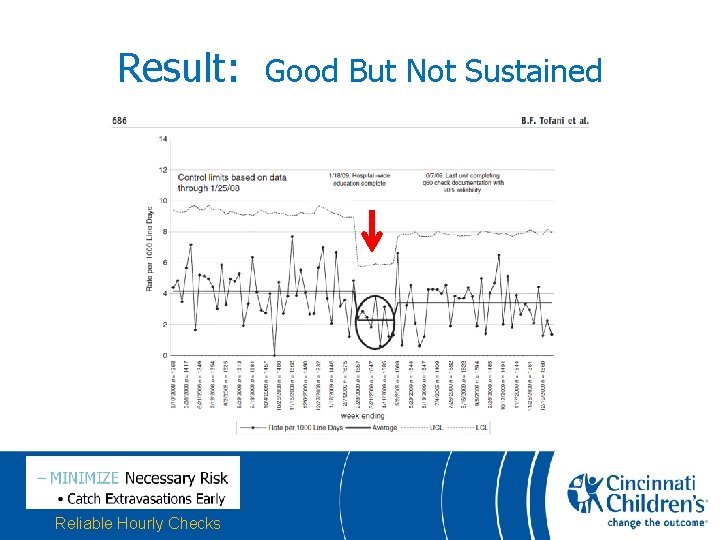
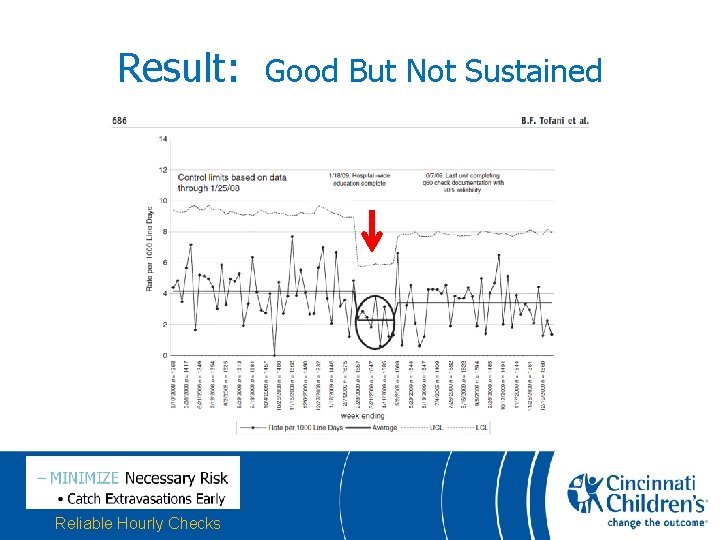
Result: Reliable Hourly Checks Good But Not Sustained
New Efforts: Reliable Hourly Checks • EPIC EMR Implemented • All I/V Documentation now in ONE place • 18 month “CVAT” Project with I. T. All Vascular Access Data Abstraction Project (CVAT) • >60% Extravasation = 1 Month Manual Audit – Unpopular! • Immediate Feedback System • “Personal Interview” (>60%)
Immediate PIV Extravasation Feedback System • • • > 30% volume or R drug extravasation charted in EPIC Automatic messaging to VAT and Med Director VAT Team nurse visits bedside 24/7 Immediate Feedback Advice to bedside nurse Treatment if appropriate VAT follow-up in 1 -2 weeks – Personal interview (Nurse, supervisor, VAT leader) – Information Gathering for Analysis by VAT Improvement Team
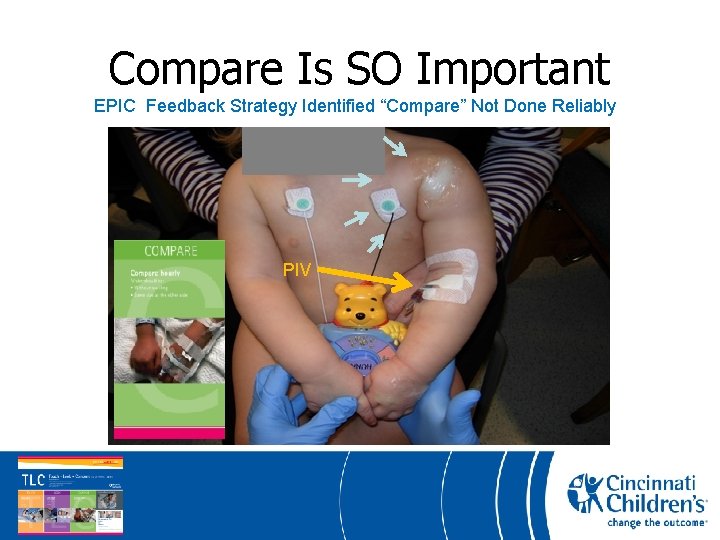
Compare Is SO Important EPIC Feedback Strategy Identified “Compare” Not Done Reliably
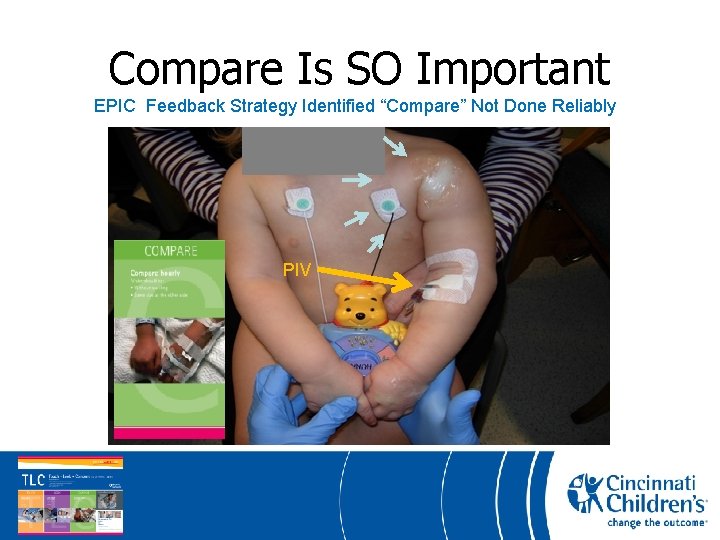
Compare Is SO Important EPIC Feedback Strategy Identified “Compare” Not Done Reliably PIV
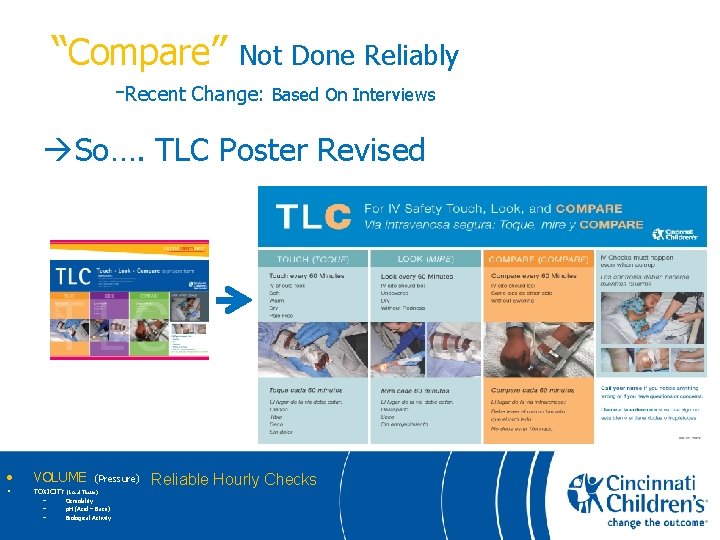
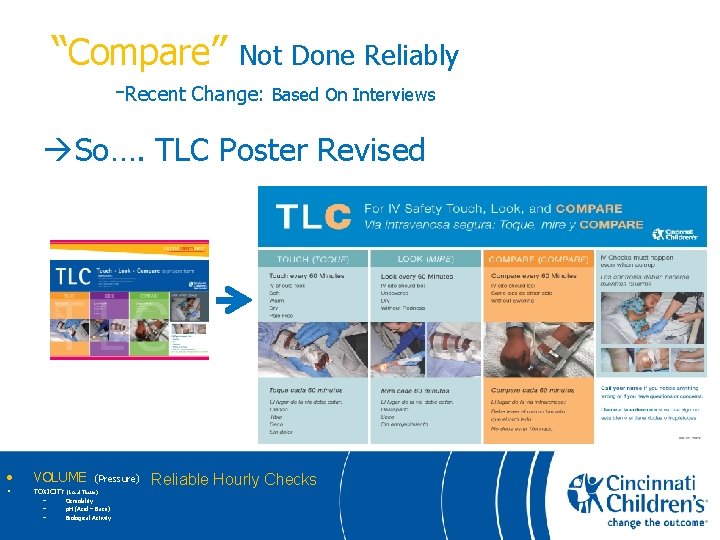
“Compare” Not Done Reliably -Recent Change: Based On Interviews So…. TLC Poster Revised • VOLUME • TOXICITY – – – (Pressure) (Local Tissue) Osmolality p. H (Acid – Base) Biological Activity Reliable Hourly Checks
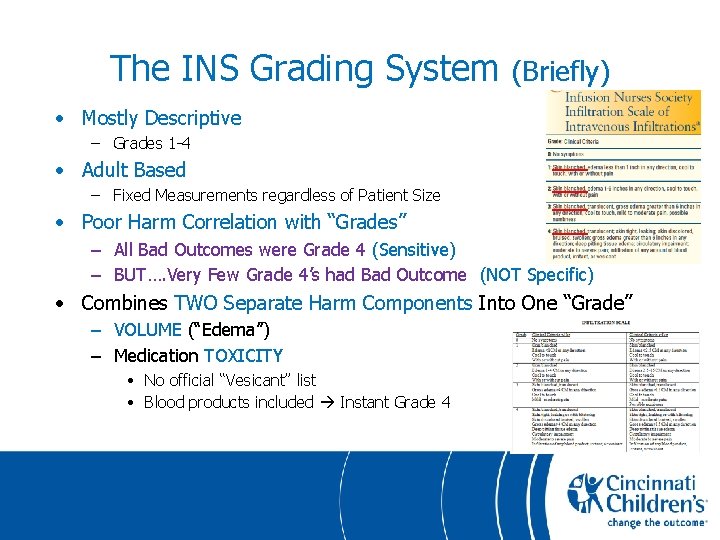
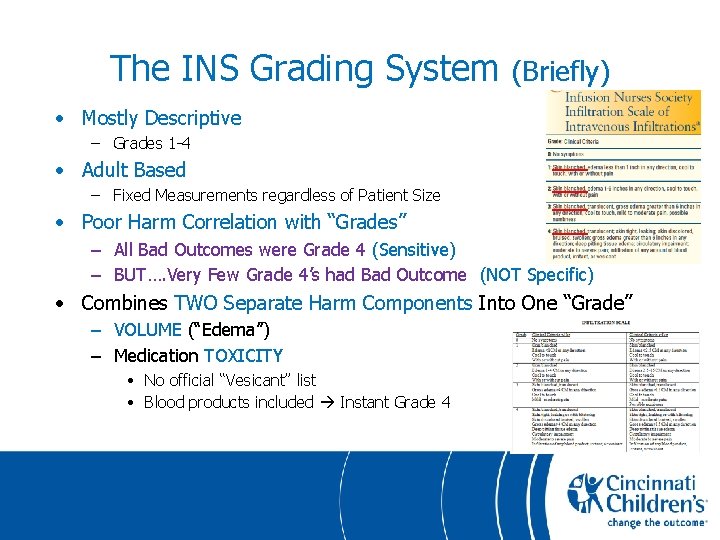
