PreOperation Evaluation of Thoracic Surgery Patient Spirometry and


- Slides: 22
Pre-Operation Evaluation of Thoracic Surgery Patient: Spirometry and Pulmonary Exercise test (PXT) 吳惠東
Risks of Operation Site n Extent of operation n Patients’ reserve n Anesthesia n Operator skill n
Pulmonary Risks by Operation Sites n Extra-thoracic Extremities n Low abdomen n Upper abdomen n n Intra-thoracic No Lung resection n Lung parenchyma resection n
Overview n ~ 30% of patients undergoing lung resection develop cardiopulmonary complications with a 30 -day mortality varying between 0. 6% and 5%, depending on the extent of lung resection. n Mortality: 5. 7% after pneumonectomy, 4. 4% after bilobectomy, 3. 9% after lobectomy.
Lung Function Test in Surgery Patients n Indication All Chest surgery patients n History of lung/airway disease n Heavy smoker n Exertional dyspnea n n Risks evaluation Peri-operation n Subacute, long-term n n Avoid pulmonary complication
Preoperative evaluation n n Identifying patients at risk evaluating the risk finding modified factors to decrease risk. Detailed medical history, physical examination Patient’s functional capacity, the degree of limitation of activity Pulmonary function testing: spirometry, lung volumes, diffusing capacity, oximetry, and arterial blood gases. Radionuclide lung scanning, exercise testing, invasive pulmonary hemodynamic measurements, and risk stratification analysis. Chest 2003; 123: 2096 -2103 Respir Med 2004; 98(7): 598 -605
Preoperative evaluation: Spirometry n n - - - Maximal voluntary ventilation < 50% of predicted and FVC < 70% of predicted were associated with a 40% risk for death. FEV 1 Most common PFT used for prediction Accounts for variability in the gender and size of patients for lung resection The important determinant of