Preterm Labor RUSM ObGyn Clinical Core Case Presentation
Preterm Labor • RUSM Ob-Gyn Clinical Core • Case Presentation © 2013 Global Education International. All rights reserved. M-1301
Intended Learning Outcomes A student should be able to: A. Identify the modifiable and non-modifiable risk factors and causes for preterm labor B. Describe the signs and symptoms of preterm labor C. Describe the initial management of preterm labor D. List indications and contraindications of medications used in preterm labor E. List the adverse outcomes associated with preterm birth F. Describe the counseling for reducing preterm birth risk © 2013 Global Education International. All rights reserved. M-1301
• An 18 -year-old African-American, G 2 P 0101 woman who is 12 weeks pregnant, presents to your prenatal clinic for a new patient visit. Before you walk into the room to see the patient, you look through her records and note that she delivered her last pregnanc just 12 months ago. Beginning at 24 weeks in her previous pregnancy, the patient presented numerous times to Labor and Delivery reporting contractions, and was sent home each time with a diagnosis of “Braxton. Hicks contractions. ” She eventually presented at 28 weeks gestation and was diagnosed with preterm labor. She delivered at 29 weeks. The neonate’s course was complicated by intra-ventricular hemorrhage and respiratory distress syndrome. The child now appears to have cerebral palsy and chronic lung disease due to bronchopulmonary dysplasia. © 2013 Global Education International. All rights reserved. M-1301
What are the risk factors for preterm labor (PTL), and which ones does this patient have? © 2013 Global Education International. All rights reserved. M-1301
But first, how do you define PTL? © 2013 Global Education International. All rights reserved. M-1301
But first, how do you define PTL? • The diagnosis of preterm labor generally is based on clinical criteria of regular uterine contractions accompanied by a change in cervical dilation, effacement, or both or initial presentation with regular contractions and cervical dilation of at least 2 cm between 20 0/7 - 36 6/7 weeks of gestation. Preterm birth related to spontaneous preterm labor should be distinguished from preterm birth that is iatrogenic due to maternal or fetal complications. © 2013 Global Education International. All rights reserved. M-1301

