PRESSURE ULCERS Kansas Reynolds Program in Aging Shelley

- Slides: 57
PRESSURE ULCERS Kansas Reynolds Program in Aging Shelley B. Bhattacharya, D. O. , M. P. H. Assistant Professor, Director of Geriatric Education Department of Family Medicine
OBJECTIVES Know and understand: n The morbidity and mortality associated with pressure ulcers for older adults n The common risk factors for pressure ulcer development n Evidence based techniques for preventing pressure ulcers n The pressure ulcer staging system and treatment strategies for each stage
ACOVE INDICATOR Concerning the pressure ulcer care of an older adult : n If a vulnerable older adult is admitted to an intensive care unit or a medical or surgical unit of a hospital and cannot reposition himself or herself or has limited ability to do so, THEN risk assessment for pressure ulcers should be performed on admission n If a vulnerable older adult is identified as at risk for pressure ulcer development or a pressure ulcer risk assessment score indicates that the person is at risk, THEN preventive intervention must be instituted within 12 hours, addressing repositioning needs and pressure reduction (or management of tissue loads)
ACOVE INDICATOR n n If a vulnerable older adult presents with a pressure ulcer, THEN the pressure ulcer should be assessed for 1) location, 2) depth and stage, 3) size and 4) presence of necrotic tissue If a vulnerable older adult is identified as at risk for pressure ulcer development and has malnutrition (involuntary weight loss >10% over 1 year or low albumin or prealbumin levels), THEN nutritional intervention or dietary consultation should be instituted
TOPICS COVERED n Epidemiology n Complications n Risk Factors and Risk Assessment n Evidence based review of prevention techniques n Ulcer Assessment and 2007 Staging definitions n Monitoring and Treatment
PRESSURE ULCER: DEFINITION n Definition (2007 National Pressure Ulcer Advisory Panel): an injury caused by unrelieved pressure on a specific region of skin and muscle in bed or chair bound patients n The time for pressure ulcer development is variable due to severity of illness and a number of comorbid conditions
PRESSURE ULCERS: A MAJOR ISSUE IN GERIATRIC MEDICINE n Affects 1 million adults annually n Higher risk in older persons because: Ø Ø Ø n Local blood supply to skin decreases Epithelial layers flatten and thin Subcutaneous fat decreases Collagen fibers lose elasticity Tolerance to hypoxia decreases 1 of 3 sentinel events for long-term care
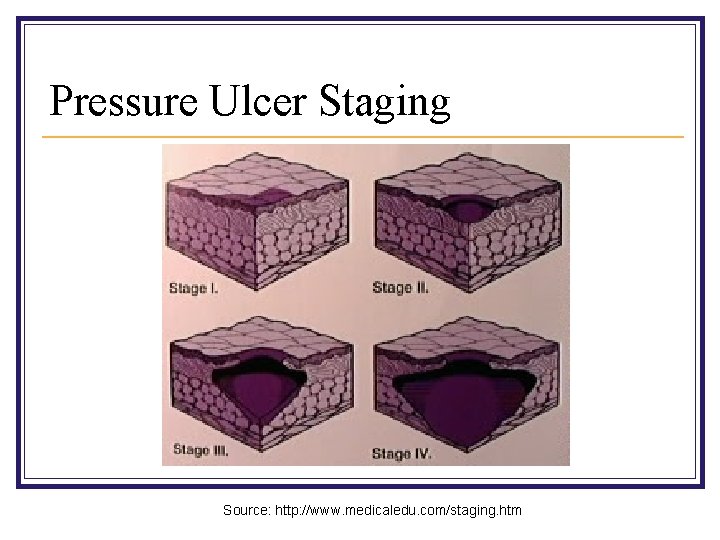
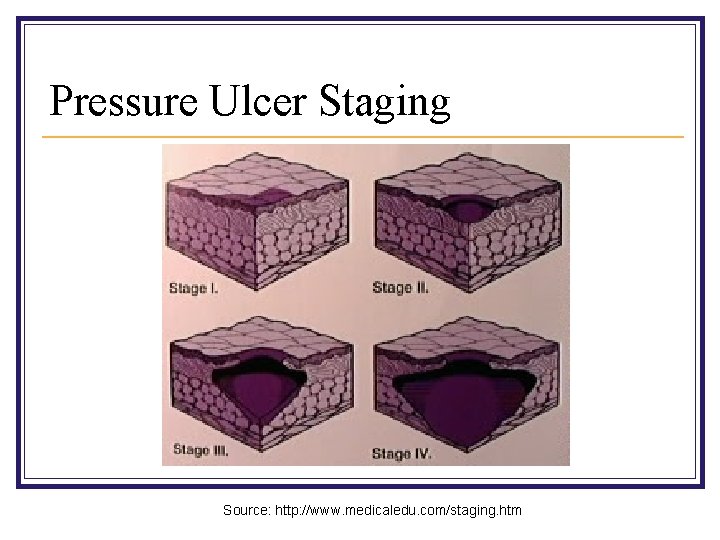