The INS Grading System (Briefly) • Mostly Descriptive – Grades 1 -4 • Adult Based – Fixed Measurements regardless of Patient Size • Poor Harm Correlation with “Grades” – All Bad Outcomes were Grade 4 (Sensitive) – BUT…. Very Few Grade 4’s had Bad Outcome (NOT Specific) • Combines TWO Separate Harm Components Into One “Grade” – VOLUME (“Edema”) – Medication TOXICITY • No official “Vesicant” list • Blood products included Instant Grade 4
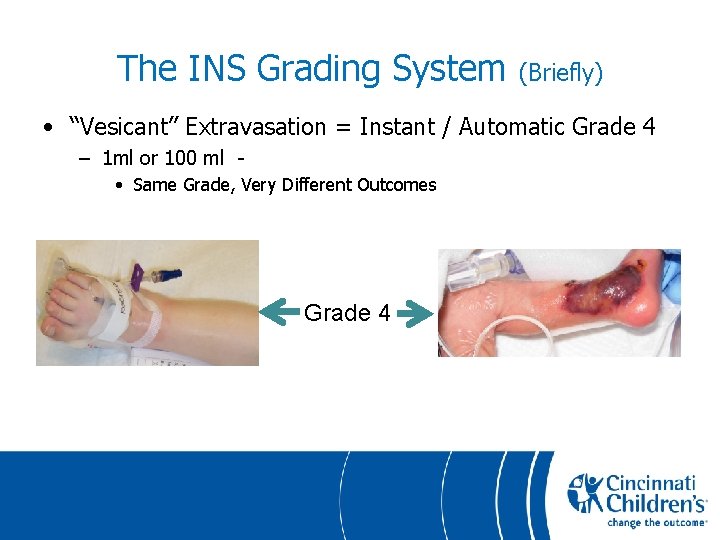
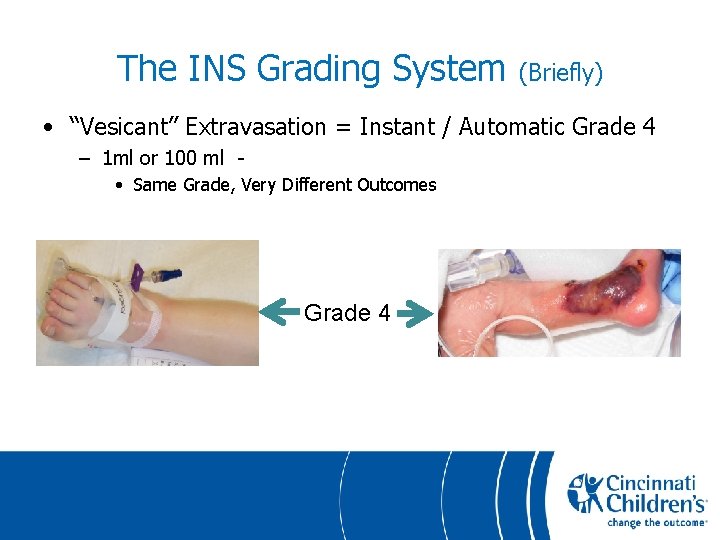
The INS Grading System (Briefly) • “Vesicant” Extravasation = Instant / Automatic Grade 4 – 1 ml or 100 ml • Same Grade, Very Different Outcomes Grade 4
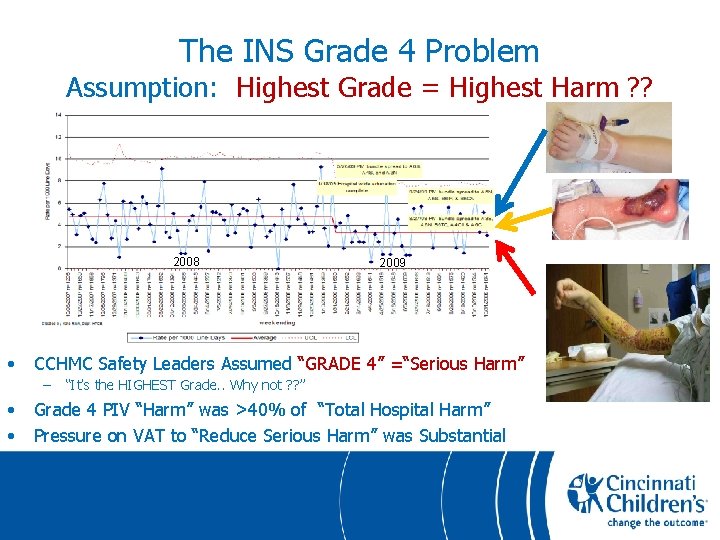
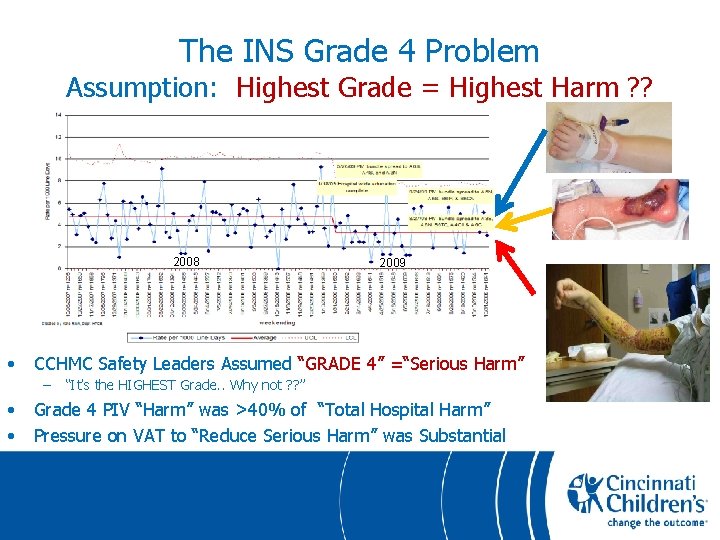
The INS Grade 4 Problem Assumption: Highest Grade = Highest Harm ? ? 2008 • CCHMC Safety Leaders Assumed “GRADE 4” =“Serious Harm” – • • 2009 “It’s the HIGHEST Grade. . Why not ? ? ” Grade 4 PIV “Harm” was >40% of “Total Hospital Harm” Pressure on VAT to “Reduce Serious Harm” was Substantial
The CCHMC Extravasation Documentation Tool • • It’s ONLY a Tool Does NOT Change Outcomes Itself Requires Leadership and Accountability Informs Change and Quality Processes Separates The Two Major Harm Components Used for ALL Extravasations, Not Only PIV Compulsory at CCHMC - INS Grades Not Available EMR (EPIC) Very Helpful
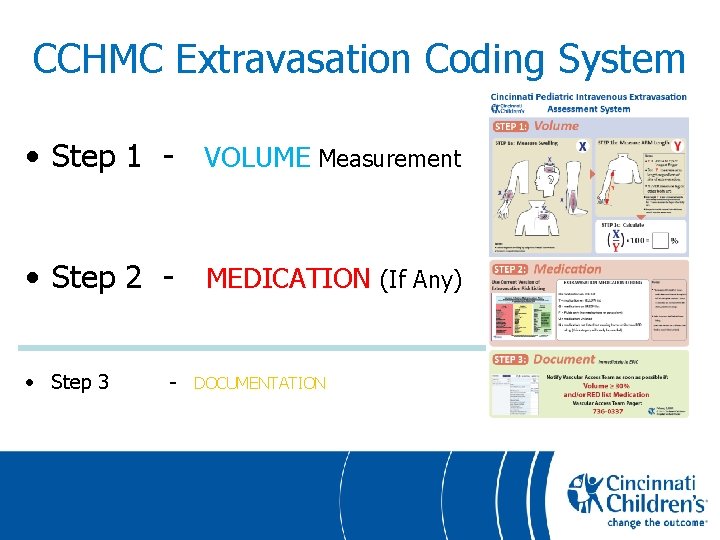
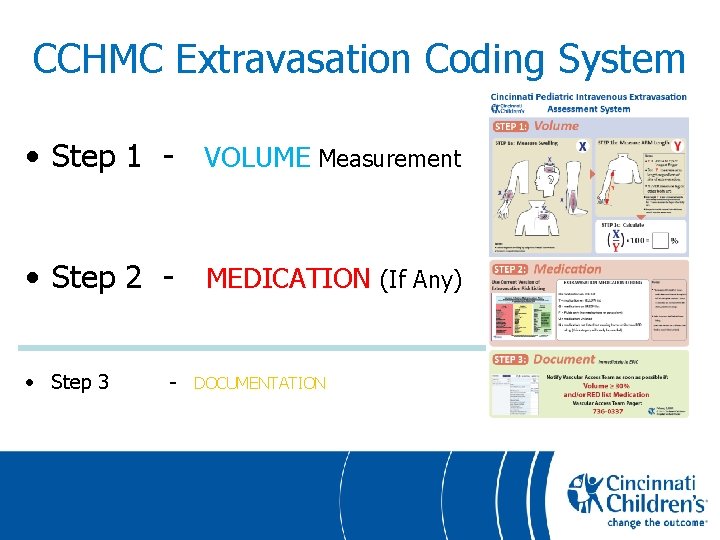
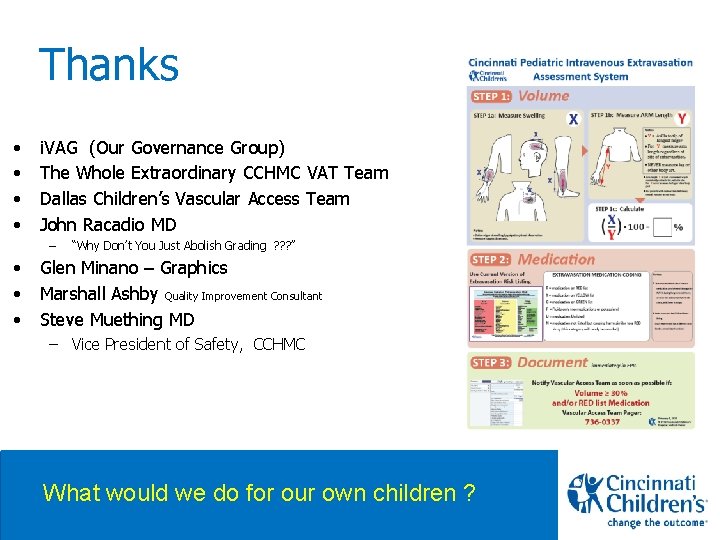
CCHMC Extravasation Coding System • Step 1 - VOLUME Measurement • Step 2 - MEDICATION (If Any) • Step 3 - DOCUMENTATION
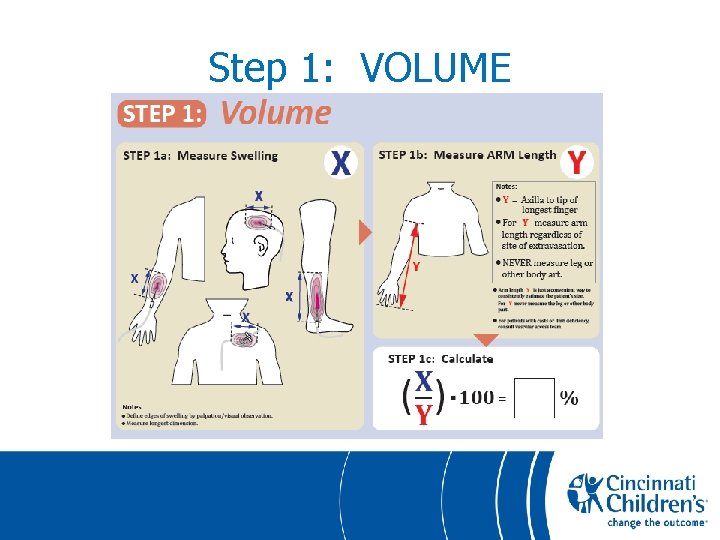
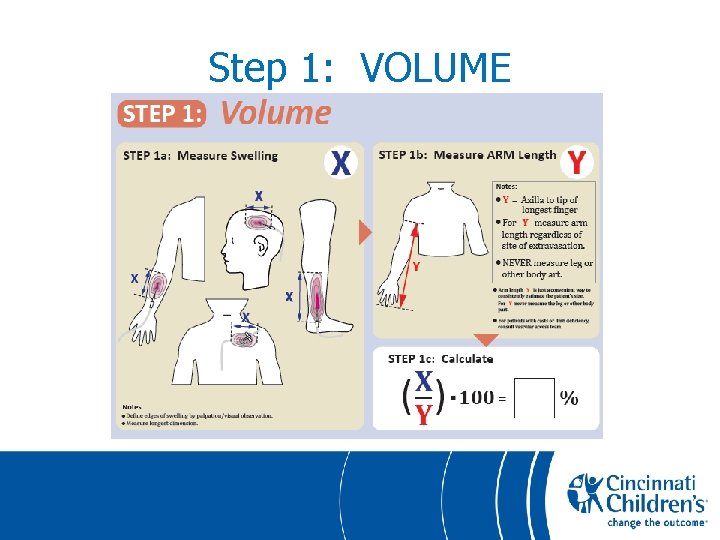
Step 1: VOLUME
