Preparing Health Professionals for Models of Interdisciplinary Practice


- Slides: 35
Preparing Health Professionals for Models of Interdisciplinary Practice in an Aging Society Jo. Ann Damron-Rodriguez, Ph. D, LCSW School of Public Affairs Department of Social Welfare University of California, Los Angeles Taipei, Taiwan May 17, 2010
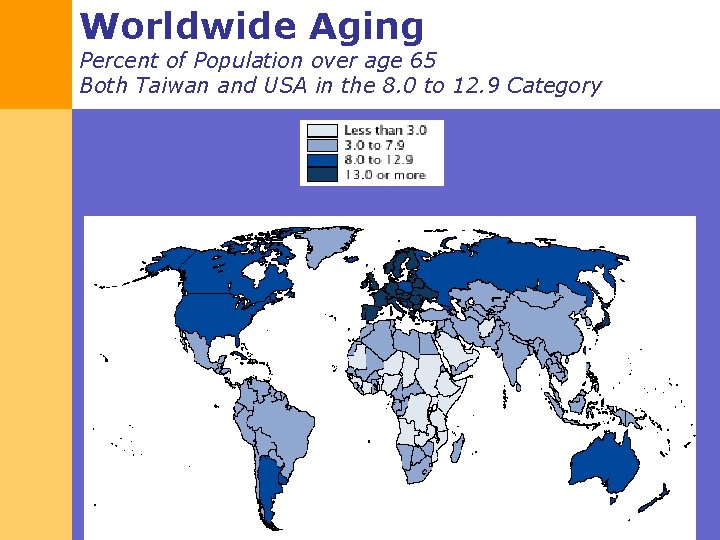
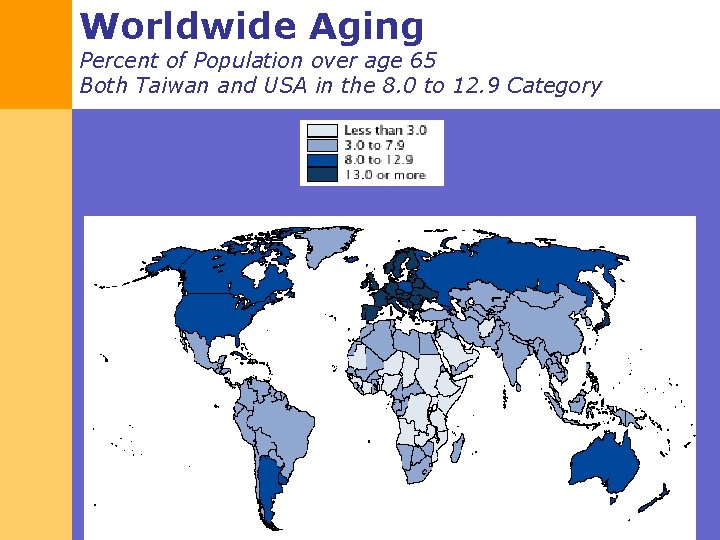
Worldwide Aging Percent of Population over age 65 Both Taiwan and USA in the 8. 0 to 12. 9 Category
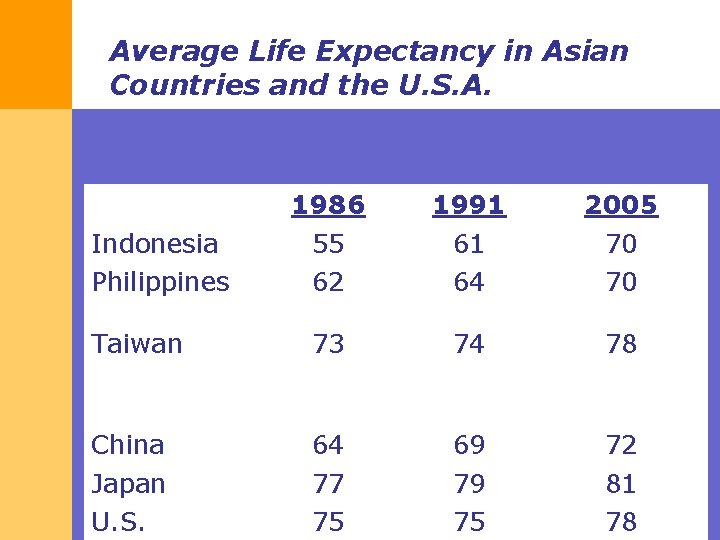
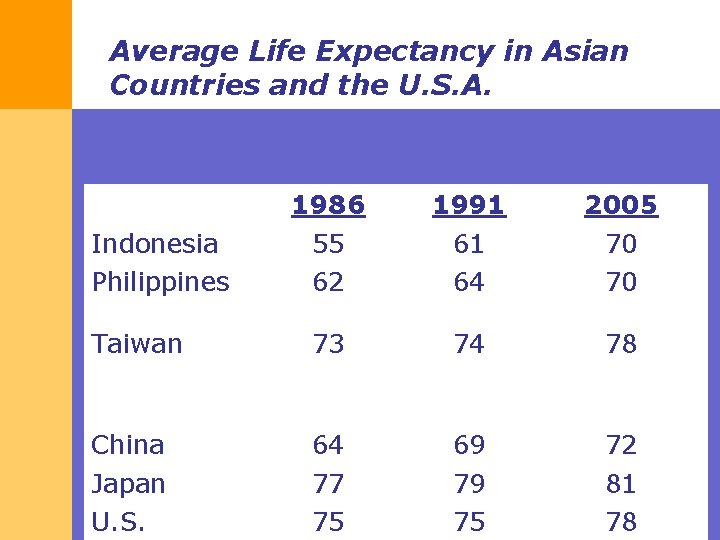
Average Life Expectancy in Asian Countries and the U. S. A. 1986 55 62 1991 61 64 2005 70 70 Taiwan 73 74 78 China Japan U. S. 64 77 75 69 79 75 72 81 78 Indonesia Philippines
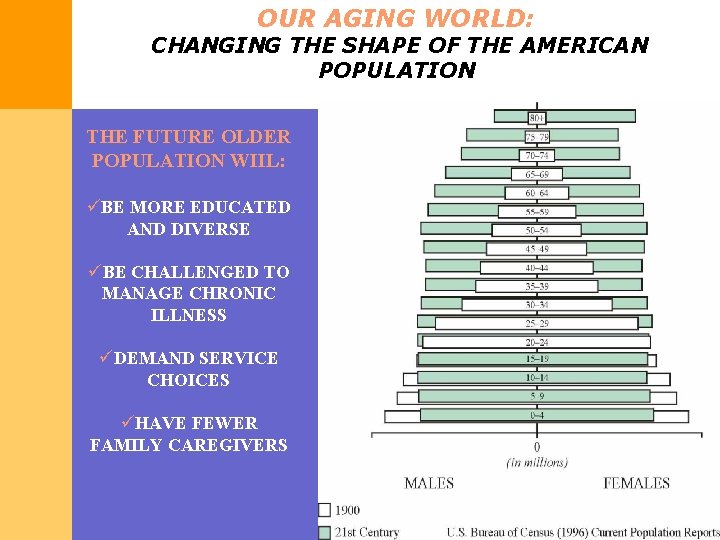
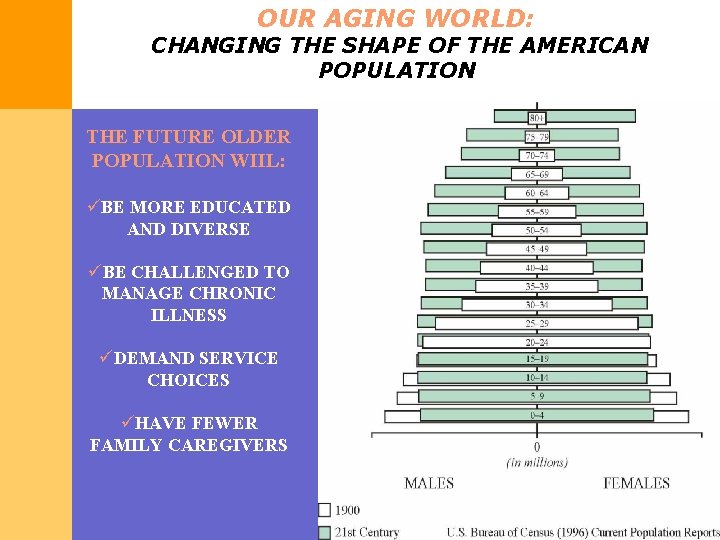
OUR AGING WORLD: CHANGING THE SHAPE OF THE AMERICAN POPULATION THE FUTURE OLDER POPULATION WIIL: üBE MORE EDUCATED AND DIVERSE üBE CHALLENGED TO MANAGE CHRONIC ILLNESS üDEMAND SERVICE CHOICES üHAVE FEWER FAMILY CAREGIVERS
OUTLINE I. Preparing Competent Health Professionals in the Field of Aging II. Interdisciplinary and Cross. Cultural Competence III. Evidence-based Models of Interdisciplinary Healthcare
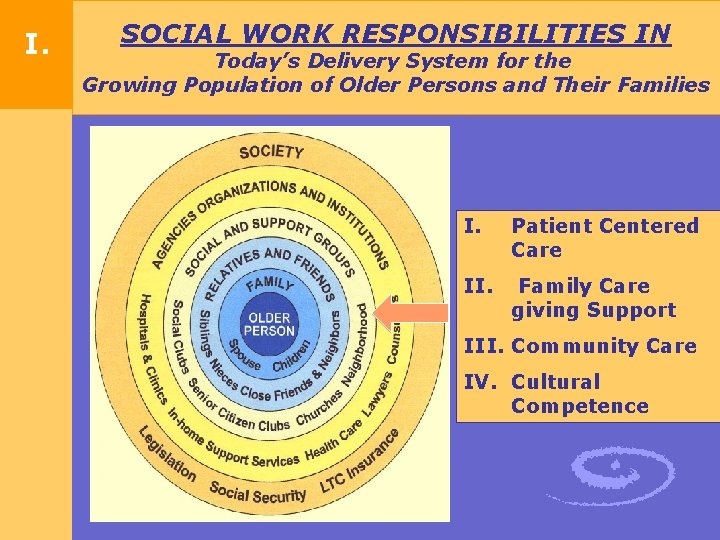
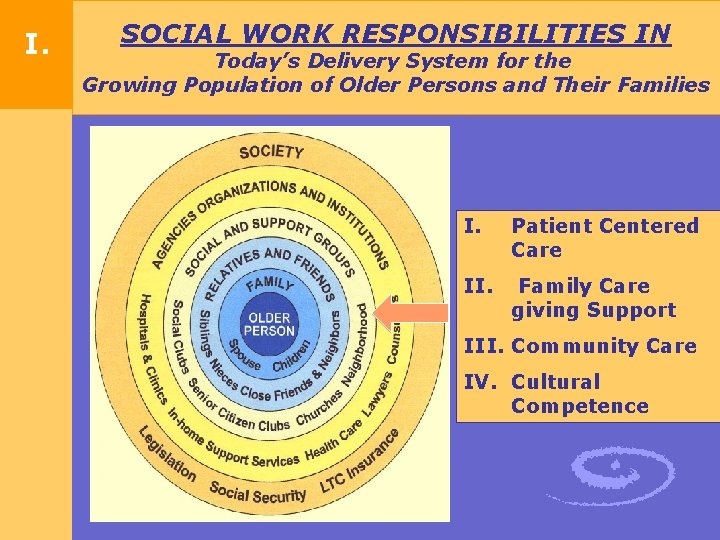
I. SOCIAL WORK RESPONSIBILITIES IN Today’s Delivery System for the Growing Population of Older Persons and Their Families I. Patient Centered Care II. Family Care giving Support III. Community Care IV. Cultural Competence
COMPETENCE IS THE STANDARD Council on Higher Education Accreditation (CHEA) CBE Now Required 76 Different Professions Define Competence § Competence: The state or quality of being adequately or well qualified… a specific range of skill, knowledge or ability § Professional Competence: The achievement and demonstration of core knowledge, values and skills in social work practice § Geriatric Competence: Establishing geriatric competencies shape curricular, field training, and continuing education programs that effectively prepare practitioners to address the need of older adults and their families
