PRESENTED BY Ms S V Shekade M Pharm
PRESENTED BY: Ms. S. V. Shekade M. Pharm (Pharmaceutics) DYPIPSR, Pune
CONTENTS • • • INTRODUCTION DEFINITION CLASSIFICATION LOCAL EFFECTOF DIET ON PERIODONTALHEALTH INTERACTION OF IMMUNITY, INFECTION &NUTRITIONAL STATUS NUTRITION AND PERIODONTAL HEALTH INTERRELATIONSHIP EFFECTOF NUTRITION UPON ORAL MICROORGANISMS. HOST NUTRITION AND PLAQUE BIOFILM CONCLUSION REFERENCES
INTRODUCTION • The diet plays primarily a modifying role in the progression of periodontal disease. • Nutrient deficiencies, excesses, or imbalances do not initiate periodontal disease nor do mega doses of supplements cure or prevent periodontal disease. • However, nutrition may alter development, resistance, and/or repair of the periodontium.
DEFINITIONS • DIET: pattern of individual food intake, habit, kind amount of food eaten. • NUTRITION: science of how the body uses food to meet its requirement of growth, repair, development and maintenance. • NUTRITIONALSTATUS: condition of health as it relates to food and nutrient intake, absorption and utilization. • MALNUTRITION: impaired health related to nutrient or caloric deficiency, absorption, utilization or excretion.
BALANCED DIET ABALANCEDDIETis defined as one which contains a variety of foods in such quantities and proportions that the need for energy, amino acids, vitamins, minerals, fats, carbohydrates and other nutrients is adequately met for maintaining health, vitality and general well being and also makes a small provision for extra nutrients to withstand short duration of leanness. – Park. Abalanced diet has become an accepted means to safeguard a population from nutritional deficiencies.
• In constructing balanced diet, following principles has to be followed-- • Daily requirement of protein should be 15 -20 %of daily energy intake. • Fat requirement should be limited to 20 -30 %of daily energy intake. • Carbohydrates rich in natural fibers should constitute remaining energy intake. • Requirements of micronutrients should be met.
INTRODUCTION Nutrition may be defined as the science of food and its relationship to health. It is concerned primarily with the part played by nutrients in body growth, development and maintenance. The word nutrient or “food factor” is used for specific dietary constituents such as proteins, vitamins and minerals. Dietetics is the practical application of the principles of nutrition; it includes the planning of meals for the well and the sick. Good nutrition means “maintaining a nutritional status that enables us to grow well and enjoy good health. ” 7
Protein, carbohydrate and fat had been recognized early in the 19 th century as energy-yielding foods and much attention was paid to their metabolism and contribution to energy requirements. 8
CLASSIFICATION OF FOODS Classification by origin: - Foods of animal origin - Foods of vegetable origin Classification by chemical composition: - Proteins Fats Carbohydrates Vitamins Minerals 9
CLASSIFICATION BY PREDOMINANT FUNCTION Body building foods: -meat, milk, poultry, fish, eggs, pulses etc Energy giving foods: -cereals, sugars, fats, oils etc. Protective foods: -vegetables, fruits, milk, etc 10
NUTRIENTS Organic and inorganic complexes contained in food are called nutrients. They are broadly divided in to: Macronutrients: -proteins -fats -carbohydrates Micronutrients: -vitamins -minerals 11
Protein, carbohydrate and fat had been recognized early in the 19 th century as energy-yielding foods and much attention was paid to their metabolism and contribution to energy requirements. 12
NUTRIENTS • Organic and inorganic complexes contained in food. • About 50 different nutrients are normally supplied through the foods we eat. • Each nutrient has specific functions in the body. • Most natural foods contain more than one nutrient. • may be divided into : MACRONUTRIENTS proteins, fats, and carbohydrates, MICRONUTRIENTS vitamins and minerals
PROTEINS Complex organic nitrogenous compounds composing of carbon, hydrogen, oxygen, nitrogen and sulphur in varying amounts. Some proteins also contain iron and phosphorous. Made up off smaller units called amino acids. • SOURCES • Animal sources– milk, meat, eggs, cheese, fish. • Vegetable sources– pulses, cereals, beans, nuts, oil seeds. • DAILYREQUIREMENT: 60 -65 gms/day for adults.
• FUNCTIONS: • Necessary for growth and repair of the body. • Build up new tissues during the period of growth or pregnancy & lactation. • Required for the formation of digestive enzymes, hormones, plasma proteins, hemoglobin and vitamins. • Provide 10 -15% of the energy during emergencies e. g. , starvation, inadequate food intake. • Act as buffers helping to maintain the PH of plasma at a constant level.