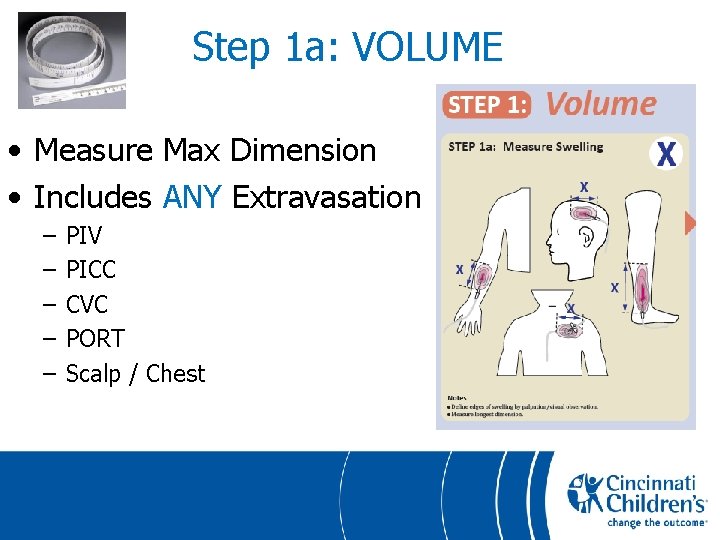
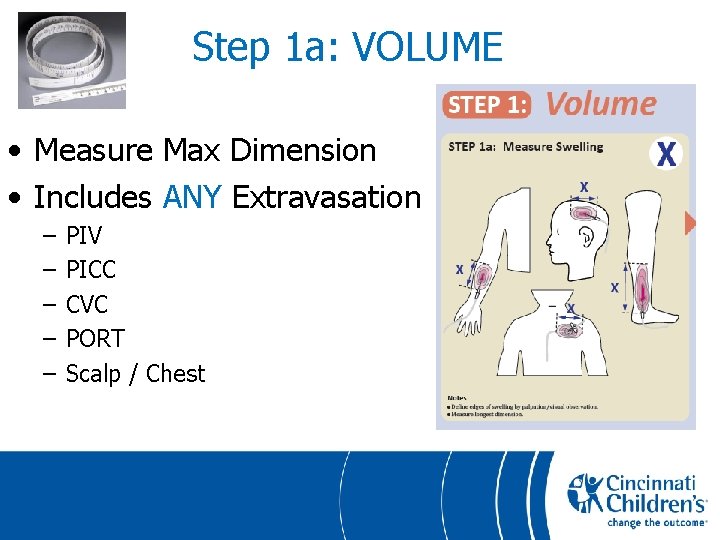
Step 1 a: VOLUME • Measure Max Dimension • Includes ANY Extravasation – – – PIV PICC CVC PORT Scalp / Chest
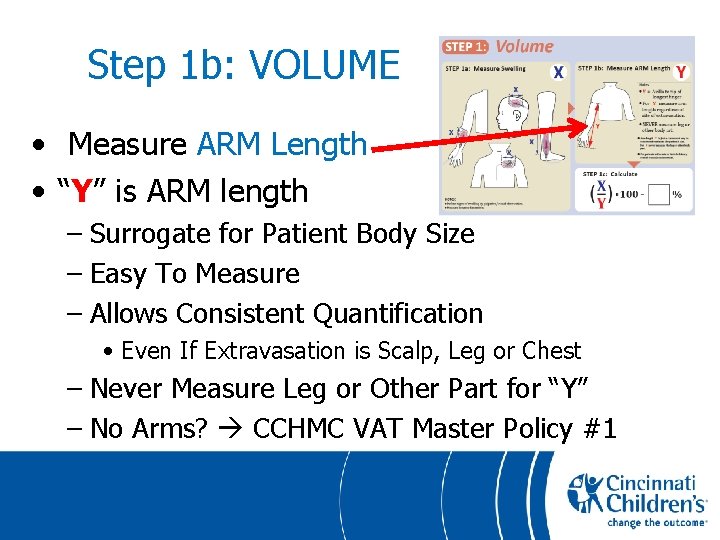
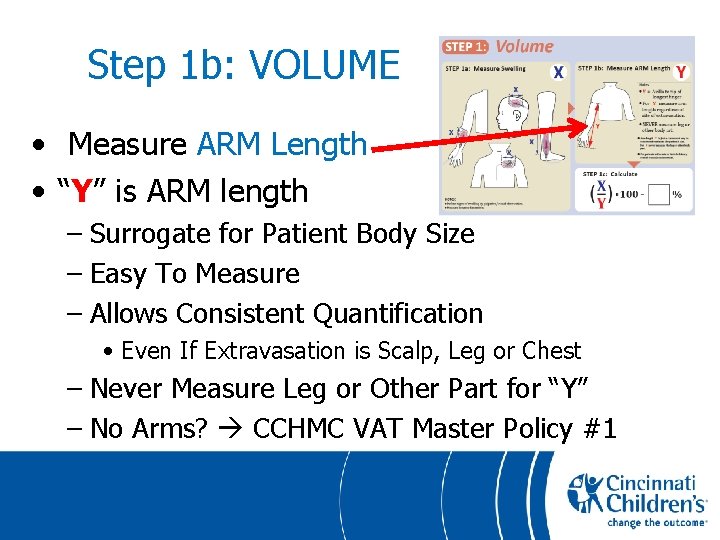
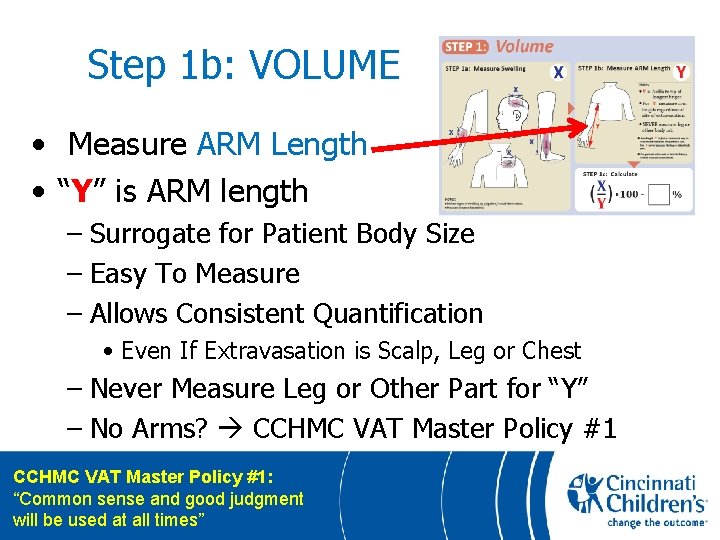
Step 1 b: VOLUME • Measure ARM Length • “Y” is ARM length – Surrogate for Patient Body Size – Easy To Measure – Allows Consistent Quantification • Even If Extravasation is Scalp, Leg or Chest – Never Measure Leg or Other Part for “Y” – No Arms? CCHMC VAT Master Policy #1
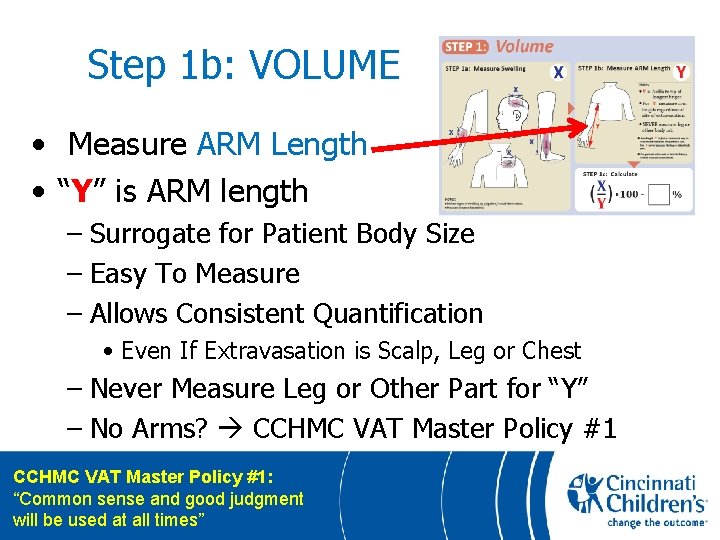
Step 1 b: VOLUME • Measure ARM Length • “Y” is ARM length – Surrogate for Patient Body Size – Easy To Measure – Allows Consistent Quantification • Even If Extravasation is Scalp, Leg or Chest – Never Measure Leg or Other Part for “Y” – No Arms? CCHMC VAT Master Policy #1: “Common sense and good judgment will be used at all times”
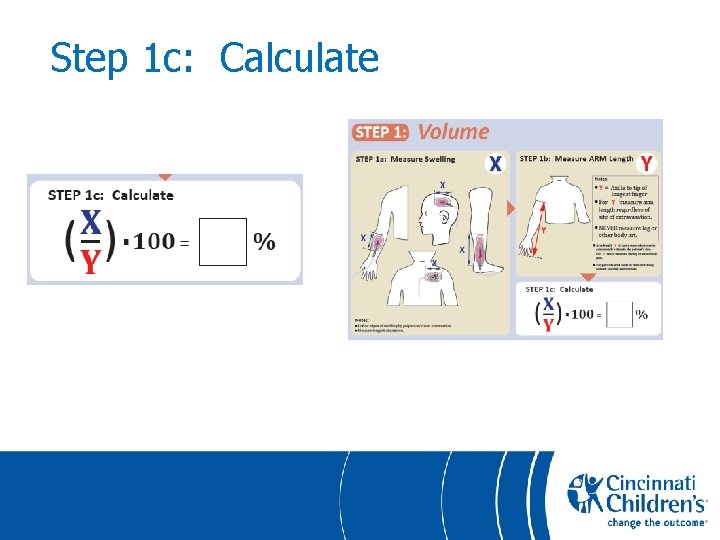
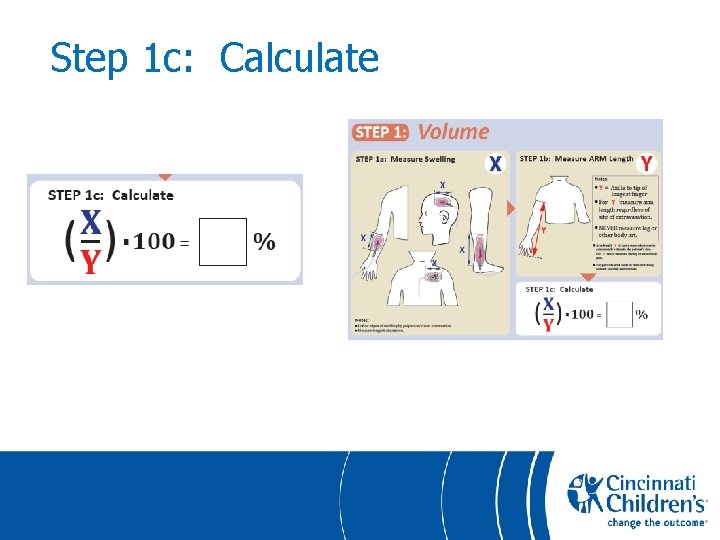
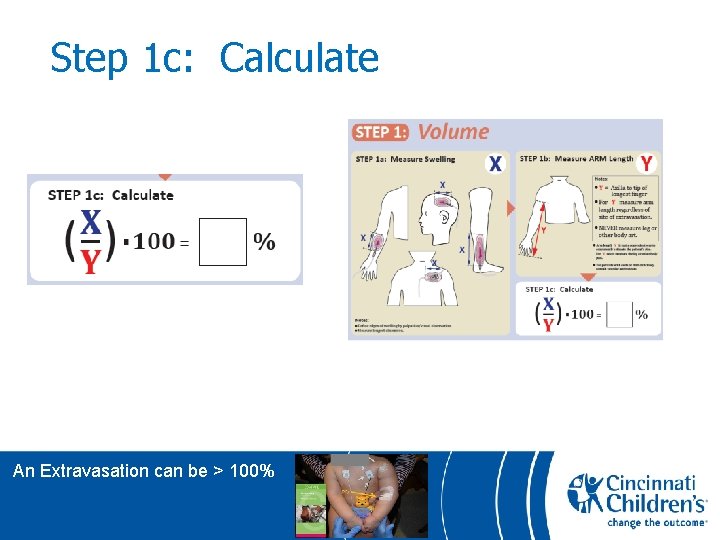
Step 1 c: Calculate
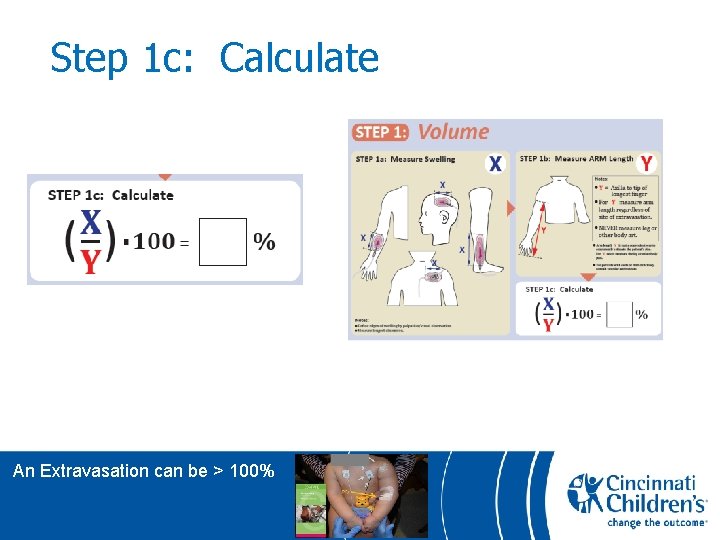
Step 1 c: Calculate An Extravasation can be > 100%
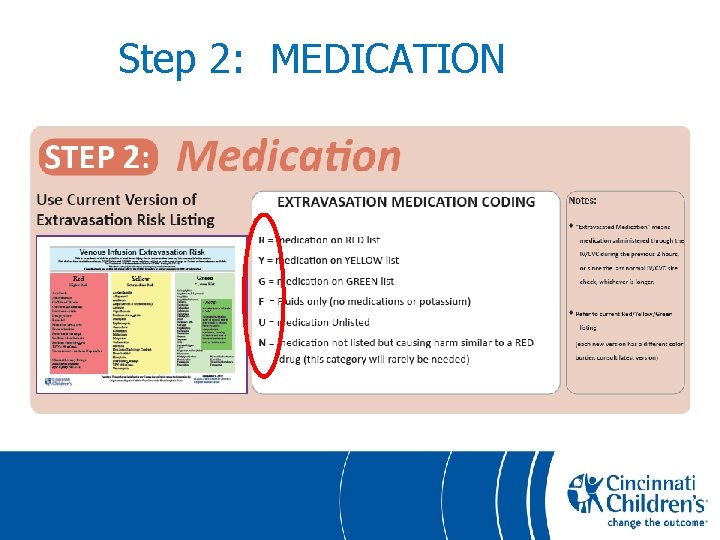
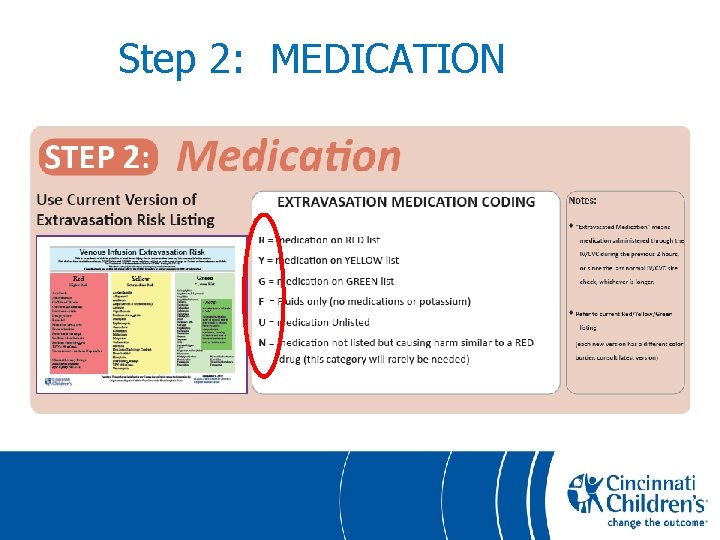
Step 2: MEDICATION
Step 3: DOCUMENT • Other Institutions
Step 3: DOCUMENT • Other Institutions http: //cincinnatichildrens. org/vascularaccess
Implementation • BIG Education Effort – – Julie Stalf, RN Sylvia Rineair, RN Mary Haygood, RN Barb Tofani, RN • CCHMC Education Team • Institution Wide Initiative