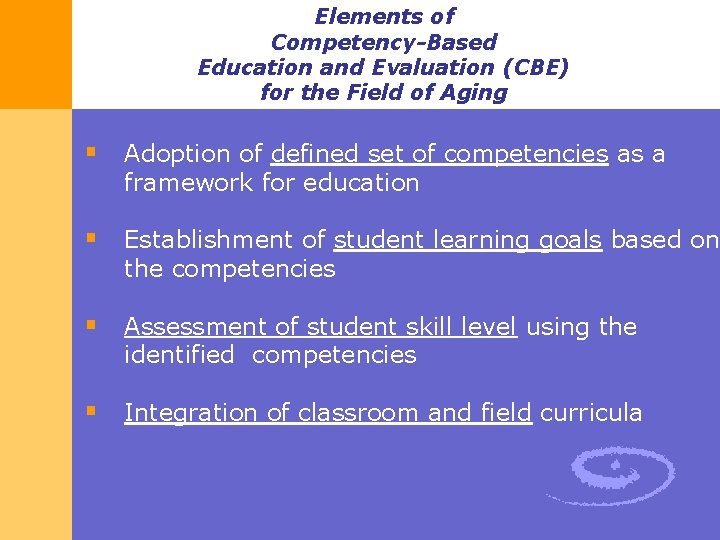
Elements of Competency-Based Education and Evaluation (CBE) for the Field of Aging § Adoption of defined set of competencies as a framework for education § Establishment of student learning goals based on the competencies § Assessment of student skill level using the identified competencies § Integration of classroom and field curricula
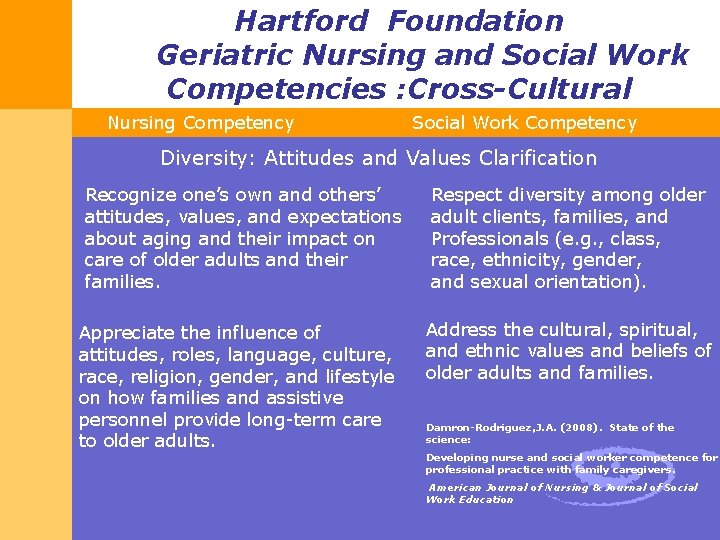
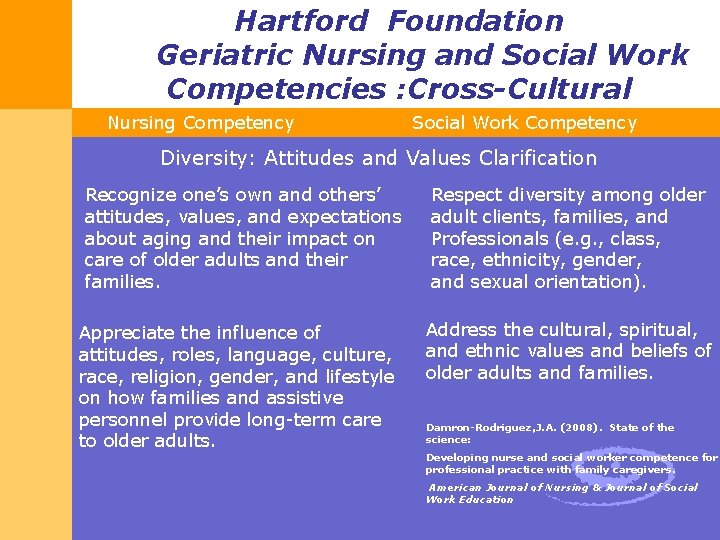
Hartford Foundation Geriatric Nursing and Social Work Competencies : Cross-Cultural Nursing Competency Social Work Competency Diversity: Attitudes and Values Clarification Recognize one’s own and others’ attitudes, values, and expectations about aging and their impact on care of older adults and their families. Appreciate the influence of attitudes, roles, language, culture, race, religion, gender, and lifestyle on how families and assistive personnel provide long-term care to older adults. Respect diversity among older adult clients, families, and Professionals (e. g. , class, race, ethnicity, gender, and sexual orientation). Address the cultural, spiritual, and ethnic values and beliefs of older adults and families. Damron-Rodriguez, J. A. (2008). State of the science: Developing nurse and social worker competence for professional practice with family caregivers. American Journal of Nursing & Journal of Social Work Education
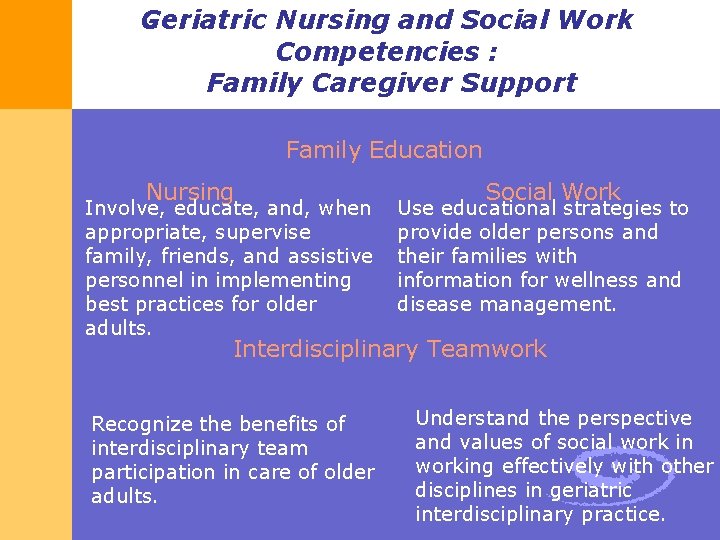
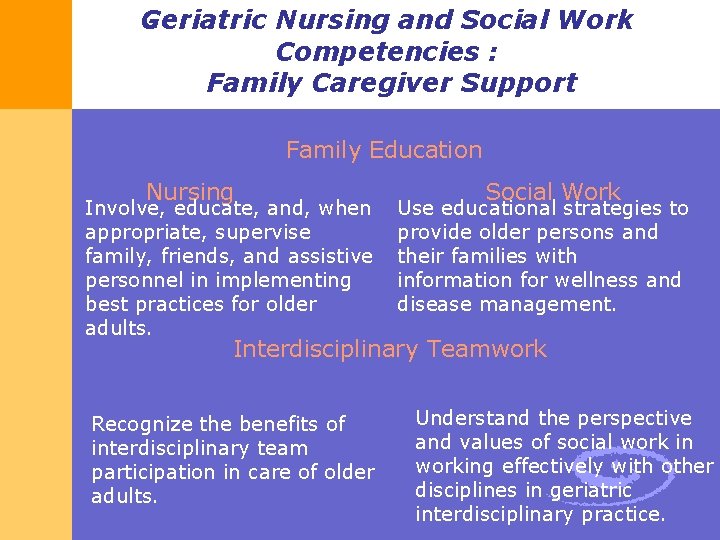
Geriatric Nursing and Social Work Competencies : Family Caregiver Support Family Education Nursing Involve, educate, and, when appropriate, supervise family, friends, and assistive personnel in implementing best practices for older adults. Social Work Use educational strategies to provide older persons and their families with information for wellness and disease management. Interdisciplinary Teamwork Recognize the benefits of interdisciplinary team participation in care of older adults. Understand the perspective and values of social work in working effectively with other disciplines in geriatric interdisciplinary practice.
