Prevent Perioperative Pressure Injury What is a Pressure





- Slides: 42

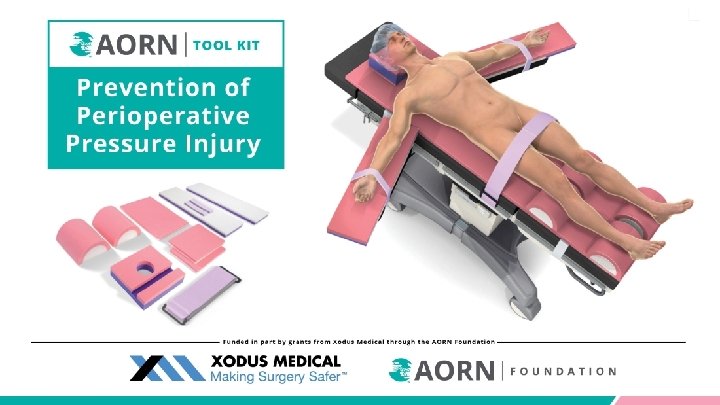
Prevent Perioperative Pressure Injury
What is a Pressure Injury? “A pressure injury is localized damage to skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, comorbid conditions, and condition of the soft tissue. ” Edsberg LE, Black JM, Goldber M, Mc. Nichol L, Moore, L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System. J Wound Ostomy Continence Nurs. 2016; 43(6): 585– 597. https: //journals. lww. com/jwocnonline/Fulltext/2016/11000/Revised_National_Pressure_Ulcer_Advisory_Panel. 3. aspx
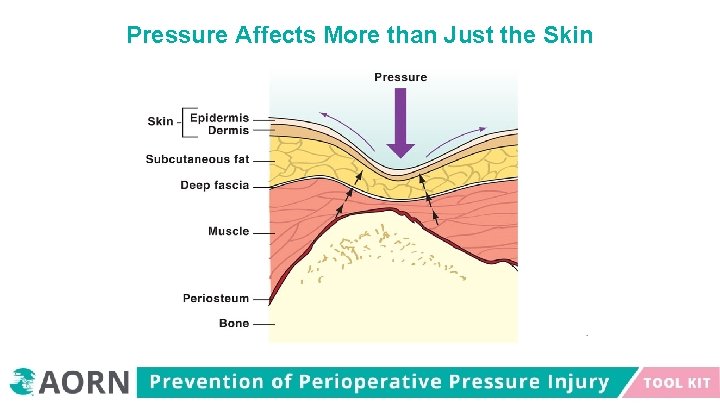
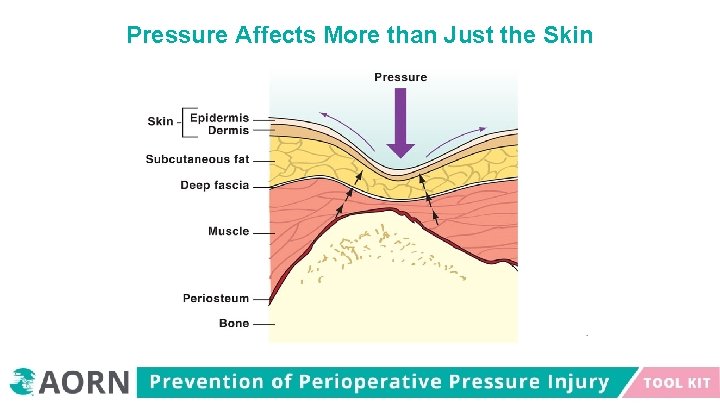
Pressure Affects More than Just the Skin
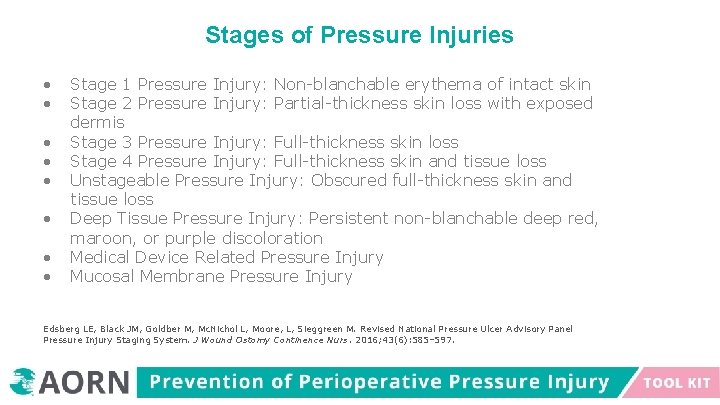
Stages of Pressure Injuries Stage 1 Pressure Injury: Non-blanchable erythema of intact skin Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis Stage 3 Pressure Injury: Full-thickness skin loss Stage 4 Pressure Injury: Full-thickness skin and tissue loss Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss Deep Tissue Pressure Injury: Persistent non-blanchable deep red, maroon, or purple discoloration Medical Device Related Pressure Injury Mucosal Membrane Pressure Injury Edsberg LE, Black JM, Goldber M, Mc. Nichol L, Moore, L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System. J Wound Ostomy Continence Nurs. 2016; 43(6): 585– 597.
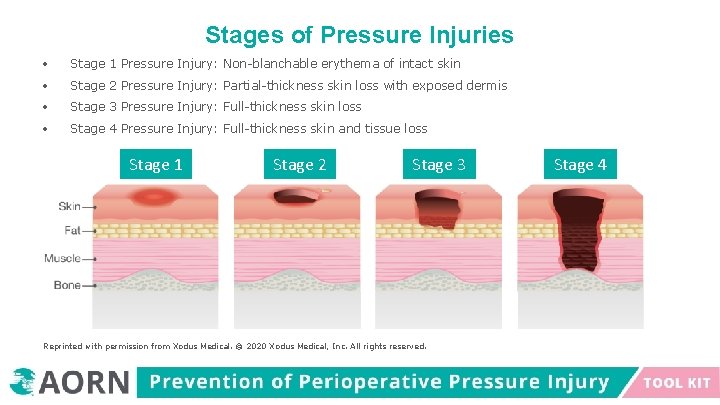
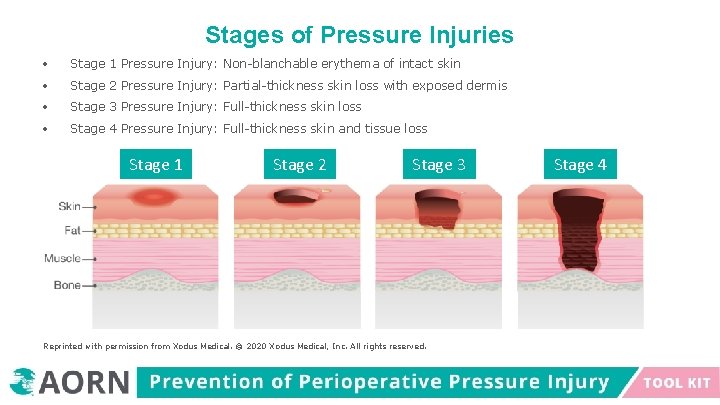
Stages of Pressure Injuries Stage 1 Pressure Injury: Non-blanchable erythema of intact skin Stage 2 Pressure Injury: Partial-thickness skin loss with exposed dermis Stage 3 Pressure Injury: Full-thickness skin loss Stage 4 Pressure Injury: Full-thickness skin and tissue loss Stage 1 Stage 2 Stage 3 Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved. Stage 4
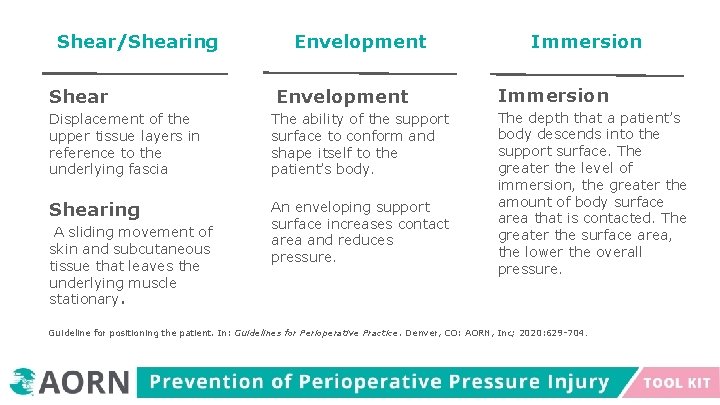
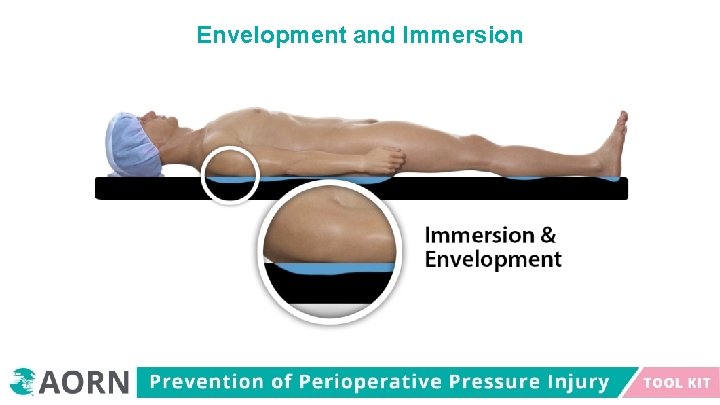