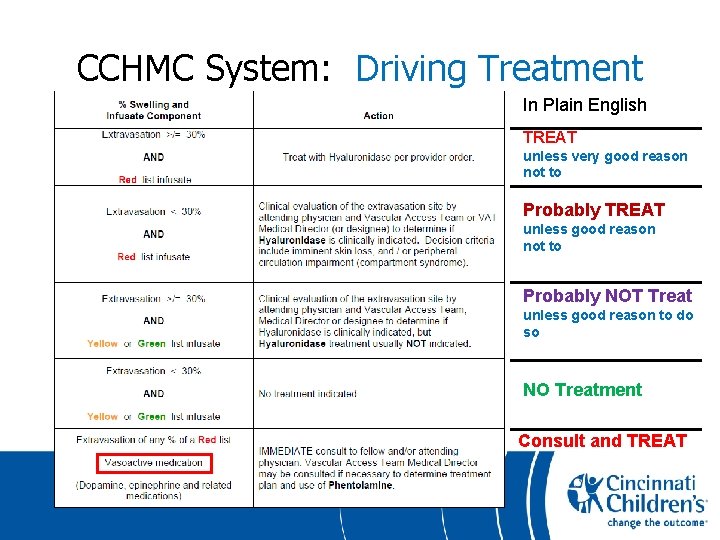
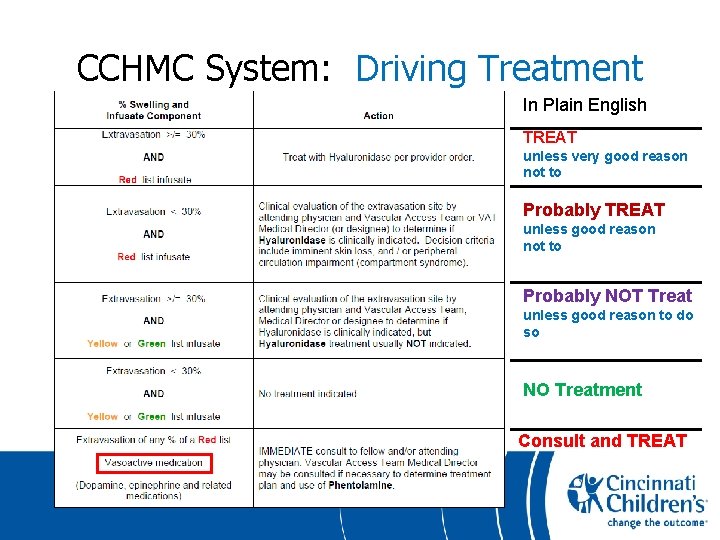
CCHMC System: Driving Treatment In Plain English TREAT unless very good reason not to Probably TREAT unless good reason not to Probably NOT Treat unless good reason to do so NO Treatment Consult and TREAT
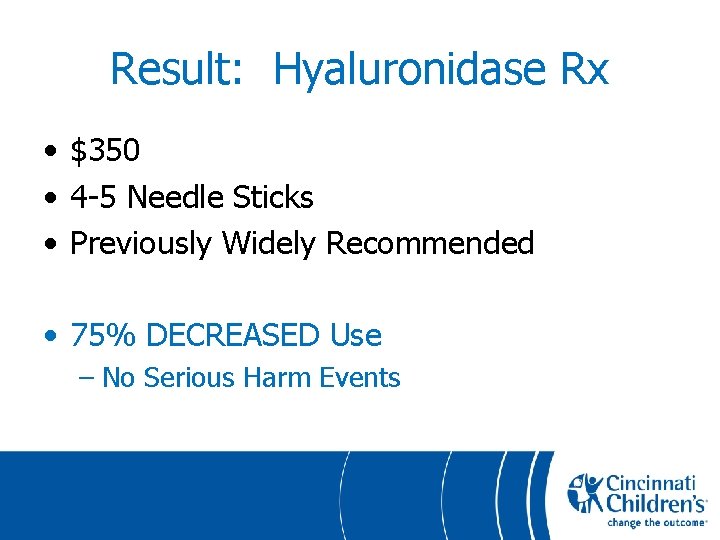
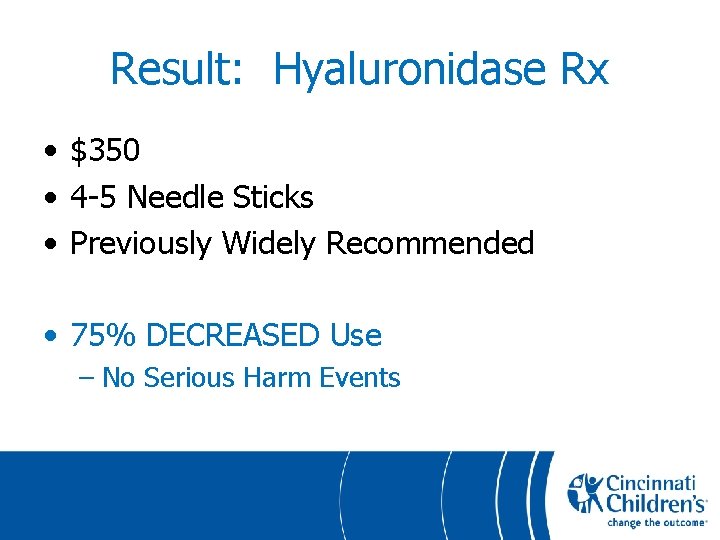
Result: Hyaluronidase Rx • $350 • 4 -5 Needle Sticks • Previously Widely Recommended • 75% DECREASED Use – No Serious Harm Events
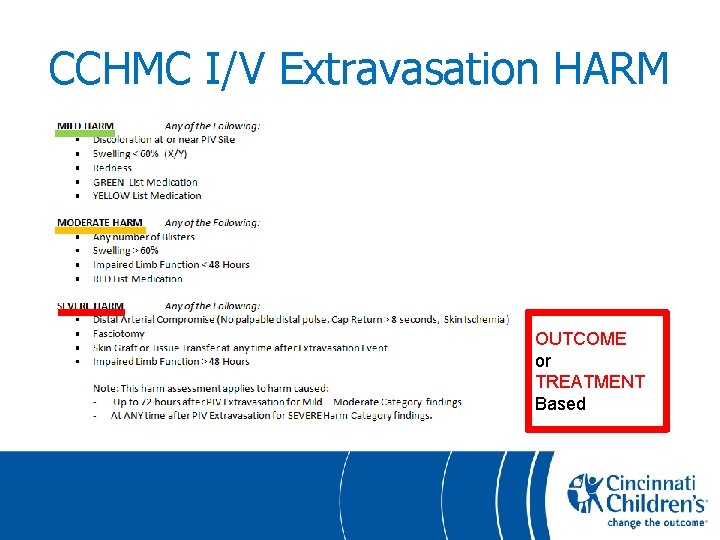
CCHMC I/V Extravasation HARM OUTCOME or TREATMENT Based

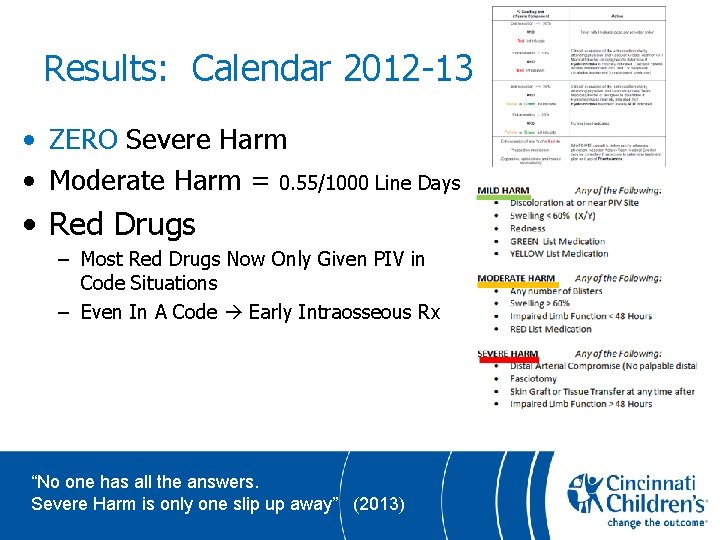
Results: Calendar 2012 -13 • ZERO Severe Harm • Moderate Harm = 0. 55/1000 Line Days • Red Drugs – Most Red Drugs Now Only Given PIV in Code Situations – Even In A Code Early Intraosseous Rx
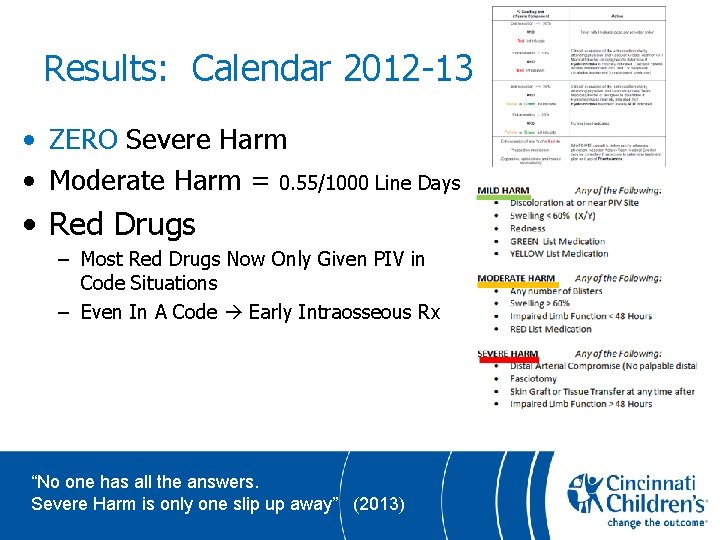
Results: Calendar 2012 -13 • ZERO Severe Harm • Moderate Harm = 0. 55/1000 Line Days • Red Drugs – Most Red Drugs Now Only Given PIV in Code Situations – Even In A Code Early Intraosseous Rx “No one has all the answers. Severe Harm is only one slip up away” (2013)
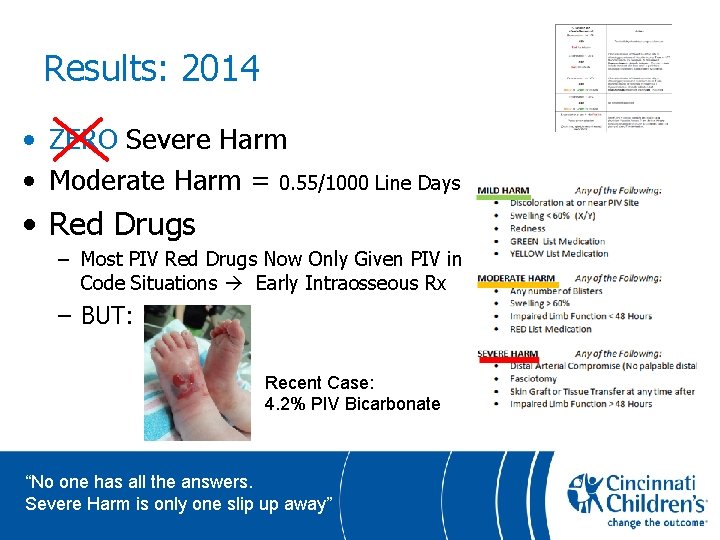
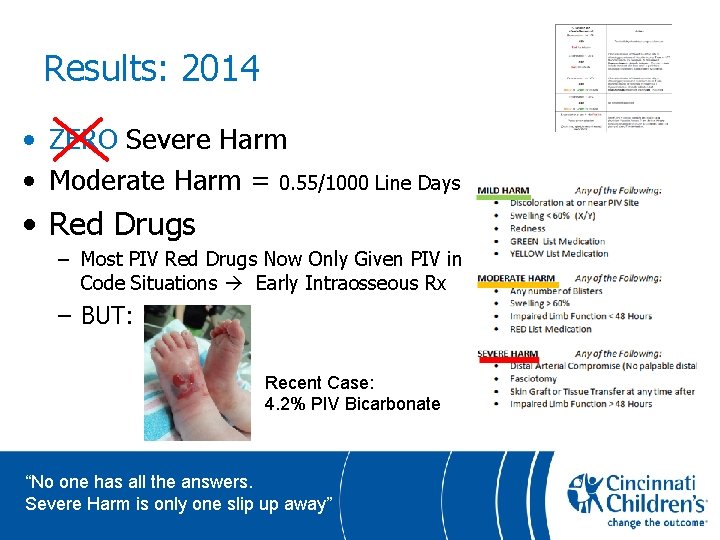
Results: 2014 • ZERO Severe Harm • Moderate Harm = 0. 55/1000 Line Days • Red Drugs – Most PIV Red Drugs Now Only Given PIV in Code Situations Early Intraosseous Rx – BUT: Recent Case: 4. 2% PIV Bicarbonate “No one has all the answers. Severe Harm is only one slip up away”
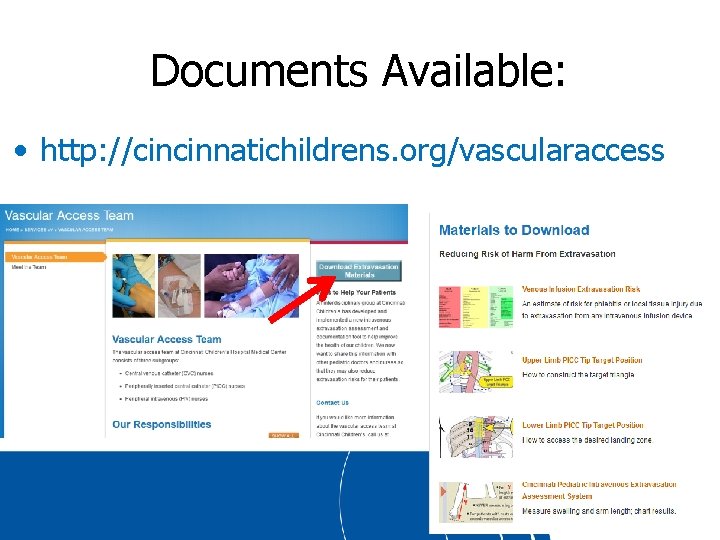
Documents Available: • http: //cincinnatichildrens. org/vascularaccess
