PRESSURE ULCER PROGRAM Developed by HELEN HOLDER RN
PRESSURE ULCER PROGRAM Developed by HELEN HOLDER RN, BSN Alverno College Milwaukee holderhc@alverno. edu
This site was designed with nursing assistants in mind! You’ll learn: What is a pressure ulcer? What is really going on under the skin? What part does nutrition play? What part do you play to keep them away?
What should I know after viewing this site? • Be able to name layers and functions of the skin. • Name those at risk. • Explain how pressure ulcers are formed. • Become aware of complications from pressure ulcers • Understand the importance of nutrition. • Identify the important prevention techniques used by CNA’s. Printshop 2005
Why Skin? • One of the largest organs in the body • Vital for homeostasis • Protection • Retards water loss • Regulates body temperature • House of sensory nerves • Contains immune system cells • Breaks down and uses various chemicals • Excretes waste Printshop 2005
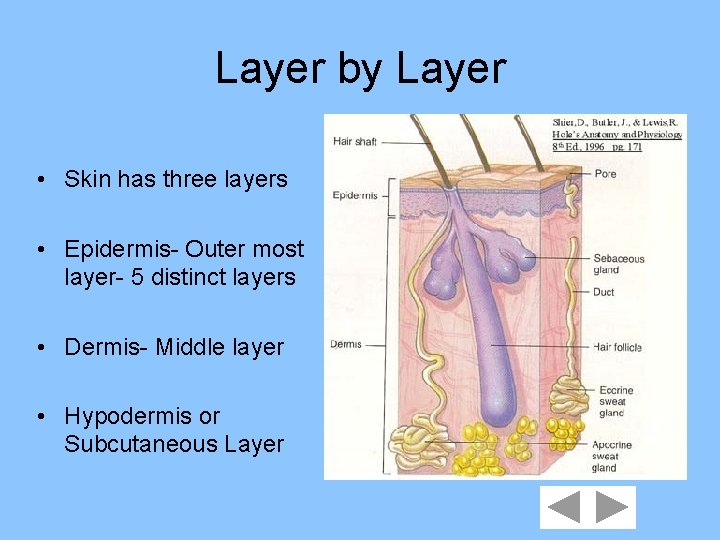
Layer by Layer • Skin has three layers • Epidermis- Outer most layer- 5 distinct layers • Dermis- Middle layer • Hypodermis or Subcutaneous Layer
EPIDERMIS • Lacks blood vessels • Cells reproduce & grow and shed as “dry skin” • Contains melanocytes for skin color • Thickest area of epidermis: palms & soles
DERMIS • • • Contains blood vessels Binds epidermis to underlying tissue Contains muscle fibers-arrector pili Nerves scattered through out Contains hair follicles, sebaceous & sweat glands • Thickness: 0. 5 mm eyelids to 3. 0 mm soles
HYPODERMIS • • Subcutaneous Loose connective tissue & adipose tissue Thickness varies Holds major vessels in place that supply blood to skin • Insulates body • No definition from dermal layer
A function of the skin is? • Tan nicely • Excrete waste known as diarrhea • Regulate the temperature of the body
Name that layer! • Name the layer that contains muscle fiber. • Dermis • Subcutaneous • Epidermis
Genetic Connection • NONE Those at risk: people with Peripheral vascular disease Diabetes Paralysis of limbs Casts Obese/Thin Printshop 2005
Picture This • Crowded church, packed pews, no cushions, sermon that goes on forever and no one can move. Once you have positioned yourself you are stuck for the duration. How does it feel on your hips and tailbone? We’re talking real pressure! Now think about how someone with no control over their movements feels. Perfect set up for pressure ulcers! Printshop 2005