PROTEINDEFICIENCY&PERIODONTAL DISEASE • Degeneration of the connective tissue of the gingival and periodontal ligament. • Osteoporosis of alveolar bone. • Retardation in the deposition of cementum. • Delayed wound healing. • Atrophy of tongue epithelium. • Kwashiorkor • Marasmus

CARBOHYDATES • DAILY REQUIREMENT: 300 -500 gm/day
FUNCTIONS • Primary function is to provide a source of energy to facilitate body metabolism (1200 kcal). • Brain and nervous tissue utilize only glucose as energy source (5 grams per hour). • Muscles including the heart muscles derive energy for contraction from stored glycogen. • Protein sparing effect- adequate carbohydrate spare protein during metabolism which can be utilized for growth and repair of the body. • Major components of the ground substance are derived from carbohydrates.
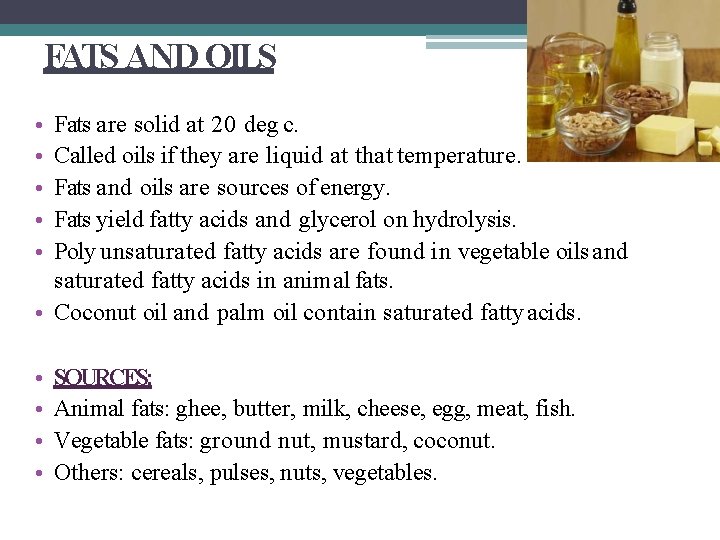
FATS AND OILS • • • Fats are solid at 20 deg c. Called oils if they are liquid at that temperature. Fats and oils are sources of energy. Fats yield fatty acids and glycerol on hydrolysis. Poly unsaturated fatty acids are found in vegetable oils and saturated fatty acids in animal fats. • Coconut oil and palm oil contain saturated fatty acids. • • SOURCES: Animal fats: ghee, butter, milk, cheese, egg, meat, fish. Vegetable fats: ground nut, mustard, coconut. Others: cereals, pulses, nuts, vegetables.
FUNCTIONS • • Provide energy - - 9 kcal every gram. Serve as vehicle for fat soluble vitamins. Act as thermal insulators for skin. Essential fatty acids are required for the body growth and structural integrity. • DAILY REQUIREMENTS: • 10 -20 gms/day
