Pregnancy at Risk Pregestational Onset Alcohol Use in



























- Slides: 147
Pregnancy at Risk: Pregestational Onset
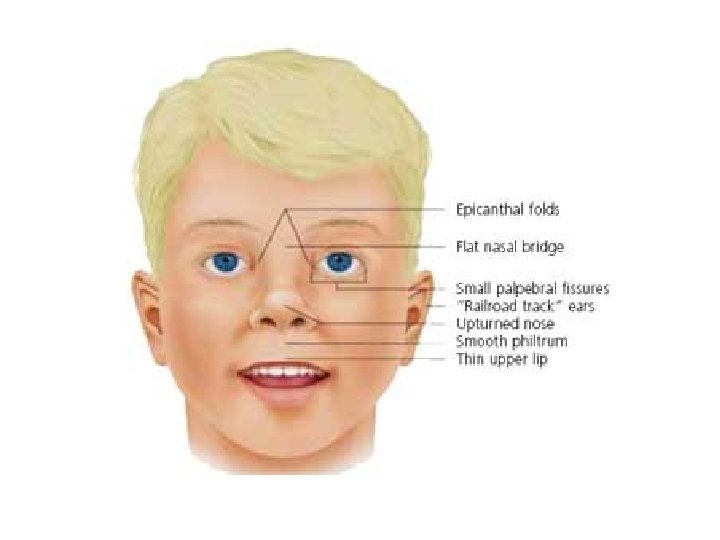
Alcohol Use in Pregnancy • Maternal effects: – Malnutrition – Bone-marrow suppression – Increased incidence of infections – Liver disease • Neonatal effects: – Fetal alcohol spectrum disorders (FASD)


Cocaine Use in Pregnancy: Maternal Effects • • • Seizures and hallucinations Pulmonary edema Respiratory failure Cardiac problems Spontaneous first trimester abortion, abruptio placentae, intrauterine growth restriction (IUGR), preterm birth, and stillbirth
Cocaine Use in Pregnancy: Fetal Effects • Decreased birth weight and head circumference • Feeding difficulties • Neonatal effects from breast milk: – Extreme irritability – Vomiting and diarrhea – Dilated pupils and apnea
Heroin Use in Pregnancy • Maternal effects: – Poor nutrition and iron-deficiency anemia – Preeclampsia-eclampsia – Breech position – Abnormal placental implantation – Abruptio placentae – Preterm labor
Heroin Use in Pregnancy (cont’d) • Maternal effects: – Premature rupture of the membranes (PROM) – Meconium staining – Higher incidence of STIs and HIV • Fetal effects: – IUGR – Withdrawal symptoms after birth
Substance Use in Pregnancy: Maternal Effects • Marijuana: difficult to evaluate, no known teratogenic effects • PCP - maternal overdose or a psychotic response • MDMA (Ecstasy) - long-term impaired memory and learning

Pathology of Diabetes Mellitus (DM) • Endocrine disorder of carbohydrate metabolism • Results from inadequate production or utilization of insulin • Cellular and extracellular dehydration • Breakdown of fats and proteins for energy
Gestational Diabetes (GDM) • Carbohydrate intolerance of variable severity • Causes: – An unidentified preexistent disease – The effect of pregnancy on a compensated metabolic abnormality – A consequence of altered metabolism from changing hormonal levels

Effect of Pregnancy on Carbohydrate Metabolism • Early pregnancy: – Increased insulin production and tissue sensitivity • Second half of pregnancy: – Increased peripheral resistance to insulin
Maternal Risks with DM • • • Hydramnios Preeclampsia-eclampsia Ketoacidosis Dystocia Increased susceptibility to infections
Fetal and Neonatal Risks with DM • • • Perinatal mortality Congenital anomalies Macrosomia IUGR RDS Polycythemia
Fetal and Neonatal Risks with DM (cont’d) • Hyperbilirubinemia • Hypocalcemia
Screening for DM in Pregnancy • Assess risk at first visit: – Low risk - screen at 24 to 28 weeks – High risk - screen as early as feasible
Risk Factors • Age over 40 • Family history of diabetes in a first-degree relative • Prior macrosomic, malformed, or stillborn infant • Obesity • Hypertension • Glucosuria
Screening Tests • One-hour glucose tolerance test: – Level greater than 130 -140 mg/dl requires further testing • 3 -hour glucose tolerance test: – GDM diagnosed if 2 levels are exceeded
Treatment Goals • Maintain a physiologic equilibrium of insulin availability and glucose utilization • Ensure an optimally healthy mother and newborn • Treatment: – Diet therapy and exercise – Glucose monitoring – Insulin therapy
Fetal Assessment • • • AFP Fetal activity monitoring NST Biophysical profile Ultrasound
Nursing Management • Assessment of glucose • Nutrition counseling • Education about the disease process and management • Education about glucose monitoring and insulin administration • Assessment of the fetus • Support
Iron-deficiency Anemia • Maternal complications: – Susceptible to infection – May tire easily – Increased chance of preeclampsia and postpartal hemorrhage – Tolerates poorly even minimal blood loss during birth
Iron-deficiency Anemia (cont’d) • Fetal complications: – Low birth weight – Prematurity – Stillbirth – Neonatal death
Iron Deficiency Anemia (cont’d) • Prevention and treatment: – Prevention - at least 27 mg of iron daily – Treatment - 60 -120 mg of iron daily
Folate Deficiency • Maternal complications: – Nausea, vomiting, and anorexia • Fetal complications: – Neural tube defects • Prevention - 4 mg folic acid daily • Treatment - 1 mg folic acid daily plus iron supplements
Folate Deficiency • Maternal complications: – Nausea, vomiting, and anorexia • Fetal complications: – Neural tube defects • Prevention - 4 mg folic acid daily • Treatment - 1 mg folic acid daily plus iron supplements
Sickle Cell Anemia • Maternal complications: – Vaso-occlusive crisis – Infections – Congestive heart failure – Renal failure
Sickle Cell Anemia (cont’d) • Fetal complications include fetal death, prematurity, and IUGR. • Treatment: – Folic acid – Prompt treatment of infections – Prompt treatment of vaso-occlusive crisis
Thalassemia • Treatment: – Folic acid – Transfusion – Chelation