How does that ulcer form? • Resident lying in bed on their back. • Buttocks, by force of gravity sink into mattress. • Soft tissue presses against the bones that don’t go anywhere. • Blood vessels are pinched between bone and weight of gravity. • Blood flow to soft tissue is cut off. • Cell starvation and death occur • Pressure ulcer is born.
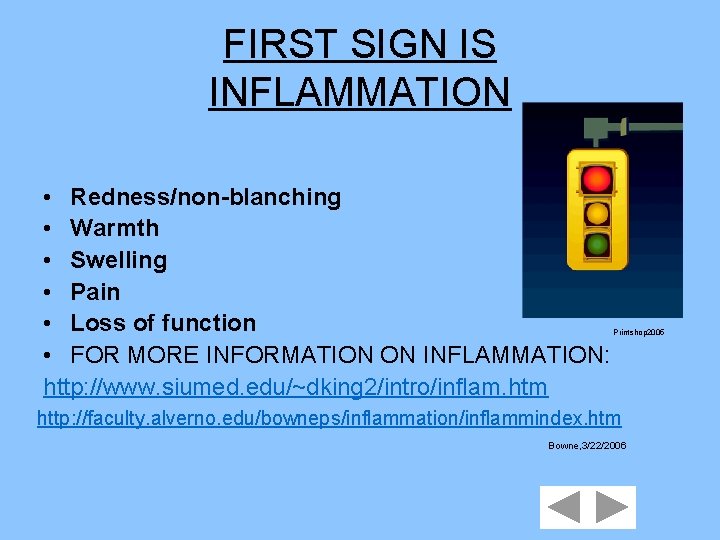
FIRST SIGN IS INFLAMMATION • Redness/non-blanching • Warmth • Swelling • Pain • Loss of function • FOR MORE INFORMATION ON INFLAMMATION: http: //www. siumed. edu/~dking 2/intro/inflam. htm Printshop 2005 http: //faculty. alverno. edu/bowneps/inflammation/inflammindex. htm Bowne, 3/22/2006

Staging • 4 levels progression • No open area Deep wound Printshop 2005
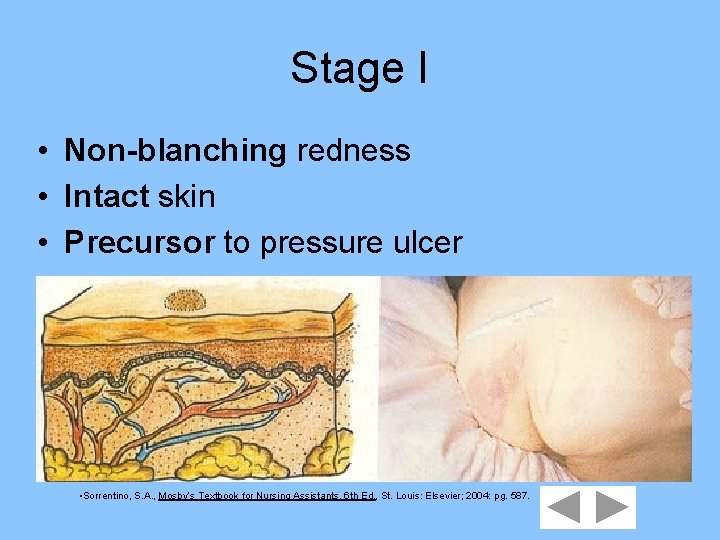
Stage I • Non-blanching redness • Intact skin • Precursor to pressure ulcer • Sorrentino, S. A. , Mosby’s Textbook for Nursing Assistants, 6 th Ed. , St. Louis: Elsevier; 2004: pg. 587.