FAT AND ITSROLE IN DISEASE • OBESITY • PHRENODERMA- deficiency of essential fatty acids in diet is associated with rough and dry skin(toad skin ) • CORONARY HEART DISEASE • CANCER • ATHEROSCLEROSIS • CHRONIC SWELLING OF PAROTID GLANDS due to disturbances in lipid metabolism.
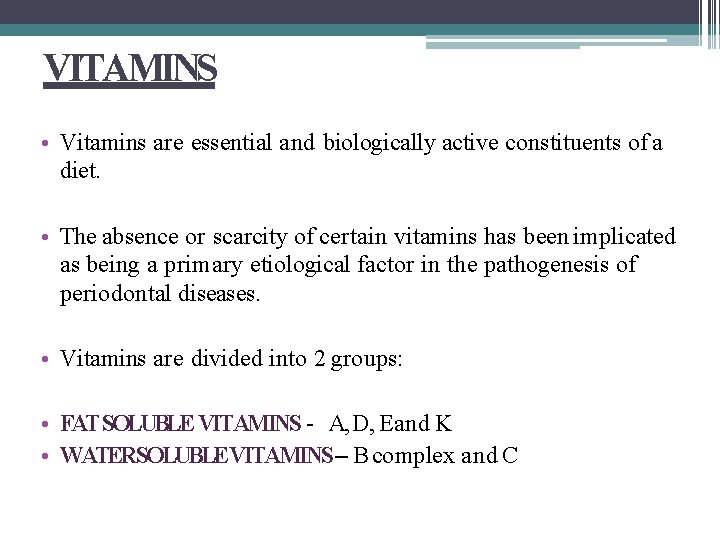
VITAMINS • Vitamins are essential and biologically active constituents of a diet. • The absence or scarcity of certain vitamins has been implicated as being a primary etiological factor in the pathogenesis of periodontal diseases. • Vitamins are divided into 2 groups: • FAT SOLUBLE VITAMINS - A, D, Eand K • WATERSOLUBLEVITAMINS – B complex and C
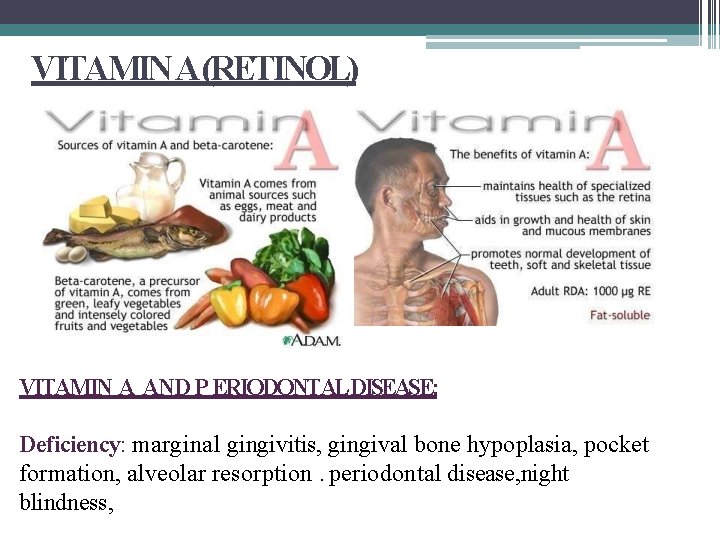
VITAMIN A(RETINOL) VITAMIN A AND P ERIODONTALDISEASE: Deficiency: marginal gingivitis, gingival bone hypoplasia, pocket formation, alveolar resorption. periodontal disease, night blindness,
VITAMIN D AND PERIODONTAL DISEASE • Asmall number of patients w ith evidence of rickets develop enamel hypoplasia. • The enamel does not appear t o be weakened, but the rougher surface may facilitate adhere n ce of dental plaque and food residue. • No studies demonstrate a rela tionship b/w vit D def and periodontal disease.
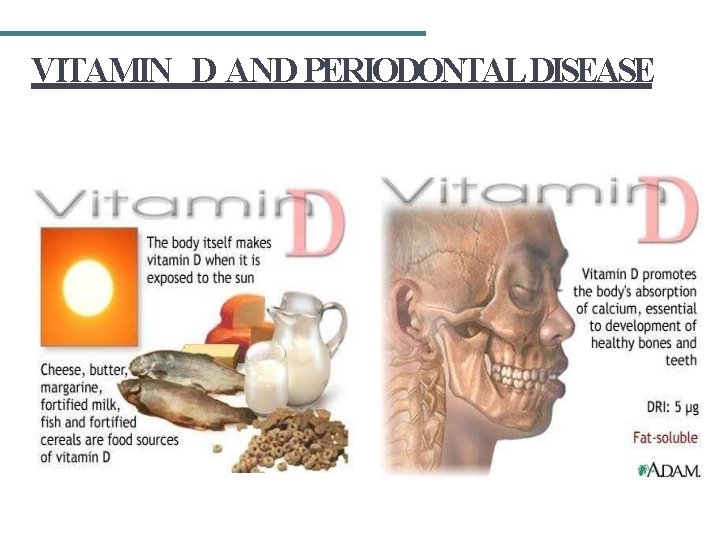
VITAMIN D AND PERIODONTAL DISEASE
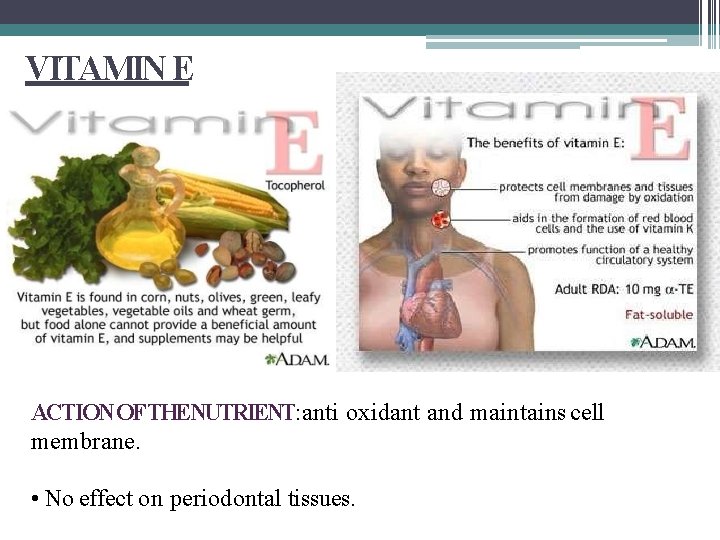
VITAMIN E ACTION OFTHENUTRIENT: anti oxidant and maintains cell membrane. • No effect on periodontal tissues.