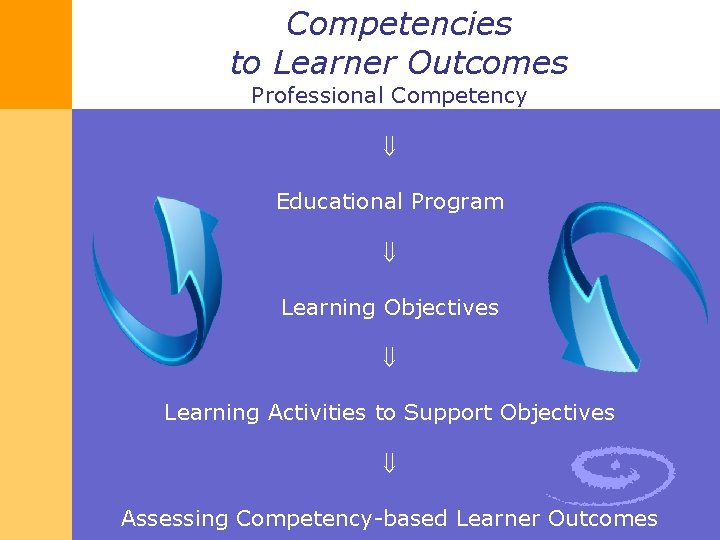
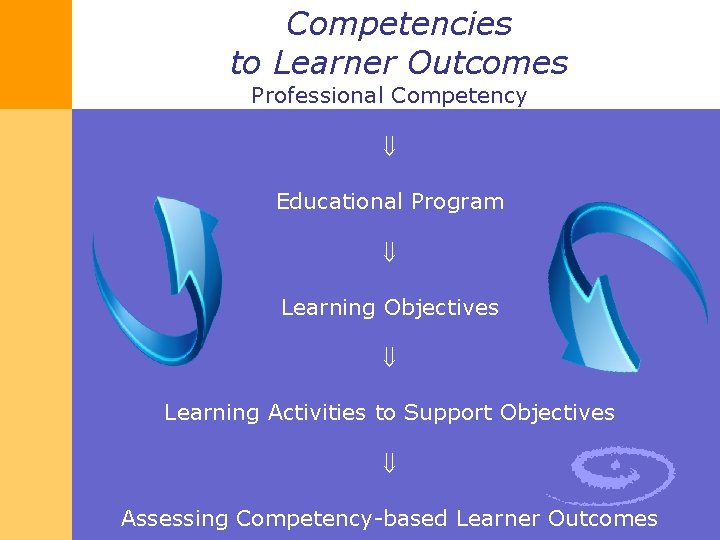
Competencies to Learner Outcomes Professional Competency Educational Program Learning Objectives Learning Activities to Support Objectives Assessing Competency-based Learner Outcomes
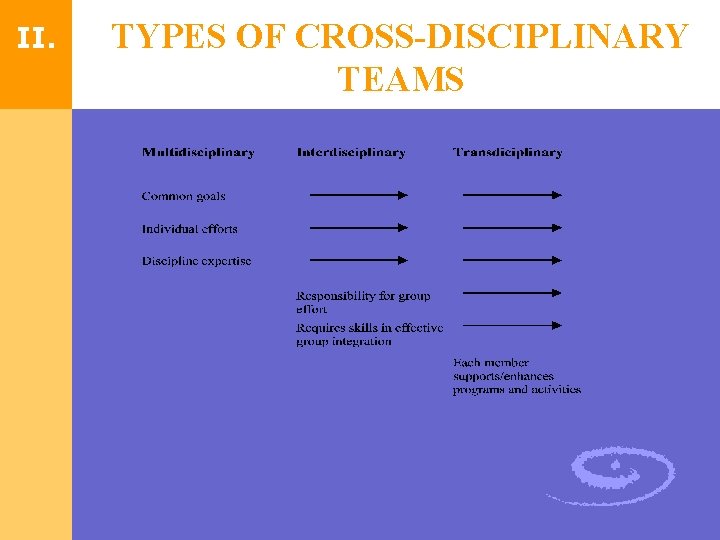
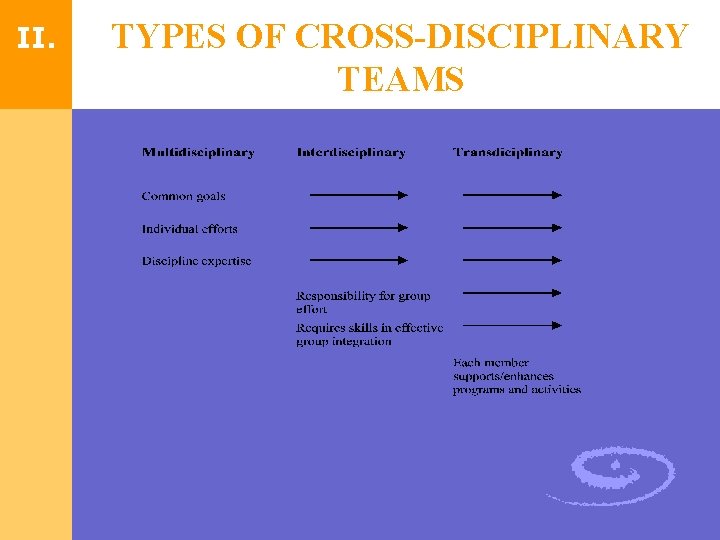
II. TYPES OF CROSS-DISCIPLINARY TEAMS
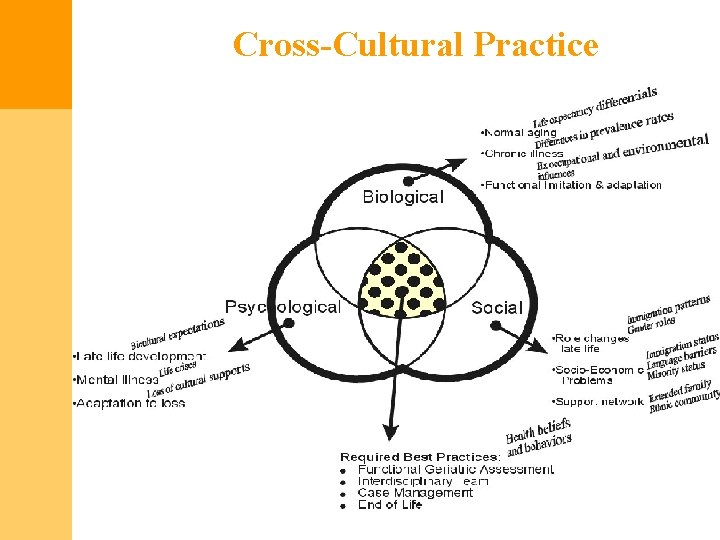
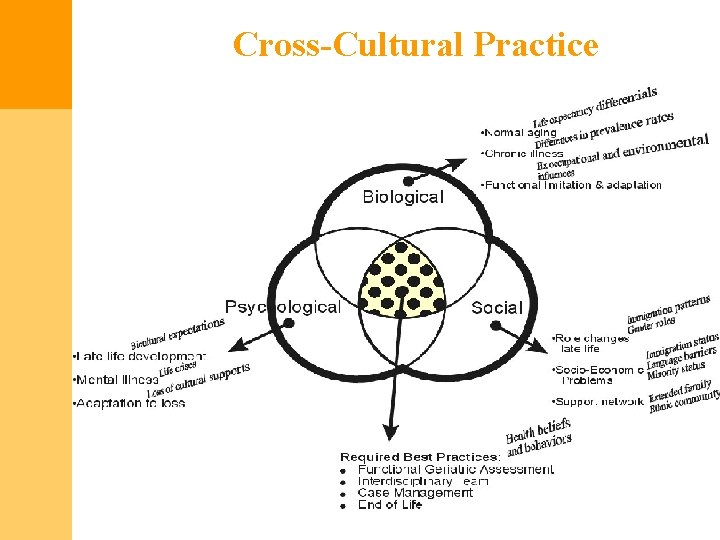
Cross-Cultural Practice
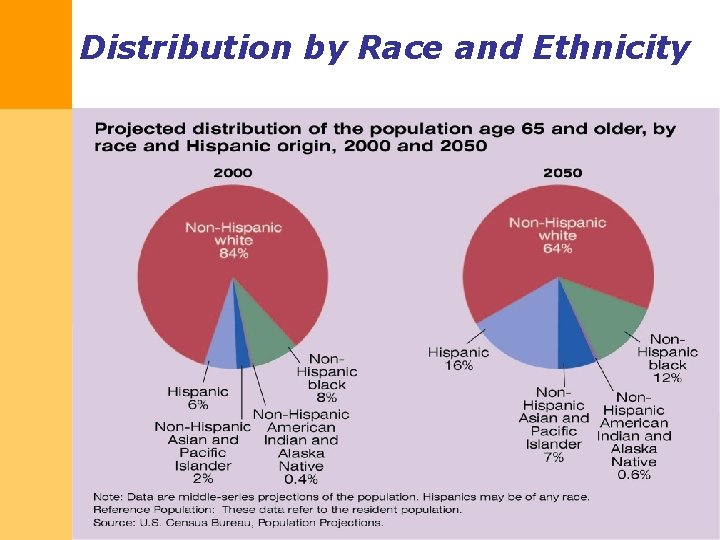
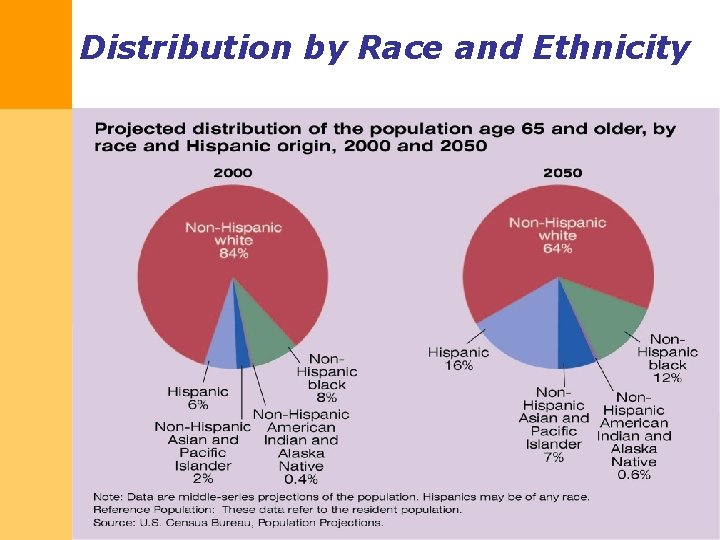
Distribution by Race and Ethnicity

Asian Americans refers to individuals who trace their heritage to the following countries: §Bangladesh §Bhutan §Cambodia §China §Hong Kong §India §Indonesia §Japan §Macau §Laos §Malaysia §Maldives §Mongolia §Myanmar §Nepal §North Korea §Pakistan §Philippines §Singapore §South Korea §Sri Lanka §Taiwan §Thailand §Vietnam
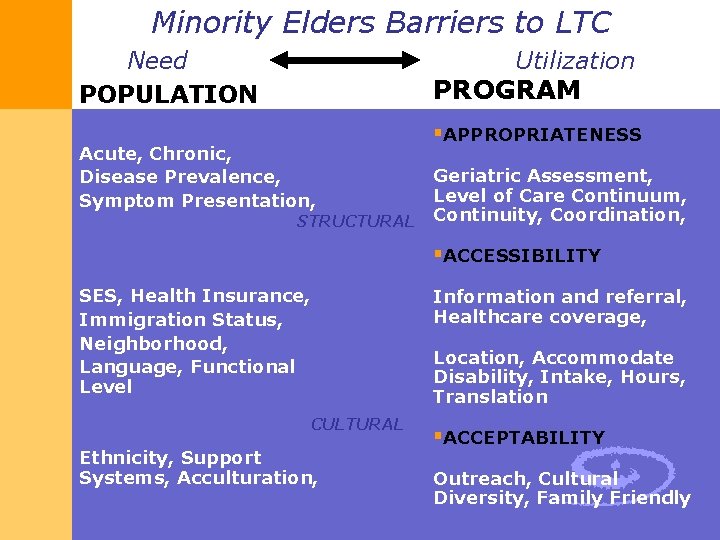
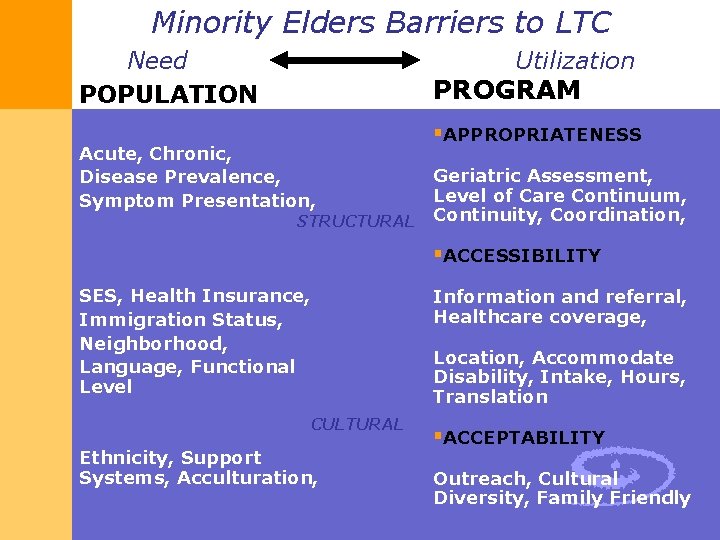
Minority Elders Barriers to LTC Need POPULATION Utilization PROGRAM Acute, Chronic, Disease Prevalence, Symptom Presentation, §APPROPRIATENESS Geriatric Assessment, Level of Care Continuum, STRUCTURAL Continuity, Coordination, §ACCESSIBILITY SES, Health Insurance, Immigration