HIV in Pregnancy • Asymptomatic women - pregnancy has no effect • Symptomatic with low CD 4 count pregnancy accelerates the disease • Zidovudine (ZDV) therapy diminishes risk of transmission to fetus • Transmitted through breast milk • Half of all neonatal infections occurs during labor and birth
HIV in Pregnancy: Maternal Risks • • Intrapartal or postpartal hemorrhage Postpartal infection Poor wound healing Infections of the genitourinary tract
HIV Effects on Fetus • Infants will often have a positive antibody titer • Infected infants are usually asymptomatic but are likely to be: – Premature – Low birth weight – Small for gestational age (SGA)
Treatment During Pregnancy • Counsel about implications of diagnosis on pregnancy: – Antiretroviral therapy – Fetal testing – Cesarean birth
Cardiac Disorders in Pregnancy • • • Congenital heart disease Marfan syndrome Peripartum cardiomyopathy Eisenmenger syndrome Mitral valve prolapse
Less Common Medical Conditions in Pregnancy • • • Rheumatoid arthritis Epilepsy Hepatitis B Hyperthyroidism Hypothyroidism Maternal phenylketonuria
Less Common Medical Conditions in Pregnancy (cont’d) • Multiple sclerosis • Systemic lupus erythematosus • Tuberculosis
Pregnancy at Risk: Gestational Onset
Spontaneous Abortion • • Threatened abortion Imminent abortion Incomplete abortion Complete abortion
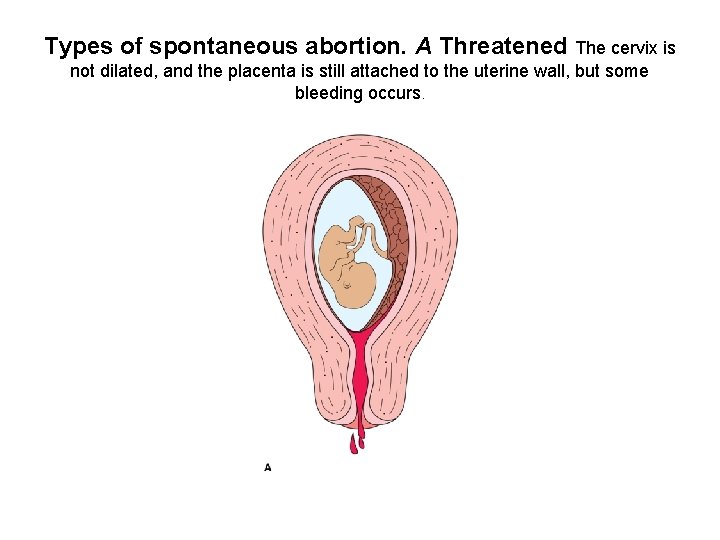
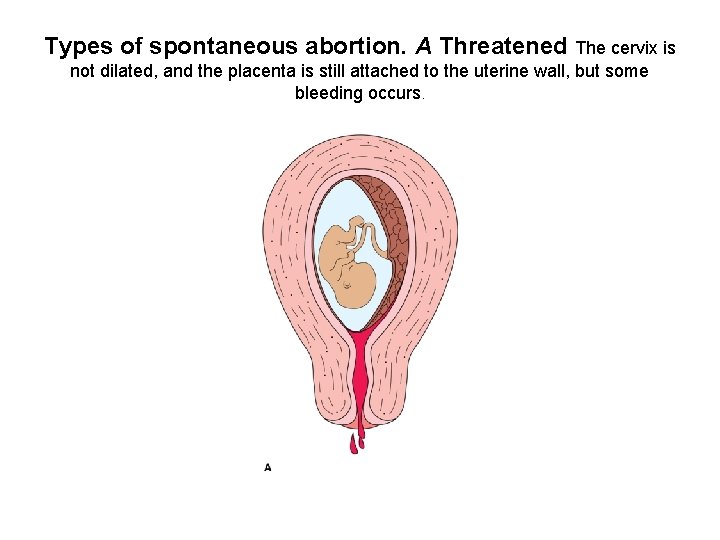
Types of spontaneous abortion. A Threatened The cervix is not dilated, and the placenta is still attached to the uterine wall, but some bleeding occurs.

B Imminent. The placenta has separated from the uterine wall, the cervix has dilated, and the amount of bleeding has increased.
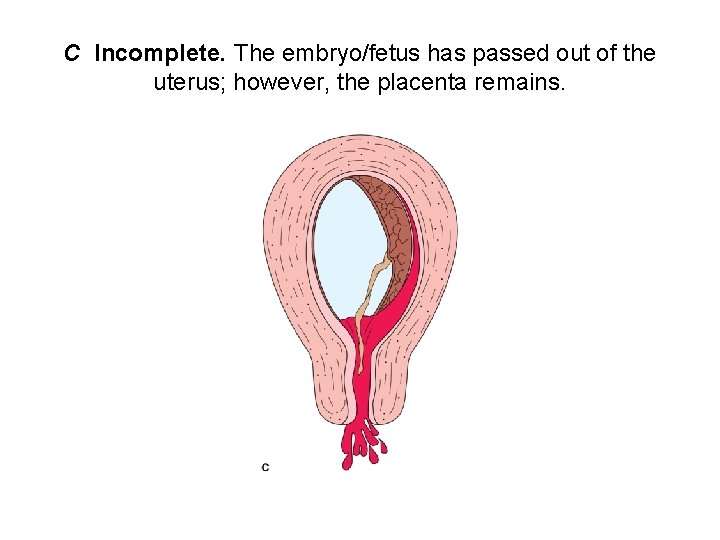
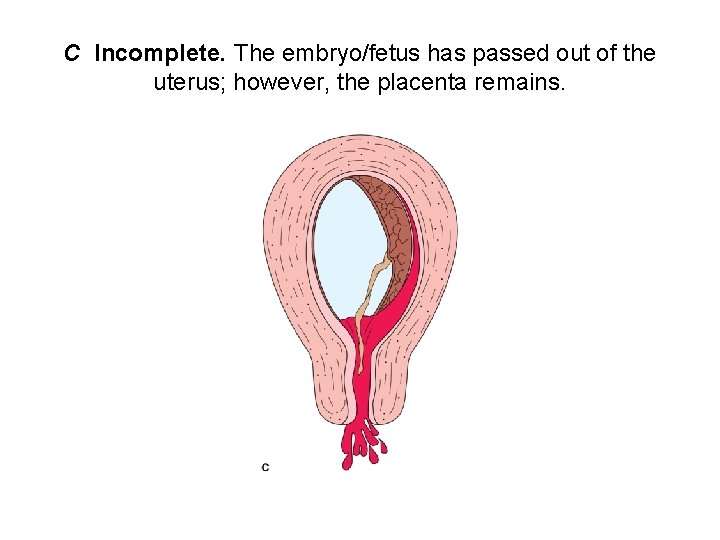
C Incomplete. The embryo/fetus has passed out of the uterus; however, the placenta remains.
Spontaneous Abortion (cont’d) • Missed abortion • Recurrent pregnancy loss • Septic abortion
Spontaneous Abortion: Treatment • • Bed rest Abstinence from coitus D&C or suction evacuation Rh immune globulin
Spontaneous Abortion: Nursing Care • Assess the amount and appearance of any vaginal bleeding • Monitor the woman’s vital signs and degree of discomfort • Assess need for Rh immune globulin. • Assess fetal heart rate • Assess the responses and coping of the woman and her family
Ectopic Pregnancy: Risk Factors • • • Tubal damage Previous pelvic or tubal surgery Endometriosis Previous ectopic pregnancy Presence of an IUD High levels of progesterone
Ectopic Pregnancy: Risk Factors (cont’d) • • • Congenital anomalies of the tube Use of ovulation-inducing drugs Primary infertility Smoking Advanced maternal age
Ectopic Pregnancy: Treatment • Methotrexate • Surgery