Definition: Preterm Labor • “Regular” uterine contractions • With • Cervical “change” or • > 2 cm dilation or • > 80% effacement © 2013 Global Education International. All rights reserved. M-1301
• The physiology of labor initiation is not completely understood. Once fetal maturity is reached, there is activation of the maternal and fetal hypothalamus/pituitary/ adrenal axis that leads to the initiation of parturition. It has been proposed that fetal inflammatory response can contribute to the onset of preterm labor. © 2013 Global Education International. All rights reserved. M-1301
Preterm Birth (PTB) § Preterm birth: < 37 completed weeks § Very Preterm birth: < 32 weeks § Extremely Preterm birth: < 28 weeks © 2013 Global Education International. All rights reserved. M-1301
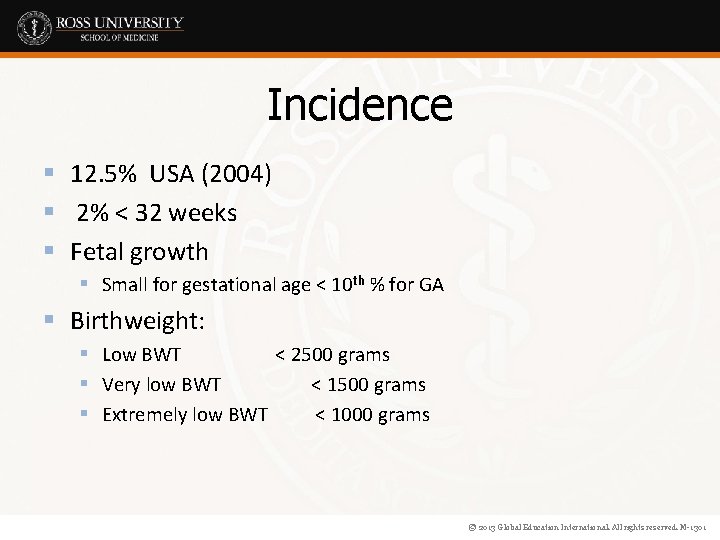
Incidence § 12. 5% USA (2004) § 2% < 32 weeks § Fetal growth § Small for gestational age < 10 th % for GA § Birthweight: § Low BWT < 2500 grams § Very low BWT < 1500 grams § Extremely low BWT < 1000 grams © 2013 Global Education International. All rights reserved. M-1301
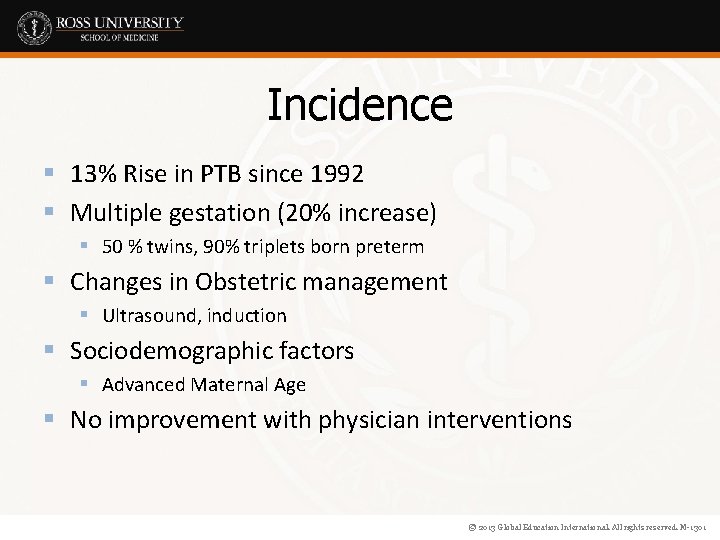
Incidence § 13% Rise in PTB since 1992 § Multiple gestation (20% increase) § 50 % twins, 90% triplets born preterm § Changes in Obstetric management § Ultrasound, induction § Sociodemographic factors § Advanced Maternal Age § No improvement with physician interventions © 2013 Global Education International. All rights reserved. M-1301
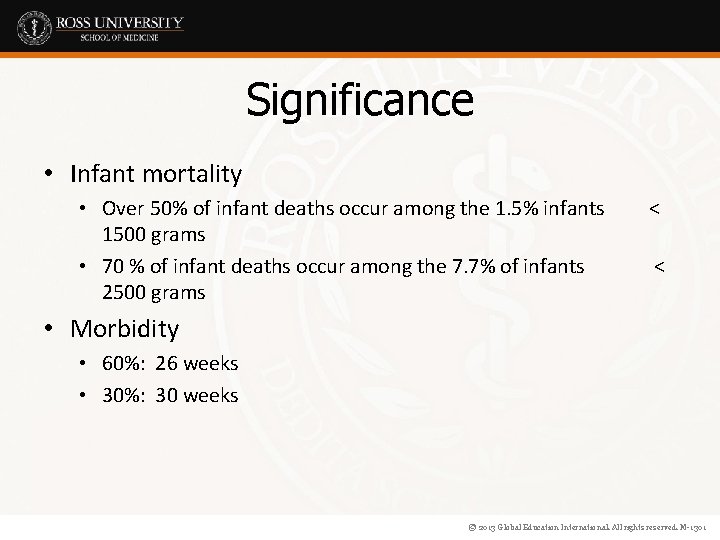
Significance • Infant mortality • Over 50% of infant deaths occur among the 1. 5% infants 1500 grams • 70 % of infant deaths occur among the 7. 7% of infants 2500 grams < < • Morbidity • 60%: 26 weeks • 30%: 30 weeks © 2013 Global Education International. All rights reserved. M-1301
What are the risk factors for preterm labor? © 2013 Global Education International. All rights reserved. M-1301
Risk factors for spontaneous preterm labor include: • • Prior history of preterm birth (highest risk) African-American race Low pre-pregnancy BMI Preterm uterine contractions Premature rupture of membranes (PROM) Incompetent cervix Shortened cervix on transvaginal ultrasound © 2013 Global Education International. All rights reserved. M-1301
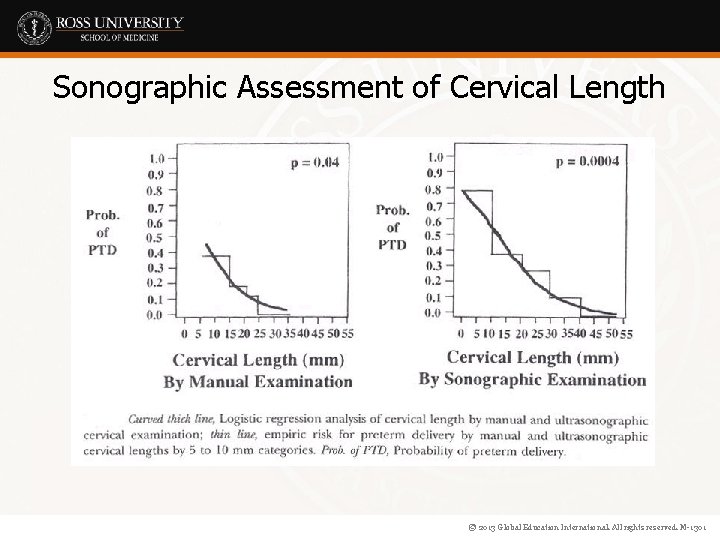
Sonographic Assessment of Cervical Length © 2013 Global Education International. All rights reserved. M-1301
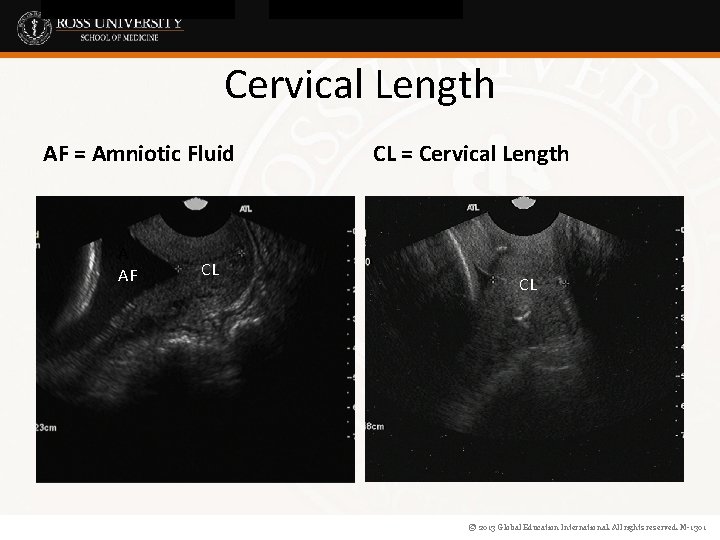
Cervical Length AF = Amniotic Fluid A AF CL CL = Cervical Length CL © 2013 Global Education International. All rights reserved. M-1301