Status, Neighborhood, Language, Functional Level CULTURAL Ethnicity, Support Systems, Acculturation, Information and referral, Healthcare coverage, Location, Accommodate Disability, Intake, Hours, Translation §ACCEPTABILITY Outreach, Cultural Diversity, Family Friendly
IOM: Redesign models of care broaden III. provider & patient roles to achieve greater system responsiveness § Needs must be addressed comprehensively § Services must be provided efficiently § Older persons must be active participants in their own care § Increased dissemination of more effective and efficient models is needed § Expanded roles of health care providers
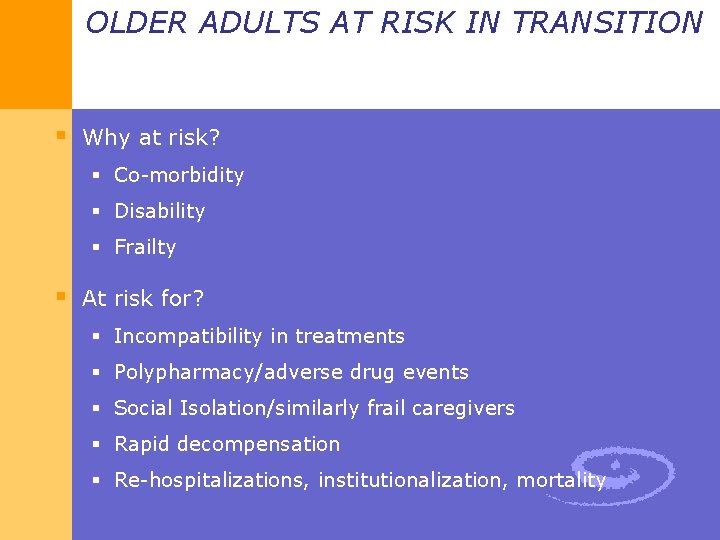
OLDER ADULTS AT RISK IN TRANSITION § Why at risk? § Co-morbidity § Disability § Frailty § At risk for? § Incompatibility in treatments § Polypharmacy/adverse drug events § Social Isolation/similarly frail caregivers § Rapid decompensation § Re-hospitalizations, institutionalization, mortality
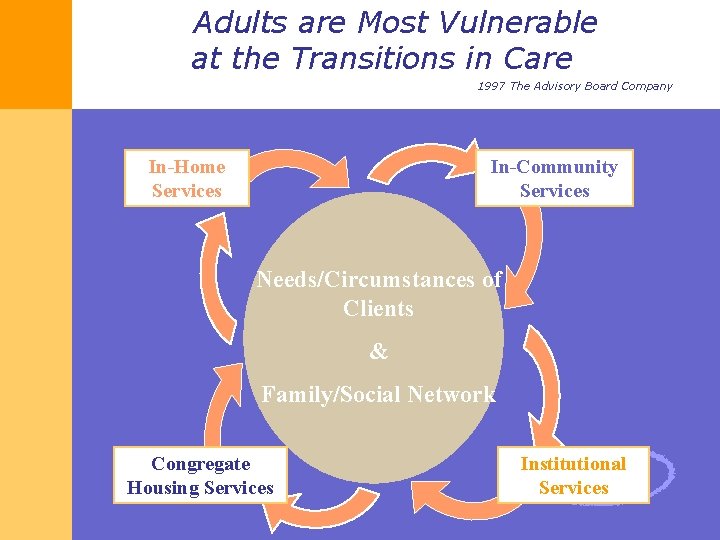
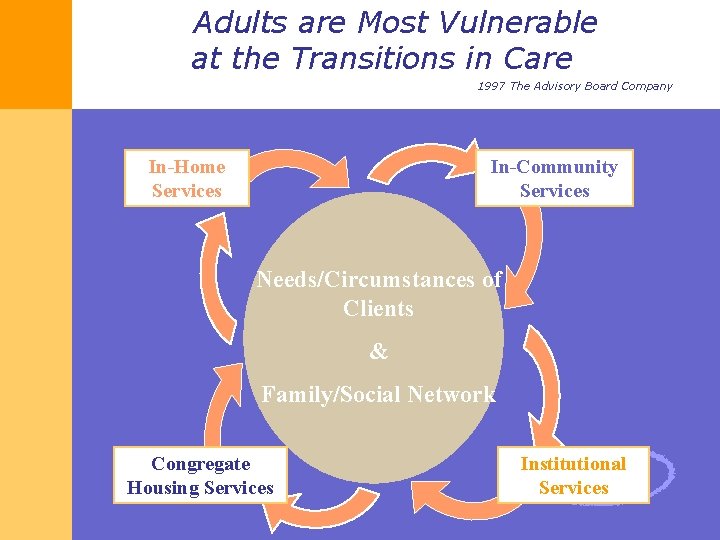
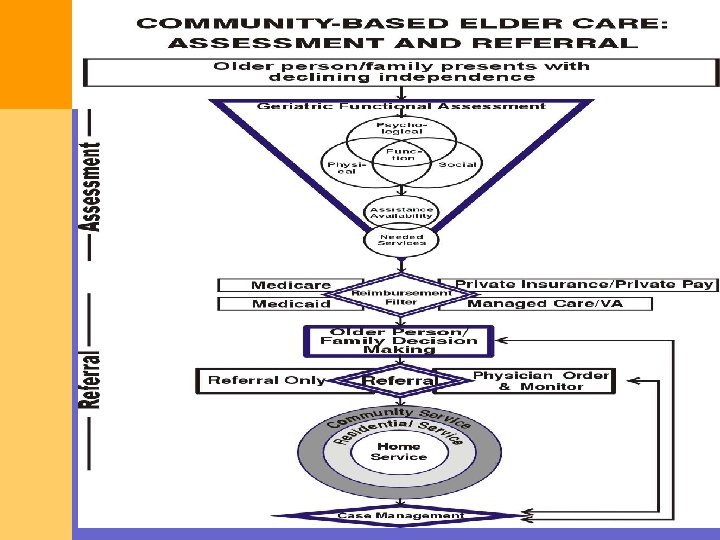
Adults are Most Vulnerable at the Transitions in Care 1997 The Advisory Board Company In-Home Services In-Community Services Needs/Circumstances of Clients & Family/Social Network Congregate Housing Services Institutional Services