FEV 1 cut-off value is the extent 5 of lung resection. the incidence of postoperative pulmonary complications in patients with FEV 1 < 2 L was 40% vs 19% for those with FEV 1 > 2 L. Chest 2003; 123: 2096 -2103 Respir Med 2004; 98(7): 598 -605

Spirometry for Lung Resection n Pneumonectomy: FEV 1 >2 L; MVV >55% of predicted; n FEF 25– 75% >1. 6 L/s. n n Lobectomy FEV 1 >1 L; MVV >40% of predicted; n FEF 25– 75% >0. 6 L/s. n n Segmentectomy or wedge resection FEV 1 >0. 6 L; MVV >40% of predicted; n FEF 25– 75% >0. 6 L/s. n Chest 2003; 123: 2096 -2103
DLCO n n Independent predictor of postoperative outcome Reflects alveolar membrane integrity and pulmonary capillary blood flow in the patient’s lungs. Patients with DLCO≥ 70% predicted had a much lower postpneumonectomy complication rate than patients with DLCO<70% predicted. A low DLCO identifies patients with significant emphysema, and reduced pulmonary capillary vascular bed postoperative pulmonary hypertension, arrhythmia, cardiac dysfunction Chest 2003; 123: 2096 -2103 Respir Med 2004; 98(7): 598 -605
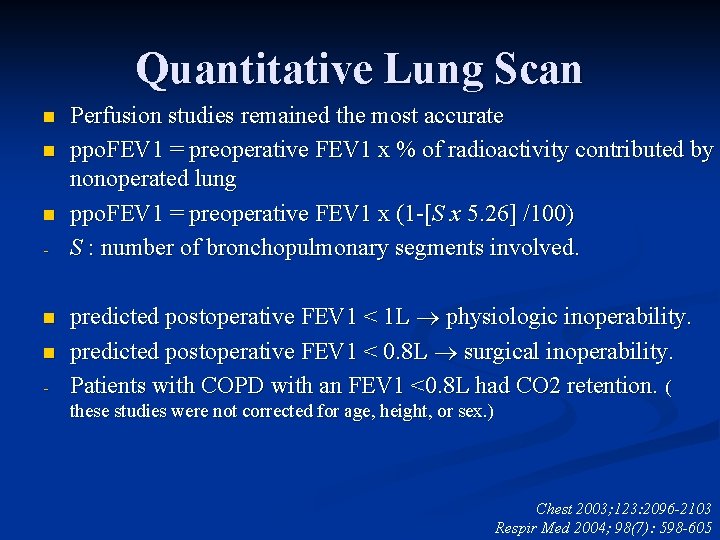
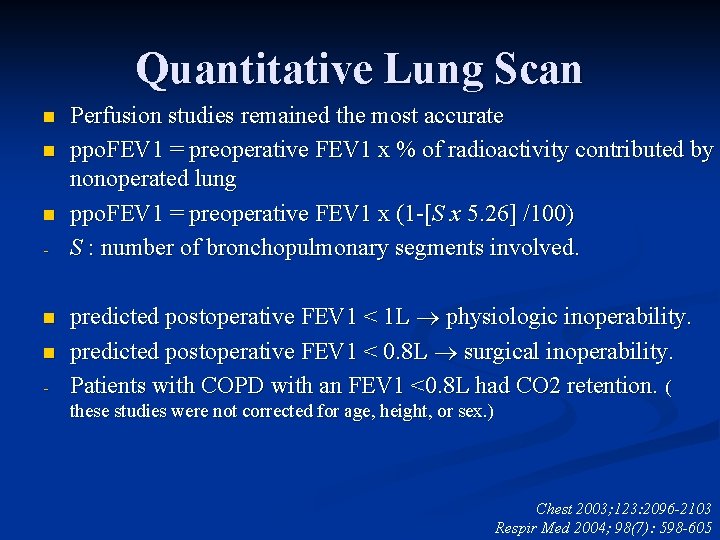
Quantitative Lung Scan n - Perfusion studies remained the most accurate ppo. FEV 1 = preoperative FEV 1 x % of radioactivity contributed by nonoperated lung ppo. FEV 1 = preoperative FEV 1 x (1 -[S x 5. 26] /100) S : number of bronchopulmonary segments involved. predicted postoperative FEV 1 < 1 L physiologic inoperability. predicted postoperative FEV 1 < 0. 8 L surgical inoperability. Patients with COPD with an FEV 1 <0. 8 L had CO 2 retention. ( these studies were not corrected for age, height, or sex. ) Chest 2003; 123: 2096 -2103 Respir Med 2004; 98(7): 598 -605
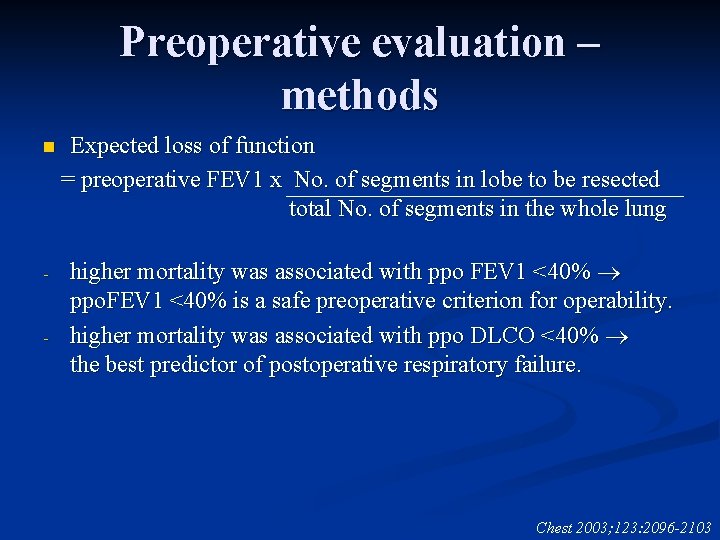
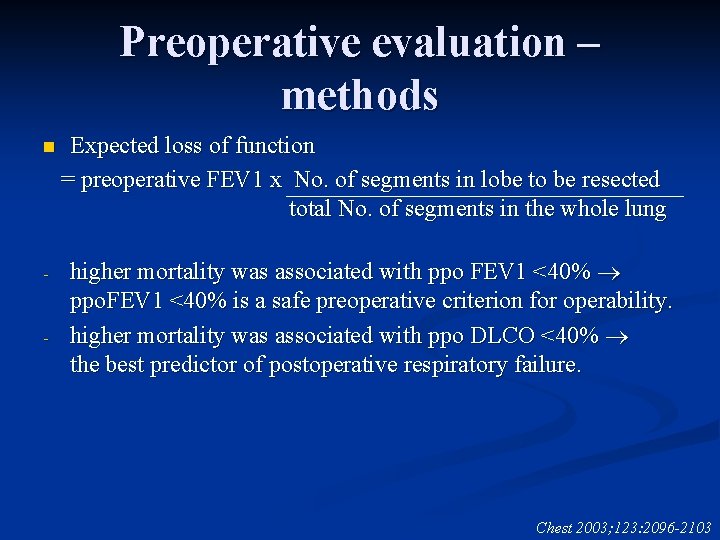