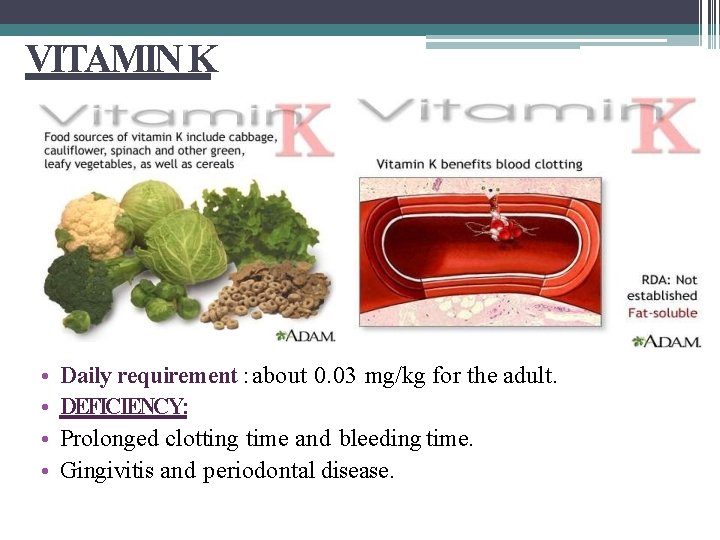
VITAMIN K • • Daily requirement : about 0. 03 mg/kg for the adult. DEFICIENCY: Prolonged clotting time and bleeding time. Gingivitis and periodontal disease.
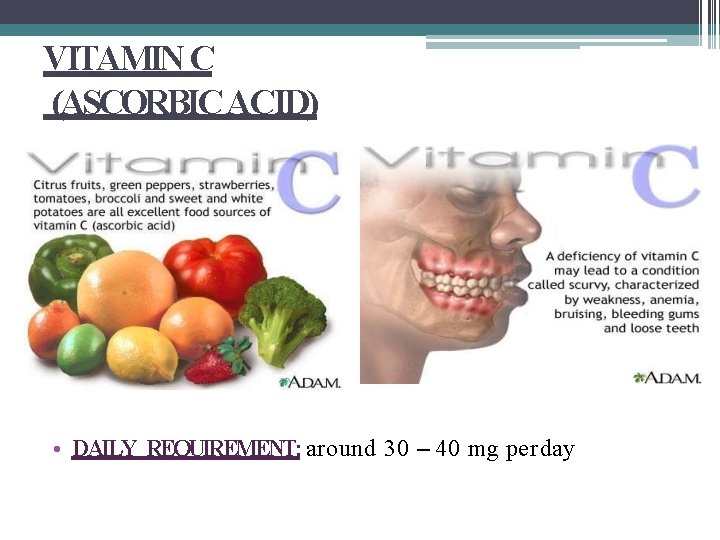
VITAMIN C (ASCORBIC ACID) • DAILY REQUIREMENT: around 30 – 40 mg per day
POSSIBLE ETIOLOGIC FACTORS: • Low levels of ascorbic acid influence the metabolism of collagen within the periodontium, affecting the ability of tissue to regenerate or repair itself. • Interferes with the bone formation, leading to loss of periodontal bone. • Deficiency can lead to defect in epithelial barrier. • Megadoses of vit C seem to impair the bactericidal activity of leukocytes. • An optimal level of ascorbic acid is required to maintain the integrity of periodontal microvasculature, as well as the vascular response to bac plaque and wound healing. • Depletion of vit C may interfere with the ecologic equilibrium of bac in plaque and thus inc its pathogenicity.
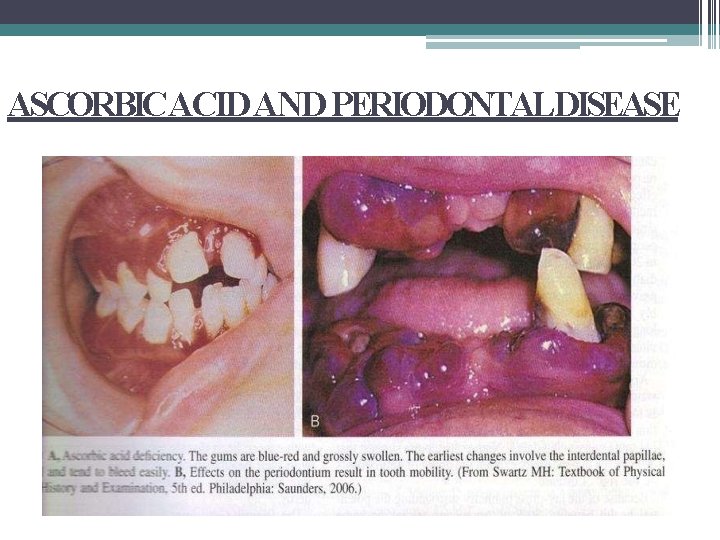
ASCORBICACID AND PERIODONTALDISEASE
VITAMIN B 1(Thiamine) • The earliest symptoms of thi amin deficiency include constipation, appetite suppre ssion, and nausea as mental depression, peripheral neuro pathy, and fatigue. • Chronic thiamin deficiency l symptoms and to cardiovascu (Winston et al. 2000). ead neurological s to more severe lar and musculature defects • Oral manifestations include: hypersensitivity of oral mucosa, under the tongue or on the palate, and erosion of the oral mucosa.