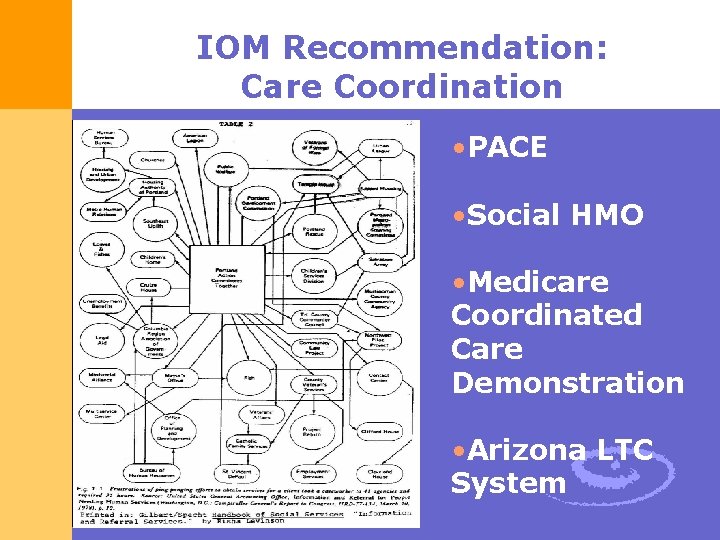
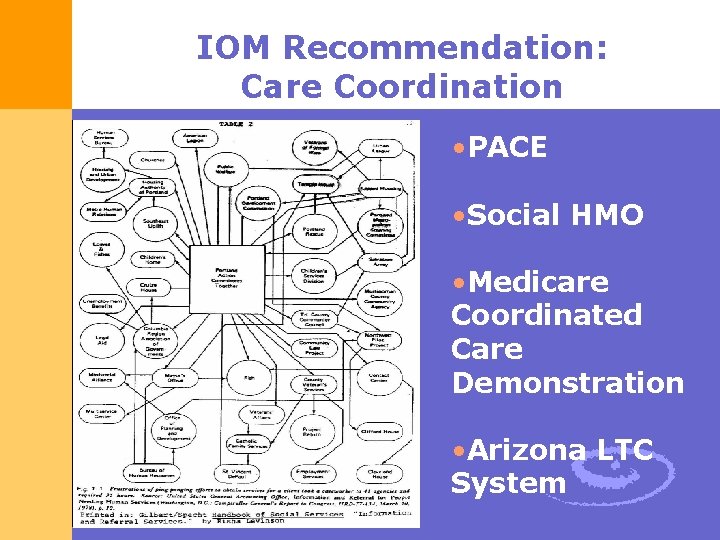
IOM Recommendation: Care Coordination • PACE • Social HMO • Medicare Coordinated Care Demonstration • Arizona LTC System
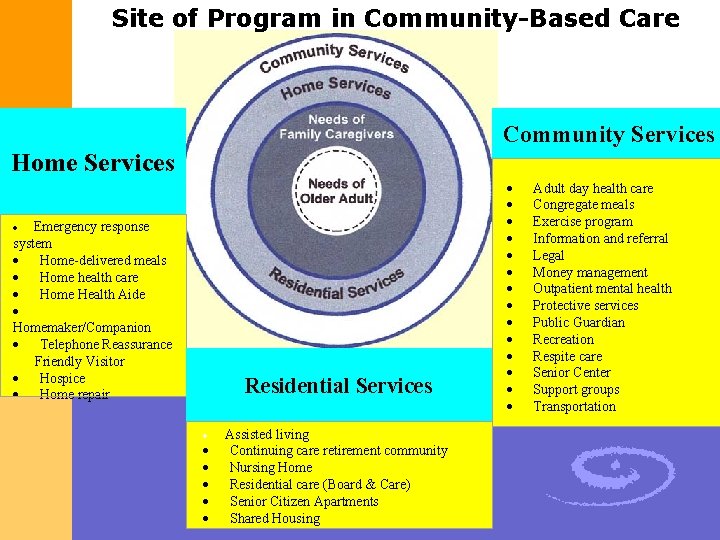
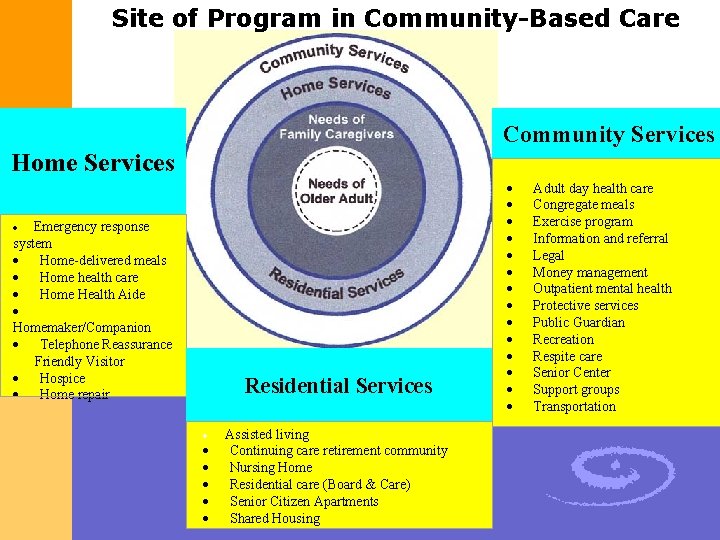
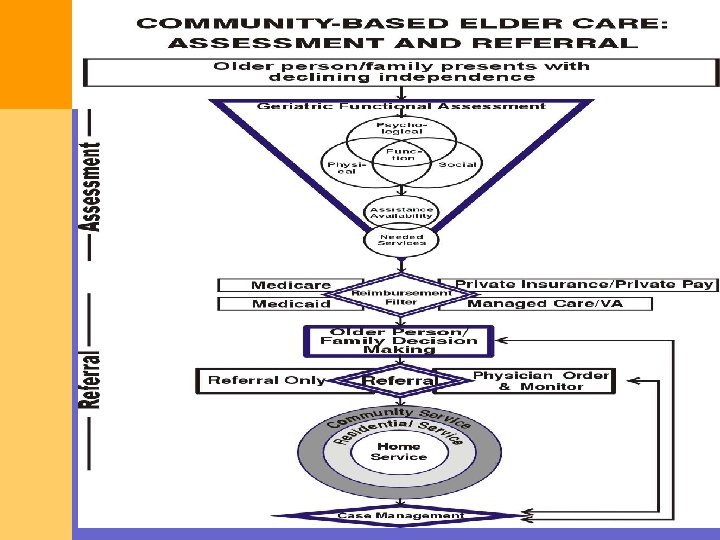
Site of Program in Community-Based Care Community Services Home Services Emergency response system · Home-delivered meals · Home health care · Home Health Aide · Homemaker/Companion · Telephone Reassurance Friendly Visitor · Hospice · Home repair · Residential Services · · · Assisted living Continuing care retirement community Nursing Home Residential care (Board & Care) Senior Citizen Apartments Shared Housing · · · · Adult day health care Congregate meals Exercise program Information and referral Legal Money management Outpatient mental health Protective services Public Guardian Recreation Respite care Senior Center Support groups Transportation
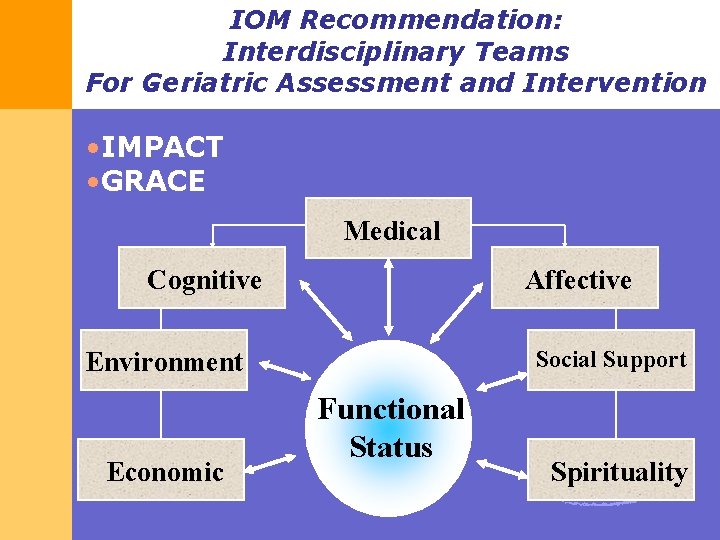
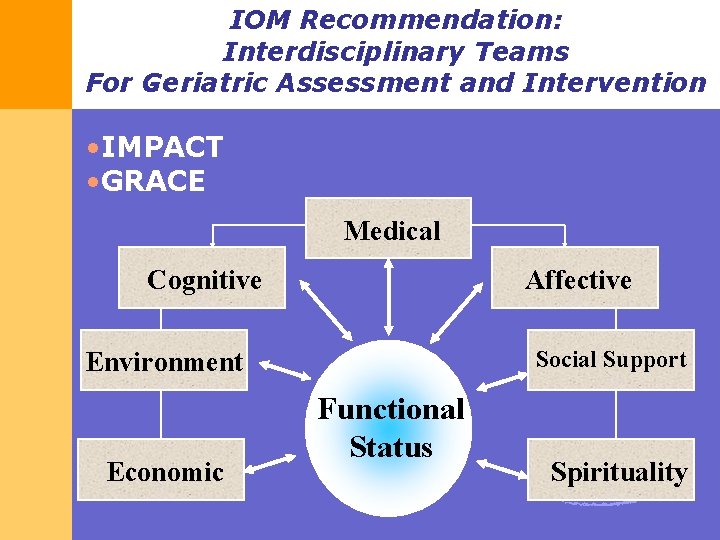
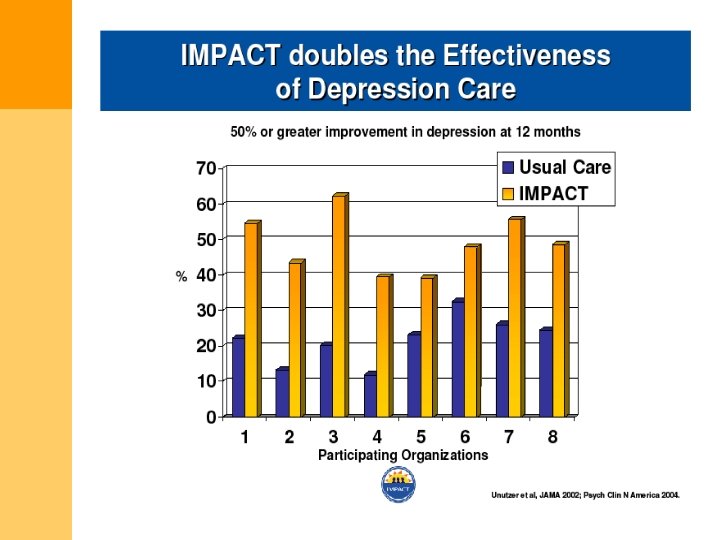
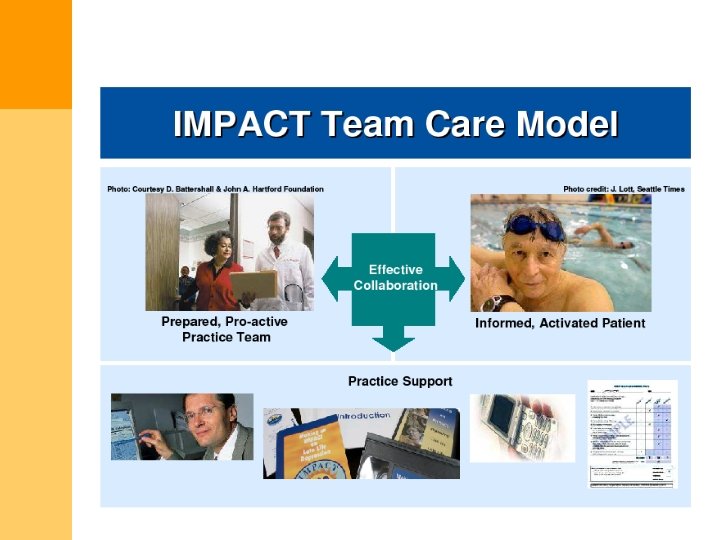
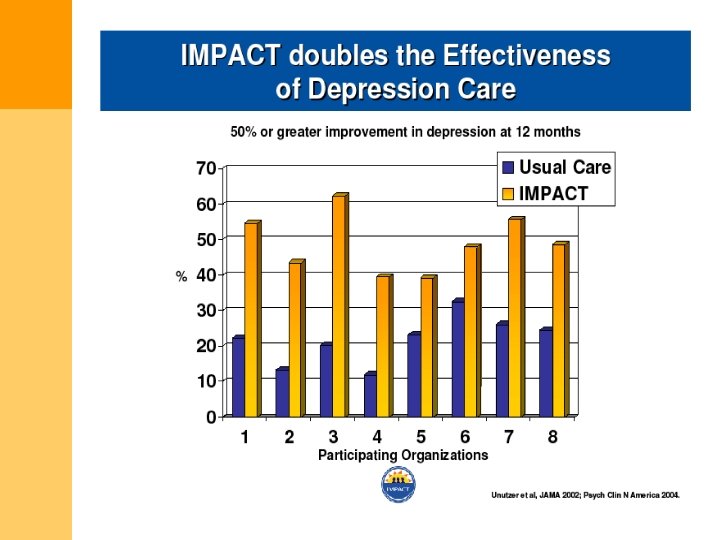