Risk factors for spontaneous preterm labor include: • Infections – Urinary – Vaginal (BV) Intra-amniotic • Excessive uterine enlargement – Polyhydramnios – Multiple gestation © 2013 Global Education International. All rights reserved. M-1301
Risk factors for spontaneous preterm labor include: • Uterine distortion – Leiomyomas – Septate uterus, uterine didelphis, and other anomalies • Placental abnormalities – Abruption placentae – Placenta previa © 2013 Global Education International. All rights reserved. M-1301
Risk factors for spontaneous preterm labor include: • • • Maternal smoking (associated with PROM) Substance abuse Inflammation Decidual hemorrhage Pathologic uterine distension © 2013 Global Education International. All rights reserved. M-1301
This patient history is notable for a number of risk factors for preterm labor, namely: • • Prior history of preterm birth African-American race Low maternal weight Short interpregnancy interval © 2013 Global Education International. All rights reserved. M-1301
What characteristics distinguish Braxton-Hicks contractions from true labor contractions? © 2013 Global Education International. All rights reserved. M-1301
What characteristics distinguish Braxton. Hicks contractions from true labor contractions? • Braxton-Hicks contractions: The uterus undergoes irregular and sporadic contractions that are usually painless or of mild intensity. The frequency of these contractions increases in the last 4 to 8 weeks of pregnancy. These contractions are not associated with progressive cervical dilation and effacement, and often is referred to as false labor. These contractions often resolve with rest, hydration, and/or sedation. • True Labor Contractions : As compared to Braxton-Hicks contractions, true labor contractions occur at regular intervals, progressively increase in frequency and intensity, and are associated with cervical dilation. True labor contractions will not resolve with sedation. © 2013 Global Education International. All rights reserved. M-1301
What should you counsel the patient regarding the signs and symptoms of preterm labor? © 2013 Global Education International. All rights reserved. M-1301
What should you counsel the patient regarding the signs and symptoms of preterm labor? • Distinguishing true preterm labor from false labor or Braxton-Hicks contractions is challenging and depends primarily on prompt patient evaluation. Efforts to develop models or tests to predict preterm labor have thus far been unsuccessful; therefore, when in doubt it is advisable to have patient come in for evaluation. © 2013 Global Education International. All rights reserved. M-1301