Stage II Partial thickness skin loss • Abrasion • • Blister • Shallow Crater • Sorrentino, S. A. , Mosby’s Textbook for Nursing Assistants, 6 th Ed. , St. Louis: Elsevier; 2004: pg. 587.
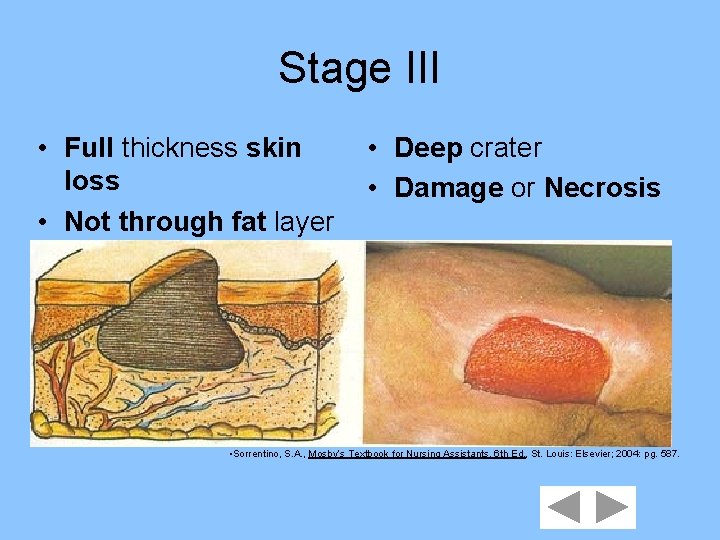
Stage III • Full thickness skin loss • Not through fat layer • Deep crater • Damage or Necrosis • Sorrentino, S. A. , Mosby’s Textbook for Nursing Assistants, 6 th Ed. , St. Louis: Elsevier; 2004: pg. 587.
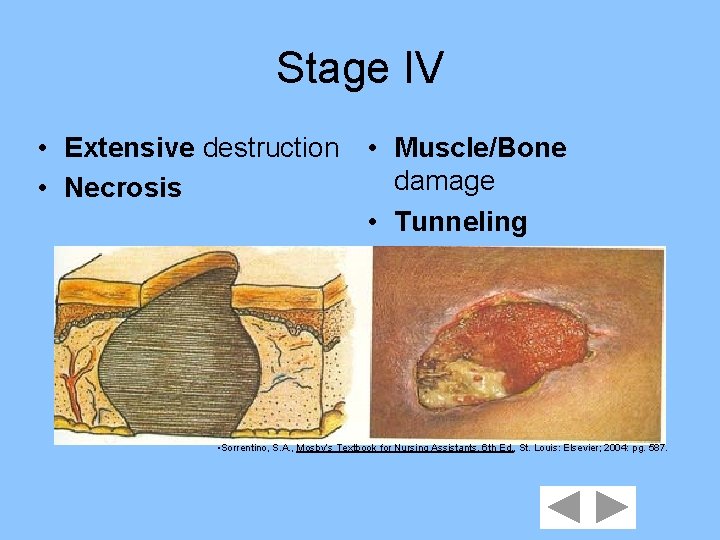
Stage IV • Extensive destruction • Muscle/Bone damage • Necrosis • Tunneling • Sorrentino, S. A. , Mosby’s Textbook for Nursing Assistants, 6 th Ed. , St. Louis: Elsevier; 2004: pg. 587.
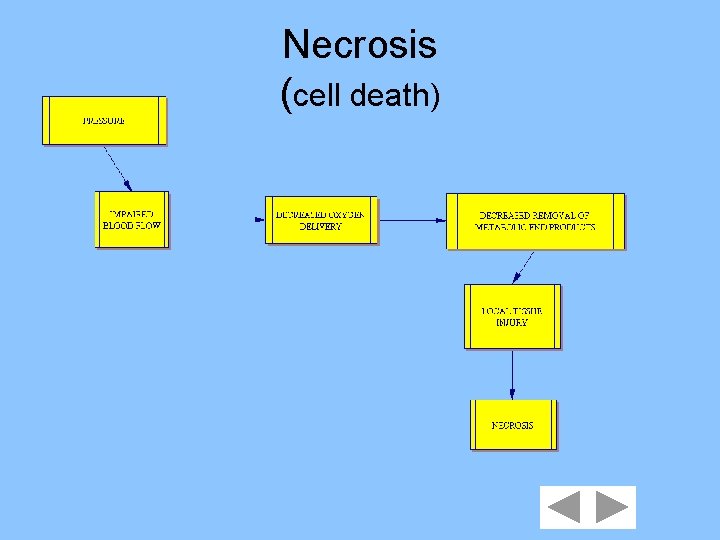
Necrosis (cell death)
What is one of the First Signs of Inflammation ? • Blanching • Warmth • Stress
Blanching • Inflammation is characterized by redness at the site of tissue injury. If you lightly put your finger on the reddened area and exert slight pressure the area will not “whiten” or blanch. Printshop 2005
Warmth • Correct. Warmth is an indicator of inflammation due to the increased blood flow to the area. Printshop 2005
Stress • Try again. Stress may lead to a different type of ulcer but doesn’t usually lead to a “pressure” ulcer. Printshop 2005
A characteristic of Stage II is ? • Blister • Full thickness skin loss • Tunneling
Yahoo! • Blistering is one of the early characteristics of the Stage II pressure ulcer. Printshop 2005
No • Full thickness skin loss happens in the Stage III pressure ulcer. The wound will appear as an open area and necrosis may be visible.
Try again • Tunneling happens during Stage VI. Wounds will begin to produce deeper pockets as the tissue is eroded away. The pocket may be narrow and proceed to another area of tissue, hence the term “tunnel”. Printshop 2005
Factors that lead to Pressure Ulcers • Malnutrition Low protein intake Inability to feed self • Immobility • Incontinence urine/feces on skin Printshop 2005
Warning Signs of Malnutrition • Sudden/Recent weight loss • Dehydration • Decrease appetite Printshop 2005