Various implantation sites in ectopic pregnancy. The most common site is within the fallopian tube, hence the name “tubal pregnancy
Ectopic Pregnancy: Nursing Care • Assess the appearance and amount of vaginal bleeding • Monitors vital signs • Assess the woman’s emotional status and coping abilities • Evaluate the couple’s informational needs. • Provide post-operative care
Gestational Trophoblastic Disease: Symptoms • • Vaginal bleeding Anemia Passing of hydropic vesicles Uterine enlargement greater than expected for gestational age • Absence of fetal heart sounds • Elevated h. CG
Gestational Trophoblastic Disease: Symptoms • Low levels of MSAFP • Hyperemesis gravidarum • Preeclampsia
Gestational Trophoblastic Disease: Treatment • D&C • Possible hysterectomy • Careful follow-up
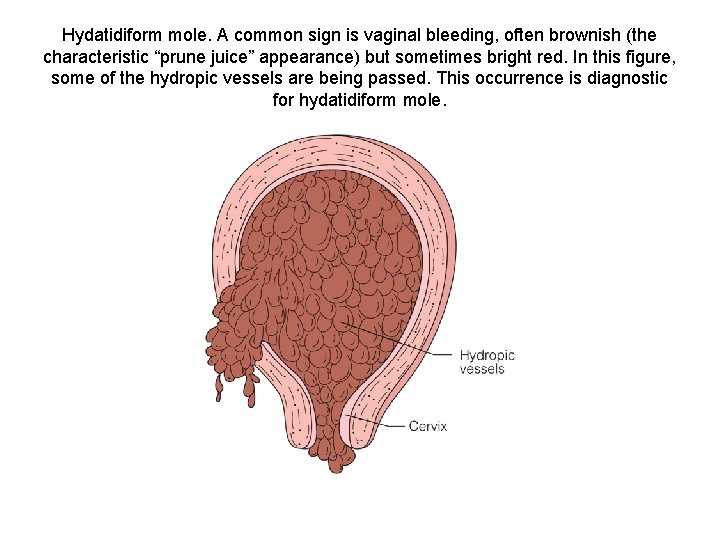
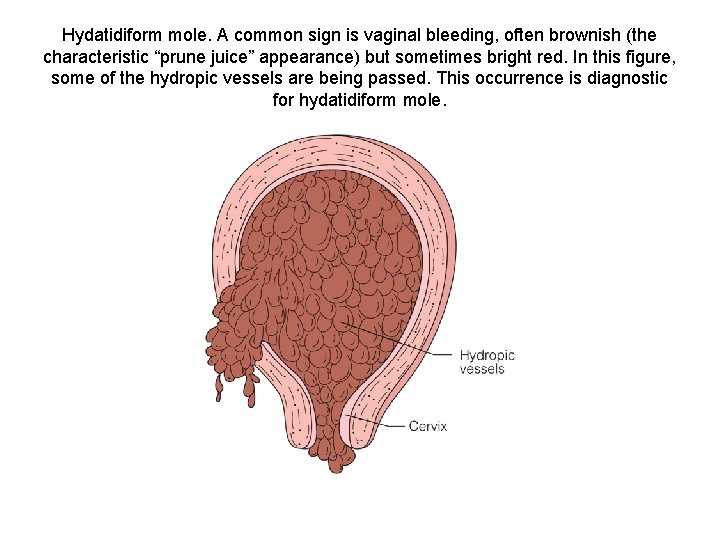
Hydatidiform mole. A common sign is vaginal bleeding, often brownish (the characteristic “prune juice” appearance) but sometimes bright red. In this figure, some of the hydropic vessels are being passed. This occurrence is diagnostic for hydatidiform mole.
Gestational Trophoblastic Disease: Nursing Care • • Monitor vital signs Monitor vaginal bleeding Assess abdominal pain Assess the woman’s emotional state and coping ability
Bleeding Disorders • Placenta previa - placenta is improperly implanted in the lower uterine segment • Abruptio placentae - premature separation of a normally implanted placenta from the uterine wall

Cervical Incompetence: Treatment • • • Serial cervical ultrasound assessments Bed rest Progesterone supplementation Antibiotics Anti-inflammatory drugs Cerclage procedures

A cerclage or purse-string suture is inserted in the cervix to prevent preterm cervical dilatation and pregnancy loss. After placement, the string is tightened and secured anteriorly.
Hyperemesis Gravidarum: Treatment • • Control vomiting Correct dehydration Restore electrolyte balance Maintain adequate nutrition

Hyperemesis Gravidarum: Nursing Care • Assess the amount and character of further emesis • Assess intake and output and weight. • Assess fetal heart rate • Assess maternal vital signs • Observe for evidence of jaundice or bleeding • Assess the woman’s emotional state
Nursing Care of Clients with PROM • Determine duration of PROM • Assess gestational age • Observe for signs and symptoms of infection • Assess hydration status • Assess fetal status • Assess childbirth preparation and coping
Nursing Clients with PROM (cont’d) • Encourage resting on left side • Provide comfort measures • Provide education
Nursing Care of Clients with Preterm Labor • Identify risk for preterm labor • Assess change in risk status for preterm labor • Assess educational needs of the woman and her loved ones • Assess the woman’s responses to medical and nursing intervention • Teach about the importance of recognizing the onset of labor
Signs and Symptoms of Preterm Labor • Uterine contractions occurring every 10 minutes or less • Mild menstrual like cramps felt low in the adbomen • Constant or intermittent feeling of pelvic pressure • Rupture of membranes • Low, dull backache, which may be constant or intermittent

Signs and Symptoms of Preterm Labor (cont’d) • A change in vaginal discharge • Abdominal cramping with or without diarrhea

Classification of Hypertension in Pregnancy • Preeclampsia-eclampsia • Chronic hypertension with superimposed preeclampsia • Gestational hypertension
Chronic Hypertension in Pregnancy • Hypertension before 20 weeks without proteinurea or stable proteinurea • At a higher risk for adverse outcomes • At risk for development of preeclampsia
Chronic Hypertension • If target organ damage present, pregnancy can exacerbate the condition • Lifestyle modifications: - Activity restrictions - Weight reduction - Sodium restriction - ETOH and tobacco strongly discouraged

Plan of Care – Chronic Hypertension in Pregnancy Medications can safely be withheld in patients: 1. Without target organ damage 2. Blood pressure less than 150 -160 mm. Hg systolic and 100 -110 diastolic
Pharmacological management: Chronic HTN in Pregnancy • Methyldopa (Aldomet) preferred alpha-2 adrenergic agonist • Labetalol (normodyne, Trandate) beta blocker • Diuretic, calcium antagonists, other beta blockers? • ACE (angiotension converting enzyme) inhibitors are contraindicated in pregnancy – IUGR, oligohydramnios, neonatal renal failure, and neonatal death • ARB (angiotension receptor blockers)not researched in pregnancy but probably contraindicated
Labatalol • Baby at risk for transient hypotension and hypogylcemia if mom on labatalol • No labatalol to clients with asthma or first degree heart block

Fetal Assessment • Fetal growth restriction • Ultrasound @ 18 -20 weeks, 28 -32 weeks & as needed thereafter • NST or biophysical profile if growth restricted
Preeclampsia-eclampsia • Increased blood pressure AND proteinurea • Highly suspected if increased BP and headache, blurred vision, abdominal pain, low platelets and/or abnormal liver enzymes

MAP • Mean Arterial Pressure – average of systolic and diastolic blood pressure readings SBP + DBP 3 • ACOG states hypertension exists when there is an increase in the MAP of 20 mm. Hg, and if no baselines are known, a MAP of 105 mm. Hg is used • Two readings 4 -6 hours apart
Hypertension in Pregnancy • Hypertension complicates 5 -7% of all pregnancies • One-half to two-thirds have preeclampsia or eclampsia • Hypertension is a leading cause of maternal and infant morbidity and mortality
Normal Adaptations to Pregnancy • Increased blood plasma volume • Vasodilation • Decreased systemic vascular resistance • Elevated cardiac output • Decreased colloid osmotic pressure
Preeclamptic Changes in Pregnancy • Renal lesions are present, especially in nulliparous women (85%) • Arteriolar vasospasm: diminishes the diameter of the blood vessels which impedes blood flow to organs and raises blood pressure (perfusion to placenta, kidneys, liver, and brain can be diminished by 40 -60%)

Etiology of Hypertension • Vasospasms are one of the underlying mechanisms for the signs and symptoms of preeclampsia • Endothelial damage (from decreased placental perfusion) contributes to preeclampsia • With endothelial damage, arteriolar vasospasm may contribute to increased capillary permeability. This increases edema and decreases intravascular volume
Other Suspected Causes • The presence of foreign protein (placenta or fetus) may trigger an immunologic response • This is supported by: - the incidence of preeclampsia in first-time mothers (first exposure to fetal tissue) - women pregnant by a new partner (different genetic material)
Pulmonary Preeclamptic Changes • At risk for development of pulmonary edema • Pulmonary capillaries susceptible to fluid leakage across membranes due to endothelial damage • Left ventricular failure from increased afterload leading to backup of fluid in pulmonary bed
Renal Preeclamptic Changes • Reduced kidney perfusion decreases the glomerular filtration rate which lead to degenerative changes and oliguria • Protein is lost in the urine, sodium and water are retained • Fluid moves out of the intravascular compartment resulting in increased blood viscosity and tissue edema
Vascular Preeclamptic Changes • Hematocrit level rises as fluid leaves the cells • Blood volume may fall to or below prepregnancy levels; severe edema develops and weight gain is seen • Decreased liver perfusion causes impaired function. Epigastric pain or RUQ pain
More Preeclamptic Changes • Arteriolar vasospasms with decreased blood perfusion to the retina causes visual changes such as blind spots and blurring • CNS changes caused by spasms as well as edema include headache, hyperreflexia, positive ankle clonus, and occasionally the development of eclampsia
Characteristics of Preeclampsia • • • Maternal vasospasm Decreased perfusion to virtually all organs Decrease in plasma volume Activation of the coagulation cascade Alterations in glomerular capillary endothelium • Edema