Pressure Ulcer Staging Source: http: //www. medicaledu. com/staging. htm
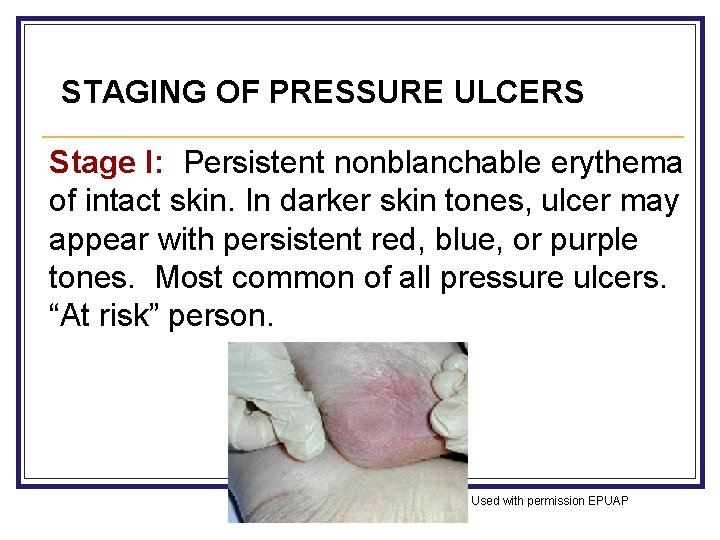
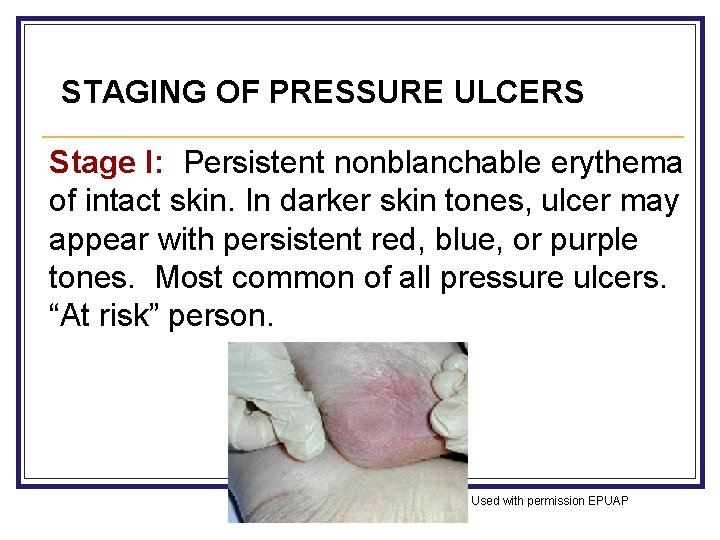
STAGING OF PRESSURE ULCERS Stage I: Persistent nonblanchable erythema of intact skin. In darker skin tones, ulcer may appear with persistent red, blue, or purple tones. Most common of all pressure ulcers. “At risk” person. Used with permission EPUAP
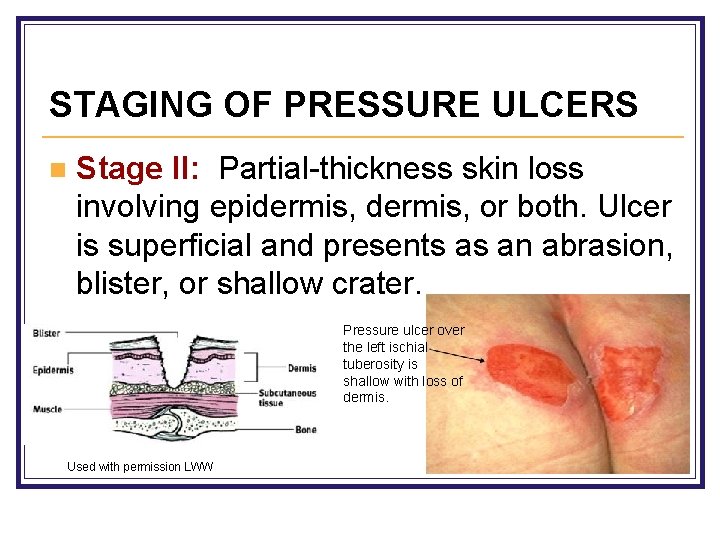
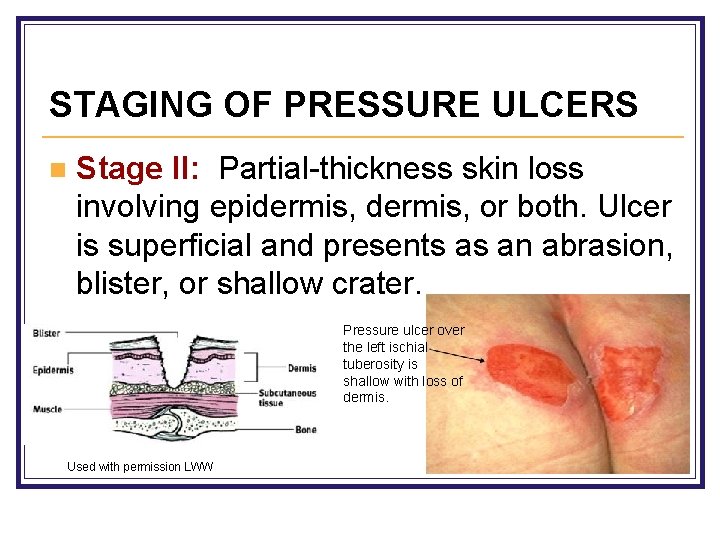
STAGING OF PRESSURE ULCERS n Stage II: Partial-thickness skin loss involving epidermis, or both. Ulcer is superficial and presents as an abrasion, blister, or shallow crater. Pressure ulcer over the left ischial tuberosity is shallow with loss of dermis. Used with permission LWW
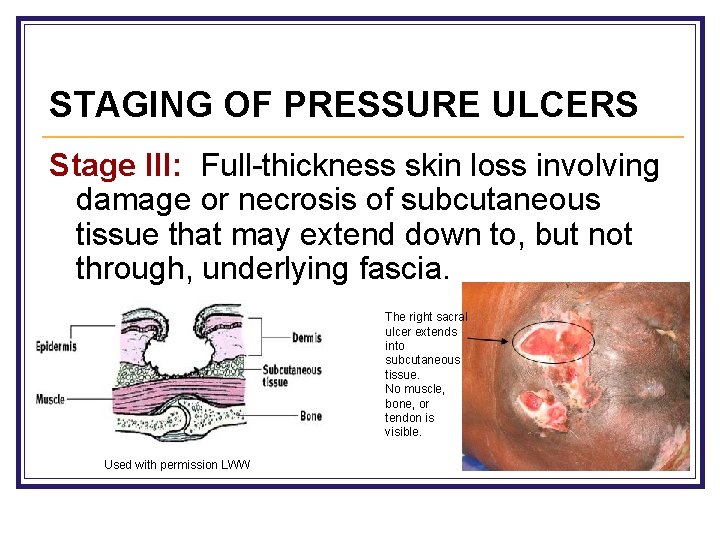
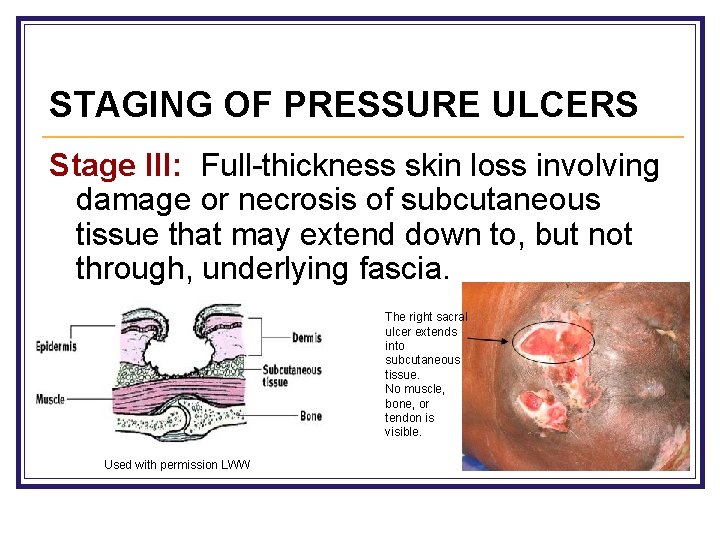
STAGING OF PRESSURE ULCERS Stage III: Full-thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia. The right sacral ulcer extends into subcutaneous tissue. No muscle, bone, or tendon is visible. Used with permission LWW
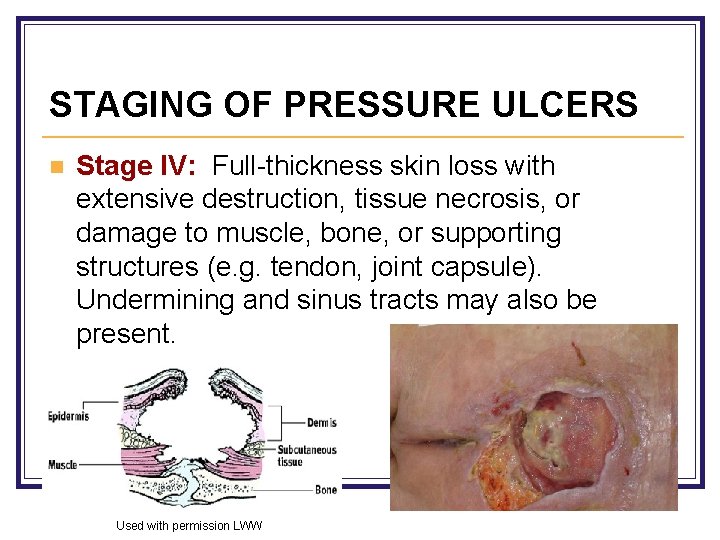
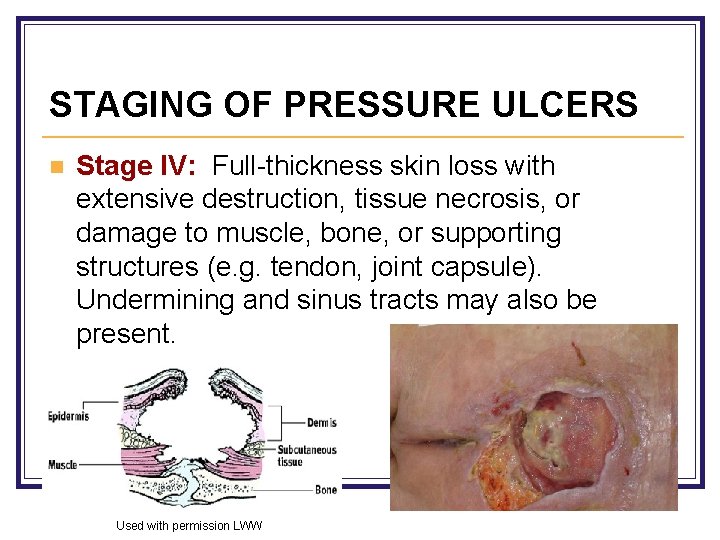
STAGING OF PRESSURE ULCERS n Stage IV: Full-thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures (e. g. tendon, joint capsule). Undermining and sinus tracts may also be present. Used with permission LWW
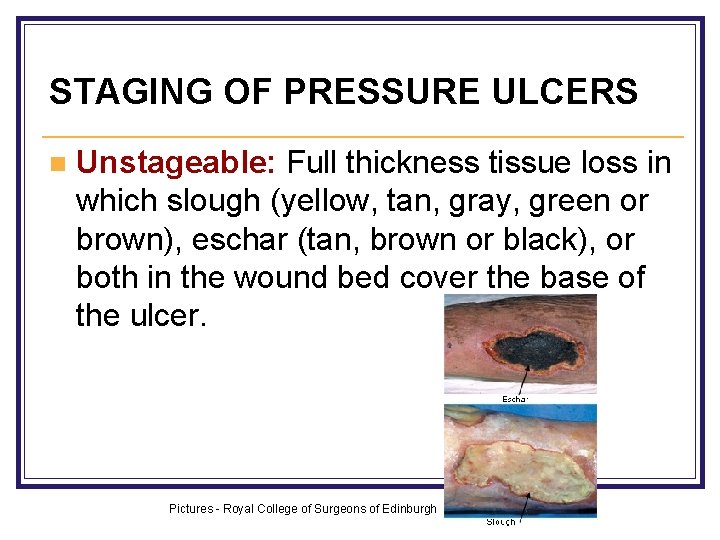
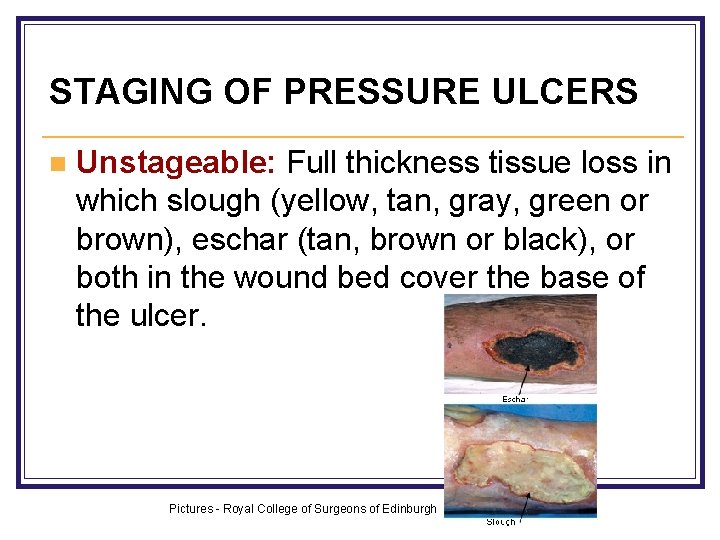
STAGING OF PRESSURE ULCERS n Unstageable: Full thickness tissue loss in which slough (yellow, tan, gray, green or brown), eschar (tan, brown or black), or both in the wound bed cover the base of the ulcer. Pictures - Royal College of Surgeons of Edinburgh
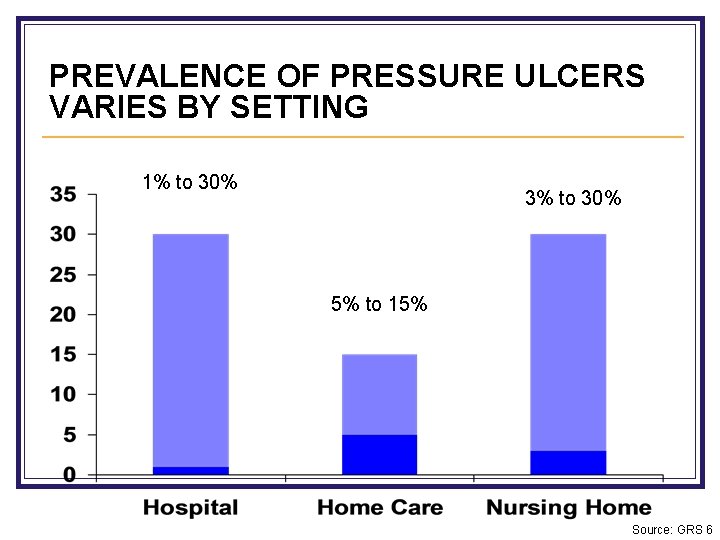
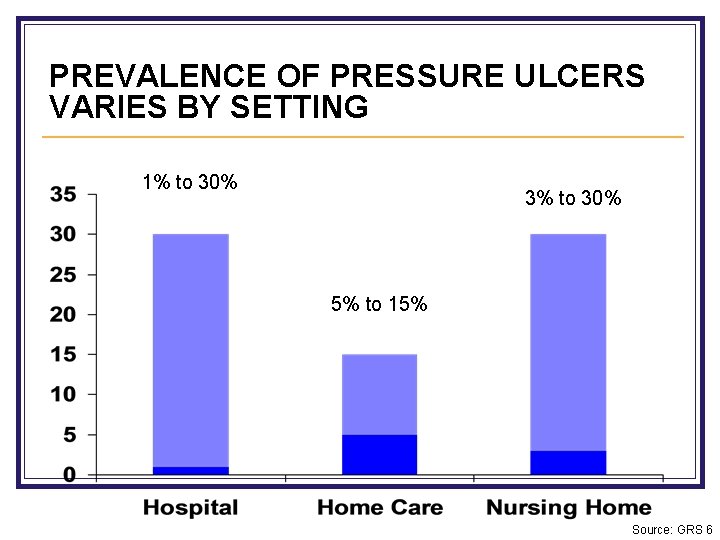
PREVALENCE OF PRESSURE ULCERS VARIES BY SETTING 1% to 30% 3% to 30% 5% to 15% Source: GRS 6
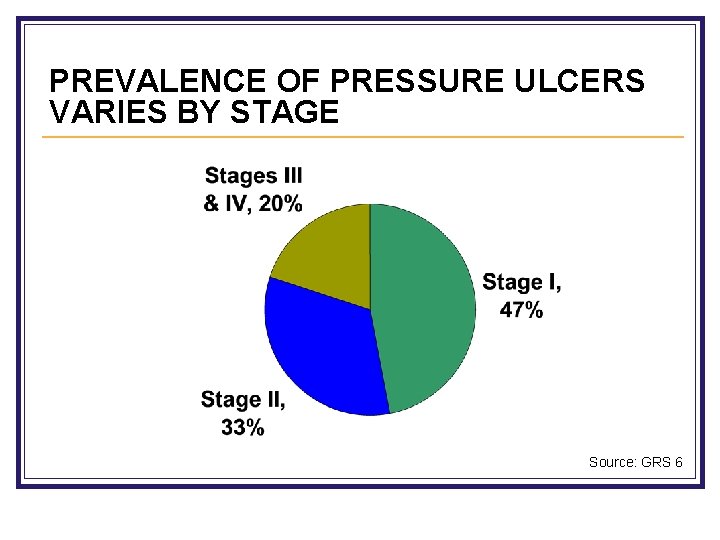
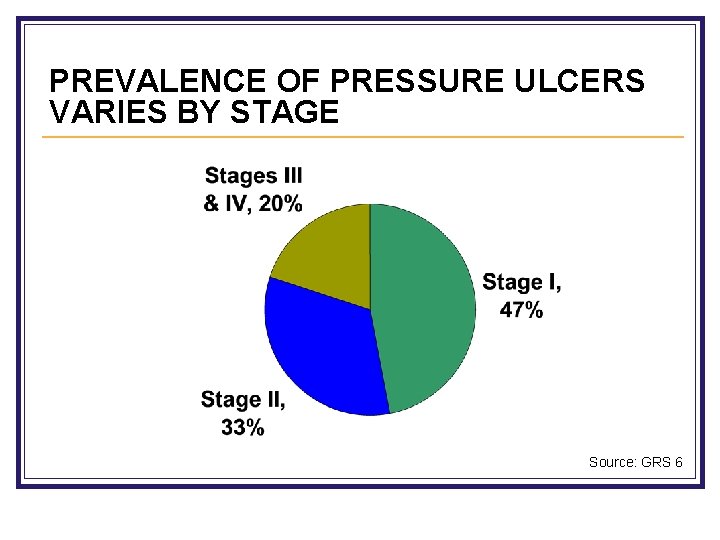
PREVALENCE OF PRESSURE ULCERS VARIES BY STAGE Source: GRS 6
RISK FACTORS n Older adults have a much higher likelihood of developing pressure ulcers due to their risk factors n Intrinsic risk factors are physiologic factors or disease states that increase the risk for pressure ulcer development n Extrinsic risk factors are external factors that damage skin
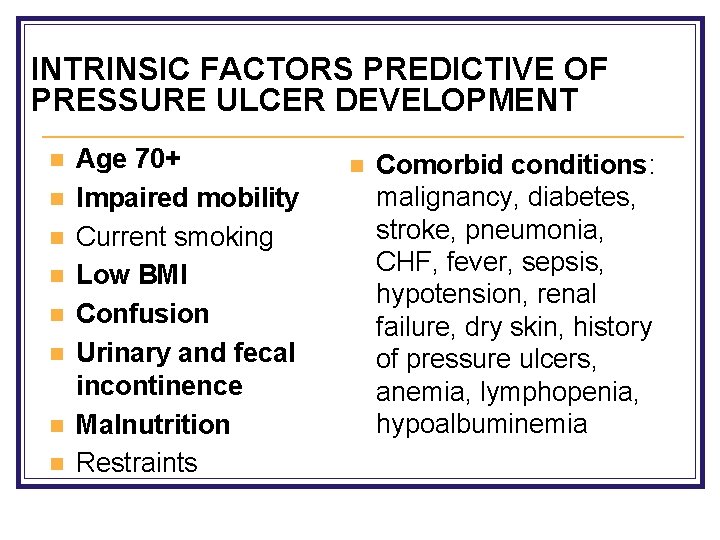
INTRINSIC FACTORS PREDICTIVE OF PRESSURE ULCER DEVELOPMENT n n n n Age 70+ Impaired mobility Current smoking Low BMI Confusion Urinary and fecal incontinence Malnutrition Restraints n Comorbid conditions: malignancy, diabetes, stroke, pneumonia, CHF, fever, sepsis, hypotension, renal failure, dry skin, history of pressure ulcers, anemia, lymphopenia, hypoalbuminemia