VITAMIN B 1
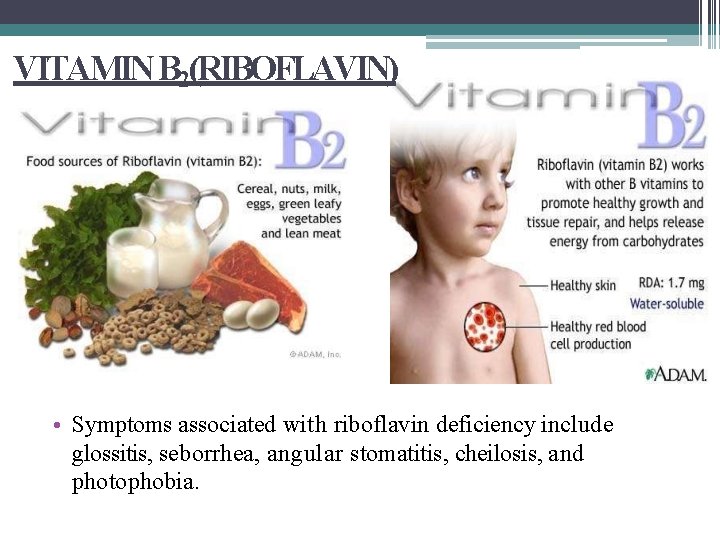
VITAMIN B 2(RIBOFLAVIN) • Symptoms associated with riboflavin deficiency include glossitis, seborrhea, angular stomatitis, cheilosis, and photophobia.
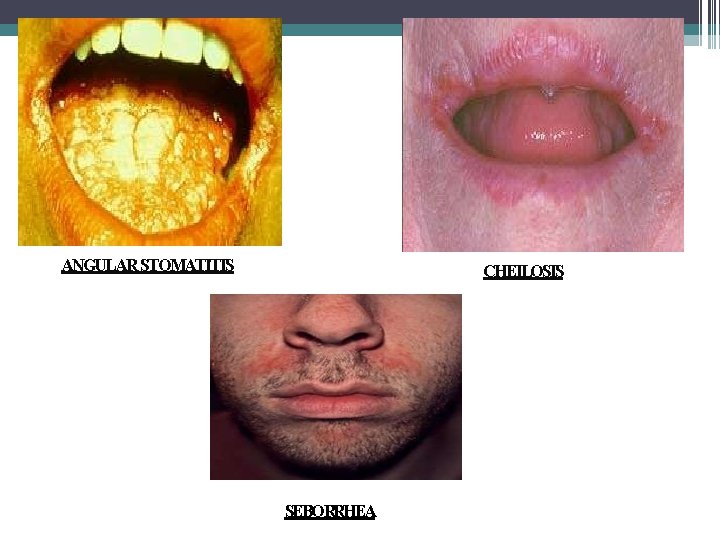
ANGULAR STOMATITIS CHEILOSIS SEBORRHEA
VITAMIN B 3 (NIACIN) • Adiet deficient in niacin le ads to glossitis, dermatitis, weight loss, diarrhea, depression and dementia. • The severe symptoms of d epression, dermatitis, and diarrhoea are associated with the con dition known as pellagra. • Several physiological cond itions (e. g. Hartnup disease and malignant carcinoid syndro me) as well as certain drug therapies (e. g. isoniazid) can l ead to niacin deficiency (Carpenter 1983).