Preoperative evaluation – methods n - - Expected loss of function = preoperative FEV 1 x No. of segments in lobe to be resected total No. of segments in the whole lung higher mortality was associated with ppo FEV 1 <40% ppo. FEV 1 <40% is a safe preoperative criterion for operability. higher mortality was associated with ppo DLCO <40% the best predictor of postoperative respiratory failure. Chest 2003; 123: 2096 -2103
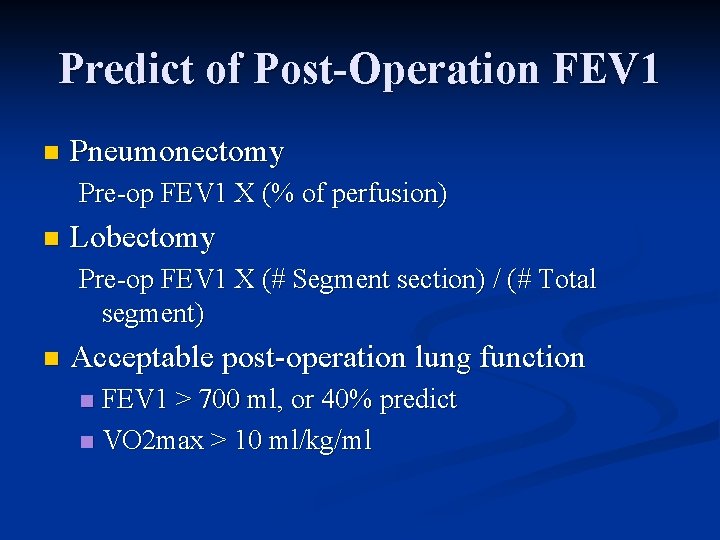
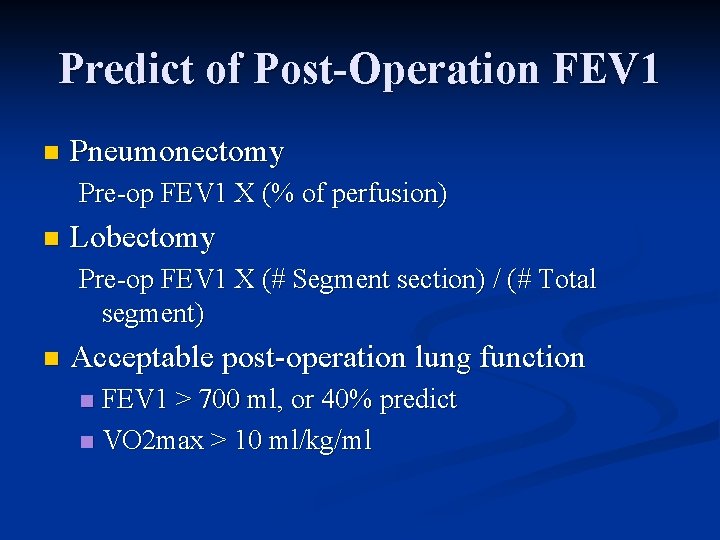
Predict of Post-Operation FEV 1 n Pneumonectomy Pre-op FEV 1 X (% of perfusion) n Lobectomy Pre-op FEV 1 X (# Segment section) / (# Total segment) n Acceptable post-operation lung function FEV 1 > 700 ml, or 40% predict n VO 2 max > 10 ml/kg/ml n
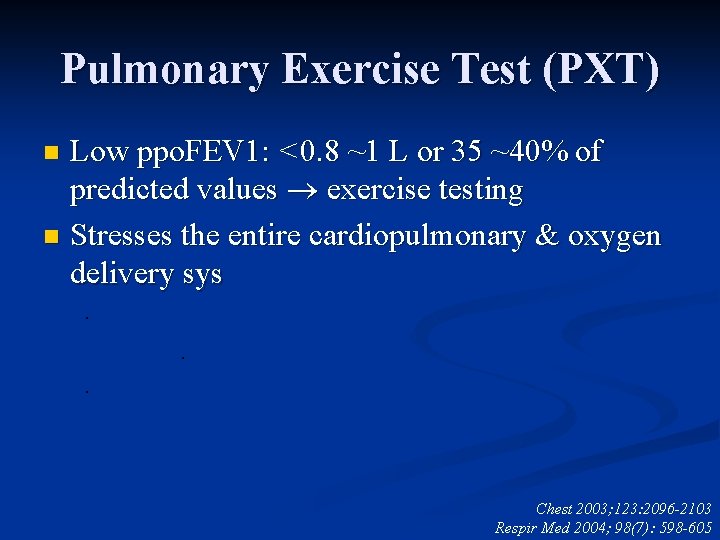
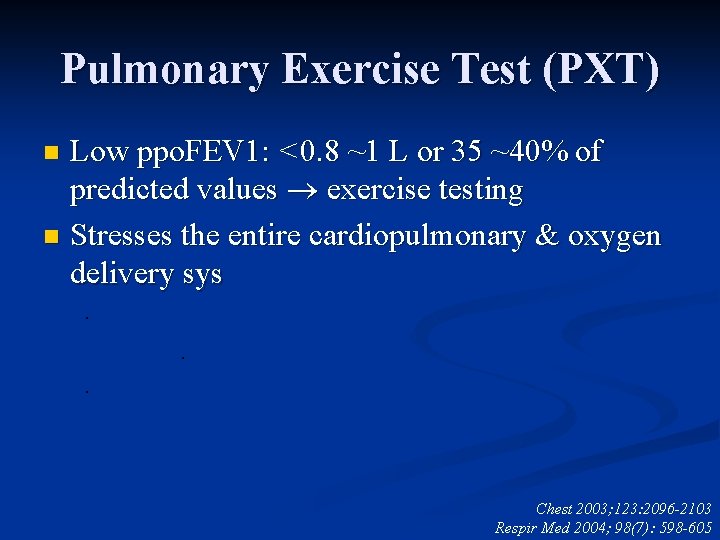