What is Needed? • Elderly need at least 1200 calories/day • Protein- for repair & regrowth • Carbohydrates & Fats-Tissue maintenance & energy source • Vitamins- promote wound healing Printshop 2005
Protein • Best Sources: eggs milk cheese yogurt Printshop 2005
Carbohydrates & Fats • Carb sources Whole grains Cereal Rice • Unsaturated fats Olive oil Canola oil Safflower oil Printshop 2005
Vitamins • Vitamin C- for collagen formation Good Sources: Citrus fruit strawberries • Vitamins A & E- for tissue repair Good Sources: orange & green vegetables • Vitamin K- for normal blood clotting Good Sources: Green leafy vegetables Printshop 2005
Name a Symptom of Malnutrition • Sudden weight gain • Consistently decreased appetite • Excessive thirst
NO • Sudden or recent weight loss is a symptom of malnutrition Printshop 2005

You’re Right • An elderly person that is not consistently eating at least 1200 calories per day, may be headed for the state of malnutrition Printshop 2005

Check again! • Dehydration is a sign of malnutrition. Excessive thirst is a symptom of Diabetes. Printshop 2005
Good Source of Vitamin C? • Green leafy vegetables • Liver • Strawberries
Not this time • Vitamin K is found in green leafy vegetables Printshop 2005
Not Liver • Liver is high in iron and cholesterol but not Vitamin C Printshop 2005
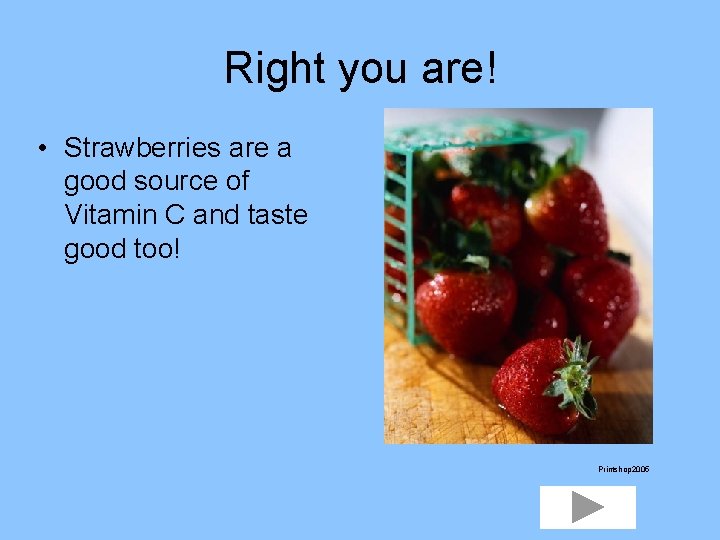
Right you are! • Strawberries are a good source of Vitamin C and taste good too! Printshop 2005