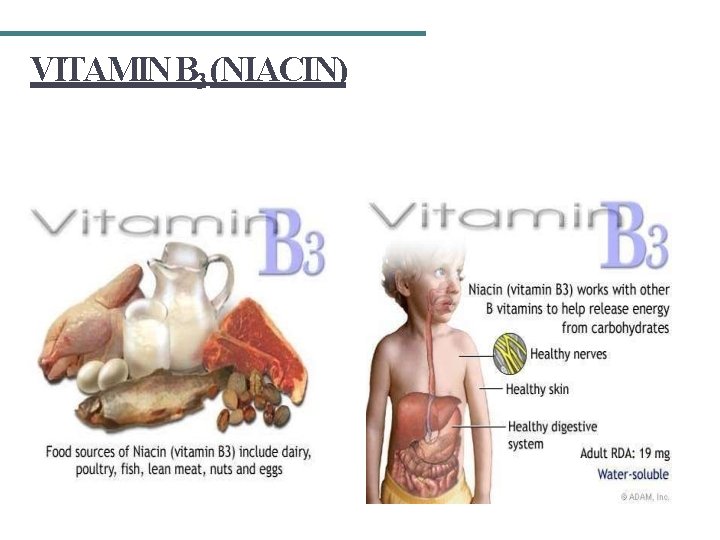
VITAMIN B 3 (NIACIN)
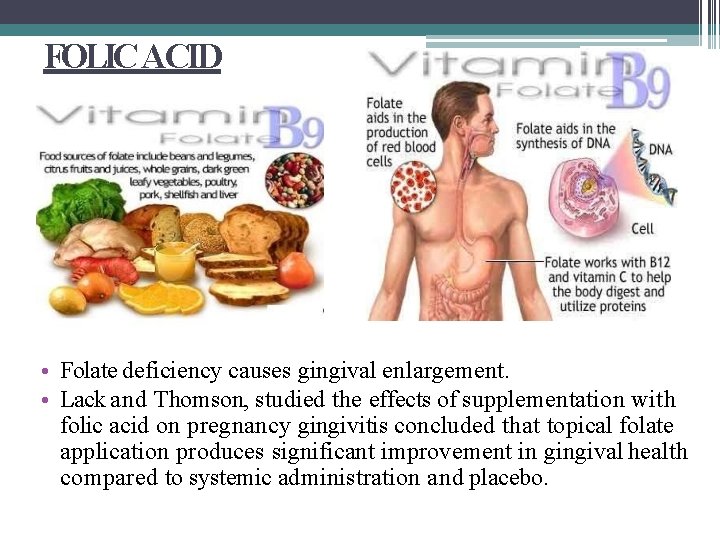
FOLIC ACID • Folate deficiency causes gingival enlargement. • Lack and Thomson, studied the effects of supplementation with folic acid on pregnancy gingivitis concluded that topical folate application produces significant improvement in gingival health compared to systemic administration and placebo.
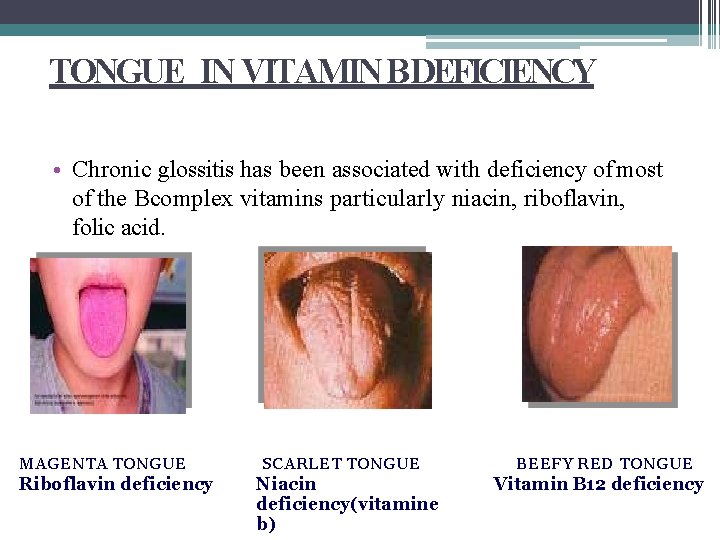
TONGUE IN VITAMIN B DEFICIENCY • Chronic glossitis has been associated with deficiency of most of the Bcomplex vitamins particularly niacin, riboflavin, folic acid. MAGENTA TONGUE Riboflavin deficiency SCARLET TONGUE Niacin deficiency(vitamine b) BEEFY RED TONGUE Vitamin B 12 deficiency
MINERALS • COPPER: • Apositive correlation has been demonstrated between serum copper and severity of periodontal disease by Freeland et al in 1976. • Copper is also essential for the development and maturation of connective tissues. (O’Dell et al 1961). • Acopper metalloenzyme contributes to the stabilization of collagen. (Burch et al 1975). • Freeland et al (1976) suggested that if this enzyme accumulates in blood or if copper is not transferred to the periodontal tissues, then an elevation of serum levels of copper will result.
• ZINC: • Zinc levels are found to decrease with an increase in alveolar bone resorption. (Frithiof et al 1980). • Zinc ions can stabilize the cell membranes of PMNs and inhibit the release of lysosomal enzymes. • The reduction in serum zinc in periodontal disease may stimulate both leucocyte function and the release of potent enzymes, which will enhance the inflammatory process and lead to loss of periodontal collagen. (Chapvil et al 1977). • Kilgore et al. (1969) failed to find a relationship between serum levels and periodontal status.
• CALCIUM AND PHOSPHATE: • Hypocalcaemia and hypophosphataemia that result from dietary imbalance of these ions will produce a nutritional, secondary hyperparathyroidism, which initiates alveolar bone resorption. • Ahypocalcaemic diet can produce inter – radicular alveolar osteoporosis and thinning of individual trabeculae but it will not initiate inflammation, migration of the epithelial attachment, loss of periodontal fibers or resorption of the alveolar margin – Svanberg et al 1973.
LOCALEFFECTOFDIETON PERIODONTAL HEALTH • Vigorous masticatory function is associated with a widening of the PDL. (Collidge 1937) • Aukes et al (1987) suggest that chewing pattern depends on the texture of the masticated food, hard and tough food requiring more vertical movements and soft food requiring less vertical movement.