Shear/Shearing Shear Envelopment Displacement of the upper tissue layers in reference to the underlying fascia The ability of the support surface to conform and shape itself to the patient’s body. Shearing An enveloping support surface increases contact area and reduces pressure. A sliding movement of skin and subcutaneous tissue that leaves the underlying muscle stationary. Immersion The depth that a patient’s body descends into the support surface. The greater the level of immersion, the greater the amount of body surface area that is contacted. The greater the surface area, the lower the overall pressure. Guideline for positioning the patient. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2020: 629 -704.
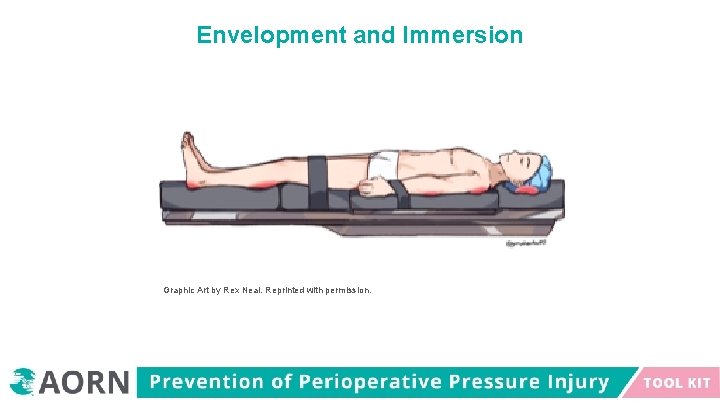
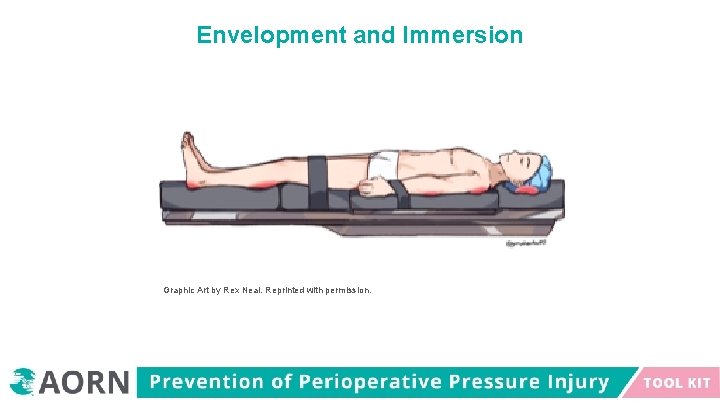
Envelopment and Immersion Graphic Art by Rex Neal. Reprinted with permission.
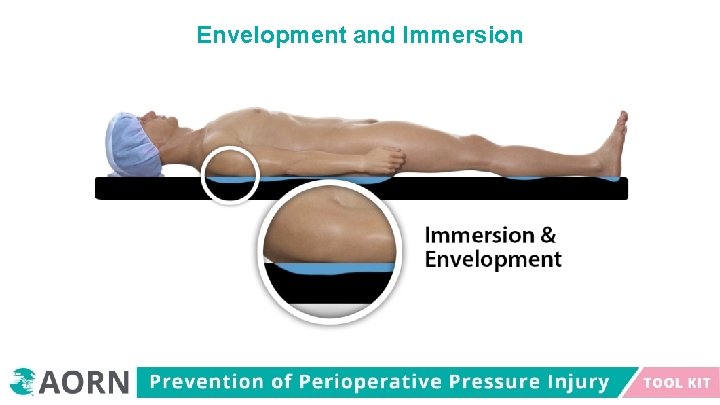
Envelopment and Immersion
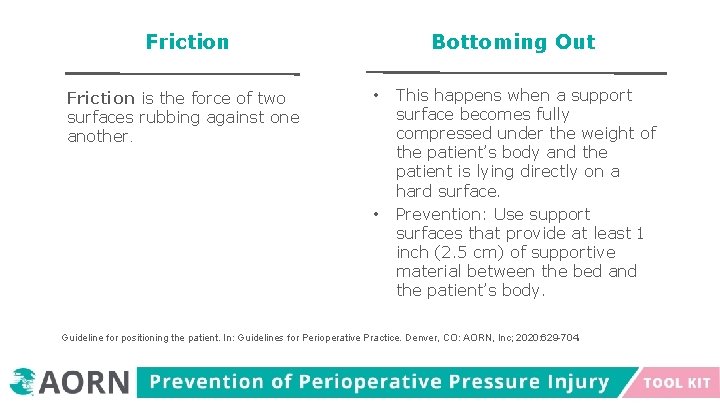
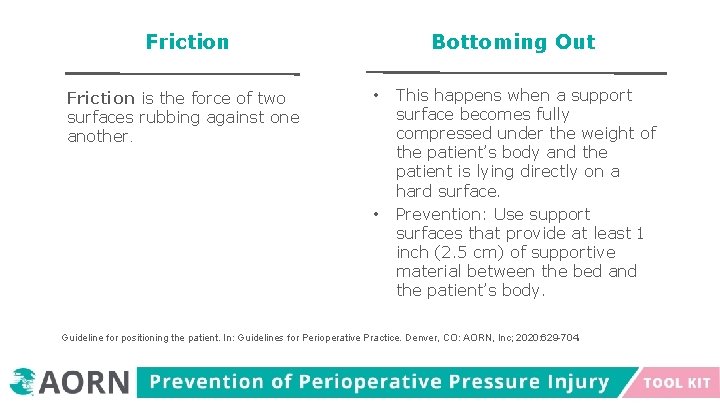
Friction is the force of two surfaces rubbing against one another. Bottoming Out • • This happens when a support surface becomes fully compressed under the weight of the patient’s body and the patient is lying directly on a hard surface. Prevention: Use support surfaces that provide at least 1 inch (2. 5 cm) of supportive material between the bed and the patient’s body. . Guideline for positioning the patient. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2020: 629 -704

Pressure, Shearing, Friction Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
Hospital-Acquired Pressure Injury (HAPI) This is a localized injury to the skin and/or underlying tissue that occurs during an inpatient hospital stay. This type of pressure injury can develop as a result of pressure, shear, or both. HAPI is also associated with other factors: o advanced age, immobility, perfusion, nutritional status, hematological measures, illness severity, and presence of diabetes This type of pressure injury is generally considered preventable, and it is identified as a nursing quality indicator. Rondinelli J, Zuniga S, Kipnis P, Najib Kawar L, Liu V, Escobar GJ. Hospital-acquired pressure injury. Risk-adjusted comparisons in an integrated healthcare delivery. Nurs Res. 2018; 67(1): 16 -25. https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 6013055/