The primary method for identifying preterm labor is by screening for maternal signs and symptoms as summarized below: Menstrual-like cramps Low, dull backache Abdominal pressure Pelvic pressure Abdominal cramping (with or without diarrhea) Increase or change in vaginal discharge (mucous, watery, light bloody discharge) • Uterine contractions, often painless • • • © 2013 Global Education International. All rights reserved. M-1301
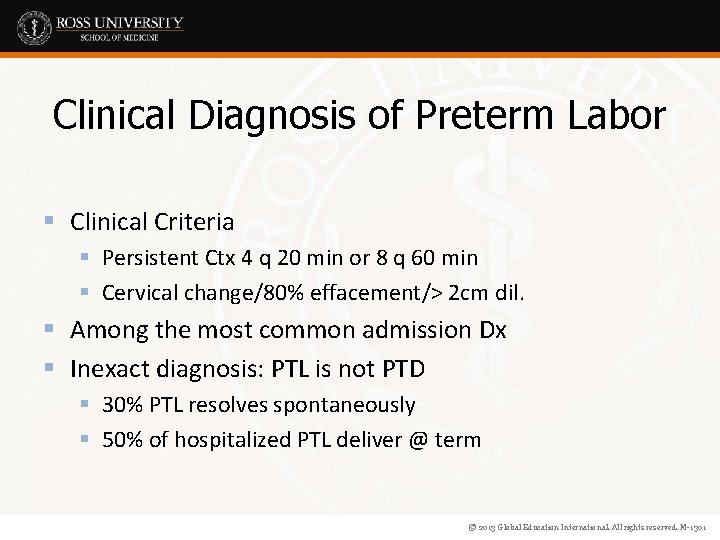
Clinical Diagnosis of Preterm Labor § Clinical Criteria § Persistent Ctx 4 q 20 min or 8 q 60 min § Cervical change/80% effacement/> 2 cm dil. § Among the most common admission Dx § Inexact diagnosis: PTL is not PTD § 30% PTL resolves spontaneously § 50% of hospitalized PTL deliver @ term © 2013 Global Education International. All rights reserved. M-1301
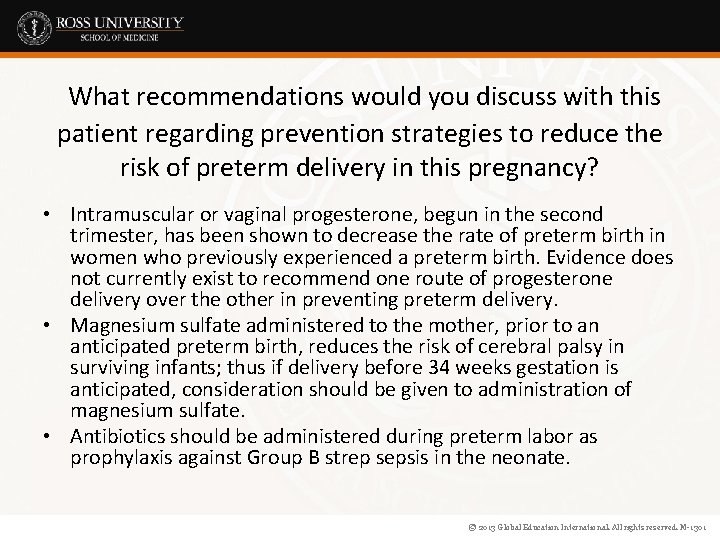
What recommendations would you discuss with this patient regarding prevention strategies to reduce the risk of preterm delivery in this pregnancy? • Intramuscular or vaginal progesterone, begun in the second trimester, has been shown to decrease the rate of preterm birth in women who previously experienced a preterm birth. Evidence does not currently exist to recommend one route of progesterone delivery over the other in preventing preterm delivery. • Magnesium sulfate administered to the mother, prior to an anticipated preterm birth, reduces the risk of cerebral palsy in surviving infants; thus if delivery before 34 weeks gestation is anticipated, consideration should be given to administration of magnesium sulfate. • Antibiotics should be administered during preterm labor as prophylaxis against Group B strep sepsis in the neonate. © 2013 Global Education International. All rights reserved. M-1301
To reduce the risk of neurodevelopmental disorders and other morbidity associated with preterm labor in this fetus: • A course of antenatal steroids (betamethasone or dexamethasone) should be administered to the mother diagnosed with preterm labor in an effort to enhance fetal lung maturity and decrease the risk of necrotizing fasciitis and intracranial bleeds in the neonate. © 2013 Global Education International. All rights reserved. M-1301