Characteristics of Preeclampsia • Increased viscosity of the blood • Hyperreflexia • Headache • Subcapsular hematoma of the liver
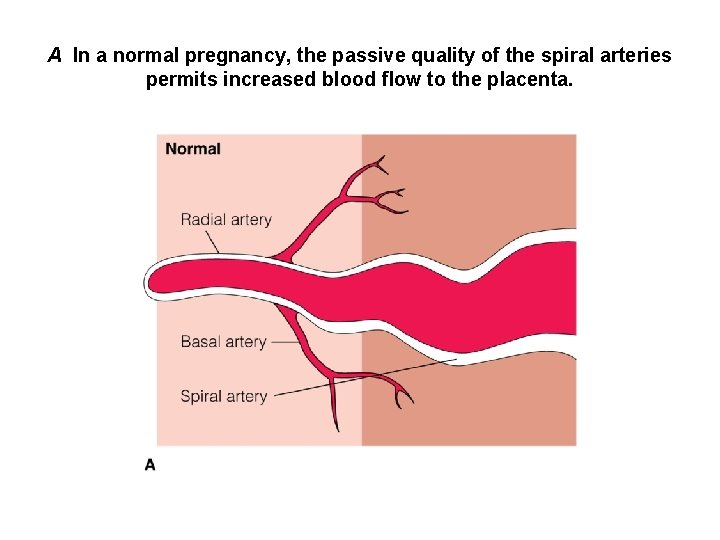
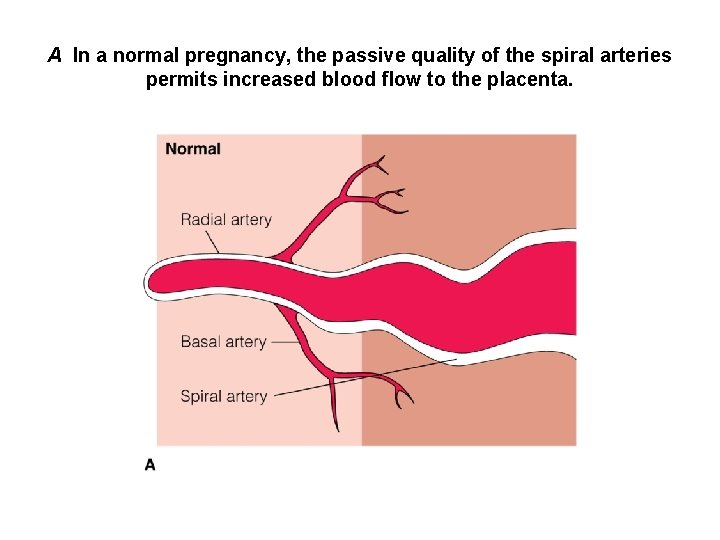
A In a normal pregnancy, the passive quality of the spiral arteries permits increased blood flow to the placenta.
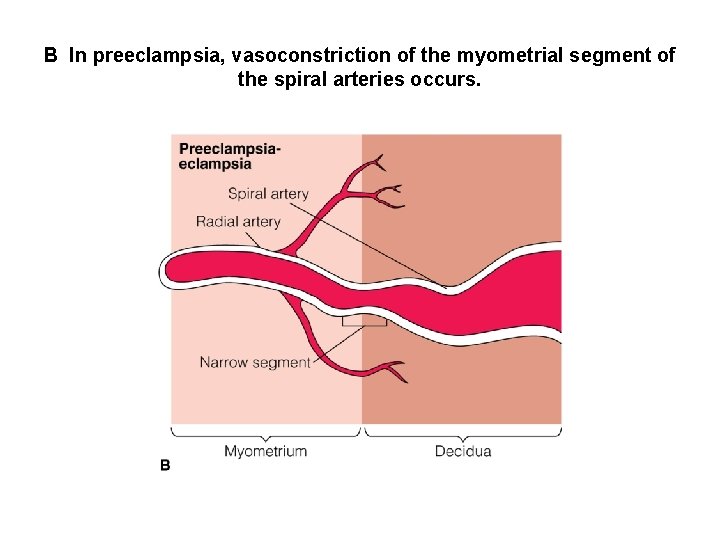
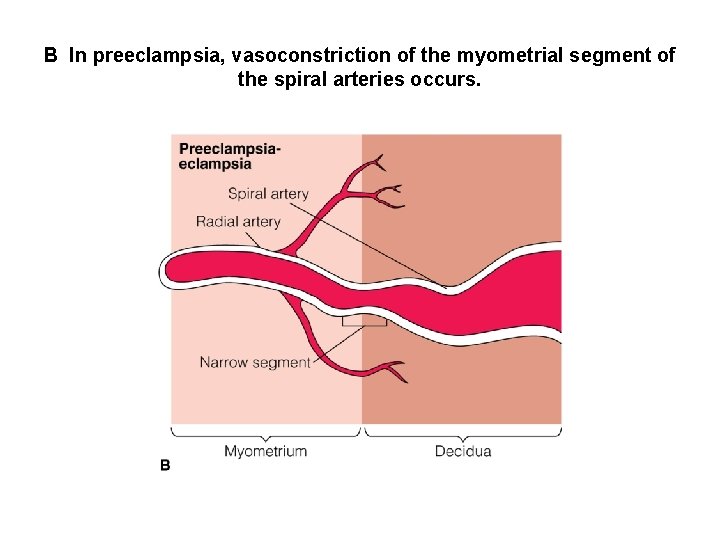
B In preeclampsia, vasoconstriction of the myometrial segment of the spiral arteries occurs.
What is the possible end result? • Heart failure, caused by circulatory collapse and shock • Pulmonary edema, associated with severe generalized edema (weak, rapid pulse, lowered blood pressure, crackles) • HELLP Syndrome: Multisystem disease in which hemolysis, elevated liver enzymes and low platelets are present • Disseminated Intravascular Coagulation: (DIC) • Clotting factors are consumed by excess fluid, generalized bleeding occurs. Thrombocytopenia