Hospital-Acquired Pressure Injury (HAPI) Stage 3 (full-thickness skin loss) or stage 4 (full-thickness skin and tissue loss) HAPI These are considered a “never event” that should be reported to the Centers for Medicare and Medicaid Services. There may be subsequent limited reimbursement when patients develop HAPI. The development of HAPI can be associated with a longer hospital stay, pain, infection, and even death. Rondinelli J, Zuniga S, Kipnis P, Najib Kawar L, Liu V, Escobar GJ. Hospital-acquired pressure injury. Risk-adjusted comparisons in an integrated healthcare delivery. Nurs Res. 2018; 67(1): 16 -25. https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 6013055/
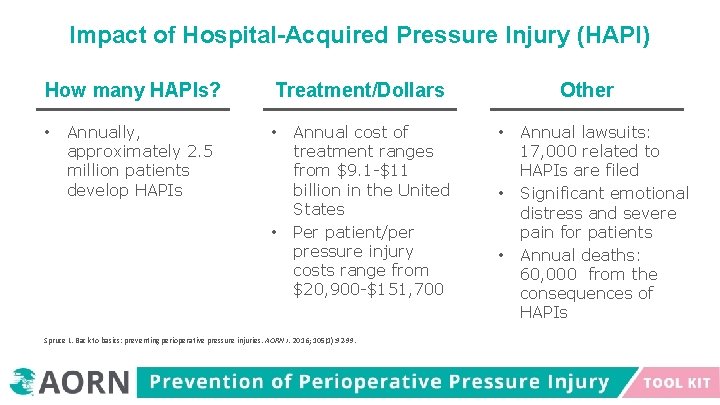
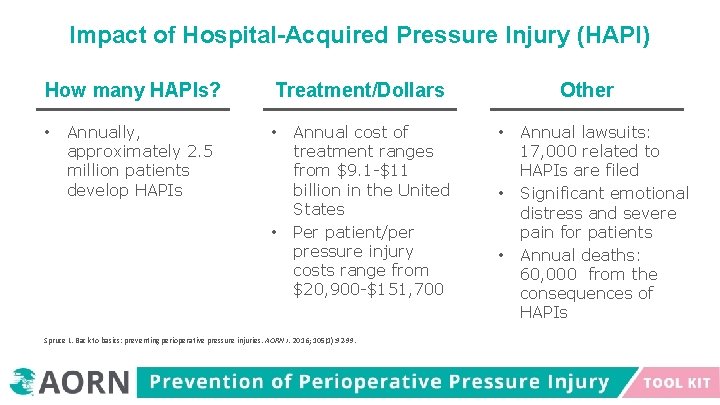
Impact of Hospital-Acquired Pressure Injury (HAPI) How many HAPIs? • Annually, approximately 2. 5 million patients develop HAPIs Treatment/Dollars • • Annual cost of treatment ranges from $9. 1 -$11 billion in the United States Per patient/per pressure injury costs range from $20, 900 -$151, 700 Spruce L. Back to basics: preventing perioperative pressure injuries. AORN J. 2016; 105(1): 92 -99. Other • • • Annual lawsuits: 17, 000 related to HAPIs are filed Significant emotional distress and severe pain for patients Annual deaths: 60, 000 from the consequences of HAPIs
Who is at Risk for Pressure Injury Development? All Surgical Patients Are at Risk for Pressure Injury
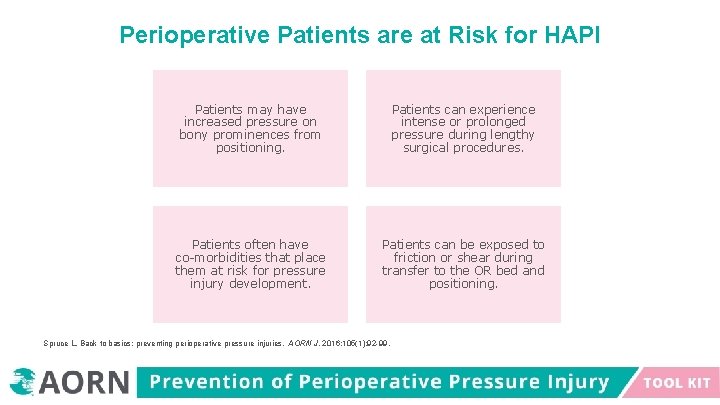
Perioperative Patients are at Risk for HAPI Patients may have increased pressure on bony prominences from positioning. Patients can experience intense or prolonged pressure during lengthy surgical procedures. Patients often have co-morbidities that place them at risk for pressure injury development. Patients can be exposed to friction or shear during transfer to the OR bed and positioning. Spruce L. Back to basics: preventing perioperative pressure injuries. AORN J. 2016; 105(1): 92 -99.
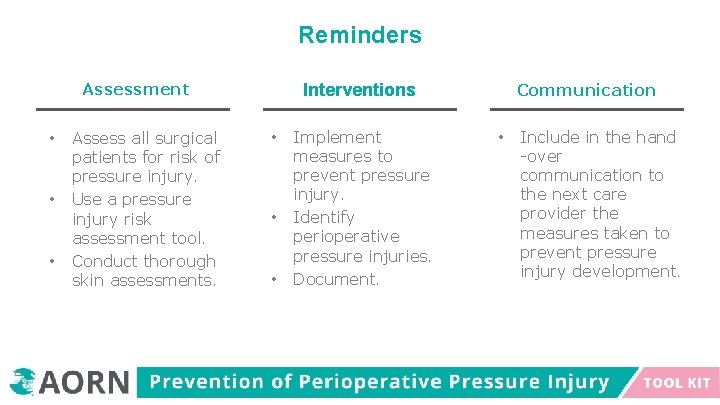
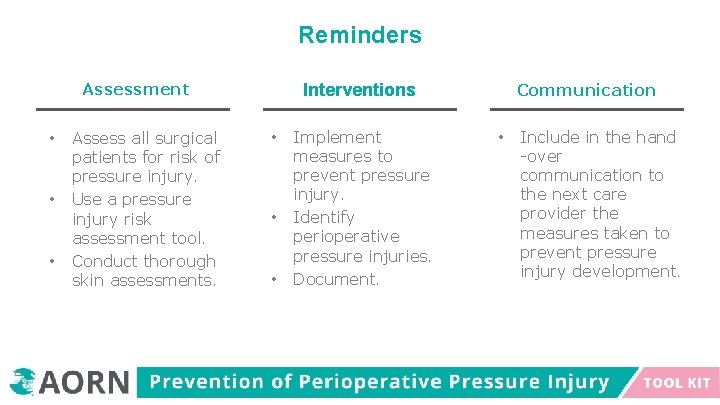
Reminders Assessment • • • Assess all surgical patients for risk of pressure injury. Use a pressure injury risk assessment tool. Conduct thorough skin assessments. Communication Interventions • • • Implement measures to prevent pressure injury. Identify perioperative pressure injuries. Document. • Include in the hand -over communication to the next care provider the measures taken to prevent pressure injury development.