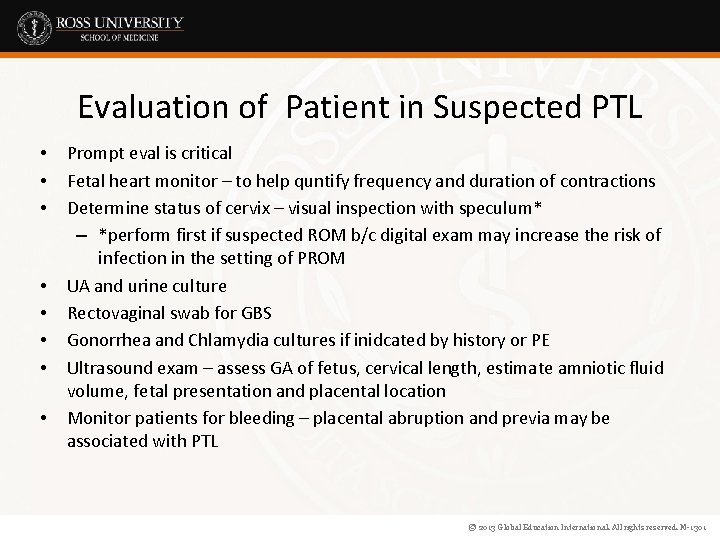
Evaluation of Patient in Suspected PTL • • Prompt eval is critical Fetal heart monitor – to help quntify frequency and duration of contractions Determine status of cervix – visual inspection with speculum* – *perform first if suspected ROM b/c digital exam may increase the risk of infection in the setting of PROM UA and urine culture Rectovaginal swab for GBS Gonorrhea and Chlamydia cultures if inidcated by history or PE Ultrasound exam – assess GA of fetus, cervical length, estimate amniotic fluid volume, fetal presentation and placental location Monitor patients for bleeding – placental abruption and previa may be associated with PTL © 2013 Global Education International. All rights reserved. M-1301
If you dx PTL, what recommendations would you make regarding treatment and management? • Fetal fibronectin testing (negative) and cervical length (greater than 2. 5 cm) have good negative predictive value in deciding which patients do not require treatment for preterm labor. • There is no clear first line tocolytic medication; however, current medications in use include magnesium sulfate, nifedipine, indomethacin, and beta -mimetics. The primary benefit of tocolytics appears to be delaying delivery in order to complete a course of antenatal steroids and transport the mother to a tertiary care facility for adequate care of the premature newborn. © 2013 Global Education International. All rights reserved. M-1301
Management of Preterm Labor • Two goals of management: • Detection and treatment of disorders associated with PTL • Therapy for PTL itself • Bedrest, hydration, sedation • NO evidence to support in the literature © 2013 Global Education International. All rights reserved. M-1301
Fetal Fibronectin (f. FN) § Glycoprotein in amnion, decidua, cytotrophoblast § Increased levels secondary to breakdown of the chorionic-decidual interface § Inflammation, shear, movement © 2013 Global Education International. All rights reserved. M-1301
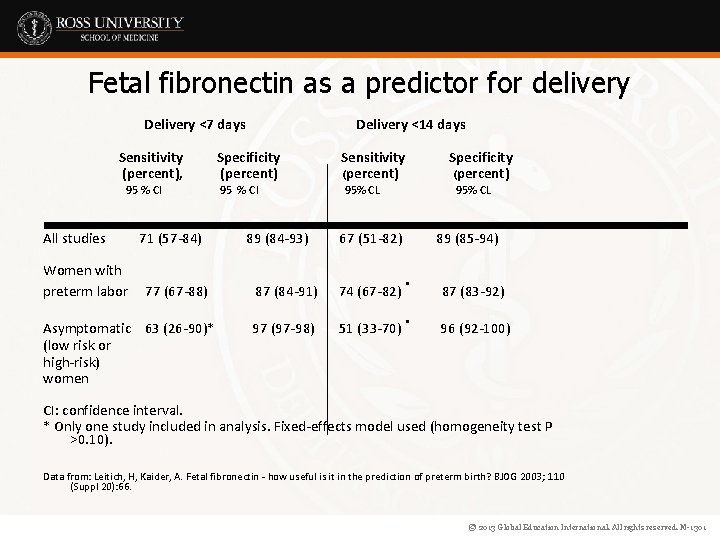
Fetal fibronectin as a predictor for delivery Delivery <7 days Sensitivity (percent), 95 % CI All studies Women with preterm labor 71 (57 -84) 77 (67 -88) Asymptomatic 63 (26 -90)* (low risk or high-risk) women Delivery <14 days Specificity (percent) Sensitivity (percent) 95 % CI 95% CL 89 (84 -93) 95% CL 67 (51 -82) 87 (84 -91) 74 (67 -82) 97 (97 -98) 51 (33 -70) Specificity (percent) 89 (85 -94) . . 87 (83 -92) 96 (92 -100) CI: confidence interval. * Only one study included in analysis. Fixed-effects model used (homogeneity test P >0. 10). Data from: Leitich, H, Kaider, A. Fetal fibronectin - how useful is it in the prediction of preterm birth? BJOG 2003; 110 (Suppl 20): 66. © 2013 Global Education International. All rights reserved. M-1301
