Prevalence and social structural health and healthcarerelated correlates
![AOR[]: Adjusted odds ratios[95%Confidence Intervals] AOR: 2. 38[1. 26 -4. 48] AOR: 2. 86[1. AOR[]: Adjusted odds ratios[95%Confidence Intervals] AOR: 2. 38[1. 26 -4. 48] AOR: 2. 86[1.](https://slidetodoc.com/presentation_image_h/30fa328b917fdc9b916aebf9f6f16112/image-7.jpg)

- Slides: 11
Prevalence and social, structural, health- and healthcare-related correlates of HIV stigma among women living with HIV in Metro Vancouver, Canada Kathleen N. Deering; Carmen Logie; Andrea Krüsi; Flo Ranville; Melissa Braschel; Putu Duff; Kate Shannon
Conflict of interest statement I have no conflicts of interest to disclose
We would like to acknowledge the expertise and invaluable contributions of our study participants to the work presented today.
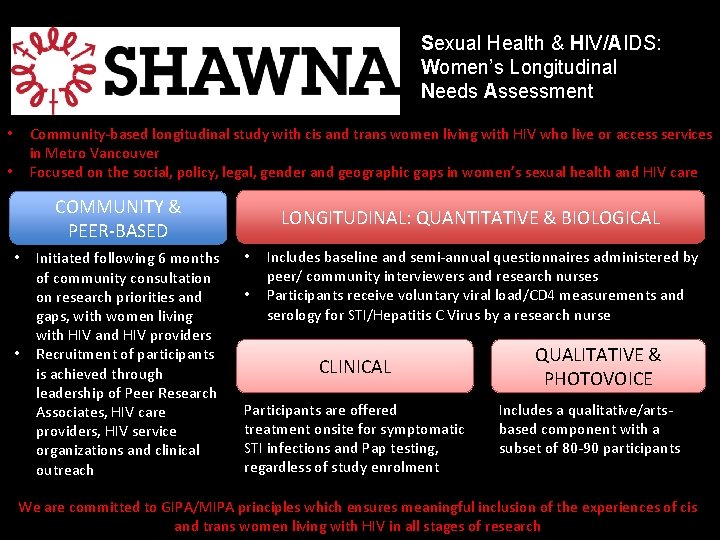
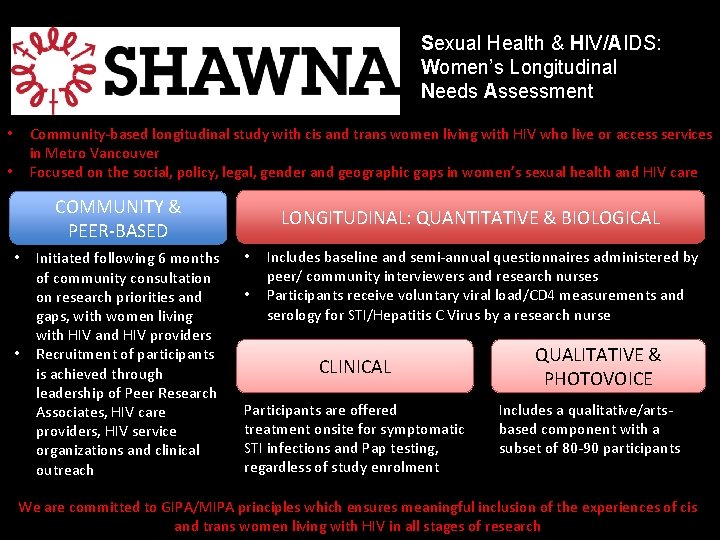
Sexual Health & HIV/AIDS: Women’s Longitudinal Needs Assessment Community-based longitudinal study with cis and trans women living with HIV who live or access services in Metro Vancouver Focused on the social, policy, legal, gender and geographic gaps in women’s sexual health and HIV care • • COMMUNITY & PEER-BASED • • Initiated following 6 months of community consultation on research priorities and gaps, with women living with HIV and HIV providers Recruitment of participants is achieved through leadership of Peer Research Associates, HIV care providers, HIV service organizations and clinical outreach LONGITUDINAL: QUANTITATIVE & BIOLOGICAL • • Includes baseline and semi-annual questionnaires administered by peer/ community interviewers and research nurses Participants receive voluntary viral load/CD 4 measurements and serology for STI/Hepatitis C Virus by a research nurse CLINICAL Participants are offered treatment onsite for symptomatic STI infections and Pap testing, regardless of study enrolment QUALITATIVE & PHOTOVOICE Includes a qualitative/artsbased component with a subset of 80 -90 participants We are committed to GIPA/MIPA principles which ensures meaningful inclusion of the experiences of cis and trans women living with HIV in all stages of research
STUDY OBJECTIVE • Given that HIV stigma and discrimination globally is recognized as a barrier to HIV and related health outcomes, and is identified as a priority to people living with HIV: • Our primary study objective was to understand the prevalence and social, structural, health- and healthcare-related correlates of four measures of HIV stigma among women living with HIV (WLWH) in Vancouver, Canada. • Bivariate and multivariable ordinal logistic regression using generalized estimating equations to take into account repeated measures across study period was used.