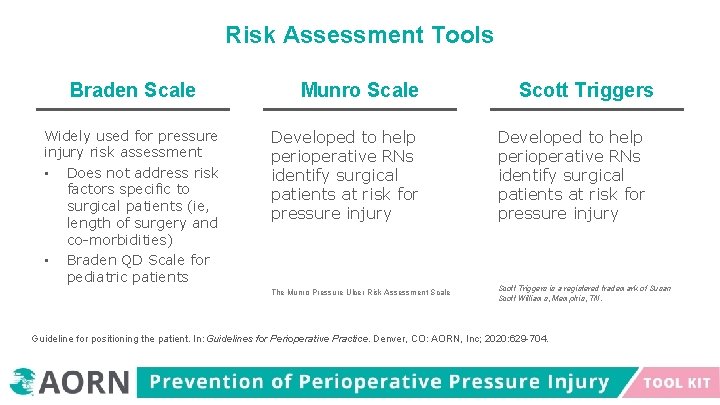
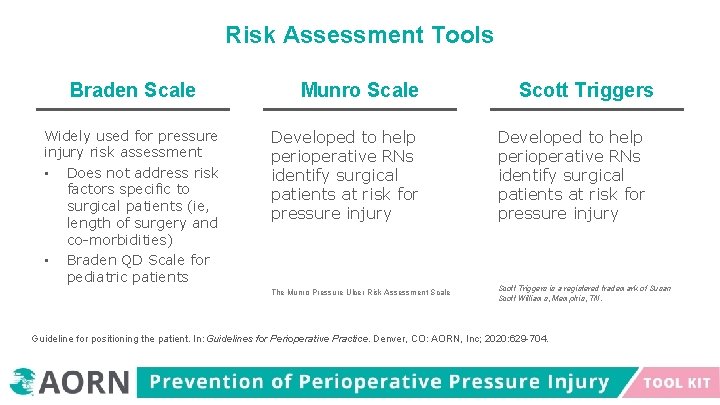
Risk Assessment Tools Braden Scale Widely used for pressure injury risk assessment • Does not address risk factors specific to surgical patients (ie, length of surgery and co-morbidities) • Braden QD Scale for pediatric patients Munro Scale Scott Triggers Developed to help perioperative RNs identify surgical patients at risk for pressure injury The Munro Pressure Ulcer Risk Assessment Scale Scott Triggers is a registered trademark of Susan Scott Williams, Memphis, TN. Guideline for positioning the patient. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2020: 629 -704.

Quality Management Program Quality Improvement Performance Improvement
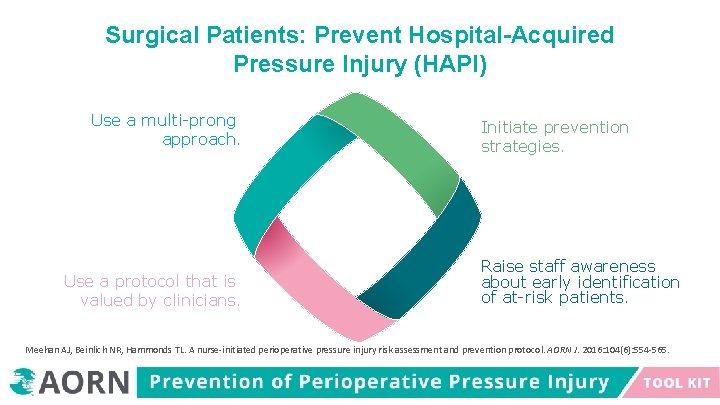
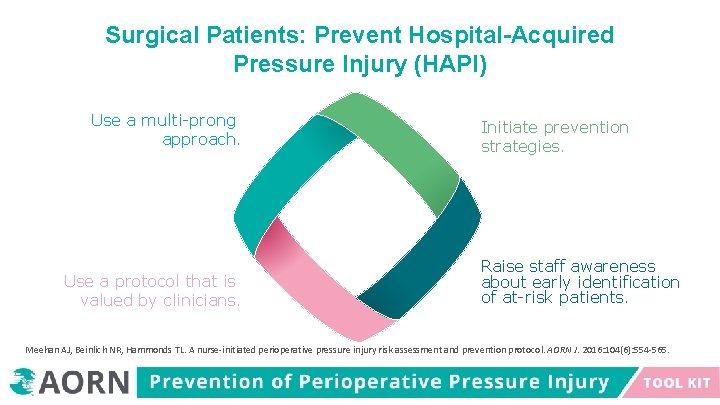
Surgical Patients: Prevent Hospital-Acquired Pressure Injury (HAPI) Use a multi-prong approach. Use a protocol that is valued by clinicians. Initiate prevention strategies. Raise staff awareness about early identification of at-risk patients. Meehan AJ, Beinlich NR, Hammonds TL. A nurse-initiated perioperative pressure injury risk assessment and prevention protocol. AORN J. 2016: 104(6): 554 -565.
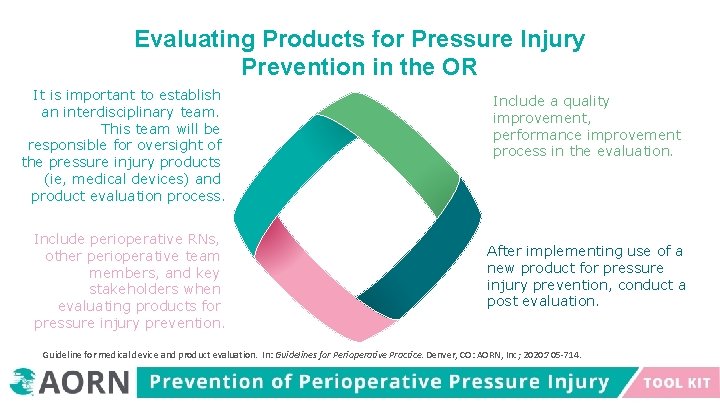
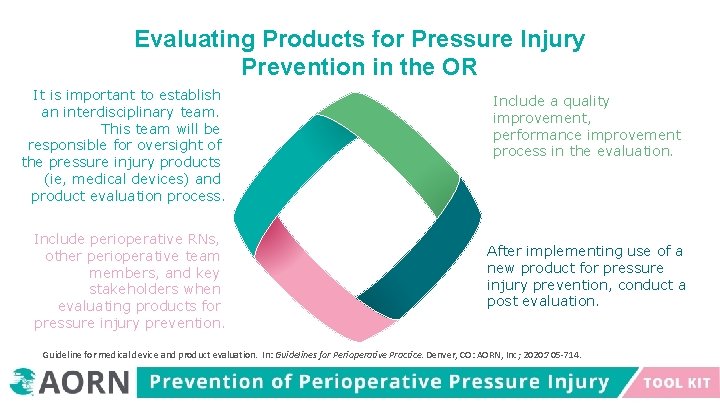
Evaluating Products for Pressure Injury Prevention in the OR It is important to establish an interdisciplinary team. This team will be responsible for oversight of the pressure injury products (ie, medical devices) and product evaluation process. Include perioperative RNs, other perioperative team members, and key stakeholders when evaluating products for pressure injury prevention. Include a quality improvement, performance improvement process in the evaluation. After implementing use of a new product for pressure injury prevention, conduct a post evaluation. Guideline for medical device and product evaluation. In: Guidelines for Perioperative Practice. Denver, CO: AORN, Inc; 2020: 705 -714.