Undernutrition The manifestation of inadequate nutrition Common in sub-Saharan Africa 1/3 of all children < 5 years old underweight 38% of children with low height for age Many causes Inadequate access to food/nutrients Improper care of mothers and children Limited health services Unhealthy environment 43
Conditions Associated with Under- and Overnutrition Vitamin deficiency disorders Scurvy (deficiency of vitamin C) Rickets (deficiency of vitamin D) Mental, adrenal disorders (deficiency of B vitamins) Mineral deficiency Osteoporosis (deficiency of calcium) Diet-related non-communicable diseases Diabetes Coronary heart disease Obesity High blood pressure 44
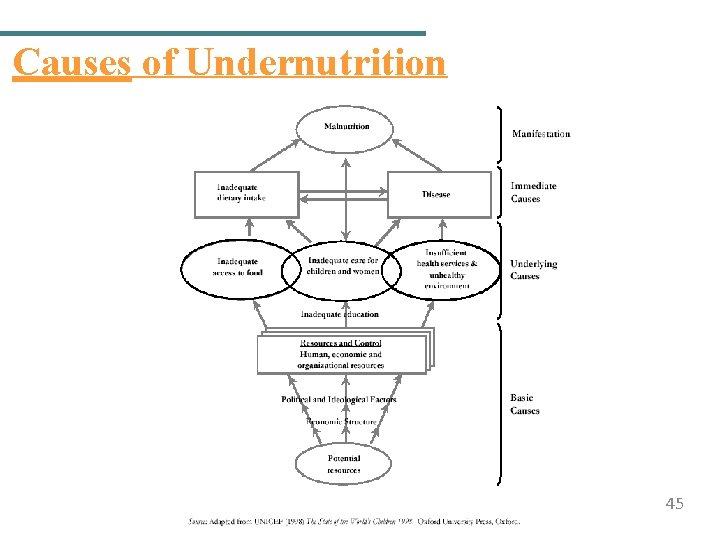
Causes of Undernutrition 45
Nutritional Status Determined by Anthropometry Underweight: Low weight for age compared to reference standard, a composite measure of stunting and wasting Stunting: Low height for age compared to reference standard, an indicator of chronic or past growth failure Wasting: Low weight for height, an indicator of short -term nutritional stress 46
Other Anthropometric Measurements MUAC (mid-upper arm circumference) BMI (body mass index): Compares height and weight BMI = Weight (kg) ÷ height (m)2 47
Manifestations of Protein-Energy Malnutrition (PEM) Marasmus: Severe growth failure Weight < 60% weight for age Frailty, thinness, wrinkled skin, drawn-in face, possible extreme hunger Kwashiorkor: Severe PEM Weight 60− 80% weight for age Swelling (edema), dry flaky skin, changes in skin and hair, appetite loss, lethargy Marasmic kwashiorkor: Most serious form of PEM, combining both conditions above −Weight < 60% weight for age 48
Strategies to Prevent and Control Undernutrition Improve household food security. Improve diversity of diet. Improve maternal nutrition and health care. Improve child feeding practices. Ensure child health care (immunization, medical care, growth monitoring). Provide nutrition rehabilitation. 49
Nutritional Anemia Most common type of anemia Caused by malaria, hookworm, and inadequate iron and vitamin intake resulting in low hemoglobin levels Affects mainly children < 5 years old and pregnant women Detected by measuring blood hemoglobin levels 50
Effects of Anemia Adults Reduced work capacity Reduced mental capacity Reduced immune competence Poor pregnancy outcomes Increased risk of maternal death Infants and children Reduced cognitive development Reduced immune competence Reduced work capacity 51
Strategies to Prevent and Control Anemia Promote iron, folic acid, and B 12 -rich foods. Treat and prevent anemia-related diseases (malaria and worms). Provide iron and folic acid supplements to infants and pregnant and lactating women. Fortify foods. Promote vitamin C-rich foods with meals. Discourage drinking coffee or tea with meals. 52
Iodine Deficiency Disorders (IDD) Caused by inadequate intake of iodine Only 1 tsp. needed over entire lifetime Iodine in food sources varies by geography. Less in highlands and mountain regions Leached from soil and carried to lowlands 53
Manifestations of IDD Goiter: Enlarged neck region from overactive thyroid gland Hypothyroidism: Dry skin, weight gain, puffy face, lethargy from underactive thyroid Hyperthyroidism: Rapid pulse and weight loss from overactive thyroid Cretinism: Mental retardation, physical development problems, spasticity from IDD in mother during pregnancy 54
Strategies to Control IDD Iodize salt, dairy products, and bread where iodine is deficient in local foods. Provide iodine drops. Inject people with iodized oil (expensive). 55
Causes of Vitamin A Deficiency (VAD) Low consumption of vitamin A-rich foods. Dietary deficiency due to food processing Limited consumption of fats and oils Poor breastfeeding (no colostrum, insufficient breastfeeding) Diseases affecting absorption (e. g. , worms, chronic diarrhea) 56
Manifestations of VAD Xerophthalmia (eye conditions) Blindness (VAD is the leading cause of blindness in children < 5 years old) Bitot’s spots Damage to the cornea Slowed growth and development Reduced reproductive health Increased risk of anemia 57
Strategies to Control VAD Promote vitamin A-rich foods (fruits, vegetables, red palm oil). Give infants and women low-dose iron supplements according to WHO protocols. Improve food security. Feed children properly. Prevent disease and treat disease early. Fortify foods. 58
