preoperative evaluation and preparation for gynecologic surgery Dr


- Slides: 52
preoperative evaluation and preparation for gynecologic surgery Dr kh. Elmizadeh Gyneoncologist
The preoperative process should include comprehensive counseling of the patient regarding alternative treatment options (including expectant management) and risks and benefits of the procedure.
History 1 -Medical condition for which the procedure is performed 2 -Medical conditions and risk factors that increase the risk of perioperative complications 3 - Personal or family history or risk factors for thromboembolism 4 - Personal or family history of anesthesiarelated complications
Preoperative medical evaluation questions for a healthy patient Questions 1. Do you usually get chest pain or breathlessness when you climb up two flights of stairs at normal speed? 2. Do you have kidney disease? 3. Has anyone in your family (blood relatives) had a problem following an anaesthetic? 4. Have you ever had a heart attack? 5. Have you ever been diagnosed with an irregular heartbeat? 6. Have you ever had a stroke? 7. If you have been put to sleep for an operation were there any anaesthetic problems? 8. Do you suffer from epilepsy or seizures?
9. Do you have any problems with pain, stiffness or arthritis in your neck or jaw? 10. Do you have thyroid disease? 11. Do you suffer from angina? 12. Do you have liver disease? 13. Have you ever been diagnosed with heart failure? 14. Do you suffer from asthma? 15. Do you have diabetes that requires insulin? 16. Do you have diabetes that requires tablets only? 17. Do you suffer from bronchitis?
Medical comorbidities : Women with known or suspected medical comorbidities should be identified prior to surgery and referred for appropriate consultation regarding surgical clearance and perioperative management.
CLINICAL EVALUATION Age Exercise capacity Obesity Obstructive sleep apnea Alcohol misuse Smoking
All patients should be asked about their exercise capacity as part of the preoperative evaluation. Exercise capacity is an important determinant of overall perioperative risk; patients with good exercise tolerance generally have low risk.
Obesity in noncardiac surgery obesity is not a risk factor for most major adverse postoperative outcomes, with the exception of pulmonary embolism And obesity increases rates for wound infections
In cardiac surgery, some studies have shown higher complication rates for obese patients, including increased hospital stay , wound infections , prolonged mechanical ventilation , and atrial arrhythmias.
Obstructive sleep apnea OSA increases the risk for postoperative complications including hypoxemia, respiratory failure, , and ICU transfer. ……screening is reasonable.
misuse alcohol an increased risk for postoperative complications Surgical site infections, other infections, and cardiopulmonary complications The optimal period of cessation is unknown but at least four weeks
smoking current smokers have an increased risk for postoperative complications including general morbidity , wound complications , general infections, pulmonary complications, neurological complications and admission to an intensive care unit.
Laboratory studies While preoperative laboratory testing is not routinely indicated, selective testing is appropriate in specific circumstances, including patients with known underlying diseases or risk factors that would affect operative management or increase risk, and specific high-risk surgical procedures.
Pregnancy testing should be performed prior to gynecologic surgery in all women of reproductive age. This also applies to patients for whom there is uncertainty about sexual activity, effectiveness of contraception, or about menopausal status. If the patient is pregnant, procedures that may cause fetal harm or loss should be cancelled or postponed. Decisions regarding nonelective procedures that do not interfere with the pregnancy should be individualized and surgical planning should include measures to safeguard and monitor. The prevalence of unrecognized pregnancy was 0. 3 percent.
Hb, Hct Anemia is present in approximately 1 percent of asymptomatic patients; surgically significant anemia has an even lower prevalence However, anemia is common following major surgery and the preoperative hemoglobin level predicts postoperative mortality.
A baseline hemoglobin measurement is suggested for all patients≥ 65 years who are undergoing major surgery, and for younger patients undergoing major surgery that is expected to result in significant blood loss. In contrast, hemoglobin measurement is not necessary for those undergoing minor surgery unless the history suggests anemia.
WBC, , Platelet obtaining a CBC , including white count and platelet measurement, can be recommended if the cost is not substantially greater than the cost of a hemoglobin concentration alone. It is reasonable to measure platelet count when neuraxial anesthesia (spinal or epidural) is planned.
Renal function We suggest NOT obtaining a serum creatinine concentration, except in the following patients. Patients over the age of 50 undergoing intermediate or high risk surgery. Younger patients suspected of having renal disease, when hypotension is likely during surgery, or when nephrotoxic medications will be used.
Electrolytes The frequency of electrolyte abnormalities is low. While preoperative hypernatremia associated with an increase in perioperative 30 -day morbidity and mortality , the relationship between most electrolyte derangements and operative morbidity is not clear.

Thus, routine electrolyte determinations are NOT recommended unless the patient has a history that increases the likelihood of an abnormality.
Blood glucose There is no evidence that asymptomatic hyperglycemia, in a patient not previously known to have diabetes, increases surgical risk. Thus, routine measurement of blood glucose is NOT recommended for healthy patients.
Liver function tests Severe liver function test abnormalities are associated with increased surgical morbidity and mortality, but not mild abnormalities. Clinically-significant liver disease would most likely be suspected on the basis of the history and physical examination; thus, routine liver enzyme testing is NOT recommended.