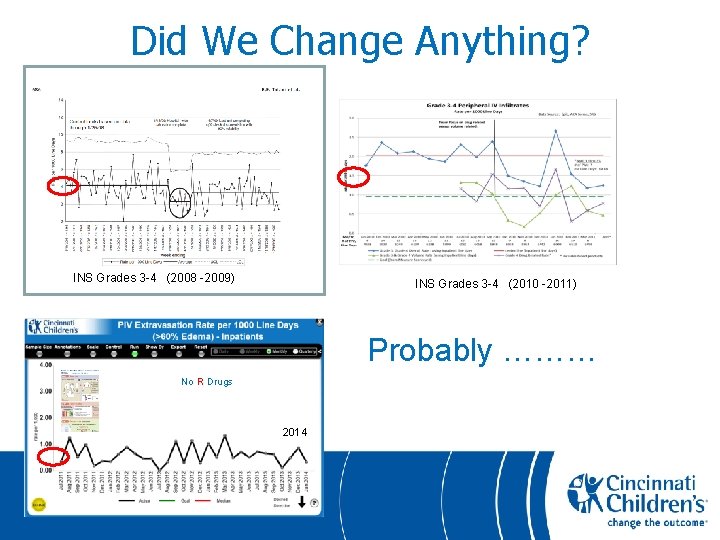
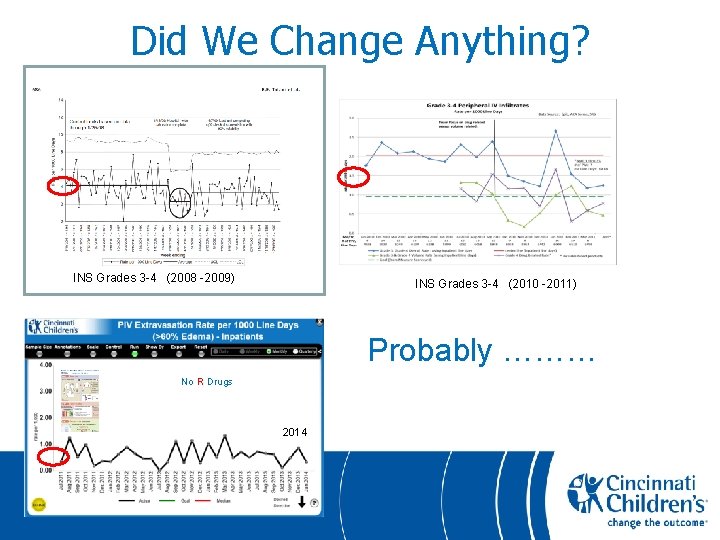
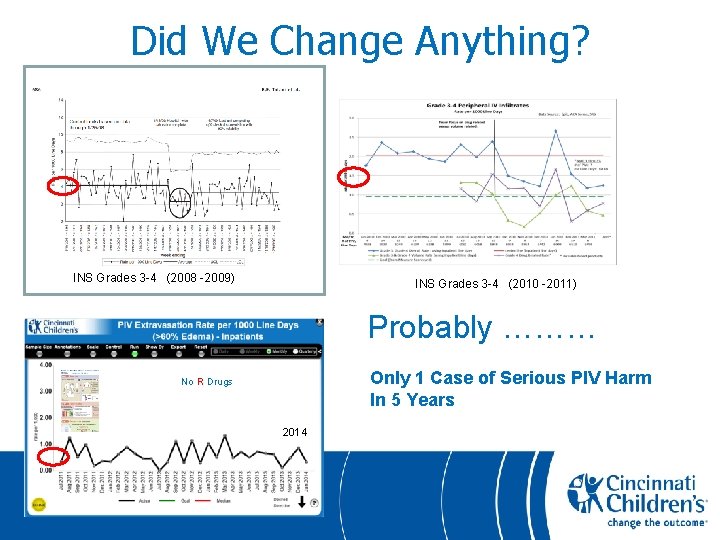
Did We Change Anything? INS Grades 3 -4 (2008 -2009) INS Grades 3 -4 (2010 -2011) Probably ……… No R Drugs 2014
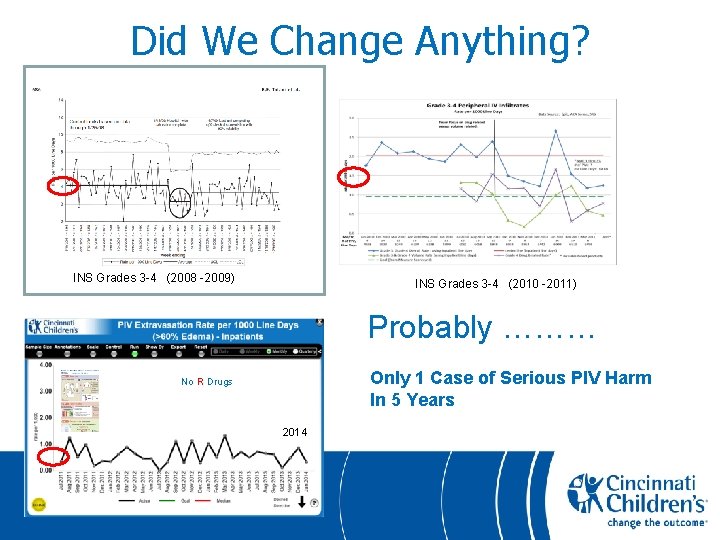
Did We Change Anything? INS Grades 3 -4 (2008 -2009) INS Grades 3 -4 (2010 -2011) Probably ……… Only 1 Case of Serious PIV Harm In 5 Years No R Drugs 2014
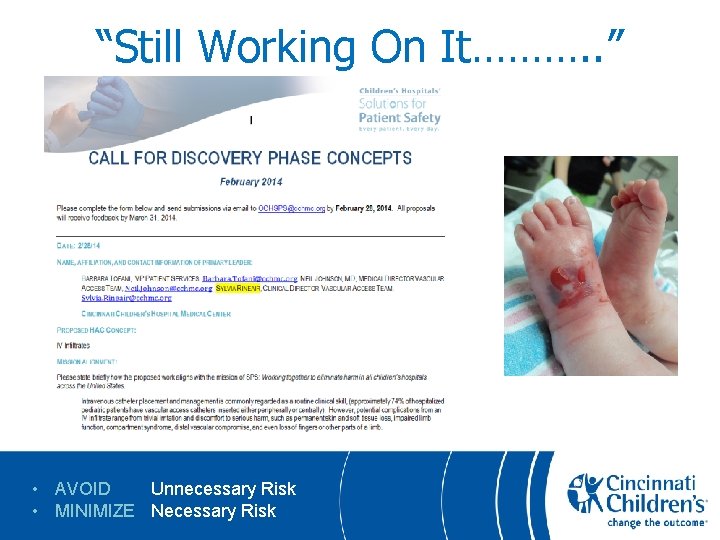
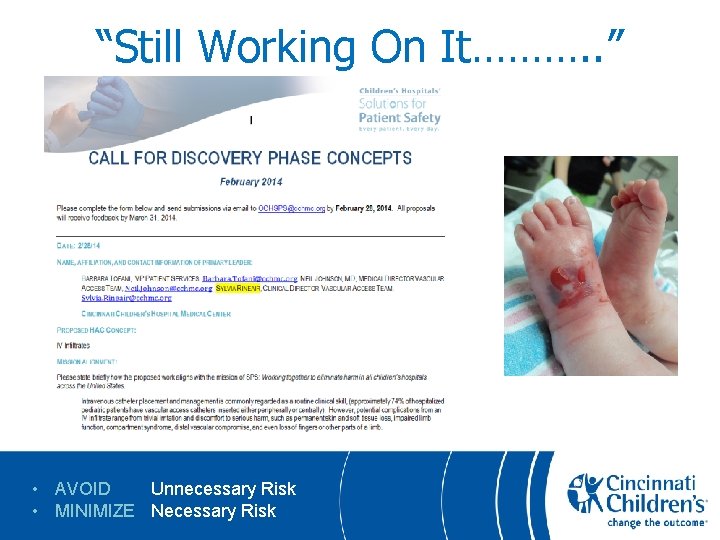
“Still Working On It………. . ” • AVOID Unnecessary Risk • MINIMIZE Necessary Risk
Summary • Overview: – 4 Year IV Extravasation Harm Reduction: • Most Effort is Culture Change / Leadership • Hard Work: MD / Nursing / Administration Silos are SOLID • Our 4 Components – – Reliable Hourly Bedside PIV Checks Evidence Based 3 Tier Medication Tissue Toxicity List “No Grade” 2 Component Assessment / Documentation Tool Real Cross-Cultural Leadership
Thanks • • • i. VAG (Our Governance Group) The Whole Extraordinary CCHMC VAT Team “r. VAG” Dallas Children’s Vascular Access Team John Racadio MD – • • • “Why Don’t You Just Abolish Grading ? ? ? ” Glen Minano – Graphics Marshall Ashby Quality Improvement Consultant Steve Muething MD – Vice President of Safety, CCHMC Manuscript In Preparation:
Thanks • • i. VAG (Our Governance Group) The Whole Extraordinary CCHMC VAT Team Dallas Children’s Vascular Access Team John Racadio MD – • • • “Why Don’t You Just Abolish Grading ? ? ? ” Glen Minano – Graphics Marshall Ashby Quality Improvement Consultant Steve Muething MD – Vice President of Safety, CCHMC What would we do for our own children ?