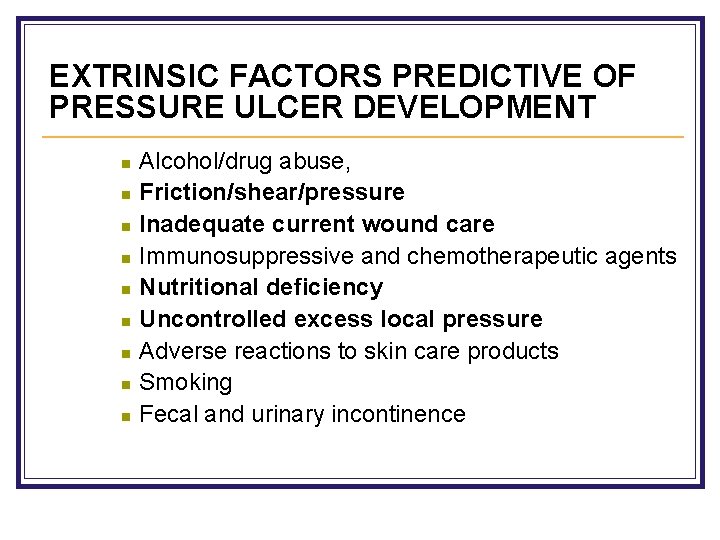
EXTRINSIC FACTORS PREDICTIVE OF PRESSURE ULCER DEVELOPMENT n n n n n Alcohol/drug abuse, Friction/shear/pressure Inadequate current wound care Immunosuppressive and chemotherapeutic agents Nutritional deficiency Uncontrolled excess local pressure Adverse reactions to skin care products Smoking Fecal and urinary incontinence
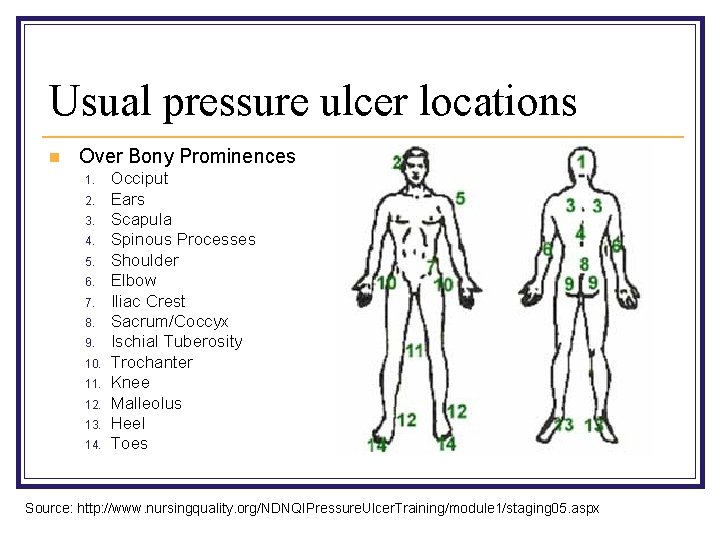
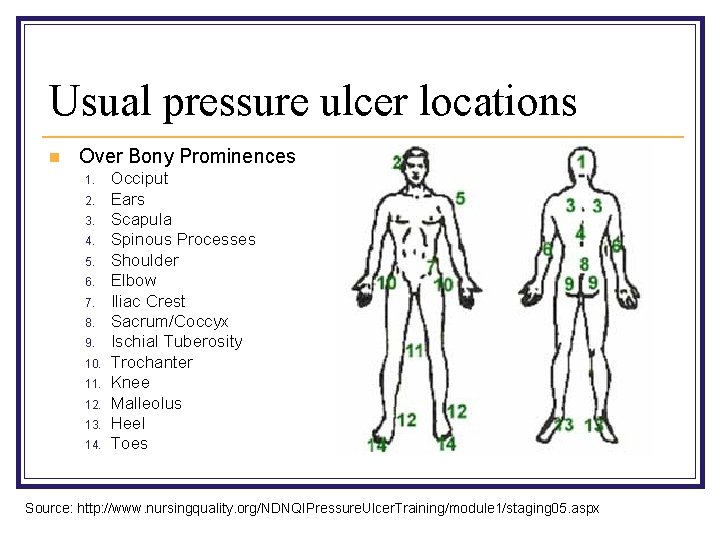
Usual pressure ulcer locations n Over Bony Prominences 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Occiput Ears Scapula Spinous Processes Shoulder Elbow Iliac Crest Sacrum/Coccyx Ischial Tuberosity Trochanter Knee Malleolus Heel Toes Source: http: //www. nursingquality. org/NDNQIPressure. Ulcer. Training/module 1/staging 05. aspx
Other locations… n Any skin surface subject to excess pressure n Examples include skin surfaces under: n n Oxygen tubing Urinary catheter drainage tubing Casts Cervical collars
POSSIBLE COMPLICATIONS n Sepsis (aerobic or anaerobic bacteremia) n Localized infection, cellulitis, osteomyelitis n Pain n Depression Mortality rate = 60% in older persons who develop a pressure ulcer within 1 year of hospital discharge
RISK ASSESSMENT INSTRUMENTS Widely used tools for identifying older patients at risk for developing ulcers: SCREENING TOOLS n Norton scale: sensitivity =73%– 92%, specificity = 61%– 94% n Braden scale: sensitivity = 83%– 100%, specificity = 64%– 77% Both recommended by Agency for Healthcare Research and Quality
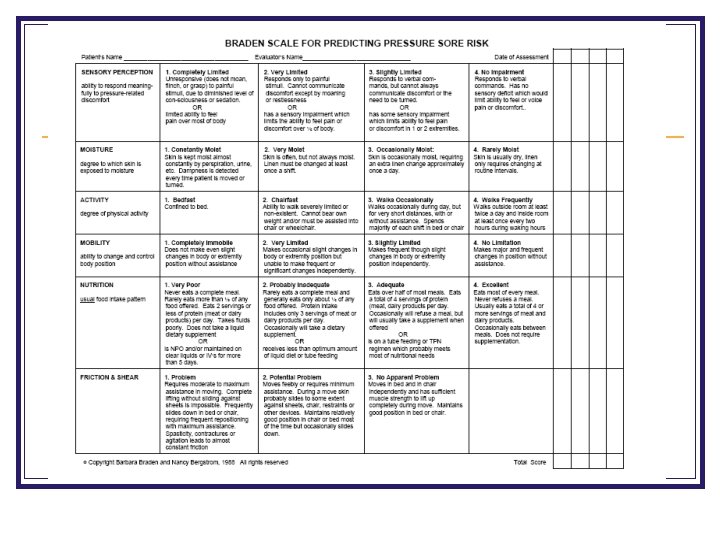
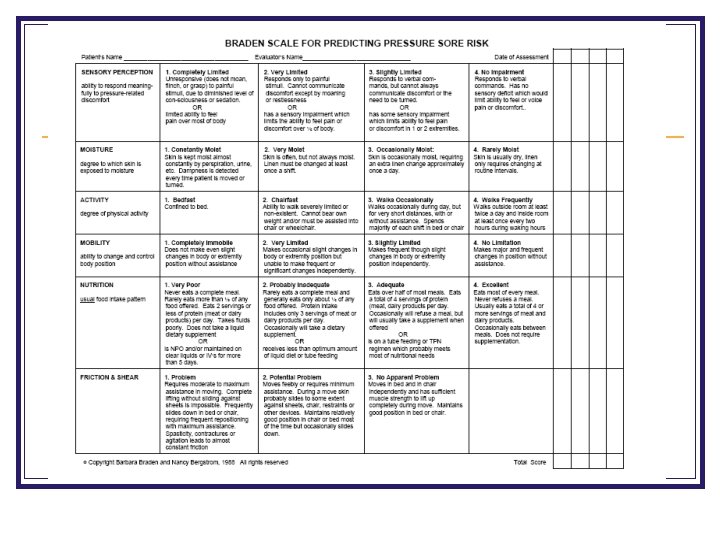
BRADEN SCALE Provides method for assessing a patient’s pressure ulcer risk by evaluating: n Sensory perception: ability to respond to pressurerelated discomfort n Moisture: degree to which skin is exposed to moisture n Activity: degree of physical activity n Mobility: ability to change and control body position n Nutrition: usual food intake n Friction and Shear
NORTON SCALE Provides method for assessing a patient’s pressure ulcer risk by evaluating: n n n Physical condition Mental condition Level of physical activity Mobility Continence or incontinence
Scale Documentation Frequency n October 2007 JAGS article recommends using the scales: n n n If in hospital setting: on admission, if at risk then q 48 hours thereafter; If in skilled nursing facility: on admission, q wk for 1 st 4 weeks, then q 3 mos thereafter; If in home health program: on admission, if found to be at risk, then q wk for 4 weeks and every other week thereafter.