Tests of hemostasis Routine preoperative tests of hemostasis are NOT recommended. If the evaluation suggests the presence of a bleeding disorder, appropriate screening tests should be performed, including (PT), (a. PTT), and platelet count.
Urinalysis Routine urinalysis is NOT recommended preoperatively for most surgical procedures.
ECG We suggest NOT ordering an ECG for asymptomatic patients undergoing low risk surgical procedures. a resting 12 -lead ECG should be part of the evaluation in patients with known coronary artery disease, significant arrhythmia, peripheral arterial disease, cerebrovascular disease, or other significant structural heart disease, except for those undergoing low-risk surgery. A preoperative resting ECG can be considered for asymptomatic patients undergoing surgery with elevated risk.
chest x-rays We suggest that clinicians NOT order routine preoperative chest x-rays or pulmonary function tests in the healthy patient.
SURGICAL SITE INFECTION PREVENTION
Antibiotic prophylaxis Antibiotics should be given prior to gynecologic surgery or procedures to prevent surgical site infection when the reproductive tract is entered or there is likely to be contamination of the peritoneal cavity from the vagina.
prophylactic antimicrobials can be given as a single IV dose begun within 60 minutes before the procedure. If vancomycin or a fluoroquinolone is used, the infusion should be given over 60 to 90 minutes and started within 60 to 120 minutes before the initial incision.
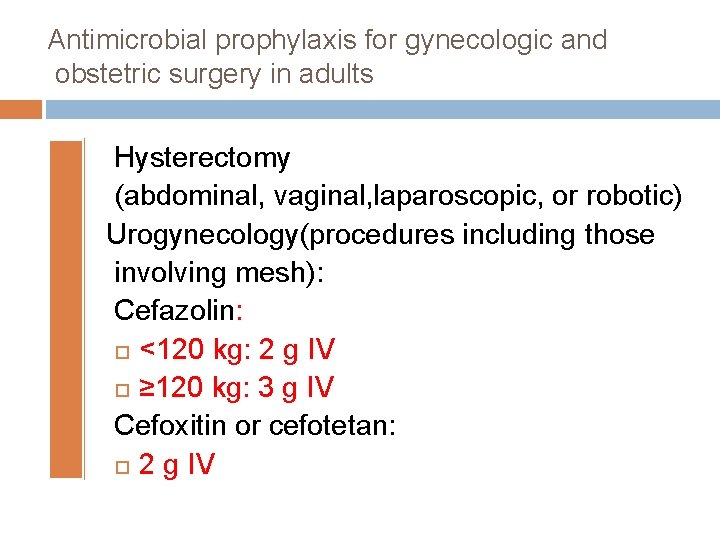
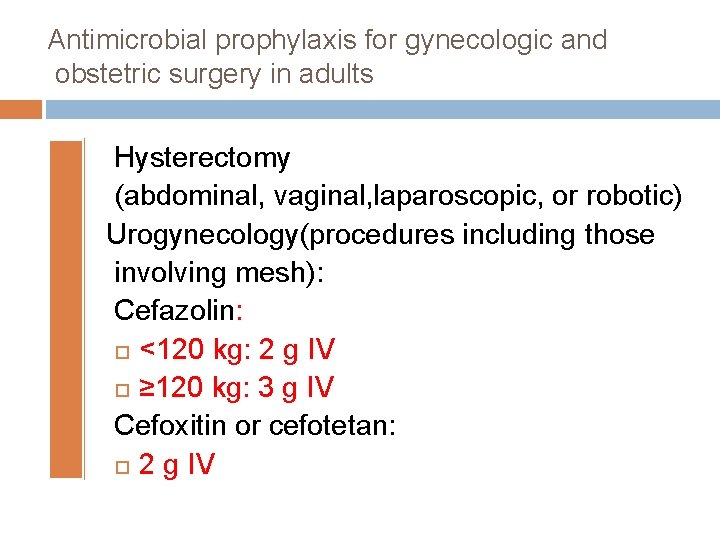