Preventing Pediatric Intravenous Extravasation Injuries • Questions – Discussion …….
 Chapter 14:1 using body mechanics
Chapter 14:1 using body mechanics Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Chapter 4 preventing injuries through fitness
Chapter 4 preventing injuries through fitness Preventing hand injuries
Preventing hand injuries Neil johnson md
Neil johnson md Line & catheter label - intravenous burette
Line & catheter label - intravenous burette Medication administration 4 pretest
Medication administration 4 pretest Line & catheter label - intravenous burette
Line & catheter label - intravenous burette Concepts of medication administration pretest
Concepts of medication administration pretest Cannula colour coding
Cannula colour coding Intravenous combining vowel
Intravenous combining vowel Intravenous cannulation ppt
Intravenous cannulation ppt Iv cannula labelling
Iv cannula labelling Phlebitis vs infiltration
Phlebitis vs infiltration Piggyback administration
Piggyback administration Johnson and johnson organizational structure
Johnson and johnson organizational structure Dreikurs classroom management theory
Dreikurs classroom management theory Johnson and johnson bcg matrix
Johnson and johnson bcg matrix Johnson and johnson botnet infections
Johnson and johnson botnet infections Johnson and johnson md&d
Johnson and johnson md&d Laurie johnson brad johnson
Laurie johnson brad johnson Johnson & johnson swot
Johnson & johnson swot Johnson and johnson values