Differential Diagnosis • BP of > 160 systolic or > 110 diastolic • Proteinurea of 1 -2+ on 2 dipsticks at least 4 hours apart or. 3 grams or more in 24 hours • Increased serum creatinine > 1. 2 unless prior elevation • Platelet count less than 100, 000 • Elevated ALT or AST • Persistent headache or visual changes • Persistent epigastric pain, nausea and vomiting
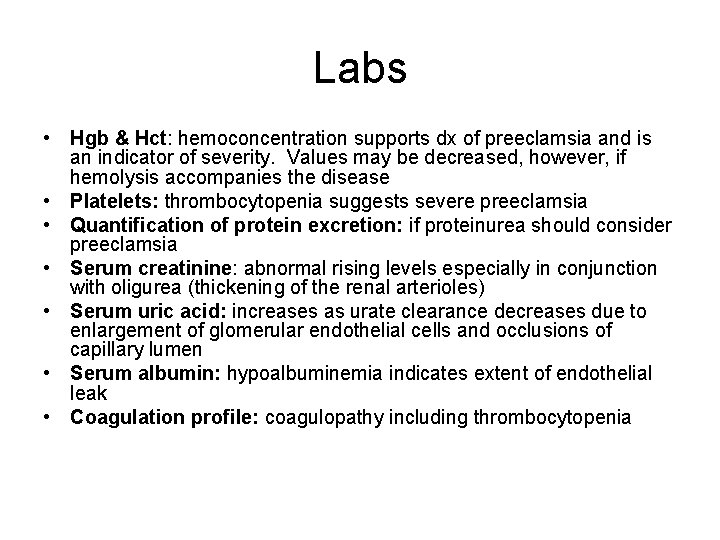
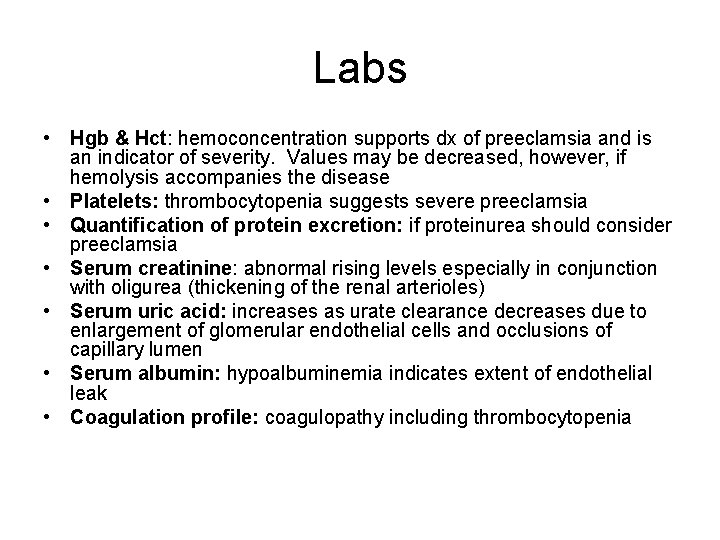
Labs • Hgb & Hct: hemoconcentration supports dx of preeclamsia and is an indicator of severity. Values may be decreased, however, if hemolysis accompanies the disease • Platelets: thrombocytopenia suggests severe preeclamsia • Quantification of protein excretion: if proteinurea should consider preeclamsia • Serum creatinine: abnormal rising levels especially in conjunction with oligurea (thickening of the renal arterioles) • Serum uric acid: increases as urate clearance decreases due to enlargement of glomerular endothelial cells and occlusions of capillary lumen • Serum albumin: hypoalbuminemia indicates extent of endothelial leak • Coagulation profile: coagulopathy including thrombocytopenia
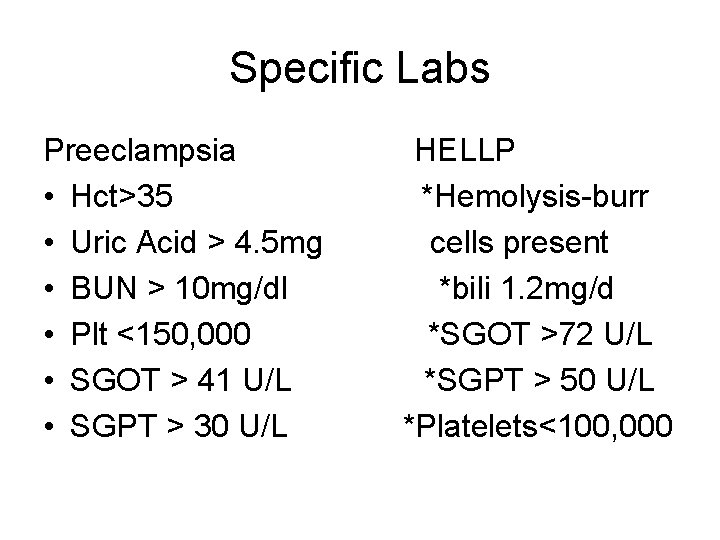
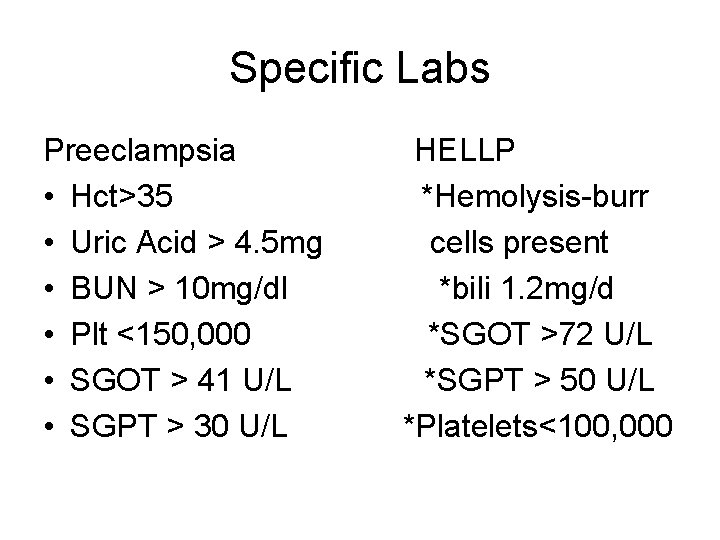
Specific Labs Preeclampsia • Hct>35 • Uric Acid > 4. 5 mg • BUN > 10 mg/dl • Plt <150, 000 • SGOT > 41 U/L • SGPT > 30 U/L HELLP *Hemolysis-burr cells present *bili 1. 2 mg/d *SGOT >72 U/L *SGPT > 50 U/L *Platelets<100, 000

Hypertensive Effects on Fetus • Small for gestational age • Fetal hypoxia • Death related to abruption • Prematurity
Home Management • Monitoring for signs and symptoms of worsening condition • Fetal movement counts • Frequent rest in the left lateral position • Monitoring of blood pressure, weight, and urine protein daily • NST • Laboratory testing
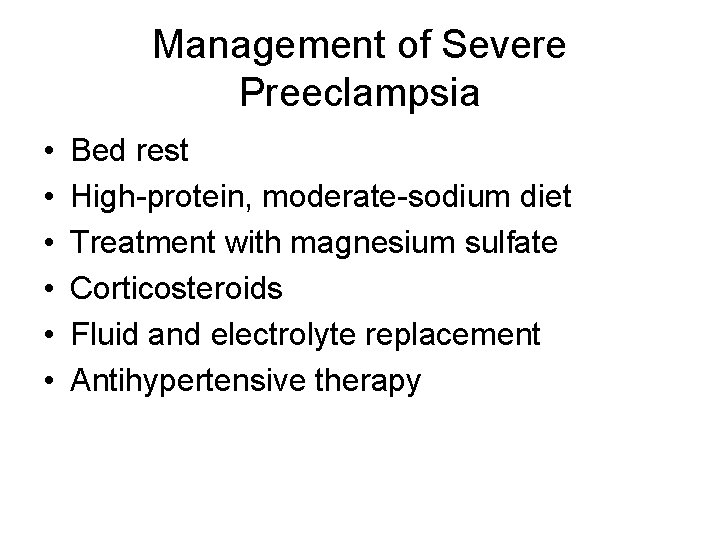
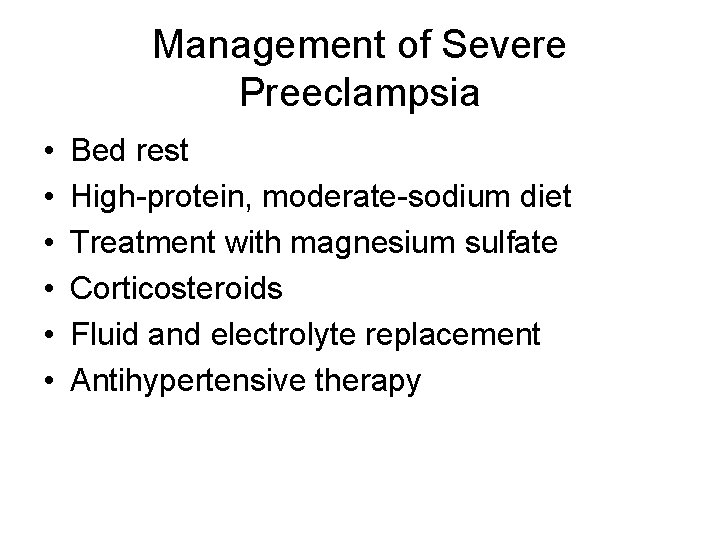
Management of Severe Preeclampsia • • • Bed rest High-protein, moderate-sodium diet Treatment with magnesium sulfate Corticosteroids Fluid and electrolyte replacement Antihypertensive therapy
Fetal Indications for Delivery • Severe IUGR • Nonreassuring fetal surveillance • oligohydramnios