PREVENTION An evidence-based approach to preventing pressure ulcers focuses on: Skin care Mechanical loading Support surfaces
PREVENTION: SKIN CARE n Daily systematic skin inspection and cleansing n factors that promote dryness n Avoid massaging over bony prominences n moisture (incontinence, perspiration, drainage) n Minimize friction and shear
PREVENTION: MECHANICAL LOADING n Reposition at least every 2 hours (may use pillows, foam wedges) n Keep head of bed at lowest elevation possible n Use lifting devices to decrease friction and shear n Remind patients in chairs to shift weight every 15 min “Doughnut” seat cushions are contraindicated, may cause pressure ulcers n Pay special attention to heels (heel ulcers account for 20% of all pressure ulcers)
PREVENTING HEEL ULCERS n Assess heels of high-risk patients every day n Use moisturizer on heels (no massage) twice a day n Apply dressings to heels: Ø Ø Transparent film for patients prone to friction problems Single or extra-thick hydrocolloid dressing for those with pre-stage 1 reactive hyperemia
PREVENTING HEEL ULCERS n Have patients wear: Ø Ø Socks to prevent friction (remove at bedtime) Properly fitting sneakers or shoes when in wheelchair n Place pillow under legs to support heels off bed n Place heel cushions to prevent pressure n Turn patients every 2 hours, repositioning heels
PRESSURE-REDUCING SUPPORT SURFACES **Use for all older persons at risk for ulcers** n Static Ø n Foam, static air, gel, water, combination (less expensive) Dynamic Ø Ø Ø Alternating air, low-air-loss, or air-fluidized Use if the status surface is compressed to <1 inch or high-risk patient has reactive hyperemia on a bony prominence despite use of static support Potential adverse effects: dehydration, sensory deprivation, loss of muscle strength, difficulty with mobilization
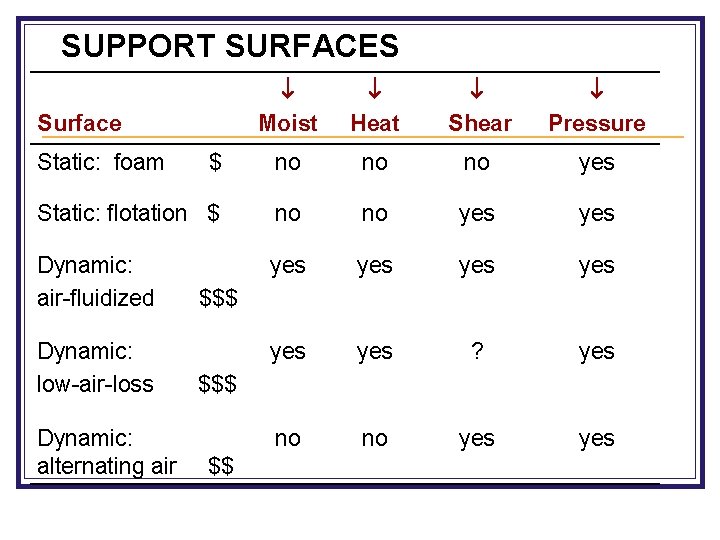
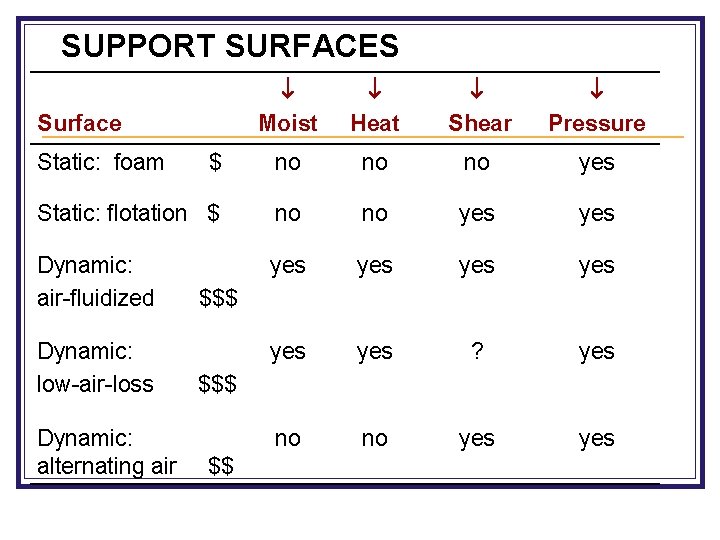
SUPPORT SURFACES Moist Heat Shear Pressure $ no no no yes Static: flotation $ no no yes Dynamic: air-fluidized yes yes yes ? yes no no yes Surface Static: foam Dynamic: low-air-loss Dynamic: alternating air $$$ $$
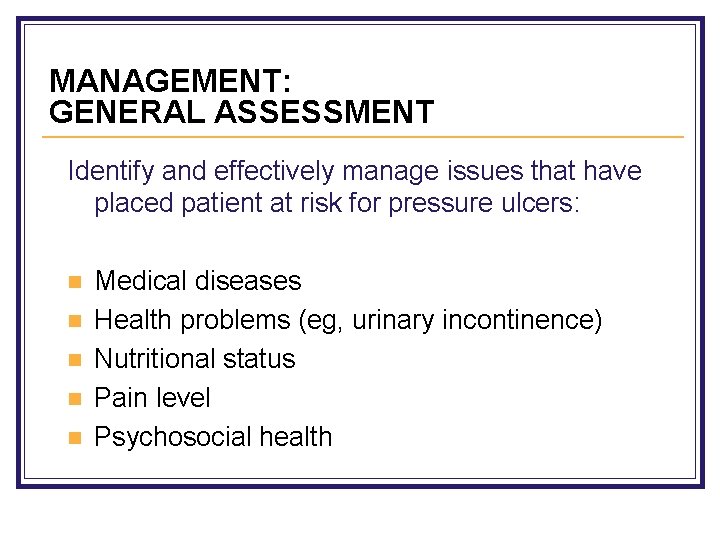
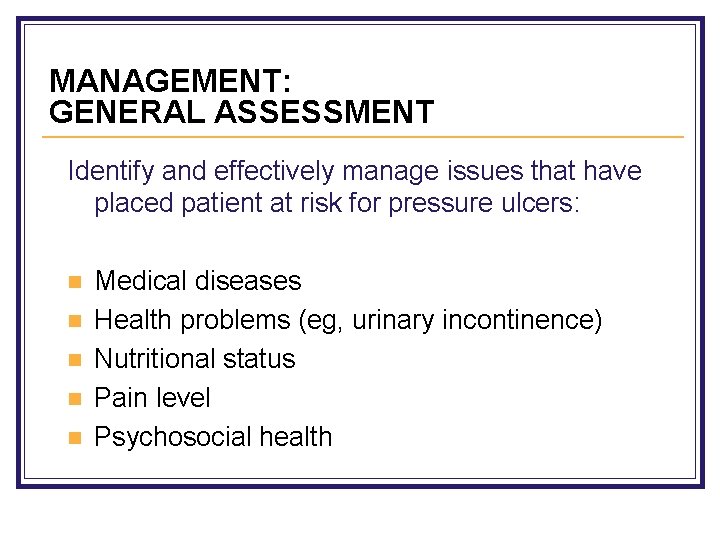
MANAGEMENT: GENERAL ASSESSMENT Identify and effectively manage issues that have placed patient at risk for pressure ulcers: n n n Medical diseases Health problems (eg, urinary incontinence) Nutritional status Pain level Psychosocial health
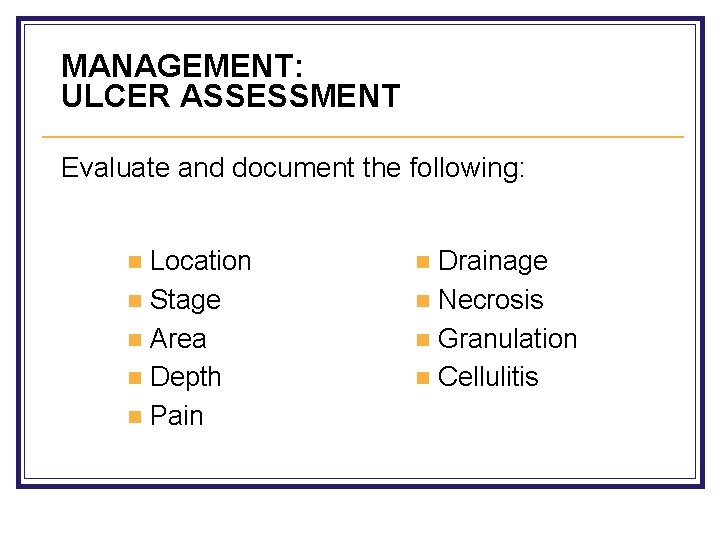
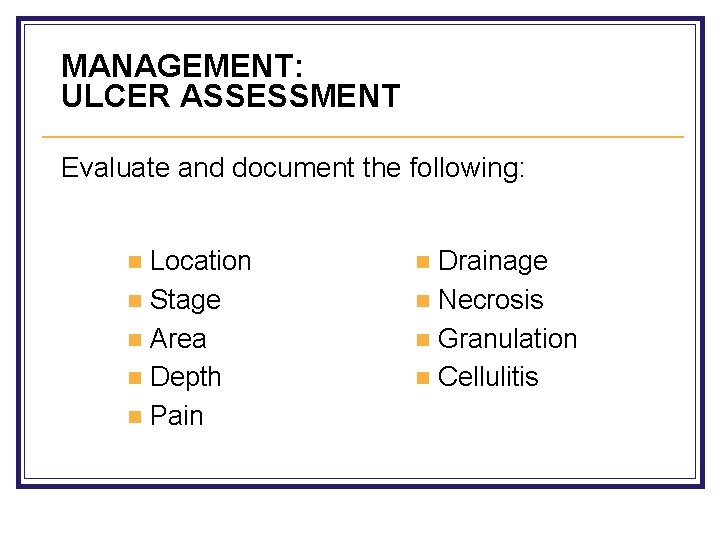
MANAGEMENT: ULCER ASSESSMENT Evaluate and document the following: Location n Stage n Area n Depth n Pain n Drainage n Necrosis n Granulation n Cellulitis n
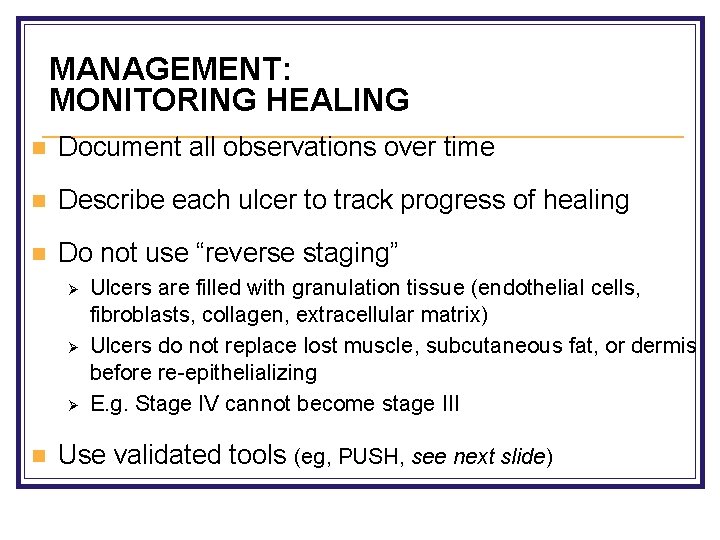