Antimicrobial prophylaxis for gynecologic and obstetric surgery in adults Hysterectomy (abdominal, vaginal, laparoscopic, or robotic) Urogynecology(procedures including those involving mesh): Cefazolin: <120 kg: 2 g IV ≥ 120 kg: 3 g IV Cefoxitin or cefotetan: 2 g IV
Alternative regimens Ampicillin-sulbactam 3 g IV
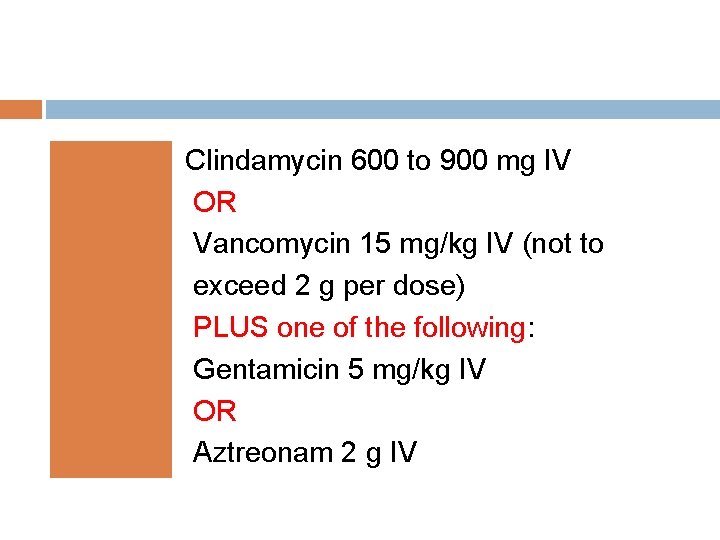
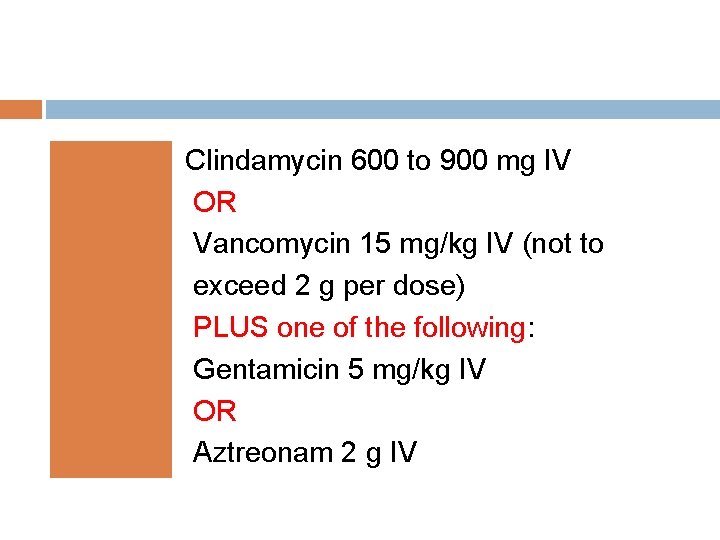
Clindamycin 600 to 900 mg IV OR Vancomycin 15 mg/kg IV (not to exceed 2 g per dose) PLUS one of the following: Gentamicin 5 mg/kg IV OR Aztreonam 2 g IV
Metronidazole 500 mg IV PLUS : Gentamicin 5 mg/kg IV
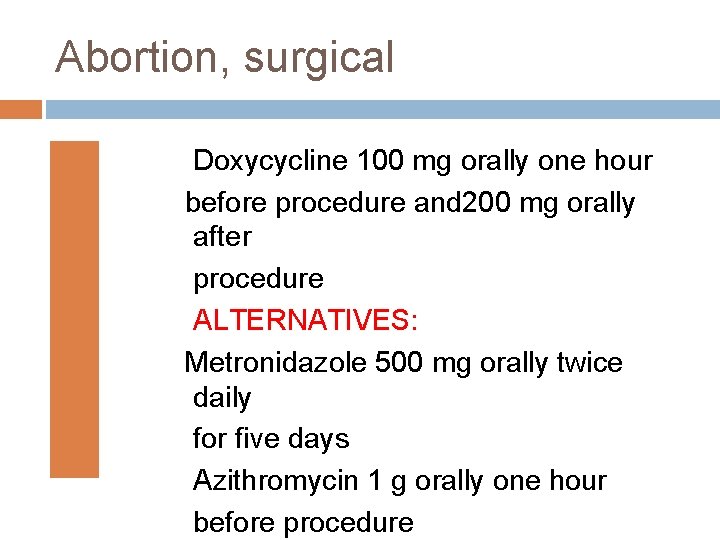
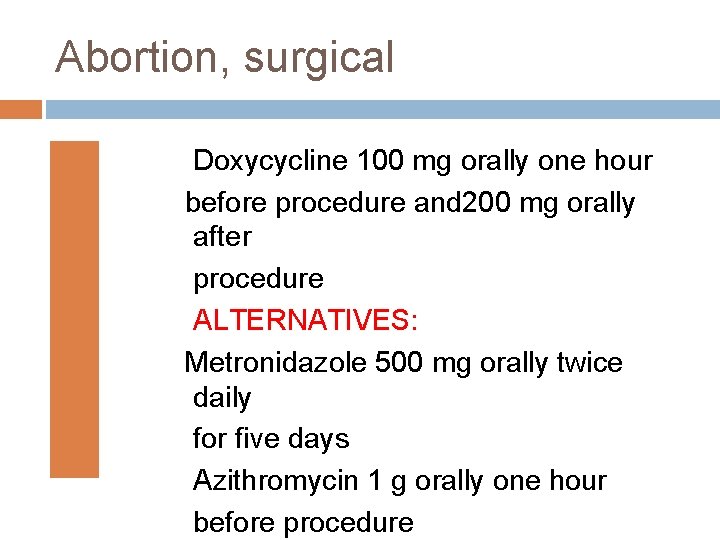
Abortion, surgical Doxycycline 100 mg orally one hour before procedure and 200 mg orally after procedure ALTERNATIVES: Metronidazole 500 mg orally twice daily for five days Azithromycin 1 g orally one hour before procedure

Hysterosalpingography Doxycycline 100 mg orally twice daily for five days Prophylaxis is warranted for patients with history of pelvic inflammatory disease or if the procedure demonstrates dilated fallopian tubes. ¤
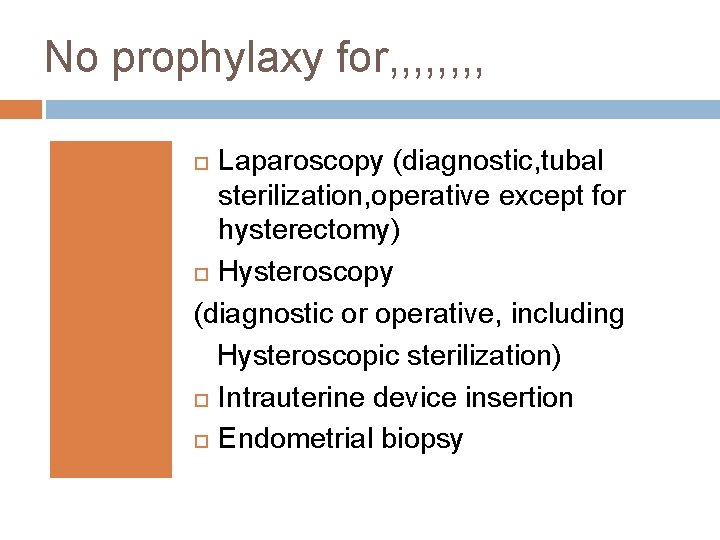
No prophylaxy for, , , , Laparoscopy (diagnostic, tubal sterilization, operative except for hysterectomy) Hysteroscopy (diagnostic or operative, including Hysteroscopic sterilization) Intrauterine device insertion Endometrial biopsy
Prevention of surgical site infection includes other measures in addition to antibiotics: These include skin antisepsis, hair removal, drapes, surgical hand hygiene, and surgical technique.