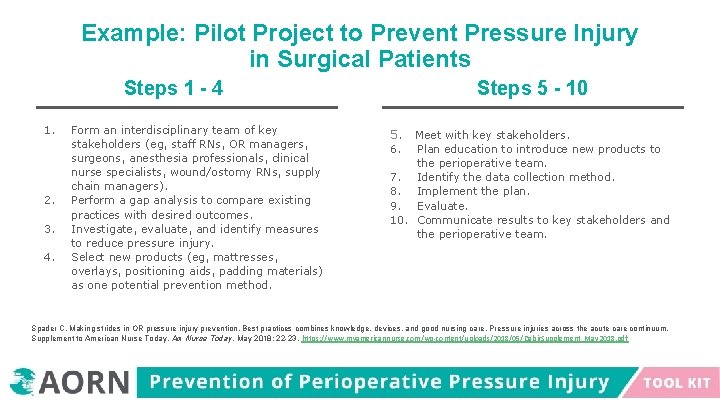
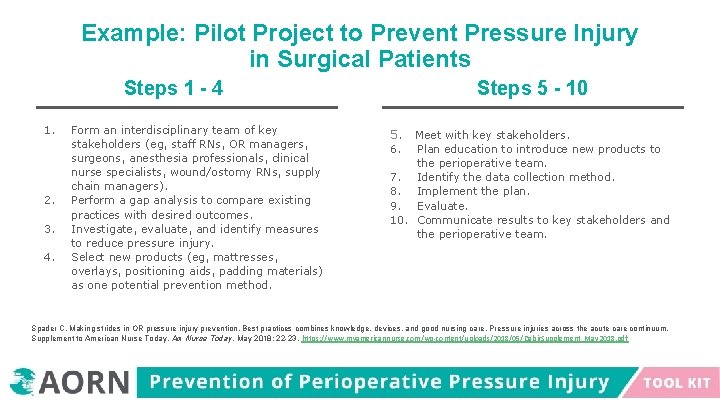
Example: Pilot Project to Prevent Pressure Injury in Surgical Patients Steps 1 - 4 1. 2. 3. 4. Form an interdisciplinary team of key stakeholders (eg, staff RNs, OR managers, surgeons, anesthesia professionals, clinical nurse specialists, wound/ostomy RNs, supply chain managers). Perform a gap analysis to compare existing practices with desired outcomes. Investigate, evaluate, and identify measures to reduce pressure injury. Select new products (eg, mattresses, overlays, positioning aids, padding materials) as one potential prevention method. Steps 5 - 10 5. 6. Meet with key stakeholders. Plan education to introduce new products to the perioperative team. 7. Identify the data collection method. 8. Implement the plan. 9. Evaluate. 10. Communicate results to key stakeholders and the perioperative team. Spader C. Making strides in OR pressure injury prevention. Best practices combines knowledge, devices, and good nursing care. Pressure injuries across the acute care continuum. Supplement to American Nurse Today. Am Nurse Today. May 2018; 22 -23. https: //www. myamericannurse. com/wp-content/uploads/2018/05/Dabir. Supplement_May 2018. pdf
Support Surfaces Protect the Patient Equipment and Purchasing Decisions
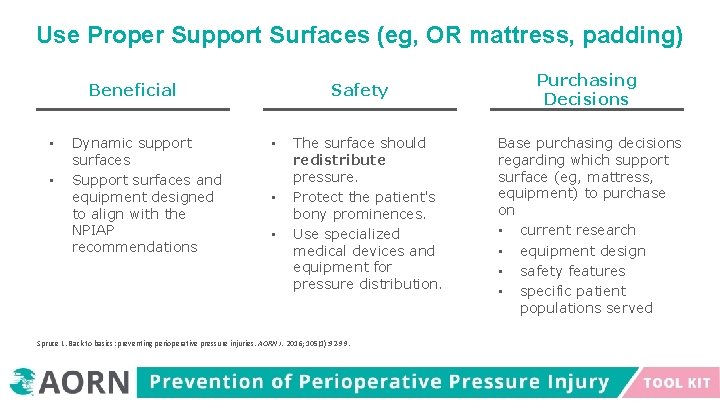
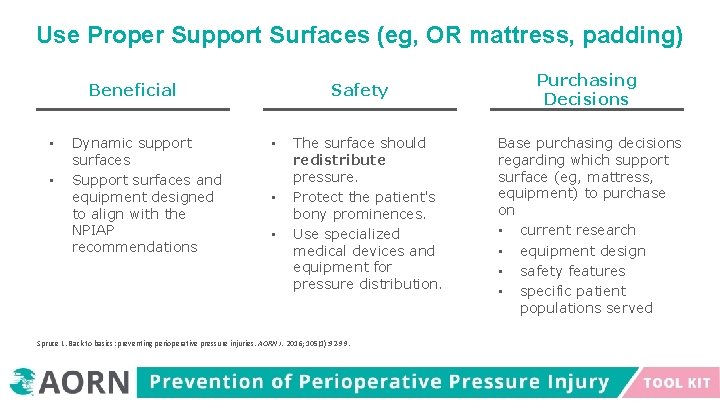
Use Proper Support Surfaces (eg, OR mattress, padding) Beneficial • • Dynamic support surfaces Support surfaces and equipment designed to align with the NPIAP recommendations Safety • • • The surface should redistribute pressure. Protect the patient's bony prominences. Use