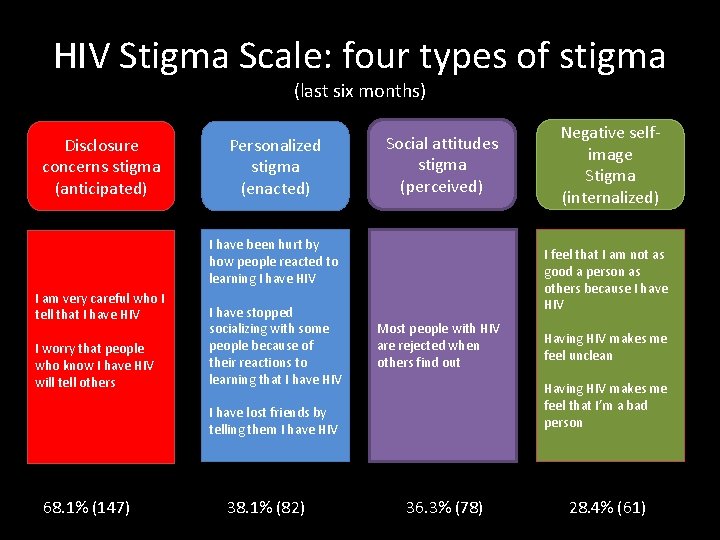
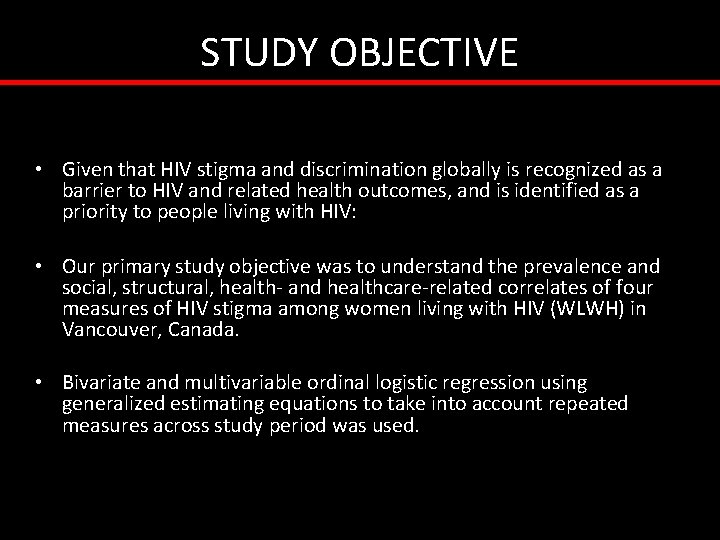
HIV Stigma Scale: four types of stigma (last six months) Disclosure concerns stigma (anticipated) Personalized stigma (enacted) Social attitudes stigma (perceived) I have been hurt by how people reacted to learning I have HIV I am very careful who I tell that I have HIV I worry that people who know I have HIV will tell others I have stopped socializing with some people because of their reactions to learning that I have HIV I feel that I am not as good a person as others because I have HIV Most people with HIV are rejected when others find out 38. 1% (82) Having HIV makes me feel unclean Having HIV makes me feel that I’m a bad person I have lost friends by telling them I have HIV 68. 1% (147) Negative selfimage Stigma (internalized) 36. 3% (78) 28. 4% (61)
![AOR Adjusted odds ratios95Confidence Intervals AOR 2 381 26 4 48 AOR 2 861 AOR[]: Adjusted odds ratios[95%Confidence Intervals] AOR: 2. 38[1. 26 -4. 48] AOR: 2. 86[1.](https://slidetodoc.com/presentation_image_h/30fa328b917fdc9b916aebf9f6f16112/image-7.jpg)
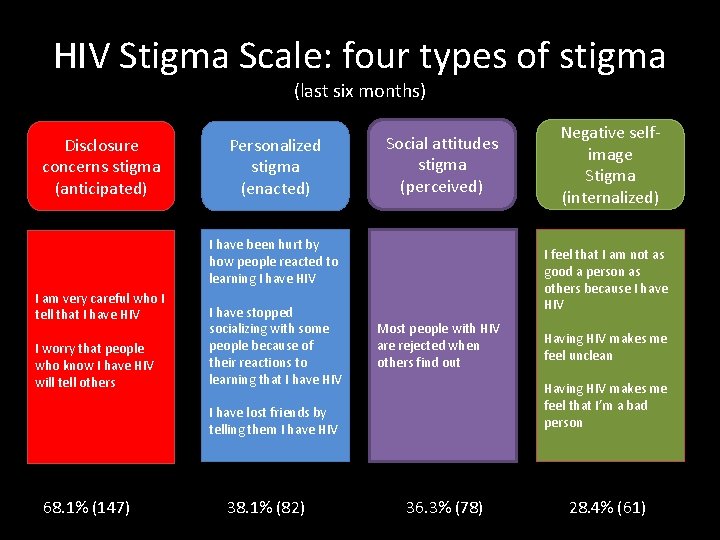
AOR[]: Adjusted odds ratios[95%Confidence Intervals] AOR: 2. 38[1. 26 -4. 48] AOR: 2. 86[1. 65 -4. 95] Verbal/physic al violence (HIV status) AOR: 4. 35[2. 65 -7. 12] Personalized stigma Verbal/physic al violence (HIV status) Negative selfimage stigma HIV disclosure without consent AOR: 1. 68[1. 16 -2. 44] Negative physical effects/ symptoms of HIV AOR: 1. 74[1. 03 -2. 93] Health access barriers (safety and respect) AOR: 2. 09[1. 25 -3. 50] Advised not to become pregnant I have been hurt by how people reacted to learning I have HIV I have stopped socializing with some people because of their reactions to learning that I have HIV I have lost friends by telling them I have HIV AOR: 2. 13[1. 48 -3. 05] Negative physical effects/ symptoms of HIV AOR: 1. 56[1. 04 -2. 34] Injection drug use AOR: 0. 97[0. 94 -1. 00 Duration since first diagnosed with HIV I feel that I am not as good a person as others because I have HIV Having HIV makes me feel unclean Having HIV makes me feel that I’m a bad person
CONCLUSIONS AND POLICY IMPLICATIONS • Address social and structural violence against women living with HIV • Engage broad health care professionals in addressing HIV stigma via a care approach based on traumainformed/women-centred principles • Amend Canada’s restrictive HIV disclosure laws as a structural intervention to reduce HIV stigma and promote safe disclosure • Meaningful inclusion of the expertise and perspectives of women living with HIV in all discussions on how to reduce HIV stigma