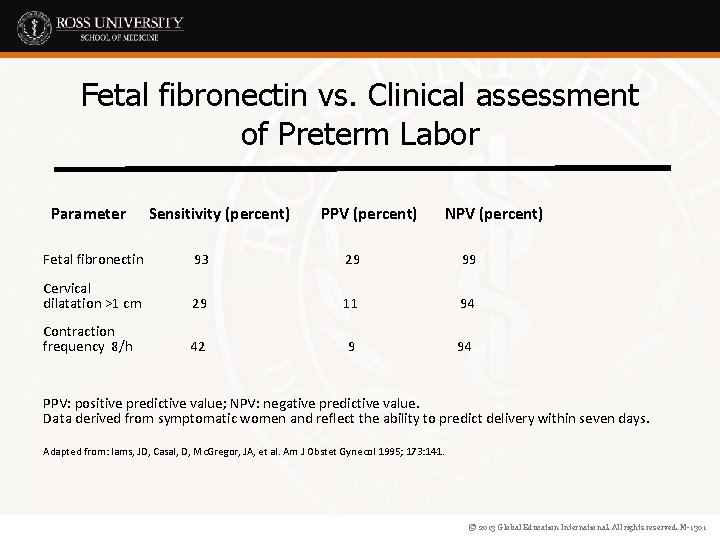
Fetal fibronectin vs. Clinical assessment of Preterm Labor Parameter Sensitivity (percent) PPV (percent) NPV (percent) Fetal fibronectin 93 29 99 Cervical dilatation >1 cm 29 11 94 Contraction frequency 8/h 42 9 94 PPV: positive predictive value; NPV: negative predictive value. Data derived from symptomatic women and reflect the ability to predict delivery within seven days. Adapted from: Iams, JD, Casal, D, Mc. Gregor, JA, et al. Am J Obstet Gynecol 1995; 173: 141. © 2013 Global Education International. All rights reserved. M-1301
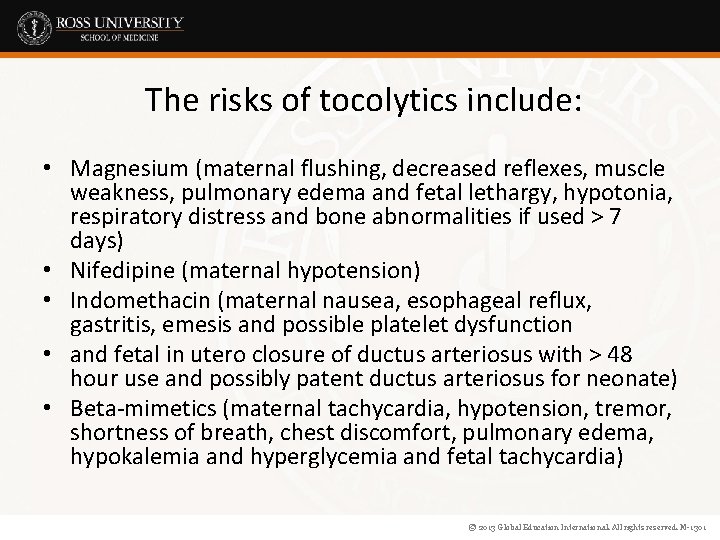
The risks of tocolytics include: • Magnesium (maternal flushing, decreased reflexes, muscle weakness, pulmonary edema and fetal lethargy, hypotonia, respiratory distress and bone abnormalities if used > 7 days) • Nifedipine (maternal hypotension) • Indomethacin (maternal nausea, esophageal reflux, gastritis, emesis and possible platelet dysfunction • and fetal in utero closure of ductus arteriosus with > 48 hour use and possibly patent ductus arteriosus for neonate) • Beta-mimetics (maternal tachycardia, hypotension, tremor, shortness of breath, chest discomfort, pulmonary edema, hypokalemia and hyperglycemia and fetal tachycardia) © 2013 Global Education International. All rights reserved. M-1301
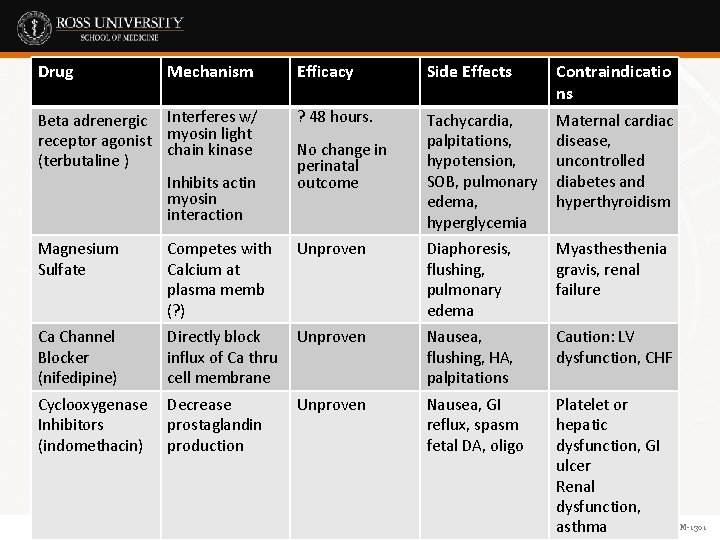
Drug Mechanism Efficacy Side Effects Contraindicatio ns Beta adrenergic Interferes w/ receptor agonist myosin light chain kinase (terbutaline ) Inhibits actin myosin interaction ? 48 hours. Tachycardia, palpitations, hypotension, SOB, pulmonary edema, hyperglycemia Maternal cardiac disease, uncontrolled diabetes and hyperthyroidism Magnesium Sulfate Competes with Calcium at plasma memb (? ) Unproven Diaphoresis, flushing, pulmonary edema Myasthenia gravis, renal failure Ca Channel Blocker (nifedipine) Directly block influx of Ca thru cell membrane Unproven Nausea, flushing, HA, palpitations Caution: LV dysfunction, CHF Cyclooxygenase Inhibitors (indomethacin) Decrease prostaglandin production Unproven Nausea, GI reflux, spasm fetal DA, oligo No change in perinatal outcome Platelet or hepatic dysfunction, GI ulcer Renal dysfunction, © 2013 Global Educationasthma International. All rights reserved. M-1301