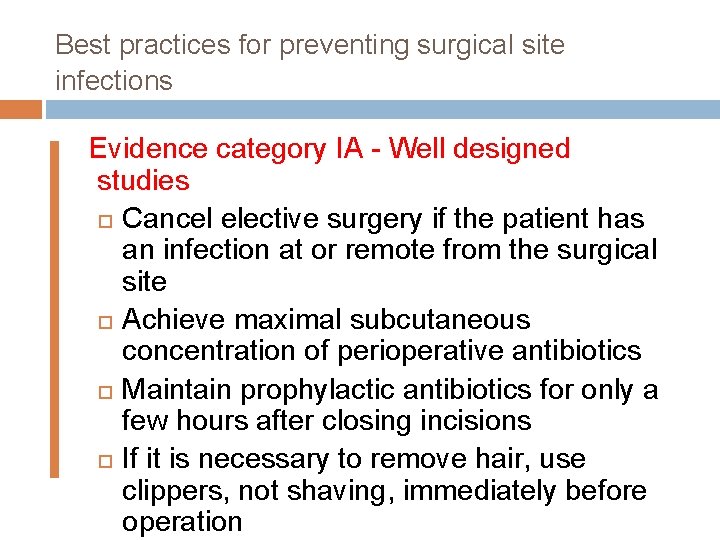
Best practices for preventing surgical site infections Evidence category IA - Well designed studies Cancel elective surgery if the patient has an infection at or remote from the surgical site Achieve maximal subcutaneous concentration of perioperative antibiotics Maintain prophylactic antibiotics for only a few hours after closing incisions If it is necessary to remove hair, use clippers, not shaving, immediately before operation
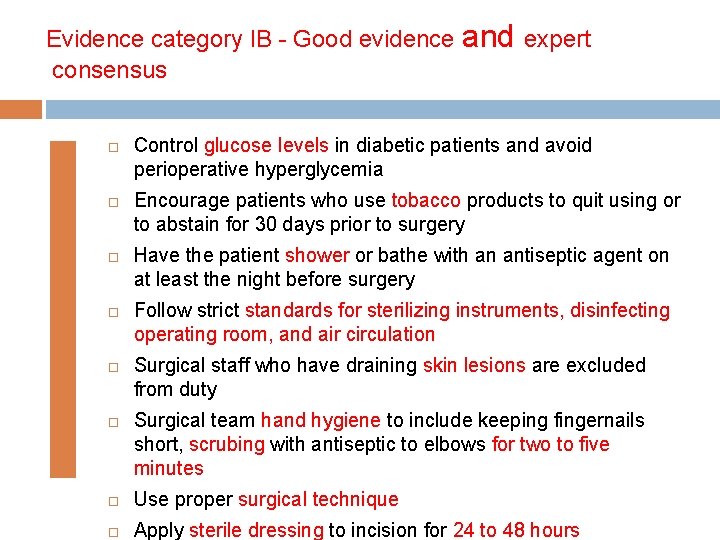
Evidence category IB - Good evidence and expert consensus Control glucose levels in diabetic patients and avoid perioperative hyperglycemia Encourage patients who use tobacco products to quit using or to abstain for 30 days prior to surgery Have the patient shower or bathe with an antiseptic agent on at least the night before surgery Follow strict standards for sterilizing instruments, disinfecting operating room, and air circulation Surgical staff who have draining skin lesions are excluded from duty Surgical team hand hygiene to include keeping fingernails short, scrubing with antiseptic to elbows for two to five minutes Use proper surgical technique Apply sterile dressing to incision for 24 to 48 hours
Vaginal preparation We suggest sterile preparation of the vagina if a procedure includes a vaginal incision or transvaginal use of instruments. There is no high-quality evidence to confirm that vaginal preparation alone or in addition to antibiotics contributes to surgical site infection prevention Povidone-iodine solution, , povidoneiodine gel, , , Chlorhexidine
THROMBOPROPHYLAXIS Thromboprophylaxis reduces the incidence of symptomatic DVT or pulmonary embolism. Decisions regarding the method, dose, and timing ofprophylaxis depend upon balancing a patient's risk of thrombosis versus bleeding. The most highly regarded guidelines regarding perioperative thromboprophylaxis are published by the American College of Chest Physicians.