specialized medical devices and equipment for pressure distribution. Spruce L. Back to basics: preventing perioperative pressure injuries. AORN J. 2016; 105(1): 92 -99. Purchasing Decisions Base purchasing decisions regarding which support surface (eg, mattress, equipment) to purchase on • current research • equipment design • safety features • specific patient populations served
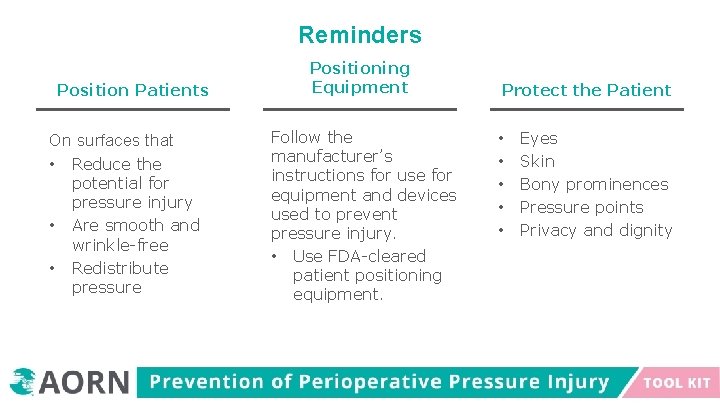
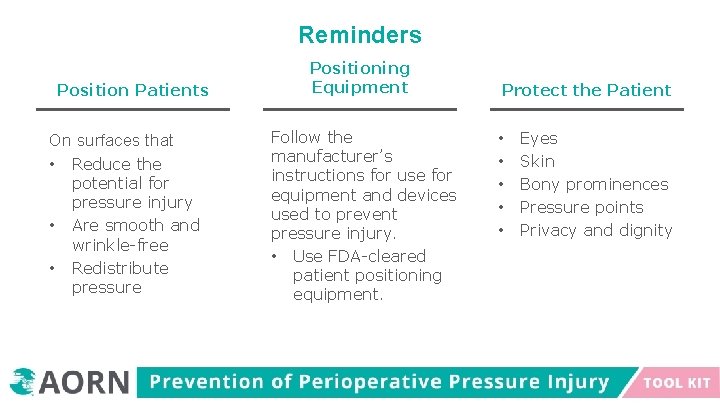
Reminders Position Patients On surfaces that • Reduce the • • potential for pressure injury Are smooth and wrinkle-free Redistribute pressure Positioning Equipment Follow the manufacturer’s instructions for use for equipment and devices used to prevent pressure injury. • Use FDA-cleared patient positioning equipment. Protect the Patient • • • Eyes Skin Bony prominences Pressure points Privacy and dignity
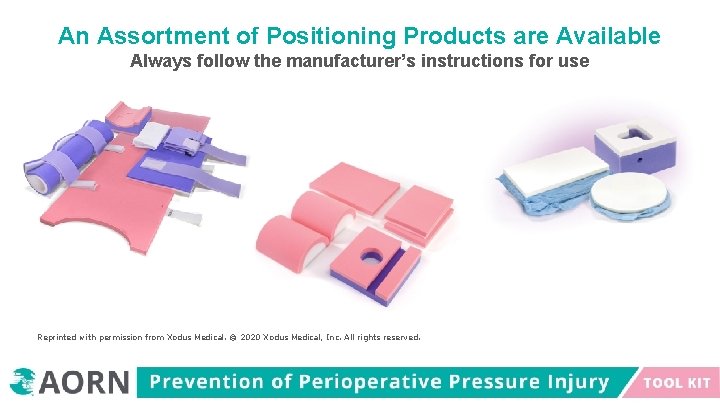
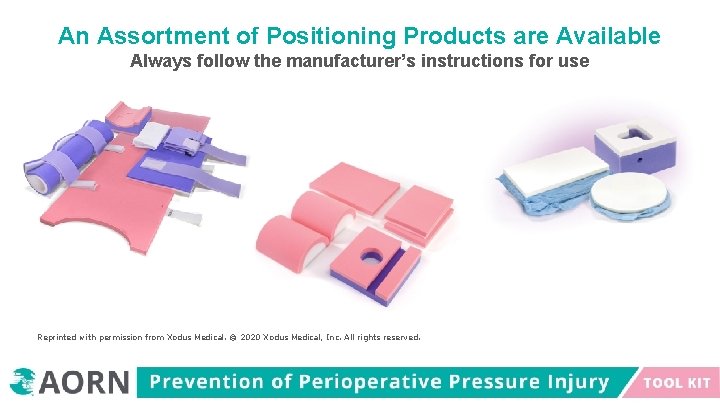
An Assortment of Positioning Products are Available Always follow the manufacturer’s instructions for use Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
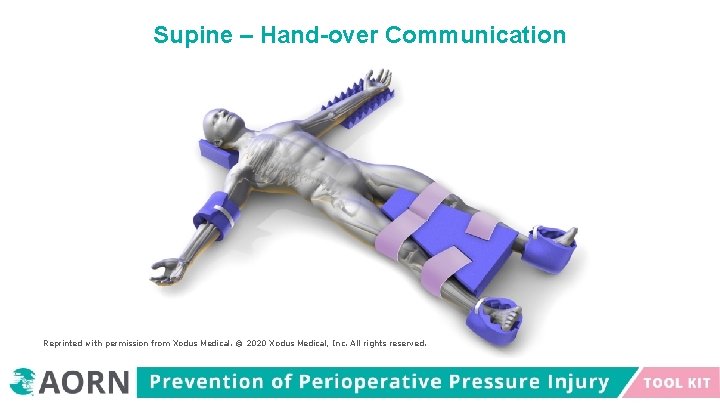
Group Activity – Sample Positioning Images Review images. Review pressure points. Discuss implementation measures to prevent hospitalacquired perioperative pressure injuries.
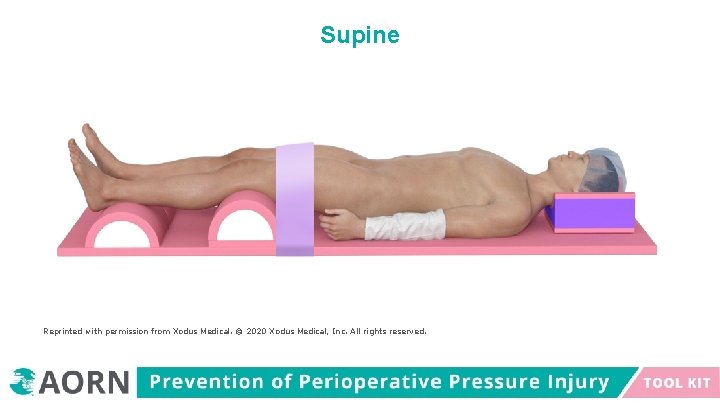
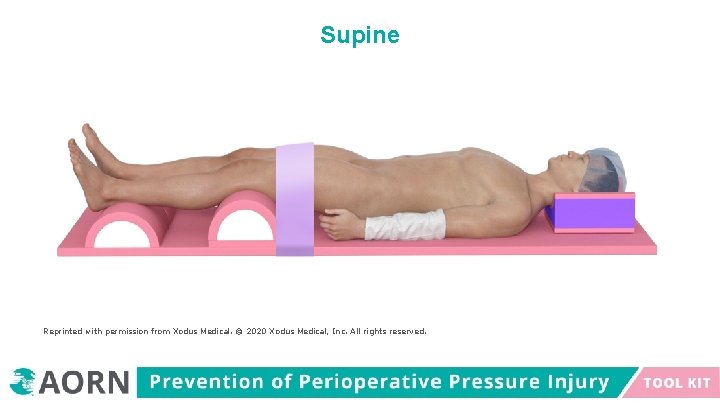
Supine Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
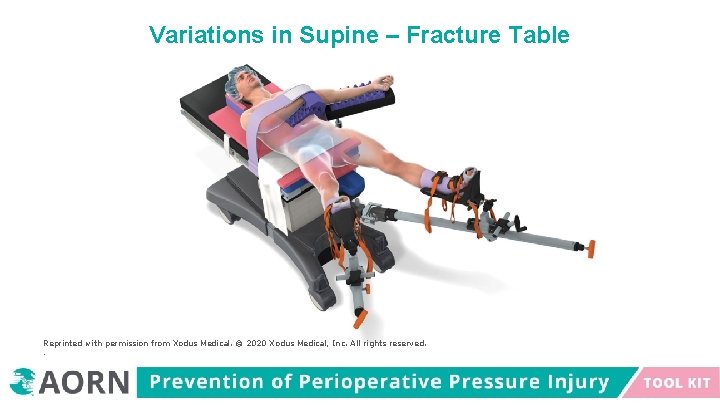
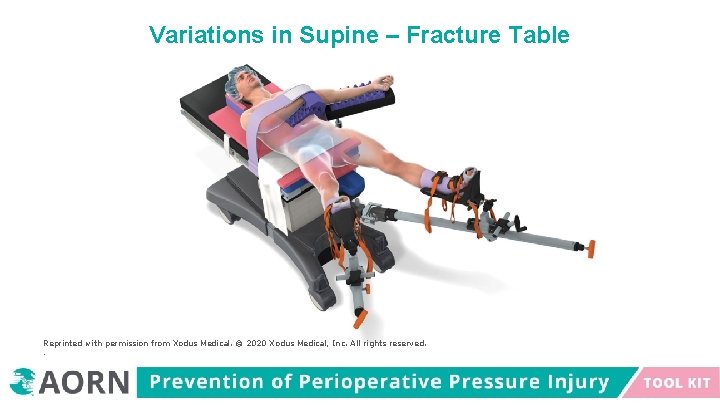
Variations in Supine – Fracture Table Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved. .