Pulmonary Exercise Test (PXT) Low ppo. FEV 1: <0. 8 ~1 L or 35 ~40% of predicted values exercise testing n Stresses the entire cardiopulmonary & oxygen delivery sys n . . . Chest 2003; 123: 2096 -2103 Respir Med 2004; 98(7): 598 -605
Oxygen uptake VO 2 is related to age, sex, weight, and type of work performed n VO 2 max >20 m. L/kg/min will tolerate surgery with acceptable morbidity and mortality n
PXT. Eugene et al. n VO 2 max > 1 L/min: Little complication Smith et al n VO 2 max > 20 ml/kg/min postoperative complications 10%. . VO 2 max 15~20 ml/kg/min postoperative complications 66% n . VO 2 max < 15 ml/kg/min postoperative complications 100% n Markos et al n oxygen desaturation during a 12 -min walk, ppo. DLCO, and ppo FEV 1 were more reliable predictors of postoperative mortality Chest 2003; 123: 2096 -2103

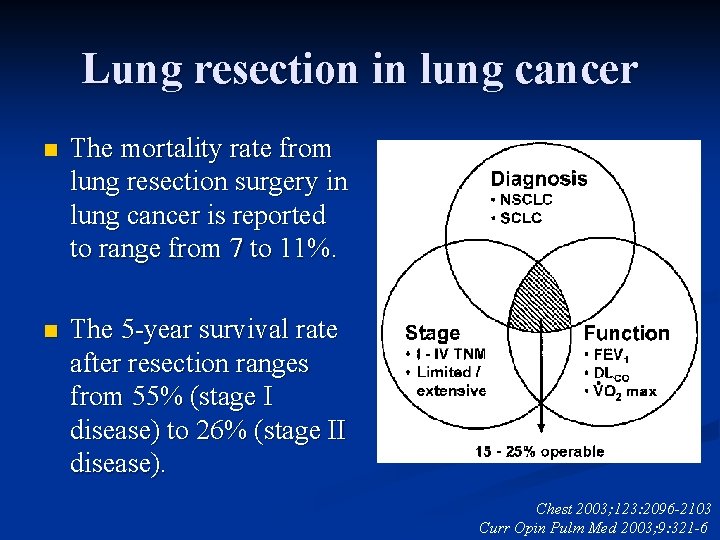
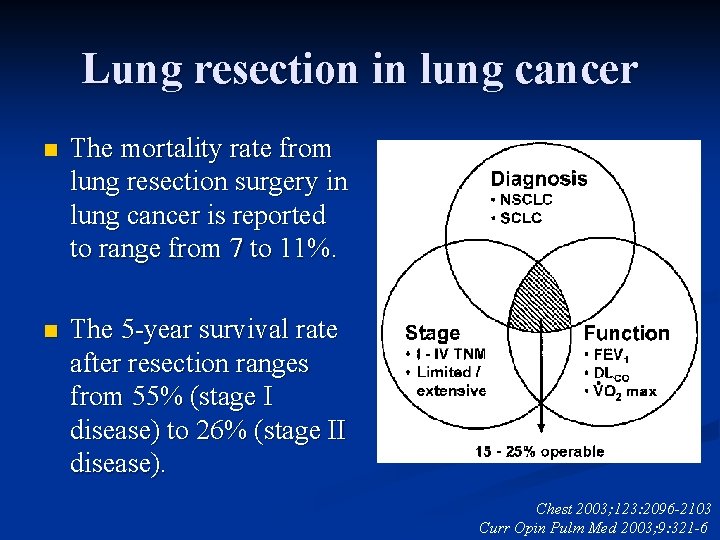