IOM Recommendation: Interdisciplinary Teams For Geriatric Assessment and Intervention • IMPACT • GRACE Medical Cognitive Affective Social Support Environment Economic Functional Status Spirituality
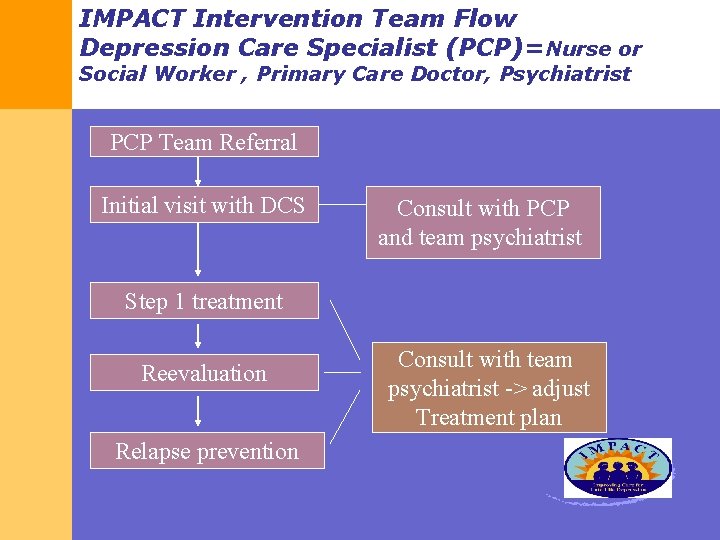
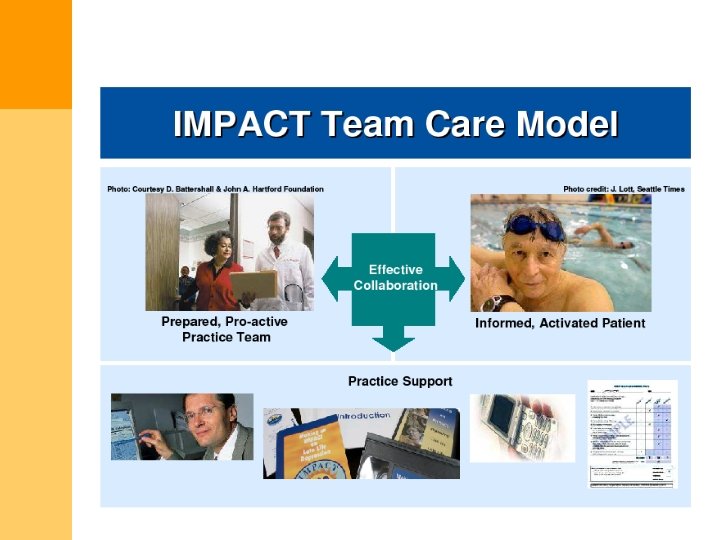
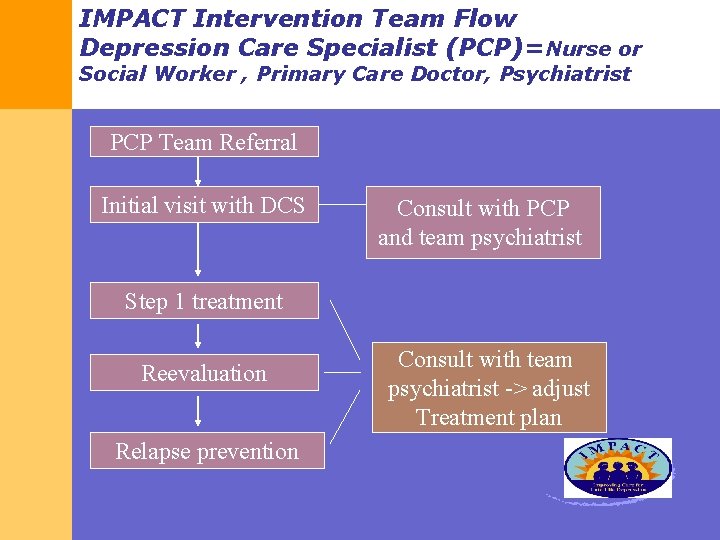
IMPACT Intervention Team Flow Depression Care Specialist (PCP)=Nurse or Social Worker , Primary Care Doctor, Psychiatrist PCP Team Referral Initial visit with DCS Consult with PCP and team psychiatrist Step 1 treatment Reevaluation Relapse prevention Consult with team psychiatrist -> adjust Treatment plan
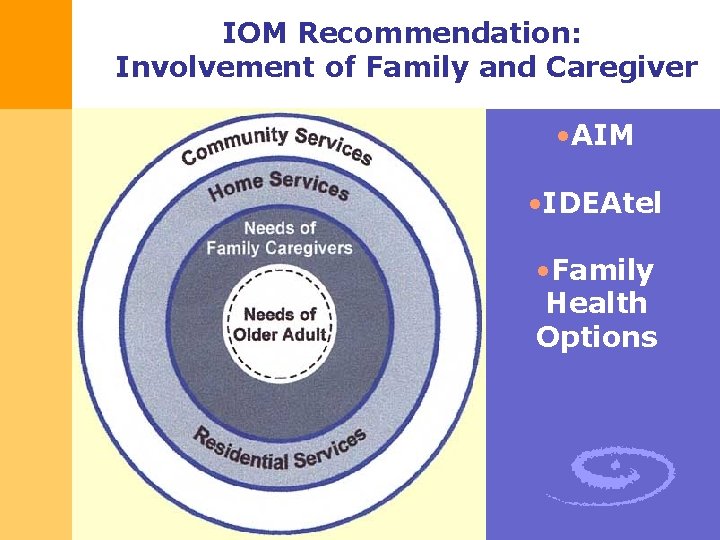
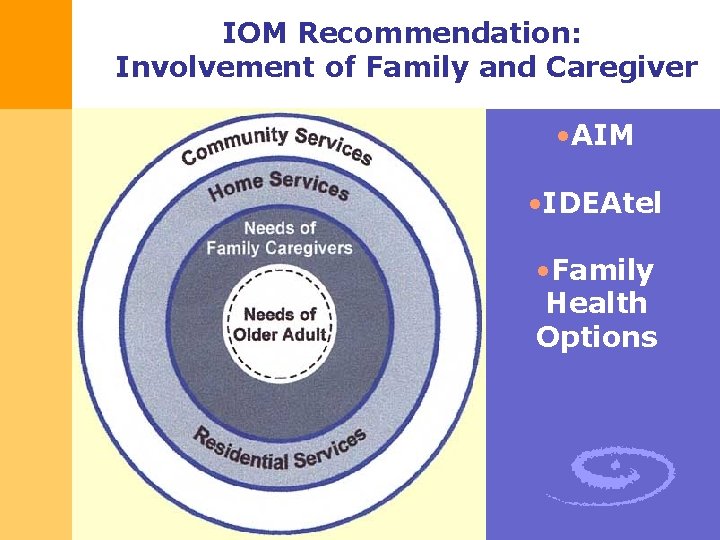
IOM Recommendation: Involvement of Family and Caregiver • AIM • IDEAtel • Family Health Options
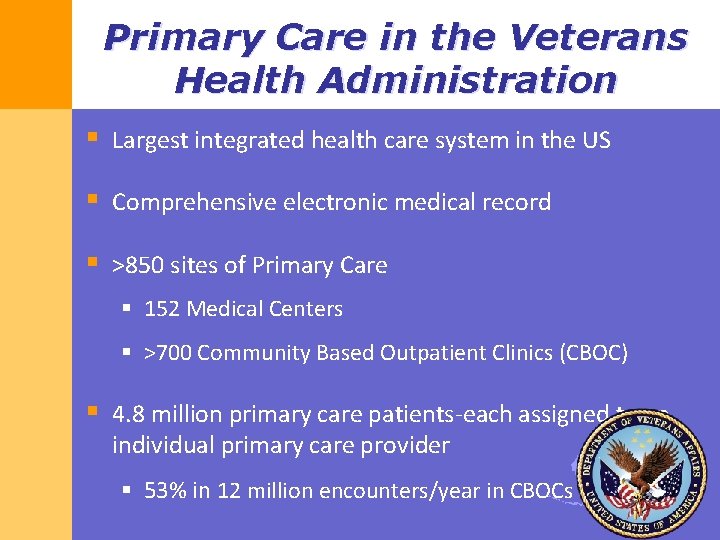
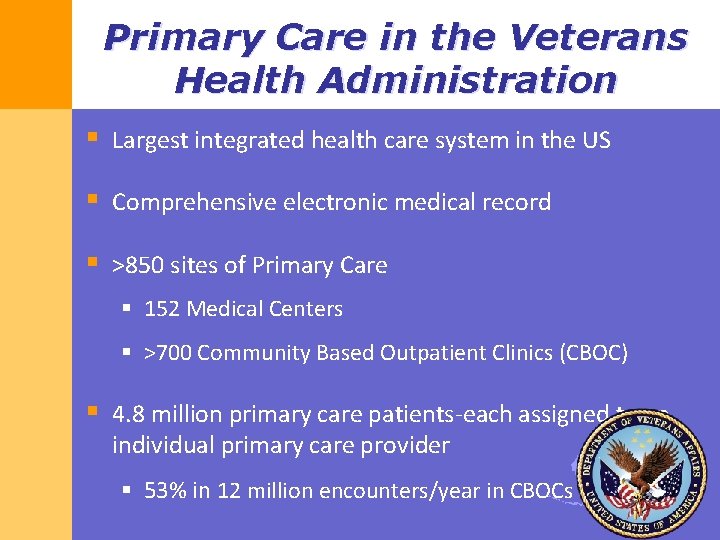
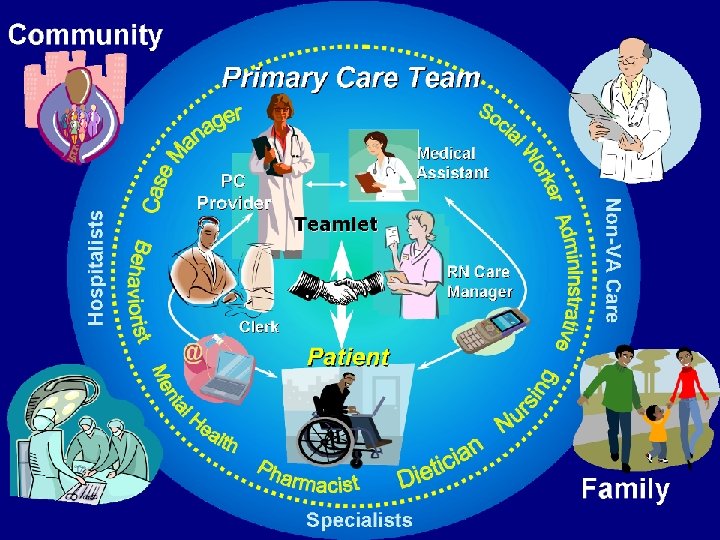
Primary Care in the Veterans Health Administration § Largest integrated health care system in the US § Comprehensive electronic medical record § >850 sites of Primary Care § 152 Medical Centers § >700 Community Based Outpatient Clinics (CBOC) § 4. 8 million primary care patients-each assigned to an individual primary care provider § 53% in 12 million encounters/year in CBOCs
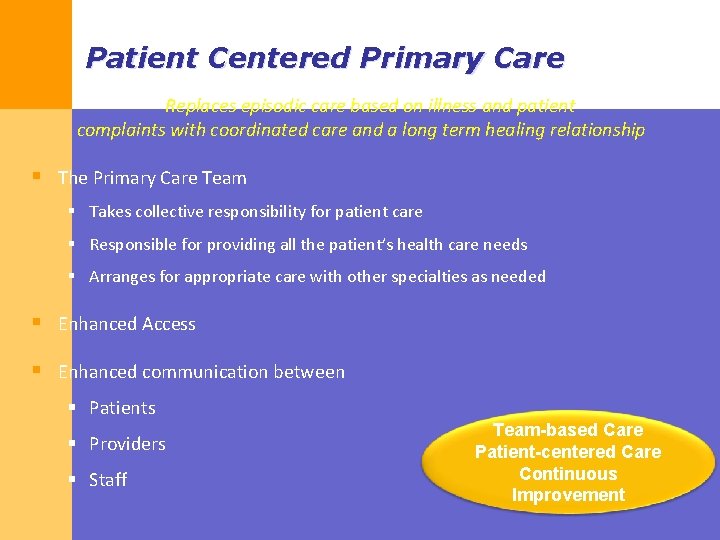
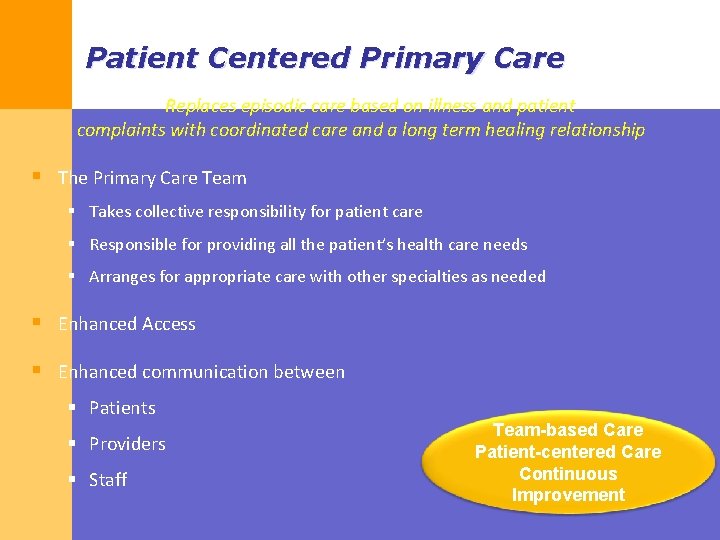