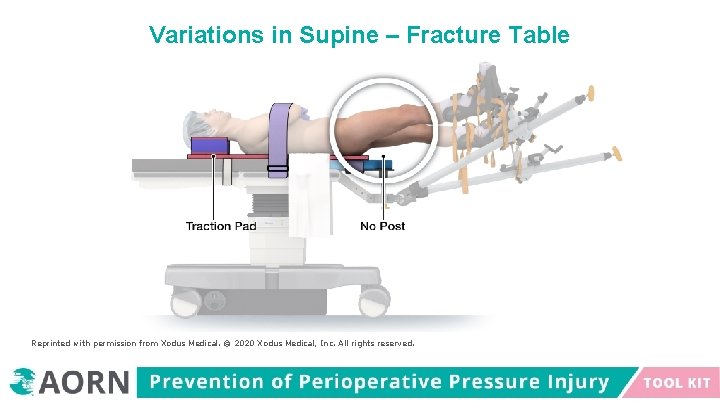
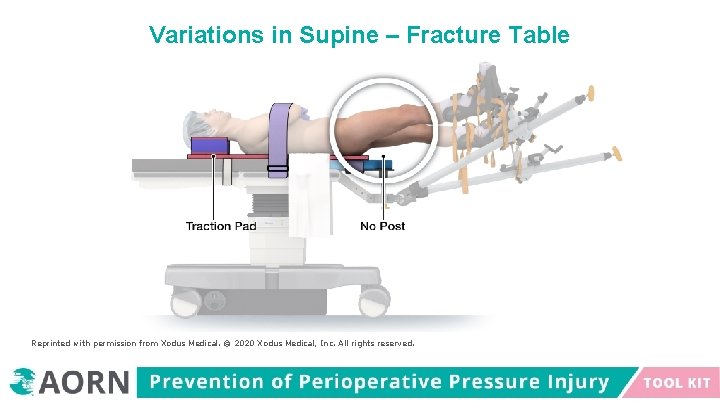
Variations in Supine – Fracture Table Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
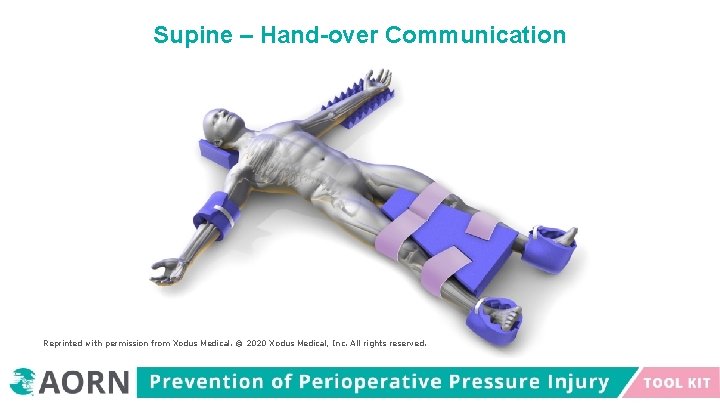
Supine – Hand-over Communication Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.

Trendelenburg Position Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
Trendelenburg Position • The patient’s feet are higher than the patient’s head by 15 to 30 degrees. • Patients who are positioned in the Trendelenburg position for long periods are at risk for postoperative vision loss associated with increased intraocular pressure. • Increased intraocular pressure is directly correlated with the amount of time in Trendelenburg position.
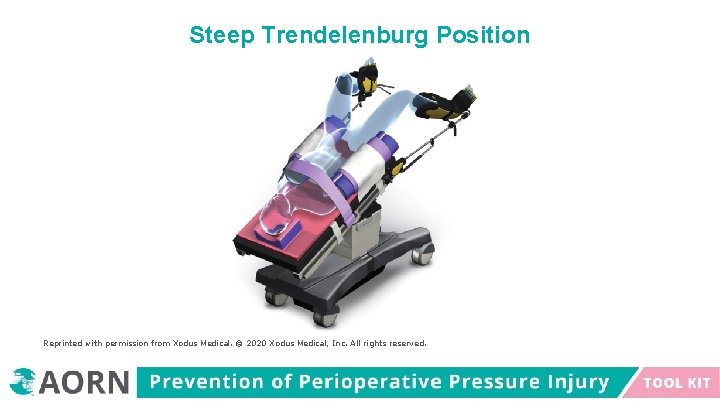
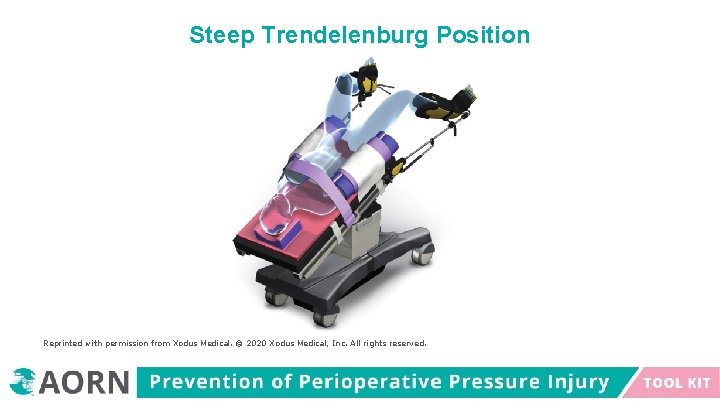
Steep Trendelenburg Position Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
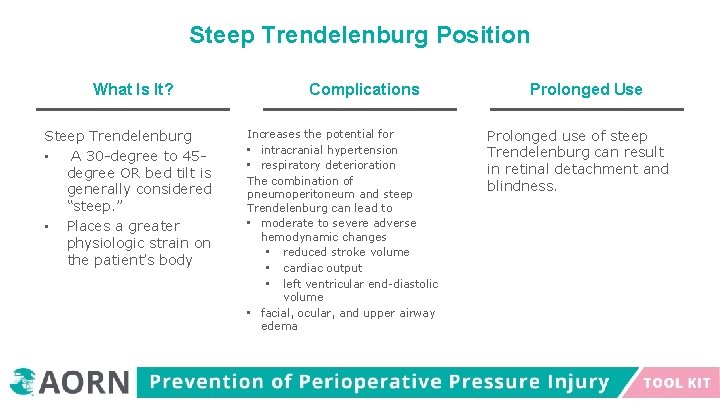
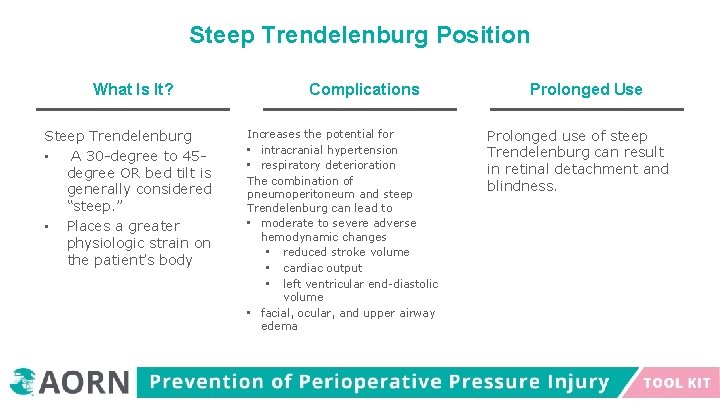
Steep Trendelenburg Position What Is It? Steep Trendelenburg • A 30 -degree to 45 degree OR bed tilt is generally considered “steep. ” • Places a greater physiologic strain on the patient’s body Complications Increases the potential for • intracranial hypertension • respiratory deterioration The combination of pneumoperitoneum and steep Trendelenburg can lead to • moderate to severe adverse hemodynamic changes • reduced stroke volume • cardiac output • left ventricular end-diastolic volume • facial, ocular, and upper airway edema Prolonged Use Prolonged use of steep Trendelenburg can result in retinal detachment and blindness.