Risk factors for the development of venous thrombosis
Inherited thrombophilia Factor V Leiden mutation Prothrombin gene mutation Protein S deficiency Protein C deficiency Antithrombin (AT) deficiency Dysfibrinogenemia
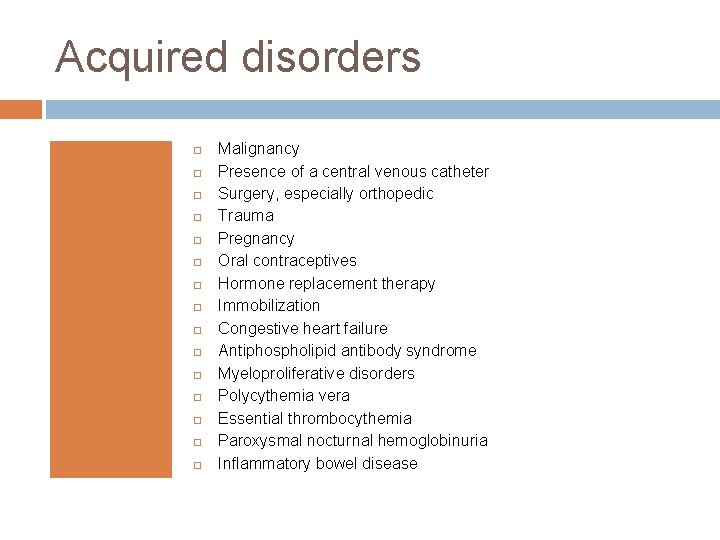
Acquired disorders Malignancy Presence of a central venous catheter Surgery, especially orthopedic Trauma Pregnancy Oral contraceptives Hormone replacement therapy Immobilization Congestive heart failure Antiphospholipid antibody syndrome Myeloproliferative disorders Polycythemia vera Essential thrombocythemia Paroxysmal nocturnal hemoglobinuria Inflammatory bowel disease
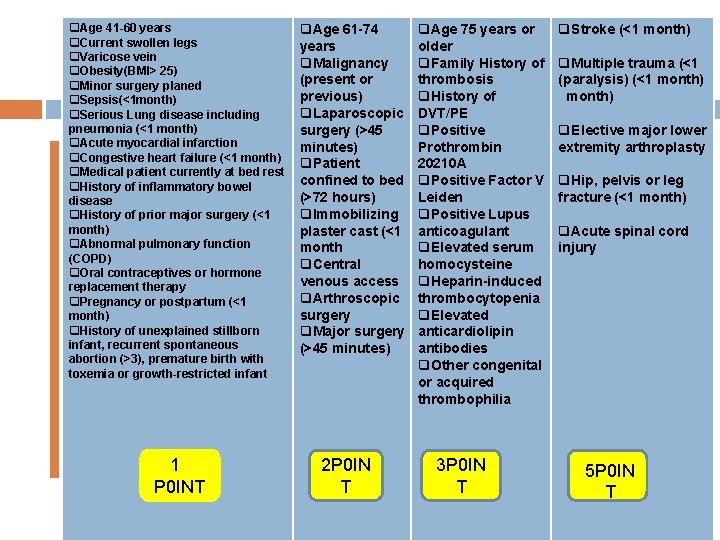
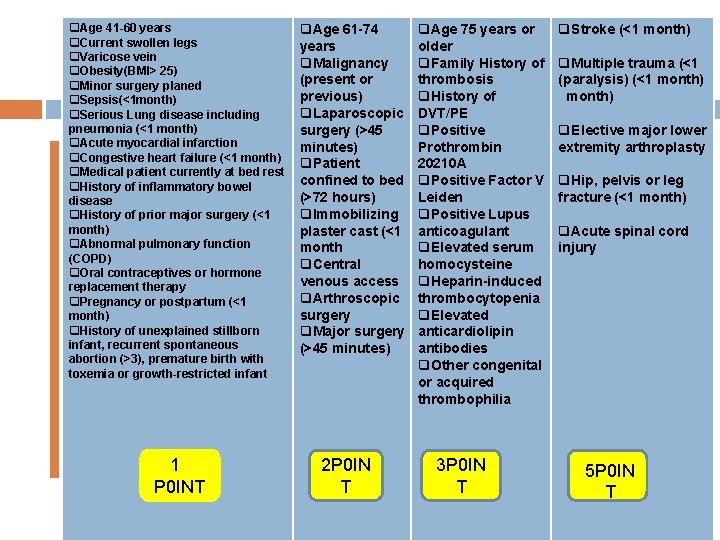
q. Age 41 -60 years q. Current swollen legs q. Varicose vein q. Obesity(BMI> 25) q. Minor surgery planed q. Sepsis(<1 month) q. Serious Lung disease including pneumonia (<1 month) q. Acute myocardial infarction q. Congestive heart failure (<1 month) q. Medical patient currently at bed rest q. History of inflammatory bowel disease q. History of prior major surgery (<1 month) q. Abnormal pulmonary function (COPD) q. Oral contraceptives or