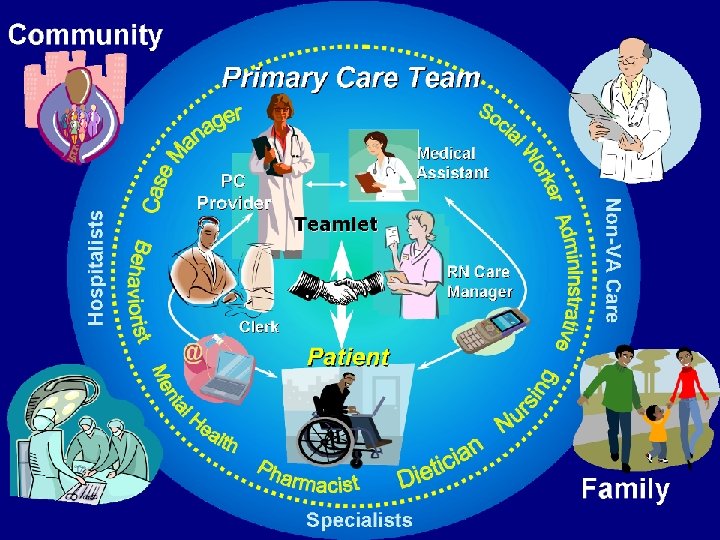
Patient Centered Primary Care Replaces episodic care based on illness and patient complaints with coordinated care and a long term healing relationship § The Primary Care Team § Takes collective responsibility for patient care § Responsible for providing all the patient’s health care needs § Arranges for appropriate care with other specialties as needed § Enhanced Access § Enhanced communication between § Patients § Providers § Staff Team-based Care Patient-centered Care Continuous Improvement
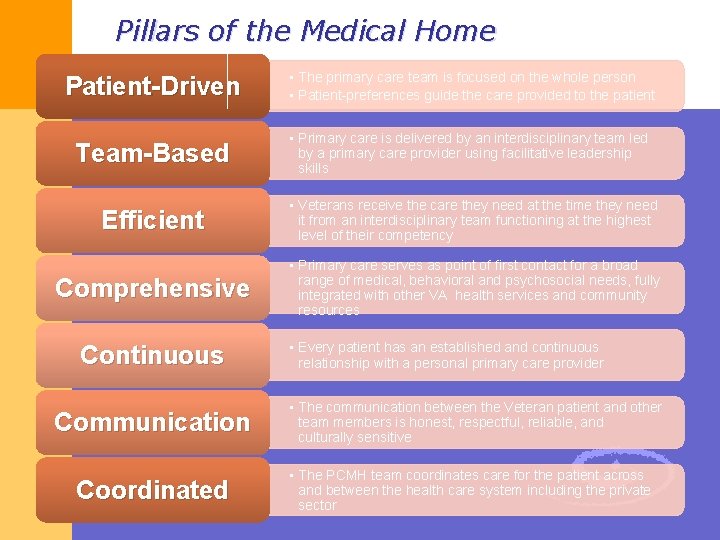
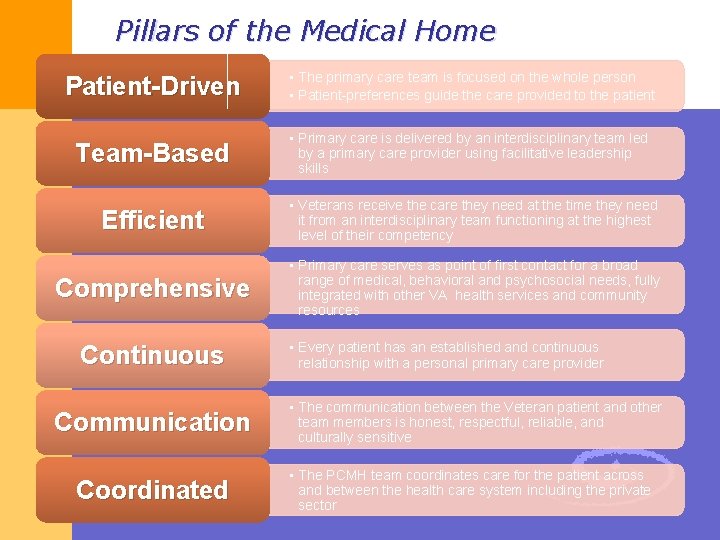
Pillars of the Medical Home Patient-Driven • The primary care team is focused on the whole person • Patient-preferences guide the care provided to the patient Team-Based • Primary care is delivered by an interdisciplinary team led by a primary care provider using facilitative leadership skills Efficient • Veterans receive the care they need at the time they need it from an interdisciplinary team functioning at the highest level of their competency Comprehensive • Primary care serves as point of first contact for a broad range of medical, behavioral and psychosocial needs, fully integrated with other VA health services and community resources Continuous Communication