INTERACTION OF IMMUNITY, INFECTION AND NUTRITIONAL STATUS • Nutrients interact with immune cells in the blood streams, lymph nodes and specialized immune system of the gastrointestinal tract. • Majority of nutrient deficiencies will impair the immune response and predispose the individual to infection. • Individuals who are undernourished have impaired immune response including abnormality in adaptive immunity , phagocytosis and antibody function. • Epidemiological and clinical data also suggests that nutritional deficiencies alter immune responses and increase the risk of infection. (R. K. Chandra. Am J clin Nutrition 1997)

NUTRITION AND PERIODONTAL HEALTH INTERRELATIONSHIP • Periodontal destruction is a consequence of infection and a nutritional deficiency alone is no longer believed to initiate periodontal disease, it is more likely, that a state of malnutrition will predispose a subject to onset of a periodontal infection, or will modify the rate of progression of established disease. (Glickman 1964, Ferguson 1969)
Food and nutrition affect periodontal health at 3 levels: Contributing to microbial growth in gingival crevice Affecting the immunological response to bacterial antigen Assisting in the repair of connective tissue at the local site after injury from plaque calculus and so forth
NUTRITION AND EPITHELIALBARRIER • Rapid rate of turn over of epithelial cells of gingival sulcus indicates the need of continuous synthesis of DNA, RNA and tissue protein. • This indicates that sulcular epithelium has high requirement of such nutrients as folic acid and protein which are involved in cell formation. • At the base of the sulcular epithelium is a narrow basement membrane made up of collagen. • Since collagen is the major component of basement membrane and ascorbic acid and zinc are important for collagen synthesis. • This membrane act as a barrier for entrance of toxic material.
THEEFFECTOFNUTRITION UPON ORAL MICROORGANISMS. • Although dietary intake is generally thought of in terms of sustaining the individual it also source of bacterial nutrients. Composition of the diet may influence the relative distribution of types of microorganism their metabolic activity, their pathogenic potential which in turn affects the occurrence and severity of oral disease. (Morhant &Fitzgerald 1976)
HOST NUTRITION AND PLAQUE BIOFILM Nutrition has both direct and indirect effects on development and composition of plaque biofilm The biofilm is made up primarily of microorganisms that include bacteria. Fungi, yeasts. and viruses In addition, 20 to 3 O% of the plaque mass is made up of intracellular matrix consisting of organic and inorganic components The organic components include polysaccharides, proteins, glycoproteins and lipids. Inorganic components are primarily calcium and phosphorus with trace amounts of sodium, potassium and fluoride
The early bacteria colonizing the dental pellicle are aerobic, gram-positive and primarily use sugars as an energy source The secondary colonizers of the more mature plaque biofilm are anaerobic, gram negative bacteria and use amino acids and small peptides as energy sources The primary mechanism by which nutrition impacts the biofilm is through a direct supply or specific nutrients (such as sucrose) as substrates for energy, nitrogen, or carbon for the bacteria. An example of this is the introduction of excess glucose to a plaque biofilm which has been shown to result in an increased rate of bacterial growth in the early stages of biofilm development
CONCLUSION Awell balanced diet is required for the normal growth and development of an individual. Any increase or decrease of the nutrients in the long run may lead to devastating situations. There are nutritional deficiencies that produce changes in the oral cavity. But, there are no nutritional deficiencies that by themselves will cause these changes. They can only affect the condition of the periodontium and thereby aggravate the injurious effects of local factors and excessive occlusal forces.
REFERENCES • Satyanarayana U. Essentials of Biochemistry. • MR Milward, ILC Chapple. THE ROLE OF DIET IN PERIODONTAL DISEASE. Volume 52 No 3 of 6 May 2013 • Vasudevan DM, Sreekumari S. Text Book of Biochemistry. 3 rd Ed. • Carranza’s. Clinical Periodontology. 10 th ed. • Robert E. Schifferle. Periodontal Disease And Nutrition Separating The Evidence From Current Fads. Periodontology 2000: vol. 50: 2009, 78 -89. • Boyd LD, Theresa ME. Nutrition, infection and periodontal disease. Dent Clin N Am 2003 ; 47: 337 -354.
- Slides: 67