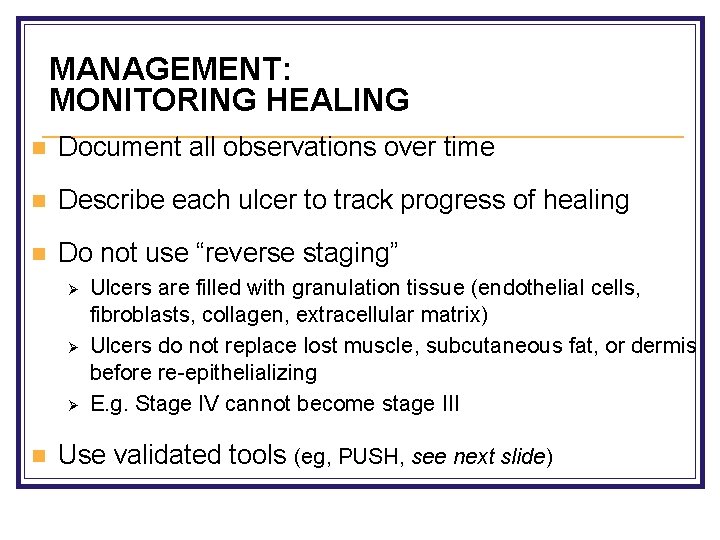
MANAGEMENT: MONITORING HEALING n Document all observations over time n Describe each ulcer to track progress of healing n Do not use “reverse staging” Ø Ø Ø n Ulcers are filled with granulation tissue (endothelial cells, fibroblasts, collagen, extracellular matrix) Ulcers do not replace lost muscle, subcutaneous fat, or dermis before re-epithelializing E. g. Stage IV cannot become stage III Use validated tools (eg, PUSH, see next slide)
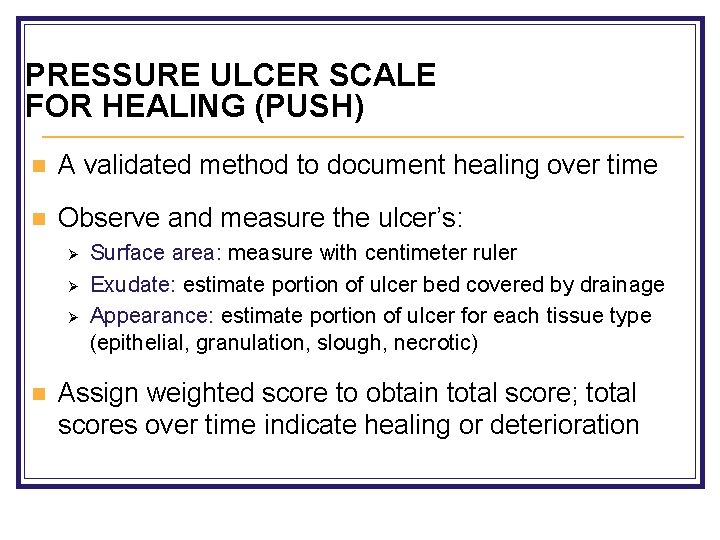
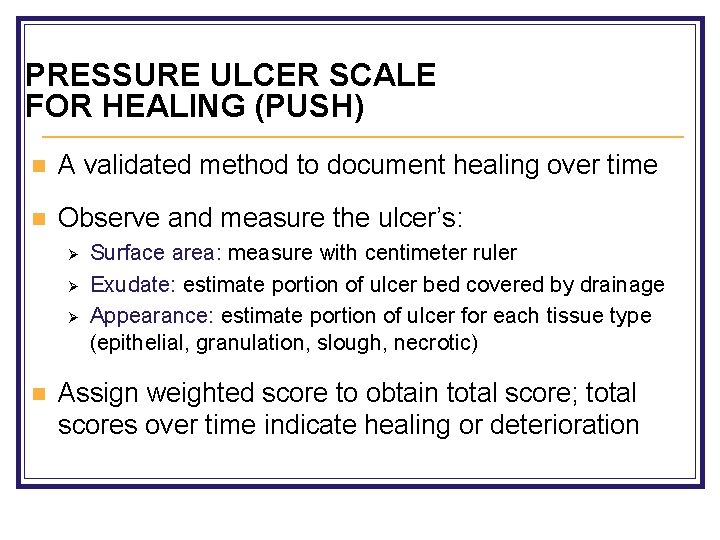
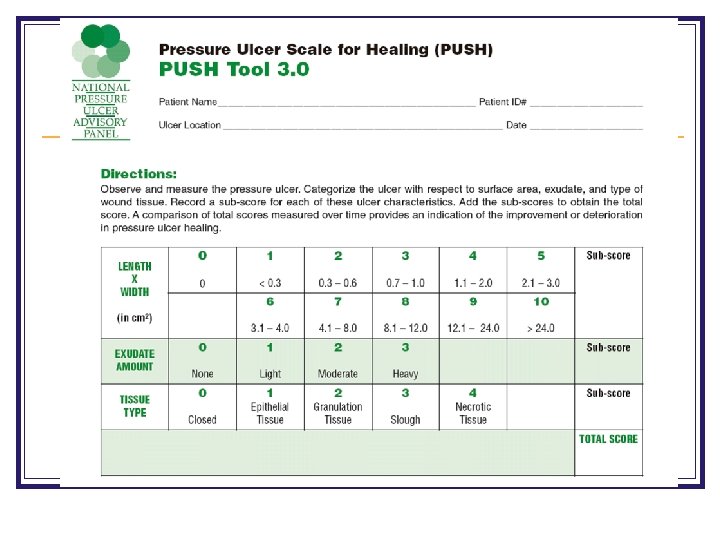
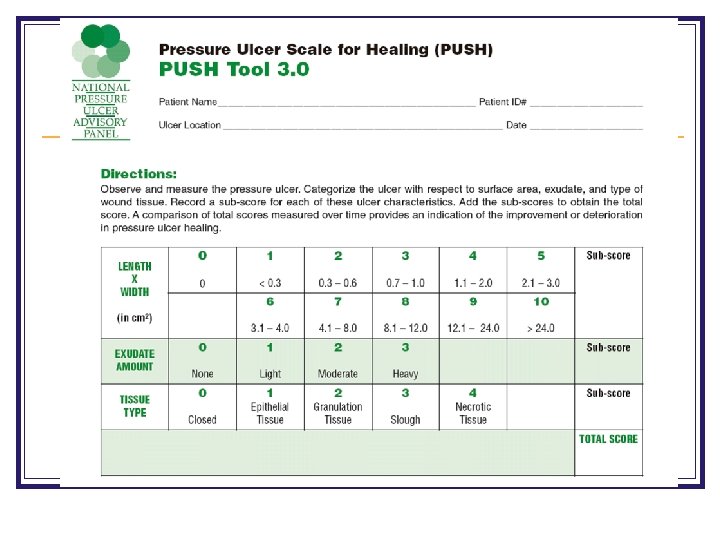
PRESSURE ULCER SCALE FOR HEALING (PUSH) n A validated method to document healing over time n Observe and measure the ulcer’s: Ø Ø Ø n Surface area: measure with centimeter ruler Exudate: estimate portion of ulcer bed covered by drainage Appearance: estimate portion of ulcer for each tissue type (epithelial, granulation, slough, necrotic) Assign weighted score to obtain total score; total scores over time indicate healing or deterioration

Evidence for Wound Assessments n No direct evidence that wound assessments improve clinical outcomes, but has been found that identifying wound characteristics can predict time to healing n Adequate assessment guides treatment, provides data for comparison and can help predict time to healing
MANAGEMENT: CONTROL OF INFECTIONS n Wound cleansing and dressing are the key n n n frequency when purulent or foul-smelling drainage is first observed Avoid topical antiseptics because of their tissue toxicity With failure to heal or persistent exudate after 2 weeks of optimal cleansing, consider trial of topical antibiotics
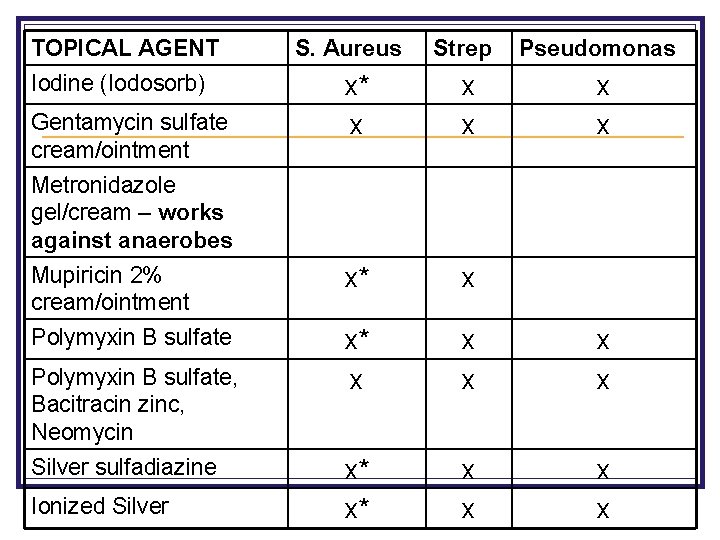
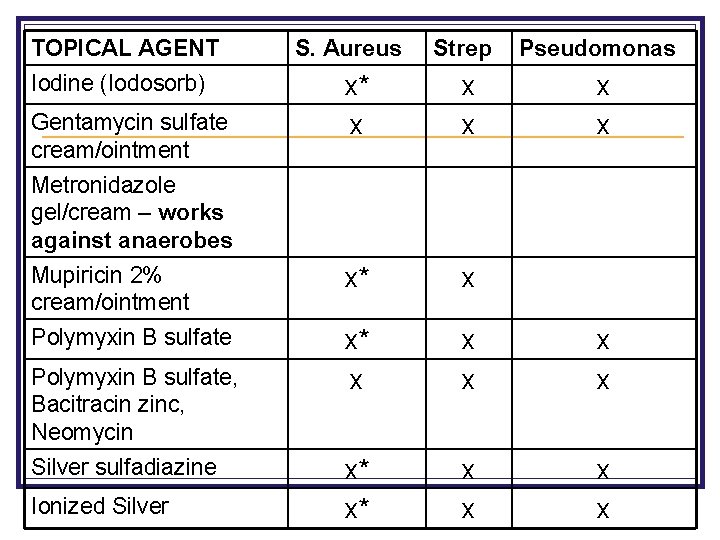
TOPICAL AGENT Strep Pseudomonas x* x x x Mupiricin 2% cream/ointment x* x Polymyxin B sulfate x* x x x* x* x x Iodine (Iodosorb) Gentamycin sulfate cream/ointment S. Aureus Metronidazole gel/cream – works against anaerobes Polymyxin B sulfate, Bacitracin zinc, Neomycin Silver sulfadiazine Ionized Silver
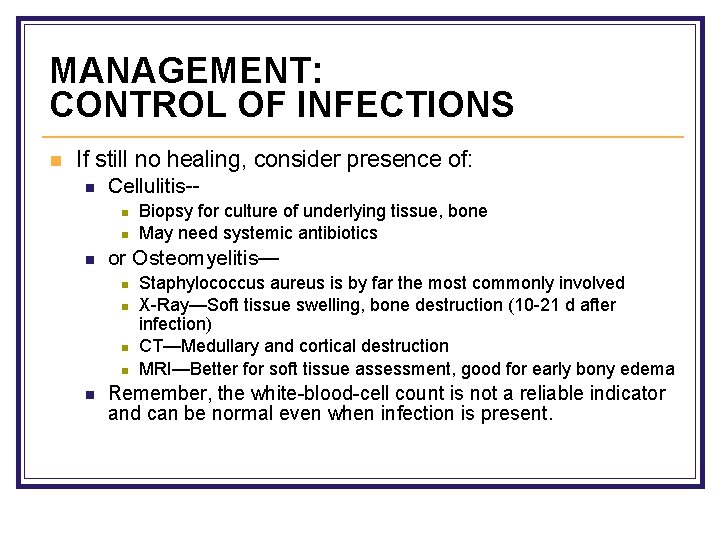
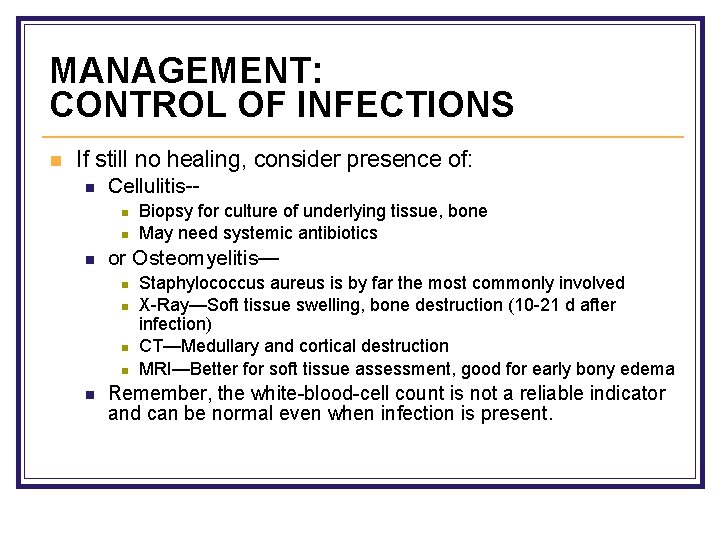
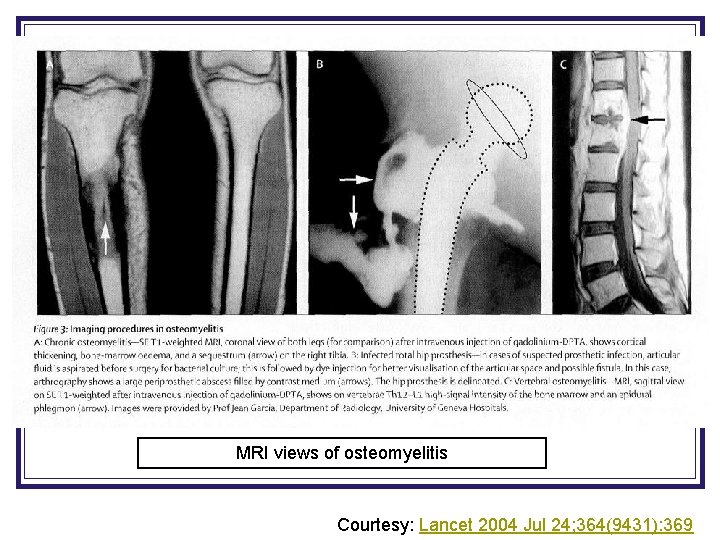
MANAGEMENT: CONTROL OF INFECTIONS n If still no healing, consider presence of: n Cellulitis-n n n or Osteomyelitis— n n n Biopsy for culture of underlying tissue, bone May need systemic antibiotics Staphylococcus aureus is by far the most commonly involved X-Ray—Soft tissue swelling, bone destruction (10 -21 d after infection) CT—Medullary and cortical destruction MRI—Better for soft tissue assessment, good for early bony edema Remember, the white-blood-cell count is not a reliable indicator and can be normal even when infection is present.