hormone replacement therapy q. Pregnancy or postpartum (<1 month) q. History of unexplained stillborn infant, recurrent spontaneous abortion (>3), premature birth with toxemia or growth-restricted infant 1 P 0 INT q. Age 61 -74 years q. Malignancy (present or previous) q. Laparoscopic surgery (>45 minutes) q. Patient confined to bed (>72 hours) q. Immobilizing plaster cast (<1 month q. Central venous access q. Arthroscopic surgery q. Major surgery (>45 minutes) 2 P 0 IN T q. Age 75 years or older q. Family History of thrombosis q. History of DVT/PE q. Positive Prothrombin 20210 A q. Positive Factor V Leiden q. Positive Lupus anticoagulant q. Elevated serum homocysteine q. Heparin-induced thrombocytopenia q. Elevated anticardiolipin antibodies q. Other congenital or acquired thrombophilia 3 P 0 IN T q. Stroke (<1 month) q. Multiple trauma (<1 (paralysis) (<1 month) q. Elective major lower extremity arthroplasty q. Hip, pelvis or leg fracture (<1 month) q. Acute spinal cord injury 5 P 0 IN T
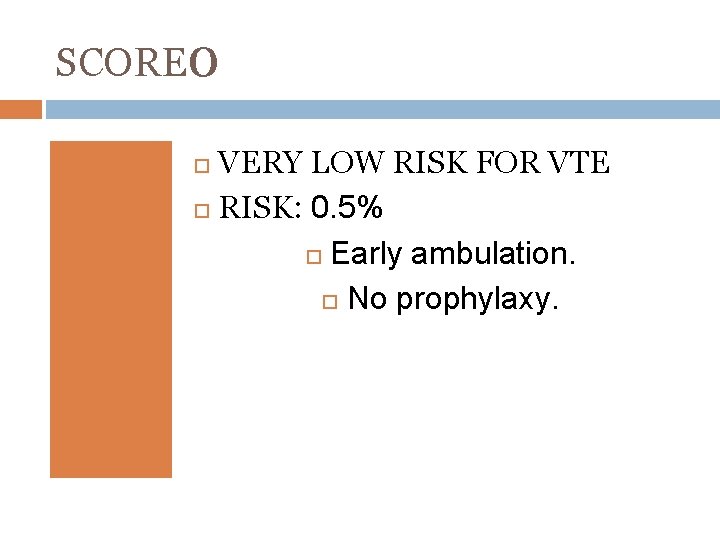
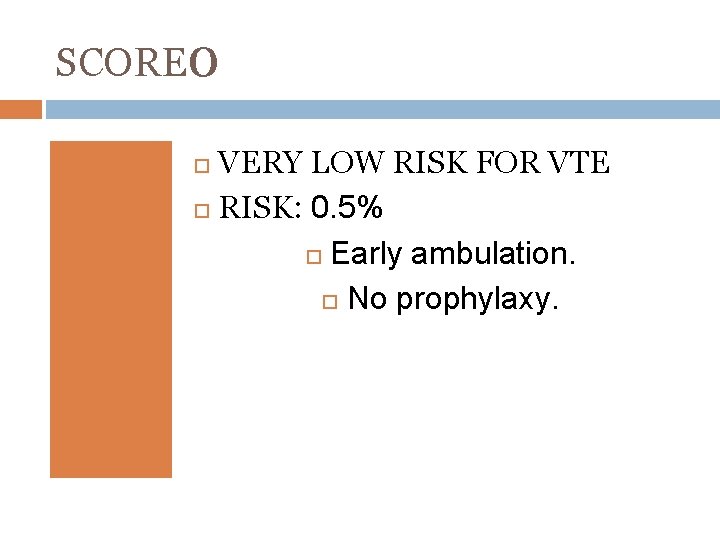
SCORE 0 VERY LOW RISK FOR VTE RISK: 0. 5% Early ambulation. No prophylaxy.