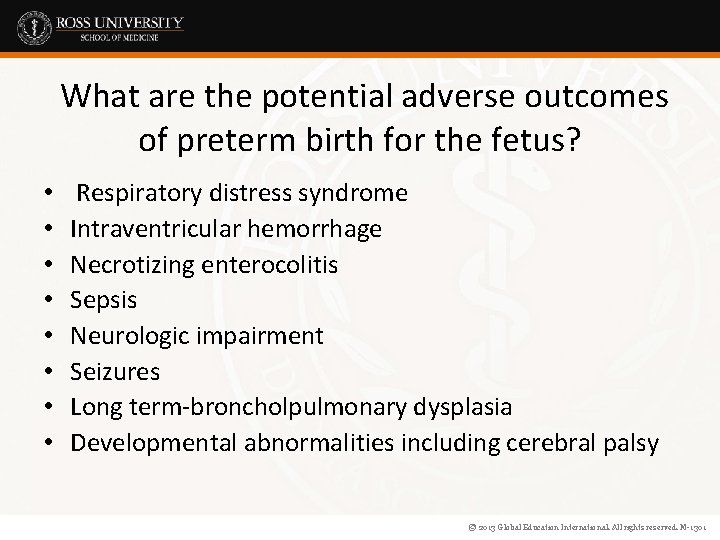
What are the potential adverse outcomes of preterm birth for the fetus? • • Respiratory distress syndrome Intraventricular hemorrhage Necrotizing enterocolitis Sepsis Neurologic impairment Seizures Long term-broncholpulmonary dysplasia Developmental abnormalities including cerebral palsy © 2013 Global Education International. All rights reserved. M-1301
Pathogenesis § 80% of Preterm births are spontaneous § 50% Preterm labor § 30% Preterm premature rupture of the membranes § Pathogenic processes § Activation of the maternal or fetal hypothalamic pituitary axis § Infection § Decidual hemorrhage § Pathologic uterine distention © 2013 Global Education International. All rights reserved. M-1301
Activation of the HPA Axis § § Premature activation Major maternal physical/psychologic stress Stress of uteroplacental vasculopathy Mechanism § Increased Corticotropin-releasing hormone § Fetal ACTH § Estrogens (incr myometrial gap junctions) © 2013 Global Education International. All rights reserved. M-1301
Inflammation § Clinical/subclinical chorioamnionitis § Up to 50% of preterm birth < 30 wks GA § Proinflammatory mediators § Maternal/fetal inflammatory response § Activated neutrophils/macrophages § TNF alpha, interleukins (6) § Bacteria § Degradation of fetal membranes § Prostaglandin synthesis © 2013 Global Education International. All rights reserved. M-1301
Evaluation of Patient in Suspected PTL • • Prompt eval is critical Fetal heart monitor – to help quntify frequency and duration of contractions Determine status of cervix – visual inspection with speculum* – *perform first if suspected ROM b/c digital exam may increase the risk of infection in the setting of PROM UA and urine culture Rectovaginal swab for GBS Gonorrhea and Chlamydia cultures if inidcated by history or PE Ultrasound exam – assess GA of fetus, cervical length, estimate amniotic fluid volume, fetal presentation and placental location Monitor patients for bleeding – placental abruption and previa may be associated with PTL © 2013 Global Education International. All rights reserved. M-1301
Management of Preterm Labor • Two goals of management: • Detection and treatment of disorders associated with PTL • Therapy for PTL itself • Bedrest, hydration, sedation • NO evidence to support in the literature © 2013 Global Education International. All rights reserved. M-1301