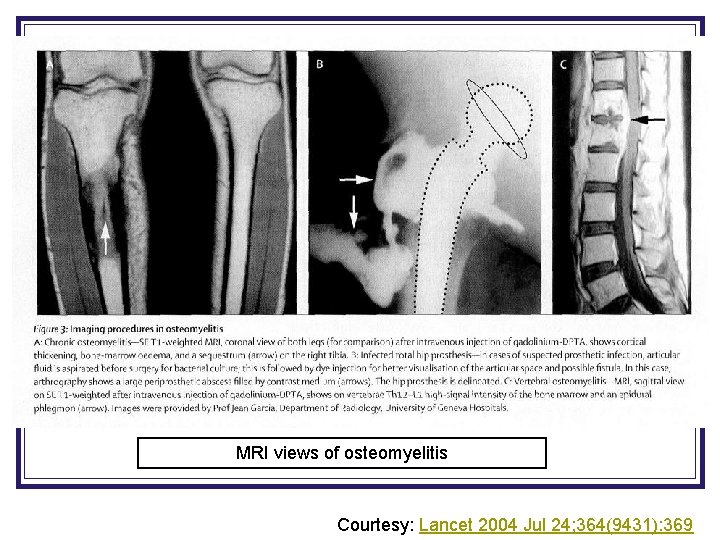
MRI views of osteomyelitis Courtesy: Lancet 2004 Jul 24; 364(9431): 369
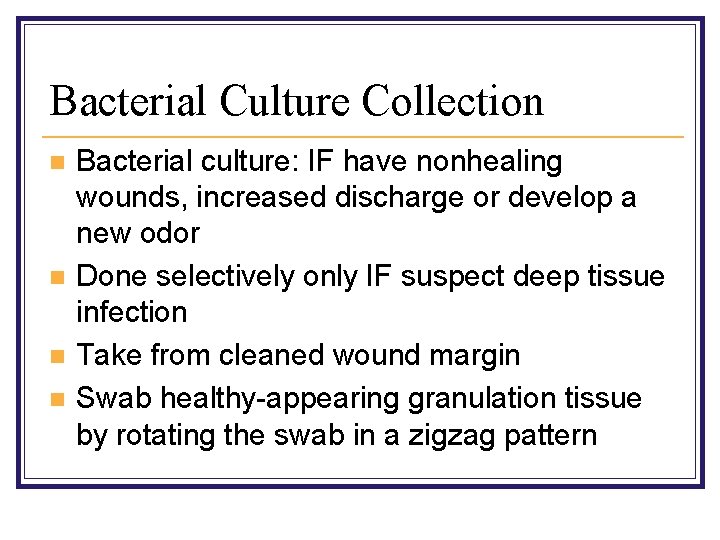
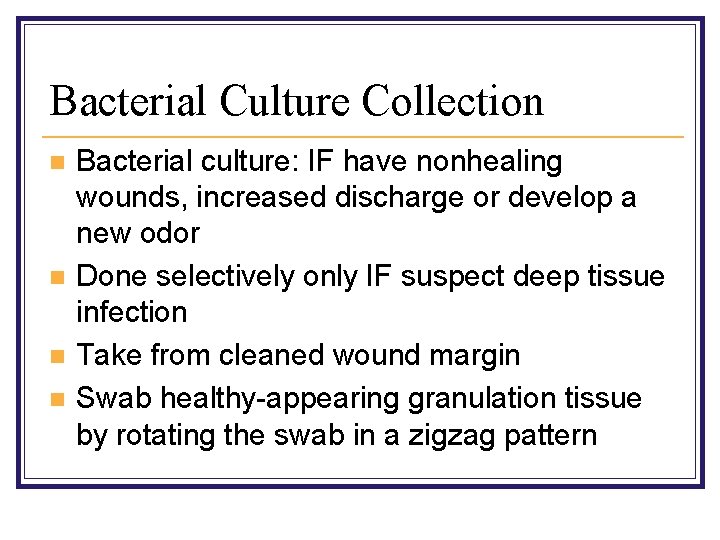
Bacterial Culture Collection n n Bacterial culture: IF have nonhealing wounds, increased discharge or develop a new odor Done selectively only IF suspect deep tissue infection Take from cleaned wound margin Swab healthy-appearing granulation tissue by rotating the swab in a zigzag pattern
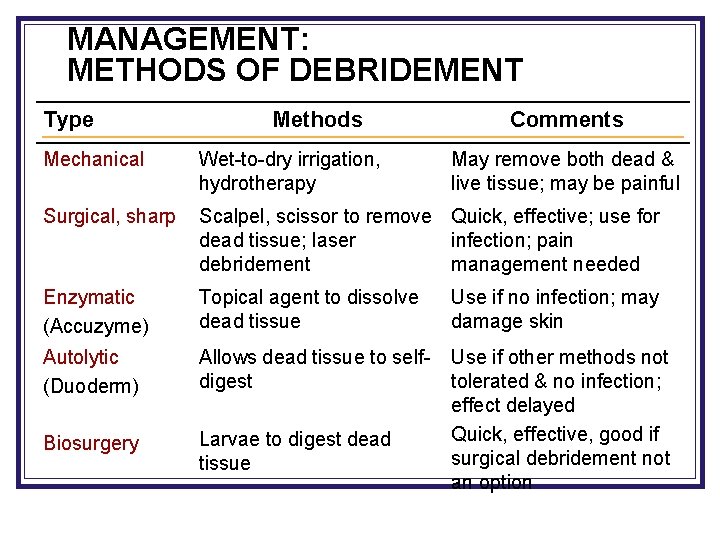
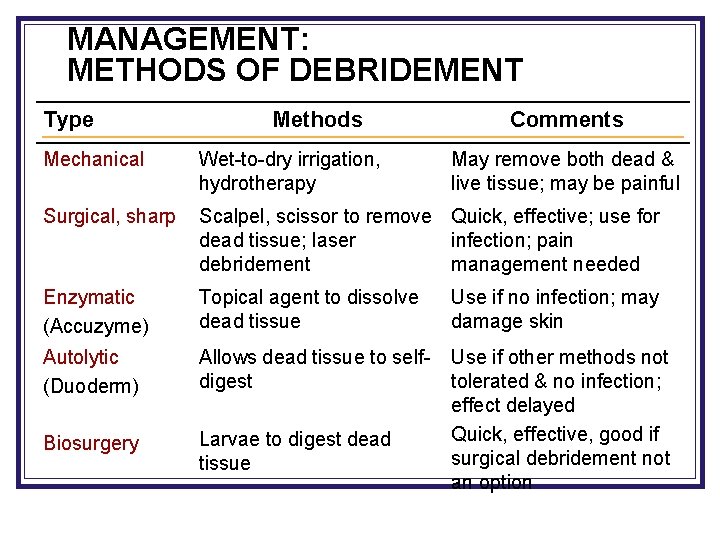
MANAGEMENT: METHODS OF DEBRIDEMENT Type Methods Comments Mechanical Wet-to-dry irrigation, hydrotherapy May remove both dead & live tissue; may be painful Surgical, sharp Scalpel, scissor to remove Quick, effective; use for dead tissue; laser infection; pain debridement management needed Enzymatic (Accuzyme) Topical agent to dissolve dead tissue Use if no infection; may damage skin Autolytic (Duoderm) Allows dead tissue to selfdigest Biosurgery Larvae to digest dead tissue Use if other methods not tolerated & no infection; effect delayed Quick, effective, good if surgical debridement not an option
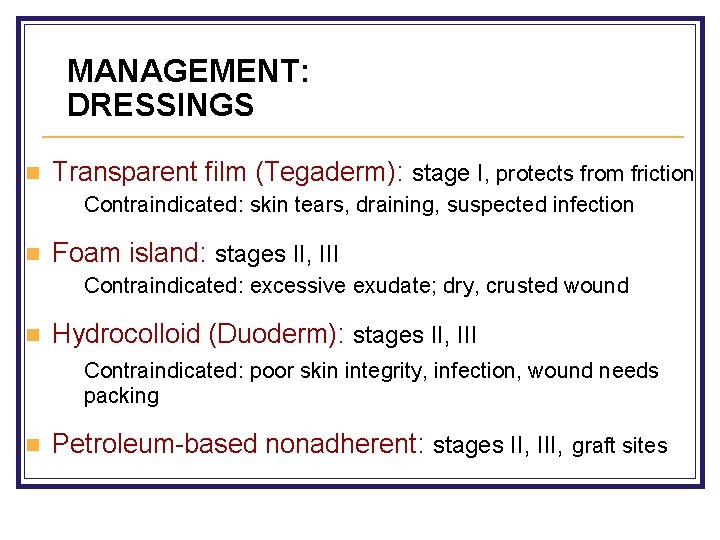
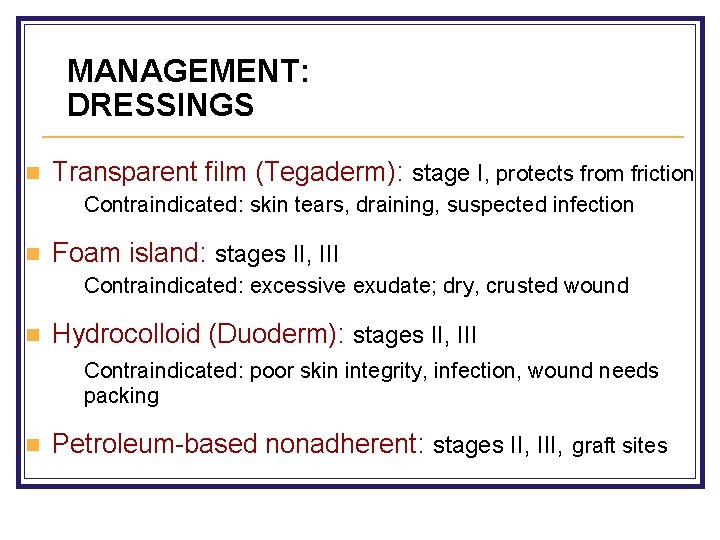
MANAGEMENT: DRESSINGS n Transparent film (Tegaderm): stage I, protects from friction Contraindicated: skin tears, draining, suspected infection n Foam island: stages II, III Contraindicated: excessive exudate; dry, crusted wound n Hydrocolloid (Duoderm): stages II, III Contraindicated: poor skin integrity, infection, wound needs packing n Petroleum-based nonadherent: stages II, III, graft sites
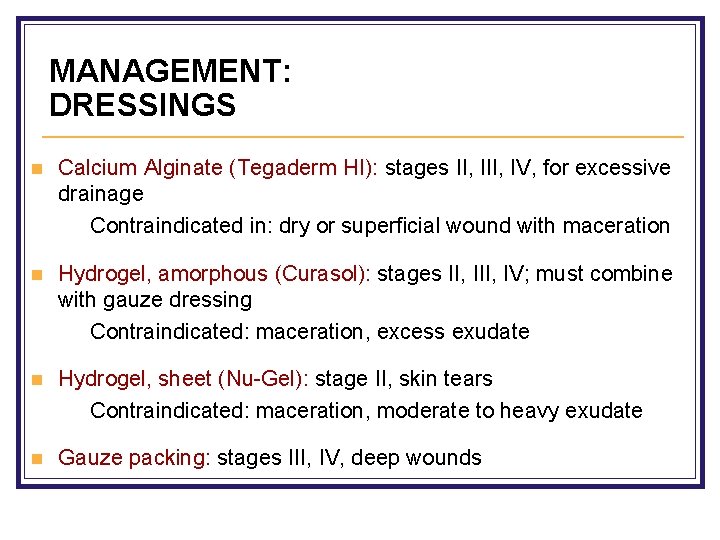
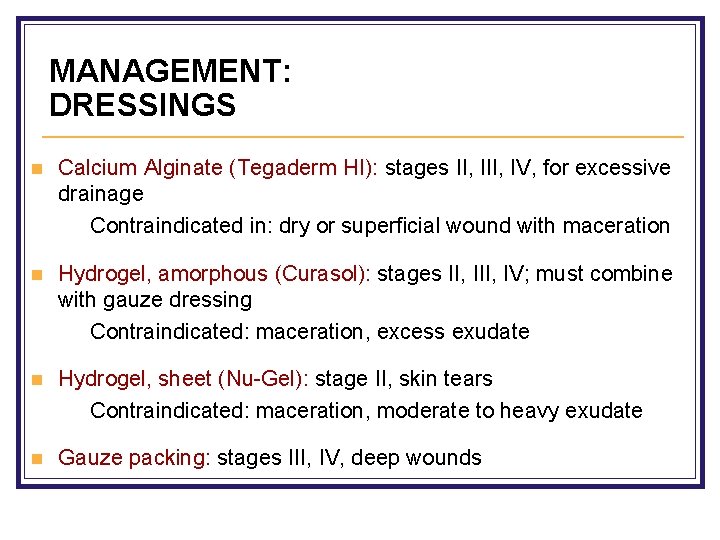
MANAGEMENT: DRESSINGS n Calcium Alginate (Tegaderm HI): stages II, IV, for excessive drainage Contraindicated in: dry or superficial wound with maceration n Hydrogel, amorphous (Curasol): stages II, IV; must combine with gauze dressing Contraindicated: maceration, excess exudate n Hydrogel, sheet (Nu-Gel): stage II, skin tears Contraindicated: maceration, moderate to heavy exudate n Gauze packing: stages III, IV, deep wounds
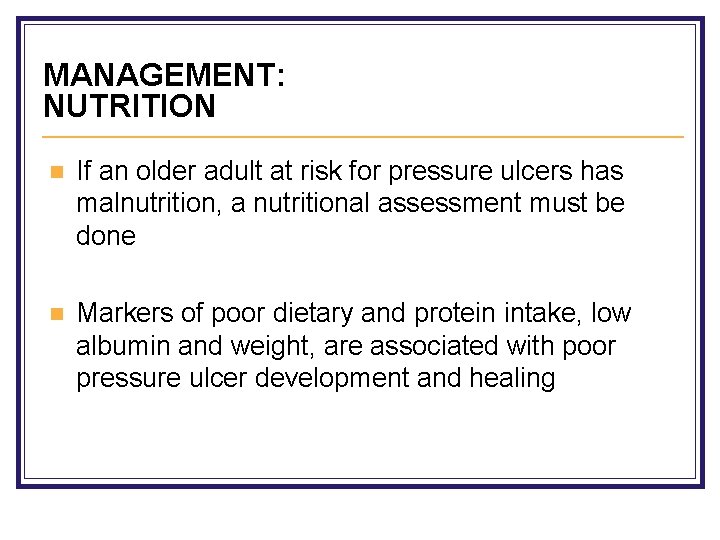
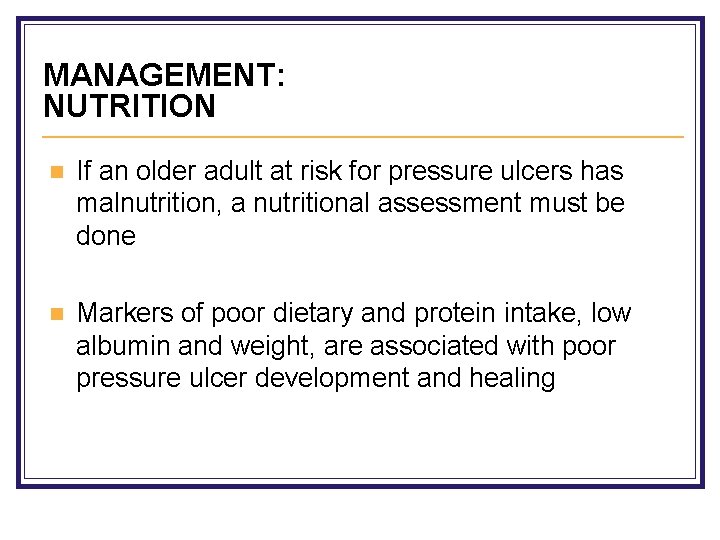
MANAGEMENT: NUTRITION n If an older adult at risk for pressure ulcers has malnutrition, a nutritional assessment must be done n Markers of poor dietary and protein intake, low albumin and weight, are associated with poor pressure ulcer development and healing
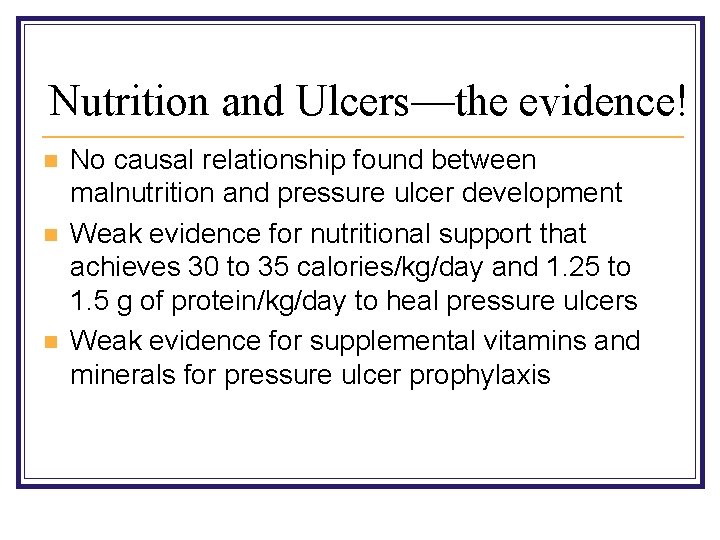
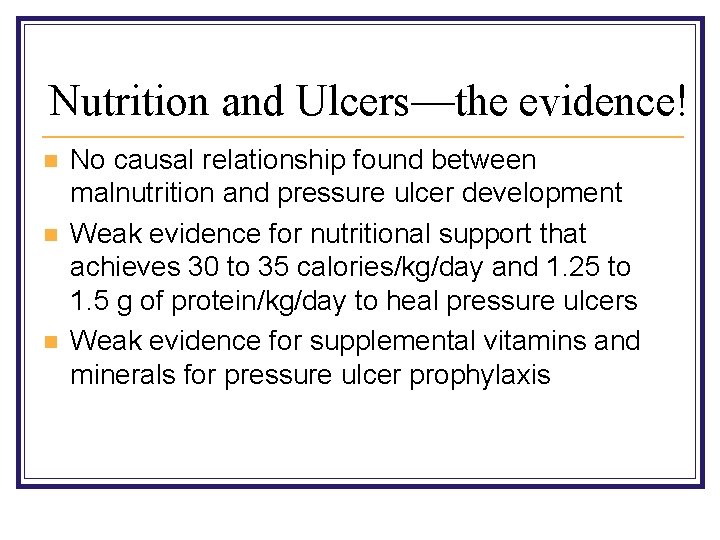