Maternal Indications for Delivery • • Gestational age of 38 weeks or greater Platelet count below 100 K Progressive deterioration of hepatic function Progressive deterioration of renal function Suspected placental abruption Persistent severe headache or visual changes Persistent severe epigastric pain, nausea, or vomiting • eclampsia
Plan of Care for the Preeclamptic • Complete bedrest • Left lying position-increases kidney glomerular function and urine output • Provide darkened quiet room • Limit visitation • Fluid restriction (125 -150 ml/hr) • Seizure precautions • Magnesium sulfate • Antihypertensives
Preeclampsia Assessment • • • Edema DTRs and clonus Assess fluid balance-strict I & O Breath sounds (pulmonary edema) Vital signs: BP, respiratory rate & Sa. O 2 LOC c/o HA or visual disturbances Proteinurea Epigastric pain
Edema • 1+ edema is minimal (2 mm) at pedal and pretibial sites • 2+ (4 mm) edema of lower extrmities is marked • 3+ (6 mm) edema is evident in hands, face, lower abdominal wall and sacrum • 4+ (8 mm) generalized massive edema is evident including ascites from accumulaton of fluid in the peritoneal cavity
Assessment of CNS Changes DTRs and Clonus • DTRs 0 -4+ patellar and brachial 0=no response 1+=low normal 2+=average 3+=brisk 4+=hyperactive
Clonus • Extreme hyperreflexia • Involuntary oscillations that may be seen between flexion and extension when continuous pressure is applied to the sole of the foot • Counted in “beats”
Plan of Care for the Preeclamptic • Magnesium Sulfate: used to prevent or control seizures-it is a CNS depressant and smooth muscle relaxant-increases blood flow to the fetus • It does not treat the BP • Interferes with the release of acetylcholine at the synapses, decreases neuromuscular irritability
Magnesium Sulfate • Loading dose: 4 -6 grams over 15 -30 minutes • Maintenance dose: 1 -2 grams/hour • Therapeutic levels: 4. 8 -9. 6 mg/dl • Always IVPB to mainline • Calcium gluconate available as antidate
Renal Insufficiency • Magnesium sulfate is hazardous to women with severe renal failure and maintenance dose must be reduced
Assessment of Patients on Magnesium Sulfate • BP, pulse, and respiratory status should be monitored at least every 5 minutes with the loading dose, and every 15 minutes while on maintenance • Continued the first 24 hours postpartum to prevent seizures • Monitor I & O 30 ml/hr • Serum levels every 4 -6 hours – therapeutic 4. 8 -9. 6 mg/dl
Side Effects of Mag Sulfate • • • Flushing Sweating Thirst Drying mucous membranes Depression of reflexes Muscle flaccidity Nausea Blurred visoin HA tachycardia
Clinicial Manifestations of Hypermagnesemia • • • • Weakness Paresthesias Dcreased deep tendon reflexes Lethargy, confusion, disorientation Hypoventilatoin Seizures Paralysis Bradyarrythmias Heart block Decreased cardiac contractility Impaired protein synthesis Decreased skeletal mineralization Hepatic dysfunction
Calcium Gluconate • Antidote for mag sulfate • 1 g of 10% calcium gluconate is administered slow IV push over 3 minutes and repeated every hour until signs and sxs of toxicity have been resolved • Should be kept at the bedside
Control of BP • Antihypertensives may be needed to lower the diastolic pressure • This reduces maternal mortality and morbidity associated with left ventricular failure and cerebral hemorrhage • Placental perfusion is controlled by maternal blood pressure, drug must be calibrated carefully
Antihypertensives • If BP reaches 150/100 mm. Hg or higher Labatalol (alpha/beta adrenergic blocker) - Begin with 20 mg IVP slowly over 2 minutes - Or continuous infusion of 1 mg/kg can be used - May double dose up to 80 mg every 15 -20 minutes - Maximum dose 220 mg Apresoline (vasodilator) - Begin with 5 -20 mg infused over 2 -4 minutes - May be repeated every 20 -30 minutes - If no success by 20 mg IV or 30 mg IM try another drug
Eclampsia • Derives from the Greek word meaning “like a flash of lightening” • a condition that seems to strike out of the blue • 75% of the time it occurs intrapartum
Eclampsia • Characterized by seizures or coma • Is a major hazard with poor outcomes in: - gestations of less than 28 weeks - mothers older than 35 years of age - multigravidas - chronic HTN, renal disease or diabetes
Eclampsia • Rare in the Western world because doctors can diagnose the condition in its earliest phase (preeclampsia) and they are constantly on the alert for the warning signs • Earliest signs: drowsiness, HA, dimness of vision, rising BP, protein in the urine, edema, RUQ pain
Etiology • Cerebral vasospasm, hemorrhage or edema, platelet and fibrin clots occlude vasculature leading to seizure • Blood vessels in the uterus go into spasm cutting blood flow to the baby • Spasms lead to kidney failure • Tissues become water-logged because of fluid retention • Hemorrhages happen in the liver • Brain oxygen levels are lowered causing heightened brain sensitivity which shows as seizures
Signs and Symptoms of Impending Seizures • Extreme hypertension – 200/140 not uncommon • Hyperreflexia • 4+ proteinurea • Generalized marked edema • Severe headache with or without visual distrubances
Management of Care During a Seizure • CALL FOR HELP! • Immediate care; Take care of the mother first -patent airway -adequate oxygenation -turn on side to prevent aspiration Magnesium Sulfate administration Assessment of the fetus, birth if threatened Steroid administration if fetal lungs are not mature
PNEUMONIC S E I Z U R E safety establish airway IV bolus zealous observation uterine activity rapid resuscitation evaluate fetus
Postictal State • Central venous pressure monitoring • Establish second indwelling catheter • Blood glucose level to rule out hypogylcemia due to liver not functioning properly • Blood should be available for emergency infusion due to abruptio • Do not leave patient alone
REMEMBER!!! • All medications and therapy are merely temporary measures • Delivery is the only cure
Signs and Symptoms of Eclampsia • • Scotomata Blurred vision Epigastric pain Vomiting Persistent or severe headache Neurologic hyperactivity Pulmonary edema Cyanosis
Management of Eclampsia • • • Assess characteristics of seizure Assess status of the fetus Assess for signs of placental abruption Maintain airway and oxygenation Position on side to avoid aspiration Suction to keep the airway clear
Management of Eclampsia (cont’d) • To prevent injury, raise padded side rails • Administer magnesium sulfate
Postpartum Management • Symptoms usually resolve within 48 hours of birth • Lab abnormalities usually resolve from 7296 hours after birth • Careful assessment continues, mag sulfate may continue to be infused for 1248 hours after the birth • Bleeding must be assessed
Hemorrhage & Hypertension • NO Methergine • Causes vasospasm and increases blood pressure • CONTRAINDICATED in pts with HTN • Use hemabate or cytotec for PPH
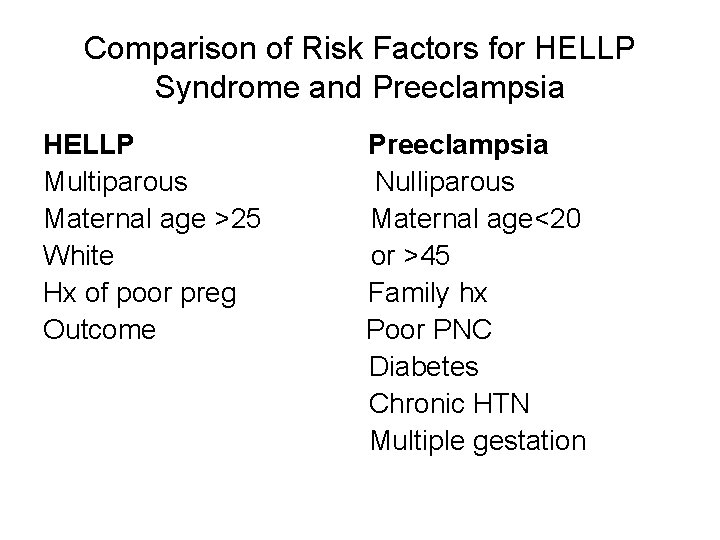
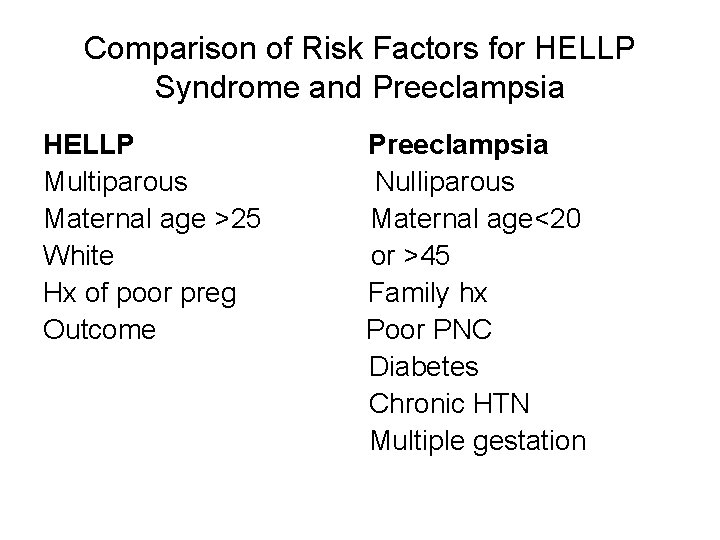
Comparison of Risk Factors for HELLP Syndrome and Preeclampsia HELLP Multiparous Maternal age >25 White Hx of poor preg Outcome Preeclampsia Nulliparous Maternal age<20 or >45 Family hx Poor PNC Diabetes Chronic HTN Multiple gestation
HELLP • Hemolysis, Elevated liver enzymes, Low platelet count • Prevalence is higher among older, white, multiparous women • Carries a mortality rate of 2 -24% • Occurs in 4 -12% of severe preeclampsia
DX • Platelet < 100, 000 • Liver enzymes AST ALT elevated • Evidence of intravascular hemolysis must be present
Complications of HELLP • • Renal failure Pulmonary edema Ruptured liver hematoma DIC Abruptio placenta Fetal death Perinatal asphyxia Maternal death
Sx of HELLP • • Epigastric pain Mailaise Nausea and vomiting Mild jaundice often noted Sound like the flu?
DIC • Prothrombin time, partial thromboplastin time and fibrinogenlevels are normal in patients with HELLP • In a patient with a plasma fibrinogen level of less than 300 mg/d. L, DIC should be suspected, especially if other laboratory abnormalities are also present • Oozing from venipuncture sited, hemorrhage, uterine atony
DIC • Systemic thrombohemorrhagic disorder involving the generation of intravascular fibrin and the consumption of procoagulants and platelets • Causes in pregnancy: abruptio placenta, IUFD with retained dead fetus, AFE, endotoxin sepsis, preeclampsia with HELLP and massive transfusion