Coordinated • Every patient has an established and continuous relationship with a personal primary care provider • The communication between the Veteran patient and other team members is honest, respectful, reliable, and culturally sensitive • The PCMH team coordinates care for the patient across and between the health care system including the private sector
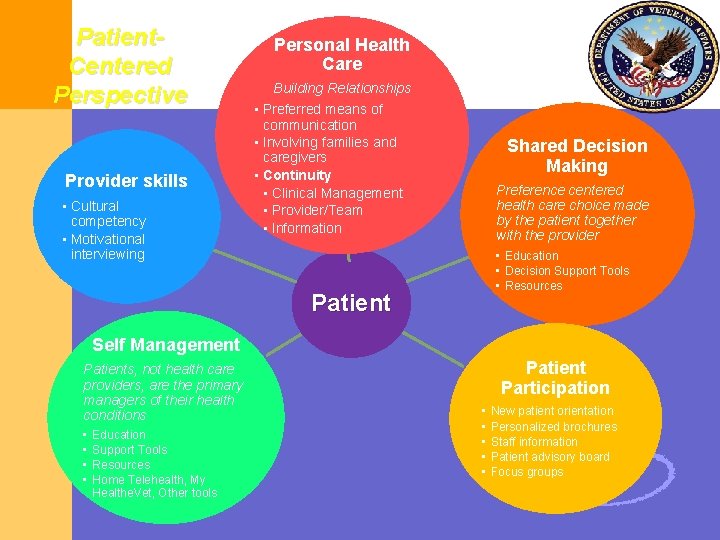
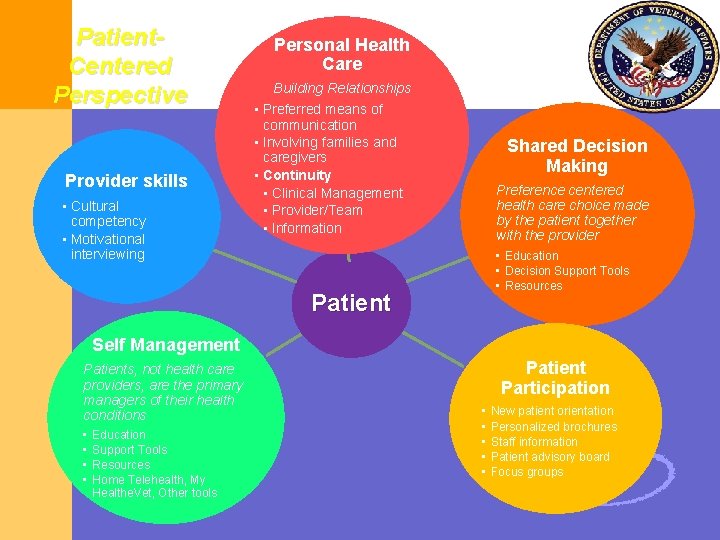
Patient. Centered Perspective Provider skills • Cultural competency • Motivational interviewing Personal Health Care Building Relationships • Preferred means of communication • Involving families and caregivers • Continuity • Clinical Management • Provider/Team • Information Shared Decision Making Preference centered health care choice made by the patient together with the provider • Education • Decision Support Tools • Resources Patient Self Management Patients, not health care providers, are the primary managers of their health conditions • • Education Support Tools Resources Home Telehealth, My Healthe. Vet, Other tools Patient Participation • • • New patient orientation Personalized brochures Staff information Patient advisory board Focus groups
34

THANK YOU FOR INVITING ME 感謝聆聽 Jo. Ann Damron-Rodriguez’s e-mail: jdamron@ucla. edu