Nutrition and Ulcers—the evidence! n n n No causal relationship found between malnutrition and pressure ulcer development Weak evidence for nutritional support that achieves 30 to 35 calories/kg/day and 1. 25 to 1. 5 g of protein/kg/day to heal pressure ulcers Weak evidence for supplemental vitamins and minerals for pressure ulcer prophylaxis
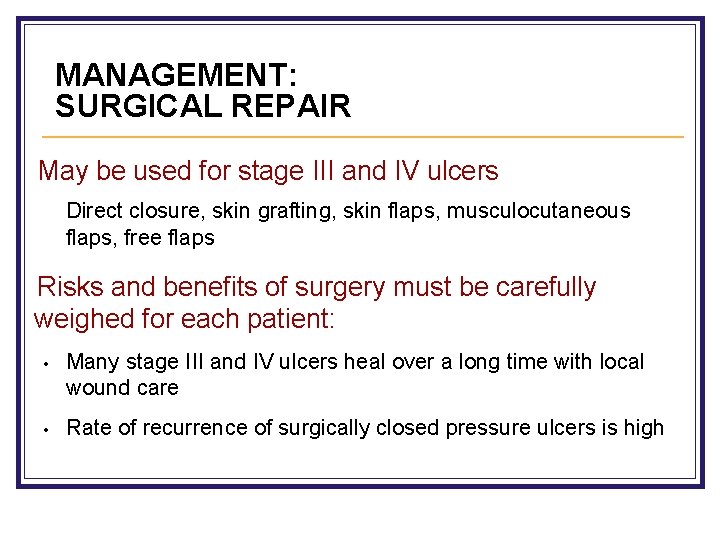
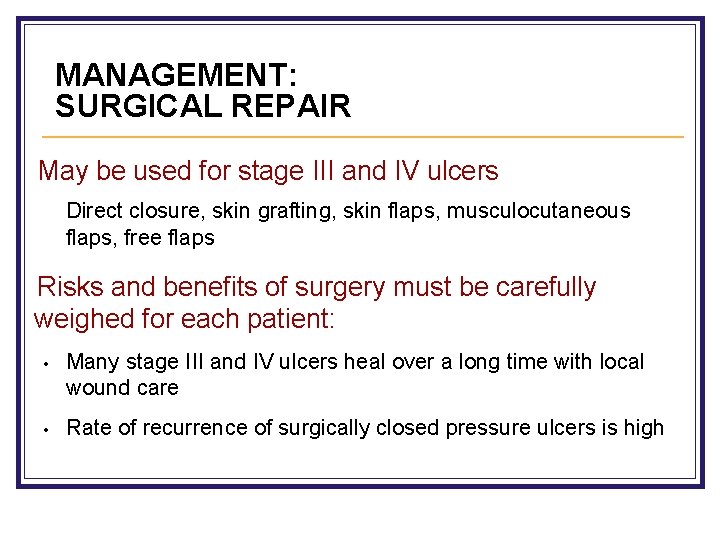
MANAGEMENT: SURGICAL REPAIR May be used for stage III and IV ulcers Direct closure, skin grafting, skin flaps, musculocutaneous flaps, free flaps Risks and benefits of surgery must be carefully weighed for each patient: • Many stage III and IV ulcers heal over a long time with local wound care • Rate of recurrence of surgically closed pressure ulcers is high
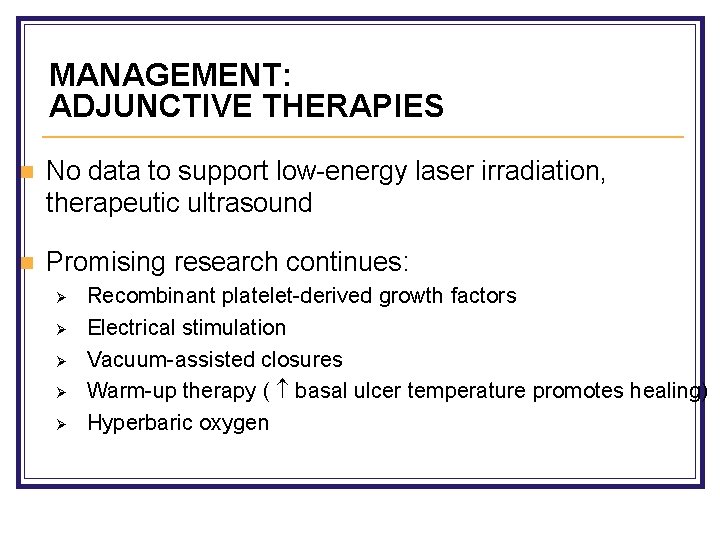
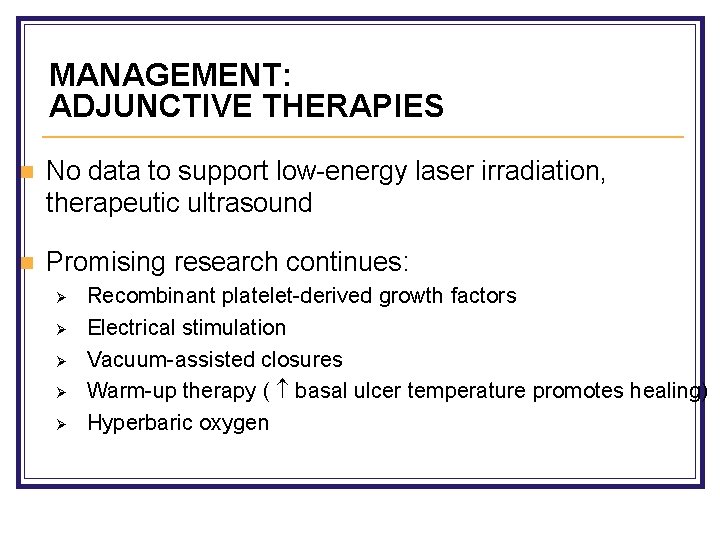
MANAGEMENT: ADJUNCTIVE THERAPIES n No data to support low-energy laser irradiation, therapeutic ultrasound n Promising research continues: Ø Ø Ø Recombinant platelet-derived growth factors Electrical stimulation Vacuum-assisted closures Warm-up therapy ( basal ulcer temperature promotes healing) Hyperbaric oxygen
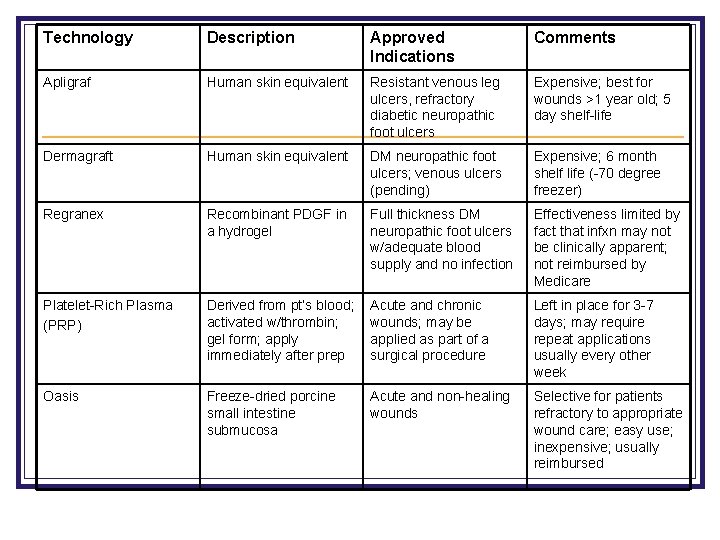
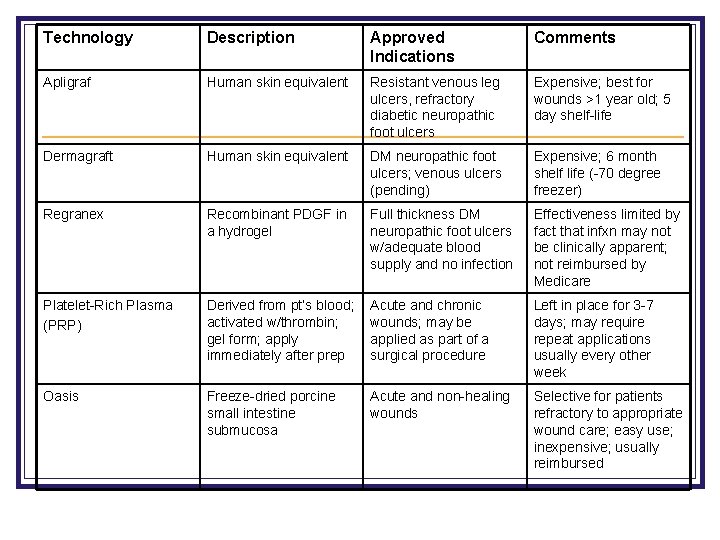
Technology Description Approved Indications Comments Apligraf Human skin equivalent Resistant venous leg ulcers, refractory diabetic neuropathic foot ulcers Expensive; best for wounds >1 year old; 5 day shelf-life Dermagraft Human skin equivalent DM neuropathic foot ulcers; venous ulcers (pending) Expensive; 6 month shelf life (-70 degree freezer) Regranex Recombinant PDGF in a hydrogel Full thickness DM neuropathic foot ulcers w/adequate blood supply and no infection Effectiveness limited by fact that infxn may not be clinically apparent; not reimbursed by Medicare Platelet-Rich Plasma (PRP) Derived from pt’s blood; activated w/thrombin; gel form; apply immediately after prep Acute and chronic wounds; may be applied as part of a surgical procedure Left in place for 3 -7 days; may require repeat applications usually every other week Oasis Freeze-dried porcine small intestine submucosa Acute and non-healing wounds Selective for patients refractory to appropriate wound care; easy use; inexpensive; usually reimbursed
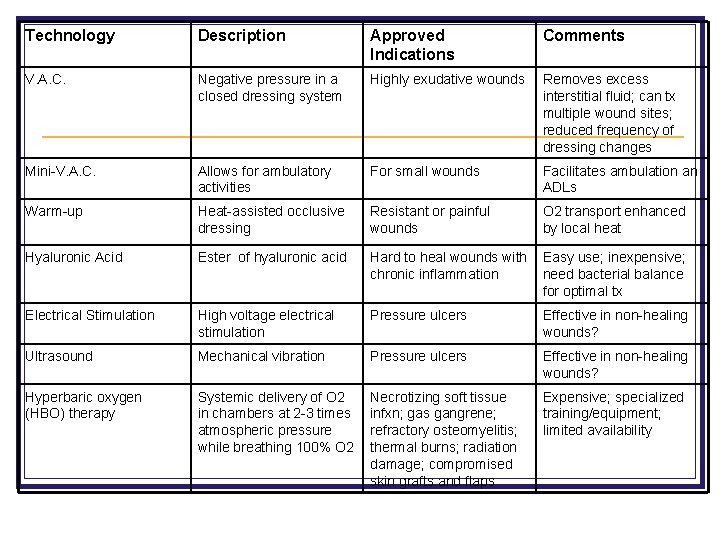
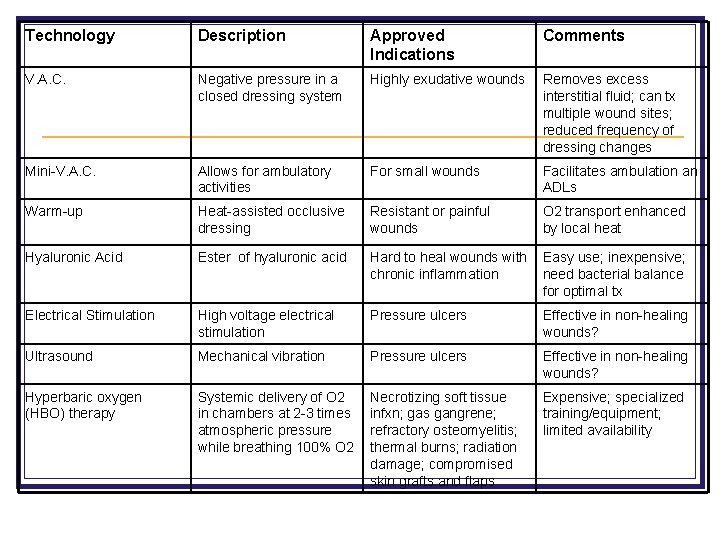