SHAWNA Project Team, Partners, & Advisories PI: Dr. Kate Shannon, GSHI Co-PI: (Quali): Dr. Andrea Krüsi, GSHI Site PI: Dr. Mary Kestler, Oak Tree Clinic • • • • Dr. Neora Pick, Oak Tree Clinic Dr. Charlotte Loppie, UVic Dr. Gina Ogilvie, BC Women’s Hospital, BCCDC Dr. Deborah Money, UBC Dr. Jeannie Shoveller, UBC Dr. Ruth Elwood Martin, UBC Dr. Putu Duff, GSHI Dr. Kathleen Deering, GSHI, UBC Flo Ranville, GSHI PRAs: Lulu Gurney, Barb Borden Sarah Moreheart, Brittney Udall, Bridget Simpson, Lauren Martin Mc. Craw, Jenn Mc. Dermid, Anita Dhanoa, Abby Rolston, Desire Tibashoboka, Maya Henriquez, Jessica Stortz, Peter Vann, Erin Seatter, GSHI Dr. Evan Wood, BCCSU Dr. Julio Montaner, BC-Cf. E Jill Chettiar, GSHI Dr. Carmen Logie, University of Toronto Positive Women’s Advisory Board Community Partner Advisory Board • • • Positive Women’s Network Sherri Pooyak, Canadian Aboriginal AIDS Network Patience Magagula, Afro-Canadian Positive Network of BC Sarah Chown, Youth. CO Jesse Brown, PAN Terry Howard, Glass. House Consultants Andrea Langlois, PAN Sandra Chu & Cécile Kazatchkine, Canadian HIV/AIDS Legal Network Dr. Sylvia Guillemi, BC-Cf. E, IDC Students/research assistants/fellows: Daniella Barreto, Meaghan Thumath, Margaret Erickson, Ofer Amran, Ariel Sernick

Acknowledgements www. gshi. cfenet. ubc. ca/SHAWNA
Scale measures – Internal consistency reliability » Cronbach’s alpha: 0. 74 -0. 88 – Construct validity » Supported by associations with variables considered to have related constructs and were available in our study, including depression and social support – Content validity » confirmed through our SHAWNA consultation process and questionnaire piloting, as judged by study participants, peers, interviewers, clinical nurses and research staff
 Period prevalence vs point prevalence
Period prevalence vs point prevalence Epidemiology defination
Epidemiology defination Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Correlates of effective schools
Correlates of effective schools Health and social component 3
Health and social component 3 Incidence density formula
Incidence density formula How to calculate incidence rate example
How to calculate incidence rate example Contoh soal secondary attack rate
Contoh soal secondary attack rate Epidemiologi adalah
Epidemiologi adalah Obesity prevalence europe
Obesity prevalence europe Prevalence ratio
Prevalence ratio