Lung resection in lung cancer n The mortality rate from lung resection surgery in lung cancer is reported to range from 7 to 11%. n The 5 -year survival rate after resection ranges from 55% (stage I disease) to 26% (stage II disease). Chest 2003; 123: 2096 -2103 Curr Opin Pulm Med 2003; 9: 321 -6
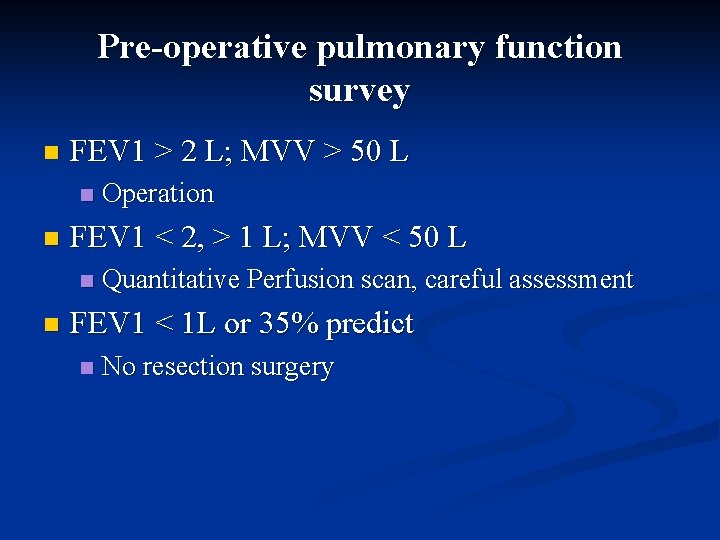
Pre-operative pulmonary function survey n FEV 1 > 2 L; MVV > 50 L n n FEV 1 < 2, > 1 L; MVV < 50 L n n Operation Quantitative Perfusion scan, careful assessment FEV 1 < 1 L or 35% predict n No resection surgery
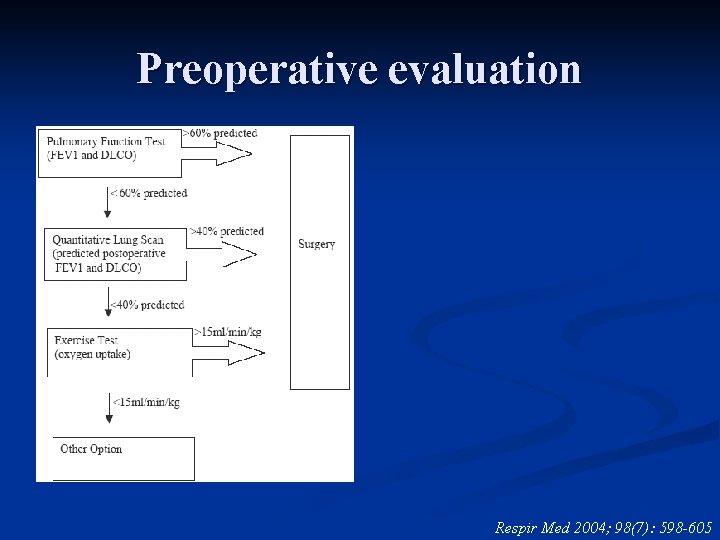
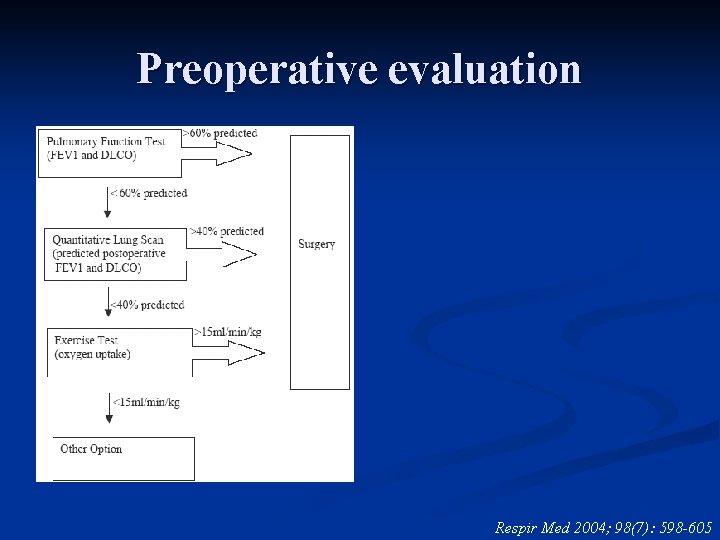
Preoperative evaluation Respir Med 2004; 98(7): 598 -605
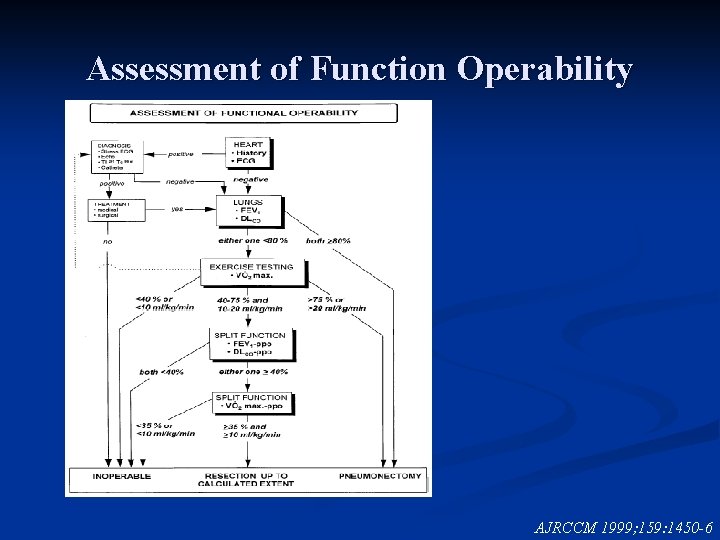
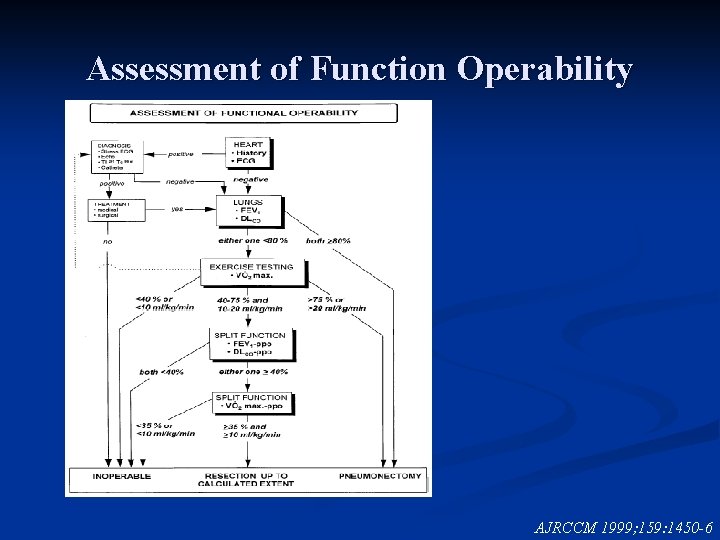
Assessment of Function Operability AJRCCM 1999; 159: 1450 -6
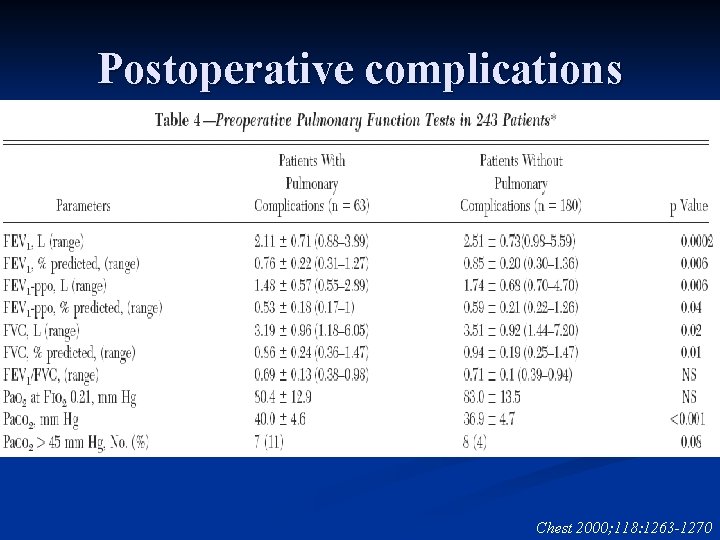
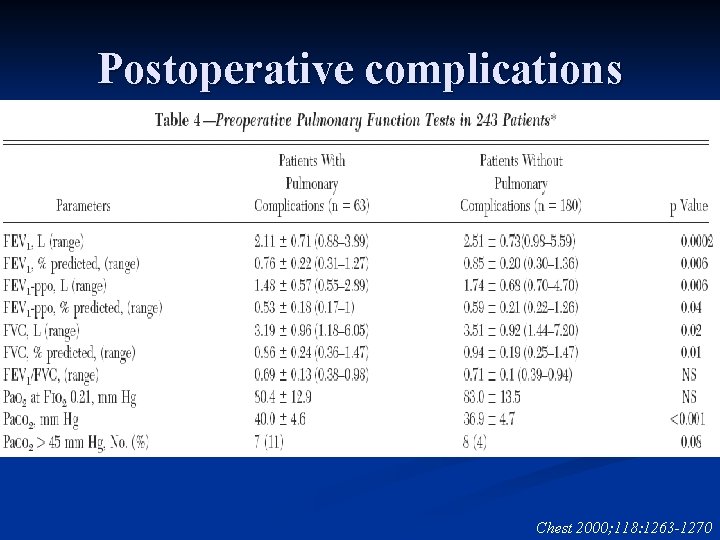
Postoperative complications Chest 2000; 118: 1263 -1270
Thanks