TX of DIC • Replacement of volume, blood products, and coagulation components • Cardiovascular and respiratory support • Elimination of underlying triggering mechanism • Anticoagulation • Replace blood products as indicated-packed RBCs, platelets, FFP, cryo • Antithrombin III concentrate • Hematology, transfusionist, critical care consultants.
Treatment for HELLP • Delivery is the only cure • Antenatal administration of dexamethasone (Decadron) 10 mg IV every 12 hours • Mag Sulfate bolus of 4 -6 g as a 20% soln then mainenance of 2 g /hr • Antihypertensive therapy should be initiated if BP > 160/110
Rh Incompatibility • • • Rh – mother, Rh + fetus Maternal Ig. G antibodies produced Hemolysis of fetal red blood cells Rapid production of erythroblasts Hyperbilirubinemia
Administration of Rh Immune Globulin • • After birth of an Rh+ infant After spontaneous or induced abortion After ectopic pregnancy After invasive procedures during pregnancy • After maternal trauma
ABO Incompatibility • Mom is type O • Infant is type A or B • Maternal serum antibodies are present in serum • Hemolysis of fetal red blood cells

Surgery During Pregnancy • Incidence of spontaneous abortion is increased in first trimester • Insert nasogastric tube prior to surgery • Insert indwelling catheter • Encourage patient to use support stockings • Assess fetal heart tones • Position to maximize utero-placental circulation
Trauma During Pregnancy • Greater volume of blood loss before signs of shock • More susceptible to hypoxemia with apnea • Increased risk of thrombosis • DIC • Traumatic separation of placenta • Premature labor
Battering During Pregnancy • • • Psychological distress Loss of pregnancy Preterm labor Low-birth-weight infants Fetal death Increased risk of STIs

Perinatal Infections • • • Toxoplasmosis Rubella Cytomegalovirus Herpes simplex virus Group B streptococcus Human B-19 parvovirus

Fetal Risks: Toxoplasmosis • • • Retinochoroiditis Convulsions Coma Microcephaly Hydrocephalus

Fetal Risks: Rubella • Congenital cataracts • Sensorineural deafness • Congenital heart defects
Fetal Risks: Chlamydia • • • Neurologic complications Anemia Hyperbilirubinemia Thrombocytopenia Hepatosplenomegaly SGA
Fetal Risks: Herpes • Preterm labor • Intrauterine growth restriction • Neonatal infection

Fetal Risks: GBS • • • Respiratory distress or pneumonia Apnea Shock Meningitis Long-term neurologic complications