PREVENTION • Best protections against pressure ulcers is observation, good skin care, mobility, and good nutrition. • CNA’s importance---most direct contact with residents Microsoft Office XP 2002
CNA Role in Nutrition • Assist at Mealtime make it social and take your time feeding the resident. • Give supplements as required. Ensure or 2 Cal or whatever other supplement is ordered. • Substitute food dislikes for preference. • Report & Record appropriately. Microsoft Office. XP 2002
CNA Role in Immobility • Reduce pressure: Turn bed residents every 2 hours. Even a 15 degree turn helps to relieve pressure on skin surface. Use a written turning schedule so that others know in which direction the resident is to go. Microsoft Office. XP 2002
Positioning • Position correctly! Use pillows to support joints Avoid skin touching skin Check to make sure no body part is hitting a wall or railing Remember! Check positioning in the chairs. Chairs too small or residents that lean to one side may have pressure. Microsoft Office. XP 2002

Keep Resident Moving!! Printshop 2005
Shearing & Friction • Shearing- Skin layers slide in different directions • Friction- causes a rug burn on skin Microsoft Office. XP 2002
Avoid Shearing & Friction • Use lifter sheet to move resident up in bed • Use assistance of over bed trapeze • Keep HOB 30 degrees or lower to avoid slipping down in bed • Cup heels & elbows during ROM exercises • Don’t drag heels over sheets when using lifts. Print. Shop 2005
Importance of Skin Care • Check every 2 hours for incontinence. Feces, urine and even soap are abrasive to the skin due to a ph imbalance. Print. Shop 2005

• Clean, Rinse and thoroughly Dry skin after each incontinent episode. Print. Shop 2005
• Moisturize skin with lotion to prevent dry skin. Use lotion over bony prominences but do not massage reddened areas as it may cause more damage to underlying tissue • Use special barrier creams as ordered Microsoft Outlook. XP 2002
To avoid a shearing incident the CNA should ……. . ? • Elevate the HOB 45 degrees • Use a lifter sheet • Support the head during ROM
Too High! • Never raise the HOB over 30 degrees when a resident is confined to bed. Anything over 30 degrees may cause a shearing incident! Microsoft Office. XP 2002
YEAH!!! • Use the lifter sheet to move resident more easily and saves your back too! Microsoft Office. XP 2002
Not this head! • When doing ROM you want to protect the heels and elbows from dragging across the sheets and causing a friction burn. Microsoft Office. XP 2002
How often do you turn a bed ridden resident? • Every 30 minutes • Every 4 hours • Every 2 hours

That’s Lunch! • This is the time allotment for your lunch. It is important that you take care of yourself and don’t skip that part of your day! Microsoft Office. XP 2002
TPR • Temperature, Pulse, and Respirations are usually done every 4 hours on residents that may be ill. For the bedridden resident, this is far too long to lay in one position! Microsoft Office. XP 2002
YES! • Remember to turn your bedridden resident every 2 hours to prevent pressure ulcers. Microsoft Office. XP 2002
You never have to worry about residents that sit in wheelchairs. • TRUE • FALSE
Wrong! • Residents don’t always sit nor are they always positioned in the wheelchair correctly. Take a minute to make sure there are no areas rubbing or resting against hardware on the wheelchair. Microsoft Office. XP 2002
Correct • You must have checked your resident after you positioned them. Obviously there are no areas pressed against the hardware of the wheelchair! Microsoft Office. XP 2002

BEST PREVENTION • Superior Care! • Keen Observation! • Prompt Reporting! Print. Shop 2005
References • Slide 5 - Shier, D. , Butler, J. , & Lewis, R. , 1996. Hole’s anatomy & physiology, 8 th Ed. , Mc. Graw-Hill; pg. 171. • Slides 22 -25 - Sorrentino, S. A. , 2004. Mosby’s Textbook for Nursing Assistants, 6 th Ed. , St. Louis: Elsevier; pg. 587. • Slide 20 - Bowne, P. , 2004. Inflammation Tutorial. Retrieved on March 22, 2006 from the World Wide Web at http: //facultyalverno. edu/bowneps/inflammation/inflammindex. htm • Slide 20 - King, D. , 2006. Southern Iowa University. Personal communication.
- Slides: 65