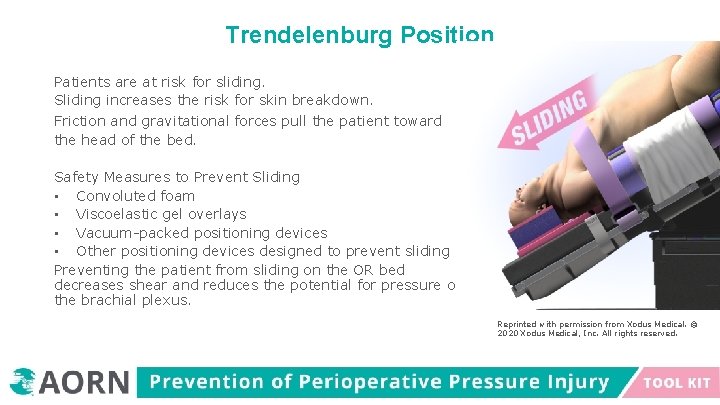
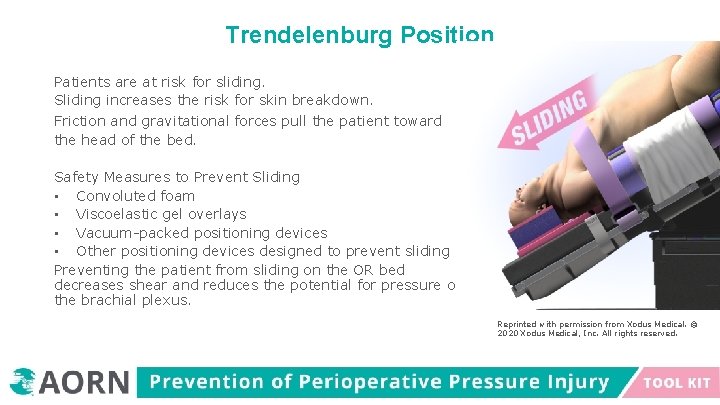
Trendelenburg Position Patients are at risk for sliding. Sliding increases the risk for skin breakdown. Friction and gravitational forces pull the patient toward the head of the bed. Safety Measures to Prevent Sliding • Convoluted foam • Viscoelastic gel overlays • Vacuum-packed positioning devices • Other positioning devices designed to prevent sliding Preventing the patient from sliding on the OR bed decreases shear and reduces the potential for pressure on the brachial plexus. Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
Reverse Trendelenburg Position In the reverse Trendelenburg position, the patient’s head is positioned 15 degrees to 30 degrees higher than the feet.

Variation in Supine – Reverse Trendelenburg Position Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
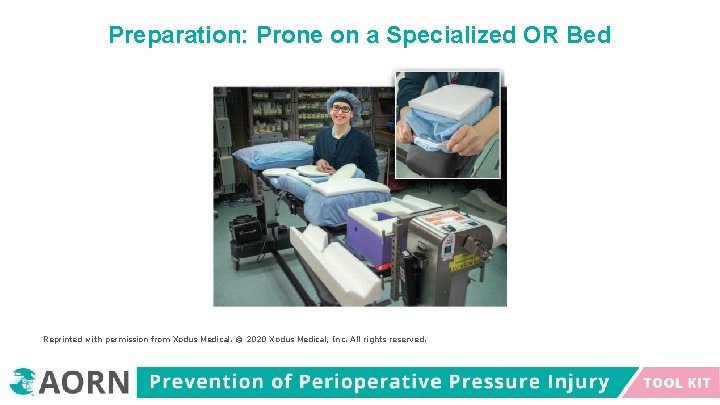
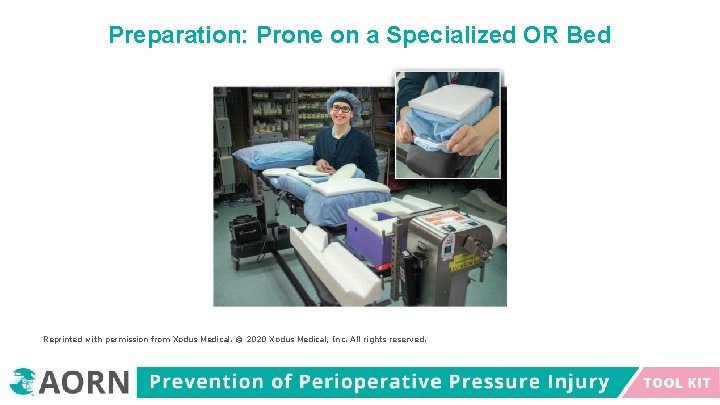
Preparation: Prone on a Specialized OR Bed Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
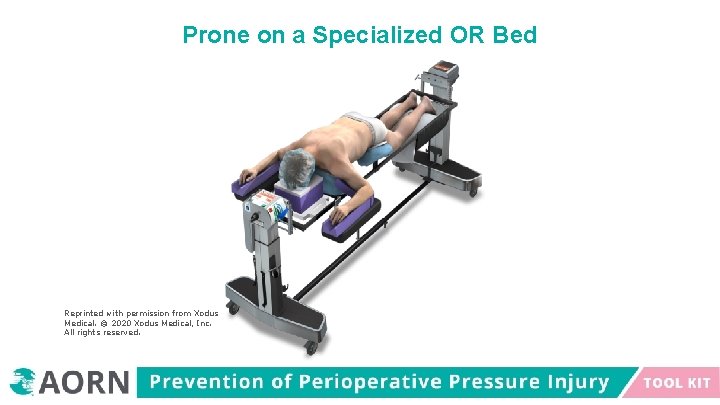
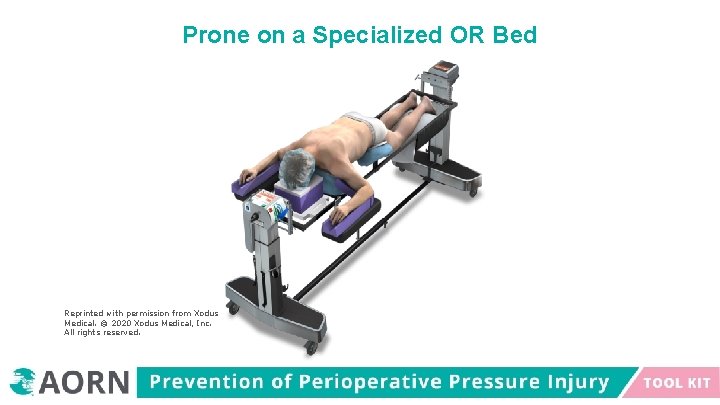
Prone on a Specialized OR Bed Reprinted with permission from Xodus Medical. © 2020 Xodus Medical, Inc. All rights reserved.
Summary • • Individualize each patient’s plan of care to include prevention of pressure injury. All surgical patients are at risk for the development of perioperative pressure injury. Be aware, it is a team effort to prevent a hospital-acquired pressure injury. Participate in or create a prevention of perioperative pressure injury program at your facility.