Technology Description Approved Indications Comments V. A. C. Negative pressure in a closed dressing system Highly exudative wounds Removes excess interstitial fluid; can tx multiple wound sites; reduced frequency of dressing changes Mini-V. A. C. Allows for ambulatory activities For small wounds Facilitates ambulation an ADLs Warm-up Heat-assisted occlusive dressing Resistant or painful wounds O 2 transport enhanced by local heat Hyaluronic Acid Ester of hyaluronic acid Hard to heal wounds with chronic inflammation Easy use; inexpensive; need bacterial balance for optimal tx Electrical Stimulation High voltage electrical stimulation Pressure ulcers Effective in non-healing wounds? Ultrasound Mechanical vibration Pressure ulcers Effective in non-healing wounds? Hyperbaric oxygen (HBO) therapy Systemic delivery of O 2 in chambers at 2 -3 times atmospheric pressure while breathing 100% O 2 Necrotizing soft tissue infxn; gas gangrene; refractory osteomyelitis; thermal burns; radiation damage; compromised skin grafts and flaps Expensive; specialized training/equipment; limited availability
SUMMARY n Older adults are at high risk for development of pressure ulcers n Pressure ulcers may result in serious morbidity and mortality n Techniques that reduce pressure, moisture, friction, and shear can prevent pressure ulcers n Pressure ulcers should be treated with proper cleansing, dressings, debridement, or surgery as indicated
References n n n Geriatrics Review Syllabus, 6 th edition, p 259 -268 Bates-Jensen, B et al. Quality Indicators for the care of pressure ulcers in vulnerable elders; JAGS: 55: S 409 -S 416, October 2007 AHCPR, Pressure Ulcers in Adults: Prediction and Prevention. Rockville, MD: US Dept of Health and Human Services, Public Health Service, Agency for Healthcare Policy and Research. May 1992 Fowler E, Krasner D, et al. Healing Environments for chronic wound care: optimizing local wound management as a component of holistic interdisciplinary patient care. Treatment of Chronic Wounds: Number 11 in a series. Krasner D, Margolis DJ, et al. Prevention and management of pressure ulcers. Treatment of Chronic Wounds: Number 6 in a series. Patterson, BL. A Pictorial Guide to Pressure Ulcers. Consultant. Feb 2006: 205 -8.
References n http: //www. nursingquality. org/NDNQIPressure. Ulcer. Train ing/index 2. htm n n www. medicaledu. com - Wound Care Information Network www. etrs. org – European Tissue Repair Society www. woundsource. com n http: //www. npuap. org/PDF/push 3. pdf n n Sussman C, Bates-Jensen BM. Wound Care: A Collaborative Practice Manual for Physical Therapists and Nurses. 1 st edition. 1998. Ham et al, Primary Care Geriatrics, 3 rd ed. , p. 431 -439 n Lancet 2004 Jul 24; 364(9431): 369 n