Antenatal Steroids § Recommended for: § Preterm labor 24 – 34 weeks § PPROM 24 – 32 weeks § Reduction in: § Mortality, IVH, NEC, RDS § Mechanism of action: § Enhanced maturation lungs § Biochemical maturation © 2013 Global Education International. All rights reserved. M-1301
Antenatal Steroids § Dosage: § Dexamethasone 6 mg q 12 h § Betamethasone 12. 5 mg q 24 h § Repeated doses - NO § Effect: § Within several hours § Max @ 48 hours © 2013 Global Education International. All rights reserved. M-1301
Progesterone for History of PTB § 17 alpha OH Progesterone § Women with prior PTB (singleton) 24 – 26 wks § (16 – 20 wks) – 36 weeks § Reduces the risk of recurrent preterm birth § < 37 wks 36% vs 55% § < 35 wks 21% vs 31% § < 32 wks 11% vs 20% © 2013 Global Education International. All rights reserved. M-1301
Key Concepts § Preterm labor - “Regular” uterine contractions, with cervical “change” or > 2 cm dilation or > 80% effacement, occurring before 37 weeks § There are numerous risk factors – both modifiable and non-modifiable. Counsel patients regarding ways to reduce their modifiable risk factors § Clinical assessment of risk includes consideration and evaluation of history, cervical length and fetal fibronectin § There a variety of tocolytic drugs available, though most have unproven efficacy § Antenatal steroids are recommended for: Preterm labor 24 – 34 weeks and PPROM 24 – 32 weeks © 2013 Global Education International. All rights reserved. M-1301
• As a means of determining your comprehension of the key concepts presented, please answer the APGO u. WISE questions in Unit 2, Chapter 24. © 2013 Global Education International. All rights reserved. M-1301
Competencies Addressed • • • Patient Care Medical Knowledge Professionalism Interpersonal and Communication Skills Systems-Based Practice © 2013 Global Education International. All rights reserved. M-1301
References ACOG Practice Bulletin 127, June 2012. ACOG Practice Bulletin 130, October 2012. ACOG Committee Opinion 455, reaffirmed 2013. ACOG Committee Opinion 120, June 2011. • APGO Medical Student Educational Objectives, 10 th edition, (2014), Educational Topic 24. • APGO Clinical Teaching Cases • Beckman CRB, et al. Obstetrics and Gynecology. 7 th ed. Chapter 15, Philadelphia: Lippincott, Williams & Wilkins, 2013. • • © 2013 Global Education International. All rights reserved. M-1301
- Slides: 49