Johnson and johnson values Jjeds johnson and johnson
Jjeds johnson and johnson Johnson & johnson swot
Johnson & johnson swot Work comp puncture
Work comp puncture Chapter 20 preventing kitchen accidents
Chapter 20 preventing kitchen accidents Initiatives aimed at preventing discrimination
Initiatives aimed at preventing discrimination Preventing ageing unequally
Preventing ageing unequally Chapter 16 preventing infection
Chapter 16 preventing infection Chapter 9 resolving conflicts and preventing violence
Chapter 9 resolving conflicts and preventing violence Which is mainly responsible for preventing erosion
Which is mainly responsible for preventing erosion Chapter 24 lesson 2 preventing and treating stds
Chapter 24 lesson 2 preventing and treating stds Preventing kitchen accidents worksheet
Preventing kitchen accidents worksheet Chapter 15 preventing infection
Chapter 15 preventing infection Chapter 9 lesson 2 resolving conflicts
Chapter 9 lesson 2 resolving conflicts Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries How to protect yourself from intentional injuries
How to protect yourself from intentional injuries Tnt swimming
Tnt swimming Westfield sports injuries
Westfield sports injuries Common track injuries
Common track injuries Pa wc bureau
Pa wc bureau Jsp539
Jsp539 Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Chapter 14 bleeding shock and soft tissue injuries
Chapter 14 bleeding shock and soft tissue injuries Unit 15:1 providing first aid
Unit 15:1 providing first aid Sports injuries angus, on
Sports injuries angus, on Bo taoshi injuries