Fetal Risks: Human B-19 Parvovirus • Spontaneous abortion • Fetal hydrops • Stillbirth
 Menstruation during pregnancy symptoms
Menstruation during pregnancy symptoms Epoxide reaction with grignard reagent
Epoxide reaction with grignard reagent Primary alcohol secondary alcohol
Primary alcohol secondary alcohol Credit risk market risk operational risk
Credit risk market risk operational risk Silbengewicht
Silbengewicht Maximal onset principle example
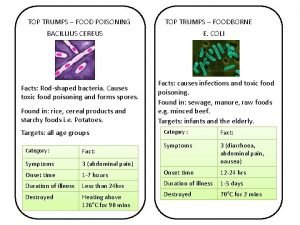
Maximal onset principle example Food poisoning onset
Food poisoning onset Voice onset time
Voice onset time Silbenkern
Silbenkern What are minimal pairs in linguistics
What are minimal pairs in linguistics Coronal consonants
Coronal consonants Marginalization probability
Marginalization probability Continuous subcutaneous infusion
Continuous subcutaneous infusion Gastroenterritis
Gastroenterritis Anaphylaxis onset
Anaphylaxis onset Onset reim beispiel
Onset reim beispiel Nph onset and peak
Nph onset and peak Onset coda and nucleus
Onset coda and nucleus Maternal pelvis and fetal skull
Maternal pelvis and fetal skull Maximal onset principle
Maximal onset principle Abrupt stormy onset
Abrupt stormy onset Onset and coda examples
Onset and coda examples Webtopings
Webtopings Early onset scoliosis classification
Early onset scoliosis classification Onset nucleus coda examples
Onset nucleus coda examples Insulin types
Insulin types Onset offset trial
Onset offset trial Draw rmmm plan
Draw rmmm plan Avoidance risk
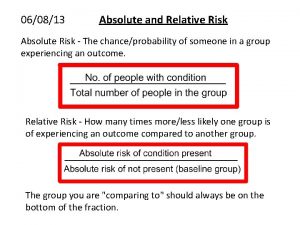
Avoidance risk How to calculate relative risk
How to calculate relative risk Residual risk and secondary risk pmp
Residual risk and secondary risk pmp Ar = ir x cr x dr
Ar = ir x cr x dr Absolute risk vs relative risk
Absolute risk vs relative risk Activity sheet 2: stock market calculations
Activity sheet 2: stock market calculations Classification of risk
Classification of risk Pembelanjaan resiko
Pembelanjaan resiko The biggest risk is not taking any risks
The biggest risk is not taking any risks Key risk indicators financial risk management
Key risk indicators financial risk management Ir x cr x dr
Ir x cr x dr Business risk vs financial risk capital structure
Business risk vs financial risk capital structure Relative risk
Relative risk Risk map risk management
Risk map risk management Relative risk
Relative risk Which risk analysis approach makes use of ale?
Which risk analysis approach makes use of ale? Pregnancy declaration
Pregnancy declaration Sheep pregnancy toxemia
Sheep pregnancy toxemia Virgo pregnancy
Virgo pregnancy Astelazine
Astelazine Chapter 16 lesson 1 the endocrine system
Chapter 16 lesson 1 the endocrine system Tiroid storm
Tiroid storm What is hydrops
What is hydrops Nursing theories related to teenage pregnancy
Nursing theories related to teenage pregnancy Way to prevent teenage pregnancy
Way to prevent teenage pregnancy Folic acid dose in pregnancy
Folic acid dose in pregnancy Epilization
Epilization Anemia in pregnancy guideline
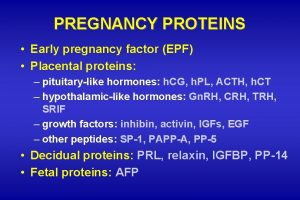
Anemia in pregnancy guideline Early pregnancy factor
Early pregnancy factor Medicolegal importance of delivery
Medicolegal importance of delivery Hormone levels during pregnancy
Hormone levels during pregnancy Hegar's sign
Hegar's sign Modified bishop score
Modified bishop score Post dated pregnancy complications
Post dated pregnancy complications Pregnancy category a
Pregnancy category a Name that
Name that Normal pregnancy definition
Normal pregnancy definition Total bilirubin newborn chart
Total bilirubin newborn chart Side effects of magnesium sulfate in pregnancy
Side effects of magnesium sulfate in pregnancy Causes of teenage pregnancy
Causes of teenage pregnancy Normal ast and alt levels in pregnancy
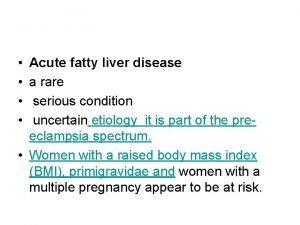
Normal ast and alt levels in pregnancy Acute fatty liver of pregnancy
Acute fatty liver of pregnancy 1 week darkening areola early pregnancy pictures
1 week darkening areola early pregnancy pictures 1 week darkening areola early pregnancy pictures
1 week darkening areola early pregnancy pictures Inj haemaccel uses
Inj haemaccel uses Pregnancy
Pregnancy Episiotomy types
Episiotomy types Icd 10 code for twin pregnancy
Icd 10 code for twin pregnancy Hypothyroidism pregnancy
Hypothyroidism pregnancy Coker definition
Coker definition What is high parity
What is high parity Endoscopy in pregnancy guidelines
Endoscopy in pregnancy guidelines Complete vs incomplete hydatidiform mole
Complete vs incomplete hydatidiform mole Follow up of molar pregnancy
Follow up of molar pregnancy High levels of fibrinogen in pregnancy
High levels of fibrinogen in pregnancy Galactorrhea pregnancy
Galactorrhea pregnancy Biophysical profile score
Biophysical profile score 2232021
2232021 Endocrinology of pregnancy
Endocrinology of pregnancy Dxn spirulina nasa
Dxn spirulina nasa Ioidine
Ioidine Rapiprazole
Rapiprazole Diabetic ketoacidosis anion gap
Diabetic ketoacidosis anion gap Childbirth definition
Childbirth definition Pregnancy mri
Pregnancy mri Trimester breakdown
Trimester breakdown Lightening pregnancy
Lightening pregnancy Prenatal care and adaptations to pregnancy
Prenatal care and adaptations to pregnancy Hormones during pregnancy
Hormones during pregnancy Chapter 20 reproduction and pregnancy
Chapter 20 reproduction and pregnancy Molar pregnancy hcg levels
Molar pregnancy hcg levels Sheep pregnancy toxemia
Sheep pregnancy toxemia Dashod dog
Dashod dog Hypolastic
Hypolastic Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Hispanic cultural views on teenage pregnancy
Hispanic cultural views on teenage pregnancy Stages of implantation pregnancy
Stages of implantation pregnancy Fire hydrant exercise pregnancy
Fire hydrant exercise pregnancy Trimester graphic organizer
Trimester graphic organizer Roxanne borja sex
Roxanne borja sex Causes of post term pregnancy
Causes of post term pregnancy Malaria in pregnancy definition
Malaria in pregnancy definition Malaria in pregnancy definition
Malaria in pregnancy definition Picme2.0
Picme2.0 Position couchée grossesse
Position couchée grossesse Chapter 5 reproducible master a pregnancy vocabulary
Chapter 5 reproducible master a pregnancy vocabulary Antiarrhythmic drugs classification
Antiarrhythmic drugs classification Objectives of teenage pregnancy
Objectives of teenage pregnancy Lack of knowledge in teenage pregnancy
Lack of knowledge in teenage pregnancy Management of allergic rhinitis
Management of allergic rhinitis Dr. parul jahan
Dr. parul jahan Nexdum
Nexdum Acute fatty liver of pregnancy
Acute fatty liver of pregnancy American thyroid association guidelines pregnancy 2017
American thyroid association guidelines pregnancy 2017 Metoprolol svt
Metoprolol svt Pregnancy gestational diabetes mellitus
Pregnancy gestational diabetes mellitus Mtp act
Mtp act Endoderm
Endoderm Fanc
Fanc With whom did shilpi and her husband discuss pregnancy?
With whom did shilpi and her husband discuss pregnancy? Magnesium for preterm labor
Magnesium for preterm labor Horse fetus development
Horse fetus development Prayer point for expectations
Prayer point for expectations Reprotx
Reprotx Prelying
Prelying Calculating insulin dose in pregnancy
Calculating insulin dose in pregnancy Mitchella repens pregnancy
Mitchella repens pregnancy Figo prognostic scoring system gtn
Figo prognostic scoring system gtn Sedilar tablet
Sedilar tablet Chapter 4 prenatal care and adaptations to pregnancy
Chapter 4 prenatal care and adaptations to pregnancy Icd 10 code for ectopic pregnancy
Icd 10 code for ectopic pregnancy Epididymous
Epididymous Clexane dose in pregnancy
Clexane dose in pregnancy Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt What is fetal pole
What is fetal pole Molar pregnancy differential diagnosis
Molar pregnancy differential diagnosis Gpla in pregnancy
Gpla in pregnancy Contraindicated drugs in pregnancy
Contraindicated drugs in pregnancy Nulliparous
Nulliparous A raisin in the sun symbolism
A raisin in the sun symbolism