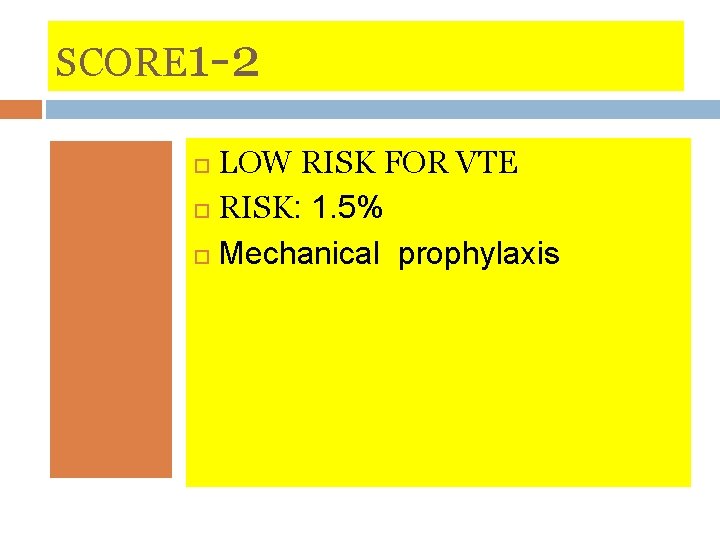
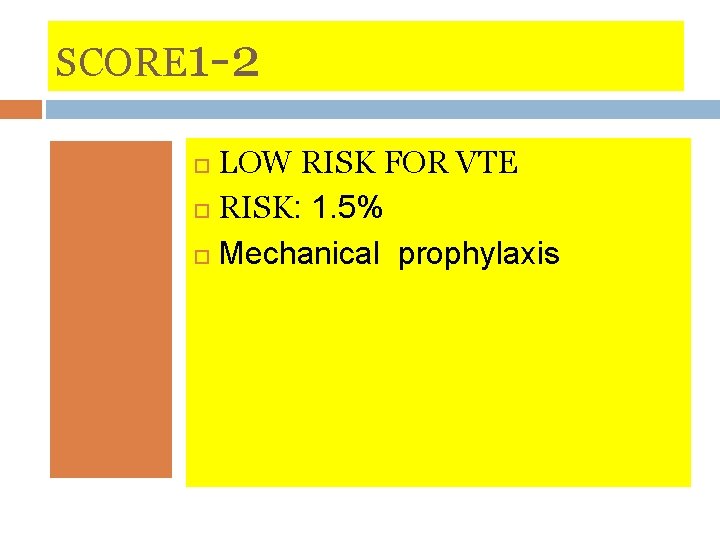
SCORE 1 -2 LOW RISK FOR VTE RISK: 1. 5% Mechanical prophylaxis
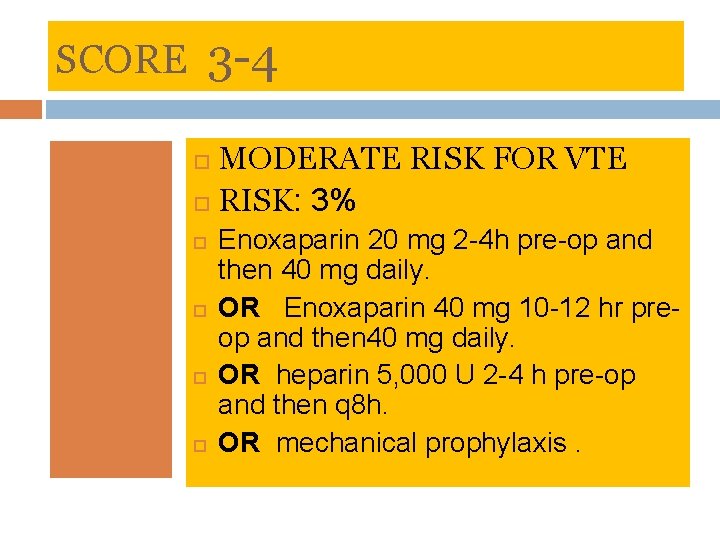
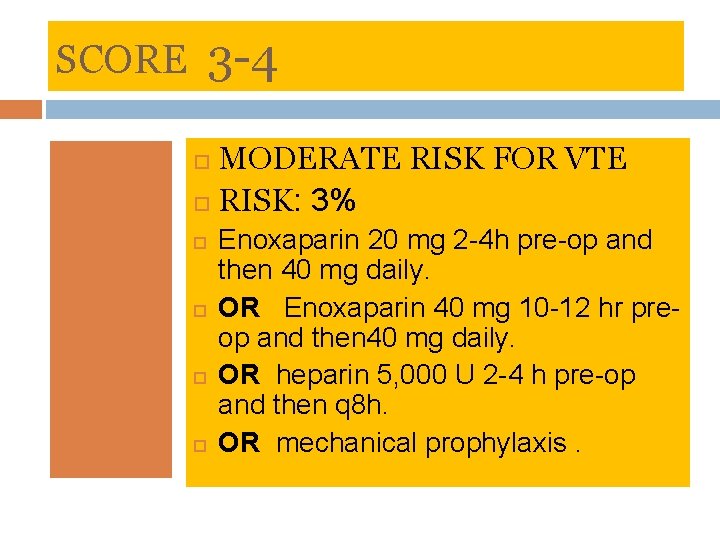
SCORE 3 -4 MODERATE RISK FOR VTE RISK: 3% Enoxaparin 20 mg 2 -4 h pre-op and then 40 mg daily. OR Enoxaparin 40 mg 10 -12 hr preop and then 40 mg daily. OR heparin 5, 000 U 2 -4 h pre-op and then q 8 h. OR mechanical prophylaxis.