Bo taoshi injuries Moulage recipes
Moulage recipes Uc davis web scheduler
Uc davis web scheduler Stobhill miu
Stobhill miu Chapter 21 hunger games questions and answers
Chapter 21 hunger games questions and answers Deadly dozen chest injuries
Deadly dozen chest injuries Injuries first aid
Injuries first aid Chapter 12 lesson 3 planning a personal activity program
Chapter 12 lesson 3 planning a personal activity program Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region Hunger games chapter 21 questions and answers
Hunger games chapter 21 questions and answers Biomechanics of throwing a football
Biomechanics of throwing a football Miniscus replacement
Miniscus replacement Intentional fallacy examples
Intentional fallacy examples An epidemiologic survey of roller skating injuries
An epidemiologic survey of roller skating injuries Human crutch method first aid
Human crutch method first aid Chapter 17:11 providing first aid for sudden illness
Chapter 17:11 providing first aid for sudden illness How are sports injuries classified and managed
How are sports injuries classified and managed Carl clinton construction
Carl clinton construction Characters of firearm injuries
Characters of firearm injuries Chapter 13 worksheet recognizing different sports injuries
Chapter 13 worksheet recognizing different sports injuries Chapter 11 assessment and evaluation of sports injuries
Chapter 11 assessment and evaluation of sports injuries What are sentinel injuries
What are sentinel injuries Summarize mayella's testimony
Summarize mayella's testimony Injuries first aid
Injuries first aid