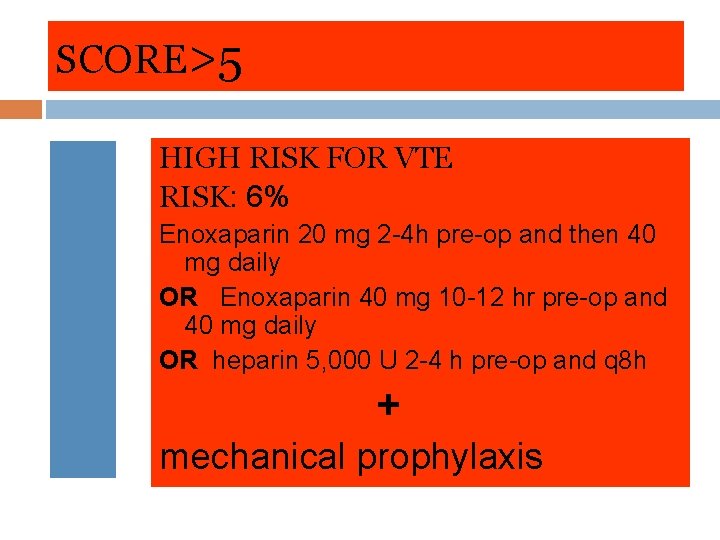
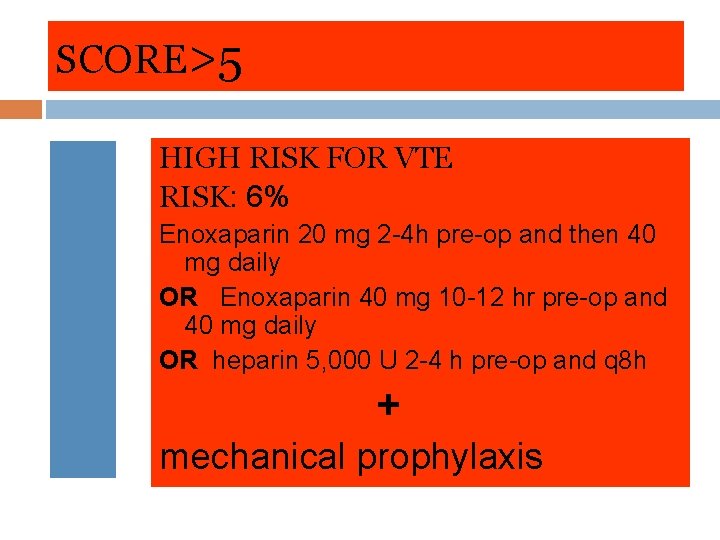
SCORE>5 HIGH RISK FOR VTE RISK: 6% Enoxaparin 20 mg 2 -4 h pre-op and then 40 mg daily OR Enoxaparin 40 mg 10 -12 hr pre-op and 40 mg daily OR heparin 5, 000 U 2 -4 h pre-op and q 8 h + mechanical prophylaxis
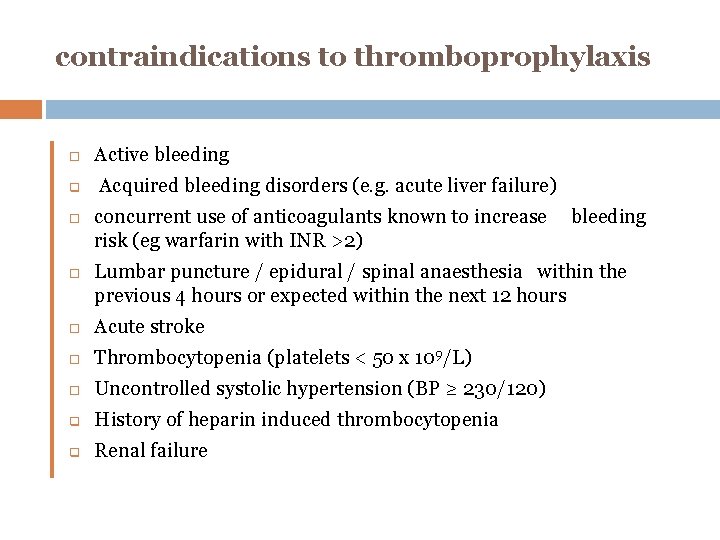
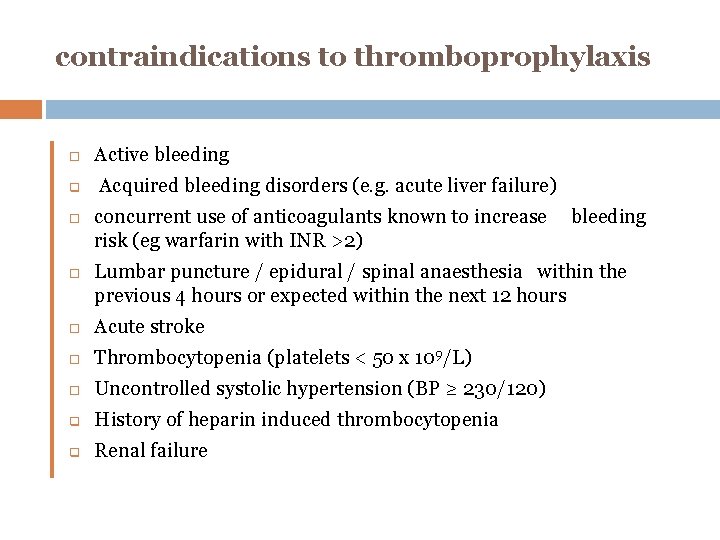
contraindications to thromboprophylaxis q Active bleeding Acquired bleeding disorders (e. g. acute liver failure) concurrent use of anticoagulants known to increase risk (eg warfarin with INR >2) bleeding Lumbar puncture / epidural / spinal anaesthesia within the previous 4 hours or expected within the next 12 hours Acute stroke Thrombocytopenia (platelets < 50 x 109/L) Uncontrolled systolic hypertension (BP ≥ 230/120) q History of heparin induced thrombocytopenia q Renal failure
THANKS FOR YOUR ATTENTION